Abstract
Background
A variety of in‐service emergency care training courses are currently being promoted as a strategy to improve the quality of care provided to seriously ill newborns and children in low‐income countries. Most courses have been developed in high‐income countries. However, whether these courses improve the ability of health professionals to provide appropriate care in low‐income countries remains unclear. This is the first update of the original review.
Objectives
To assess the effects of in‐service emergency care training on health professionals' treatment of seriously ill newborns and children in low‐income countries.
Search methods
For this update, we searched the Cochrane Database of Systematic Reviews, part of The Cochrane Library (www.cochranelibrary.com); MEDLINE, Ovid SP; EMBASE, Ovid SP; the Cochrane Central Register of Controlled Trials (CENTRAL), part of The Cochrane Library (www.cochranelibrary.com) (including the Cochrane Effective Practice and Organisation of Care (EPOC) Group Specialised Register); Science Citation Index and Social Sciences Citation Index, Institute for Scientific Information (ISI) Web of Knowledge/Science and eight other databases. We performed database searches in February 2015. We also searched clinical trial registries, websites of relevant organisations and reference lists of related reviews. We applied no date, language or publication status restrictions when conducting the searches.
Selection criteria
Randomised trials, non‐randomised trials, controlled before and after studies and interrupted‐time‐series studies that compared the effects of in‐service emergency care training versus usual care were eligible for inclusion. We included only hospital‐based studies and excluded community‐based studies. Two review authors independently screened and selected studies for inclusion.
Data collection and analysis
Two review authors independently extracted data and assessed study risk of bias and confidence in effect estimates (certainty of evidence) for each outcome using GRADE (Grades of Recommendation, Assessment, Development and Evaluation). We described results and presented them in GRADE tables.
Main results
We identified no new studies in this update. Two randomised trials (which were included in the original review) met the review eligibility criteria. In the first trial, newborn resuscitation training compared with usual care improved provider performance of appropriate resuscitation (trained 66% vs usual care 27%, risk ratio 2.45, 95% confidence interval (CI) 1.75 to 3.42; moderate certainty evidence) and reduced inappropriate resuscitation (trained mean 0.53 vs usual care 0.92, mean difference 0.40, 95% CI 0.13 to 0.66; moderate certainty evidence). Effect on neonatal mortality was inconclusive (trained 28% vs usual care 25%, risk ratio 0.77, 95% CI 0.40 to 1.48; N = 27 deaths; low certainty evidence). Findings from the second trial suggest that essential newborn care training compared with usual care probably slightly improves delivery room newborn care practices (assessment of breathing, preparedness for resuscitation) (moderate certainty evidence).
Authors' conclusions
In‐service neonatal emergency care courses probably improve health professionals' treatment of seriously ill babies in the short term. Further multi‐centre randomised trials evaluating the effects of in‐service emergency care training on long‐term outcomes (health professional practice and patient outcomes) are needed.
Plain language summary
In‐service training for health professionals to improve care of seriously ill newborns and children in low‐income countries
What question was the review asking?
This is the first update of the original Cochrane review, whose objective was to find out whether additional emergency care training programmes can improve the ability of health workers in poor countries to care for seriously ill newborns and children admitted to hospitals. Researchers at The Cochrane Collaboration searched for all studies that could answer this question and found two relevant studies.
What are the key messages?
The review authors suggest that giving health professionals in poor countries additional training in emergency care probably improves their ability to care for seriously ill newborns. We need additional high‐quality studies, including studies in which health professionals are trained to care for seriously ill older children.
Background: training health professionals to care for seriously ill babies and children
In poor countries, many babies and children with serious illnesses die even though they have been cared for in hospitals. One reason for this may be that health workers in these countries often are not properly trained to offer the care that these children need.
In poor countries, children often become seriously ill because of conditions such as pneumonia, meningitis and diarrhoea, and may need emergency care. For newborn babies, the most common reason for emergency care is too little oxygen to the baby during birth. If this goes on for too long, the person delivering the baby has to help the baby breathe, and sometimes has to get the baby’s heart rate back to normal. This is called neonatal resuscitation.
Neonatal resuscitation is a skilled task, and the health worker needs proper training. As babies need to be resuscitated quickly, the health worker needs to know how to prepare for this before the baby is born. For instance, he or she needs to know how to prepare the room and proper equipment. Health workers in poor countries often do not have these skills, and these babies are likely to die. Babies can also be harmed if the health worker does not resuscitate the baby correctly.
Several training programmes have been developed to teach health workers how to give emergency care to seriously ill babies and children. But most of these have been developed and tested in wealthy countries, and we don’t know whether they would work in poor countries.
What happens when health professionals in poor countries are given extra training?
The review authors found two relevant studies. These studies compared the practices of health professionals who had been given extra training in the care of newborns with the practices of health professionals who did not receive extra training.
In the first study, nurses at a maternity hospital in Kenya completed a one‐day training course on how to resuscitate newborn babies. This course was adapted from the UK Resuscitation Council, and it included lectures and practical training. The study suggests that after these training courses:
• health professionals are probably more likely to resuscitate newborn babies correctly (moderate certainty of the evidence); and
• newborn babies may be less likely to die while being resuscitated (low certainty of the evidence).
In the second study, doctors, nurses and midwives in five Sri Lankan hospitals were given a four‐day training course on how to prepare for and provide care for newborns. This course was adapted from the World Health Organization (WHO) Training Modules on Essential Newborn Care and Breastfeeding, and included lectures, demonstrations, hands‐on training and small group discussions. This study suggests that after these training courses:
• health professionals probably are more likely to be well prepared to resuscitate newborn babies (moderate certainty of the evidence).
Unfortunately, the two studies followed up with health professionals for only two to three months after they received training. We therefore don’t know if the benefits of the training courses lasted over time.
The review authors found no studies that looked at the effects of training programmes on the care of older children.
How up‐to‐date is this review?
Review authors searched for studies that had been published up to February 2015.
Summary of findings
for the main comparison.
| In‐service neonatal emergency care training versus usual care for healthcare professionals | |||||
|
Population: nurses and midwives Setting: delivery room/theatre (Kenya) Intervention: 1‐day newborn resuscitation training Comparison: usual care | |||||
| Outcomes | Absolute effect* (95% CI) |
Relative effect (95% CI) |
Number of resuscitation practices (studies) | Certainty of the evidence (GRADE)¶ | |
| Without training (usual care) | With in‐service training | ||||
|
Health workers' resuscitation practices: proportion of adequate initial resuscitation practices Direct observation Follow‐up: 50 days |
27 per 100 | 66 per 100 (47 to 92) | RR 2.45 (1.75 to 3.42) | 212 (1 study) | ⊕⊕⊕⊝a* Moderate |
| Difference: 39 more adequate resuscitation practices per 100 resuscitation practices (from 20 more to 65 more) | |||||
|
Health workers' resuscitation practices: inappropriate and potentially harmful practices per resuscitation Direct observation Scale: 0 to 1 (better indicated by lower values) Follow‐up: 50 days |
Mean: 0.92 | Mean: 0.53 Mean difference: 0.40 (0.13 to 0.66) |
‐ | 212 (1 study) | ⊕⊕⊕⊝a* Moderate |
|
Neonatal mortality in all resuscitation episodes Medical records (resuscitation observation sheet) Follow‐up: 50 days |
36 per 100 | 28 per 100 (14 to 53) | RR 0.77 (0.40 to 1.48) | 90 (1 study) | ⊕⊕⊝⊝a,b* Low |
| Difference: 8 fewer deaths per 100 resuscitation episodes (from 22 fewer to 17 more) | |||||
| CI: Confidence interval; RR: Risk ratio; GRADE: GRADE Working Group grades of evidence. *The risk WITHOUT the intervention is based on control group risk. The corresponding risk WITH the intervention (and the 95% confidence interval for the difference) is based on the overall relative effect (and its 95% confidence interval). | |||||
|
aDowngraded from high to moderate because of risk of bias (details about allocation sequence generation and concealment were not reported in the article; potential cross‐group contamination cannot be excluded). bDowngraded from moderate to low because of imprecision (few events, N = 27 deaths). *See Appendix 2 for evidence profile (detailed judgements on certainty of evidence). | |||||
| About the certainty of the evidence (GRADE).† High: This research provides a very good indication of the likely effect. The likelihood that the effect will be substantially different‡ is low. Moderate: This research provides a good indication of the likely effect. The likelihood that the effect will be substantially different‡ is moderate. Low: This research provides some indication of the likely effect. However, the likelihood that it will be substantially different‡ is high. Very low: This research does not provide a reliable indication of the likely effect. The likelihood that the effect will be substantially different‡ is very high. †This is sometimes referred to as ‘quality of evidence’ or ‘confidence in the estimate’. ‡Substantially different = a large enough difference that it might affect a decision. | |||||
2.
| In‐service neonatal emergency care training versus standard care for healthcare professionals | ||||
|
Participants: doctors, nurses and midwives Settings: delivery room (Sri Lanka) Intervention: 4‐day essential newborn care training Comparison: usual care | ||||
| Outcomes | Absolute effect* (95% CI) | Relative effect (95% CI) | Certainty of the evidence (GRADE)†¶ | |
| Without training (usual care) | With in‐service training | |||
|
Preparedness for resuscitation‡ Scale: 0 to 100% (better indicated by higher values) Follow‐up: 90 days |
Mean percentage: 10.46% | Mean percentage: 19.29% Mean percentage change: 8.83% (6.41% to 11.25%) |
‐ | ⊕⊕⊕⊝a§ Moderate |
| CI: Confidence interval; RR: Risk ratio; GRADE: GRADE Working Group grades of evidence. * The risk WITHOUT the intervention is based on the control group risk. The corresponding risk WITH the intervention (and the 95% confidence interval for the difference) is based on the overall relative effect (and its 95% confidence interval). | ||||
| †About the certainty of the evidence (GRADE).¶ High: This research provides a very good indication of the likely effect. The likelihood that the effect will be substantially different# is low. Moderate: This research provides a good indication of the likely effect. The likelihood that the effect will be substantially different# is moderate. Low: This research provides some indication of the likely effect. However, the likelihood that it will be substantially different# is high. Very low: This research does not provide a reliable indication of the likely effect. The likelihood that the effect will be substantially different# is very high. ‡Improvement also observed in assessment of breathing (however, re‐analysis to calculate intervention effect was not done owing to baseline imbalance between study groups). §See Appendix 3 for evidence profile (detailed judgements of certainty of evidence). ¶This is sometimes referred to as ‘quality of evidence’ or ‘confidence in the estimate’. #Substantially different = a large enough difference that it might affect a decision. | ||||
| aDowngraded from high to moderate because of risk of bias (methods of allocation sequence generation and concealment were not reported; 'unit of analysis error' was present). | ||||
Background
In low‐income countries, most deaths among seriously ill children who come into contact with referral level health services occur within 48 hours of when they are seen (Berkley 2005). It is possible that good quality immediate and effective care provided by health professionals could reduce these deaths (Nolan 2001). Provision of appropriate care however depends on the presence of skilled health personnel at the point of care delivery (WHO 2005). To improve health workers' capacity to provide effective care for seriously ill newborns and children in low‐income countries, various in‐service training courses, based mainly on models of high‐income countries, are proposed. This is the first update of the original review.
Description of the condition
Severe illness remains a leading cause of newborn and child deaths in low‐income countries (LICs) (Liu 2012; Seale 2014). Major conditions contributing to severe illness include sepsis, pneumonia, meningitis and diarrhoea (Liu 2012; Seale 2014). Early recognition of severe illness with prevention of cardiorespiratory arrest through resuscitation represents a critical step towards reducing mortality and long‐term disability in seriously ill newborns and children. However, the clinical diagnosis of severe illness can be difficult, as signs are often non‐specific and deteriorate rapidly.
Description of the intervention
A variety of in‐service emergency courses for care of seriously ill newborns and children are available. These courses include (1) neonatal life support courses (e.g. Newborn Life Support (NLS), Neonatal Resuscitation Programme (NRP)); (2) paediatric life support courses (e.g. Paediatric Advanced Life Support (PALS), Paediatric Life Support (PLS)); (3) life support/emergency care elements within the Integrated Management of Pregnancy and Childbirth programme (e.g. Essential Newborn Care (ENC)); and (4) components of other in‐service child health training courses that deal with the care of children with serious illness (e.g. Emergency Triage, Assessment and Treatment (ETAT), Control of Diarrheal Diseases (CDD), and Acute Respiratory Infection (ARI) case management programmes; training components of the Integrated Management of Childhood Illness (IMCI) strategy) (Table 3).
1. Summary of in‐service neonatal and paediatric emergency care courses*.
| Course | Content | Duration (days) | Target audience |
| Neonatal Life Support (NLS) | Neonatal resuscitation | 1 | Midwives, paediatricians, general practitioners |
| Neonatal Resuscitation Programme (NRP) | Neonatal resuscitation | 1 | Midwives, paediatricians, general practitioners |
| Paediatric Life Support (PLS) | Basic Life Support (BLS) and Advanced Life Support (ALS) for children; recognition of paediatric emergencies | 1 | Nurses and doctors involved in paediatric care |
| Paediatric Advanced Life Support (PALS) | BLS and ALS for children; recognition of paediatric emergencies; some neonatal life support | 2 | Nurses and doctors involved in paediatric care |
| Prehospital Paediatric Life Support (PHPLS) | Prehospital paediatric emergency care | 2+ | General practitioners, paramedics, some nurses, emergency medicine staff |
| Advanced Paediatric Life Support (APLS) | BLS and ALS for children; paediatric emergencies, including serious illness and major trauma, some neonatal life support | 3 | Paediatricians, emergency medicine doctors, some anaesthetists, senior paediatric nurses |
| Emergency Triage Assessment and Treatment (ETAT) | Very ill children presenting to hospital | 3.5 | Doctors, nurses, paramedics |
| Essential Newborn Care Course (ENC) | Aspects of newborn care (including neonatal resuscitation) in the Integrated Management of Pregnancy and Childbirth (IMPAC) | 5 | Nurses, midwives, doctors |
| Integrated Management of Childhood Illness (IMCI) | Ill children and neonates including emergency care or identification and referral of the seriously ill | 11 | Nurses, midwives, doctors |
Although such formalised educational programmes vary in origin, scope and target audience, they typically are aimed at in‐service rather than preservice training, and are short and intensive with a structured approach to presentation of the clinical subject. The one‐day NRP course was first taught in 1987 in the USA, and the one‐day NLS course was initiated in the UK in 2001 (Raupp 2007). PALS, a two‐day course, was piloted in the USA in 1988. Advanced Paediatric Life Support (APLS), a three‐day course, was developed and piloted in the UK in 1992. Two other courses ‐ the one‐day PLS course and Prehospital PLS ‐ have been designed to complement the APLS (Jewkes 2003). The World Health Organization (WHO) has added to this list the three and one‐half‐day ETAT course based on and validated against the APLS course in Malawi (Gove 1999; Molyneux 2006). This course is specifically aimed at low‐income countries and is intended to improve prompt identification and institution of life‐saving emergency treatment for very ill children.
The more general CDD and ARI programmes were developed by the WHO in 1980, in recognition of high childhood mortality due to diarrhoea/dehydration and pneumonia among very ill neonates and children; they focus on case management training rather than life support (Forsberg 2007; Pio 2003). Although these courses concentrate on community‐based or out‐patient‐based management, with good evidence for their success (Sazawal 2001), they also include guidance on management of very severe illness. These disease‐specific training approaches were incorporated into the broader package of the IMCI strategy. Here the particular focus for management of the very ill child is the decision to provide prereferral care and referral to hospital. In addition to this, the WHO has developed a specific five‐day course on hospital management of severe malnutrition (WHO 2002).
How the intervention might work
The effectiveness of in‐service training of healthcare professionals depends on changes in health worker practices, which, plausibly, should precede any impact on mortality or morbidity.
Why it is important to do this review
In‐service training costs both time and money, for example, the cost of the two‐day European Paediatric Life Support (EPLS) course is estimated to be about USD 190 per trainee in Kenya (personal communication with ME, 2009). Apart from the sometimes high costs of providing courses (often recovered in high‐income countries with high course fees), attendance at such courses often means that important staff are absent from their normal duties with potential disruption to patient care and, for some, loss of personal income (Jabbour 1996). Despite their high costs, emergency care courses remain a thriving enterprise in many high‐income countries, as is reflected in their ever increasing number and variety (Jewkes 2003). In the hope that they might improve the quality of care in low‐ and middle‐income countries, considerable global efforts and investments have gone into further development, refinement and adaptation of these courses to meet the needs of individual countries (Baskett 2005). Yet despite these investments and the faith placed in them by many organisations and institutions, evidence of their effectiveness in improving treatment of seriously ill newborns and children remains unclear. Several studies on in‐service emergency care training for newborns and children have been completed since our original review was published, in 2010. Therefore an updated review of the effectiveness of these courses is needed.
Objectives
To assess the effects of in‐service emergency care training on health professionals' treatment of seriously ill newborns and children in low‐income countries.
Methods
Criteria for considering studies for this review
Types of studies
Randomised trials, non‐randomised trials, controlled before‐after studies and interrupted‐time‐series studies were eligible for inclusion (EPOC 2014). We excluded community‐based studies.
Types of participants
Qualified healthcare professionals (doctors, nurses, midwives, physician assistants) in outpatient/hospital‐based settings responsible for care of seriously ill newborns and children were eligible for inclusion. We excluded non‐qualified healthcare providers (e.g. medical students/trainees, medical interns, community health workers). We did not exclude studies on the basis of their income classification (low, middle or high income).
Types of interventions
In‐service training courses aimed at changing health provider behaviour in the care of seriously ill newborns and children were eligible for inclusion (Table 3).
Neonatal life support courses (e.g. NLS, NRP).
Paediatric life support courses (e.g. PALS, PLS).
Life support elements within the Integrated Management of Pregnancy and Childbirth (e.g. ENC).
Other in‐service newborn and child health training courses aimed at recognition and management of seriously ill newborns and children (e.g. ETAT, CDD, ARI, malaria case management, training components of IMCI strategy).
We excluded studies of complex training interventions in which training was combined with and was impossible to separate from additional health system changes (e.g. improved staffing, health facility reorganisation).
Types of outcome measures
Primary outcomes
We included studies only if they reported objectively measured health professional (in practice) performance outcomes (e.g. clinical assessment/diagnosis, recognition and management/referral of seriously ill newborn/child, prescribing practices).
Secondary outcomes
We also considered the following outcomes when reported.
Participant outcomes (e.g. mortality, morbidity).
Health resource utilisation (e.g. drug use, laboratory tests).
Health services utilisation (e.g. length of hospital stay).
Other markers of clinical performance (e.g. simulated health worker performance in practice settings).
Training/implementation costs.
Impact on equity.
Adverse effects.
We excluded studies that reported only other markers of performance/simulations/skill testing done outside practice settings/in classrooms (e.g. practicing/demonstrating resuscitation techniques using a dummy). We considered for inclusion simulations of emergency care in practice settings that were designed to reflect real practice.
Search methods for identification of studies
Electronic searches
We searched the following databases for related reviews.
Cochrane Database of Systematic Reviews (CDSR) (2015, Issue 2), part of The Cochrane Library (www.cochranelibrary.com) (searched 24/02/2015).
Database of Abstracts of Reviews of Effects (DARE) (2015, Issue 1), part of The Cochrane Library (www.cochranelibrary.com) (searched 24/02/2015).
Health Technology Assessment Database (HTA) (2015, Issue 1), part of The Cochrane Library (www.cochranelibrary.com) (searched 24/02/2015).
We searched the following databases for primary studies.
Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 1), part of The Cochrane Library (www.cochranelibrary.com) (including the Effective Practice and Organisation of Care (EPOC) Register) (searched 24/02/2015).
MEDLINE In‐Process and Other Non‐Indexed Citations, and MEDLINE daily, MEDLINE and OLDMEDLINE, 1946 to present, Ovid SP (searched 23/02/2015).
EMBASE, 1980 to 2015 Week 08, Ovid SP (searched 23/02/2015).
Cumulative Index to Nursing and Allied Health Literature (CINAHL), 1981 to present, EBSCOHost (searched 24/02/2015).
Education Resources Information Center (ERIC), 1966 to present, ProQuest (searched 24/02/2015).
World Health Organization Library Information System (WHOLIS), WHO (searched 24/02/2015).
Latin American Caribbean Health Sciences Literature (LILACS), VIrtual Health Library (VHL) (searched 24/02/2015).
Science Citation Index, 1975 to present; Social Sciences Citation Index, 1975 to present; Institute for Scientific Information (ISI) Web of Science (searched 24/02/2015) for papers that cite included studies.
We developed search strategies for electronic databases using the methodological component of the EPOC search strategy combined with selected Medical Subject Heading (MeSH) terms and free‐text terms. We applied no date, language or publication status restrictions. See Appendix 1 for strategies used.
Searching other resources
We also searched clinical trial registries (https://clinicaltrials.gov/, the WHO International Clinical Trials Registry Platform (ICTRP, http://www.who.int/ictrp/en/), both searched 11/02/2014) and websites of relevant organisations (Helping Babies Breathe, http://www.helpingbabiesbreathe.org/, searched 11/02/2014). We used a combination of search terms derived from the MEDLINE search strategy. In addition, we screened reference lists of related reviews.
Data collection and analysis
Selection of studies
Review authors (NO and ME) independently screened the titles, abstracts and full texts of retrieved articles and applied the predefined study eligibility criteria to select studies. We resolved disagreements through discussion.
Data extraction and management
Review authors (NO and ME) independently extracted the following data using a modified EPOC data collection tool (EPOC 2014). We resolved disagreements by discussion.
Study characteristics (e.g. study design, sample size, setting).
Participants (e.g. number of healthcare providers randomly assigned, number of practices performed).
Intervention (e.g. type and duration of training courses)/co‐interventions.
Targeted health provider behaviour (e.g. resuscitation practices).
Outcome measures (e.g. proportion of providers with the event of interest in study groups).
Assessment of risk of bias in included studies
Review authors (NO and ME) independently assessed study risk of bias using the Cochrane risk of bias tool (Higgins 2011). Quality domains assessed included allocation sequence generation, allocation concealment, blinding of outcome assessors, completeness of participant follow‐up, handling of incomplete outcome data, protection against selective outcome reporting and contamination. We classified findings into three categories: low (low risk of bias for all key quality domains), high (high risk of bias for one or more key domains) and unclear risk of bias (unclear risk of bias for one or more key domains). We did not exclude studies on the basis of their risk of bias.
Data synthesis
Included studies assessed different interventions and outcomes. Meta‐analysis was therefore inappropriate. We undertook a structured synthesis of results.
In Senarath 2007, a unit of analysis error occurred; hospitals were randomly assigned and performance at deliveries was analysed, without adjustment for clustering. In addition, outcomes in intervention and control groups were not directly compared (comparisons were made within comparison groups before and after the intervention). Re‐analysis was possible for only one outcome ‐ preparedness for resuscitation ‐ for which baseline levels of resuscitation practices were comparable between study groups. In the re‐analysis, we assessed training effect by computing mean differences in outcomes, using reported standard deviations to estimate standard errors. To account for clustering, we assumed an intracluster correlation coefficient (ICC) of 0.015 (with a design effect of 1.129) that was based on published data (Rowe 2002).
Review authors (NO and ME) independently assessed the certainty of evidence for each outcome using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (Guyatt 2008). This approach classifies the certainty of evidence (defined as ‘the extent to which one can be confident that an estimate of effect or association is correct’) into one of four categories ('high', 'moderate', 'low' or 'very low'). We resolved disagreements on certainty ratings by discussion. We did not exclude studies on the basis of their GRADE certainty ratings; we took into account the certainty of evidence when synthesising overall findings. We report the results of certainty assessments in the 'Summary of findings tables' section.
Results
Description of studies
Results of the search
In the original review, 2480 references were identified. Of these, 2334 articles were excluded following a review of titles and abstracts. Reasons for exclusion included inappropriate study designs/interventions/outcomes; enrolment of trainee/community health workers; and enrolment of non‐paediatric patients. The full texts of 146 papers were retrieved for detailed eligibility assessment. Of these, eight studies were identified as potentially meeting the review inclusion criteria. Six were subsequently excluded. Overall, two studies were included: Opiyo 2008 and Senarath 2007.
In this review update, we identified a total of 4768 articles. We excluded 4754 articles after a review of titles and abstracts. We retrieved the full texts of 14 articles for detailed assessment. Of these, 14 articles were excluded because of ineligible study design or setting (n = 7 studies), participants (n = 1 study) and outcomes (n = 6 studies). We identified no ongoing studies. No new studies met all of the review eligibility criteria. The study flow diagram is presented in Figure 1.
1.
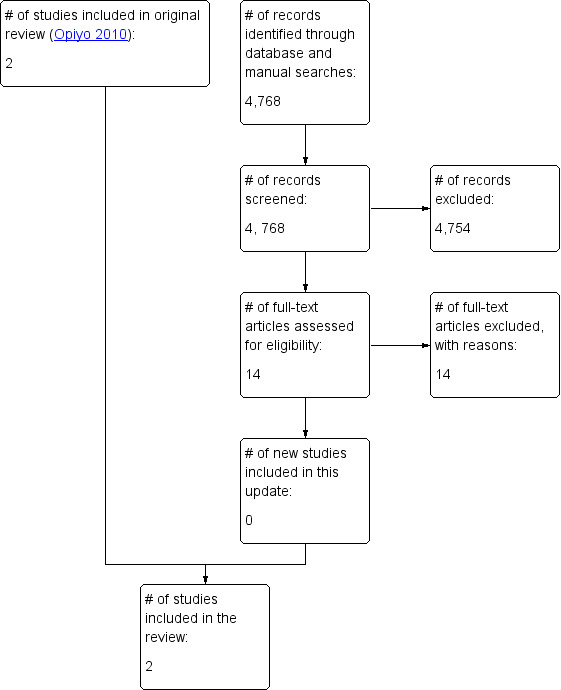
Study flow diagram.
Included studies
Both studies were randomised trials done in delivery rooms/theatres in Kenya (Opiyo 2008) and Sri Lanka (Senarath 2007). Healthcare providers were nurses in Opiyo 2008 and were mixed (doctors, nurses, midwives) in Senarath 2007. Targeted behaviours included newborn resuscitation (Opiyo 2008) and general management/preparation and conduct of delivery care for newborns (Senarath 2007). Postintervention data were collected over a period of 50 days in Opiyo 2008 and three months in Senarath 2007. Individual healthcare providers (n = 83) were randomly assigned in Opiyo 2008, and hospitals (n = 5) were randomly assigned in Senarath 2007. Both studies were adequately powered (90%) for primary outcomes. Neither study examined training/implementation costs.
Opiyo 2008 assessed the effects of one‐day newborn resuscitation training on health worker resuscitation practices in a maternity hospital in Kenya. The course, which was adapted from the UK Resuscitation Council,presented an A (airway), B (breathing), C (circulation) approach to resuscitation and laid down a clear step‐by‐step strategy for the first minutes of resuscitation at birth. Training included focused lectures and practical scenario sessions in which infant manikins were used. Participants were provided a course manual two weeks before training for self learning. Participants were randomly allocated to receive early training (n = 28) or late training (control group, n = 55). Data were collected on 97 and 115 resuscitation episodes over seven weeks after early and late training, respectively.
Senarath 2007 assessed the effects of four‐day essential newborn care training on health provider practices in hospitals in Sri Lanka. The course was adapted from the WHO Training Modules on Essential Newborn Care and Breastfeeding. Participants were provided teaching aids on newborn care and resuscitation. Training comprised lectures, demonstrations, hands‐on training and small group discussions. Hospitals were randomly assigned to intervention (n = 2 hospitals) and control groups (n = 3 hospitals). The main sample for data collection by exit interview included 446 mother/newborn pairs before intervention and 446 pairs after intervention (223 each in intervention and control groups). These exit interview data were not relevant to the topic of this review. Direct observations of delivery practices were made on a subsample consisting of 96 healthcare providers (48 before and 48 after the intervention). Postintervention data collection commenced three months after training.
Excluded studies
We eventually excluded 20 studies that initially met the review eligibility criteria. These are listed in the Characteristics of excluded studies table.
Six studies were excluded in the original review: Bryce 2005, a non‐randomised controlled study on health facility IMCI training, was excluded, as the training intervention was combined with and was impossible to separate from concurrent district health strengthening activities (skills reinforcement through supervised clinical practice). El‐Arifeen 2004, a cluster‐randomised trial on the effects of IMCI training on quality of care, was excluded, as data on referral rate (appropriate health worker response to an encounter with a seriously ill child and our outcome of interest) were not reported for seriously ill children. Gouws 2004, a cluster‐randomised trial on the effects of IMCI training on health worker antibiotic use, was excluded, as no baseline assessment of outcomes was performed. Nadel 2000, an intervention study of periodic mock resuscitations combined with an eight‐hour resuscitation course, was excluded, as it lacked a concurrent comparison group/used a historical control group. Two further studies were excluded, as they enrolled only apparently well children (Pelto 2004) or those with mild acute respiratory infection episodes (Ochoa 1996).
In this update, we excluded 14 studies because of ineligible designs (non‐randomised designs, uncontrolled before‐after designs, community‐based settings) (n = 6 studies) and inappropriate outcome measures/simulated provider practices (n = 8 studies).
Risk of bias in included studies
Both randomised trials had serious limitations. In Opiyo 2008, allocation sequence generation, concealment, blinding of outcome assessors, follow‐up of health providers and reporting of outcome measures were adequate (however, details about allocation sequence generation and concealment were not reported in the article). Potential cross‐group contamination in the trial cannot be excluded. In Senarath 2007, outcome data were completely reported and the study was adequately protected against contamination and selective outcome reporting. However, methods of allocation sequence generation and concealment were not reported. Baseline differences in health providers and outcomes were evident between study groups. Blinding of outcome assessment was inadequate, and the presence of a 'unit of analysis error' added further uncertainty regarding the results.
Effects of interventions
In Opiyo 2008, newborn resuscitation training improved health workers' resuscitation practices (trained 66% vs control 27%; risk ratio (RR) 2.45, 95% confidence interval (CI) 1.75 to 3.42) (moderate certainty evidence). Training also reduced the frequency of inappropriate/harmful resuscitation practices (trained 0.53 vs control 0.92; mean difference (MD) 0.40, 95% CI 0.13 to 0.66; Appendix 2) (moderate certainty evidence). Effects on neonatal mortality were inconclusive (trained 0.28 vs usual care 0.25; RR 0.77, 95% CI 0.40 to 1.48; N = 27 deaths; Figure 2) (low certainty evidence).
2.
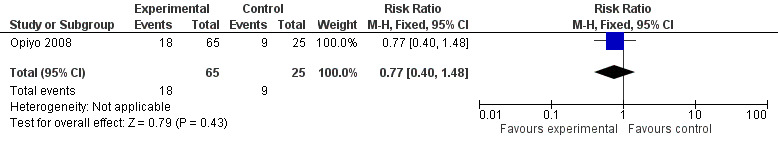
Forest plot of comparison: 2 Opiyo 2008, outcome: 2.1 Mortality.
In Senarath 2007, assessment of breathing of the newborn at birth and four of the five components of essential newborn care practices were improved in the intervention group after training, but it was possible to re‐analyse the data to compare intervention and control groups and to adjust for clustering for only one outcome: preparedness for resuscitation. Findings suggest that essential newborn care training probably slightly improves resuscitation preparedness (mean percentage change 8.83%, 95% CI 6.41% to 11.25%; Figure 3 and Figure 4) (moderate certainty evidence).
3.
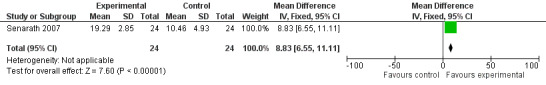
Forest plot of comparison: 1 Senarath 2007, outcome: 1.1 Practice of preparedness of resuscitation. Mean difference = mean percentage change.
4.
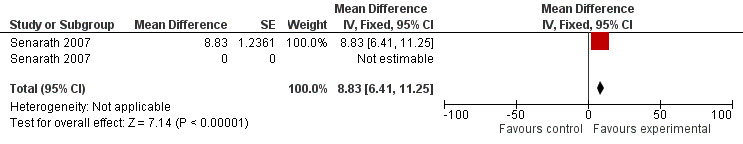
Forest plot of comparison: 1 Senarath 2007, outcome: 1.2 Preparedness for resuscitation ‐ adjusted for clustering. Mean difference = mean percentage change.
Discussion
This review found few well‐conducted studies on the effects of in‐service training aimed at improving care of the seriously ill newborn. Findings from the two included studies suggest a beneficial effect on health provider outcomes (resuscitation practices, assessment of breathing, resuscitation preparedness) in the short term. However, effects on neonatal mortality were inconclusive (although the only study that reported this outcome was underpowered to detect a mortality effect). Even though both included studies reported improvement in health provider practices after training, a generalisable conclusion of effectiveness cannot be inferred given the sparse data available and differences between training interventions and outcomes examined.
Reported benefits should be interpreted with caution. First, in Opiyo 2008, assessment of outcomes was conducted immediately after training for a short period (50 days). Therefore instantaneous improvement in provider performance could have been expected. Clinical skills have been shown to 'decay' over time, with as much as a 50% reduction in appropriate practice (as assessed in classroom simulations) within six months of intense training (McKenna 1985). Assessment of training effects over a longer time could have improved our confidence in the results. The potential for a ‘decay effect’ underscores the need for periodic refresher training to maintain recommended provider practice. Second, in Senarath 2007, a large number of health providers demonstrated appropriate newborn care practices at baseline. The narrow ‘performance improvement' gap possibly limited demonstration of the real impact of the training. Third, training coverage was low in Opiyo 2008 and unclear in Senarath 2007. Saturation training to the level of that reported in one excluded study (94%) (El‐Arifeen 2004) can potentially create a ‘herd effect’ on provider practices. Thus, possible mediation of reported effects by level of training coverage cannot be excluded. Finally, none of the included studies examined implementation costs. Thus, whether the observed benefits of training interventions are worth the costs remains uncertain.
The duration of training courses was varied (one‐day vs four‐day course). Apart from the clear effect on costs, training duration may modify their impact: One review (Rowe 2008) (n = 2 studies) found marginal effectiveness of standard IMCI training (≥ 11 days) compared with shortened IMCI training (five to 11 days). The complexity of the targeted behaviour may also modify training effects: Practices such as holding the baby upside during resuscitation may be easier to change than complex ones such as performing bag‐valve‐mask resuscitation. In Opiyo 2008, the teaching strategy consisted of focused lectures and practical scenario sessions using an infant manikin, and in Senarath 2007, the strategy involved lectures, demonstrations, hands‐on training and small group discussions. The format of training courses could influence their effect: One review found mixed interactive and didactic/lecture‐based educational meetings to be more effective than didactic meetings or interactive meetings (Forsetlund 2009).
The limited available evidence can be explained by several factors. First, a large number of studies were excluded on the basis of weak design (lack of appropriate controls, retrospective surveys). Most of the available evidence is therefore unreliable because of high risk of bias. Second, the lack of rigorous studies could be due to design and ethical challenges in the evaluation of educational interventions in practice settings. Desirable features such as protection against contamination cannot be fully achieved within routine clinical settings. In addition, random assignment of health providers and sick babies to a control arm and observation of practices performed by untrained providers raise clear ethical concerns. Third, effective sample sizes will always be difficult to achieve, as severe illness episodes and resuscitation events remain relatively uncommon events in practice. Large multi‐centre studies with relatively long observation periods would be needed to effectively assess the effects of emergency care courses. Apart from high costs, such studies would have to contend with the difficulty of securing continued availability and participation of health providers.
Findings of the present review are consistent with those of previous reviews (Jabbour 1996; Rowe 2008), which found limited evidence on the effectiveness of in‐service neonatal and paediatric emergency care courses.
Authors' conclusions
Implications for practice.
The findings of this review suggest that in‐service neonatal care courses probably improve health professional practices in caring for seriously ill newborns. Decisions to scale up these courses in low‐income countries must be based on consideration of costs and logistics associated with their implementation, including the need for adequate numbers of skilled instructors, appropriate locally adapted training materials and the availability of basic resuscitation equipment.
Implications for research.
Large pragmatic multi‐centre randomised trials (with appropriate controls and adequate randomisation procedures) evaluating the impact of emergency care in‐service training on long‐term outcomes (health professional practices and patient outcomes) are needed (given the current uncertainty on how long short‐term benefits are retained, particularly in settings in which they are used infrequently).
Such trials should:
involve direct head‐to‐head comparison of courses of varied length (e.g. one‐day vs four‐day courses);
aim to include children (in both out‐patient and hospital settings);
be preceded by pilot cost impact evaluation studies (given current uncertainty regarding the economic consequences of in‐service emergency care training); and
collect data on resource use and cost of training implementation (to optimise appropriate policy decisions regarding which interventions are worthy of investment).
To facilitate implementation and replication, studies should provide sufficient detail regarding their content (e.g. need for equipment, teamwork) and format (e.g. small group interactive vs lecture, hands‐on skills with dummies). Further studies are needed to determine optimal refresher training intervals for in‐service emergency care courses.
What's new
| Date | Event | Description |
|---|---|---|
| 10 March 2015 | New citation required but conclusions have not changed | We have included no new studies in this update. |
| 10 March 2015 | New search has been performed | This is the first update of the original review. We conducted a new search and updated content. |
History
Protocol first published: Issue 2, 2008 Review first published: Issue 4, 2010
| Date | Event | Description |
|---|---|---|
| 22 March 2010 | Amended | We have made minor edits. |
Acknowledgements
We would like to thank Marit Johansen for help with the literature searches and Andy Oxman for advice on the update process. NO is supported by funding from a Wellcome Trust Strategic Award (#084538). ME is funded by a Wellcome Trust Senior Fellowship (#097170).
Appendices
Appendix 1. Detailed search strategies
CDSR, The Cochrane Library
| ID | Search | Hits |
| #1 | MeSH descriptor: [Inservice Training] explode all trees | 567 |
| #2 | MeSH descriptor: [Health Personnel] explode all trees and with qualifier(s): [Education ‐ ED] | 1112 |
| #3 | MeSH descriptor: [Internship and Residency] this term only | 763 |
| #4 | (staff or employee* or clinician* or physician* or nurse* or midwif* or midwives or pharmacist* or specialist* or practitioner* or dietician* or dietitian* or nutritionist*) next (train* or course* or development or education or teach*):ti,ab,kw | 840 |
| #5 | (inservice or "in service" or "life support") near/2 (train* or course* or development or education or teach*):ti,ab,kw | 709 |
| #6 | ("on the job training" or internship or residency):ti,ab,kw | 1071 |
| #7 | (#1 or #2 or #3 or #4 or #5 or #6) | 3354 |
| #8 | MeSH descriptor: [Case Management] this term only | 651 |
| #9 | MeSH descriptor: [Critical Care] explode all trees | 1861 |
| #10 | MeSH descriptor: [Life Support Care] this term only | 85 |
| #11 | MeSH descriptor: [Critical Illness] this term only | 1232 |
| #12 | MeSH descriptor: [Acute Disease] this term only | 8984 |
| #13 | MeSH descriptor: [Emergency Medical Services] explode all trees | 2992 |
| #14 | MeSH descriptor: [Emergency Medicine] this term only | 216 |
| #15 | MeSH descriptor: [Emergency Treatment] explode all trees | 4066 |
| #16 | MeSH descriptor: [Emergency Nursing] this term only | 58 |
| #17 | "case management":ti,ab,kw | 1289 |
| #18 | (emergency near/2 (service* or medicine or nursing or triage)):ti,ab,kw | 3885 |
| #19 | "life support":ti,ab,kw | 484 |
| #20 | resuscitation:ti,ab,kw | 2730 |
| #21 | "first aid":ti,ab,kw | 129 |
| #22 | ((referral or urgent) near/2 care):ti,ab,kw | 573 |
| #23 | (critical* or emergency or intensive or serious* or sever* or acute*) near/2 (care or ill or illness* or treatment or therap* or disease*):ti,ab,kw | 62061 |
| #24 | (#8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23) | 69565 |
| #25 | MeSH descriptor: [Child] explode all trees | 135 |
| #26 | MeSH descriptor: [Infant] explode all trees | 13304 |
| #27 | MeSH descriptor: [Child Care] explode all trees | 867 |
| #28 | MeSH descriptor: [Pediatrics] explode all trees | 546 |
| #29 | MeSH descriptor: [Pediatric Nursing] explode all trees | 253 |
| #30 | MeSH descriptor: [Perinatal Care] this term only | 124 |
| #31 | MeSH descriptor: [Infant Death] this term only | 0 |
| #32 | MeSH descriptor: [Perinatal Death] this term only | 0 |
| #33 | (child* or infant* or pediatric* or paediatric* or perinat* or newborn* or new next born* or neonat* or baby or babies or kid or kids or toddler*):ti,ab,kw | 105756 |
| #34 | (#25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33) | 105756 |
| #35 | MeSH descriptor: [Pediatrics] explode all trees and with qualifier(s): [Education ‐ ED] | 155 |
| #36 | MeSH descriptor: [Pediatric Nursing] explode all trees and with qualifier(s): [Education ‐ ED] | 36 |
| #37 | (#35 or #36) | 188 |
| #38 | MeSH descriptor: [Emergency Medicine] explode all trees and with qualifier(s): [Education ‐ ED] | 86 |
| #39 | MeSH descriptor: [Emergency Nursing] this term only and with qualifier(s): [Education ‐ ED] | 9 |
| #40 | #38 or #39 | 95 |
| #41 | MeSH descriptor: [Intensive Care, Neonatal] this term only | 275 |
| #42 | MeSH descriptor: [Diarrhea, Infantile] this term only | 455 |
| #43 | MeSH descriptor: [Infant, Newborn, Diseases] explode all trees | 4391 |
| #44 | ("Acute Respiratory Infection" or "Acute Respiratory Infections"):ti,ab,kw | 287 |
| #45 | (#41 or #42 or #43 or #44) | 5308 |
| #46 | ("Control of Diarrheal Disease" or "Control of Diarrheal Diseases"):ti,ab,kw | 2 |
| #47 | Neonatal next Resuscitation next Program*:ti,ab,kw | 30 |
| #48 | "Essential Newborn Care":ti,ab,kw | 22 |
| #49 | "Integrated Management of Childhood Illness":ti,ab,kw | 26 |
| #50 | (#46 or #47 or #48 or #49) | 76 |
| #51 | #7 and #24 and #34 | 140 |
| #52 | #24 and #37 | 50 |
| #53 | #34 and #40 | 23 |
| #54 | #7 and #45 | 20 |
| #55 | #50 or #51 or #52 or #53 or #54 in Cochrane Reviews (Reviews and Protocols) | 14 |
CENTRAL; DARE; HTA, The Cochrane Library
| ID | Search | Hits |
| #1 | MeSH descriptor: [Inservice Training] explode all trees | 567 |
| #2 | MeSH descriptor: [Health Personnel] explode all trees and with qualifier(s): [Education ‐ ED] | 1112 |
| #3 | MeSH descriptor: [Internship and Residency] this term only | 763 |
| #4 | (staff or employee* or clinician* or physician* or nurse* or midwif* or midwives or pharmacist* or specialist* or practitioner* or dietician* or dietitian* or nutritionist*) next (train* or course* or development or education or teach*) | 1507 |
| #5 | (inservice or "in service" or "life support") near/2 (train* or course* or development or education or teach*) | 755 |
| #6 | ("on the job training" or internship or residency) | 1318 |
| #7 | (#1 or #2 or #3 or #4 or #5 or #6) | 4091 |
| #8 | MeSH descriptor: [Case Management] this term only | 651 |
| #9 | MeSH descriptor: [Critical Care] explode all trees | 1861 |
| #10 | MeSH descriptor: [Life Support Care] this term only | 85 |
| #11 | MeSH descriptor: [Critical Illness] this term only | 1232 |
| #12 | MeSH descriptor: [Acute Disease] this term only | 8984 |
| #13 | MeSH descriptor: [Emergency Medical Services] explode all trees | 2992 |
| #14 | MeSH descriptor: [Emergency Medicine] this term only | 216 |
| #15 | MeSH descriptor: [Emergency Treatment] explode all trees | 4066 |
| #16 | MeSH descriptor: [Emergency Nursing] this term only | 58 |
| #17 | "case management" | 1625 |
| #18 | (emergency near/2 (service* or medicine or nursing or triage)) | 6233 |
| #19 | "life support" | 582 |
| #20 | resuscitation | 3357 |
| #21 | "first aid" | 181 |
| #22 | ((referral or urgent) near/2 care) | 724 |
| #23 | (critical* or emergency or intensive or serious* or sever* or acute*) near/2 (care or ill or illness* or treatment or therap* or disease*) | 78684 |
| #24 | (#8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23) | 86892 |
| #25 | MeSH descriptor: [Child] explode all trees | 135 |
| #26 | MeSH descriptor: [Infant] explode all trees | 13304 |
| #27 | MeSH descriptor: [Child Care] explode all trees | 867 |
| #28 | MeSH descriptor: [Pediatrics] explode all trees | 546 |
| #29 | MeSH descriptor: [Pediatric Nursing] explode all trees | 253 |
| #30 | MeSH descriptor: [Perinatal Care] this term only | 124 |
| #31 | MeSH descriptor: [Infant Death] this term only | 0 |
| #32 | MeSH descriptor: [Perinatal Death] this term only | 0 |
| #33 | (child* or infant* or pediatric* or paediatric* or perinat* or newborn* or new next born* or neonat* or baby or babies or kid or kids or toddler*) | 120110 |
| #34 | (#25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33) | 120110 |
| #35 | MeSH descriptor: [Pediatrics] explode all trees and with qualifier(s): [Education ‐ ED] | 155 |
| #36 | MeSH descriptor: [Pediatric Nursing] explode all trees and with qualifier(s): [Education ‐ ED] | 36 |
| #37 | (#35 or #36) | 188 |
| #38 | MeSH descriptor: [Emergency Medicine] explode all trees and with qualifier(s): [Education ‐ ED] | 86 |
| #39 | MeSH descriptor: [Emergency Nursing] this term only and with qualifier(s): [Education ‐ ED] | 9 |
| #40 | #38 or #39 | 95 |
| #41 | MeSH descriptor: [Intensive Care, Neonatal] this term only | 275 |
| #42 | MeSH descriptor: [Diarrhea, Infantile] this term only | 455 |
| #43 | MeSH descriptor: [Infant, Newborn, Diseases] explode all trees | 4391 |
| #44 | ("Acute Respiratory Infection" or "Acute Respiratory Infections") | 475 |
| #45 | (#41 or #42 or #43 or #44) | 5493 |
| #46 | ("Control of Diarrheal Disease" or "Control of Diarrheal Diseases") | 3 |
| #47 | Neonatal next Resuscitation next Program* | 37 |
| #48 | "Essential Newborn Care" | 30 |
| #49 | "Integrated Management of Childhood Illness" | 38 |
| #50 | (#46 or #47 or #48 or #49) | 99 |
| #51 | #7 and #24 and #34 | 413 |
| #52 | #24 and #37 | 51 |
| #53 | #34 and #40 | 24 |
| #54 | #7 and #45 | 46 |
| #55 | #50 or #51 or #52 or #53 or #54 in Trials | 230 |
| #56 | #50 or #51 or #52 or #53 or #54 in Other Reviews | 25 |
| #57 | #50 or #51 or #52 or #53 or #54 in Technology Assessments | 3 |
MEDLINE, Ovid SP
| # | Searches | Results |
| 1 | exp Inservice Training/ | 24528 |
| 2 | exp Health Personnel/ed [Education] | 47977 |
| 3 | "Internship and Residency"/ | 35999 |
| 4 | ((staff or employee? or clinician? or physician? or nurse* or midwif* or midwives or pharmacist? or specialist? or practitioner? or dietician? or dietitian? or nutritionist?) adj (train* or course? or development or education or teach*)).ti,ab. | 14885 |
| 5 | ((inservice or in‐service or life support) adj2 (train* or course? or development or education or teach*)).ti,ab. | 2872 |
| 6 | on the job training.ti,ab. | 403 |
| 7 | or/1‐6 | 112597 |
| 8 | Case Management/ | 8484 |
| 9 | exp Critical Care/ | 44683 |
| 10 | Life Support Care/ | 7041 |
| 11 | Critical Illness/ | 17499 |
| 12 | Acute Disease/ | 183549 |
| 13 | exp Emergency Medical Services/ | 98322 |
| 14 | Emergency Medicine/ | 10129 |
| 15 | exp Emergency Treatment/ | 95314 |
| 16 | Emergency Nursing/ | 5782 |
| 17 | case management.ti,ab. | 7765 |
| 18 | emergency triage.ti,ab. | 98 |
| 19 | life support.ti,ab. | 8072 |
| 20 | resuscitation.ti,ab. | 39573 |
| 21 | first aid.ti,ab. | 4342 |
| 22 | ((referral or urgent) adj2 care).ti,ab. | 3612 |
| 23 | ((critical* or emergency or intensive or serious* or sever* or acute*) adj2 (care or ill or illness* or treatment or therap*)).ti,ab. | 291118 |
| 24 | or/8‐23 | 656528 |
| 25 | exp Child/ | 1563941 |
| 26 | exp Infant/ | 948338 |
| 27 | exp Child Care/ | 19934 |
| 28 | Pediatrics/ | 41434 |
| 29 | Neonatology/ | 2135 |
| 30 | Perinatology/ | 1623 |
| 31 | Pediatric Nursing/ | 12308 |
| 32 | Perinatal Care/ | 2918 |
| 33 | Neonatal Nursing/ | 3264 |
| 34 | Infant Death/ | 4 |
| 35 | Perinatal Death/ | 14 |
| 36 | (child* or infant? or pediatric? or paediatric? or perinat* or newborn? or new born? or neonat* or baby or babies or kid? or toddler?).ti,ab. | 1556796 |
| 37 | or/25‐36 | 2524543 |
| 38 | exp Child Care/ed [Education] | 65 |
| 39 | Pediatrics/ed [Education] | 5869 |
| 40 | Neonatology/ed [Education] | 231 |
| 41 | Perinatology/ed [Education] | 122 |
| 42 | Pediatric Nursing/ed [Education] | 1939 |
| 43 | Neonatal Nursing/ed [Education] | 405 |
| 44 | or/38‐43 | 8503 |
| 45 | exp Critical Care/ed [Education] | 30 |
| 46 | Life Support Care/ed [Education] | 2 |
| 47 | exp Emergency Medical Services/ed [Education] | 28 |
| 48 | Emergency Medicine/ed [Education] | 3805 |
| 49 | exp Emergency Treatment/ed [Education] | 2374 |
| 50 | Emergency Nursing/ed [Education] | 972 |
| 51 | or/45‐50 | 7031 |
| 52 | Intensive Care, Neonatal/ | 4422 |
| 53 | Diarrhea, Infantile/ | 6498 |
| 54 | Acute Respiratory Infection?.ti,ab. | 2868 |
| 55 | or/52‐54 | 13751 |
| 56 | exp Infant, Newborn, Diseases/ | 144228 |
| 57 | Control of Diarrheal Disease?.ti,ab. | 72 |
| 58 | Neonatal Resuscitation Program*.ti,ab. | 135 |
| 59 | Essential Newborn Care.ti,ab. | 65 |
| 60 | Integrated Management of Childhood Illness.ti,ab. | 253 |
| 61 | or/57‐60 | 516 |
| 62 | 7 and 24 and 37 | 2196 |
| 63 | 24 and 44 | 1201 |
| 64 | 37 and 51 | 1137 |
| 65 | 7 and 55 | 182 |
| 66 | 7 and 24 and 56 | 69 |
| 67 | or/61‐66 | 3589 |
| 68 | randomized controlled trial.pt. | 385110 |
| 69 | controlled clinical trial.pt. | 88641 |
| 70 | pragmatic clinical trial.pt. | 114 |
| 71 | multicenter study.pt. | 179618 |
| 72 | non‐randomized controlled trials as topic/ | 11 |
| 73 | interrupted time series analysis/ | 17 |
| 74 | controlled before‐after studies/ | 25 |
| 75 | (randomis* or randomiz* or randomly).ti,ab. | 586615 |
| 76 | groups.ab. | 1416282 |
| 77 | (trial or multicenter or multi center or multicentre or multi centre).ti. | 156718 |
| 78 | (intervention? or controlled or control group? or (before adj5 after) or (pre adj5 post) or ((pretest or pre test) and (posttest or post test)) or quasiexperiment* or quasi experiment* or evaluat* or effect? or impact? or time series or time point? or repeated measur*).ti,ab. | 6748504 |
| 79 | or/68‐78 | 7556657 |
| 80 | exp Animals/ | 17695852 |
| 81 | Humans/ | 13705040 |
| 82 | 80 not (80 and 81) | 3990812 |
| 83 | review.pt. | 1938147 |
| 84 | meta analysis.pt. | 53216 |
| 85 | news.pt. | 166920 |
| 86 | editorial.pt. | 370013 |
| 87 | comment.pt. | 613174 |
| 88 | cochrane database of systematic reviews.jn. | 10975 |
| 89 | comment on.cm. | 613174 |
| 90 | (systematic review or literature review).ti. | 57343 |
| 91 | or/82‐90 | 6791681 |
| 92 | 79 not 91 | 5187655 |
| 93 | 67 and 92 | 1636 |
EMBASE, Ovid SP
| # | Searches | Results |
| 1 | In Service Training/ | 13956 |
| 2 | Staff Training/ | 9388 |
| 3 | Nurse Training/ | 1372 |
| 4 | Continuing Education/ | 27705 |
| 5 | Professional Development/ | 5127 |
| 6 | Medical Education/ | 180041 |
| 7 | Residency Education/ | 20953 |
| 8 | ((staff or employee? or clinician? or physician? or nurse* or midwif* or midwives or pharmacist? or specialist? or practitioner? or dietician? or dietitian? or nutritionist?) adj (train* or course? or development or education or teach*)).ti,ab. | 18251 |
| 9 | ((inservice or in‐service or life support) adj2 (train* or course? or development or education or teach*)).ti,ab. | 3324 |
| 10 | on the job training.ti,ab. | 472 |
| 11 | or/1‐10 | 254380 |
| 12 | Case Management/ | 8051 |
| 13 | exp Intensive Care/ | 468236 |
| 14 | Critical Illness/ | 21660 |
| 15 | Disease Severity/ | 382573 |
| 16 | Acute Disease/ | 88120 |
| 17 | Injury Severity/ | 9155 |
| 18 | Emergency Medicine/ | 28345 |
| 19 | exp Emergency Treatment/ | 181735 |
| 20 | Emergency Nursing/ | 5225 |
| 21 | case management.ti,ab. | 9205 |
| 22 | emergency triage.ti,ab. | 130 |
| 23 | life support.ti,ab. | 10351 |
| 24 | resuscitation.ti,ab. | 50652 |
| 25 | first aid.ti,ab. | 5023 |
| 26 | ((referral or urgent) adj2 care).ti,ab. | 4817 |
| 27 | ((critical* or emergency or intensive or serious* or sever* or acute*) adj2 (care or ill or illness* or treatment or therap*)).ti,ab. | 381035 |
| 28 | or/12‐27 | 1290485 |
| 29 | exp Child/ | 2059816 |
| 30 | exp Newborn/ | 459451 |
| 31 | exp Child Health Care/ | 65699 |
| 32 | exp Pediatrics/ | 77383 |
| 33 | exp Pediatric Nursing/ | 12018 |
| 34 | exp Postnatal Care/ | 80179 |
| 35 | Perinatal Care/ | 10465 |
| 36 | (child* or infant? or pediatric? or paediatric? or perinat* or newborn? or new born? or neonat* or baby or babies or kid? or toddler?).ti,ab. | 1819970 |
| 37 | or/29‐36 | 2707589 |
| 38 | Newborn Intensive Care/ | 21801 |
| 39 | Newborn Intensive Care Nursing/ | 62 |
| 40 | Pediatric Intensive Care Nursing/ | 124 |
| 41 | Pediatric Advanced Life Support/ | 450 |
| 42 | Infantile Diarrhea/ | 3767 |
| 43 | Acute Respiratory Infection?.ti,ab. | 3176 |
| 44 | or/38‐43 | 29320 |
| 45 | Emergency Medical Services Education/ | 274 |
| 46 | exp Newborn Disease/ | 976796 |
| 47 | Control of Diarrheal Disease?.ti,ab. | 38 |
| 48 | Neonatal Resuscitation Program*.ti,ab. | 161 |
| 49 | Essential Newborn Care.ti,ab. | 81 |
| 50 | Integrated Management of Childhood Illness.ti,ab. | 286 |
| 51 | or/47‐50 | 560 |
| 52 | 11 and 28 and 37 | 3887 |
| 53 | 11 and 44 | 708 |
| 54 | 37 and 45 | 30 |
| 55 | 11 and 28 and 46 | 560 |
| 56 | or/51‐55 | 4600 |
| 57 | Randomized Controlled Trial/ | 360662 |
| 58 | Controlled Clinical Trial/ | 390355 |
| 59 | Quasi Experimental Study/ | 2271 |
| 60 | Pretest Posttest Control Group Design/ | 220 |
| 61 | Time Series Analysis/ | 14979 |
| 62 | Experimental Design/ | 10740 |
| 63 | Multicenter Study/ | 115711 |
| 64 | (randomis* or randomiz* or randomly).ti,ab. | 764795 |
| 65 | groups.ab. | 1779704 |
| 66 | (trial or multicentre or multicenter or multi centre or multi center).ti. | 203366 |
| 67 | (intervention? or controlled or control group? or (before adj5 after) or (pre adj5 post) or ((pretest or pre test) and (posttest or post test)) or quasiexperiment* or quasi experiment* or evaluat* or effect? or impact? or time series or time point? or repeated measur*).ti,ab. | 8028100 |
| 68 | or/57‐67 | 8974919 |
| 69 | Nonhuman/ | 4453670 |
| 70 | editorial.pt. | 463033 |
| 71 | (systematic review or literature review).ti. | 68545 |
| 72 | "cochrane database of systematic reviews".jn. | 3777 |
| 73 | or/69‐72 | 4952684 |
| 74 | 68 not 73 | 6996420 |
| 75 | 56 and 74 | 2176 |
| 76 | limit 75 to embase | 1816 |
CINAHL, EBSCOHost
| # | Query | Results |
| S97 | S90 OR S91 OR S92 OR S93 OR S94 OR S95 [Exclude MEDLINE records] | 329 |
| S96 | S90 OR S91 OR S92 OR S93 OR S94 OR S95 | 1,391 |
| S95 | S74 and S89 | 108 |
| S94 | S70 and S89 | 83 |
| S93 | S16 and S65 and S89 | 390 |
| S92 | S39 and S57 and S89 | 224 |
| S91 | S29 and S49 and S89 | 230 |
| S90 | S16 and S29 and S39 and S89 | 935 |
| S89 | S75 or S76 or S77 or S78 or S79 or S80 or S81 or S82 or S83 or S84 or S85 or s86 or S87 or S88 | 1,105,239 |
| S88 | TI (effect* or impact* or intervention* or before N5 after or pre N5 post or ((pretest or "pre test") and (posttest or "post test")) or quasiexperiment* or quasi W0 experiment* or evaluat* or "time series" or time W0 point* or repeated W0 measur*) OR AB (before N5 after or pre N5 post or ((pretest or "pre test") and (posttest or "post test")) or quasiexperiment* or quasi W0 experiment* or evaluat* or "time series" or time W0 point* or repeated W0 measur*) | 411,775 |
| S87 | TI ( randomis* or randomiz* or randomly) OR AB ( randomis* or randomiz* or randomly) | 101,250 |
| S86 | (MH "Health Services Research") | 6,930 |
| S85 | (MH "Multicenter Studies") | 8,926 |
| S84 | (MH "Quasi‐Experimental Studies+") | 7,802 |
| S83 | (MH "Pretest‐Posttest Design+") | 24,583 |
| S82 | (MH "Experimental Studies") | 13,976 |
| S81 | (MH "Nonrandomized Trials") | 157 |
| S80 | (MH "Intervention Trials") | 5,536 |
| S79 | (MH "Clinical Trials") | 81,250 |
| S78 | (MH "Randomized Controlled Trials") | 21,621 |
| S77 | PT research | 937,077 |
| S76 | PT clinical trial | 51,827 |
| S75 | PT randomized controlled trial | 26,075 |
| S74 | S71 or S72 or S73 | 158 |
| S73 | TI control W1 diarrhea* W1 disease* or AB control W1 diarrhea* W1 disease* | 1 |
| S72 | TI neonatal W1 resuscitation W1 program* or AB neonatal W1 resuscitation W1 program* | 80 |
| S71 | TI integrated W1 management W1 childhood W1 Illness* or AB integrated W1 management W1 childhood W1 Illness* | 77 |
| S70 | S66 or S67 or S68 or S69 | 256 |
| S69 | (MH "Pediatric Advanced Life Support/ED") | 44 |
| S68 | (MH "Pediatric Critical Care Nursing+/ED") | 145 |
| S67 | (MH "Intensive Care Units, Pediatric+/ED") | 13 |
| S66 | (MH "Intensive Care, Neonatal+/ED") | 61 |
| S65 | S58 or S59 or S60 or S61 or S62 or S63 or S64 | 29,360 |
| S64 | TI ( "acute respiratory infection*" or "acute respiratory syndrome" or sars ) or AB ( "acute respiratory infection*" or "acute respiratory syndrome" or sars ) | 1,756 |
| S63 | (MH "Severe Acute Respiratory Syndrome") | 1,491 |
| S62 | (MH "Infant, Newborn, Diseases+") | 15,314 |
| S61 | (MH "Pediatric Advanced Life Support") | 186 |
| S60 | (MH "Pediatric Critical Care Nursing+") | 3,286 |
| S59 | (MH "Intensive Care Units, Pediatric+") | 8,776 |
| S58 | (MH "Intensive Care, Neonatal+") | 3,412 |
| S57 | S50 or S51 or S52 or S53 or S54 or S55 or S56 | 3,500 |
| S56 | (MH "Emergency Nursing+/ED") | 582 |
| S55 | (MH "Resuscitation+/ED") | 1,326 |
| S54 | (MH "First Aid/ED") | 224 |
| S53 | (MH "Education, Emergency Medical Services") | 874 |
| S52 | (MH "Emergency Medical Services+/ED") | 353 |
| S51 | (MH "Life Support Care/ED") | 33 |
| S50 | (MH "Critical Care+/ED") | 228 |
| S49 | S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 | 2,735 |
| S48 | (MH "Severe Acute Respiratory Syndrome/ED") | 15 |
| S47 | (MH "Infant, Newborn, Diseases+/ED") | 55 |
| S46 | (MH "Pediatric Nursing+/ED") | 1,124 |
| S45 | (MH "Pediatric Care+/ED") | 242 |
| S44 | (MH "Prenatal Care/ED") | 61 |
| S43 | (MH "Perinatal Care/ED") | 50 |
| S42 | (MH "Pediatrics+/ED") | 868 |
| S41 | (MH "Child Health/ED") | 48 |
| S40 | (MH "Child Care+/ED") | 302 |
| S39 | S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 | 396,979 |
| S38 | TI ( child* or infant* or pediatric* or paediatric* or perinat* or newborn* or new W0 born* or neonat* or baby or babies or kid or kids or toddler* ) or AB ( child* or infant* or pediatric* or paediatric* or perinat* or newborn or new W0 born* or neonat* or baby or babies or kid or kids or toddler* ) | 268,672 |
| S37 | (MH "Pediatric Nursing+") | 15,707 |
| S36 | (MH "Pediatric Care+") | 8,942 |
| S35 | (MH "Prenatal Care") | 8,159 |
| S34 | (MH "Perinatal Care") | 1,887 |
| S33 | (MH "Pediatrics+") | 7,689 |
| S32 | (MH "Child Health") | 9,312 |
| S31 | (MH "Child Care+") | 6,214 |
| S30 | (MH "Child+") | 305,018 |
| S29 | S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 | 201,390 |
| S28 | TI ( "case management" or emergency or "life support" or resuscitation or "first aid" or referral N2 care or urgent N2 care or critical* N2 care or critical* N2 ill or critical* N2 illness or critical* N2 treatment or critical* N2 therap* or intensive N2 care or intensive N2 ill or intensive N2 illness or intensive N2 treatment or intensive N2 therap* or serious* N2 care or serious* N2 ill or serious* N2 illness or serious* N2 treatment or serious* N2 therap* or sever* N2 care or sever* N2 ill or sever* N2 illness or sever* N2 treatment or sever* N2 therap* or acute* N2 care or acute* N2 ill or acute* N2 illness or acute* N2 treatment or acute* N2 therap* or "trauma nursing" ) or AB ( "case management" or emergency or "life support" or resuscitation or "first aid" or referral N2 care or urgent N2 care or critical* N2 care or critical* N2 ill or critical* N2 illness or critical* N2 treatment or critical* N2 therap* or intensive N2 care or intensive N2 ill or intensive N2 illness or intensive N2 treatment or intensive N2 therap* or serious* N2 care or serious* N2 ill or serious* N2 illness or serious* N2 treatment or serious* N2 therap* or sever* N2 care or sever* N2 ill or sever* N2 illness or sever* N2 treatment or sever* N2 therap* or acute* N2 care or acute* N2 ill or acute* N2 illness or acute* N2 treatment or acute* N2 therap* or "trauma nursing" ) | 128,460 |
| S27 | (MH "Emergency Nursing+") | 11,165 |
| S26 | (MH "Resuscitation+") | 21,788 |
| S25 | (MH "First Aid") | 1,505 |
| S24 | (MH "Emergency Medicine") | 5,367 |
| S23 | (MH "Emergency Medical Services+") | 54,380 |
| S22 | (MH "Catastrophic Illness") | 269 |
| S21 | (MH "Acute Disease") | 11,446 |
| S20 | (MH "Critical Illness") | 4,448 |
| S19 | (MH "Life Support Care") | 1,578 |
| S18 | (MH "Critical Care+") | 13,895 |
| S17 | (MH "Case Management") | 11,630 |
| S16 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 | 65,588 |
| S15 | TI ( "life support" N2 train* or "life support" N2 course or "life support" N2 development or "life support" N2 education or "life support" N2 teach* or "job training" ) or AB ( "life support" N2 train* or "life support" N2 course or "life support" N2 development or "life support" N2 education or "life support" N2 teach* or "job training" ) | 531 |
| S14 | TI ( inservice N2 train* or inservice N2 course or inservice N2 development or inservice N2 education or inservice N2 teach* or "in service" N2 train* or "in service" N2 course or "in service" N2 development or "in service" N2 education or "in service" N2 teach* ) or AB ( inservice N2 train* or inservice N2 course or inservice N2 development or inservice N2 education or inservice N2 teach* or "in service" N2 train* or "in service" N2 course or "in service" N2 development or "in service" N2 education or "in service" N2 teach* ) | 994 |
| S13 | TI ( dieti?ian* N2 train* or dieti?ian* N2 course or dieti?ian* N2 development or dieti?ian* N2 education or dieti?ian* N2 teach* or nutritionist* N2 train* or nutritionist* N2 course or nutritionist* N2 development or nutritionist* N2 education or nutritionist* N2 teach* ) or AB ( dieti?ian* N2 train* or dieti?ian* N2 course or dieti?ian* N2 development or dieti?ian* N2 education or dieti?ian* N2 teach* or nutritionist* N2 train* or nutritionist* N2 course or nutritionist* N2 development or nutritionist* N2 education or nutritionist* N2 teach* ) | 156 |
| S12 | TI ( practitioner* N2 train* or practitioner* N2 course or practitioner* N2 development or practitioner* N2 education or practitioner* N2 teach* ) or AB ( practitioner* N2 train* or practitioner* N2 course or practitioner* N2 development or practitioner* N2 education or practitioner* N2 teach* ) | 1,842 |
| S11 | TI ( specialist* N2 train* or specialist* N2 course or specialist* N2 development or specialist* N2 education or specialist* N2 teach* ) or AB ( specialist* N2 train* or specialist* N2 course or specialist* N2 development or specialist* N2 education or specialist* N2 teach* ) | 1,126 |
| S10 | TI ( pharmacist* N2 train* or pharmacist* N2 course or pharmacist* N2 development or pharmacist* N2 education or pharmacist* N2 teach* ) or AB ( pharmacist* N2 train* or pharmacist* N2 course or pharmacist* N2 development or pharmacist* N2 education or pharmacist* N2 teach* ) | 237 |
| S9 | TI ( midwif* N2 train* or midwif* N2 course or midwif* N2 development or midwif* N2 education or midwif* N2 teach* or midwives N2 train* or midwives N2 course or midwives N2 development or midwives N2 education or midwives N2 teach* ) or AB ( midwif* N2 train* or midwif* N2 course or midwif* N2 development or midwif* N2 education or midwif* N2 teach* or midwives N2 train* or midwives N2 course or midwives N2 development or midwives N2 education or midwives N2 teach* ) | 1,549 |
| S8 | TI ( nurse* N2 train* or nurse* N2 course or nurse* N2 development or nurse* N2 education or nurse* N2 teach* ) or AB ( nurse* N2 train* or nurse* N2 course or nurse* N2 development or nurse* N2 education or nurse* N2 teach* ) | 13,757 |
| S7 | TI ( physician* N2 train* or physician* N2 course or physician* N2 development or physician* N2 education or physician* N2 teach* ) or AB ( physician* N2 train* or physician* N2 course or physician* N2 development or physician* N2 education or physician* N2 teach* ) | 2,544 |
| S6 | TI ( clinician* N2 train* or clinician* N2 course or clinician* N2 development or clinician* N2 education or clinician* N2 teach* ) or AB ( clinician* N2 train* or clinician* N2 course or clinician* N2 development or clinician* N2 education or clinician* N2 teach* ) | 1,025 |
| S5 | TI ( employee* N2 train* or employee* N2 course or employee* N2 development or employee* N2 education or employee* N2 teach* ) or AB ( employee* N2 train* or employee* N2 course or employee* N2 development or employee* N2 education or employee* N2 teach* ) | 434 |
| S4 | TI ( staff N2 train* or staff N2 course or staff N2 development or staff N2 education or staff N2 teach* ) or AB ( staff N2 train* or staff N2 course or staff N2 development or staff N2 education or staff N2 teach* ) | 6,579 |
| S3 | (MH "Internship and Residency") | 6,452 |
| S2 | (MH "Health Personnel+/ED") | 19,663 |
| S1 | (MH "Staff Development") | 19,164 |
ERIC, ProQuest
ALL(inservice P/2 education or "in service" P/2 education or inservice P/2 training or "in service" P/2 training or "on the job training" or "on the job education" or inservice P/2 course* or "in service" P/2 course* or inservice P/2 workshop* or "in service" P/2 workshop* or inservice P/2 program* or "in service" P/2 program*) and ALL("crisis management" or crisis P/0 intervention* or acute P/2 care or acute* P/2 treatment* or acute* P/2 therap* or emergency P/2 care or emergency P/2 treatment* or emergency P/2 therap* or emergency P/2 program* or intensive P/2 care or intensive P/2 treatment* or intensive P/2 therap*or critical P/2 care or critical P/2 treatment* or critical P/2 therap* or urgent P/2 care or urgent P/2 treatment or "first aid" or "life support" or resuscitation or acute* P/0 ill* or emergency P/0 ill* or critical* P/0 ill* or serious* P/0 ill* or sever* P/0 ill*) and ALL(child or children or infant or infants or pediatric* or paediatric* or newborn* or new P/0 born* or neonat* or perinat* baby or babies or kid or kids or toddler)
WHOLIS, WHO
Words or phrase: inservice or job
AND
Words or phrase: training or education or course$ or workshop$ or program$
AND
Words or phrase: child$ or infant$ or pediatric$ or paediatric$ or newborn$ or new born or neonat$ or perinat$ or baby or babies or kid or kids or toddler$
LILACS, VHL (IAH interface)
(inservice and training) or (inservice and course$) or (inservice and workshop$) or (inservice and education) or (inservice and program$) or (capacitación and servicio) or (capacitação and serviço) [Words]
And
child or children or niño or criança or infant or infants or lactante or lactente or pediatric$ or paediatric$ or pediatría or pediatria or newborn or (recién and nacidos) or (recém and nascidos) or neonat$ or baby or babies or kid or kids or toddler$ [Words]
Science Citation Index and Social Sciences Citation Index (ISI Web of Science)
Citation search for two included studies:
1. Opiyo N, Were F, Govedi F, Fegan G, Wasunna A, English M. Effect of newborn resuscitation training on health worker practices in Pumwani Hospital, Kenya. PLoS ONE 2008;13;3(2):e1599.
2. Senarath U, Fernando DN, Rodrigo I. Effect of training for care providers on practice of essential newborn care in hospitals in Sri Lanka. Journal of Obstetric, Gynecologic and Neonatal Nursing 2007;36(6):531‐41.
Appendix 2. GRADE evidence profile
|
In‐service neonatal emergency care training versus usual care for healthcare professionals Participants: nurses and midwives Settings: delivery room/theatre (Kenya) Intervention: 1‐day newborn resuscitation training Comparison: usual care | |||||||||||||
| Quality assessment | Number of practices | Effect | Quality | Importance | |||||||||
| Number of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | With in‐service training | Usual care | Relative (95% CI) | Absolute | |||
| Health workers' resuscitation practices (proportion of adequate initial resuscitation steps; follow‐up 50 days; assessed with direct observation) | |||||||||||||
| 1 | Randomised trial | Serious1 | No serious inconsistency | No serious indirectness | No serious imprecision | None | 64/97 (66%) | 31/115 (27%) | RR 2.45 (1.75 to 3.42) |
39 more per 100 (from 20 more to 65 more) | ⊕⊕⊕Οa Moderate | CRITICAL | |
| Health workers' resuscitation practices (inappropriate and potentially harmful practices per resuscitation; follow‐up 50 days; measured with direct observation; better indicated by lower values) | |||||||||||||
| 1 | Randomised trial | Serious1 | No serious inconsistency | No serious indirectness | No serious imprecision | None | 97 | 115 | ‐ | MD 0.39 higher (0.13 to 0.66 higher) | ⊕⊕⊕Οa Moderate | CRITICAL | |
| Neonatal mortality in all resuscitation episodes (follow‐up 50 days; assessed with medical records ‐ resuscitation observation sheets) | |||||||||||||
| 1 | Randomised trial | Serious1 | No serious inconsistency | No serious indirectness | Serious2 | None | 18/65 (27.7%) | 9/25 (36%) | RR 0.77 (0.40 to 1.48) |
8 fewer per 100 (from 22 fewer to 17 more) | ⊕⊕ΟΟa,b Low | CRITICAL | |
| CI: Confidence interval; MD: Mean difference. aDowngraded from high to moderate because of risk of bias (details about allocation sequence generation and concealment were not reported in the article; potential cross‐group contaminaton cannot be excluded). bDowngraded from moderate to low because of imprecision (few events, N = 27 deaths). | |||||||||||||
Appendix 3. GRADE evidence profile
|
In‐service neonatal emergency care training versus standard care for healthcare professionals Participants: doctors, nurses and midwives Setting: delivery room, Sri Lanka Intervention: 4‐day essential newborn care training Comparison: usual care | ||||||||||||
| Quality assessment | Practices (number of providers) | Effect | Quality | Importance | ||||||||
| Number of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | With in‐service training | Usual care | Relative (95% CI) | Absolute | ||
| Preparedness for resuscitation* (follow‐up 90 days; measured with direct observation; better indicated by higher values) | ||||||||||||
| 1 | Randomised trial | Serious1 | No serious inconsistency | No serious indirectness | No serious imprecision | None | Mean percentage: 19.29% (24 providers) |
Mean percentage: 10.46% (24 providers) |
‐ | Mean percentage change: 8.83% higher (6.41% to 11.25% higher) |
⊕⊕⊕⊝a Moderate | CRITICAL |
|
aDowngraded from high to moderate because of risk of bias (allocation sequence generation and concealment were not reported). *Improvement also observed in assessment of breathing (however, re‐analysis to calculate intervention effect was not done owing to baseline imbalance between study groups). | ||||||||||||
Appendix 4. Inappropriate and harmful practices
Inappropriate breathing support/oxygen use
Inappropriate stimulation (performed before drying)
Inappropriate positioning
|
Appendix 5. Planned methods not used in the review
|
Complexity of targeted interventions If it is possible that the training by itself would not have made a difference unless major interventions were provided in other areas (e.g. improved supervision/drug supply, provision of new or enhanced equipment/facility management skills or technical improvements), two authors (ON and ME) will assess and summarise the contribution of such external influences as high, moderate or low. Differences in the ratings will be resolved through discussion between review authors. Reporting For ITS, we will report the change in the level of outcome immediately after introduction of the intervention and the change in the slopes of the regression lines. For the change in slope, we will present the effects of interventions as the difference between the fitted value for the first six months post intervention data point minus the predicted outcome six months after the intervention based on the preintervention slope when possible. The same measurement will be used for the change in the trend of outcomes when data points are available after one and two years. If available, we will report the costs of in‐service training (resource use) including direct costs (such as costs for purchasing training materials) and cost impacts (such as impact of in‐service guidelines on treatment costs). If available, cost data will be presented in both physical/natural and monetary units. Analysis Similarly, if needed, we will re‐analyse ITSs using time series regression (if possible) by estimating the best fit before the intervention and after the intervention lines using linear regression. Sensitivity analyses will be used to assess the effects of incorporating these corrected analyses into the analysis. Primary analyses We will conduct meta‐analysis using a random‐effects model for direct comparisons, if a pooled estimate makes practical sense and data are available or can be obtained. For example, we will consider calculating an overall effect for paediatric and other child health training courses if they have minimal variations (e.g. in intensity, types of participants) that are unlikely to alter the results. We will assess the presence of heterogeneity by visually examining forest plots to check for overlapping confidence intervals and by calculating a test of heterogeneity (i.e. Chi2 test using a 10% level of statistical significance, and I² test), taking values < 25% to represent low heterogeneity, and values between 25% and 50% to represent moderate heterogeneity. Exploring heterogeneity We do expect considerable heterogeneity due to differences in study designs (RCTs, CRTs, CCTs, CBAs and ITSs), diagnoses (malaria, diarrhoea, malnutrition, pneumonia, etc) and participants (nurses, doctors, etc). We will prepare tables and bubble plots to explore potential heterogeneity due to the above factors. A bubble plot graphically presents the relationship between the outcome of each study and a given modifier with the use of regression lines. We will perform, if possible, sensitivity analyses to assess the extent to which the above differences influence reported results. In addition, we will explore, if sufficient data are available, the impact of potential explanatory factors such as duration of training courses, baseline performance, format of training (mixed interactive, didactic), single vs multiple topics, on‐site training or supportive interventions (e.g. supervision, incentives) (Appendix 6). Ongoing studies We will describe identified ongoing studies when available, detailing the primary author, research questions(s), methods and outcome measures, together with an estimate of the reporting date. |
Appendix 6. Explanatory factors: hypothesis
| Factor | Hypothesised effect on professional practice |
| Training duration | Increase |
| High baseline performance | Decrease |
| Mixed interactive format | Increase |
| Multiple topics | Decrease |
| On‐site training | Increase |
| Supportive interventions | Increase |
Data and analyses
Comparison 1. Opiyo 2008.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.40, 1.48] |
1.1. Analysis.
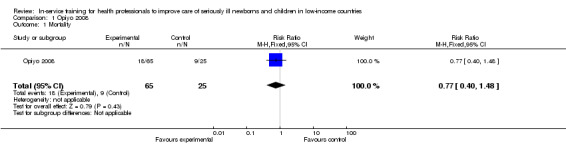
Comparison 1 Opiyo 2008, Outcome 1 Mortality.
Comparison 2. Senarath 2007.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Preparedness for resuscitation | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 8.83 [6.55, 11.11] |
| 2 Preparedness for resuscitation ‐ adjusted for clustering | 1 | Mean Difference (Fixed, 95% CI) | 8.83 [6.41, 11.25] |
2.1. Analysis.
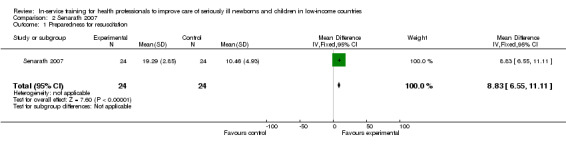
Comparison 2 Senarath 2007, Outcome 1 Preparedness for resuscitation.
2.2. Analysis.
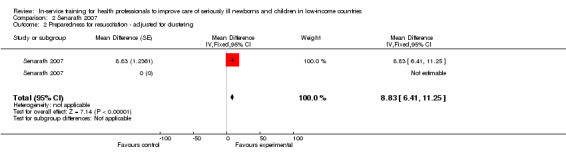
Comparison 2 Senarath 2007, Outcome 2 Preparedness for resuscitation ‐ adjusted for clustering.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Opiyo 2008.
| Methods | Randomised controlled trial Country: Kenya Setting: delivery room/theatre Type of targeted behaviour: newborn resuscitation |
|
| Participants | Nurses/midwives Phase 1: 83 nurses (28 intervention, 55 control) 97 practices in the intervention group; 115 practices in the control group |
|
| Interventions | Newborn resuscitation training Duration of training: 1 day Co‐intervention: self learning instruction manual provided to participants 2 weeks before training Control: usual/standard practice Postintervention data collection period: 50 days (phase 1) |
|
| Outcomes | Proportion of appropriate initial resuscitation practices Frequency of inappropriate/harmful practices (Appendix 4) Neonatal mortality |
|
| Notes | Participants (nurses): no differences between study groups in age and number of years worked Primary analysis based on phase 1 data only Overall risk of bias assessment: high risk of bias |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Our intention was to randomise staff, stratified by place of work…' Details about the method used to generate allocation sequence were not reported |
| Allocation concealment (selection bias) | Low risk | 'Our intention was to randomise staff, stratified by place of work…' Details about the method used to conceal allocation sequence were not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | '32 allocated to intervention….28 providers observed', '58 allocated to control…55 providers observed' |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes reported |
| Blinding All outcomes | Low risk | Observers were blind to the training status of health workers and were instructed not to try to ascertain health workers' training status |
| Contamination All outcomes | Unclear risk | 'We cannot exclude the possibility of cross‐group contamination…' |
Senarath 2007.
| Methods | Randomised controlled trial Country: Sri Lanka Setting: delivery room Type of targeted behaviour: general management/preparation and conduct of delivery care for newborn |
|
| Participants | Doctors, nurses, midwives 110 participants (59 intervention, 61 control) |
|
| Interventions | Essential newborn care course Duration of training: 4 days Co‐interventions: none Control: usual/standard practice |
|
| Outcomes | Assessment of breathing, preparedness for resuscitation (i.e. "suction device prepared, neonatal ambu bag and mask prepared, neonatal emergency tray prepared, breathing of newborn checked") | |
| Notes | Reported data restricted to results of direct observations of delivery practices made on a subsample consisting of 96 health providers (48 before and 48 after the intervention) Postintervention data collection period: 3 months 'Unit of analysis error present': The unit of randomisation was hospitals, while the unit of analysis was observed delivery room care practices. Effects in training and control groups were not directly compared in the analysis Overall risk of bias assessment: high risk of bias |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method used to generate allocation sequence was not reported |
| Allocation concealment (selection bias) | Unclear risk | The method used to conceal allocation sequence was not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes were reported |
| Blinding All outcomes | High risk | The principal investigator made observations in the labour room |
| Contamination All outcomes | Low risk | It is unlikely that the control group received the training intervention |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bryce 2005 | Non‐randomised controlled trial |
| Carlo 2010a | Community setting; primary outcome for the review not reported |
| Carlo 2010b | Community‐setting; primary outcome for the review not reported |
| Chomba 2008 | Primary outcome for the review not reported |
| El‐Arifeen 2004 | Data on referral rate for very ill children (outcome of interest) not reported |
| Ersdal 2013 | Uncontrolled before and after study |
| Gill 2011 | Non‐qualified healthcare workers (traditional birth attendants) |
| Goudar 2012 | Community‐based setting |
| Goudar 2013 | Primary outcome for the review not reported |
| Gouws 2004 | No baseline assessment of outcomes in Integrated Management of Childhood Illness (IMCI) trained and untrained groups |
| Hoban 2013 | Primary outcome for the review not reported |
| Irimu 2012 | Uncontrolled before‐after design |
| Kirkwood 2013 | Community‐based cluster‐randomised trial |
| Manasyan 2011 | Primary outcome for the review not reported |
| Msemo 2013 | Primary outcome for the review not reported |
| Nadel 2000 | Study includes a historical group only and used mock scenarios to assess practice |
| Ochoa 1996 | Study did not include seriously ill children (considered only mild acute respiratory infection (ARI) episodes) |
| Pelto 2004 | Study focused on an Integrated Management of Childhood Illness (IMCI)‐derived nutritional counselling protocol in apparently well children |
| Rovamo 2013 | Non‐randomised controlled trial |
| Xu 2014 | Primary outcome for the review not reported |
Differences between protocol and review
Several procedures planned in the protocol were not implemented in the review. These procedures could provide guidance for future updates of this review and are reported in Appendix 5
Contributions of authors
NO and ME screened articles for eligibility, assessed study risk of bias and quality of evidence, interpreted findings and wrote the review.
Sources of support
Internal sources
KEMRI/Wellcome Trust Research Programme, Kenya.
External sources
South African Cochrane Centre, South Africa.
Cochrane Effective Practice and Organisation of Care Group (EPOC), Norway.
Declarations of interest
Both review authors are authors of one included study (Opiyo 2008).
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Opiyo 2008 {published data only}
- Opiyo N, Were F, Govedi F, Fegan G, Wasunna A, English M. Effect of newborn resuscitation training on health worker practices in Pumwani Hospital, Kenya. PLoS ONE 2008;13;3(2):e1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Senarath 2007 {published data only}
- Senarath U, Fernando DN, Rodrigo I. Effect of training for care providers on practice of essential newborn care in hospitals in Sri Lanka. Journal of Obstetric, Gynecologic and Neonatal Nursing 2007;36(6):531‐41. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bryce 2005 {published data only}
- Bryce J, Gouws E, Adam T, Black RE, Schellenberg JA, Manzi F, et al. Improving quality and efficiency of facility‐based child health care through Integrated Management of Childhood Illness in Tanzania. Health Policy and Planning 2005;20(Suppl 1):i69‐i76. [DOI] [PubMed] [Google Scholar]
Carlo 2010a {published data only}
- Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al. High mortality rates for very low birth weight infants in developing countries despite training. Pediatrics 2010;126(5):e1072‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carlo 2010b {published data only}
- Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al. Newborn‐care training and perinatal mortality in developing countries. New England Journal of Medicine 2010;18(7):614‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chomba 2008 {published data only}
- Chomba E, McClure EM, Wright LL, Carlo WA, Chakraborty H, Harris H. Effect of WHO newborn care training on neonatal mortality by education. Ambulatory Pediatrics 2008;8(5):300‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
El‐Arifeen 2004 {published data only}
- Arifeen S, Blum LS, Hoque DM, Chowdhury EK, Khan R, Black RE, et al. Integrated Management of Childhood Illness (IMCI) in Bangladesh: early findings from a cluster‐randomised study. Lancet 2004;364(9445):1595‐602. [DOI] [PubMed] [Google Scholar]
Ersdal 2013 {published data only}
- Ersdal HL, Vossius C, Bayo E, Mduma E, Perlman J, Lippert A, et al. A one‐day "Helping Babies Breathe" course improves simulated performance but not clinical management of neonates. Resuscitation 2013;84(10):1422‐7. [DOI] [PubMed] [Google Scholar]
Gill 2011 {published data only}
- Gill CJ, Phiri‐Mazala G, Guerina NG, Kasimba J, Mulenga C, MacLeod WB, et al. Effect of training traditional birth attendants on neonatal mortality (Lufwanyama Neonatal Survival Project): randomised controlled study. BMJ 2011;Feb 3:342:d346. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goudar 2012 {published data only}
- Goudar SS, Dhaded SM, McClure EM, Derman RJ, Patil VD, Mahantshetti NS, et al. ENC training reduces perinatal mortality in Karnataka, India. Journal of Maternal‐Fetal & Neonatal Medicine 2012;25(6):568‐74. [DOI] [PubMed] [Google Scholar]
Goudar 2013 {published data only}
- Goudar SS, Somannavar MS, Clark R, Lockyer JM, Revankar AP, Fidler HM, et al. Stillbirth and newborn mortality in India after Helping Babies Breathe training. Pediatrics 2013;131(2):e344‐52. [DOI] [PubMed] [Google Scholar]
Gouws 2004 {published data only}
- Gouws E, Bryce J, Habicht JP, Amaral J, Pariyo G, Schellenberg JA, et al. Improving antimicrobial use among health workers in first‐level facilities: results from the multi‐country evaluation of the Integrated Management of Childhood Illness strategy. Bulletin of the World Health Organization 2004;82(7):509‐15. [PMC free article] [PubMed] [Google Scholar]
Hoban 2013 {published data only}
- Hoban R, Bucher S, Neuman I, Chen M, Tesfaye N, Spector JM. 'Helping babies breathe' training in sub‐saharan Africa: educational impact and learner impressions. Journal of Tropical Pediatrics 2013;59(3):180‐6. [DOI] [PubMed] [Google Scholar]
Irimu 2012 {published data only}
- Irimu GW, Gathara D, Zurovac D, Kihara H, Maina C, Mwangi J, et al. Performance of health workers in the management of seriously sick children at a Kenyan tertiary hospital: before and after a training intervention. PLoS One 2012;7(7):e39964. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirkwood 2013 {published data only}
- Kirkwood BR, Manu A, Asbroek AH, Soremekun S, Weobong B, Gyan T, et al. Effect of the Newhints home‐visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet 2013;381(9884):2184‐92. [DOI] [PubMed] [Google Scholar]
Manasyan 2011 {published data only}
- Manasyan A, Chomba E, McClure EM, Wright LL, Krzywanski S, Carlo WA. Cost‐effectiveness of essential newborn care training in urban first‐level facilities. Pediatrics 2011;127(5):e1176‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Msemo 2013 {published data only}
- Msemo G, Massawe A, Mmbando D, Rusibamayila N, Manji K, Kidanto HL, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics 2013;131(2):e353‐60. [DOI] [PubMed] [Google Scholar]
Nadel 2000 {published data only}
- Nadel FM, Lavelle JM, Fein JA, Giardino AP, Decker JM, Durbin DR. Teaching resuscitation to pediatric residents: the effects of an intervention. Archives of Pediatrics and Adolescent Medicine 2000;154(10):1049‐54. [DOI] [PubMed] [Google Scholar]
Ochoa 1996 {published data only}
- González Ochoa E, Armas Pérez L, Bravo González JR, Cabrales Escobar J, Rosales Corrales R, Abreu Suárez G. Prescription of antibiotics for mild acute respiratory infections in children. Bulletin of the Pan American Health Organisation 1996;30(2):106‐17. [PubMed] [Google Scholar]
Pelto 2004 {published data only}
- Pelto GH, Santos I, Gonçalves H, Victora C, Martines J, Habicht JP. Nutrition counseling training changes physician behavior and improves caregiver knowledge acquisition. The Journal of Nutrition 2004;134(2):357‐62. [DOI] [PubMed] [Google Scholar]
Rovamo 2013 {published data only}
- Rovamo LM, Mattila MM, Andersson S, Rosenberg PH. Testing of midwife neonatal resuscitation skills with a simulator manikin in a low‐risk delivery unit. Pediatrics International 2013;55(4):465‐71. [DOI] [PubMed] [Google Scholar]
Xu 2014 {published data only}
- Xu T, Wang H, Gong L, Ye H, Yu R, Wang D, et al. The impact of an intervention package promoting effective neonatal resuscitation training in rural China. Resuscitation 2014;85(2):253‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Baskett 2005
- Baskett PJ, Nolan JP, Handley A, Soar J, Biarent D, Richmond S. European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2005. Section 9. Principles of training in resuscitation. Resuscitation 2005;67S1:S181–9. [DOI] [PubMed] [Google Scholar]
Berkley 2005
- Berkley JA, Maitland K, Mwangi I, Ngetsa C, Mwarumba S, Lowe BS, et al. Use of clinical syndromes to target antibiotic prescribing in seriously ill children in malaria endemic area: observational study. BMJ 2005;330(7498):995. [DOI] [PMC free article] [PubMed] [Google Scholar]
EPOC 2014
- Effective Practice and Organisation of Care (EPOC). EPOC Resources for Review Authors. Oslo: Norwegian Knowledge Centre for the Health Services, 2014. http://epoc.cochrane.org/epoc‐specific‐resources‐review‐authors.
Forsberg 2007
- Forsberg BC, Petzold MG, Thompson G, Allebeck P. Diarrhoea case management in low‐ and middle‐income countries ‐ an unfinished agenda. Bulletin of the World Health Organization 2007;85(1):42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Forsetlund 2009
- Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf F, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD003030.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gove 1999
- Gove S, Tamburlini G, Molyneux E, Whitesell P, Campbell H. Development and technical basis of simplified guidelines for emergency triage assessment and treatment in developing countries. WHO Integrated Management of Childhood Illness (IMCI) Referral Care Project. Archives of Disease in Childhood 1999;81(6):473–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ, GRADE Working Group. Rating quality of evidence and strength of recommendations: what is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336(7651):995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Irimu 2008
- Irimu G, Wamae A, Wasunna A, Were F, Ntoburi S, Opiyo N, et al. Developing and introducing evidence based clinical practice guidelines for serious illness in Kenya. Archives of Disease in Childhood 2008;93(9):799‐804. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jabbour 1996
- Jabbour M, Osmond MH, Klassen TP. Life support courses: are they effective?. Annals of Emergency Medicine 1996;28:690‐8. [DOI] [PubMed] [Google Scholar]
Jewkes 2003
- Jewkes F, Phillips B. Resuscitation training of paediatricians. Archives of Disease in Childhood 2003;88:118–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2012
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Child Health Epidemiology Reference Group of WHO and UNICEF. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012;379(9832):2151‐61. [DOI] [PubMed] [Google Scholar]
McKenna 1985
- McKenna S, Glendon A. Occupational first aid training: decay in cardiopulmonary resuscitation (CPR) skills. Journal of Occupational Psychology 1985;58:109‐17. [Google Scholar]
Mello 2003
- Mello MJ, dos Santos ER, Buzzati R, et al. Pregnancy, childbirth, postpartum and newborn care guide for essential practice. Integrated Management of Childbirth. Geneva, Switzerland: World Health Organization, 2003:1‐178. [Google Scholar]
Molyneux 2006
- Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource‐constrained setting. Bulletin of the World Health Organization 2006;84(4):314–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nolan 2001
- Nolan T, Angos P, Cunha AJ, Muhe L, Qazi S, Simoes EA, et al. Quality of hospital care for seriously ill children in less‐developed countries. Lancet 2001;357(9250):106‐10. [DOI] [PubMed] [Google Scholar]
Pio 2003
- Pio A. Standard case management of pneumonia in children in developing countries: the cornerstone of the acute respiratory infection programme. Bulletin of the World Health Organization 2003;81(4):298–300. [PMC free article] [PubMed] [Google Scholar]
Raupp 2007
- Raupp P, McCutcheon C. Neonatal resuscitation ‐ An analysis of the transatlantic divide. Resuscitation 2007;75(2):345–9. [DOI] [PubMed] [Google Scholar]
Rowe 2002
- Rowe AK. Design effects and intraclass correlation coefficients from a health facility cluster survey in Benin. International Journal for Quality in Health Care 2002;14(6):521‐3. [DOI] [PubMed] [Google Scholar]
Rowe 2008
- Rowe AK, Rowe SY, Holloway KA, Ivanovska I, Muhe L, Lambrechts T. A systematic review of the effectiveness of shortening Integrated Management of Childhood Illness guidelines training: final report. A Systematic Review of the Effectiveness of Shortening Integrated Management of Childhood Illness Guidelines Training: Final Report. Geneva, Switzerland: World Health Organization, 2008. [Google Scholar]
Sazawal 2001
- Sazawal S, Black RE, for the Pneumonia Case Management Trials Group. Effect of pneumonia case management on mortality in neonates, infants, and preschool children: a meta‐analysis of community‐based trials. Lancet Infectious Diseases 2001;3(9):547–56. [DOI] [PubMed] [Google Scholar]
Seale 2014
- Seale AC, Blencowe H, Manu AA, Nair H, Bahl R, Qazi SA, et al. pSBI Investigator Group. Estimates of possible severe bacterial infection in neonates in sub‐Saharan Africa, south Asia, and Latin America for 2012: a systematic review and meta‐analysis. Lancet Infectious Disease 2014;14(8):731‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tulloch 1999
- Tulloch J. Integrated approach to child health in developing countries. Lancet 1999;354(Suppl 2):S1116‐20. [DOI] [PubMed] [Google Scholar]
WHO 2002
- World Health Organization. Training course on the management of severe malnutrition. Training Course on the Management of Severe Malnutrition. Geneva, Switzerland: World Health Organization, 2002. [Google Scholar]
WHO 2005
- World Health Organization. The World Health Report: 2005: make every mother and child count. The World Health Report 2005: Make Every Mother and Child Count. Geneva, Switzerland: World Health Organization, 2005. [Google Scholar]
References to other published versions of this review
Opiyo 2010
- Opiyo N, English M. In‐service training for health professionals to improve care of the seriously ill newborn or child in low and middle‐income countries. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD007071.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


