We read with great interest the paper published by Guneyli et al. (1) in Diagnostic and Interventional Radiology along with the other impressive papers regarding the use of Amplatzer® Vascular Plugs (AVPs, AGA Medical Corp., Golden Valley, Minnesota, USA) (1–3). We would like to share our experience about using the AVP for treating a rectovaginal fistula (RVF). Although initially successful, this treatment unfortunately failed in the long-term follow-up.
A 47-year-old female patient was referred to our department for interventional radiologic treatment of RVF, which occurred following a low anterior resection for T2N0M0 rectal cancer, performed 10 months ago in another center. On postoperative day 12 the patient suffered vaginal fecal discharge. Initial emergent loop diversion colostomy and primary surgical repair of the fistula six months later, were both unsuccessful. Double-contrast barium enema (Prontobario Colon, Bracco, Milan, Italy) revealed passage of contrast and air from rectum to vagina consistent with RVF, and embolization of the fistula was planned (Fig. 1a).
Figure 1. a–d.
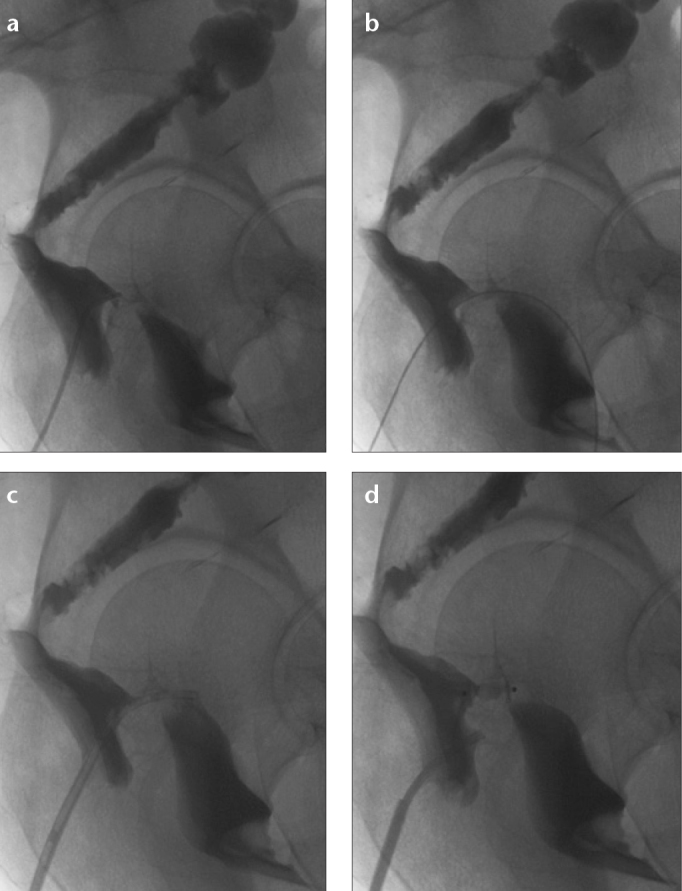
Lateral iodinated contrast study of the colon (a) demonstrates the passage of contrast material from the rectum to vagina through a fistulous tract. Treatment begins with the passage of the wire through the fistula (b). Panel (c) shows catheterization of the fistula tract. Repeat colonography (d) confirms position before deployment of a 12 mm Amplatzer Vascular Plug in the rectovaginal fistula tract.
Under the guidance of a 5 F vertebral catheter (Cordis, Johnson & Johnson, Miami, Florida, USA) and an angled hydrophilic 0.035-inch radiofocus glidewire (Terumo, Somerset, New Jersey, USA) the fistula was catheterized, and the wire accessed into the vaginal lumina. The glidewire was exchanged for a stiff Amplatz guidewire (Cook Medical, Bloomington, Indiana, USA). An 8 F long sheath and a dilator (Shuttle, Cook Medical) were inserted over the exchange wire into the fistula and advanced to the measured area. The dilator and the wire were removed, and angiography was performed through the guiding catheter to confirm satisfactory location of the guiding catheter. An AVP 2 was introduced through the 8 F sheath. While the medial part of the plug was in the fistula, the distal and proximal parts were in the vaginal and rectal walls, respectively (Fig. 1). The plug was deployed following confirmation of the device position. Postembolization angiography revealed occlusion of the fistula. The patient was discharged the next day. The control double-contrast barium enema examination at the first month revealed complete healing and the patient was free of symptoms (Fig. 2). However, the second control imaging performed at the third month, after relapsed complaints of the patient, revealed loss of the plug and reappearance of the fistula. In addition, there was a new blind-ended fistula towards the presacral space (Fig. 3). Although we could not demonstrate direct passage of contrast in to vagina, there was a late slight fluid discharge consistent with contrast material from the vagina.
Figure 2. a,b.
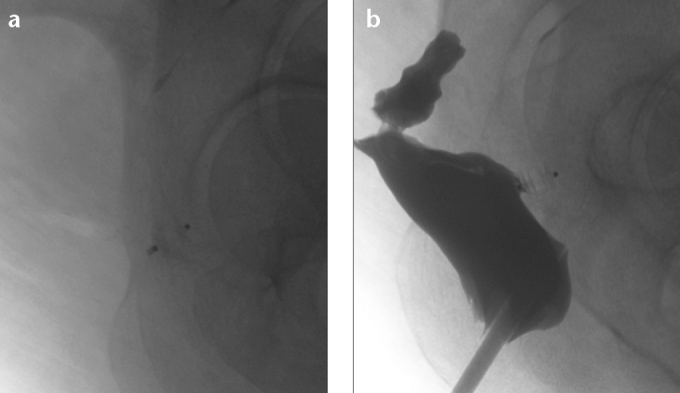
Lateral x-ray image (a) shows the plug in the expected position in the first month follow-up of the patient. Control colonography (b) confirms the unchanged position of the plug and healed fistulous tract.
Figure 3.

Contrast-injected lateral colonography performed at the third month reveals the loss of the plug and a recently developed presacral blind-ended fistulous tract.
First-line treatment options for this patient include palliative colostomy and surgical repair. An alternative method could be the use of an occlusion device designed for nonsurgical treatment of patients with acquired RVF, as reported by Lee et al. (4). Although this device is reported to have a high success rate, there are certain limitations: each device should be constructed according to the diameter and length of the fistula tract and deployed through a 24 F chest tube.
In this letter we present a case of initially succesful nonsurgical technique for RVF treatment. To the best of our knowledge this is the first case in the literature reporting the use of an AVP in RVF. The late-onset failure and loss of AVP might be related to physiological rises in rectal pressure during the passage of stool and regional movements.
Since the introduction of AVPs for use in the cardiovascular system, various applications have been reported in different diseases and organ systems. Their applicability and effectiveness have been proved in numerous vascular diseases along with reports confirming successful use in esophagobronchial, gastrocolonic, and ureterovesical fistulas (1–3).
In conclusion, RVFs are rare complications of various diseases or surgical procedures, and they should be treated immediately for distressing symptoms. The long-term failure of AVP must be kept in mind, when considering treatment options.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Guneyli S, Cinar C, Bozkaya H, Parildar M, Oran I. Applications of the Amplatzer Vascular Plug to various vascular lesions. Diagn Interv Radiol. 2014;20:155–159. doi: 10.5152/dir.2013.13139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cil B, Peynircioğlu B, Canyiğit M, Geyik S, Çiftçi T. Peripheral vascular applications of the Amplatzer vascular plug. Diagn Interv Radiol. 2008;14:35–39. [PubMed] [Google Scholar]
- 3.Young JA, Shimi SM, Alijani A, Patil PV, Bhat R. Occlusion of a neo-esophageal-bronchial fistula using the Amplatzer Vascular Plug 2. Diagn Interv Radiol. 2013;19:259–262. doi: 10.5152/dir.2013.026. [DOI] [PubMed] [Google Scholar]
- 4.Lee BH, Choe DH, Lee JH, et al. Device for occlusion of rectovaginal fistula: clinical trials. Radiology. 1997;203:65–69. doi: 10.1148/radiology.203.1.9122417. [DOI] [PubMed] [Google Scholar]


