Abstract
PURPOSE
We aimed to evaluate the frequency and features of dual left anterior descending artery (LAD) variants using computed tomography (CT) angiography.
METHODS
A total of 1337 consecutive coronary CT angiography examinations performed between April 2010 and December 2013 were retrospectively evaluated for the presence of dual LAD. CT examinations were performed with either 64- or 320-row multidetector CT scanners. All CT angiography images were evaluated for the presence and morphologic features of dual LAD subtypes.
RESULTS
Fifty-six dual LAD variations (4%) were identified in this study population. Type 1 was the most common type of dual LAD (n=48), while Type 3 (n=3) and Type 4 (n=2) were infrequent and Type 2 was not detected. Additionally, we detected previously unclassified dual LAD variations in three cases.
CONCLUSION
Dual LAD may be a relatively more common variant than described in the medical literature, which is mostly based on catheter angiography studies. Coronary CT angiography seems markedly efficacious for detecting and documenting the anatomical details of dual LAD subtypes, as well as showing other associated cardiocoronary anomalies.
Dual left anterior descending (LAD) coronary artery is a rare congenital anomaly (1), basically defined as the existence of two distinct segments of the vessel occupying the anterior interventricular sulcus (AIS) of the heart.
First study classifying dual LAD anomalies based on coronary catheter angiography was published in 1983 by Spindola-Franco et al. (2), which has served as a primary classification system. However, individual reports further described previously unclassified LAD variants (3, 4). Most of the recent publications about dual LAD anomalies involve case reports and there is a paucity of large series using coronary computed tomography (CT) angiography (3–8).
At present, quite a large number of coronary CT angiography examinations are being performed and recognition of dual LAD variations by CT angiography requires familiarity. Being aware of dual LAD anomalies could be critical for coronary bypass surgery and interventions. Surely, sound knowledge on dual LAD anomalies is a prerequisite for proper management of patients with coronary artery disease.
In this study, we aimed to identify the frequency of dual LAD variations, and define the morphoanatomical features based on Spindola-Franco classification, using CT angiography. Appendageal subtypes of this variation were also documented and discussed.
Methods
Patients
The study was approved by our institutional review board. A total of 1337 consecutive coronary CT angiography examinations performed in our department from April 2010 to December 2013 were retrospectively evaluated for dual LAD anomalies. These examinations had been performed for various reasons including, but not limited to, the assessment of coronary and cardiac morphology, electrocardiography (ECG) abnormalities, coronary bypass graft evaluation, coronary stent evaluation, coronary atherosclerosis evaluation and screening for high risk patients (with diabetes, smoking history, family history, and hypertension).
Imaging
Out of 1337 coronary CT angiography examinations, 417 were obtained with 64-row multidetector computed tomography (MDCT) scanner (Toshiba Aquilion 64, Toshiba Medical System, Tokyo, Japan) while the remaining 920 were obtained with 320-row MDCT scanner (Toshiba Aquilion One, Toshiba Medical System, Japan).
All CT angiography examinations were performed with ECG-gating prospectively or retrospectively, according to patient’s heart rate and cardiac rhythm.
With 64-row MDCT, helical scanning protocol was used and images were acquired in the craniocaudal direction during suspended respiration with 0.5 mm slice thickness and 0.3 mm reconstruction interval, 0.4 s gantry rotation speed, 100–120 kVp with automated tube current modulation.
With 320-row MDCT, mostly volume and sometimes helical scanning protocol was employed. Images were acquired during suspended respiration at 0.5 mm slice thickness and 0.25 mm reconstruction intervals, 0.35 s gantry rotation speed, 80–120 kVp with automated tube current modulation.
Nonionic iodinated contrast material of 320–400 mgI/mL was delivered at 5–6 mL/s injection rate, and bolus tracking injection protocol was used. Peak density in the region-of-interest was selected as 120 HU at the ascending aorta level for 64-row MDCT scanner and 180 HU at the descending aorta level for 320-row MDCT scanner (per routine clinical protocol used in our department). The biphasic injection for coronary CT angiography consisted of 70–90 mL of contrast medium followed by a saline chase bolus of 30–40 mL at 5–6 mL/s injection rate.
Coronary CT angiography images were reconstructed at 5% to 10% reconstruction intervals and stored in the picture archiving and communication system.
Image evaluation
Dual LAD was diagnosed when two different vessels were identified in the AIS of the heart. Spindola-Franco classification was used to determine dual LAD subtypes (2) (Table 1). Two subtypes described in the literature in addition to Spindola-Franco classification were also searched in this study (3, 4) (Table 2). In addition, dual LAD anomalies inconsistent with any of the previously described subtypes were also recorded.
Table 1.
The original dual LAD classification made by Spindola-Franco et al. (2)
| Origin | Course | Location of long LAD | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| LMCA | LAD proper | Short LAD | Long LAD | Short LAD | Long LAD | Proximal long LAD | Distal long LAD | |
| Type 1 | Present | Present | LAD proper | LAD proper | Originates from the LAD proper, terminates in the proximal AIS | Originates from the LAD proper, courses on LV side of the proximal AIS, and reenters the distal AIS | Epicardial (LV side) | Distal AIS |
| Type 2 | Present | Present | LAD proper | LAD proper | Originates from the LAD proper, terminates in the proximal AIS | Originates from the LAD proper, courses on RV side of the proximal AIS, and reenters the distal AIS | Epicardial (RV side) | Distal AIS |
| Type 3 | Present | Present | LAD proper | LAD proper | Originates from the LAD proper, terminates in the proximal AIS | Originates from the LAD proper, follows an intramyocardial course in the septum proximally, and emerges epicardially in the distal AIS (or does not emerge in the AIS and terminated, intramyocardially) | Intramyocardial (interventricular septum) | Distal AIS |
| Type 4 | Present | Absent | LMCA | Proximal RCA | Originates from the LMCA, terminates in the proximal AIS | Originates from the proximal RCA, follows an anomalous prepulmonic course anterior to the RVOT, and enters the distal AIS | Epicardial (prepulmonic) | Distal AIS |
LMCA, left main coronary artery; LAD, left anterior descending artery; AIS, anterior interventricular sulcus; LV, left ventricle; RV, right ventricle; RCA, right coronary artery; RVOT, right ventricular outflow tract.
Table 2.
| Origin | Course | Location of long LAD | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| LMCA | LAD proper | Short LAD | Long LAD | Short LAD | Long LAD | Proximal long LAD | Distal long LAD | |
| Type 5 | Absent | Absent | LCS | RCS | Originates from the LCS, terminates in the proximal AIS | Originates from the proximal RCS, follows an anomalous intramyocardial course within the septal crest, emerges epicardially, and enters the distal AIS | Intramyocardial (septal crest) | Distal AIS |
| Type 6 | Present | Absent | LMCA | Proximal RCA | Originates from the LMCA, terminates in the proximal AIS | Originates from proximal RCA, follows an anomalous course between the RVOT and the aortic root, and enters the distal AIS | Epicardial (retropulmonic) | Distal AIS |
LMCA, left main coronary artery; LAD, left anterior descending artery; LCS, left coronary sinus; RCS, right coronary sinus; AIS, anterior interventricular sulcus; RCA, right coronary artery; RVOT, right ventricular outflow tract.
Besides determining the type of dual LAD anomalies, left main coronary artery (LMCA) length and caliber, proper LAD caliber (in the proximal 1 cm segment), long LAD caliber (in the proximal 1 cm segment) and short LAD caliber (in the proximal 1 cm segment) were also measured. All assessments of coronary CT angiography examinations were made on workstation (Vitrea FX, Version 6.2, Vital Images, Minnetonka, Minnesota, USA).
Additionally, diagonal and septal branching patterns were assessed and concomitant cardiocoronary variations/ anomalies were noted when present.
Coronary dominance was determined by identifying the vessel that forms the crux and gives the posterior descending (PD) artery branch in the posterior interventricular sulcus.
Descriptive statistics, including means and percentages, were used to summarize the data.
Results
Fifty-six dual LAD variations were detected among 1337 cases (4%). Data of these 56 cases were retrieved for further evaluation and analysis. Thirty-nine cases were male and 17 cases were female (age range, 19–68 years; mean age, 39.5 years).
Type 1 dual LAD was detected in 48 cases (86%, Fig. 1). Type 2 dual LAD was not observed. Type 3 dual LAD was detected in three cases (5%, Fig. 2) and type 4 was detected in two cases (4%, Fig. 3). Type 5 and Type 6 were not observed; however, previously unclassified anomalies were detected in three cases (5%, Table 3). In the first one of these cases, both the LMCA and right coronary artery (RCA) originated from the right coronary sinus with different ostia (Fig. 4). LMCA reached the left atrioventricular sulcus after coursing in between the aorta and the main pulmonary artery (malignant course anomaly). In that location, LMCA formed a trifurcation giving rise to the proper LAD, intermediate artery, and left circumflex artery (LCx). Proper LAD divided into the short and long LAD branches in the AIS.
Figure 1.
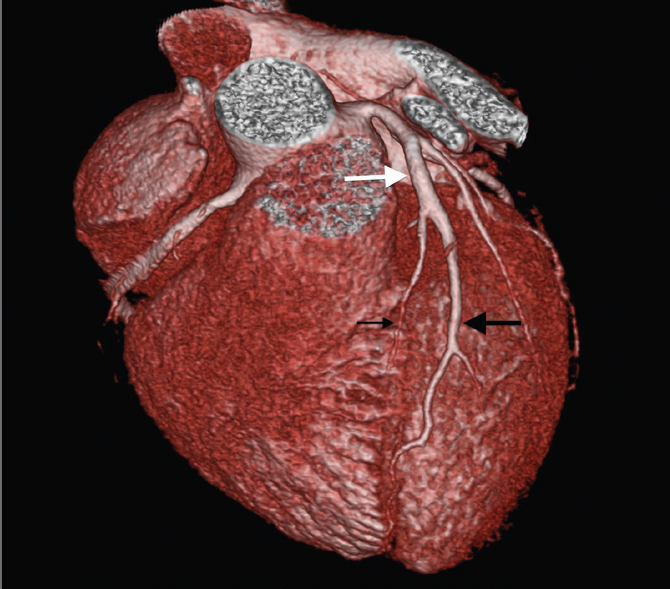
Type 1 dual LAD anomaly in a 43-year-old male patient. Colored three-dimensional (3D) volume rendered CT angiography image shows long (thick black arrow) and short (thin black arrow) LAD branches of the proper LAD (white arrow) in the anterior interventricular sulcus (AIS). Long LAD is on the left ventricle side of the AIS.
Figure 2.

Type 3 dual LAD anomaly in a 54-year-old female patient. Colored 3D volume rendered CT angiography image shows long (thick black arrow) and short (thin black arrow) LAD branches of the proper LAD (white arrow) in the anterior interventricular sulcus. Middle portion of long LAD follows an intramyocardial course.
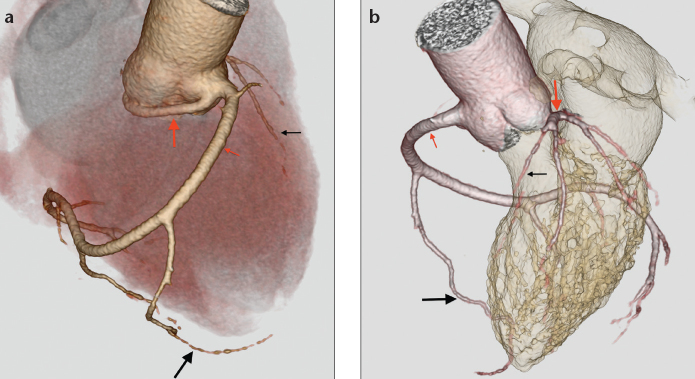
Figure 3.
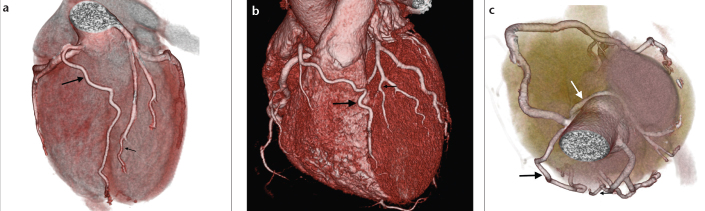
a–c. Type 4 dual LAD anomalies in two different cases. Colored 3D volume rendered CT angiography image (a) shows the long LAD (thick black arrow) originating from the right coronary artery ostia, following a prepulmonic course and reaching to the distal anterior interventricular sulcus (AIS). Short LAD (thin black arrow) originates from the left coronary sinus and courses in the proximal and middle portion of the AIS. In a different patient, colored 3D volume rendered CT angiography images (b, c) show the long LAD (thick black arrow) originating from the right coronary artery ostia, following a prepulmonic course, and reaching the mid and distal portion of the AIS. Short LAD (thin black arrow) originates from the left coronary sinus and courses in the proximal AIS. Left circumflex artery (white arrow) originates from the right coronary sinus with different ostia, follows a posteroinferior course in the retroaortic location and reaches to normal location in the left atrioventricular sulcus as an additional abnormality.
Table 3.
Morphologic features of novel dual LAD subtypes described in this series
| Origin | Course | Location of long LAD | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| LMCA | LAD proper | Short LAD | Long LAD | Short LAD | Long LAD | Proximal long LAD | Distal long LAD | |
| Type 7 | Present (LMCA originates from the RCS and shows interarterial malignant course) | Present | LAD proper | LAD proper | Originates from the LAD proper, terminates in the proximal AIS | Originates from the LAD proper, courses on LV side of the proximal AIS, and reenters the distal AIS | Epicardial (LV side) | Distal AIS |
| Type 8 | Present (LMCA originates from the RCS and shows retroaortic course) | Absent | LMCA | Mid RCA (branch of the right marginal artery) | Originates from the LMCA, terminates in the proximal AIS | Originates from the mid RCA, courses inferior wall surface of the RV, turns around the apex, and reaches to the distal AIS | Epicardial (RV inferior side) | Distal AIS |
| Type 9 (triple LAD) | Present | Present | LAD proper | LAD proper | Originates from the LAD proper, terminates in the mid AIS | Originates from the LAD proper, courses on LV side of the mid AIS, reenters the distal AIS, and terminates before reaching to the apex | Epicardial (LV side) | Distal AIS |
AIS, anterior interventricular sulcus; LAD, left anterior descending artery; LCS, left coronary sinus; LMCA, left main coronary artery; LV, left ventricle; RCA, right coronary artery; RCS, right coronary sinus; RV, right ventricle.
Figure 4.
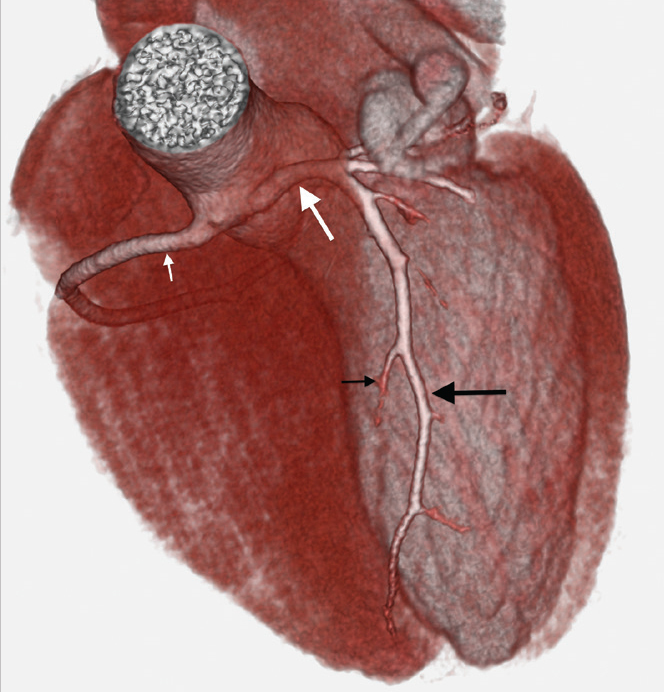
Type 7 dual LAD anomaly in a 27-year-old male patient. Colored 3D volume rendered CT angiography image shows both the left main coronary artery (LMCA) (thick white arrow) and right coronary artery (thin white arrow) originating from the right coronary sinus with different ostia. LMCA reaches the left atrioventricular sulcus after following a course in between the aorta and the main pulmonary artery (malignant course anomaly). LMCA forms trifurcation into the proper LAD, the intermediate artery, and the left circumflex artery. Proper LAD separates into the short (thin black arrow) and long LAD (thick black arrow) branches in the AIS.
In the second case, both the LMCA and RCA originated from the right coronary sinus with separate ostia (Fig. 5). LMCA reached the left atrioventricular sulcus after following a posteroinferior course and localizing in a retroaortic position. LMCA branched off to short LAD and LCx upon reaching its normal location. Right marginal branch of the RCA formed the long LAD and took a curve at the cardiac apex reaching to the distal AIS.
Figure 5.
a, b. Type 8 dual LAD anomaly in a 55-year-old female patient. Colored 3D volume rendered CT angiography images (a, b) show both the left main coronary artery (LMCA) (thick red arrow) and right coronary artery (RCA) (thin red arrow) originating from the right coronary sinus with separate ostia. LMCA reaches to the left atrioventricular sulcus after coursing posteroinferiorly with retroaortic localization. LMCA gives rise to the short LAD (thin black arrow) and left circumflex artery branches. Right marginal branch of the RCA forms the long LAD (thick black arrow), turns around the cardiac apex and reaches to the distal AIS.
In the third case, proper LAD divided into the long and short LAD branches, and the long LAD coursed on the left ventricle side of the AIS, being apart from AIS proximally (Fig. 6). Short LAD took course in the proximal AIS and following its termination, long LAD reentered to the distal AIS, followed a short course and terminated before the apex. Meanwhile, the PD artery extended towards the apical region of the AIS after turning around the cardiac apex. Hence, in this last case there were three different vessels in the AIS. All subtypes of dual LAD variations are illustrated in Fig. 7.
Figure 6.
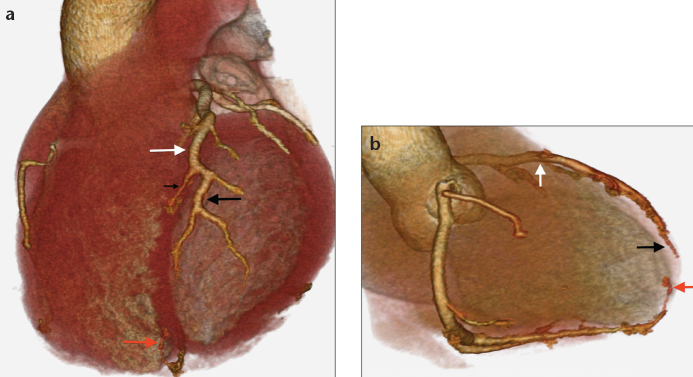
a, b. Type 9 dual LAD anomaly in a 42-year-old male patient. Colored 3D volume rendered CT angiography images (a, b) show the proper LAD (white arrow) branching into the short (thin black arrow) and long LAD (thick black arrow) and the long LAD on the left ventricle side of the AIS. Long LAD terminates early in the distal portion of the AIS and the posterior descending coronary artery (red arrow) extends towards the apical region of the AIS after turning around the cardiac apex. Hence, there are three different vessels in the AIS (may be called triple LAD).
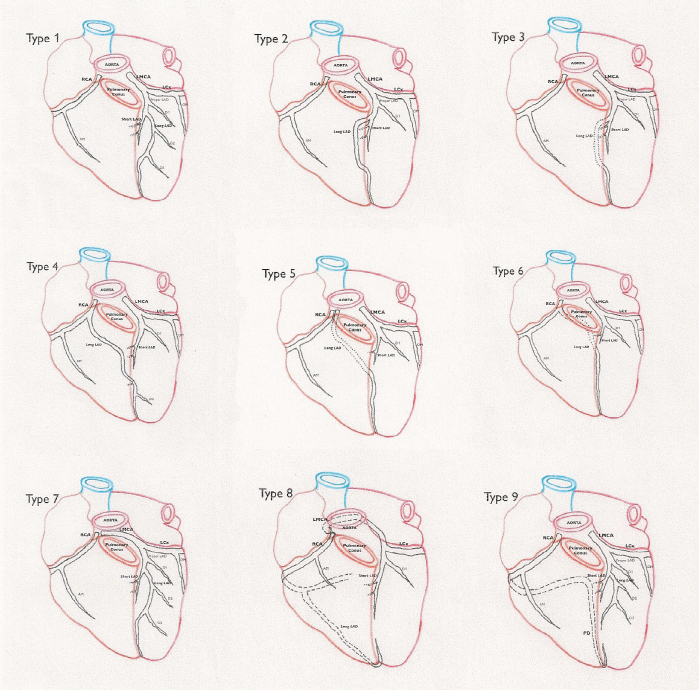
Figure 7.
Illustrations show nine subtypes of dual LAD. The first four subtypes were described by Spindola-Franco et al. (2), Type 5 by Manchanda et al. (3), and Type 6 by Maroney et al. (4). The final three new types (Type 7, Type 8, and Type 9) were described in this study. Dotted lines indicate intramyocardial course of the coronary arteries. Dashed lines indicate retroaortic course of the LMCA in Type 8 and normal course of the RCA and PD in Type 8 and Type 9. LMCA, left main coronary artery; RCA, right coronary artery; PD, posterior descending artery; LAD, left anterior descending artery; LCx, left circumflex artery; D1, D2, D3, diagonal arteries; OM, obtuse marginal artery; AM, acute marginal branch.
Length and caliber measurements of the LMCA and caliber measurements of the short, long, and proper LADs in the first 1 cm are given in Table 4.
Table 4.
Length and caliber measurements of the LMCA and caliber measurements of the proper, short, and long LADs in the first 1 cm
| LMCA length | LMCA caliber | Proper LAD caliber | Long LAD caliber | Short LAD caliber | |
|---|---|---|---|---|---|
| Mean | 9.3 | 4.2±0.6 | 3.6±0.6 | 2.8±0.5 | 1.8±0.5 |
| Minimum | 3.1 | 2.6 | 2.3 | 1.6 | 1.0 |
| Maximum | 33.4 | 5.8 | 5.6 | 4.3 | 3.0 |
| Median | 8.2 | 4.3 | 3.6 | 2.7 | 1.7 |
Measurements are given in millimeters.
LMCA, left main coronary artery; LAD, left anterior descending artery.
Diagonal and septal branching patterns of dual LAD types are summarized in Table 5.
Table 5.
Septal and diagonal branching patterns of dual LAD subtypes based on the literature (1–8) and our series
| Dual LAD type | Proper LAD | Short LAD | Long LAD | Additional feature |
|---|---|---|---|---|
| Type 1 | LV diagonal, proximal septal | Proximal septals, RV diagonal | LV diagonals | Short LAD never gives rise to an LV diagonal |
| Type 2 | Major LV diagonals | Proximal septals | Distal LV diagonals, RV diagonal | |
| Type 3 | LV diagonal | Proximal septal, RV diagonal, proximal LV diagonal | Distal septals, distal LV diagonal | |
| Type 4 | N/A | Proximal septal, proximal LV diagonal | Distal septals, distal LV diagonal | |
| Type 5 | N/A | Proximal septal, proximal LV diagonals | Distal septals, distal LV diagonals | |
| Type 6 | N/A | Proximal septals, proximal LV diagonal | Distal septals, distal diagonal | |
| Type 7 | Proximal LV diagonal, proximal septal | Proximal septals | Distal LV diagonal, distal septal | |
| Type 8 | N/A | Proximal septals, proximal LV diagonal | Distal septals | Morphologically long but anatomically short LAD gives rise to LV diagonal |
| Type 9 (triple LAD) | LV diagonal, proximal septal | Mid septals | Distal LV diagonals, distal septals | PD turns around the apex and reaches to the distal AIS |
LAD, left anterior descending artery; LV, left ventricle; RV, right ventricle; N/A, not applicable; PD, posterior descending artery; AIS, anterior interventricular sulcus.
Some extra-cardiac and vascular abnormalities and variations were associated with dual LAD variants such as; ramus intermedius branch in 27 cases (48%), coronary artery bridging in 24 cases (42%), patent foramen ovale in seven cases (13%), ventricular septal defect in one case (2%), LCx formed by RCA continuation in the left atrioventricular sulcus in one case (2%), abnormal origin of LMCA from the right coronary sinus in one case (2%), abnormal origin of LCx from the right coronary sinus in one case (2%), malignant course anomaly of LMCA abnormally originated from the right coronary sinus in one case (2%), and abnormal origin of long LAD from the right coronary sinus in one case (2%).
While right coronary dominance was detected in 50 cases (89%), left coronary dominance was observed in six cases (11%). Coronary codominance was not observed.
Discussion
Our study is the largest series of dual LAD variants in the existing literature. To date, Spindola-Franco et al. (2) reported the largest case series encompassing 23 dual LAD variations based on conventional coronary angiography. Our study emphasizes the CT angiography features of dual LAD, which allows three-dimensional evaluation of coronary and cardiac morphology besides cross-sectional information.
In this study, the frequency of dual LAD was four times greater than the frequency described in the catheter angiography literature. In addition, we described three additional subtypes of dual LAD variation, which had not been listed in the prior classification. It is not surprising that CT angiography revealed more cases with dual LAD and more subtypes of dual LAD itself. Three-dimensional anatomy is more readily demonstrated by CT angiography compared with catheter angiography. Awareness of dual LAD anomalies could be very important for coronary surgery and interventional procedures. Shortcomings of publications based on catheter angiography are hidden in the inherent invasive nature of the procedure and in being limited to cases undergoing catheter angiography; whereas CT angiography has the advantages of noninvasiveness and being able to reach a higher number of cases, hence, proper sampling of the population is more likely.
In normal anatomy, LAD originates from the LMCA, courses in the AIS towards the cardiac apex, and gives diagonal and septal branches. While septal branches extend to interventricular septum, diagonal branches extend to LV anterior wall (LV diagonals) and sometimes to RV anterior wall (RV diagonals) (1, 2).
Dual LAD anomaly is characterized by the presence of two distinct segments of LAD in the AIS and generally designates a short LAD terminating in the proximal AIS and a long LAD (which proximally courses outside the AIS), terminating in the distal AIS. Although four subtypes of this variation had initially been described based on morphoanatomical features of the coronaries, two additional subtypes were later published as case reports (2–4).
In line with the existing literature (2), type 1 dual LAD was the most common type of dual LAD (n=48, 86%) in our study. Type 3 and Type 4 dual LAD anomalies are rare, occurring in three and two cases, respectively, among the 23 cases of dual LAD in the angiographic series described by Spindola-Franco et al. (2). Similarly, we detected three cases of Type 3 and two cases of Type 4 in our study population. We did not detect any Type 2, Type 5 or Type 6 dual LAD anomalies in our study. These are not common types of this anomaly spectrum anyway, hence they are found in the literature only on a case report basis (2–5).
This case series added three more subtypes (Type 7, Type 8, and Type 9) to so far described dual LAD variants. Type 9 could also be named as “triple LAD” anomaly, since there were three different vessels in the AIS. As far as we know this is the first description of this extraordinary morphology in the literature, and it also indicates the possibility of further variant types, which can be detected by the contemporary state-of-the-art coronary CT angiography examinations. Our series did not include all known subtypes, but new subtypes were identified, suggesting that knowing about the variety of subtypes is the main issue, rather than listing and enumerating subtypes. Case-based CT angiography analyses may well contribute to diagnostic, surgical, and interventional procedures for clinical applications. Raising diagnostic awareness is among the main conclusions emerging from this study.
Measurement of the LMCA length and caliber, and calibers of the proper, short, and long LADs have not been documented in the literature previously (Table 4). Our results will be the first in the literature and constitute a source for future anatomo-morphological studies.
Diagonal and septal branching patterns also present with specific features in dual LAD anomalies. In general, major septal branches arise from the short and proper LADs, while diagonal branches arise from the long and proper LADs. This is completely true for particularly the most frequent variant, i.e., Type 1, while other variants may have some exceptions. A review of the literature with regard to diagonal and septal branches, revealed some branching specifications, as summarized in Table 5. Diagonal and septal branching patterns of Type 1, 3 and 4 dual LAD variants in our series are consistent with the existing literature (1, 2). In the most frequent Type 1 variant, short LAD never gives rise to an LV diagonal branch and our cases were in accordance with this (2). Similar to existing literature, non-Type 1 variants showed occasional diagonal branches originating from the short LAD (Table 5).
Among other coronary anatomic variants and anomalies accompanying dual LAD cases, ramus intermedius variation (48%) and coronary artery bridging (42%) were the most fre quent ones. Data emerging from our series show definitely higher prevalence of these two anatomic variations among dual LAD cases compared with the previously described frequency for normal population (15%–30% for ramus intermedius and 3.5%–26% for bridging) (9–12). The reason for generally higher prevalence of bridging detected by CT angiography compared with conventional catheter angiography lies in the nature and capabilities of the CT technique, as CT angiography examination can easily identify bridging, regardless of the shortness of the segment it involves, its superficiality, and presence of luminal narrowing. However, data from this series still shows higher prevalence of bridging among double LAD cases than the prevalence for general population obtained from previous CT angiography series (11, 12).
The prevalence of cardiac morphology abnormalities such as patent foramen ovale in our series (13%) was no different than in normal population (11%–17%) (13, 14).
In the literature, 86%–87% of the general population show right coronary dominance, while 9%–9.5% show left dominance, and 3%–4% show co-dominance (15, 16). Results from our dual LAD series are in accordance with the general population in terms of coronary dominance (89% right-dominance and 11% left dominance), except for the absence of codominance in this study. Spindola-Franco et al. (2), reported right dominance in 22 out of 23 cases (96%) and codominance in the remaining case (4%) (2). Our series shows a higher prevalence of left-dominance among dual LAD cases.
It is vital to know whether there is a dual LAD before any surgical intervention. Lack of this knowledge may end up with coronary bypass graft surgery covering only one of those LADs, which in turn may cause wrong or deficient revascularization of the anterolateral wall, interventricular septum, or apex. Similarly, recognition of Type 3 dual LAD variation prior to surgery is important for correct localization of dissection.
It is important for the interpreters of CT angiography to be aware of dual LAD anomalies. Conventional coronary catheter angiography is insufficient to visualize entire coronary vasculature particularly in the identification of coronary vessels with aberrant origin (17). For instance, in cases with long LAD originating from the right coronary sinus, only short LAD can be visualized during catheter angiography, which in turn can be misinterpreted as mid-LAD occlusion (1). Again, it may be difficult by catheter angiography to explain the reason for regional wall motion abnormality in case of occlusion of one of the dual LAD vessels, owing to lack of global visualization of the dual LAD system. Identification of duplicated or aberrant-origin vessels simultaneously and in three-dimension by CT angiography is useful for making a correct diagnosis and proper management planning.
Our study has some limitations. First, only those coronary and cardiac abnormalities that accompany dual LAD variants were included in this study; thus, their prevalence could not be compared with the prevalence in the non-dual LAD population. To overcome this, prevalence rates in the general population were estimated based on CT angiography reports or other methods reported in the current literature. Although utilization of CT angiography data in this series without referral to gold standard catheter angiography results of the same population may be listed as another limitation, many can argue against it. Coronary catheter angiography is the gold standard in terms of its capability to demonstrate luminal narrowing in more distal tiny vessels thanks to its very high spatial resolution and its ability to give real-time dynamic functional data. However, in terms of morphological details, CT angiography provides cross-sectional and three-dimensional data which is highly advantageous over catheter angiography.
In conclusion, the prevalence of dual LAD anomaly is higher in this CT angiography study than in previous catheter angiography-based studies probably due to better visualization of morphologic anatomy by CT. Coronary CT angiography seems markedly efficacious for detecting and documenting the anatomical details of dual LAD subtypes, as well as showing other associated cardiac and coronary anomalies.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Agarwal PP, Kazerooni EA. Dual left anterior descending coronary artery: CT findings. AJR Am J Roentgenol. 2008;191:1698–1701. doi: 10.2214/AJR.08.1193. [DOI] [PubMed] [Google Scholar]
- 2.Spindola-Franco H, Grose R, Solomon N. Dual left anterior descending coronary artery: Angiographic description of important variants and surgical implications. Am Heart J. 1983;105:445–455. doi: 10.1016/0002-8703(83)90363-0. [DOI] [PubMed] [Google Scholar]
- 3.Manchanda A, Qureshi A, Brofferio A, Go D, Shirani J. Novel variant of dual left anterior descending coronary artery. J Cardiovasc Comput Tomogr. 2010;4:139–141. doi: 10.1016/j.jcct.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Maroney J, Klein LW. Report of a new anomaly of the left anterior descending artery: type VI dual LAD. Catheter Cardiovasc Interv. 2012;80:626–629. doi: 10.1002/ccd.23219. [DOI] [PubMed] [Google Scholar]
- 5.Lee Y, Lim YH, Shin J, Kim KS. A case report of type VI dual left anterior descending coronary artery anomaly presenting with non-ST-segment elevation myocardial infarction. BMC Cardiovasc Disord. 2012;12:101. doi: 10.1186/1471-2261-12-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Namboodiri N, Ajitkumar V, Tharakan J. A rare type of dual left anterior descending artery distribution demonstrated by multislice cardiac computerized tomography in a patient with anterior wall infarction. J Invasive Cardiol. 2008;20:367–369. [PubMed] [Google Scholar]
- 7.Belostotsky V, Veljanovska L, Hristov N, Mitrev Z. Dual left anterior descending artery distribution. Interact Cardiovasc Thorac Surg. 2010;10:648–649. doi: 10.1510/icvts.2009.221820. [DOI] [PubMed] [Google Scholar]
- 8.Yoshikai M, Kamohara K, Fumoto H, Kawasaki H. Dual left anterior descending coronary artery: report of a case. Surg Today. 2004;34:453–455. doi: 10.1007/s00595-003-2733-x. [DOI] [PubMed] [Google Scholar]
- 9.Koşar P, Ergun E, Oztürk C, Koşar U. Anatomic variations and anomalies of the coronary arteries: 64-slice CT angiographic appearance. Diagn Interv Radiol. 2009;15:275–283. doi: 10.4261/1305-3825.DIR.2550-09.1. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien JP, Srichai MB, Hecht EM, Kim DC, Jacops JE. Anatomy of the heart at multidetector CT: what the radiologist needs to know. Radiographics. 2007;27:1569–1582. doi: 10.1148/rg.276065747. [DOI] [PubMed] [Google Scholar]
- 11.Zeina AR, Odeh M, Blinder J, Rosenschein U, Barmeir E. Myocardial bridge: evaluation on MDCT. AJR Am J Roentgenol. 2007;188:1069–1073. doi: 10.2214/AJR.06.0714. [DOI] [PubMed] [Google Scholar]
- 12.Kantarci M, Duran C, Durur I, et al. Detection of myocardial bridging with ECG-gated MDCT and multiplanar reconstruction. AJR Am J Roentgenol. 2006;186:S391–394. doi: 10.2214/AJR.05.0307. [DOI] [PubMed] [Google Scholar]
- 13.Purvis JA, Morgan DR, Hughes SM. Prevalence of patent foramen ovale in a consecutive cohort of 261 patients undergoing routine “coronary” 64-multi-detector cardiac computed tomography. Ulster Med J. 2011;80:72–75. [PMC free article] [PubMed] [Google Scholar]
- 14.Saremi F, Channual S, Raney A, et al. Imaging of patent foramen ovale with 64-section multidetector CT. Radiology. 2008;249:483–492. doi: 10.1148/radiol.2492080175. [DOI] [PubMed] [Google Scholar]
- 15.Ozturk E, Duran C, Sonmez G, et al. Arterial supply of the posterior interventricular sulcus: a CT coronary angiographic study. Surg Radiol Anat. 2011;33:27–34. doi: 10.1007/s00276-010-0695-4. [DOI] [PubMed] [Google Scholar]
- 16.Cademartiri F, La Grutta L, Malagò R, et al. Prevalence of anatomical variants and coronary anomalies in 543 consecutive patients studied with 64-slice CT coronary angiography. Eur Radiol. 2008;18:781–791. doi: 10.1007/s00330-007-0821-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clinical situations in which coronary CT angiography confers superior diagnostic information compared with coronary angiography. Diagn Interv Radiol. 2012;18:261–269. doi: 10.4261/1305-3825.DIR.5064-11.1. [DOI] [PubMed] [Google Scholar]