Abstract
Transcatheter coil embolization is used primarily to treat arterial hemorrhages, tumors, aneurysms, and vascular malformations. However, conventional microcatheter systems cannot always be employed in difficult cases. In this technical note, we describe how small-diameter primary coils and microcatheter tips that are thinner than normal can be used to increase the safety and reliability of coil embolization.
Transcatheter embolization can be performed with the aid of coils, n-butyl cyanoacrylate, detachable balloons, gelatin sponges, polyvinyl alcohol particles, and other embolic materials (e.g., embospheres). Usually, the diameter of the primary coil is 0.018–0.035 inches, and the catheter tip size is 2.0–5.0 F. Transcatheter embolization occasionally requires superselective catheterization, and embolization of only a short segment, to ensure successful endovascular treatment. In some instances, the target arteries may be very thin, and extensively twisted and winding. Other patients may require embolization of short segments and/or tight packing of embolization materials, to prevent development of complications such as organ ischemia or infarction. In this technical note, we describe cases requiring ultraselective and/or short-segment embolization. We used microcoils that were thinner than normal, and small-tipped microcatheters, to treat such patients. Our experience supports the use of these materials. The procedures are technically feasible and are clinically effective alternatives to conventional transcatheter embolization.
Technique
Diagnostic angiography and transcatheter embolization were performed under local anesthesia, with the aid of a flat-panel angiographic imaging system (Innova 4100, General Electric, Milwaukee, Wisconsin, USA). We selected the femoral artery approach and placed a 4.0 F diagnostic catheter (the Shepherd hook or Cobra type, Medikit, Tokyo, Japan) into the main trunk of the target artery. A 1.7 F microcatheter (Excelsior SL-10, Stryker Neurovascular, Fremont, California, USA) was next introduced coaxially over a guidewire 0.014 inches in diameter. We used SilverSpeed (Micro Therapeutics, Irvine, California, USA) or Transend EX (Stryker Neurovascular) guidewires to perform embolizations that could not be achieved using conventional microcatheter systems (e.g., 0.018-inch microcoils and a 2.0 F microcatheter). The embolic agents used were 0.010-inch detachable microcoils (GDC-10 UltraSoft, Stryker Neurovascular or Cerecyte, Codman and Shurtleff, Raynham, Massachusetts, USA). Microcoil diameter and length were selected after consideration of the diameter of the target vessel.
Coil embolization of small-caliber vessels
A 52-year-old male presented with an acute ascending colonic hemorrhage associated with diverticular disease. Conventional transcatheter embolization, attempted after performance of hemostatic clipping via colonoscopy, was initially unsuccessful. Superior mesenteric angiography revealed contrast extravasation from the vasa recta (Fig. 1a). A 1.7 F microcatheter was placed into the distal end of the long branch of the vasa recta (Fig. 1b). Three 0.010-inch detachable coils (Guglielmi Detachable Coils 2 mm×2 cm, 2 mm×3 cm, and 2 mm×6 cm) were placed at the site of extravasation. Superior mesenteric angiography revealed that contrast extravasation ceased after the procedure, and no clinical complication was observed (Fig. 1c). Specifically, the patient did not experience recurrent bleeding, bowel ischemia, or infarction.
Figure 1. a–c.
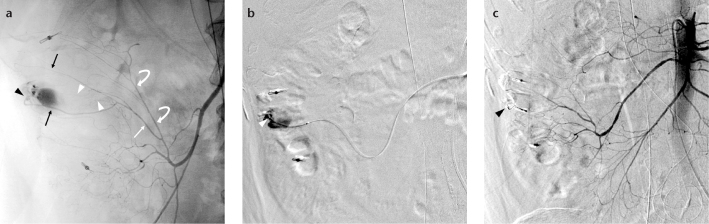
A 52-year-old male presented with an acute ascending colonic hemorrhage after failure of endoscopy. Superior mesenteric angiography (a) showed extravasation at the distal end (black arrowhead) of the vasa recta (white arrow) (long branches, black arrows; short branches, white arrowheads) arising from the marginal artery (curved arrows). A 1.7 F microcatheter was placed into the distal end (the site of bleeding) of the long branch of the vasa recta (b, arrowhead). Three 0.010-inch detachable coils were placed at the site of extravasation. After the procedure, superior mesenteric angiography (c) showed no further contrast extravasation (arrowhead).
A 64-year-old male presented with post-traumatic retroperitoneal hemorrhage. Contrast-enhanced computed tomography revealed a retroperitoneal hematoma and a suspected pseudoaneurysm. Lumbar angiography was used to locate the pseudoaneurysm on the right second branch of the lumbar artery (Fig. 2a). A 1.7 F microcatheter was placed into the distal site of the pseudoaneurysm. Two 0.010-inch detachable coils (Guglielmi Detachable Coils, 2 mm×6 cm) were placed distal and proximal to the pseudoaneurysm (one at either site). Lumbar angiography revealed that contrast extravasation ceased after the procedure (Fig. 2b).
Figure 2. a, b.
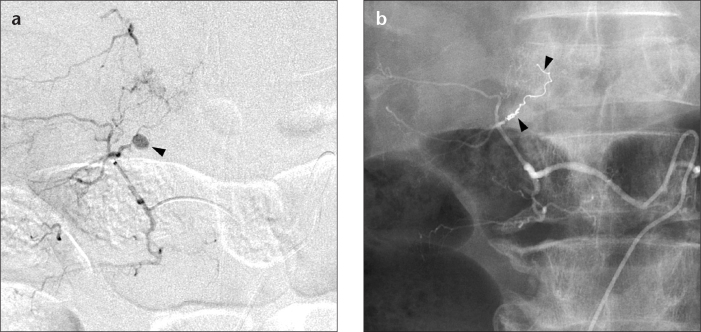
A 64-year-old male presented with post-traumatic retroperitoneal hemorrhage. Lumbar angiography (a) showed a pseudoaneurysm (arrowhead) on the right second branch of the lumbar artery. A 1.7 F microcatheter was placed into the distal site of the pseudoaneurysm. Two 0.010-inch detachable coils were placed distally and proximally (one coil each) to the pseudoaneurysm (b, arrowheads). After the procedure, lumbar angiography showed no further extravasation.
Coil embolization of large-caliber vessels and short vessel segments
A 77-year-old female presented with an aneurysm of the common hepatic artery. Celiac angiography revealed a saccular true common hepatic artery aneurysm (Fig. 3a). Parent artery embolization (at sites distal and proximal to the aneurysm) was performed via placement of 0.018-inch microcoils. Blood flow in the celiac and splenic arteries was preserved by placement and inflation of a microballoon catheter. However, an incomplete proximally located aneurysmal occlusion inhibited blood flow in the parent artery. Celiac angiography performed after embolization showed that coil packing in the region proximal to the aneurysm was relatively loose (Fig. 3b). Further embolization was performed using a 1.7 F microcatheter located proximal to the aneurysmic site to place three 0.010-inch detachable coils (Guglielmi Detachable Coils, 4 mm×4 cm). Celiac (Fig. 3c) and superior mesenteric angiography performed after coil embolization showed that the aneurysm was completely occluded.
Figure 3. a–c.
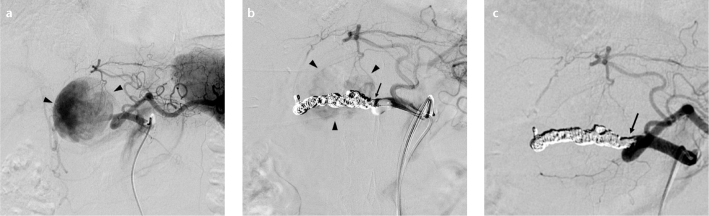
A 77-year-old female presented with an aneurysm of the common hepatic artery. Celiac angiography revealed a saccular true common hepatic artery aneurysm (a, arrowheads) and an incomplete aneurysmal occlusion (b, arrowheads) proximal to the aneurysm. The occlusion became apparent only after parent artery embolization using 0.018-inch microcoils. A 1.7 F microcatheter was placed proximal to the parent artery to allow additional tightly packed embolization (b, c, arrows) using three 0.010-inch detachable coils. Celiac angiography after coil embolization (c) showed complete occlusion of the aneurysm.
Tight packing of a visceral artery aneurysm via coil embolization
An 80-year-old female presented with an aneurysm of the splenic artery. Celiac angiography revealed a saccular true splenic artery aneurysm. During coil embolization with twelve 0.018-inch microcoils using the neck remodeling technique, digital radiography revealed that the microcoils were relatively loosely packed (Fig. 4a; the packing rate was 16%). Additional coil embolization was attempted using a 0.018-inch microcoil. The coil migrated to the splenic artery but was retrieved prior to detachment. Embolization was attempted once more, using seven 0.010-inch detachable coils (Cerecyte microcoils: one 4 mm×10 cm; three 4 mm×8 cm; one 4 mm×6 cm; and two 3 mm×6 cm). The coils did not migrate, rather becoming tightly packed (Fig. 4b; the packing rate was 19%). Celiac angiography performed after coil embolization revealed complete aneurysmal occlusion with preservation of parental arterial circulation.
Figure 4. a, b.
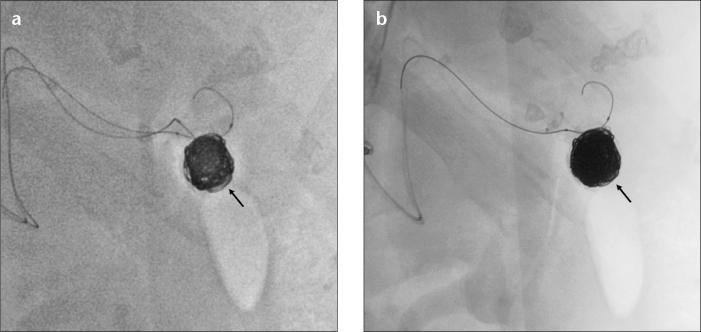
An 80-year-old female presented with a true splenic artery aneurysm. After coil embolization using twelve 0.018-inch microcoils placed via the neck remodeling technique, a digital radiograph (a) showed relatively loose packing (arrow). Additional embolization involved placement of seven 0.010-inch detachable coils (b). The coils did not migrate and were tightly packed (b, arrow).
Discussion
Because it is difficult to selectively insert a 2.0 F microcatheter into a small-caliber vessel, we rather embolized selected target arteries using 0.010-inch microcoils (2 mm in diameter) and 1.7 F microcatheters.
Transcatheter arterial embolization is required to treat active hemorrhages that are resistant to conservative medical management, and when endoscopic therapy is either impossible or unsuccessful. Embolization to treat acute lower gastrointestinal hemorrhages requires superselective catheterization to prevent later development of complications such as intestinal ischemia. Superselective arterial embolization of three or fewer vasa recta yielded relatively acceptable results in this context (1). However, late-onset occlusion or severe stenosis of the gastrointestinal tract sometimes developed at the sites of embolization (2). In the large intestinal wall, the vasa recta has both long and short branches, both of which are rich in anastomoses (3). Embolization must therefore be ultraselective in small-caliber vessels (e.g., vessels of the long branch), and only short segments should be treated whenever possible. Limitation of the area of ultraselective embolization using 0.010-inch detachable coils (2 mm in diameter) successfully preserved blood flow, possibly because of anastomosis of surrounding arteries. Intact short and nonembolized long branches were thus less likely to develop intestinal ischemia or infarction after embolization (4).
Lumbar or intercostal artery embolizations infrequently cause paraplegia, when embolic materials (either particles or liquids) migrate into the spinal artery (5). Embolic coils are less likely to become displaced, and thus afford reliable and safe hemostasis. In most instances of hemorrhage, extravasation and pseudoaneurysms (with vasospasm) develop around the parent artery. Delivery of a catheter to the site of hemorrhage is thus sometimes difficult, particularly if selective insertion of a microcatheter into a site proximal to a pseudoaneurysm is required.
Occasionally, only short segments of large-caliber vessels require coil embolization, to avoid unnecessary treatment. We treated a patient with a large aneurysm of the common hepatic artery; the aneurysm had a relatively wide neck. The usual approach is coil embolization seeking to block both the inflow and outflow of the aneurysmal parent artery (6). We initially used 0.018-inch microcoils, and failed to achieve complete aneurysmal occlusion at sites distal and proximal to embolization. This was because coil packing was relatively loose, and the packed area was short in length, proximal to the aneurysmal parent artery. It was critical to limit the area of embolization, and we used 0.010-inch detachable microcoils to preserve nearby arterial circulation. This illustrated the utility of tight packing and short-segment embolization. We did not encounter any procedural complication.
One treatment option for true visceral artery aneurysms is selective exclusion of the aneurysmic sac using 0.018-inch microcoils, with preservation of parent arterial circulation by employing a neck remodeling technique (7). This has the advantage of preventing organ infarction, but may increase the risk of recanalization/coil compaction. Such risk is elevated when the coil packing density is low (8). The highest level of aneurysmic packing was achieved using initial placement of 0.018-inch, followed by 0.010-inch, microcoils (3 or 4 mm in diameter), particularly at the aneurysmal neck. We recommend that additional coil embolization, using smaller-sized microcoils, be performed when dense endovascular packing is required.
In conclusion, all embolization procedures described in the present technical note were uneventful, and we experienced no difficulties when inserting 1.7 F microcatheters. The 0.010-inch detachable microcoil is of small primary diameter and is highly flexible. We were thus able to control coil movement by slowly pushing the delivery wire back and forth. This allowed us to place tightly overlapping coils when performing embolizations, facilitating treatment of short segments (only) and tight packing of target vessels. Precise catheter placement depends to some extent on the experience level of the clinician, and 0.010-inch detachable coils are relatively expensive. However, our approach is highly efficacious, and we encountered no postprocedural complications.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Jae HJ, Chung JW, Kim HC, et al. Experimental study on acute ischemic small bowel changes induced by superselective embolization of superior mesenteric artery branches with N-butyl cyanoacrylate. J Vasc Interv Radiol. 2008;19:755–763. doi: 10.1016/j.jvir.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 2.Toyoda H, Kumada T, Sone Y, Isogai M, Kaneoka Y. Late-onset colonic occlusion after emergent selective embolization of sigmoid artery with N-butyl cyanoacrylate for life-threatening traumatic bleeding. J Vasc Interv Radiol. 2009;20:1376–1379. doi: 10.1016/j.jvir.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 3.Kachlik D, Baca V, Stingl J. The spatial arrangement of the human large intestinal wall blood circulation. J Anat. 2010;216:335–343. doi: 10.1111/j.1469-7580.2009.01199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koganemaru M, Abe T, Iwamoto R, et al. Ultraselective arterial embolization of vasa recta using 1.7 French microcatheter with small-sized detachable coils in acute colonic hemorrhage after failed endoscopic treatment. AJR Am J Roentgenol. 2012;198:W370–372. doi: 10.2214/AJR.11.7295. [DOI] [PubMed] [Google Scholar]
- 5.Park SJ, Kim CH, Kim JD, et al. Spinal cord injury after conducting transcatheter arterial chemoembolization for costal metastasis of hepatocellular carcinoma. Clin Mol Hepatol. 2012;18:316–320. doi: 10.3350/cmh.2012.18.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Etezadi V, Gandhi RT, Benenati JF, et al. Endovascular treatment of visceral and renal artery aneurysms. J Vasc Interv Radiol. 2011;22:1246–1253. doi: 10.1016/j.jvir.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Uchiyama D, Koganemaru M, Abe T, Hirose Y, Hayabuchi N, Akashi H. Coil embolization of splenic artery aneurysm with preservation of the parent artery using a neck remodelling technique. J Vasc Interv Radiol. 2007;18:447–450. doi: 10.1016/j.jvir.2006.12.727. [DOI] [PubMed] [Google Scholar]
- 8.Yasumoto T, Osuga K, Yamamoto H, et al. Long-term outcomes of coil packing for visceral aneurysms: correlation between packing density and incidence of coil compaction or recanalization. J Vasc Interv Radiol. 2013;24:1798–1807. doi: 10.1016/j.jvir.2013.04.030. [DOI] [PubMed] [Google Scholar]


