Abstract
Tinnitus is a common disorder, it can be classified as pulsatile and non-pulsatile or objective and subjective. Pulsatile tinnitus is less common than non-pulsatile and can be due to vascular tumour such as glomus or vascular abnormality. We presented an interesting case of a 30 year-old Malay lady with a two-year history of pulsatile tinnitus which was worsening in three months duration. It was associated with intermittent headache. Clinical examination and tuning fork test were unremarkable. Apart from mild hearing loss at high frequency on the left ear, the pure tone audiogram (PTA) was otherwise normal. In view of the patient’s young age with no risk factor for high frequency loss, a magnetic resonance imaging (MRI) was performed to look for any abnormality in the cerebellopontine angle. It revealed a single vessel looping around the left vestibulocochlear and facial nerves at the cisternal portion, likely a branch of the anteroinferior cerebellar artery (AICA). Literature review on the pathophysiology and treatment option in this condition is discussed.
Keywords: tinnitus, hearing loss, magnetic resonance imaging, vestibulocochlear
Introduction
Tinnitus is a perception of sound in the absence of external sounds (Fornaro and Martino, 2010[4]). It can be pulsatile, which is the most common type, or non-pulsatile. It can also be classified as subjective (audible only to the patient), or objective (audible to both the patient and the examiner). There are two plausible pathophysiology of pulsatile tinnitus. The first explanation is that changes in the blood flow disrupt the laminar flow, and the resulting local turbulence is audible. Secondly, normal flow sounds within the body are perceived more intensely with increased bone conduction or the disturbance of sound conduction leads to loss of the masking effect of external sounds (Hofmann et al., 2013[5]).
Pulsatile tinnitus is commonly seen in the presence of anatomical variants or abnormal extracranial or intracranial blood vessels, or intracranial hypertension (De Ridder et al., 2013[3]). It is not related to abnormal auditory system in most cases. As it is vascular in origin, it can be arterial or venous in origin, or it may originate from capillaries or arteriovenous transition. Typical arterial causes include atherosclerosis, fibromusculardysplasia, arterial aneurysm, dissection, and anatomical variants like aberrant internal carotid artery, laterally displaced carotid artery, persistent stapedial artery and vascular loops. Common arteriovenous causes include arteriovenous fistulae and malformations and highly vascularised skull base tumours such as paragangliomas (glomus tumour), tumours of the temporal bone (metastases, basal meningiomas, haemangiomas, Heffner tumours) and Paget’s disease. Venous causes include idiopathic intracranial hypertension, jugular bulb variants and dural venous thrombosis (Hofmann et al., 2013[5]; Panda et al., 2013[9]). Among the vascular variants, vascular loops in the cerebellopontine angle are the most common cause of pulsatile tinnitus, and are thought to cause neurovascular contact with the vestibulocochlear nerve leading to tinnitus (Panda et al., 2013[9]; Nowé et al., 2004[8]).
As most pulsatile tinnitus cases are of vascular origin, it is often possible to diagnose the underlying cause with imaging, either MRI, CT or magnetic resonance angiography. Any patient presented with pulsatile tinnitus should have an imaging done to diagnose the underlying cause.
Case presentation
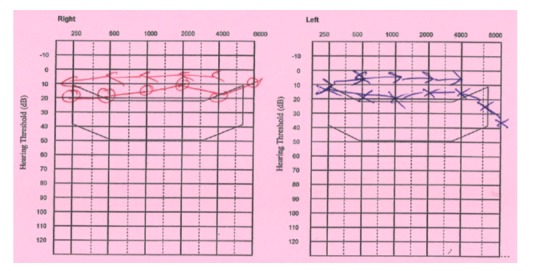
A 30 year-old lady with a two-year history of pulsatile tinnitus in the left ear presented to our clinic with worsening tinnitus in the last three months. This was accompanied by a generalised intermittent headache. She denied any vertigo. She was previously fit and well with no co-morbidities. She works as a call centre agent at an insurance company which involves wearing a speaker phone on the right ear. Clinical examination was unremarkable with normal otoscopic examination, tuning fork test and facial nerve function. Her pure-tone audiometry showed mild hearing loss at high frequency on the left, the right side was normal (Figure 1(Fig. 1)).
Figure 1. Pure-tone audiometry of mild hearing loss at high frequency on the left compared to the normal hearing threshold on the right.
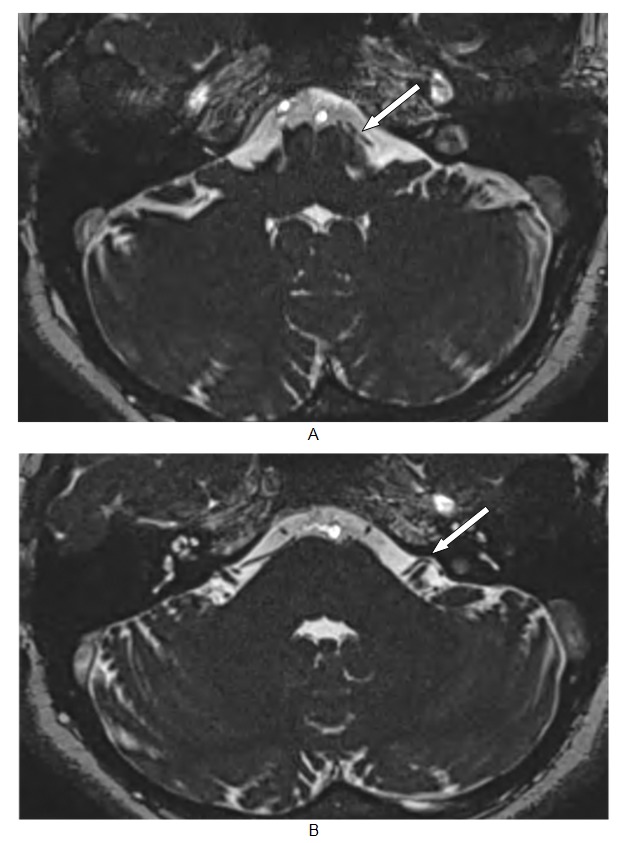
In view of the unilateral tinnitus and her young age without any risk factor for a high frequency hearing loss, an MRI was performed to look for any abnormality in the cerebellopontine angle. This revealed a single vessel looping around the cisternal portion of the left vestibulocochlear and facial nerves, the vessel is most likely a branch of the left AICA. There was no focal enhancing lesion seen at the left cerebellopontine angle or the internal auditory canal (Figure 2(Fig. 2)).
Figure 2. Axial 3D CISS image showing (A) a linear structure originating from the basilar artery corresponding to the left anterior inferior cerebellar artery (white arrow) which loops around the cisternal portion of left VIIth and VIIIth nerve (white arrow) (B). The VIIth nerve is not well-visualized as the vascular loop causes overlapping of the structure.
Discussion
The anatomy of the neurovascular complex at the cerebellopontine angle is highly variable. This has been attributed to the late development of the anterior inferior cerebellar artery (AICA) and the posterior inferior cerebellar artery (PICA) from the primitive lateral basilovertebral anastomosis. This is largely seen in the posterior fossa vessels with relation to the facial-vestibulocochlear nerve complex (Wuertenberger and Rosahi, 200[11]9; Kim et al., 1990[6]). Vascular compression of the eighth nerve may lead to related symptoms such as tinnitus, hearing loss, vertigo and imbalance. Similarly, compression of the facial nerve may cause hemifacial spasm. Interestingly, there was a radiological study that found patients with pulsatile tinnitus have vascular loops in the internal auditory canal, whereas the non-pulsatile tinnitus group was found to have vascular loops in the cisternal portion of the eighth cranial nerve (Nowé et al., 2004[8]).
Our patient has a vascular loop which originates from the AICA around the cisternal portion of the vestibulocochlear and facial nerves which may have explained her pulsatile tinnitus. In most reported cases, vascular loop around the seventh and eighth nerve would cause pulsatile tinnitus, hearing loss, vertigo and hemifacial spasm (Kim et al., 1990[6]; Chang et al., 2013[1]). However, our patient presented with pulsatile tinnitus, mild hearing loss and headache instead, without vertigo or hemifacial spasm.
Microvascular decompression (MVD) surgery has been used to treat tinnitus as neurovascular compression of the vestibulocochlear nerve is assumed to be one of the causes of tinnitus. This type of tinnitus is similar to other neurovascular compression syndromes, such as hemifacial spasm and trigeminal neuralgia (Chang et al., 2013[1]). MVD is also practised in other cranial rhizopathies such as trigeminal neuralgia and hemifacial spasm which has led to symptomatic relief in majority of the sufferers.
Several published reports have been focusing on MVD of the eighth nerve in the cerebellopontine angle by isolating the nerve from the compressing vessel with Teflon felt or muscle grafts (Wuertenberger and Rosahi, 2009[11]; Møller et al., 1993[7]; De Ridder et al., 2010[2]; Roland et al., 1995[10]). This technique has shown to improve or eliminate tinnitus, thus it seems to confirm that these abnormalities were indeed a direct effect of compression of the eighth nerve by the offending vessels. Having said this, other proposed theories of pathophysiology which cause tinnitus need to be considered as some MVD yielded no success. This is especially true in patients with both tinnitus and hemifacial spasm, in that after MVD, the hemifacial spasm outcome is better than its tinnitus counterpart. An irreversible change in the central auditory nervous system may be attributable to these symptoms, and further study would be helpful in understanding this change (Chang et al., 2013[1]).
This subject is opened for further discussion as the pathophysiology of tinnitus remains poorly understood. This hopefully will invite many studies or research to help us further understand this phenomenon, which in turn will benefit our patients in receiving the best possible treatment.
References
- 1.Chang WS, Kim BS, Lee JE, Jung HH, Kim K, Kwon HC, et al. Is tinnitus accompanied by hemifacial spasm in normal-hearing patients also a type of hyperactive neurovascular compression syndrome: a magnetoencephalography study. BMC Neurol. 2013;13:42. doi: 10.1186/1471-2377-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Ridder D, Vanneste S, Adriaenssens I, Lee AP, Plazier M, Menovsky T, et al. Microvascular decompression for tinnitus: significant improvement for tinnitus intensity without improvement for distress. A 4-year limit. Neurosurgery. 2010;66:656–660. doi: 10.1227/01.NEU.0000366110.87836.53. [DOI] [PubMed] [Google Scholar]
- 3.De Ridder D, Vanneste S, Menovsky T. Pulsatile tinnitus due to a tortuous siphon-like internal carotid artery successfully treated by arterial remodelling. Case Rep Otolaryngol. 2013;2013:938787. doi: 10.1155/2013/938787.. Available from: http://dx.doi.org/10.1155/2013/938787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fornaro M, Martino M. Tinnitus psychopharmacology: A comprehensive review of its pathomechanisms and management. Neuropsychiatr Dis Treat. 2010;6:209–218. doi: 10.2147/ndt.s10361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hofmann E, Behr R, Neumann-Haefelin T, Schwager K. Pulsatile tinnitus: imaging and differential diagnosis. Dtsch Arztebl Int. 2013;110:451–458. doi: 10.3238/arztebl.2013.0451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim HN, Kim Y, Park IY, Kim GR, Chung IH. Variability of the surgical anatomy of the neurovascular complex of the cerebellopontine angle. Ann Otol Rhinol Laryngol. 1990;99:288–296. doi: 10.1177/000348949009900408. [DOI] [PubMed] [Google Scholar]
- 7.Møller MB, Møller AR, Jannetta PJ, Jho HD, Sekhar LN. Microvascular decompression of the eighth nerve in patients with disabling positional vertigo: selection criteria and operative results in 207 patients. Acta Neurochir. 1993;125:75–82. doi: 10.1007/BF01401831. [DOI] [PubMed] [Google Scholar]
- 8.Nowé V, De Ridder D, Van de Heyning PH, Wang XL, Gielen J, Van Goethem J, et al. Does the location of a vascular loop in the cerebellopontine angle explain pulsatile and non-pulsatile tinnitus? Eur Radiol. 2004;14:2282–2289. doi: 10.1007/s00330-004-2450-x. [DOI] [PubMed] [Google Scholar]
- 9.Panda A, Arora A, Jana M. Persistent primitive trigeminal artery: an unusual cause of vascular tinnitus. Case Rep Otolaryngol. 2013;2013:275820. doi: 10.1155/2013/275820.. Available from: http://dx.doi.org/10.1155/2013/275820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roland PS, Fell W, Meyerhoff W. Surgical decompression of the eighth nerve for tinnitus. Int Tinnitus J. 1995;1:139–146. [PubMed] [Google Scholar]
- 11.Wuertenberger CJ, Rosahi SK. Vertigo and tinnitus caused by vascular compression of the vestibulocochlear nerve, not intracanalicular vestibular schwannoma: review and case presentation. Skull Base. 2009;19:417–424. doi: 10.1055/s-0029-1220209. [DOI] [PMC free article] [PubMed] [Google Scholar]


