Abstract
Objectives:
The objective was to determine the repeatability of intraocular pressure (IOP) measurements made through a soft contact lens (CL) using the Scheimpflug noncontact tonometry in healthy subjects.
Methods:
This prospective, randomized, single-center study included one eye of 88 subjects (40 male and 48 female). Only participants without glaucoma or any other ocular pathology were included in this study. Three consecutive IOP measurements by the Scheimpflug noncontact tonometry were performed with and without daily disposable hydrogel CLs (−0.50 DS) (Dailies-nelfilcon A, 69% water, 8.7 mm base curve, 14 mm diameter, center thickness 0.10 mm) by a single operator. To avoid any bias arising from diurnal variation, all measurements were made at a similar time of day (11 am ± 1 h). The repeatability of IOP measurements using the Scheimpflug noncontact tonometry with and without CLs was evaluated using Pearson's correlation analysis. Bland-Altman plotting was used to assess the limits of agreement between the measurements with and without CLs.
Results:
The mean (± standard deviation) IOPs with and without CL were 13.80 ± 2.70 and 13.79 ± 2.54 mm of Hg respectively. The mean difference was 0.01 ± 0.16 (95% confidence interval, +1.97 to − 2.00) mm Hg. Statistical analysis via paired t-test showed no statistical difference between the two groups with (P = 0.15). A good correlation was found for IOP measurements with and without CL (r = 0.93, P < 0.001). Good test-retest reliability was found when IOP was measured with and without CL.
Conclusion:
There was no significant difference between IOP measured with and without CLs by Scheimpflug noncontact tonometry.
Keywords: Contact lens, Corvis ST, intraocular pressure
Glaucoma is a pathological eye condition that affects millions of people worldwide, making it the second-leading cause of global blindness.[1] Since raised intraocular pressure (IOP) is a cardinal feature of glaucoma, lowering of IOP is essential to prevent further progression of the disease.[2,3] Periodic measurement of IOP is highly recommended for both diagnosis and management of glaucoma.[4] Goldmann applanation tonometry (GAT) is currently considered the gold standard for the measurement of IOP.[5,6] The main advantages of GAT are that it is inexpensive, portable, and easy to handle. However, it has a few disadvantages such as requirement of topical anesthesia to reduce patient discomfort, increased risk of corneal injury and fluctuations of IOP measurement depending on the corneal thickness.[7] Furthermore, GAT and other forms of contact tonometry are unsuitable during a few clinically significant scenarios including the immediate postoperative period, infectious keratitis or in the presence of therapeutic contact lenses (CLs). Since GAT is calibrated for 520 μm corneal thickness, it usually underestimates IOP in thinner corneas and overestimates it in thicker corneas.[8]
Soft CLs are used for correction of refractive errors and therapeutically for ocular conditions like epithelial defects, filamentous keratitis, bullous keratopathy and postrefractive surgery.[9] During follow-up visits, due to existing ocular conditions it is often impractical to remove the CL for IOP measurement. Previous studies have shown that in healthy eyes, there is a negligible difference between IOP measured over a soft CL with pneumotonometry, Tonopen, GATs, and noncontact tonometers.[10,11,12,13,14]
The Corvis® ST (OCULUS Optikgerate GmbH, Germany) is a new noncontact tonometer that allows the investigation of the dynamic reaction of the cornea to an air impulse.[15] It measures IOP by analyzing the deformation of the corneal profile at 4330 frames/s. The mechanism of the Corvis® ST is not fully published.[16] It is mainly designed to measure noncontact IOP and corneal biomechanics. Being a new instrument, recent studies have compared and investigated the agreement of IOP measured by Corvis® ST with the GAT and the rebound tonometer,[16,17,18] with both studies showing high correlation and good agreement between the Corvis® ST and other instruments. While assessing the reliability and comparability of a new instrument, the applicability of the measurements in various situations is also important. The Corvis® ST noncontact tonometer is well-suited for situations wherein therapeutic CL are applied, such as laser refractive surgery. To the best of our knowledge, the accuracy of IOP measurement over CLs by theCorvis® ST has never been reported. Therefore, the aim of this study was to investigate the precision of IOP measurement by the Corvis® ST with and without hydrogel CLs on healthy eyes.
Methods
Eighty-eight eyes of 88 healthy adult volunteers (40 males and 48 females) were included in this study. The study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by an institutional review board. The participants had to be at least 18 years of age and able to comply with the lens wearing and clinical trial visits scheduled as directed by the investigator. The participants had to have ocular health findings considered to be “normal,” and they should not have conditions that would prevent them wearing CLs safely. The corrected vision had to be 20/40 or better in each eye with spherical CLs. The participants were required to have prior experience using CLs. Exclusion criteria include any current ocular disease, history of ocular surgery, ocular hypertension or any evidence of corneal pathology such as keratoconus.
All subjects provided signed informed consent prior to the study entry. One eye of each participant was randomly selected for the study. All subjects underwent a comprehensive examination including visual acuity measurement, with anterior and posterior segment evaluation.
The Corvis® ST is a noncontact tonometer equipped with an optical pachymetry function.[19,20] It measures IOP using an air puff and without any physical contact with the eye. During the air puff, a 9 mm slit through the apex illuminates the eye, and a built-in high-speed camera records the movement of the eye at 4330 images/s. The camera uses a sequence of 140 Scheimpflug images of the cornea, which are analyzed by a built-in computer. The device increases the air pressure puffed on the cornea in proportion to time. The shape of the cornea changes from the normal convex surface to a concave surface. This change is optically detected within 140 Scheimpflug images. The device then calculates the time required to applanate the cornea with the air puff.
For each patient, three consecutive measurements with the Corvis® ST were performed by a single examiner, under the same conditions first without and then after 15 min of wearing a CL. All of the worn CLs were discarded immediately following removal. To minimize diurnal variation, all measurements were done during the same session at the same time of the day (11 am ± 1 h). In this study, −0.50 DS CLs (Dailies, Alcon, TX, 69% water, 8.7 mm base curve, 14 mm diameter, center thickness 0.10 mm) were used.
Statistical analysis
Patient data were analyzed using SPSS software version 17 (SPSS, Inc., Chicago, IL, USA). Normality of the obtained data was assessed using the Kolmogorov-Smirnov test. The repeatability of IOP measurement using the Corvis® ST with and without CL was evaluated using Pearson's correlation analysis. Bland-Altman plotting was used to assess the limits of agreement between the measurements with and without CLs. Measurement differences obtained with and without CLs were evaluated using paired t-test. The effect of CLs in IOP measurement was analyzed using Levene's test. A P value of 0.05 or less was considered statistically significant.
Results
This study evaluated 88 healthy eyes of 88 participants. There were 40 males and 48 females with a mean (± standard deviation [SD]) age of 25 ± 4 years (range 20–35 years). The average IOPs measured by the Corvis® ST with and without CL were 13.79 ± 2.54 and 13.80 ± 2.70 mm of Hg respectively [Table 1]. The mean difference was 0.01 ± 0.16 (95% confidence interval [CI], +1.97 to −2.00) mm Hg. Statistical analysis via paired t-test found no statistical difference between the two groups (P = 0.15).
Table 1.
IOP measured by Corvis® ST
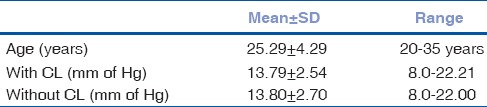
There was a good correlation between IOP measured with and without CL (r = 0.93, P < 0.001). Intra-examiner repeatability of IOP measurement with and without CLs is shown in Table 2. The correlation was good for consecutive measurements of IOP ranging 0.95–0.99 (P < 0.001 for all correlations).
Table 2.
Intra examiner repeatability of IOP measured without and with CL
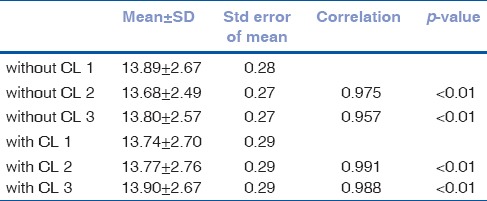
Fig. 1 shows the limits of agreement between IOP measurements with and without CLs in a Bland-Altman plot. Levene's test confirmed that the presence of CL does not significantly affect the repeatability of IOP measurements (F = 0.45, P = 0.141).
Figure 1.
Bland-Altman plot showing agreement between the intraocular pressure measured by Corvis® ST with and without contact lenses. The central line represents mean thickness differences between methods
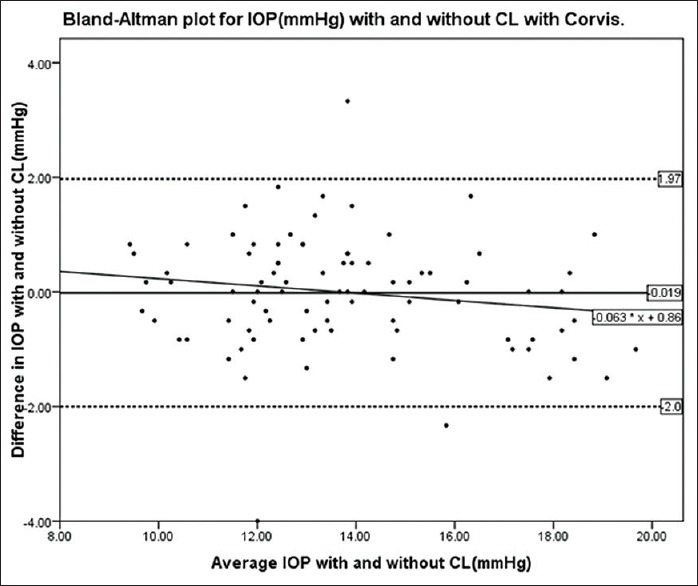
Fig. 2 shows the box plot of IOP measurements by the Corvis® ST with and without CLs. The plots indicate similar distributions and inter-quartile range on both sides of the medians.
Figure 2.
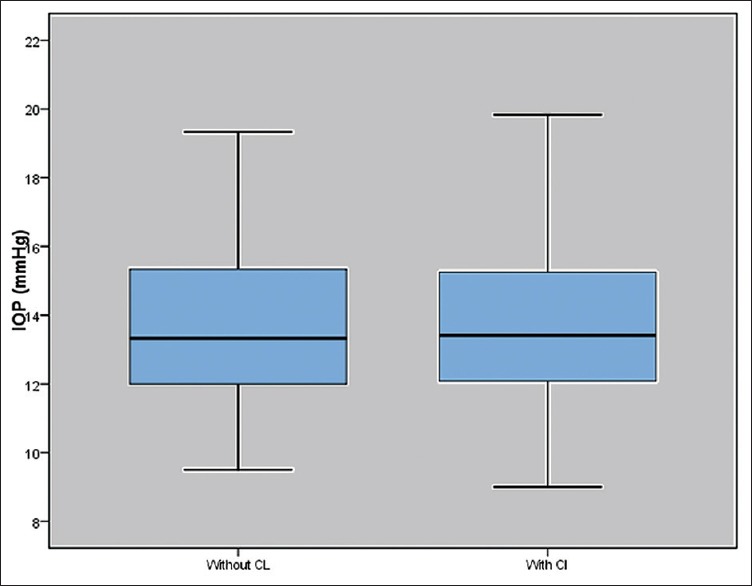
Box plot showing distribution intraocular pressure measured by Corvis® ST with and without contact lenses
Discussion
We investigated the difference in IOP measured using the Corvis® ST tonometer on healthy eyes with and without CL. Recent studies have confirmed that the Corvis® ST tonometer provides reliable and reproducible IOP measurements without the need for either local anesthesia or fluorescein staining.[17,18] In addition, variation in central corneal thickness seems to have little or no influence on IOP measurements by the Corvis® ST.[21]
Previous studies have shown that the use of soft CLs does not affect IOP when measured by the Topcon[22] or Nidek air puff noncontact tonometer.[11] However, Ogbuehi[23] found that measuring IOP through soft CLs resulted in consistent and significant differences measurements. The repeatability of IOP measurement through CLs mostly depends on the technique being used.
Insler and Robbins found that the difference in IOP measured by NCT with and without soft CLs was higher in hyperopic lenses than in myopic lenses and that the power of the soft CL was a predictor of IOP difference.[24] In addition, the water content of the CL also contributes to the IOP measurement. However, this effect is negligible when there is a high water content lens or a power of <−3.00 DS.[25]
Low minus powered silicone hydrogel lenses are also reported to have a negligible effect on the IOP. These findings are similar to those of our study which used 0.50 DS CLs.[13] Zeri et al.[26] found a good correlation between IOP measured through hydrogel and silicone hydrogel CLs. While comparing IOP in 40 normal eyes with and without a low powered minus CL, Lim et al. found that Tonopen consistently determined higher readings than GAT, however, they reported this inference may be due to the CL itself.[27]
We found a negligible difference between IOP measurements with and without CLs in our study, in addition, the difference we found, was lower than the difference in previous studies using applanation tonometry. Nosch et al.,[28] in their study comparing IOP readings over a thin hydrogel CL with DCT, found that a thin CL does not affect IOP measurements, which corroborates our findings.
We found a mean difference ± SD (95% CI) in IOP measurement without and with CLs of 0.01 ± 0.16 mm of Hg, which was statistically not significant. Our results are in agreement with a similar previous study conducted in glaucomatous patients that found a mean difference of −0.57 ± 2.3 mm Hg (95% CI, −1.5–0.3].[29]
Study limitations
Although previous studies have found that noncontact tonometry can be influenced by the central corneal thickness,[23,30] we did not evaluate implications of varying corneal thickness and the central thickness of CLs on IOP measured by the Corvis® ST. In addition, we did not measure IOP through silicone hydrogel CLs, which are the most frequently used extended wear therapeutic lens.
In summary, our results have shown that the IOP measurements in healthy eyes by the Corvis® ST were not affected by soft CLs and were reproducible. The device could, therefore, be an invaluable useful tool in the pre- and post-operative IOP measurement in patients undergoing refractive surgery. It may prove to be invaluable in those cases where measuring IOP over a CL is necessary, such as in patients with bandage CLs. Patients with corneal pathology such bullous keratopathy, abrasions or ulcers could benefit from IOP measurements over a CL as the CL would serve as a buffer and hence protect the cornea. Furthermore, the use of anesthetic drops can be avoided, making further corneal evaluation possible. Additional studies are needed to evaluate the accuracy of the Corvis® ST readings over different CL powers and in diseases like glaucoma.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma: Clinical and experimental concepts. Clin Experiment Ophthalmol. 2012;40:341–9. doi: 10.1111/j.1442-9071.2012.02773.x. [DOI] [PubMed] [Google Scholar]
- 2.Thylefors B, Négrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ. 1995;73:115–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Le A, Mukesh BN, McCarty CA, Taylor HR. Risk factors associated with the incidence of open-angle glaucoma: The visual impairment project. Invest Ophthalmol Vis Sci. 2003;44:3783–9. doi: 10.1167/iovs.03-0077. [DOI] [PubMed] [Google Scholar]
- 4.Jorge J, González-Méijome JM, Díaz-Rey JA, Almeida JB, Ribeiro P, Parafita MA. Clinical performance of non-contact tonometry by Reichert AT550 in glaucomatous patients. Ophthalmic Physiol Opt. 2003;23:503–6. doi: 10.1046/j.1475-1313.2003.00139.x. [DOI] [PubMed] [Google Scholar]
- 5.Goldmann H, Schmidt T. Applanation tonometry. Ophthalmologica. 1957;134:221–42. doi: 10.1159/000303213. [DOI] [PubMed] [Google Scholar]
- 6.Sudesh S, Moseley MJ, Thompson JR. Accuracy of Goldmann tonometry in clinical practice. Acta Ophthalmol (Copenh) 1993;71:185–8. doi: 10.1111/j.1755-3768.1993.tb04988.x. [DOI] [PubMed] [Google Scholar]
- 7.Whitacre MM, Stein R. Sources of error with use of Goldmann-type tonometers. Surv Ophthalmol. 1993;38:1–30. doi: 10.1016/0039-6257(93)90053-a. [DOI] [PubMed] [Google Scholar]
- 8.Argus WA. Ocular hypertension and central corneal thickness. Ophthalmology. 1995;102:1810–2. doi: 10.1016/s0161-6420(95)30790-7. [DOI] [PubMed] [Google Scholar]
- 9.Khan JA, Graham CE. Effect of contact lens removal or displacement on intraocular pressure. Arch Ophthalmol. 1991;109:825–8. doi: 10.1001/archopht.1991.01080060089031. [DOI] [PubMed] [Google Scholar]
- 10.Panek WC, Boothe WA, Lee DA, Zemplenyi E, Pettit TH. Intraocular pressure measurement with the Tono-Pen through soft contact lenses. Am J Ophthalmol. 1990;109:62–5. doi: 10.1016/s0002-9394(14)75580-1. [DOI] [PubMed] [Google Scholar]
- 11.Rossini L, Pè ME, Frova C, Hein K, Sari-Gorla M. Molecular analysis and mapping of two genes encoding maize glutathione S-transferases (GST I and GST II) Mol Gen Genet. 1995;248:535–9. doi: 10.1007/BF02423448. [DOI] [PubMed] [Google Scholar]
- 12.Scibilia GD, Ehlers WH, Donshik PC. The effects of therapeutic contact lenses on intraocular pressure measurement. CLAO J. 1996;22:262–5. [PubMed] [Google Scholar]
- 13.Allen RJ, Dev Borman A, Saleh GM. Applanation tonometry in silicone hydrogel contact lens wearers. Cont Lens Anterior Eye. 2007;30:267–9. doi: 10.1016/j.clae.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Sugimoto-Takeuchi R, Yamamoto R, Kuwayama Y, Kinoshita S. Effect of intraocular pressure measurement through therapeutic soft contact lenses by noncontact tonometer. Nihon Ganka Gakkai Zasshi. 1991;95:869–72. [PubMed] [Google Scholar]
- 15.Reznicek L, Muth D, Kampik A, Neubauer AS, Hirneiss C. Evaluation of a novel Scheimpflug-based non-contact tonometer in healthy subjects and patients with ocular hypertension and glaucoma. Br J Ophthalmol. 2013;97:1410–4. doi: 10.1136/bjophthalmol-2013-303400. [DOI] [PubMed] [Google Scholar]
- 16.Bañeros-Rojas P, Martinez de la Casa JM, Arribas-Pardo P, Berrozpe-Villabona C, Toro-Utrera P, García-Feijoó J. Comparison between Goldmann, Icare Pro and Corvis ST tonometry. Arch Soc Esp Oftalmol. 2014;89:260–4. doi: 10.1016/j.oftal.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Hong J, Xu J, Wei A, Deng SX, Cui X, Yu X, et al. A new tonometer - The Corvis ST tonometer: Clinical comparison with noncontact and Goldmann applanation tonometers. Invest Ophthalmol Vis Sci. 2013;54:659–65. doi: 10.1167/iovs.12-10984. [DOI] [PubMed] [Google Scholar]
- 18.Hon Y, Lam AK. Corneal deformation measurement using Scheimpflug noncontact tonometry. Optom Vis Sci. 2013;90:e1–8. doi: 10.1097/OPX.0b013e318279eb87. [DOI] [PubMed] [Google Scholar]
- 19.Ambrósio R, Jr, Nogueira LP, Caldas DL, Fontes BM, Luz A, Cazal JO, et al. Evaluation of corneal shape and biomechanics before LASIK. Int Ophthalmol Clin. 2011;51:11–38. doi: 10.1097/IIO.0b013e31820f1d2d. [DOI] [PubMed] [Google Scholar]
- 20.Jr A. Corneal biomechanical assessment using dynamic ultra high-speed scheimpflug technology non contact tonometry. San Diego: ASCRS; 2011. [Google Scholar]
- 21.Valbon BF, Ambrósio R, Jr, Fontes BM, Luz A, Roberts CJ, Alves MR. Ocular biomechanical metrics by CorVis ST in healthy Brazilian patients. J Refract Surg. 2014;30:468–73. doi: 10.3928/1081597X-20140521-01. [DOI] [PubMed] [Google Scholar]
- 22.Firat PG, Cankaya C, Doganay S, Cavdar M, Duman S, Ozsoy E, et al. The influence of soft contact lenses on the intraocular pressure measurement. Eye (Lond) 2012;26:278–82. doi: 10.1038/eye.2011.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogbuehi KC. The influence of lens power and center thickness on the intraocular pressure measured through soft lenses: A comparison of two noncontact tonometers. Cont Lens Anterior Eye. 2012;35:118–28. doi: 10.1016/j.clae.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 24.Insler MS, Robbins RG. Intraocular pressure by noncontact tonometry with and without soft contact lenses. Arch Ophthalmol. 1987;105:1358–9. doi: 10.1001/archopht.1987.01060100060025. [DOI] [PubMed] [Google Scholar]
- 25.Patel S, Illahi W. Non-contact tonometry over soft contact lenses: Effect of contact lens power on the measurement of intra-ocular pressure. Cont Lens Anterior Eye. 2004;27:33–7. doi: 10.1016/j.clae.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Zeri F, Calcatelli P, Donini B, Lupelli L, Zarrilli L, Swann PG. The effect of hydrogel and silicone hydrogel contact lenses on the measurement of intraocular pressure with rebound tonometry. Cont Lens Anterior Eye. 2011;34:260–5. doi: 10.1016/j.clae.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Lim L, Ng TP, Tan DT. Accurate intraocular pressure measurement in contact lens wearers with normal pressures. CLAO J. 1997;23:130–3. [PubMed] [Google Scholar]
- 28.Nosch DS, Duddek AP, Herrmann D, Stuhrmann OM. Dynamic Contour Tonometry (DCT) over a thin daily disposable hydrogel contact lens. Cont Lens Anterior Eye. 2010;33:219–24. doi: 10.1016/j.clae.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Gomes BA, Turiel P, Cavalcanti RS, Moraes HV, Jr, Santhiago MR. The accuracy of Goldmann applanation tonometry over silicone hydrogel contact lenses in patients with glaucoma. Cont Lens Anterior Eye. 2014;37:297–9. doi: 10.1016/j.clae.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 30.Pelit A, Altan-Yaycioglu R, Pelit A, Akova YA. Effect of corneal thickness on intraocular pressure measurements with the Pascal dynamic contour, Canon TX-10 non-contact and Goldmann applanation tonometers in healthy subjects. Clin Exp Optom. 2009;92:14–8. doi: 10.1111/j.1444-0938.2008.00299.x. [DOI] [PubMed] [Google Scholar]


