Abstract
Objectives. We examined whether community translation of an effective evidence-based fall prevention program via standard monetary support can produce a community-wide reduction in fall injuries in older adults and evaluated whether an enhanced version with added technical support and capacity building amplified the fall reduction effect.
Methods. We completed a randomized controlled community trial among adults aged 65 and older in (1) 10 control communities receiving no special resources or guidance on fall prevention, (2) 5 standard support communities receiving modest funding to implement Stepping On, and (3) 5 enhanced support communities receiving funding and technical support. The primary outcome was hospital inpatient and emergency department discharges for falls, examined with Poisson regression.
Results. Compared with control communities, standard and enhanced support communities showed significantly higher community-wide reductions (9% and 8%, respectively) in fall injuries from baseline (2007–2008) to follow-up (2010–2011). No significant difference was found between enhanced and standard support communities.
Conclusions. Population-based fall prevention interventions can be effective when implemented in community settings. More research is needed to identify the barriers and facilitators that influence the successful adoption and implementation of fall prevention interventions into broad community practice.
In 2010, injuries resulting from unintentional falls in adults aged 65 years and older accounted for 21 649 deaths nationally (54 per 100 000 population), which was the leading cause of fatal injury in that age group and the ninth overall cause of death.1 On the basis of 2011 emergency department data, the Centers for Disease Control and Prevention (CDC) estimated that more than 2.4 million unintentional fall injuries required treatment in emergency departments in adults aged 65 years and older, appreciably more than any other injury-related cause of emergency department visits.1 The CDC estimated that fatal and nonfatal unintentional falls in adults aged 65 years and older have lifetime costs greater than $18.6 billion (according to 2005 prices).2
Wisconsin has a higher fall injury mortality rate than does the nation as a whole.3,4 In 2010, Wisconsinites aged 65 years and older had the second highest rate of unintentional fall injury fatality among all states for that age group, a rate of 111 per 100 000 population.1 Morbidity resulting from unintentional fall-related injuries in Wisconsin is also substantial. In 2010, the inpatient hospitalization rate due to falls was 2175 per 100 000 population aged 65 years and older,5 and the emergency department visit rate was 3892 per 100 000.6
A challenge for the field of injury prevention and control is the translation of research findings into effective community-based prevention programs and practices.7 Systematic reviews report a steady increase in the number of effective interventions for the prevention of falls in older adults.8,9 Clinical practice guidelines and a compendium of community-based fall prevention programs have been published for prevention professionals.10,11 Despite the existence of evidence-based fall prevention interventions, there has been minimal widespread implementation by public health and aging agencies. Wandersman et al.12 identified the need for an effective way to bridge the gap between research and practice.
To address the question of how best to translate evidence-based interventions into community practice and whether this translation can produce a community-wide reduction in hospitalizations and emergency department visits for fall injuries, we conducted a randomized community trial from May 2008 through January 31, 2012. The intervention provided enhanced technical and capacity-building support (enhanced support system) to facilitate implementation of the evidence-based fall prevention program, Stepping On. Stepping On, a multifaceted intervention developed by Clemson et al.,13 showed a 31% reduction in fall rate for program participants compared with nonparticipants.14 The enhanced support system provided technical assistance, capacity building, and support in community and infrastructure assessment; engagement of key agencies; and access to local data to build a broader strategy around fall prevention in the community. Here we describe the effect of the enhanced support system intervention on fall injury hospital and emergency department discharge occurrence in the enhanced support system communities compared with standard and control communities.
METHODS
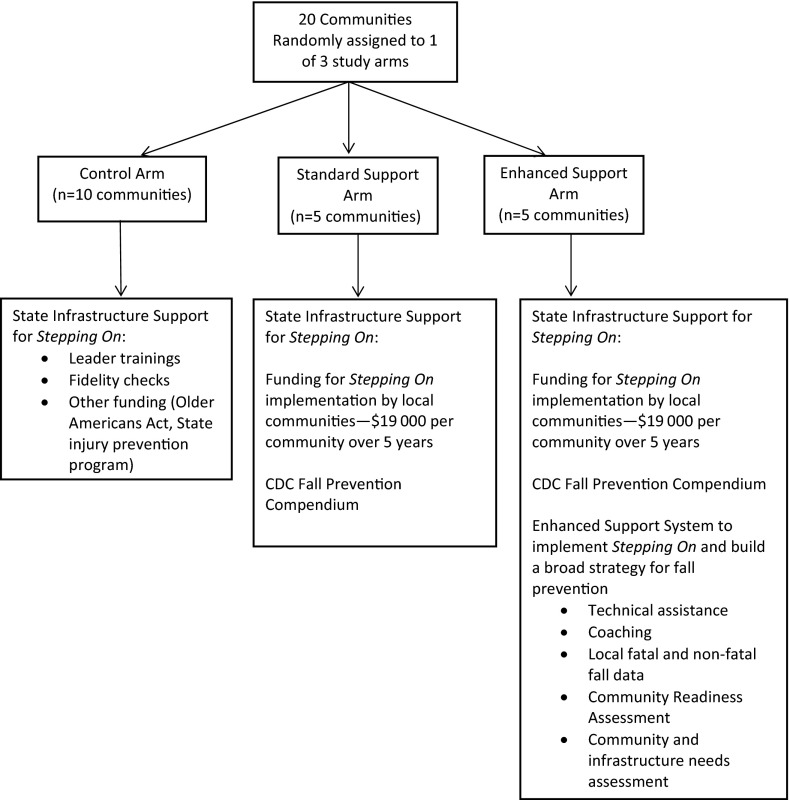
This study used a randomized community trial design to evaluate hospital and emergency department fall injury discharge occurrence in 3 groups of communities: (1) a control arm of 10 communities receiving no special resources related to fall injury prevention beyond the support available to them from the state’s aging network and health department, (2) a standard support arm of 5 communities receiving modest funding to implement Stepping On, and (3) an enhanced support system arm of 5 communities receiving technical assistance and support from the study team in addition to the same funding as that received by the standard support arm (Figures 1 and 2).
FIGURE 1—
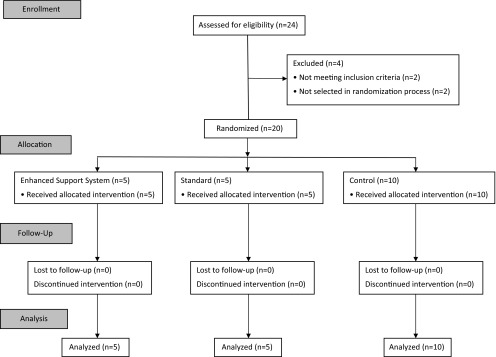
Flow diagram of study communities: Wisconsin, May 2008 through January 31, 2012.
FIGURE 2—
Support provided to communities in each study arm: Wisconsin, May 2008 through January 31, 2012.
Recruitment
Study team members collaborated with the Wisconsin Department of Health Services (DHS) to recruit communities beginning in May 2008. Study and DHS staff developed a document introducing the project, which was e-mailed to leaders at county health departments and aging units and regional aging and disability resource centers. DHS staff also spoke directly with agency leaders in counties where they knew of interest in fall prevention and discussed the project at various local and regional meetings with health department and aging agency leaders.
The study team received notice of interest from 24 agencies, representing 29 of Wisconsin’s 72 counties. Two communities were excluded because of extensive ongoing fall prevention activities.
Randomization
We used block randomization in late June 2008 to randomly assign 20 of the remaining 22 communities to 1 of the 3 arms, taking into account whether the lead agency was a health department or an aging agency and whether the community already had at least 1 trained Stepping On leader. The lead agency for one county was a Safe Communities coalition; this agency was classified as an aging agency. This led to 3 groups: aging agency and no leaders (7 communities); aging agency and at least 1 leader (6 communities); and health department and no leaders (7 communities).
The communities within each agency or leader group were assigned random numbers, ordered by the random number, and assigned sequentially within each group. These communities represented 17 single counties, 2 tricounty units, and 1 city.
Fall Prevention Program
The Stepping On program was chosen as the evidence-based fall prevention program because it was highly effective in the original study, it was scalable for implementing in a community setting, and state resources existed for training program leaders.13 Stepping On consists of 7 weekly sessions led by 1 health, fitness, or aging professional and 1 peer leader, covering topics such as strength and balance exercise, vision, medication, vitamin D, home hazards, community safety, and incorporating exercise practice. Participants receive a follow-up telephone call or home visit 3 weeks after the last session and a booster session 3 months after the final session.
The Greater Wisconsin Agency on Aging Resources hosted periodic trainings for Stepping On leaders and provided fidelity checks for newly trained leaders. Thirteen leader training sessions were held around the state during the study period.
Study Intervention
The enhanced support system intervention and methods are described in detail elsewhere.15 Briefly, in addition to existing state support and study funding ($19 000 over 5 years), the enhanced support system communities received reports with local data on fatal and nonfatal fall injuries; tailored technical assistance; and coaching to assist with the implementation of Stepping On, coalition development, and infrastructure and needs assessment (Figure 2). Planning teleconferences were held with the enhanced support system communities during February and March 2009, and monthly telephone calls were conducted from April 2009 to December 2011 with each of these communities. Site visits by study staff were conducted between October 2009 and mid-February 2010 and again between September and October 2010. The standard support communities also received $19 000 through the study to support the implementation of Stepping On, as well as copies of the CDC publications A CDC Compendium of Effective Fall Interventions and Preventing Falls: How to Develop Community-Based Fall Prevention Programs for Older Adults.11,16
Although we funded the enhanced support system and standard support communities to specifically implement Stepping On, we did not limit those communities to implementing only this program. We wanted them to have a variety of other evidence-based programs to choose from. This would allow communities to extend their fall prevention programming to a greater number of older adults, and the guide provided a planning process to identify and select programs.15 The control communities were free to avail themselves of support for fall prevention through Wisconsin’s state aging agency and health department but received no direction or funding from the study team to do so.
Variables
The primary outcome measure was fall injury morbidity in adults aged 65 years and older, as measured by Wisconsin inpatient and emergency department hospital discharge data. Data were obtained from the Wisconsin Hospital Association, which collects and cleans information on all emergency department and hospital discharges for general, acute-care, and nonfederal health care facilities in Wisconsin. Zip code and county of residence are available for each discharge, as are 1 principal discharge diagnosis, up to 8 other diagnoses, and a dedicated field for an external cause code (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] external-cause-of-injury code [E-code]).17 Discharges related to an unintentional fall were identified by the presence of an ICD-9-CM E-code in the range E880.0 to E886.9 or E888.0 to E888.9 in any of the diagnosis fields.17 We excluded deaths and admissions from acute-care facilities from the data set, the former because they represent only the small portion of fall-related deaths that make it to a health care facility before death and the latter to avoid double-counting fall-related admissions.
We computed discharge rates for a fall diagnosis per 100 population per year for the communities in each of the study arms for a 2-year baseline period (2007–2008) and for a 2-year follow-up period (2010–2011). Data from 2009 were excluded. We calculated observed fall discharge rates and their 95% confidence intervals (CIs). Denominators for the 65 years and older population in each community were based on estimates from the US Census Bureau18 and the Wisconsin DHS Office of Health Informatics.19 One participating community was a city, contained entirely within a single zip code. The 2007 to 2008 populations for this community were interpolated, and the 2011 population was predicted with the 2000 and 2010 federal census estimates and assuming a linear change. We used the 2003 county-level Rural-Urban Continuum Codes to characterize the rurality of the communities.20 These codes range from 1 at the most urban to 9 at completely rural.
We obtained sociodemographic data on gender, race, and poverty level from the 5-year estimates in the American Community Survey (2008–2012).21 The calculation of numbers of Stepping On workshops, leaders, and participants per 100 000 population aged 65 years and older was based on Stepping On participant data for 2007 to 2008 (baseline) and 2010 to 2011 (follow-up). Participant counts were restricted to those aged 65 years and older or of unknown age. We calculated community readiness scores, which measure a community’s level of readiness in 6 dimensions (efforts, community knowledge of efforts, leadership, community climate, community knowledge of the issue, and resources), to develop and implement prevention programming for the standard and enhanced support system communities for 2009 and 2012.22,23 Community readiness assessment interviews were not conducted in the control arm communities to avoid a potential Hawthorne effect.24 The presence of a community coalition addressing falls in 2010 or 2011 was obtained from annual statewide surveys on fall prevention activities conducted by the Wisconsin DHS.
Statistical Methods
We used a mixed-effects Poisson regression model in this event-rate longitudinal study to account for correlation of observations. Because the goal of the study was to detect differential temporal changes among the study arms, in the primary analysis we tested for the presence of interaction between study arm and time period (baseline or follow-up).25(p275–292) This model, with main effects for study arm and time period and an interaction term, random effects specified at the community level, and yearly community population as the exposure variable, is referred to as the primary model. We calculated incidence rate ratios (IRRs) with 95% CIs.
Prior to the study, we performed sample size and power calculations for various possible population sizes, injury rates, and effect sizes. All calculations used a 2-sided test, and to adjust for 2 simultaneous comparisons versus control, α was set to 0.025. The sample size of 5 communities per arm yielded sufficient power. For example, with a population of 10 000 and an injury rate of 4 per 100, the power was 0.88 to detect a 15% decline in injury rate. Post hoc power was considerably more favorable because the observed injury rate was 6 per 100, and the average 2-year population per community was 24 000. With these data, power to detect a 7% decline was 0.79 and a 9% decline was 0.96. As a reference for a negative conclusion, the post hoc power was 0.48 for a 5% decline.
In secondary analyses, we considered possible confounders and mediators, again using the mixed-effects Poisson model described earlier but adding in a given confounder or mediator. Potential confounders were the percentage of the 65 years and older population in the community that was 85 years or older and the degree of rurality of the community. Potential mediators were the annual rates of Stepping On workshops, leaders, and participants, per 100 000 population, and the presence of a community coalition addressing falls in 2010 or 2011. We tested an additional 2 potential mediators with only the data from the enhanced support system and standard support arms because they did not apply to the control arm: aging agency or health department as lead grant agency and community readiness score. We used Poisson regression to test for differences among the 3 study arms in the Stepping On workshop and leader and participant rates for the combined 4 study years by examining only the study arms in relation to the given outcome. IRRs and their 95% CIs are reported. We used a paired t test to compare change in community readiness scores. We used Stata version 12 for analyses.25
RESULTS
The total target population 65 years and older ranged from 154 027 in the enhanced support system arm to 499 767 in the control arm (Table 1). The study arms were similar in percentages of those aged 85 years and older, gender, race, and poverty level. As measured by the 2003 Rural-Urban Continuum Codes, the standard support communities were more rural than either the enhanced support system or the control communities. In 13 of the communities, grant activities were led by the aging agency at the beginning of the grant. The rates of Stepping On classes and leaders per 100 000 population 65 years and older was highest for the 4 analytic years (2007–2008 and 2010–2011) in the enhanced support system arm (Table 1).
TABLE 1—
Community Characteristics for Combined Baseline (2007–2008) and Follow-Up (2010–2011) Years: Wisconsin
| Characteristic | Enhanced Support System Communities | Standard Support Communities | Control Communities |
| Sociodemographic characteristics | |||
| Total population ≥ 65 y | 154 027 | 296 840 | 499 767 |
| % ≥ 85 y of those ≥ 65 y | 14.9 | 14.8 | 14.8 |
| % female of those ≥ 65 y,a range | 51.5–57.7 | 51.9–57.1 | 51.3–57.2 |
| % White, not Hispanic or Latino, of those ≥ 65 y, rangea | 93.3–98.6 | 95.2–99.5 | 95.5–99.5 |
| % below poverty level of those ≥ 65 y, rangea | 6.0–9.1 | 4.1–10.8 | 4.9–11.8 |
| Rural-Urban Continuum Code,b median (interquartile range) | 3 (3–7) | 6 (6–8) | 3 (1.5–4.5) |
| Lead agency at time of randomization, no. | |||
| Aging agency or group | 3 | 4 | 6 |
| Health department | 2c | 1 | 4 |
| Stepping On program characteristicsd | |||
| Rate of workshops per 100 000 population ≥ 65 y (no. of workshops) | 19.5 (30)e | 14.1 (42) | 12.0 (60) |
| Rate of leaders per 100 000 population ≥ 65 (no. of leaders) | 42.8 (66)f | 27.3 (81) | 21.2 (106) |
| Rate of participants per 100 000 population ≥ 65 y (no. of participants) | 192.2 (276)g | 142.2 (398)g | 107.0 (498) |
Percentage female, percentage White (not Hispanic or Latino), and percentage below poverty level taken from American Community Survey (2008–2012) 5-year estimates.21
Rural-Urban Continuum Codes range from 1 (most urban) to 9 (most rural).20
One community transferred control of grant activities to the aging agency midgrant.
Baseline and follow-up periods combined.
P = .03 for enhanced support system vs control.
P < .001 for enhanced support system vs control.
P < .001 for both enhanced support system and standard support vs control.
The Poisson model showed that, compared with the control arm, being in the enhanced support system arm was associated with a significantly higher number of workshops for the combined 4 analytic years (IRR = 1.62; 95% CI = 1.05, 2.51; Table 1), whereas being in the standard support arm had a nonsignificant 18% higher number of workshops (IRR = 1.18; 95% CI = 0.79, 1.75). Similarly, compared with the control arm, being in the enhanced support system arm was associated with a significantly higher number of leaders (IRR = 2.02; 95% CI = 1.49, 2.75), whereas the standard support arm had a nonsignificant 29% higher number of leaders (IRR = 1.29; 95% CI = 0.96, 1.72). Community readiness scores for the standard and enhanced support system communities increased from 2009 to 2012 (4.40 to 4.78 standard; 3.13 to 4.39 enhanced), but the increases were not significantly different between the 2 arms. The observed fall rate declined from 6.09 (95% CI = 5.92, 6.27) to 5.58 (95% CI = 5.42, 5.75) per 100 population in the enhanced support system arm, declined from 5.88 (95% CI = 5.75, 6.01) to 5.34 (95% CI = 5.23, 5.46) per 100 population in the standard support arm, and dropped from 5.80 (95% CI = 5.71, 5.90) to 5.78 (95% CI = 5.69, 5.88) in the control arm.
In our primary multivariate analyses, both the standard and the enhanced support system arms showed a significant reduction in inpatient and emergency department discharges for falls from baseline to follow-up compared with the control arm (Table 2). However, no significant difference was found between the enhanced support system and the standard support arms. Compared with baseline, the enhanced support system arm saw an 8% reduction in inpatient and emergency department visits for falls in adults aged 65 years and older, whereas the standard support arm reduction was 9% from baseline to follow-up. None of the covariates examined in the secondary analyses confounded or mediated the results found with the primary model. The percentage of the 65 years and older population that was 85 years or older did not differ among the study arms. Adjustment for Rural-Urban Continuum Codes showed that the rurality measure, although significant, did not change the fall reduction effect size for the enhanced support system and standard support arms. The potential mediators—rates of Stepping On workshops, leaders, and participants; presence of a community coalition; aging lead agency; and community readiness score—were all insignificant when added to the primary model, and their inclusion in the model did not appreciably alter the coefficients for the interaction terms representing the effect of the intervention; therefore, they were not mediators.
TABLE 2—
Poisson Regression of the Relation Between Inpatient and Emergency Department Discharges for a Fall and Study Arm Baseline (2007–2008) and Follow-Up (2010–2011) Periods: Wisconsin
| Factor | IRR (95% CI) | P |
| Study arm | .419 | |
| Control (Ref) | 1.000a | |
| Enhanced support system | 1.478a | .283 |
| Standard support | 1.484a | .278 |
| Time period | .788 | |
| Baseline (Ref) | 1.000a | |
| Follow-up | 0.997a | |
| Interaction (study arm × time period) | < .001 | |
| Enhanced support system × follow-up | 0.918 (0.876, 0.963) | < .001 |
| Standard support × follow-up | 0.914 (0.880, 0.950) | < .001 |
| Follow-up to baseline comparison within study arms | ||
| Control | 0.997 (0.974, 1.020) | .788 |
| Enhanced support system | 0.916 (0.878, 0.954) | < .001 |
| Standard support | 0.911 (0.884, 0.940) | < .001 |
Note. CI = confidence interval; IRR = incidence rate ratio.
Because of the presence of the interaction term, these values are not interpretable.
DISCUSSION
We found a significant population-level reduction in discharges for fall injuries requiring hospitalization or an emergency department visit in both the enhanced support system and the standard support communities over the control communities, indicating that a community-wide effect can be achieved. There was, however, no extra reduction in the enhanced support system communities compared with the standard support communities, suggesting that the enhanced support system was not effective in amplifying the effect of community translation. Controlling for several potential confounders and mediators did not appreciably change our results; differences between the arms with respect to those factors did not account for our findings.
Our study found that population-based fall prevention interventions can be effective when implemented in community settings in the United States. A review by McClure et al.9 of 35 fall prevention studies evaluated the effectiveness of population-based fall interventions. Of the 35 studies, the authors identified 6 prospective controlled community trials conducted in Australia, Denmark, Norway, Sweden (2 studies), and Taiwan; no randomized controlled trials were noted in the United States. The 6 studies achieved population-level relative reductions in fall injury rates ranging from 6% to 75%. Our study findings further support McClure’s conclusion that population-based approaches can prevent fall-related injuries.
Tinetti et al.26 targeted primary care personnel with an intervention focused on promoting effective risk assessments and fall prevention strategies. They found a reduced rate of serious fall-related injuries in their intervention region compared with their control region (9%) as well as a reduced rate of fall-related use of medical services (11%) at the population level. They noted effect sizes similar to ours but used a nonrandomized design. Their study represented an effort to translate fall prevention evidence into clinical practice, in contrast to our effort to translate prevention evidence into public health practice. Targeting clinicians was an intensive effort, particularly for face-to-face outreach, and has not been widely implemented.
We found no evidence that the enhanced support system amplified the effect of community translation of a fall prevention program. This result has several possible explanations. First, any difference in the effect of the enhanced and standard support to local communities was too small to be detected in this study. Second, the technical assistance and support the enhanced support system communities received perhaps was not needed, was not tailored enough to their needs, or was insufficient in amount. Third, the study design, with its prescriptive approach directing communities to implement Stepping On, without considering the community’s values, preferences, and resources, may have limited the community buy-in and thereby the effect of the intervention.27 Fourth, the enhanced support system may have worked but did not result in a difference in the study time frame. Finally, the standard support communities may have received technical support from elsewhere (e.g., state health department and aging agency resources) that was similar to that provided to the enhanced support system communities.
It is unlikely that the mechanism of reduction in fall injuries was solely due to increased implementation of Stepping On. We suspect that other community-wide effects resulted from the intervention, such as educating physicians, pharmacists, physical therapists, and low vision experts. These professionals serve as invited experts in the workshops and receive written materials about fall prevention. They may have subsequently served as opinion leaders in their health care organization. Another mechanism may be that both the standard and the enhanced support system communities’ work with Stepping On increased the buy-in from health care and non–health care service providers for fall prevention efforts. This study may have led communities to engage in additional fall prevention activities, such as including information on fall prevention in agency newsletters, providing resources at health fairs, implementing other evidence- and non-evidence-based fall prevention programs, and conducting fall risk screenings. The study also may have encouraged discussions about fall prevention among older adults in the community, thereby promoting change in risk behaviors without any specific intervention. Thus, our findings are to some extent hypothesis-generating and pose important questions for future study.
Limitations
Stepping On was not originally intended as a population-based approach to reducing inpatient and emergency department fall injury discharges. The workshops are targeted at older adults who have fallen in the past year or have a fear of falling; thus, most participants are at a relatively high risk of falling.
Only a limited number of older adults in each community (< 20%) participated in the workshops. The effect of the program was likely diluted by older adults who did not participate. Other limitations were the real-world challenges typical of implementing any community-based program, such as bringing key stakeholders together to form a coalition, staff turnover, competing priorities, and varying levels of commitment to the program by agencies and staff. Finally, E-coding of injuries can be incomplete in administrative data sets. However, Wisconsin law mandates reporting of E-codes when there is a nature of injury (ICD-9-CM) diagnosis code between 800 and 995.89. In our data set, 99.7% of those with a diagnostic code in the range 800 to 995.89 also had an E-code. In addition, the data do not contain patient identifiers. Therefore, we may have included more than 1 admission for the same fall event. We tried to limit this possibility by excluding admissions from an acute-care facility.
Although these limitations are important, we do not believe that any of them appreciably altered our main findings.
Conclusions
The study did show a population-level reduction in fall injuries for 2 of the study arms and a greater reduction in these arms compared with a control arm. No evidence indicated that the enhanced support system had a greater population effect in reducing injurious falls over the standard support arm approach.
More research is needed to identify the barriers and facilitators that influence the successful adoption and implementation of fall prevention interventions into broad community practice.11,26
Acknowledgments
Study work was supported by the Centers for Disease Control and Prevention (grant R49/CE001175).
Human Participant Protection
This study was approved by the Medical College of Wisconsin’s institutional review board. Individuals participated in an informed consent process, but a waiver of documentation of informed consent was granted by the institutional review board.
References
- 1. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARS). Welcome to WISQARS. 2003. Available at: http://www.cdc.gov/ncipc/wisqars. Accessed November 14, 2012.
- 2. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Data & Statistics (WISQARS): Cost of Injury Reports. 2003. Available at: http://wisqars.cdc.gov:8080/costT. Accessed May 22, 2013.
- 3.Guse CE, Porinsky R. Risk factors associated with hospitalization for unintentional falls: Wisconsin hospital discharge data for patients aged 65 and over. WMJ. 2003;102(4):37–42. [PubMed] [Google Scholar]
- 4.Mahoney JE, Glysch RL, Guilfoyle SM, Hale LJ, Katcher ML. Trends, risk factors, and prevention of falls in Wisconsin. WMJ. 2005;104(1):22–28. [PubMed] [Google Scholar]
- 5. Wisconsin Department of Health Services, Division of Public Health, Office of Health Informatics. Wisconsin Interactive Statistics on Health (WISH): Injury-Related Hospitalizations. Available at: http://www.dhs.wisconsin.gov/wish/main/InjuryHosp/InjuryHospHome.htm. Accessed June 29, 2012.
- 6. Wisconsin Department of Health Services, Division of Public Health, Office of Health Informatics. Wisconsin Interactive Statistics on Health (WISH): Injury-Related Emergency Department Visits. Available at: http://www.dhs.wisconsin.gov/wish/main/InjEmergencyDeptVisits/EDvisitsHome.htm. Accessed June 29, 2012.
- 7.Sogolow E, Sleet D, Saul J. Dissemination, implementation, and widespread use of injury prevention interventions. In: Doll L, Bonzo S, Sleet D, Mercy J, editors. Handbook of Injury and Violence Prevention. New York, NY: Springer; 2007. pp. 493–510. [Google Scholar]
- 8.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;(4):CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 9.McClure RJ, Turner C, Peel N, Spinks A, Eakin E, Hughes K. Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev. 2005;(1):CD004441. doi: 10.1002/14651858.CD004441.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panel on Prevention of Falls in Older Persons. American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 11.Stevens JA. A CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 2nd ed. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 12.Wandersman A, Duffy J, Flaspohler P et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3-4):171–181. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 13.Clemson L, Cumming RG, Kendig H, Swann M, Heard R, Taylor K. The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc. 2004;52(9):1487–1494. doi: 10.1111/j.1532-5415.2004.52411.x. [DOI] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention. Home & Recreational Safety. Multifaceted Interventions: Stepping On. Available at: http://www.cdc.gov/HomeandRecreationalSafety/Falls/compendium/3.1_steppingon.html. Accessed December 19, 2013.
- 15. Peterson DJ, Christiansen A, Guse CE, Layde PM. Community translation of fall prevention interventions: the methods and process of a randomized trial. J Community Psychol. In press.
- 16.National Center for Injury Prevention and Control. Preventing Falls: How to Develop Community-Based Fall Prevention Programs for Older Adults. Atlanta, GA: Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 17. National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification. Available at: http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed February 13, 2014.
- 18. US Census Bureau. American FactFinder. Available at: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed August 22, 2011.
- 19. Wisconsin Department of Health Services, Division of Public Health, Office of Health Informatics. Wisconsin Interactive Statistics on Health (WISH): Wisconsin Population. Available at: http://www.dhs.wisconsin.gov/wish/main/wis_pop/wis_pop_home.htm. Accessed August 22, 2011.
- 20. US Department of Agriculture, Economic Research Service. Rural-Urban Continuum Codes. May 10, 2013. Available at: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed October 27, 2014.
- 21. US Census Bureau. American Community Survey. Available at: http://www.census.gov/acs/www. Accessed July 11, 2014.
- 22.Edwards RW, Jumper-Thurman P, Plested BA, Oetting ER, Swanson L. Community readiness: research to practice. J Community Psychol. 2000;28(3):291–307. [Google Scholar]
- 23. Colorado State University College of Natural Sciences Tri-Ethnic Center. Community Readiness Model. 2011. Available at: http://triethniccenter.colostate.edu/communityReadiness.htm. Accessed July 17, 2014.
- 24.McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi: 10.1016/j.jclinepi.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.StataCorp. Stata: Release 12. College Station, TX: StataCorp LP; 2011. pp. 275–292. [Google Scholar]
- 26.Tinetti ME, Baker DI, King M et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359:252–261. doi: 10.1056/NEJMoa0801748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Layde PM, Christiansen AL, Peterson DJ, Guse CE, Maurana CA, Brandenburg T. A model to translate evidence-based interventions into community practice. Am J Public Health. 2012;102(4):617–624. doi: 10.2105/AJPH.2011.300468. [DOI] [PMC free article] [PubMed] [Google Scholar]