Abstract
Objectives. We sought to characterize postimmigration tuberculosis (TB) care for Class B immigrants and refugees at the Baltimore City Health Department TB program (BCHD), and to determine the proportion of immigrants with active TB or latent TB infection (LTBI) in this high-risk population.
Methods. We conducted a retrospective chart review of Class B immigrants and refugees who reported to the BCHD for postimmigration TB evaluation from 2010 to 2012.
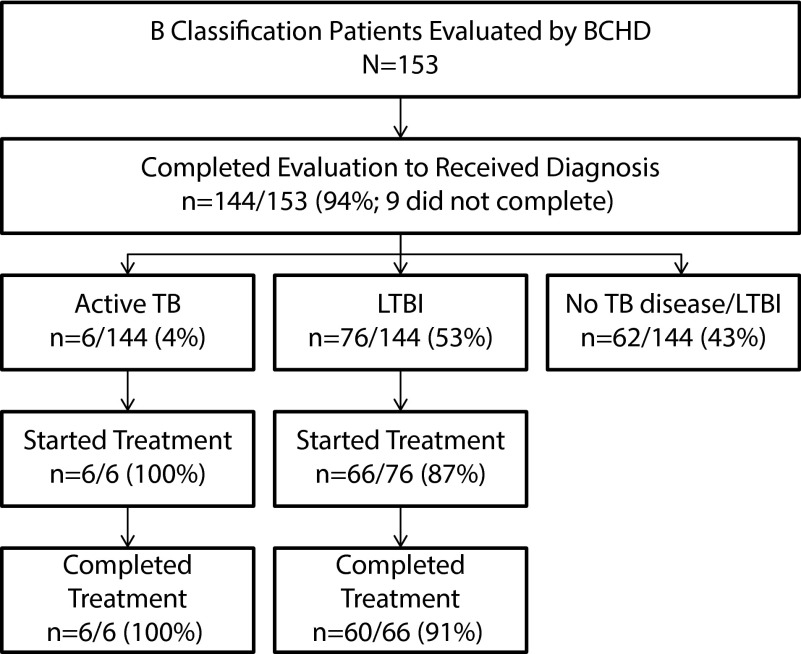
Results. We reviewed the clinical records of 153 Class B immigrants; 4% were diagnosed with active TB and 53% were diagnosed with LTBI. Fifty percent of active TB cases were culture positive, and 67% were asymptomatic; 100% received and completed active TB therapy at the BCHD. Among those diagnosed with LTBI, 87% initiated LTBI therapy and 91% completed treatment.
Conclusions. The high prevalence of active TB and LTBI found among Class B immigrants underscore the importance for postarrival TB screening. The absence of reported symptoms among the majority of active cases identified during this study suggest that reliance on symptom-based screening protocols to prompt sputa testing may be inadequate for identifying active TB among this high-risk group.
Efforts by local health departments to screen recent immigrants for tuberculosis (TB) are an important component of broader TB control goals. Foreign-born individuals represent a significant source of new cases of active TB reported in the United States. In 2012, the incidence of TB was 11.5 times as great among foreign-born individuals in the United States than it was for individuals born in the United States.1 It has been estimated by the US Centers for Disease Control and Prevention (CDC) that 4 out of 5 active TB cases among foreign-born persons is attributable to reactivation of TB that was likely acquired prior to arrival in the United States.2
To reduce the chances that TB will be introduced from abroad, US policy requires that individuals applying to immigrate or be relocated to the United States must undergo a prearrival medical exam that includes TB screening. US Department of State–appointed panel physicians, according to technical instructions developed by the conduct these exams overseas. In 2007, CDC published new technical instructions that required additional screening measures, including sputa cultures when sputa testing is indicated and drug-susceptibility testing for positive isolates.3
Under the current technical instructions, individuals with evidence of untreated, active, contagious TB are considered to have a Class A condition.4 Only those Class A applicants who receive a medical waiver are allowed to enter the United States; all other Class A applicants must demonstrate that they have undergone successful treatment of TB under directly observed therapy before they can reapply to immigrate to the United States. Individuals with some radiographic evidence of TB (including extrapulmonary TB that is not laryngeal or pleural), but negative smears and cultures, are designated as Class B1, pulmonary, or Class B1, extrapulmonary. Individuals who have a positive tuberculin skin test (TST; ≥ 5 mm if individual is a contact of known TB case, and ≥ 10 mm for all others) or Interferon-γ Release Assay (IGRA), but no other signs of TB are classified as Class B2, Latent TB Infection (LTBI) evaluation. Under the current technical instructions, the majority of immigrants who receive a B2 classification are children, as only applicants 2 to 14 years of age who are screened in a country where the World Health Organization-estimated TB incidence is 20 per 100 000 persons or greater receive TST or IGRA testing as part of initial screening. Recent contacts of a known TB case (usually, contacts of individuals who have received an A classification) are designated as Class B3, contact evaluation. All TB Class B immigrants are allowed entry to the country, but, because they are considered to be at high risk for developing TB, they are instructed to report to health departments or private clinicians for follow-up screening and, if indicated, treatment within 30 days of arrival.
The Baltimore City Health Department (BCHD) TB program provides clinical evaluation and care services to Class B immigrants that settled within the city. As of 2007, the guidelines for screening Class B immigrants as published by the State of Maryland have required sputum testing for only those Class B immigrants who, upon evaluation, were found to have a productive cough.5 In 2012, BCHD modified its protocol for evaluating Class B immigrants, to consider sputum testing of all Class B1 immigrants, regardless of whether they had TB symptoms or not.
Though US programs are designed to identify and prioritize for follow-up screening new immigrants who may be at high risk for developing TB upon arrival in the United States, few studies have been published describing postimmigration efforts to screen and treat newly arrived immigrants.6–10 In this light, we performed a retrospective chart review of Class B immigrants referred to the BCHD for TB evaluation between 2010 to 2012 to describe how Class B immigrants were screened in practice, and we compared these results with existing local protocols and national recommendations for Class B immigrant screening.
METHODS
We conducted a retrospective cohort study consisting of a chart review of Class B immigrants who reported to the health department TB program for postimmigration TB evaluation in 2010 to 2012. The study population included all patients who: (1) were classified as a Class B immigrant during their preimmigration medical exam and (2) reported to the BCHD for postimmigration screening during the study period. Class B immigrants who were referred to the BCHD for postimmigration screening but who did not appear for clinical evaluation (and therefore did not have clinical records) were not included.
We reviewed data from the BCHD’s electronic patient database and a state database to identify a list of Class B immigrants that may have been evaluated by the BCHD during the study period. We then searched the BCHD’s clinical records to see if charts existed for these individuals. For those available charts, we examined each to confirm that the individual met our inclusion criteria. Once we deemed a chart eligible for inclusion, we abstracted the following information: patient demographic information (from patients’ immigration forms); preimmigration screening information (including clinical and diagnostic results and clinician notes contained in Department of State forms and overseas medical screening forms); postimmigration TB symptom and diagnostic data (from clinicians’ notes and laboratory test reports); and clinical diagnosis and treatment data (from BCHD clinicians’ notes). Patients were considered to have had a complete medical exam if at BCHD they received a chest radiograph (X-ray), a physical exam, and, in some cases, the diagnostic testing necessary to result in a diagnosis of active TB, LTBI, or to rule out current active TB or LTBI (i.e., TST or IGRA testing and, for those with possible active TB, sputa smear).
We summarized clinical and demographic factors among individuals included in this study. We examined the association of these factors with patients’ preimmigration screening results, postimmigration diagnosis, treatment initiation, and treatment completion. Categorical data were analyzed using the χ2 test and continuous variables were analyzed using a median test. All data were analyzed using Stata Version 10.1 (StataCorp, College Station, Texas).
RESULTS
Among the 205 Class B immigrants referred to the health department TB program during 2010 to 2012 for postimmigration screening, we located and evaluated the clinical records of 153 (75%) patients who reported to the BCHD for an evaluation (Figure 1). Sixty-four percent (98/153) of immigrants were male, and the median age was 33 years (interquartile range [IQR]: 15–58 years; Table 1). Across all years in the study, most Class B patients entered the United States from Nepal (98/153, or 64%), mostly as refugees. After Nepal, the Philippines (19/153, or 12%) and Ethiopia (9/153, or 6%) were the most frequent countries of origination; however, there was some year-to-year variation in the immigration patterns noted throughout the study (P = .023).
FIGURE 1—
Flow of Class B immigrants (n = 153) screened by the BCHD for TB: Baltimore, MD, 2010–2012.
Note. BCHD = Baltimore City Health Department; LTBI = latent tuberculosis infection; TB = tuberculosis. Treatment completion among all those diagnosed with LTBI was 79% (60/76).
TABLE 1—
Description of All B Classification Patients Seen by the BCHD for TB, by Year: Baltimore, MD, 2010–2012
| Characteristic | 2010 (n = 36), No. (%) or Median (IQR) | 2011 (n = 67), No. (%) or Median (IQR) | 2012 (n = 50), No. (%) or Median (IQR) | Total (n = 153), No. (%) or Median (IQR) | P |
| Gender | |||||
| Female | 9/36 (25%) | 26/67 (39%) | 20/50 (40%) | 55/153 (34%) | |
| Male | 27/36 (75%) | 41/67 (61%) | 30/50 (60%) | 98/153 (64%) | |
| Age, y | 30 (15–51) | 42 (23–67) | 29 (14–47) | 33 (14–58) | .033 |
| 0–14 | 9/36 (25%) | 16/67 (24%) | 14/50 (28%) | 39/153 (26%) | |
| 15–24 | 6/36 (17%) | 3/67 (5%) | 7/50 (14%) | 16/153 (10%) | |
| 25–44 | 10/36 (28%) | 15/67 (22%) | 14/50 (28%) | 39/153 (26%) | |
| 45–64 | 7/36 (19%) | 14/67 (21%) | 10/50 (20%) | 31/153 (20%) | |
| ≥ 65 | 4/36 (11%) | 19/67 (28%) | 5/50 (10%) | 28/153 (18%) | |
| Country of origination/origina | |||||
| Other | 9/36 (25%) | 4/67 (6%) | 5/50 (10%) | 18/153 (12%) | |
| Nepal/Bhutan | 17/36 (47%) | 49/67 (73%) | 32/50 (64%) | 98/153 (64%) | |
| Philippines | 6/36 (17%) | 6/67 (9%) | 7/50 (14%) | 19/153 (12%) | |
| Ethiopia/Eritrea | 3/36 (8%) | 6/67 (9%) | 0/50 (0%) | 9/153 (6%) | |
| Dominican Republic | 1/36 (3%) | 1/67 (2%) | 3/50 (6%) | 5/153 (3%) | |
| Turkey/Iraq | 0/36 (0%) | 1/67 (1%) | 3/50 (6%) | 4/153 (3%) | |
| B classification | |||||
| B1 | 25/36 (69%) | 49/67 (73%) | 34/50 (68%) | 108/153 (71%) | |
| B2 | 11/36 (31%) | 17/67 (44%) | 15/50 (33%) | 43/153 (28%) | |
| B3 | 0/36 (0%) | 1/67 (1%) | 1/50 (2%) | 2/153 (1%) | |
| Abnormalities reported in preimmigration chest X-rayb | |||||
| Infiltrate or consolidation | 13/25 (52%) | 19/49 (39%) | 18/34 (53%) | 50/108 (46%) | |
| Any cavitary lesion | 2/25 (8%) | 3/49 (6%) | 2/34 (6%) | 7/108 (7%) | |
| Nodule with poorly defined margins | 1/25 (4%) | 4/49 (4%) | 2/34 (6%) | 7/108 (7%) | |
| Pleural effusion | 0/25 (0%) | 0/49 (0%) | 1/34 (3%) | 1/108 (1%) | |
| Hilar mediastinal adenopathy | 0/25 (0%) | 1/49 (2%) | 0/34 (0%) | 1/108 (1%) | |
| Linear interstitial markings | 1/25 (4%) | 0/49 (0%) | 1/34 (3%) | 2/108 (2%) | |
| Discrete fibrotic scar or linear opacity | 11/25 (44%) | 35/49 (71%) | 23/34 (68%) | 69/108 (64%) | |
| Discrete nodule without calcification | 1/25 (4%) | 2/49 (4%) | 1/34 (3%) | 4/108 (4%) | |
| Discrete fibrotic scar with volume loss or retraction | 2/25 (8%) | 4/39 (4%) | 3/34 (9%) | 9/108 (8%) | |
| Other | 5/25 (20%) | 15/39 (31%) | 9/34 (27%) | 29/108 (27%) | |
| History of prior TB noted in immigration paperwork | 6/36 (17%) | 15/67 (22%) | 11/50 (22%) | 32/153 (21%) | |
| Days from entry to evaluation by health department | 62 (53–77) | 93 (69–112) | 61 (45–80) | 75 (55–98) | < .001 |
| Days since last preimmigration chest X-ray | 194 (167–204) | 224 (196–258) | 182 (146–217) | 201 (169–241) | < .001 |
Note. BCHD = Baltimore City Health Department; IQR = interquartile range; TB = tuberculosis.
Patients commonly were screened and emigrated from a country of origination that was not their country of origin. For example, many patients who emigrated from Nepal were born and raised in Bhutan. Most patients who arrived from Ethiopia and Turkey were born and raised in Eritrea and Iraq, respectively.
Class B1 only. Percentages may sum to greater than 100 as patients frequently had more than 1 abnormality noted.
The majority of immigrants were classified during preimmigration medical evaluation as Class B1 (108/153, or 71%) and B2 (43/153, or 28%). Among B1 patients, “discrete fibrotic scar or linear opacity” and “infiltrate or consolidation” were the most common categories on overseas medical screening forms selected to describe the abnormalities found in these patients’ X-rays.
Twenty-one percent (32/153) of all immigrants had documentation of prior TB disease in their preimmigration screening (Table 2). History of TB varied by B classification: 27% (29/108) of B1, 7% (3/43) of B2, and 0% (0/2) of B3 immigrants had a prior TB noted in their preimmigration medical examination paperwork (P = .005).
TABLE 2—
Summary of Postimmigration Examination of All Immigrants for Tuberculosis (TB), By Classification: BCHD, Baltimore, MD, 2010–2012
| Post-Immigration Screening Results |
|||||
| Characteristic | B1 (n = 108), No. (%) | B2 (n = 43), No. (%) | B3 (n = 2), No. (%) | All Classes (n = 153), No (%) | P |
| History of prior TB noted in preimmigration paperwork | 29/108 (27%) | 3/43 (7%) | 0/2 (0%) | 32/153 (21%) | .005 |
| Any symptoms at time of evaluation | 19/108 (18%) | 1/43 (2%) | 0/2 (0%) | 20/153 (13%) | .034 |
| Postimmigration HIV test conducted | 70/108 (65%) | 14/43 (33%) | 0/2 (0%) | 84/153 (55%) | < .001 |
| Postimmigration HIV test positive | 0/70 (0%) | 2/14 (14%) | – | 2/84 (2%) | .001 |
| Postimmigration TST results available | 33/108 (31%) | 10/43 (23%) | 0/2 (0%) | 43/153 (29%) | – |
| Postimmigration TST positive (≥ 10mm) | 29/33 (88%) | 10/10 (100%) | – | 39/43 (91%) | – |
| Received QuantiFERON testing | 78/108 (72%) | 12/43 (28%) | 0/2 (0%) | 90/153 (59%) | < .001 |
| QuantiFERON test positive | 42/78 (54%) | 6/12 (50%) | – | 48/90 (53%) | – |
| Abnormal postimmigration chest X-ray | 62/108 (57%) | 3/43 (7%) | 0/2 (0%) | 65/153 (43%) | < .001 |
| Received sputa testinga | 60/108 (56%) | 3/43 (7%) | 0/2 (0%) | 63/153 (41%) | < .001 |
| Sputa smear positive | 0/60 (0%) | 0/3 (0%) | – | 0/63 (0%) | – |
| Sputa culture positive | 3/60 (5%) | 0/3 (0%) | – | 3/63 (5%) | – |
| Completed medical evaluation | 99/108 (92%) | 43/43 (100%) | 2/2 (100%) | 144/153 (94%) | – |
| Active TB | 5/99 (5%) | 1/43 (2%) | 0/2 (0%) | 6/144 (4%) | – |
| LTBI | 39/99 (39%) | 35/43 (81%) | 2/2 (100%) | 76/144 (53%) | – |
| No current LTBI/TB disease | 55/99 (56%) | 7/43 (16%) | 0/2 (0%) | 62/144 (43%) | < .001 |
Note. BCHD = Baltimore City Health Department; LTBI = latent tuberculosis infection; TST = tuberculin skin test. P values presented in this table represent comparison between B classification categories for each variable. Dashes indicate that data are not available.
Sputum testing includes acid-fast bacilli smear microscopy and mycobacterial liquid culture.
For all classes of immigrants, the median time period between entry to country and evaluation by the BCHD was 75 days (IQR 55–98 days; Table 1). We found that the median time to evaluation of all immigrants varied significantly by year and was highest in 2011 (93 days; IQR = 69–112 days; P < .001). Similarly, the median time that elapsed between immigrants’ preimmigration chest X-rays and when they presented to BCHD for evaluation was 201 days (IQR = 169–241 days) and was also longest in 2011 (224 days; IQR = 196–258 days; P < .001).
Post-Immigration Evaluation
All 153 immigrants that reported to BCHD received chest X-rays at the TB clinic. Abnormalities were found in 43% of all immigrants’ X-rays (Table 2). The highest percentage of abnormalities occurred among Class B1 immigrants; 57% (62/108) of B1 immigrants were found to have abnormal postimmigration chest X-rays, as compared with 7% (3/43) of B2 and 0% (0/2) of B3 immigrants (P < .001).
BCHD performed IGRA testing using QuantiFERON-TB Gold-In Tube (QFT-G; Cellestis, Ltd, Carnegie, Australia) on 59% (90/153) of immigrants, among whom 53% (48/90) tested positive. Additionally, postimmigration TST test results were available for 29% (43/153) of all immigrants who reported to the BCHD for an evaluation. Ninety-one percent (39/43) of all those with postimmigration TST results had indurations of 10 mm or greater. Twenty-four immigrants (16%) had both postimmigration TST and IGRA results available. For these individuals, 18 were IGRA positive and had TST indurations of 10 mm or greater; 5 were IGRA negative and had TST of 10 mm or greater, and 1 was IGRA negative and had a TST result of less than 10 mm. IGRA testing differed between B1, B2, and B3 immigrants, with most tests occurring among B1s (P < .001).
Overall, 41% (63/153) of immigrants evaluated by the BCHD received both sputa smear and culture testing (Table 2). Sputa testing was significantly (P < .001) more likely to occur among B1 immigrants, with 71% (60/108) receiving sputa testing, as compared with B2 (3/43, or 7%) and B3 (0/2, or 0%). The proportion of B1 immigrants that received sputa testing differed by year and was greatest in 2012 (26/34, or 76%) versus 2011 (22/49, or 45%) and 2010 (12/25, or 48%; P = .012). Sputa testing also differed between patients who reported symptoms versus asymptomatic patients. Eighty-five percent (17/20) of all symptomatic patients received sputa testing as compared with 34% of asymptomatic patients (P < .001). The proportion of asymptomatic patients who received sputa testing at the BCHD also varied with time. Sputa testing of asymptomatic patients was highest in 2012 (16/39, or 40%). This proportion was marginally significantly higher than that in 2010, when 9 out of 30 (30%) asymptomatic patients were tested (P = .055).
Postimmigration Diagnosis
Overall, 94% (144/153) of the Class B immigrants screened by the health department received complete medical evaluations (chest X-ray and physical exam) that resulted in a diagnosis of either current active TB or LTBI or a rule out of both of those conditions (Figure 1). Among these, half did not have abnormalities on their postimmigration chest X-ray and 40% percent had evidence in their immigration paperwork of having successful prior treatment of TB.
There were 6 cases of active TB among the 144 (4%) immigrants who received a complete postimmigration medical evaluation (Table 3). Three of the active TB cases were culture positive and 3 were diagnosed based on radiographic findings, clinical examination, or IGRA testing. Among the active TB cases that were not culture positive, 2 were pediatric patients and 1 had extrapulmonary TB. All newly diagnosed active TB cases completed treatment.
TABLE 3—
Characteristics of B Classification Patients Who Received Full Clinical Evaluations, by Diagnosis Category: BCHD, Baltimore, MD, 2010–2012
| Active TB (n = 6), No. (%) or Median (IQR) | Latent TB (n = 76), No. (%) or Median (IQR) | No TB Infection or Disease (n = 62), No. (%) or Median (IQR) | P | |
| B classification | < .001 | |||
| B1 | 5/6 (83%) | 39/76 (51%) | 55/62 (89%) | – |
| B2 | 1/6 (17%) | 35/76 (46%) | 7/62 (11%) | – |
| B3 | 0/6 (0%) | 2/76 (3%) | 0/62 (0%) | – |
| Gender | – | |||
| Female | 1/6 (17%) | 24/76 (32%) | 26/62 (42%) | – |
| Male | 5/6 (83%) | 52/76 (68%) | 36/62 (58%) | – |
| Age, y | 29 (14–30) | 23 (12–49) | 41 (27–59) | .021 |
| Country of origination/origin | – | |||
| Other | 0/6 (0%) | 7/76 (9%) | 10/62 (16%) | – |
| Nepal/Bhutan | 3/6 (50%) | 50/76 (66%) | 38/62 (61%) | – |
| Philippines | 0/6 (0%) | 8/76 (11%) | 11/62 (18%) | – |
| Ethiopia/Eritrea | 2/6 (33%) | 6/76 (8%) | 1/62 (2%) | – |
| Dominican Republic | 0/6 (0%) | 2/76 (3%) | 2/62 (3%) | – |
| Turkey/Iraq | 1/6 (17%) | 3/76 (4%) | 0/62 (0%) | – |
| History of prior TB noted in preimmigration paperwork | 1/6 (17%) | 4/76 (5%) | 25/62 (40%) | < .001 |
| Days from entry to country to evaluation by BCHD | 105 (63–125) | 74 (53–98) | 76 (57–98) | .653 |
| Abnormal preimmigration chest X-ray | 5/6 (83%) | 40/76 (53%) | 55/62 (89%) | < .001 |
| Infiltrate or consolidation | 2/5 (40%) | 5/40 (13%) | 9/55 (16%) | – |
| Any cavitary lesion | 0/5 (0%) | 0/40 (0%) | 2/55 (4%) | – |
| Nodule with poorly defined margins | 0/5 (0%) | 0/40 (0%) | 2/55 (4%) | – |
| Pleural effusion | 0/5 (0%) | 0/40 (0%) | 0/55 (0%) | – |
| Hilar mediastinal adenopathy | 0/5 (0%) | 1/40 (3%) | 0/55 (0%) | – |
| Linear interstitial markings | 0/5 (0%) | 0/40 (0%) | 0/55 (0%) | – |
| Discrete fibrotic scar or linear opacity | 1/5 (20%) | 24/40 (60%) | 27/55 (49%) | – |
| Discrete nodule without calcification | 1/5 (20%) | 3/40 (8%) | 1/55 (2%) | – |
| Discrete fibrotic scar with volume loss or retraction | 1/5 (20%) | 4/40 (10%) | 3/55 (6%) | – |
| Other | 0/5 (0%) | 3/40 (8%) | 11/55 (20%) | – |
| Abnormal postimmigration chest X-ray | 5/6 (83%) | 23/75 (31%) | 31/62 (50%) | < .001 |
| Reported symptoms | 2/6 (33%) | 9/76 (12%) | 9/62 (15%) | – |
| Received sputa testing | 2/2 (100%) | 8/9 (89%) | 7/9 (78%) | – |
| Culture positive | 1/2 (50%) | 0/8 (0%) | 0/7 (0%) | – |
| Did not report symptoms | 4/6 (67%) | 67/76 (88%) | 53/62 (86%) | – |
| Received sputa testing | 4/4 (100%) | 17/67 (25%) | 21/53 (43%) | – |
| Culture positive | 2/4 (50%) | 0/17 (0%) | 0/21 (0%) | – |
| Completed treatment | 6/6 (100%) | 60/66 (91%) | – | – |
Note. BCHD = Baltimore City Health Department; IQR = interquartile range. P values presented in this table represent comparison between diagnosis categories for each variable. Patients received sputum testing on the basis of postimmigration chest X-ray, clinical history, or physical exam.
Half of the active TB cases (3/6) were refugees from Nepal, the remainder from Eritrea/Ethiopia (2/6, or 33%) and Iraq (via Turkey; 1/6, or 17%). Eighty-three percent (5/6) of active TB cases were male. Among these 6 active TB cases, 4 (67%) were asymptomatic at time of evaluation but received further evaluation based on their radiographic features or clinical exam. Two of the 4 asymptomatic patients were found to be sputum culture positive. Among the 2 active TB cases that reported symptoms, 1 was culture positive.
Fifty-three percent (76/144) of Class B immigrants received a diagnosis of LTBI. Thirty-eight patients (50%) were diagnosed with LTBI on the basis of a positive IGRA, while 3 (4%) were diagnosed with LTBI based on a positive postimmigration TST. Thirty-five immigrants (46%) were diagnosed and treated for LTBI despite a lack of positive postimmigration TST or IGRA on the basis of a preimmigration TST result or postimmigration chest X-ray finding indicative of inactive TB infection. The vast majority of these patients (50/76, or 66%) were from Nepal, most of whom resettled in the United States as refugees. Eighty-two percent of LTBI patients were younger than 15 years, and 68% were male. Among those diagnosed with LTBI, 87% (66/76) initiated LTBI therapy with either a 9 month course of isoniazid or a 4 month course of rifampin, with 91% (60/66) completing treatment. Treatment completion among all those diagnosed with LTBI who were eligible for treatment was 79% (60/76).
Overall, 43% (62/144) of those who completed postimmigration evaluation were found to have no evidence of current active TB or LTBI and were not recommended to complete any further TB treatment. Among these 62 individuals, 40% (25/62) had documentation in their immigration paperwork of prior treatment of TB, while the remainder (37/62, or 60%) had active TB or LTBI excluded on the basis of a combination of QFT-G testing (negative QFT-G in 32/37, or 86%), postimmigration chest X-ray (no evidence of active or inactive TB in 31/62, or 50%), or sputum evaluation (negative mycobacterial culture in 100% of the 28/62, or 45%, of immigrants tested).
We examined differences among those who reported symptoms at time of examination versus those who did not. Of the 144 patients who received a complete medical examination, only 20 (14%) patients reported having any symptoms at the time of their examination. Active TB, LTBI, and no current TB disease or infection were diagnosed in 10% (2/20), 45% (9/20) and 45% (9/20) of symptomatic patients, respectively (P = .336). Among the asymptomatic patients, 3% (4/124) were diagnosed with active TB, 54% (67/124) with LTBI and 43% (53/124) with no current TB disease or infection.
DISCUSSION
Despite their having thorough predeparture medical examinations, we found a high period prevalence of active TB (4%) and LTBI (53%) among Class B immigrants evaluated by the BCHD-TB program. Recent (2009) guidance by the CDC has intensified the preimmigration screening procedures.4 Class B immigrants arriving in Baltimore during the study period had substantial preimmigration evaluations, including preimmigration sputum mycobacterial cultures performed for all those with abnormal chest X-rays (Class B1). Our data suggest that serial testing and evaluation of high-risk individuals, both before and after immigration, is a necessary component to enhanced TB case-finding strategies.
Among the challenges to TB screening is the ability to identify subclinical or paucibacillary disease. Many TB screening algorithms rely upon presence of symptoms to initiate further microbiologic testing or further imaging evaluations. However, our study found that in this high-risk population, two thirds of the identified active TB cases reported no symptoms; overall, half of these active TB cases were diagnosed by sputum culture, while the remainder were clinically diagnosed based on imaging, symptoms, and other clinical findings following extensive evaluations. Based on these observations, the BCHD implemented changes to screening protocol in 2012 to consider sputa testing of all B1 immigrants, regardless of reported symptoms. Though we were not able to determine based on the data contained in this study, whether these protocol changes will lead to enhanced case finding, we feel the results of this analysis offer important insights for policy related to postimmigration examinations for Class B1 immigrants. Given the high proportion of asymptomatic active TB disease identified, clinicians should strongly consider evaluating sputa for acid-fast bacilli smear and mycobacterial culture, along with other directed testing, from high-risk patients with abnormal chest X-rays, regardless of preimmigration microbiologic testing.
Nearly all immigrants diagnosed with either LTBI or active TB completed treatment of their illness. Though LTBI adherence rates observed in this analysis are similar to those among foreign-born patients reported in our previous analysis, they are higher than typically reported in the literature.11 The reasons for enhanced LTBI treatment completion in this patient population are unclear. Further research is needed to determine the health system and patient factors associated with these observed LTBI treatment completion rates.
Despite these successes, there remain challenges to local screening efforts. An important issue is the length of time between immigrants’ entry to the United States and postimmigration evaluation. Nationally, it has been reported that the median time from arrival to postimmigration evaluation for Class B immigrants is 39 days.12 However, at the BCHD, we found that the median time to evaluation was 75 days and was longer than these national survey data, and evaluation was significantly more delayed than CDC’s recommendation of 30 days. There were also delays between the time of preimmigration clinical evaluation and a patient’s arrival in the United States. In our study, greater than 4 months had elapsed between patients’ time of pre- and postimmigration evaluations; in some cases, greater than 1 year had elapsed. Though our study did not directly evaluate reasons for these delays, they are likely multifactorial and include patient factors as well as health system factors. Additional prospective studies are needed to more specifically determine where in the postimmigration time period delays in time-to-evaluation are occurring.
In light of this, time to evaluation should be considered when defining protocols for domestic screening of Class B immigrants postimmigration. Clinicians may want to consider ordering sputa and other diagnostic tests for immigrants for whom significant time has elapsed since their preimmigration medical examination. Screening protocols for immigrants should also factor in time to evaluation when defining whether to retest patients upon arrival, regardless of patients’ current symptoms.
There were some limitations to our study. First, Class B immigrants in Baltimore were largely composed of refugees from a few specific settings. The high prevalence of active TB in this group may reflect risk factors specific to these populations that are not generalizable to individuals immigrating from other settings and regions. Secondly, our overall sample size was small, which can impact point estimates and may be prone to temporal trends. Nonetheless we are among the first in recent years to report on details of postimmigration TB screening practices at a representative urban local health department across a 3-year time period, and our period prevalence estimates are consistent with other published data from the state and national level.7,9,10 Finally, our study was largely retrospective and long-term follow-up data on Class B immigrants was not available; future studies to evaluate incidence of active TB among Class B immigrants over time are warranted to help guide policy regarding further TB screening in this and other high risk groups.
The prevalence of active TB and LTBI observed among Class B immigrants in this study underscores the importance of postimmigration evaluation of this high-risk group. Diagnosis may be complicated by the absence of symptoms in active TB cases and long delays between immigrants’ entry to the United States and postimmigration evaluation. Despite these challenges, high rates of treatment completion achieved by the BCHD suggest efforts to screen and treat recent immigrants may be effective in reducing the burden of TB within the community.
Acknowledgments
The authors wish to acknowledge the assistance of Barbara Johnson, Nicketta Paige, and Judith Mutinda of the Baltimore City Health Department and Andrea Palmer of the Maryland Department of Health and Mental Hygiene for their assistance with data collection.
Human Participant Protection
Ethics committees at the Johns Hopkins University School of Medicine and the Baltimore City Health Department approved this research (IRB Study Number: NA_00086033). This study received a waiver of informed consent.
References
- 1.Centers for Disease Control and Prevention. Trends in tuberculosis - United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:201–205. [PMC free article] [PubMed] [Google Scholar]
- 2.Ricks PM, Cain KP, Oeltmann JE, Kammerer JS, Moonan PK. Estimating the burden of tuberculosis among foreign-born persons acquired prior to entering the U.S., 2005-2009. PLoS ONE. 2011;6:e27405. doi: 10.1371/journal.pone.0027405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Tuberculosis Screening and Treatment (TB TIs) using Cultures and Directly Observed Therapy (DOT) Frequently Asked Questions (FAQ) Available at: http://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/tuberculosis-panel-technical-instructions-faq.html. Accessed June 25, 2014.
- 4.Centers for Disease Control and Prevention. CDC Immigration Requirements: Technical Instructions for Tuberculosis Screening and Tretment Using Cultures and Directly Observed Therapy. 2009. Available at: http://www.cdc.gov/immigrantrefugeehealth/pdf/tuberculosis-ti-2009.pdf. Accessed June 25, 2014.
- 5.Maryland Department of Health and Mental Hygiene. Maryland TB Guidelines for Prevention and Treatment of Tuberculosis. 2007. Available at: http://phpa.dhmh.maryland.gov/OIDPCS/CTBCP/CTBCPDocuments/tbguidelines.pdf. Accessed April 16, 2014.
- 6.Sciortino S, Mohle-Boetani J, Royce SE, Will D, Chin DP. B notifications and the detection of tuberculosis among foreign-born recent arrivals in California. Int J Tuberc Lung Dis. 1999;3:778–785. [PubMed] [Google Scholar]
- 7.DeRiemer K, Chin DP, Schecter GF, Reingold AL. Tuberculosis among immigrants and refugees. Arch Intern Med. 1998;158:753–760. doi: 10.1001/archinte.158.7.753. [DOI] [PubMed] [Google Scholar]
- 8.McCaw BR, DeLay P. Demographics and disease prevalence of two new refugee groups in San Francisco. The Ethiopian and Afghan refugees. West J Med. 1985;143:271–275. [PMC free article] [PubMed] [Google Scholar]
- 9.Gacek P, Sosa L, Lobato MN. Assessment of postarrival tuberculosis examinations among immigrants and refugees screened overseas. Conn Med. 2013;77:325–330. [PubMed] [Google Scholar]
- 10.Binkin NJ, Zuber PL, Wells CD, Tipple MA, Castro KG. Overseas screening for tuberculosis in immigrants and refugees to the United States: current status. Clin Infect Dis. 1996;23:1226–1232. doi: 10.1093/clinids/23.6.1226. [DOI] [PubMed] [Google Scholar]
- 11.Nuzzo JB, Golub JE, Chaulk P, Shah M. Analysis of latent tuberculosis infection treatment adherence among refugees and other patient groups referred to the Baltimore City Health Department TB clinic, February 2009-March 2011. J Immigr Minor Health. Epub ahead of print August 2, 2013. [DOI] [PubMed]
- 12.Lee D, Philen R, Wang Z et al. Disease surveillance among newly arriving refugees and immigrants - electronic disease notification system, United States, 2009. MMWR Surveill Summ. 2013;62:1–20. [PubMed] [Google Scholar]