Abstract
Purpose.
We reported the clinical and echographic features of colobomas, prevalence of retinal detachment, and associated visual acuity in these patients
Methods.
The study is a nonrandomized consecutive case series of 140 colobomatous eyes in 98 patients (age range, 0–83 years). Coloboma depth, width, volume, and relative coloboma excavation (coloboma depth/axial length) were measured using standardized echographic images. The presence of structural and other ocular abnormalities was noted. The clinical and echographic findings present were correlated with visual acuity of the patient. In addition, these features were correlated with the presence or absence of retinal detachment.
Results.
Increased relative coloboma excavation was significantly associated with an increased risk of retinal detachment. A relative coloboma excavation (ratio of coloboma depth to axial length) greater than 0.15 was associated with an increased risk of retinal detachment (52%), compared to those with a relative coloboma excavation less than 0.15 (23%, P = 0.014). The presence of any structural abnormality and the presence of a retrobulbar cyst were associated with increased risk of retinal detachment and severe visual impairment (worse than 20/200). Increased coloboma depth, width, volume, and relative coloboma excavation were not associated with increased risk of severe visual impairment.
Conclusions.
Clinical and echographic features of colobomas may be used in predicting the risk of retinal detachment. Measuring relative coloboma excavation upon presentation may alter follow-up and assist in the diagnosis of retinal detachment.
Keywords: retina, coloboma, echography
Echography can be used to measure the size of colobomas. An increased ratio of the coloboma depth to the axial length (relative coloboma excavation) was associated with an increased risk of retinal detachment.
Congenital retinochoroidal and optic nerve colobomas are conditions characterized by altered ocular tissue in one or more locations since birth. Ocular colobomas are thought to be secondary to defects in embryogenesis in which there is impaired closure of the optic fissures resulting in a defect in the cornea, lens, optic nerve, and/or uvea.1 Colobomas are present in 0.52 to 2.43 infants per 10,000 live births, with retinochoroidal colobomas accounting for 64%.3
The visual prognosis in eyes with colobomas is highly variable and contingent on the extent of macular or optic nerve involvement, or globe disorganization. Colobomas without microcornea or microphthalmos have the best visual prognosis, while complex colobomas associated with microphthalmos and retrobulbar cysts have the worst visual prognosis.4,5 Given the heterogeneity in presentation, these patients have challenging management issues.
Currently, management involves early recognition and treatment of any associated complications, including cataracts, glaucoma, and retinal detachment.6 The rate of retinal detachment in eyes with retinochoroidal colobomas is significantly higher than the general population risk with reported cross-sectional rates of 2.4%7, 8.1%,8 and 29%.9 This increased risk is attributed to impaired differentiation and stability of the retina, which predisposes to retinal breaks often at the junction of the undifferentiated (intercalary membrane) and differentiated retina.8
In the current study, ocular echography is used to determine the extent and volume of the coloboma. Additionally, the study correlates clinical and echographic features of the coloboma with risk of retinal detachment and visual prognosis. To the best of our knowledge, this report represents the first study to use echography to evaluate this cohort of patients.
Methods
This retrospective study was approved by the Institutional Review Board of the University of Miami Miller School of Medicine and included all patients with documented retinochoroidal or optic nerve coloboma seen at the Bascom Palmer Eye Institute from 1976 to 2014. The study was conducted in compliance with the Declaration of Helsinki. Patients were identified by searching all patients for diagnosis of “retinochoroidal coloboma,” “optic nerve coloboma,” or “coloboma” in ultrasound logs. Patients with morning glory syndrome were excluded. Patient charts were reviewed and the data collected included: demographics, location, and extent of coloboma involvement, ultrasound measurement of maximal coloboma width and depth, presence of retrobulbar cysts, and, if present, their size, visual acuity, presence of retinal or choroidal detachment, structural abnormalities (microphthalmia, anophthalmia, microcornea, or any combination), other ocular conditions (amblyopia, glaucoma, cataract, anisometropia, strabismus, nystagmus), and any other nonocular associations (cardiac, ear, skeletal, or urogenital abnormalities, seizures, CHARGE syndrome).
When applicable, the Snellen decimal chart was used and expressed as a logarithm of the minimum angle of resolution (logMAR). Visual fractions were assigned for young children or those with severe visual impairments. Severe visual impairment (SVI) was defined as a visual acuity of 20/200 or worse as per the World Health Organization (WHO) Internal Classification of Diseases (ICD)–10 classification system.10 Count fingers (CF) was equivalent to 1/200 or logMAR 2.3. Hand motion (HM) was equivalent to 0.5/200 or logMAR 2.6. Light perception (LP) was equivalent to 0.2/200 or logMAR 3.0. No light perception (NLP) was equivalent to 0.02/200 or logMAR 4.0. Eyes that were enucleated or eviscerated were considered to be no light perception. A P value of <0.05 was statistically significant. The visual acuities of patients less than 2 years of age were included if they were measured by the Snellen system. Two patients less than 2 years old were excluded because their visual acuities were not measured by the Snellen system and an additional 15 patients did not have visual acuities recorded.
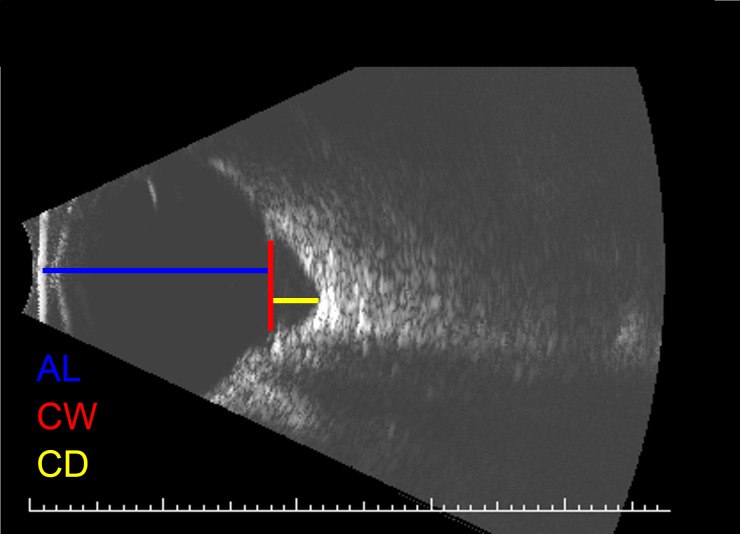
The axial length of the eye was measured with a portable ultrasound probe. The axial length was measured to the nearest millimeter with calipers and, when available, these measurements were taken directly from the image report. Care was taken to exclude the coloboma when measuring the axial length so as not to artificially increase this value. Microphthalmia was defined as an eye with axial length less than 2 SD below the mean for that age (axial length < 16 mm at birth, < 19 mm at 1 year).11 The horizontal corneal diameter was measured to the nearest millimeter with calipers and, when available, these measurements were taken directly from the image report. Microcornea was defined as a cornea with horizontal diameter less than 10 mm.12 Structural abnormality was a broad term that was defined as one or a combination of the following: microphthalmia, microcornea, or anophthalmia. When present, the maximum height and width of each retrobulbar cyst was measured with calipers from the available archived images (76 images from 1998–2014). Additionally, the maximum depth and maximum width of each coloboma was measured with calipers from the available archived images. The maximum depth of the coloboma was defined as the measurement between the apex of the coloboma and the extrapolated base of the retina. The volume of the coloboma used in the statistical analyses was an average of the coloboma volume calculated as a cylinder (3.147 * r2 * h) and as a cone (1/3 * [3.147 * r2 * h]). We believe this volume determination model provides a fair assessment of the coloboma given the limited measurement parameters that were retrospectively feasible. Relative coloboma excavation was defined as coloboma depth/axial length. This ratio was intended to normalize the coloboma over different axial lengths. When the distinction was made, the better eye was defined as the eye with the best-corrected visual acuity. In cases where visual acuity in both eyes was identical, the better eye was defined as the eye with the smallest coloboma volume. All measurements were performed by the same examiner. Hand-held calipers were used for printed images, while digital calipers were used for electronic images. An example of the measurements taken is provided in Figure 1. Because the study consisted of patients seen over a 38-year period, multiple ultrasound machines were used by different technicians to take the photos.
Figure 1.
Sample coloboma measurement. AL, axial length; CW, coloboma width; CL, coloboma length.
All statistical analyses were performed with SPSS 22.0 (SPSS, Inc., Chicago, IL, USA) statistical package. ANOVA was used to compare categorical variables with logMAR visual acuity. Pearson correlation was used to compare coloboma and retrobulbar cyst measurements with logMAR visual acuity. χ2 test was used to compare categorical variables with the presence or absence of retinal detachment. Student's t-test was used to compare coloboma and retrobulbar cyst measurements with the presence or lack of retinal detachment. Cox regression was used in the analysis of risk factors for retinal detachment.
Results
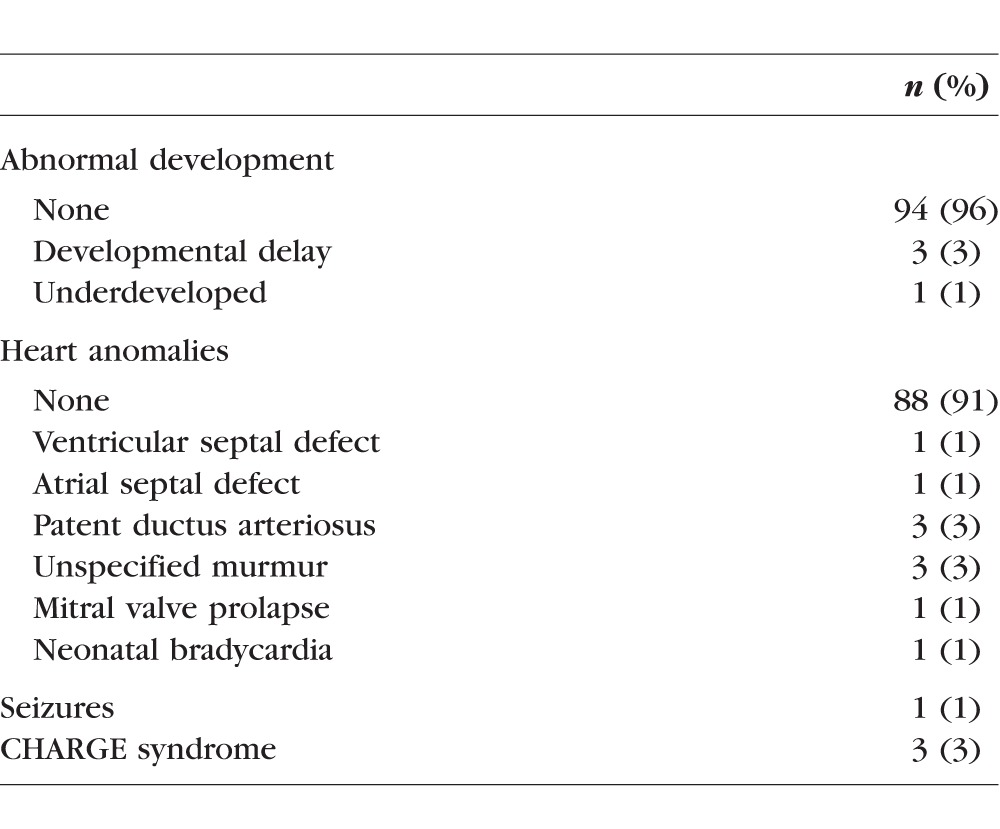
The study consisted of 140 colobomas of 98 patients. Bilateral colobomas were present in 42/98 (42.9%) patients. The mean age at diagnosis was 11 ± 22 years (median = 0.86; range, 0–83 years); the mean age at last follow-up was 14 ± 20 years (median = 6.6; range, 0.34–81 years). Of the patients, 58% (58/98) were under the age of 2 at diagnosis. Complete patient demographics are shown in Table 1. Abnormal mental development was present in four patients and CHARGE syndrome in three patients. Other associated nonocular conditions are shown in Table 2.
Table 1.
Patient Demographics
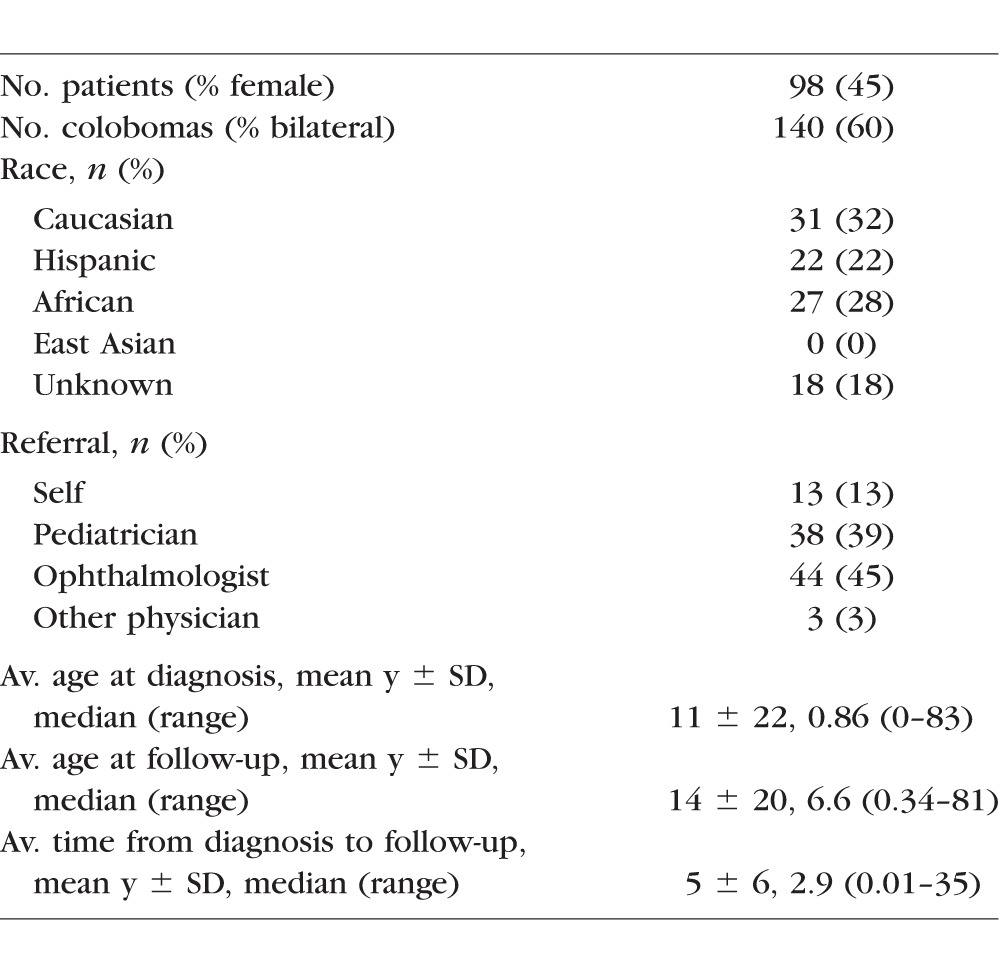
Table 2.
Nonocular Disorders Present in Cohort
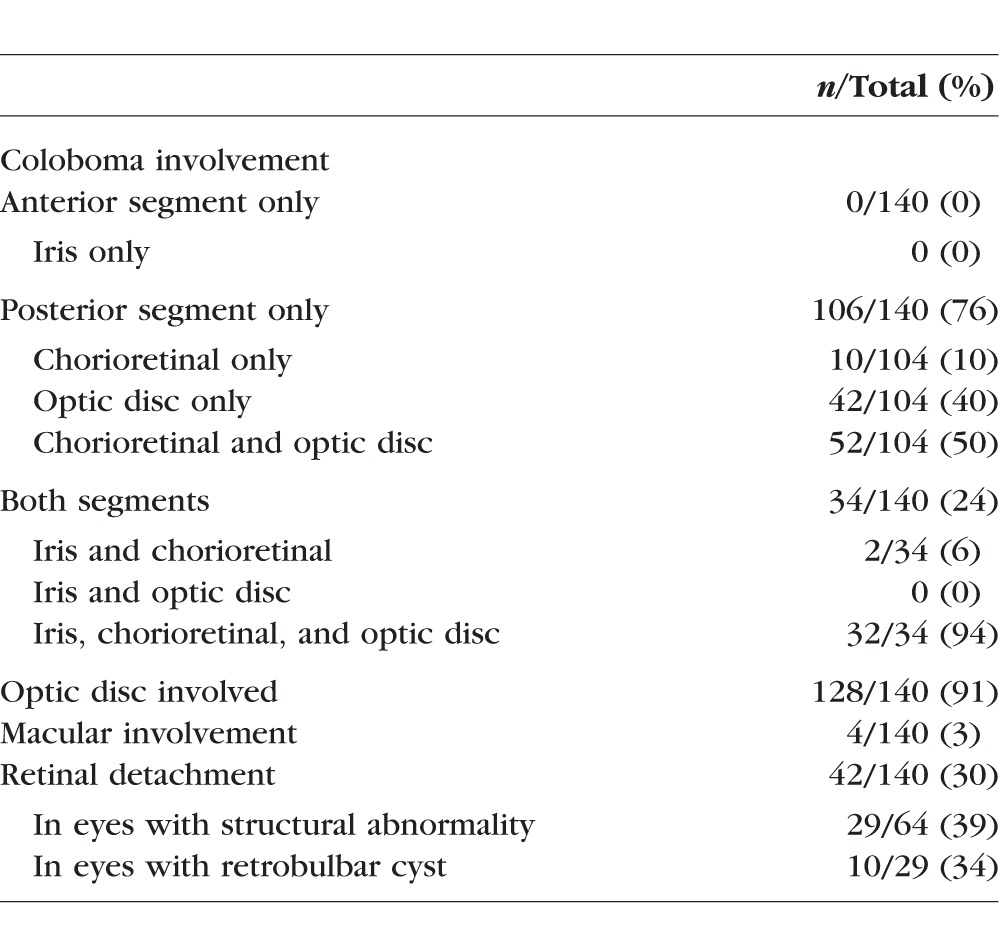
Retrobulbar cysts were present in 29 eyes (21% of total eyes) and any structural abnormality was present in 64 eyes (46%), the most common of which was microphthalmia in 58 eyes (41%). Expanded ocular characteristics are shown in Table 3. Colobomas involved the optic disc in 128 eyes (91%) and were confined to the posterior segment in 106 eyes (76%). Colobomas involved the posterior and anterior segment in 34 eyes (24%). Retinal detachment (RD) was present in 42/140 eyes (30%, Table 4).
Table 3.
Patient Ocular Characteristics
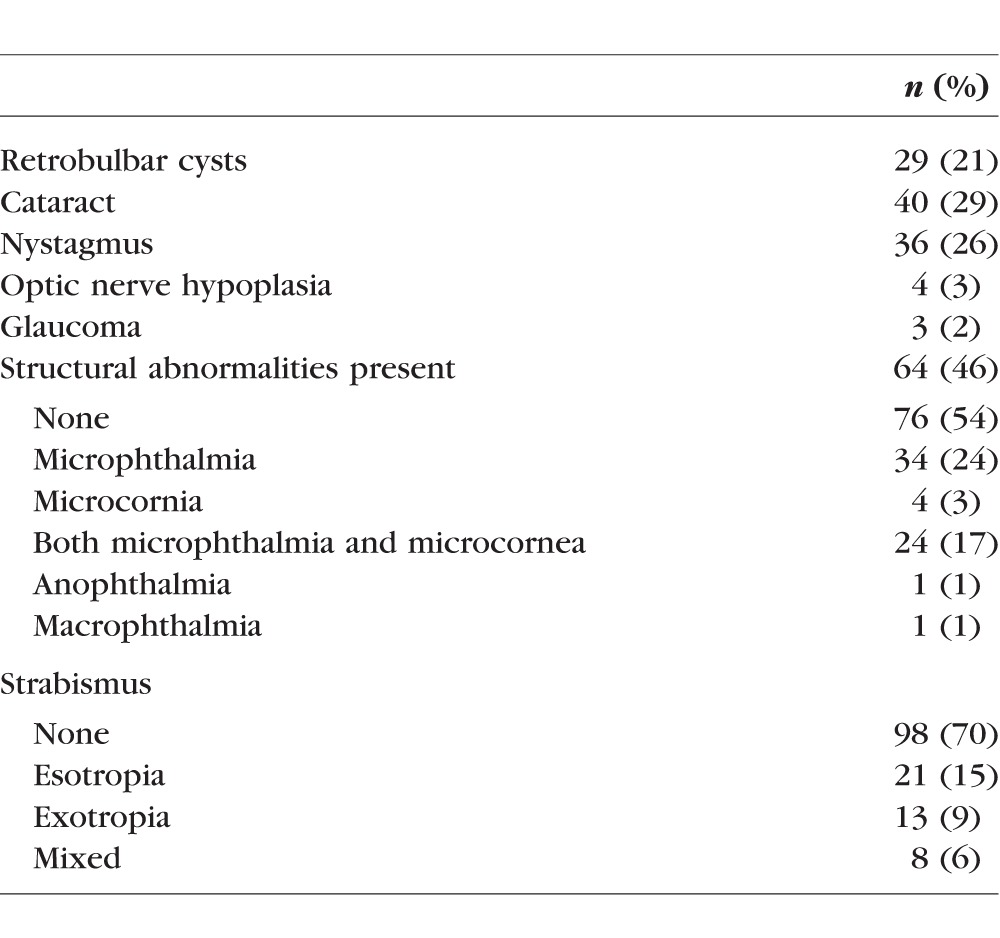
Table 4.
General Coloboma Characteristics in Cohort
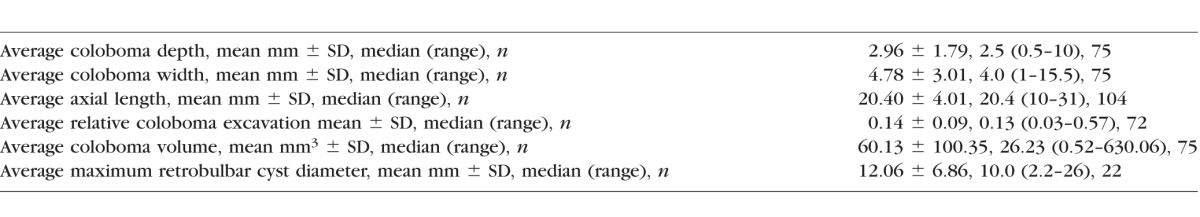
Complete echographic measurements, including depth, width, volume, and relative coloboma excavation (coloboma depth/axial length), are listed in Table 5.
Table 5.
Echographic Characteristics of Colobomas in Cohort
Correlation Between Echographic Coloboma Parameters and SVI
Coloboma width and volume were not associated with SVI. Consistent differences in magnitude existed, albeit not statistically significant, in comparing coloboma depth with SVI in the better eye (2.56 mm in eyes without SVI versus 3.04 mm in eyes with SVI, P = 0.46) and worse eye (2.25 mm in eyes without SVI versus 3.07 mm in eyes with SVI, P = 0.28) comparisons.
Relative coloboma excavation (coloboma depth/axial length) was not associated with SVI. However, there was a trend toward increasing relative coloboma excavation and SVI (0.11 in better-seeing eyes without SVI versus 0.15 in better-seeing eyes with SVI, P = 0.25).
The presence of any structural abnormality was associated with SVI in the better eye (P = 0.002) and worse eye (P = 0.002) comparisons. Further visual acuity data are represented in Table 6. There are 17 patients (17%) without visual outcomes. There was no statistically significant difference in age of the patients with reported visual acuity and those without reported visual acuity (P = 0.23).
Table 6.
Best-Corrected Visual Acuity (LogMAR) at Follow-Up in the Better Eye

Correlation Between Echographic Coloboma Parameters and RD
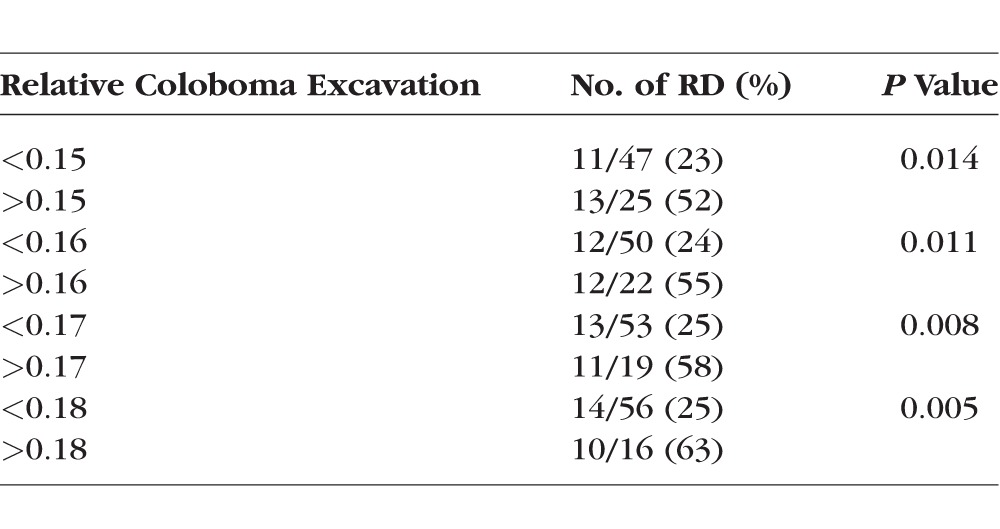
Coloboma width and volume were not associated with RD. There were consistent albeit nonsignificant differences in magnitude comparing coloboma depth to RD risk (2.69 mm in eyes without RD versus 3.5 mm in eyes with RD, P = 0.12). Relative coloboma excavation was associated with increased risk of RD (0.12 in eyes without RD versus 0.18 in eyes with RD, P = 0.04). A relative coloboma excavation greater than 0.15 was associated with increased risk of retinal detachment (52% RD rate in those with relative coloboma excavation >0.15, versus 23% in those <0.15, P = 0.014). As relative coloboma excavation increased, the risk of retinal detachment increased as well. (Table 7) Increasing age of the patient did not significantly affect the relative coloboma excavation (data not shown).
Table 7.
Demographic, Echographic, and Structural Characteristics of Eyes With and Without Retinal Detachment
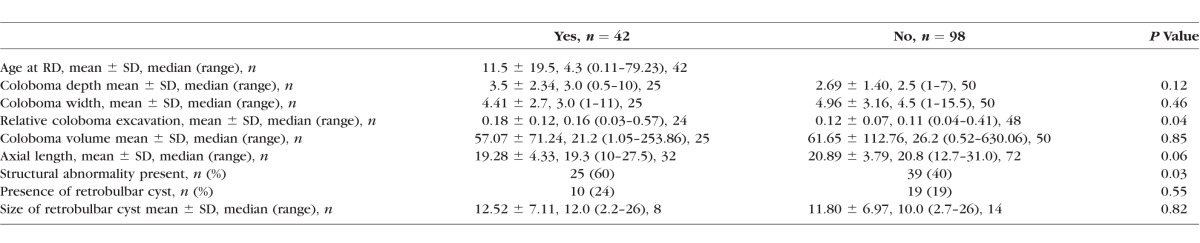
The presence of a structural abnormality was associated with increased risk of RD (40% eyes without RD were structurally abnormal versus 60% eyes with RD were structurally abnormal, P = 0.03). Complete data on RD is shown in Table 8.
Table 8.
Relative Coloboma Excavation and Risk of Retinal Detachment
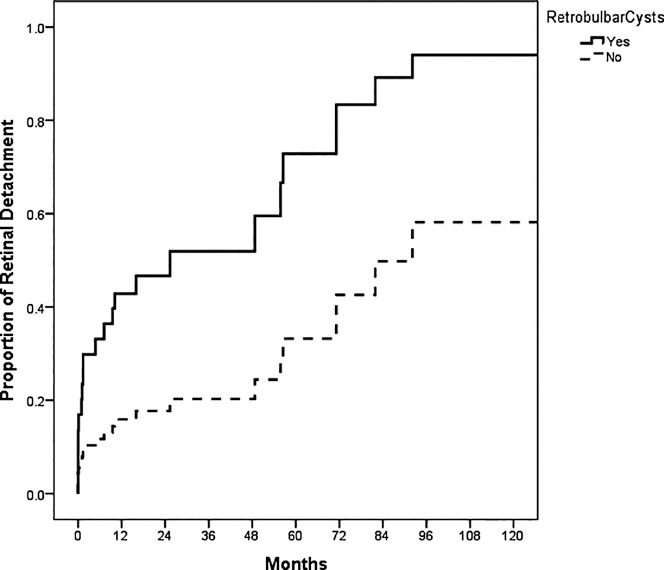
Cox regression analysis (Fig. 2) was used to evaluate the risk factors of retinal detachment, including coloboma depth, width, volume, axial length, relative coloboma excavation, structural abnormality, and presence of retrobulbar cyst. The presence of a retrobulbar cyst was associated with an increased risk of retinal detachment (P = 0.014) versus eyes without detachment.
Figure 2.
Kaplan-Meier plot comparing risk of retinal detachment with and without a retrobulbar cyst (P = 0.12). When a Cox regression analysis is performed, including coloboma depth, CW, CD/AL (coloboma excavation), coloboma volume, AL, structural abnormality, and presence of retrobulbar cyst, retrobulbar cyst is the only statistically significant risk factor (P = 0.014).
Discussion
The visual acuity in eyes with colobomas is generally poor. At last follow up, 87% of patients in the current study had a visual acuity worse than 20/200. Increased coloboma depth, width, volume, and relative coloboma excavation were not associated with an increased risk of severe visual impairment. The visual acuity was worse if structural abnormalities, particularly retrobulbar cyst, or retinal detachment were present.
Retinal detachment is a well-recognized risk in the setting of coloboma and occurred in 42 (30%) of 140 eyes in this series, consistent with previously cited studies with retinal detachment in up to 40% of eyes with coloboma.9,13–15 Given the current series and previously published reports were generated from tertiary referral centers, this high rate of detachment may represent a selection bias with an exaggerated estimation. Nonetheless, retinal detachment in the setting of retinochoroidal coloboma is a real risk with rates far surpassing the general population risk estimated at less than 1%.16,17
The surgical management of retinal detachment in eyes with coloboma is challenging. Since patients often are too young to adequately communicate visual changes, many patients present with longstanding and total retinal detachments. In the current series, only 10/42 (24%) eyes underwent surgical correction, as the remaining eyes were deemed inoperable.
The finding that structurally disrupted eyes with undifferentiated retinas are more likely to incur retinal detachment is intuitive. Therefore, it is not surprising that the current series demonstrates an association between structural abnormalities and increased risk of retinal detachment. However, inherently disrupted eyes are more likely to have nonfunctional vision at baseline, making it difficult to achieve early diagnosis. Therefore, identifying alternate features that prognosticate retinal detachment in colobomatous eyes with functional vision is important, particularly in the preverbal or minimally communicative patient.
Thus, we sought to correlate echographic characteristics of the coloboma with retinal detachment. Notably, the depth, width, and volume of the coloboma did not statistically demonstrate an increased risk of retinal detachment. One explanation for this is the size or volume of the coloboma may not alter the risk of retinal detachment. An alternative explanation was the study was not sufficiently powered to determine statistical significance. Antecedent to the data analysis, we established a ratio (relative coloboma excavation) as an attempt to normalize the coloboma measurements for axial length variations. When evaluating this parameter (coloboma depth/axial length), larger relative coloboma excavation was associated with increased risk of retinal detachment. We found that a relative coloboma excavation of greater than 0.15 was associated with increased risk of retinal detachment. This suggests that relative excavation of the coloboma may prognosticate risk of retinal detachment.
Gopal et al.,18 via the use of optical coherence tomography (OCT), evaluated colobomas to identify the transition zone between undifferentiated (intercalary membrane) and differentiated retina. In addition to detecting subclinical retinal detachments not evident on clinical examination, they were able to identify the communication between the subintercalary membrane space and the subretinal space, indicating the site of the break. While retinal breaks sometimes can occur in the peripheral retina, the majority of breaks occur at the edge of the retinal detachment inside the coloboma or as atrophic holes within the detached colobomatous retina.13 As the weak point often is at the junction between the normal and atrophic retina, we hypothesized that deeper colobomas with a sharper turn angle between the colobomatous and noncolabomatous retina would be subject to increased vitreoretinal traction and increased intercalary membrane breaks. While the angle of descent into the coloboma was not measured, volumetric parameters of the coloboma were measured in the current series. The finding that relative choroidal excavation via ultrasound was associated with increased risk of retinal detachment supports this hypothesis. A prospective evaluation and a higher-powered study would be required to further substantiate this finding.
There are limitations of this study. Given the retrospective nature, data collection was incomplete. Echo images before 1998 were not saved and catalogued, and, thus, we were not able to retrospectively measure coloboma parameters in all patients. In addition, multiple ultrasound machines were used by different technicians to produce the images over the 38-year period. Although the same examiner measured each coloboma and axial length, some patients only had printed images available, while others had digital images. Due to the nature of this study, the examiner was not blinded to the outcome of the case (i.e., presence of retinal detachment, visual impairment, and so forth). Furthermore, given the young population with 57% under the age of 2 at presentation, assessment of visual acuity was limited. Additionally, with 43% of patients with bilateral coloboma, visual acuity findings could be confounded if combined given a statistical association between the eyes and clinical effect of amblyopia. In attempt to avoid this additional confounding feature, the best visual acuity at presentation was reported. This strategy was used similarly by Hornby et al.4
To the best of our knowledge, this is the first report to describe echographic measurements of retinochoroidal and optic nerve colobomas. Additionally, we used echo parameters to find potentially more sensitive measures than gross structural abnormalities to prognosticate risk of retinal detachment. With a multimodal approach to evaluating colobomatous eyes with functional vision, early identification of comorbid complications may potentially improve our ability to stabilize vision in this population of patients. Further clinical research, however, will be required to confirm the effectiveness of echographic measurements and relative coloboma excavation to predict retinal detachment risk.
Acknowledgments
We thank Laila Teira, MD, for her help in the ultrasound department.
Supported in part by Florida Lions Eye Bank (Miami, FL, USA), Center Core Grant P30EY014801 from the National Institutes of Health (Bethesda, MD, USA), and an unrestricted grant from Research to Prevent Blindness, Inc. (New York, NY, USA). The authors alone are responsible for the content and writing of the paper.
Disclosure: V.D. Venincasa, None; Y.S. Modi, None; H.A. Aziz, None; B. Ayres, None; C. Zehetner, None; W. Shi, None; T.G. Murray, None; H.W. Flynn Jr, None; A.M. Berrocal, None
References
- 1. Gregory-Evans CY,, Williams MJ,, Halford S,, Gregory-Evans K. Ocular coloboma: a reassessment in the age of molecular neuroscience. J Med Genet. 2004; 41: 881–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bermejo E,, Martinez-Frias ML. Congenital eye malformations: clinical-epidemiological analysis of 1,124,654 consecutive births in Spain. Am J Med Genet. 1998; 75: 497–504. [PubMed] [Google Scholar]
- 3. Nakamura KM,, Diehl NN,, Mohney BG. Incidence ocular findings, and systemic associations of ocular coloboma: a population-based study. Arch Ophthalmol. 2011; 129: 69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hornby SJ,, Adolph S,, Gilbert CE,, et al. Visual acuity in children with coloboma: clinical features and a new phenotypic classification system. Ophthalmology. 2000; 107: 511–520. [DOI] [PubMed] [Google Scholar]
- 5. Berk AT,, Yaman A,, Saatci AO. Ocular and systemic findings associated with optic disc colobomas. J Pediatr Ophthalmol Strabismus. 2003; 40: 272–278. [DOI] [PubMed] [Google Scholar]
- 6. Gopal L,, Kini MM,, Badrinath SS,, Sharma T. Management of retinal detachment with choroidal coloboma. Ophthalmology. 1991; 98: 1622–1627. [DOI] [PubMed] [Google Scholar]
- 7. Maumenee IH,, Mitchell TN. Colobomatous malformations of the eye. Trans Am Ophthalmol Soc. 1990; 88: 123–132, discussion 33–35. [PMC free article] [PubMed] [Google Scholar]
- 8. Daufenbach DR,, Ruttum MS,, Pulido JS,, Keech RV. Chorioretinal colobomas in a pediatric population. Ophthalmology. 1998; 105: 1455–1458. [DOI] [PubMed] [Google Scholar]
- 9. Jesberg DO,, Schepens CL. Retinal detachment associated with coloboma of the choroid. Arch Ophthalmol. 1961; 65: 163–173. [DOI] [PubMed] [Google Scholar]
- 10. Persa C,, Osmotherly K,, Chao-Wei Chen K,, et al. The distribution of cystathionine beta-synthase (CBS) in the eye: implication of the presence of a trans-sulfuration pathway for oxidative stress defense. Exp Eye Res. 2006; 83: 817–823. [DOI] [PubMed] [Google Scholar]
- 11. Shah SP,, Taylor AE,, Sowden JC,, et al. Anophthalmos, microphthalmos, and coloboma in the United Kingdom: clinical features, results of investigations, and early management. Ophthalmology. 2012; 119: 362–368. [DOI] [PubMed] [Google Scholar]
- 12. Tucker SM,, Enzenauer RW,, Levin AV,, et al. Corneal diameter, axial length, and intraocular pressure in premature infants. Ophthalmology. 1992; 99: 1296–1300. [DOI] [PubMed] [Google Scholar]
- 13. Gopal L,, Badrinath SS,, Sharma T,, et al. Pattern of retinal breaks and retinal detachments in eyes with choroidal coloboma. Ophthalmology. 1995; 102: 1212–1217. [DOI] [PubMed] [Google Scholar]
- 14. Wang K,, Hilton GF. Retinal detachment associated with coloboma of the choroid. Trans Am Ophthalmol Soc. 1985; 83: 49–62. [PMC free article] [PubMed] [Google Scholar]
- 15. Gopal L,, Badrinath SS,, Sharma T,, et al. Surgical management of retinal detachments related to coloboma of the choroid. Ophthalmology. 1998; 105: 804–809. [DOI] [PubMed] [Google Scholar]
- 16. Mitry D,, Charteris DG,, Fleck BW,, et al. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010; 94: 678–684. [DOI] [PubMed] [Google Scholar]
- 17. Gariano RF,, Kim CH. Evaluation and management of suspected retinal detachment. Am Fam Physician. 2004; 69: 1691–1698. [PubMed] [Google Scholar]
- 18. Gopal L,, Khan B,, Jain S,, Prakash VS. A clinical and optical coherence tomography study of the margins of choroidal colobomas. Ophthalmology. 2007; 114: 571–580. [DOI] [PubMed] [Google Scholar]