Abstract
The adoption of routine prostate specific antigen screening has led to the discovery of many small and low-grade prostate cancers which have a low probability of causing mortality. These cancers, however, are often treated with radical therapies resulting in long-term side effects. There has been increasing interest in minimally invasive focal therapies to treat these tumors. While imaging modalities have improved rapidly over the past decade, similar advances in image-guided therapy are now starting to emerge—potentially achieving equivalent oncologic efficacy while avoiding the side effects of conventional radical surgery. The purpose of this article is to review the existing literature regarding the basis of various focal therapy techniques such as cryotherapy, microwave, laser, and high intensity focused ultrasound, and to discuss the results of recent clinical trials that demonstrate early outcomes in patients with prostate cancer.
Last year in the United States approximately 238 590 men were diagnosed with prostate cancer and 29 720 died as a result of their disease (1). The majority of diagnosed cases represent low-risk, organ-confined disease, and these may be over-treated if conventional treatment methods (i.e., radical prostatectomy and whole-gland external beam radiation therapy) are employed. In this setting, focal therapy has emerged as a treatment alternative that can spare patients from many of the undesired side effects associated with more radical therapies. There is currently a great demand to determine the safest and most effective focal treatment for localized prostate cancer.
Critical to the use of focal therapies is the development of good diagnostic methods that can localize cancer accurately, thereby permitting focal therapy. The effectiveness of prostate specific antigen (PSA) plus multiparametric magnetic resonance imaging (MRI), followed by an MRI/transrectal ultrasonography (MRI/TRUS) biopsy is now well documented, and can be considered a strong alternative to current routine screening practice which includes a digital rectal exam or serum PSA followed by a systematic TRUS-guided biopsy. Utility of this new, image-based approach has been reported in a large patient cohort treated at the National Institutes of Health (Bethesda, Maryland, USA) (2) and externally validated by a recent phase III clinical trial by Rastinehad et al. (3). The era of targeted biopsies has naturally led to the development of focal therapy approaches for prostate cancer.
Several methods of focal therapy using different ablative mechanisms such as cryotherapy, microwave, laser, and high intensity focused ultrasound (HIFU) have been introduced. However, there are limitations and unknowns for each of them. Little evidence is currently available to prove that any one method is more effective than the others over long-term follow-up. Several of these technologies are not yet Federal Drug Administration (FDA) approved, and they are currently undergoing clinical trials to determine their efficacy, safety, and long-term outcomes. As an added barrier, each new ablative technique requires further specialized training of the provider. Each method has its own set of side effects and/or complications. The three most common concerns regarding focal therapy are: oncologic efficacy, sexual potency, and urinary incontinence.
Many patients with low-grade cancers choose active surveillance to monitor their cancers. This includes serial PSA measurements and biopsies. Multiparametric MRI is also increasingly used to monitor patients on active surveillance (4). Unfortunately, many men fall off active surveillance and require some sort of radical therapy. However, until the various focal therapies are proven efficacious in longitudinal studies and it is determined that the “prostate trifecta” (effective cancer treatment, urinary control, and preserved erectile function) can be safely achieved, the dilemma of which treatment to choose will continue to exist for patients and their physicians. In this review, we aim to highlight the history and current status of focal therapy options in prostate cancer, as well as discuss the impact and importance of imaging.
High-intensity focused ultrasound
HIFU is a minimally-invasive procedure in which ultrasound waves are directed to specific pathologic regions and are used to generate high local tissue temperatures that rapidly heat and destroy targeted tissue via coagulative necrosis. The tissue is targeted using ultrasound or MRI, and heated for approximately five seconds up to temperatures of 90°C. The focal ablation pattern of HIFU allows for the specific targeting of a lesion while preserving the surrounding tissue. The total procedure requires 2–4 hours, and side effects have generally been noted to be fewer in comparison to more conventional surgical methods (i.e., radical prostatectomy) (5–8).
The ability of ultrasound waves to cause destruction of human tissue was first suggested in the early 1940s by Lynn et al. (9). By the 1950s, it was realized that this ultrasound technology could be implemented in the ablation of soft-tissue tumors (10). It was not until the 1990s that MRI guidance was first used with HIFU in prostate cancer (11, 12). In 2011, HIFU ablation was still not considered a standard treatment option for localized prostate cancer, likely due to the positive repeat biopsy rates ranging from 4.9%–65%, which resulted in retreatment rates varying 7.7%–43% (13). In a retrospective study by Boutier et al. (14), 99 patients were treated with HIFU using the Ablatherm system (EDAP SA, Lyon, France). The most concerning finding was the development of new cancer foci in sites which were negative prior to HIFU, which occurred in 21% of the sample group (14). In 2013, a 14-year study on 538 patients undergoing HIFU with Ablatherm, Ganzer et al. (15) concluded that HIFU therapy can be an effective and safe treatment option for localized prostate cancer, specifically in those patients with advanced age, low-to-moderate risk, and those who have a life-expectancy of at least 10 years. They reported biochemical disease-free survival rates at five and 10 years as 81% and 61%, respectively. Of the 55.2% of patients with follow-up post-treatment biopsy, 25.6% were confirmed to have cancer. This supported the previous results of the 13-year study by Uchida et al. (16) in which 884 men were treated with HIFU using the Sonublate 500 system (SonaCare Medical, Charlotte, North Carolina, USA) (16). This study showed that biochemical disease-free survival rates in low, intermediate, and high risk groups at five years were 54%, 61%, and 84% and at 10 years were 72%, 58%, and 44%, respectively (Table 1).
Table 1.
Studies published on HIFU in prostate cancer
| Study | Year | No. of patients | Guidance | Notes |
|---|---|---|---|---|
| Boutier et al. (14) | 2011 | 99 | US | Post-HIFU residual cancer in 36.4%. Of these, 41.7% were apical lesions. |
| Ganzer et al. (15) | 2013 | 538 | US | Actuarial BDFS (2 ng/mL):
|
| Lee et al. (7) | 2006 | 58 | US | BDFS at 14 months: (3 patients with PSAs over 1.0 ng/mL):
|
| Uchida et al. (16) | 2012 | 884 | MRI | 10-year BDFS (2 ng/mL):
|
| Ahmed et al. (5) | 2012 | 42 | MRI | No histological evidence of prostate cancer at six months in 30 of 39 patients. After re-treatment in 4 men, 39 of 41 had no evidence on mpMRI. |
US, ultrasonography; HIFU, high intensity focused ultrasound; BDFS, biochemical disease-free survival; PSA, prostate specific antigen; MRI, magnetic resonance imaging; mpMRI, multiparametric magnetic resonance imaging.
Today, MRI-guided HIFU is approved for use in 30 countries using the Sonublate 500 system (17). While it is not U.S. FDA approved, clinical trials are under way for the Sonublate 450 (for the U.S. market), which is being tested in low-risk, organ-confined disease and in recurrent prostate cancer (i.e., failed external beam radiation therapy) (18). The outcome of these trials could further support and expand the use of MRI-guided HIFU as a valid treatment option.
MRI-guided HIFU can be monitored nearly in real-time using quantitative MR thermometry. Accurate readouts of tissue temperature can be read out directly from MRI preventing thermal ablation of key structures like the urethra or neurovascular bundles (8). HIFU can also be directed with MRI-US registration to identify the treatment margins both prior to and during the procedure (19, 20). MRI is also useful in the follow-up of HIFU cases for detecting recurrence. In case of HIFU failure, lesions can be visualized on multi-parametric MRI and can be re-treated. This is of benefit for ensuring complete response to HIFU treatment.
Cryoablation
Cryoablation, also referred to as cryotherapy or cryosurgery, is a thermoablation technique which causes cancer cells to undergo coagulative necrosis by means of rapid cycles of freezing and thawing. Cryoablation has its roots in the 1850s, when James Arnott first used ice-salt mixtures to treat cancers (21). This method was later modernized by Irving Cooper in the 1960s with the use of liquid nitrogen. Liquid nitrogen, stored at a pressure of 22 psi, can cool tissue temperatures to as low as −196°C (22). Cells do not die by freezing but are destroyed by thawing in which rapid thermal expansion results in the formation of lethal ice crystals. Today, the technique of cryotherapy has been improved by more rapidly controlling freezing and thawing. By using argon gas, cryoprobe tips can reach temperatures of −187°C and then by rapidly exchanging helium into the probe, a thawing cycle can be created where the tip is rapidly reheated to a temperature of 67°C (23). During freezing the middle of the “iceball”, located at the tip of the probe is considered the most effective region for therapy with temperatures reaching −20°C to −50°C. In order to fully treat the margins of the tumor the iceball needs to extend beyond the border of the tumor (24). The use of advanced imaging is vital in cryoablation, specifically MR thermometry. On MRI, the iceball can be seen as a signal void due to the absence of free hydrogen atoms in frozen water. This allows the operator to determine the distance and extent of the treatment coverage.
Cryotherapy is still minimally used in focal therapy (6% of urologists, and under 25 procedures on average per year) (25, 26), and the long-term outcomes have not yet been determined. In 2002, a large seven-year multicenter trial of cryosurgical ablation of the prostate (CSAP) was reported by Bahn et al. (27) who concluded that patients treated with CSAP compare favorably to those who have undergone radiotherapy. The seven-year actuarial biochemical disease-free survival for low-, moderate, and high-risk were reported as 87%, 79%, and 71%, respectively with a threshold PSA of 1.0 ng/mL. At the five-year time-point, impotence rates were significantly higher (93%) when compared with radiotherapy (37%–70%) (28). On the other hand, bowel and rectal disturbances were minimized with CSAP and worse with radiotherapy. The same study showed biochemical disease-free survival ranging between 45%–76% for a threshold PSA of 1.0 ng/mL, and positive post-CSAP biopsy rates of 18% during the follow-up period. A five-year outcome study by Potosky et al. (29) included 286 men and reported impotency rates of 63.5% after external beam radiotherapy alone.
Like MRI-guided HIFU, cryotherapy can be repeated if required, and may be used in patients who cannot or opt not to undergo surgery or whole-gland radiation therapy (Fig. 1). However, clinical trials are still needed for more widespread acceptance and advancement of the technique as a focal therapy option.
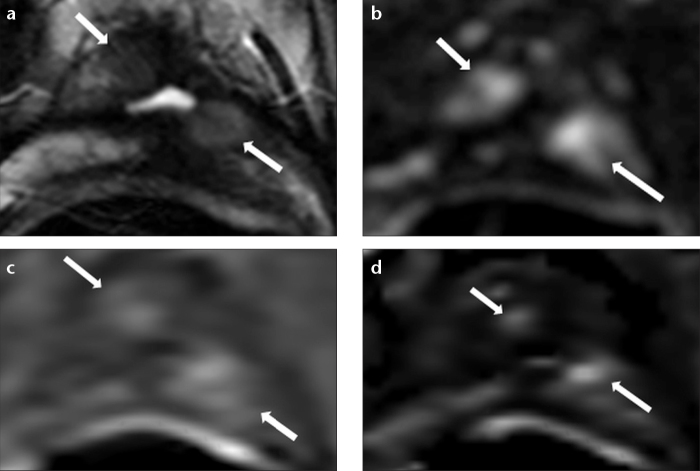
Figure 1. a–d.
A 71-year-old male with PSA recurrence after cryoablation for prostate cancer eight years ago. Axial T2-weighted MRI (a) shows two poorly defined distinct hypointense regions (arrows). Diffusion-weighted MRI (b=2000) (b) demonstrates hyperintense features within these two suspicious areas (arrows). Dynamic contrast-enhanced (DCE) MRI (c) shows hyperenhancement within these lesions (arrows). Wash out map (d) derived from DCE MRI also confirms these findings (arrows). MRI/TRUS fusion guided biopsy revealed residual/recurrent prostate cancer within these two lesions.
Stereotactic body radiotherapy/CyberKnife
In stereotactic body radiotherapy (SBRT) high doses of radiation are given to targeted tumor areas. The radiation can be given as one large dose, or the doses may be fractionated into several doses. SBRT is another advanced therapy most well known as the CyberKnife (Accuray, Sunnyvale, California, USA). The inventor and founder, John Adler had initially worked with Lars Leksell, the inventor of the Gamma Knife (Elekta, Stockholm, Sweden), used in stereotactic radiotherapy for neurosurgery, but sought to come up with a new technique which could be used for the treatment of the whole body (30). The technology was created in 1994 at Stanford University. By 2001 it was FDA approved, and in the following year, the first case of prostate cancer was treated (31, 32).
In SBRT, image guidance is used to more accurately direct radiation than is possible with traditional external beam radiation therapy. SBRT also expanded the use of hypofractionation, which was initially highly controversial but proved to be comparable to brachytherapy and external beam radiation in side effects and efficacy (33–38). The CyberKnife is currently being tested against conventional surgical methods (i.e., prostatectomy) in a phase III clinical trial (PACE study) (39). The results of this study will bring us one step closer to determining if CyberKnife can be considered a standard option in focal cancer therapy. Most recently, MacDougall et al. (40) have discussed the results of six patients in which CyberKnife was compared against the Rapidarc system (Varian Medical Systems, Palo Alto, California, USA). The results were not convincing in either direction. While the Rapidarc is faster, and a gantry-based system, it required a 66% larger margin around the target area (whole prostate) when compared with the CyberKnife (5 mm vs. 3 mm) to achieve similar dosimetry. The CyberKnife, while slower and non-gantry based, maintains better accuracy and precision (1 mm) as a result of its real-time fiducial motion tracking system. Regardless of which technique is ultimately used, MRI and CT imaging will be used during the planning, treatment, and follow-up for these patients.
Focal laser ablation
Focal laser ablation (FLA) is a thermo-ablation technique which utilizes high-energy laser light to generate coagulation through rapid heating of targeted tissue. Laser ablation for prostate cancer was first attempted in 1982 using the neodymium-doped yttrium aluminum garnet laser (Nd:YAG) (41, 42). Today, FLA is also referred to as laser interstitial thermotherapy, and a 980 nm diode laser is utilized, such as the one used in the Visualase system (Visualase, Houston, Texas, USA) (43, 44). Since 2010, MRI-guided FLA has been studied with a 1.5 Tesla (T) canine model, and a 3.0 T human cadaveric model, both concurring on its feasibility (45, 46). This was followed up with the successful treatment of two patients using in-bore MRI-guided FLA, both of whom were monitored via MR thermometry; an added benefit of MRI guidance—which is also used during cryoablation (44). In 2013, the results of two phase I studies on MRI-guided FLA were reported to further validate this therapy. Nine patients were treated by Oto et al. (47); six months after FLA, seven of these nine patients showed no signs of cancer at the site of ablation, while two cases showed a recurrence of low-risk (Gleason 6) disease. Nearly identical results (∼75% targeted tumor ablation rate) were reported by Lindner et al. (48). In this phase I study, 38 men were treated with MRI-guided FLA (using MR thermometry for monitoring) and showed minimal complications after a year of post-treatment follow-up. The most concerning outcome was that 26% of these MRI-guided FLA treated patients showed a positive biopsy at the four-month follow-up in a site other than the ablated region (48). While these results are pointing in the right direction, it is important that larger, long term trials validate these findings (Fig. 2).
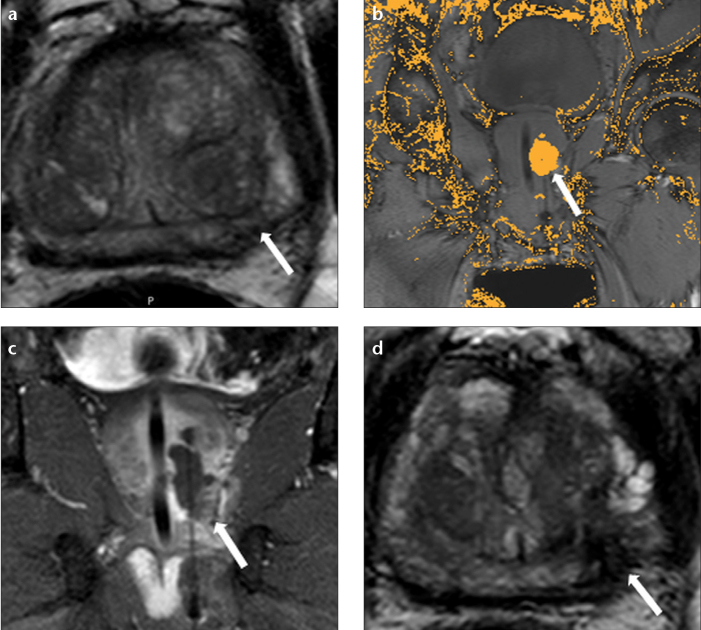
Figure 2. a–d.
A 63-year-old male presenting with an elevated PSA of 12.40 ng/mL. Axial T2-weighted MRI (a) shows a hypointense lesion in the left apical peripheral zone (arrow). TRUS/MRI fusion guided biopsy revealed Gleason 3+3 cancer within this lesion. Patient underwent focal laser ablation under MRI guidance; real-time intra-operative coronal MRI (b) shows the extent of the laser ablation area (arrow). Coronal contrast-enhanced fat-saturated T1-weighted MRI (c) shows necrosis within the laser ablated lesion (arrow). One-year follow-up axial T2-weighted MRI (d) shows necrosis within the treated lesion (arrow).
Low-energy direct current/NanoKnife
Low-energy direct current (LEDC) is a nonthermal ablation technique for prostate cancer which is now under development as the NanoKnife (AngioDynamics, Latham, New York, USA). This technology, also referred to as irreversible electroporation, uses short pulses of electrical current to puncture the cell membrane which ultimately leads to cellular death. The NanoKnife was invented by Gary Onik, who was also one of the first to use US-guidance for CSAP (49). LEDC has been tested preclinically in canines by Tsivian and Polascik (50) at the Duke Cancer Institute (Durham, North Carolina, USA). The team used TRUS guidance, and assessed the side-effects and outcomes of irreversible electroporation therapy. The most common side-effect was hematuria in 10 of 12 dogs, which resolved within three days. The most severe side-effect was loss of erectile function in all 12 dogs, but this resolved between four to 25 days post-ablation in all animals. Upon prostatectomy, histological examination revealed that there was no injury to the capsule, urethra, rectal wall, or nervous tissue. While the preclinical results are promising, human clinical trials are just getting underway. In June 2013, the U.S. FDA granted an Investigational Device Exemption for the NanoKnife device (51) for use in prostate cancer. This enabled the first pilot study to be started with an initial estimated enrollment of six patients. For the procedure, US-guidance is utilized in a method known as three-dimensional prostate mapping biopsy. Post-ablation follow up evaluation is then done using MRI (52). It will be several years before a consensus can be reached on whether LEDC can be offered as an effective option in prostate cancer focal therapy (Table 2).
Table 2.
Studies published on cryoablation, stereotactic body radiation therapy, focal laser ablation and low-energy direct current in prostate cancer
| Study | Year | Therapy | No. of patients | Guidance | Notes |
|---|---|---|---|---|---|
| Bahn et al. (27) | 2002 | CSAP | 975 | TRUS | 7-year BDFS (1.0 ng/mL):
|
| MacDougall et al. (40) | 2014 | SBRT | 6 | CT/MRI |
|
| Oto et al. (47) | 2013 | FLA | 9 | MRI | Recurrence on biopsy within six months in 2 of 9 patients. |
| Lindner et al. (48) | 2013 | FLA | 38 | MRI | Positive follow-up biopsy on opposite side of lesion in 26% of patients. |
| Tsivian and Polascik (50) | 2013 | LEDC (canine) | 12 | TRUS | Hematuria in 10 of 12 dogs, all subsided within three days. Loss of potency in all 12 dogs, but all recovered within 25 days. |
| Angiodynamics (52) | 2016 | LEDC | 6 | 3D-PMB | Currently underway |
CSAP, cryosurgical ablation of the prostate; TRUS, transrectal ultrasonography; BDFS, biochemical disease-free survival; SBRT, stereotactic body radiation therapy; CT, computed tomography; MRI, magnetic resonance imaging; FLA, focal laser ablation; LEDC, low-energy direct current; 3D-PMB, three-dimensional prostate mapping biopsy.
Radiofrequency ablation
Radiofrequency ablation (RFA) is a minimally invasive treatment in which electrodes are inserted into the tumor using a transperineal approach. A high-frequency electrical current is then passed through the electrode to induce thermal damage of the targeted tissue. There is limited literature regarding the use of radiofrequency ablation in prostate cancer. A pilot study with an enrollment of five patients (NCT01423006) has been completed in 2013 to evaluate the efficacy of RFA in low-risk organ-confined disease, for which the results are to be published (53). The most important step, electrode placement, is dependent on MRI and/or US guidance. Based on the outcome of this pilot study, a larger study will be needed to demonstrate safety and efficacy.
Conclusion
There are roughly 12 million cancer survivors in the United States, and 2.8 million of them are men living with prostate cancer. This is a result of improved screening and early detection, improved active surveillance methods, and more effective treatment options. As image-guided focal therapy methods continue to improve, the number of survivors will continue to increase. It has been over 30 years since Steyn and Smith first imaged the prostate using nuclear magnetic resonance imaging (54, 55). At the time they were comparing the 0.4 T, T1 system against the first generation CT scans. Today, the 3.0 T MRI is considered the gold standard, and T2-weighted MRI has been established as the “bread and butter” of prostate anatomical imaging. It is also shown with various studies in literature that our diagnostic ability has been improved with the use of multiparametric MRI. The modern multi-parametric MRI consists of T2-weighted diffusion-weighted imaging with “high b value”, dynamic contrast-enhanced (DCE) MRI, and MR spectroscopy (56–60). Of these, DCE MRI has proven most useful in detecting recurrence after focal therapy. A study by Del Vescovo et al. (61) in a group of 25 patients, showed that after HIFU therapy, DCE MRI showed 100% sensitivity and 96% specificity for recurrence.
Using MRI for guidance, a variety of minimally invasive methods could be of potential value in prostate cancer. Most notably these include HIFU, cryoablation, SBRT, FLA, LEDC, and RFA. Other methods are under development. At this point it is difficult to identify the superior method; each has its advantages and disadvantages. While there is an a la carte of focal therapy options, the ultimate decision on the best method, if in fact one is best, will await larger multi-institutional studies that seek to determine the side effects and efficacy of each method.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1. Prostate Cancer Home Page. Available at: http://www.cancer.gov/cancertopics/types/prostate. Accessed March 17, 2014.
- 2.Rais-Bahrami S, Siddiqui MM, Turkbey B, et al. Utility of multiparametric magnetic resonance imaging suspicion levels for detecting prostate cancer. J Urol. 2013;190:1721–1727. doi: 10.1016/j.juro.2013.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rastinehad AR, Turkbey B, Salami SS, et al. Improving Detection of Clinically Significant Prostate Cancer: MRI/TRUS Fusion-Guided Prostate Biopsy. J Urol. 2014;191:1749–1754. doi: 10.1016/j.juro.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rais-Bahrami S, Turkbey B, Grant KB, Pinto PA, Choyke PL. Role of multiparametric magnetic resonance imaging in the diagnosis of prostate cancer. Curr Urol Rep. 2014;15:387. doi: 10.1007/s11934-013-0387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmed HU, Hindley RG, Dickinson L, et al. Focal therapy for localised unifocal and multifocal prostate cancer: a prospective development study. Lancet Oncol. 2012;13:622–632. doi: 10.1016/S1470-2045(12)70121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uchida T, Ohkusa H, Yamashita H, et al. Five years experience of transrectal high-intensity focused ultrasound using the Sonablate device in the treatment of localized prostate cancer. Int J Urol. 2006;13:228–233. doi: 10.1111/j.1442-2042.2006.01272.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee HM, Hong JH, Choi HY. High-intensity focused ultrasound therapy for clinically localized prostate cancer. Prostate Cancer Prostatic Dis. 2006;9:439–443. doi: 10.1038/sj.pcan.4500901. [DOI] [PubMed] [Google Scholar]
- 8.Napoli A, Anzidei M, De Nunzio C, et al. Real-time magnetic resonance-guided high-intensity focused ultrasound focal therapy for localised prostate cancer: preliminary experience. Eur Urol. 2013;63:395–398. doi: 10.1016/j.eururo.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Lynn JG, Zwemer RL, Chick AJ. The biological application of focused ultrasonic waves. Science. 1942;96:119–120. doi: 10.1126/science.96.2483.119. [DOI] [PubMed] [Google Scholar]
- 10.Bradley WG., Jr MR-guided focused ultrasound: a potentially disruptive technology. J Am Coll Radiol. 2009;6:510–513. doi: 10.1016/j.jacr.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Hynynen K, Damianou C, Darkazanli A, Unger E, Schenck JF. The feasibility of using MRI to monitor and guide noninvasive ultrasound surgery. Ultrasound Med Biol. 1993;19:91–92. doi: 10.1016/0301-5629(93)90022-g. [DOI] [PubMed] [Google Scholar]
- 12.Cline HE, Hynynen K, Watkins RD, et al. Focused US system for MR imaging-guided tumor ablation. Radiology. 1995;194:731–737. doi: 10.1148/radiology.194.3.7862971. [DOI] [PubMed] [Google Scholar]
- 13.So AI. HIFU ablation is not a proven standard treatment for localized prostate cancer. Can Urol Assoc J. 2011;5:424–426. doi: 10.5489/cuaj.11232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boutier R, Girouin N, Cheikh AB, et al. Location of residual cancer after transrectal high-intensity focused ultrasound ablation for clinically localized prostate cancer. BJU Int. 2011;108:1776–1781. doi: 10.1111/j.1464-410X.2011.10251.x. [DOI] [PubMed] [Google Scholar]
- 15.Ganzer R, Fritsche HM, Brandtner A, et al. Fourteen-year oncological and functional outcomes of high-intensity focused ultrasound in localized prostate cancer. BJU Int. 2013;112:322–329. doi: 10.1111/j.1464-410X.2012.11715.x. [DOI] [PubMed] [Google Scholar]
- 16.Uchida T, Tomonaga T, Shoji S, Kim H, Nagata Y. High-intensity focused ultrasound (HIFU) using Sonablate devices for the treatment of localized prostate cancer: 13-year experience. AIP Conf Proc. 2012;1:293–299. [Google Scholar]
- 17. Sonablate 500. Available at: http://sonacaremedical.com/sonablate-500-high-intensity-focused-ultrasound. Accessed February 10, 2014.
- 18. Sonablate 450 Regulatory Status. Available at: http://sonacaremedical.com/sonablate-450-regulatory-status. Accessed February 10, 2014.
- 19.Dickinson L, Hu Y, Ahmed HU, et al. Image-directed, tissue-preserving focal therapy of prostate cancer: a feasibility study of a novel deformable magnetic resonance-ultrasound (MR-US) registration system. BJU Int. 2013;112:594–601. doi: 10.1111/bju.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Partanen A, Yerram NK, Trivedi H, et al. Magnetic resonance imaging (MRI)-guided transurethral ultrasound therapy of the prostate: a preclinical study with radiological and pathological correlation using customised MRI-based moulds. BJU Int. 2013;112:508–516. doi: 10.1111/bju.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper SM, Dawber RPR. The history of cryosurgery. J R Soc Med. 2001;94:196–201. doi: 10.1177/014107680109400416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Copper IS. Cryogenic surgery: a new method of destruction or extirpation of benign or malignant tissues. N Engl J Med. 1963;268:743–749. doi: 10.1056/NEJM196304042681401. [DOI] [PubMed] [Google Scholar]
- 23.De La Taille A, Benson MC, Bagiella E, et al. Cryoablation for clinically localized prostate cancer using an argon-based system: complication rates and biochemical recurrence. BJU Int. 2000;85:281–286. doi: 10.1046/j.1464-410x.2000.00456.x. [DOI] [PubMed] [Google Scholar]
- 24.Tatli S, Acar M, Tuncali K, Morrison PR, Silverman S. Percutaneous cryoablation techniques and clinical applications. Diagn Interv Radiol. 2010;16:90–95. doi: 10.4261/1305-3825.DIR.1922-08.0. [DOI] [PubMed] [Google Scholar]
- 25.O’Leary MP, Baum NH, Bohnert WW, et al. 2003 American Urological Association Gallup survey: physician practice patterns, cryosurgery/brachytherapy, male infertility, female urology and insurance/professional liability. J Urol. 2004;171:2363–2365. doi: 10.1097/01.ju.0000127745.26501.5e. [DOI] [PubMed] [Google Scholar]
- 26.O’Leary MP, Baum NH, Blizzard R, et al. 2001 American Urological Association Gallup Survey: changes in physician practice patterns, satisfaction with urology, and treatment of prostate cancer and erectile dysfunction. J Urol. 2002;168:649–652. doi: 10.1016/s0022-5347(05)64706-4. [DOI] [PubMed] [Google Scholar]
- 27.Bahn DK, Lee F, Badalament R, Kumar A, Greski J, Chernick M. Targeted cryoablation of the prostate: 7-year outcomes in the primary treatment of prostate cancer. Urology. 2002;60:3–11. doi: 10.1016/s0090-4295(02)01678-3. [DOI] [PubMed] [Google Scholar]
- 28.Long JP, Bahn D, Lee F, Shinohara K, Chinn DO, Macaluso JN., Jr Five-year retrospective, multi-institutional pooled analysis of cancer-related outcomes after cryosurgical ablation of the prostate. Urology. 2001;57:518–523. doi: 10.1016/s0090-4295(00)01060-8. [DOI] [PubMed] [Google Scholar]
- 29.Potosky AL, Davis WW, Hoffman RM, et al. Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: the prostate cancer outcomes study. J Natl Cancer Inst. 2004;96:1358–1367. doi: 10.1093/jnci/djh259. [DOI] [PubMed] [Google Scholar]
- 30.Adler JR, Jr, Chang SD, Murphy MJ, Doty J, Geis P, Hancock SL. The Cyberknife: a frameless robotic system for radiosurgery. Stereotact Funct Neurosurg. 1997;69:124–128. doi: 10.1159/000099863. [DOI] [PubMed] [Google Scholar]
- 31. History of the Stanford CyberKnife. Available at: http://stanfordhospital.org/clinicsmedServices/COE/cyberknife/history.html. Accessed March 17, 2014. [Google Scholar]
- 32.King CR, Lehmann J, Adler JR, Hai J. CyberKnife radiotherapy for localized prostate cancer: rationale and technical feasibility. Technol Cancer Res Treat. 2003;2:25–30. doi: 10.1177/153303460300200104. [DOI] [PubMed] [Google Scholar]
- 33.Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999;43:1095–1101. doi: 10.1016/s0360-3016(98)00438-6. [DOI] [PubMed] [Google Scholar]
- 34.Lee WR. Prostate cancer and the hypofractionation hypothesis. J Clin Oncol. 2013;31:3849–3851. doi: 10.1200/JCO.2013.52.4942. [DOI] [PubMed] [Google Scholar]
- 35.Ju AW, Wang H, Oermann EK, et al. Hypofractionated stereotactic body radiation therapy as monotherapy for intermediate-risk prostate cancer. Radiat Oncol. 2013;8:30. doi: 10.1186/1748-717X-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lloyd-Davies RW, Collins CD, Swan AV. Carcinoma of prostate treated by radical external beam radiotherapy using hypofractionation. Twenty-two years’ experience (1962–1984) Urology. 1990;36:107–111. doi: 10.1016/0090-4295(90)80207-4. [DOI] [PubMed] [Google Scholar]
- 37.King CR, Brooks JD, Gill H, Pawlicki T, Cotrutz C, Presti JC., Jr Stereotactic body radiotherapy for localized prostate cancer: interim results of a prospective phase II clinical trial. Int J Radiat Oncol Biol Phys. 2009;73:1043–1048. doi: 10.1016/j.ijrobp.2008.05.059. [DOI] [PubMed] [Google Scholar]
- 38.King CR, Brooks JD, Gill H, Presti JC., Jr Long-term outcomes from a prospective trial of stereotactic body radiotherapy for low-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82:877–882. doi: 10.1016/j.ijrobp.2010.11.054. [DOI] [PubMed] [Google Scholar]
- 39. Prostate advances in comparative evidence. Available at: http://www.clinicaltrials.gov/ct2/show/NCT01584258. Accessed March 17, 2014.
- 40.MacDougall ND, Dean C, Muirhead R. Stereotactic body radiotherapy in prostate cancer: is rapidarc a better solution than cyberknife? Clin Oncol (R Coll Radiol) 2014;26:4–9. doi: 10.1016/j.clon.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 41.Sander S, Beisland HO, Fossberg E. Neodymion YAG laser in the treatment of prostatic cancer. Urol Res. 1982;10:85–86. doi: 10.1007/BF00262408. [DOI] [PubMed] [Google Scholar]
- 42.Sander S, Beisland HO. Laser in the treatment of localized prostatic carcinoma. J Urol. 1984;132:280–281. doi: 10.1016/s0022-5347(17)49592-9. [DOI] [PubMed] [Google Scholar]
- 43. Visualase image-guided thermal laser ablation technology in urology. Available at: http://www.visualaseinc.com/prostate-focal-ablation/. Accessed March 17, 2014.
- 44.Raz O, Haider MA, Davidson SR, et al. Real-time magnetic resonance imaging-guided focal laser therapy in patients with low-risk prostate cancer. Eur Urol. 2010;58:173–177. doi: 10.1016/j.eururo.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 45.Stafford RJ, Shetty A, Elliott AM, et al. Magnetic resonance guided, focal laser induced interstitial thermal therapy in a canine prostate model. J Urol. 2010;184:1514–1520. doi: 10.1016/j.juro.2010.05.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Woodrum DA, Gorny KR, Mynderse LA, et al. Feasibility of 3.0T magnetic resonance imaging-guided laser ablation of a cadaveric prostate. Urology. 2010;75:1514.e1–e6. doi: 10.1016/j.urology.2010.01.059. [DOI] [PubMed] [Google Scholar]
- 47.Oto A, Sethi I, Karczmar G, et al. MR imaging-guided focal laser ablation for prostate cancer: phase I trial. Radiology. 2013;267:932–40. doi: 10.1148/radiol.13121652. [DOI] [PubMed] [Google Scholar]
- 48.Lindner U, Davidson S, Fleshner N, et al. Initial results of MR guided laser focal therapy for prostate cancer. J Urol. 2013;189:e227–e8. [Google Scholar]
- 49.Onik GM, Cohen JK, Reyes GD, Rubinsky B, Chang Z, Baust J. Transrectal ultrasound-guided percutaneous radical cryosurgical ablation of the prostate. Cancer. 1993;72:1291–1299. doi: 10.1002/1097-0142(19930815)72:4<1291::aid-cncr2820720423>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 50.Tsivian M, Polascik TJ. Bilateral focal ablation of prostate tissue using low-energy direct current (LEDC): a preclinical canine study. BJU Int. 2013;112:526–530. doi: 10.1111/bju.12227. [DOI] [PubMed] [Google Scholar]
- 51. FDA grants prostate IDE approval for AngioDynamics’ NanoKnife system. Available at: http://investors.angiodynamics.com/releasedetail.cfm?Release-ID=772028. Accessed March 17, 2014.
- 52. Pilot study of NanoKnife for ablation of prostate cancer in low risk patients. Available at: http://clinicaltrials.gov/show/NCT01972867. Accessed March 17, 2014.
- 53. Pilot Study on focal prostate radio-frequency ablation. Available at: http://clinicaltrials.gov/show/NCT01423006. Accessed March 17, 2014.
- 54.Steyn JH, Smith FW. Nuclear magnetic resonance imaging of the prostate. Br J Urol. 1982;54:726–728. doi: 10.1111/j.1464-410x.1982.tb13634.x. [DOI] [PubMed] [Google Scholar]
- 55.Steyn JH, Smith FW. Nuclear magnetic resonance (NMR) imaging of the prostate. Br J Urol. 1984;56:679–681. doi: 10.1111/j.1464-410x.1984.tb06145.x. [DOI] [PubMed] [Google Scholar]
- 56.Turkbey B, Mani H, Shah V, et al. Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol. 2011;186:1818–1824. doi: 10.1016/j.juro.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Turkbey B, Pinto PA, Mani H, et al. Prostate cancer: value of multiparametric MR imaging at 3 T for detection--histopathologic correlation. Radiology. 2010;255:89–99. doi: 10.1148/radiol.09090475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosenkrantz AB, Hindman N, Lim RP, et al. Diffusion-weighted imaging of the prostate: Comparison of b1000 and b2000 image sets for index lesion detection. J Magn Reson Imaging. 2013;38:694–700. doi: 10.1002/jmri.24016. [DOI] [PubMed] [Google Scholar]
- 59.Yagci AB, Ozari N, Aybek Z, Duzcan E. The value of diffusion-weighted MRI for prostate cancer detection and localization. Diagn Interv Radiol. 2011;17:130–134. doi: 10.4261/1305-3825.DIR.3399-10.1. [DOI] [PubMed] [Google Scholar]
- 60.Turkbey B, Bernardo M, Merino MJ, Wood BJ, Pinto PA, Choyke PL. MRI of localized prostate cancer: coming of age in the PSA era. Diagn Interv Radiol. 2012;18:34–45. doi: 10.4261/1305-3825.DIR.4478-11.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Del Vescovo R, Pisanti F, Russo V, et al. Dynamic contrast-enhanced MR evaluation of prostate cancer before and after endorectal high-intensity focused ultrasound. Radiol Med. 2013;118:851–862. doi: 10.1007/s11547-012-0876-9. [DOI] [PubMed] [Google Scholar]