Abstract
Objectives
Evaluation of double cross plasty for management of obstructive or non obstructive transverse vaginal septum.
Methods
13 patients presented either as cryptomenorrhoea or as infertility/dyspareunia were diagnosed to have transverse vaginal septum. They were subjected to double cross plasty and were subsequently followed up for period of two years.
Results
13 patients presented either as cryptomenorrhoea or infertility/dyspareunia. Nine patients had transverse vaginal septum at low level, three at midlevel, and one had high-level septum. The thickness of septum was 1–3 cms in 12 patients. Double cross plasty was performed in all patients. One patient with high vaginal septum which was thick needed bilateral labial flaps. All patients were followed up to period of 2 years and none had restenosis. Three patients had pregnancies with vaginal delivery in two of them.
Conclusion
Double cross plasty for management of transverse vaginal septum is a better technique compared with currently used surgical methods. In our series, it did not cause restenosis and some of our patients were able to deliver vaginally.
Keywords: Transverse vaginal septum, Double cross plasty, Hematocolpos
Introduction
Different anomalies of the mullerian ducts are described and one of the most difficult anomaly to manage clinically is of disorder of the vertical fusion of the mullerian ducts, i.e., transverse vaginal septum. The transverse vaginal septum—obstructive or non obstructive is a developmental defect in the embryogenesis of the vagina that leads to incomplete fusion between the mullerian duct component and the urogenital sinus component of the vagina. Transverse vaginal septum varies in thickness and can be located at almost any level in the vagina, but commonly seen in the upper and middle one-third of vagina.
Several surgical treatment modalities have been developed to treat congenital transverse vaginal septum either by simple incision to surgical excision of the thick septum followed by approximation of the cut edges of the upper and lower vaginal mucous membrane. This technique of simple approximation by interrupted sutures may result in ring of stenosis and vaginal shortening.
To overcome this complication of restenosis, we managed a case of vaginal stenosis following simple incision and drainage of haematocolpos by double crossplasty very successfully [1]. The technique of crossplasty or "Z" plasty has been employed by plastic surgeons for the permanent release of unyielding surgical scars, choanal atresia, etc., with outstanding results. But the operation has received very little attention from the gynecologists.
The procedure is described as “An ingenious but rather complicated ‘Z’ plasty method of bridging the gap has been described by GARCIA in 1967” [2].
If the vaginal septum is complete, obstruction may result in haematocolpos, haematometra, and haematosalpinx around puberty and if it is partially obstructive may be discovered on routine gynecologic examination, when patient presents for either primary infertility or dyspareunia.
We would like to share our experience of Double crossplasty technique in 13 cases of transverse vaginal septum. The technique is comparatively simple to perform in middle- and low-level transverse vaginal septae and gynecologist can successfully manage such cases. However for high vaginal septum which is near to the cervix and likely to be more thick, is better managed with the help of plastic surgeons.
The aim is to share our experience of Treating 13 cases of transverse vaginal septum by double crossplasty and evaluation of the technique for post operative results, post operative child bearing, etc.
Materials and Methods
Total no. of 13 cases of transverse vaginal septum who presented either as primary amenorrhoea, infertility/dyspareunia or with recurrence of symptoms of haematocolpos/haematometra over a period of 20 years were included in the study.
All 13 patients were subjected to double Cross Plasty/‘Z’ Plasty.
In all patients detail history was taken, general and systemic examination was done, per abdominal, per speculum, and per rectal examination was done to assess the cause of obstruction, site of vaginal septum and presence of haematocolpos/haematometra, etc.
Besides routine investigations transvaginal/transperineal ultrasonography was done to ascertain the site of transverse vaginal septum ,i.e., high, mid or low, and thickness of the transverse vaginal septum was taken. Presence of haematocolpos, haematometra, and haematosalpinx was noted. Intra venous urography was done to rule out the associated renal anomalies. Surgery was performed under regional anesthesia.
Surgical Technique
Transverse vaginal septum has two layers with fibroareolar tissue in between. The lower/distal surface is always covered by squamous epithelium and upper/proximal surface is covered by glandular epithelium with fibroareolar tissue in between [3].
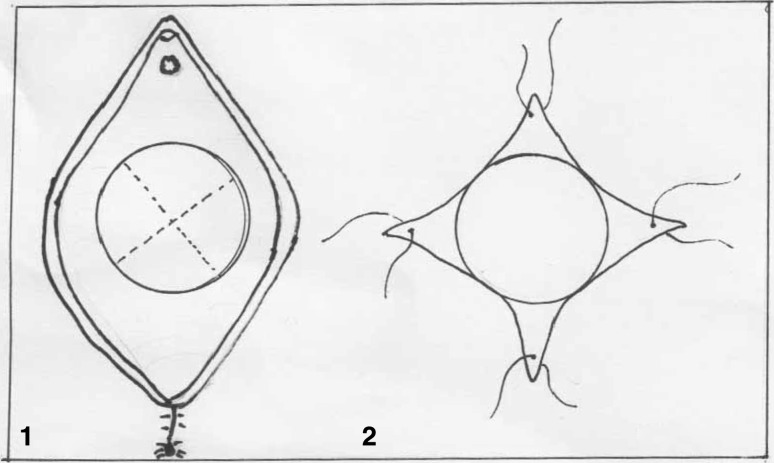
Saline Adrenaline (1:150000) infiltration was done, a cruciate incision is made on the lower/distal surface of the septum after proper marking. Four triangular flaps are dissected and held in position by stay sutures. The flaps are dissected up to lateral vaginal wall. Care is taken while dissecting the flaps to avoid injury to the bladder anteriorly and rectum posteriorly. Some areolar tissue is found in between two layers of vaginal septum, depending on the thickness of the septum (Fig. 1).
Fig. 1.
Cruciate incision on distal layer and creating 4 flaps
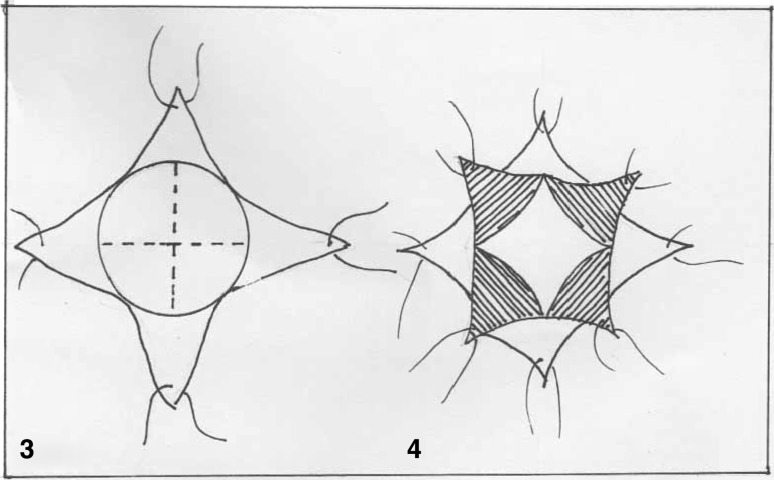
After dissecting the lower layer, the upper layer becomes prominent if the septum is thin in the presence of haematocolpos. But in case it is thick, we have to dissect the areolar tissue till the upper layer becomes visible. It is seen as bluish bulging membrane if there is haematocolpos. Cruciate incision is made on this proximal layer of the septum at right angles to previous incision after proper marking. Four more triangular flaps are created and held with stay sutures (Fig. 2). If there is haematocolpos, it is drained first, and then triangular flaps of two layers are interposed with 3–0 Vicryl. Thus, the suture line is zigzag encircling the vagina. The apex of each flap is in this way joined into the basal intersection of the two flaps (Fig. 3).
Fig. 2.
Cruciate incision on proximal layer at right angles to previous incision on distal flap
Fig. 3.
The apices joined to basal intersection creating zigzag suture line
If the vaginal septum is at high level and thick, then either a labial flap is created on either side to cover the raw area or partial thickness skin graft on mold is kept.
In post operative period, antibiotics are given. Patients were called for follow-up after next menses to ensure the drainage of the menstrual blood and in married women sexual activity was allowed 6 weeks after the procedure.
Results
The crossplasty was performed in 13 patients over a period of 20 years (Table 1).
Table 1.
Agewise distribution of patients
| Age | No.of Pts. |
|---|---|
| 14–16 Yrs. | 9 |
| 20–22 Yrs. | 4 |
There were nine patients who presented at peripubertal age, and four patients were between 20 and 22 years.
Out of nine patients of pubertal age—eight presented as primary amenorrhoea with lower abdominal pain, lump in abdomen and bladder or bowel symptoms. Two of the pubertal age group patients presented with H/O previous drainage of haematocolpos and with recurrence of symptoms. Previous drainage of haematocolpos was done by simple cruciate incision, which resulted into restenosis and closure of the opening leading to haematocolpos (Table 2).
Table 2.
Presenting Symptoms
| Presenting symptoms | No.of Pts. |
|---|---|
| Primary amenorrhoea with lower abdominal pain | 8 |
| H/O previous drainage of haematocolpos and recurrence of symptoms | 2 |
| Infertility and dysparemia | 3 |
Three patients who presented as primary infertility/dyspareunia were detected to be having blind pouch of vagina and normal pelvic findings on USG. All these three patients were called during menses to see for the vaginal opening through which menstrual blood was draining. It was found to be very small/pinpoint opening and usually patients had prolonged menstrual flow because of slow drainage.
Majority of the patients in our series of 13 cases had low vaginal septum, while three patients had middle vaginal and one had high vaginal septum. It is very essential to ascertain the level of the septum. Low- and Mid-level transverse vagina septae can be managed by gynecologist, but for high-level transverse vaginal septum help of plastic surgeon is required (Table 3).
Table 3.
Level of the transverse vaginal septum
| Site of vaginal septum | No.of Pts. |
|---|---|
| Low-level septum | 9 |
| Middle-level septum | 3 |
| High vaginal septum | 1 |
Thickness of the vaginal septum is measured by transvaginal or transperineal USG. Measurement of septum thickness preoperatively helps to plan the surgical technique (Table 4).
Table 4.
Thickness of vaginal septum
| Thickness of septum | No.of Pts. |
|---|---|
| 1–3 Cm | 12 |
| >3 Cm | 1 |
12 patients had vaginal septum <3 cm while one patient, with high vaginal septum, had thickness of 4 cm.
No intraoperative problems are expected if thickness of the vaginal septum is 3 cm or less while thicker septum >3 cm may require either a partial skin graft or labial flaps to cover large raw area.
Transverse vaginal septum with haematocolpos is easier to manage as the distended vagina causes pressure on the septum from above and it appears to be thinner and it is easy to mobilize the vaginal flaps from distended upper vagina.
In our series of 13 patients only one patient with high vaginal septum needed bilateral labial flaps along with vaginal flaps to cover the raw area.
Post Operative Follow-up
All 13 patients were followed for a period of 6 months–2 years. Speculum examination was done at each follow-up visit. None of the 13 patients had vaginal restenosis and recurrence of haematocalpos. All patients had capacious vagina post operatively. Three patients subsequently conceived and two of them had normal vaginal delivery, while one had to undergo LSCS for obstetric indication.
Discussion
The incomplete vertical fusion results in a transverse vaginal septum that varies in thickness and can be located at almost any level in the vagina. The incidence varies from 1:2100 to 1:72,000.
The conventional technique of treating transverse vaginal septum consists of excision of the septum and anastomoses of upper and lower vagina with interrupted sutures. This technique may cause shortening of vagina and some times may end up causing restenosis in most of the cases.
Garcia described "Z" Plasty in 1967, but his technique is considered to be complicated, hence not being practiced. In our experience, the technique of crossplasty/Z plasty (is little modification of Garcias technique) that is being practiced by plastic surgeons to tackle unyielding surgical scars is very effective in tackling transverse vaginal septum at various levels and of varying thickness.
It is very important to correctly diagnose/differentiate between imperforate hymen and transverse vaginal septum, as presentation is very similar at peripubertal age, i.e., cryptomenorrhea. In our experience, imperforate hymen with haematocolpos will manifest as bluish bulging membrane with haematocolpos (because hymen is very thin) while transverse vaginal septum will be bulging septum with normal looking vaginal mucous membrane even with large haematocolpos behind.
This difference in appearance is due to thickness of the vaginal septum. If not correctly diagnosed, a simple cruciate incision on transverse vaginal septum to drain haematocolpos may result in subsequent closure of the opening, restenosis and recurrence of haematocolpos as it occured is two of our cases.
It is easier to tackle transverse vaginal septum with thickness less than 3 cm and at low or middle level. It is easier to do cross plasty in the presence of haematocolpos as septum apparently appears thinner and is at lower level because of the pressure of haematocolpos. In case thickness of septum is more and it is at high level, then preoperative serial passive dilatation of the vagina is done after decompression of the haematocolpos by No 12 gauge needle followed by endometrial suppression by OCS [4]. This will maximize surgical resection and anastomosis in thick high vaginal septum.
In case the septum is at high or middle level without haematocolpos, during surgery an opening can be made in the center of the septum and Foleys catheter pushed in and the balloon is distended [5]. Traction on the catheter will make the access to the upper layer of vaginal septum easier.
For high vaginal septum concurrent laparotomy may be needed and abdominal surgeon will guide the vaginal surgeon with uterine sound pushed through Cx from above to identify the septum and this may prevent injury to bladder or bowel [5].
Pregnancy success is more likely to occur following treatment of imperforate hymen than transverse vaginal septum [6]. Because the interval between onset of symptoms, diagnosis, and treatment was longer in patients with transverse vaginal septum. Early diagnosis with removal of accumulated blood could influence pregnancy success, reducing the risk of hematocolpos, hematometra, hematosalpinx, and the subsequent development of pelvic endometriosis.
Conclusion
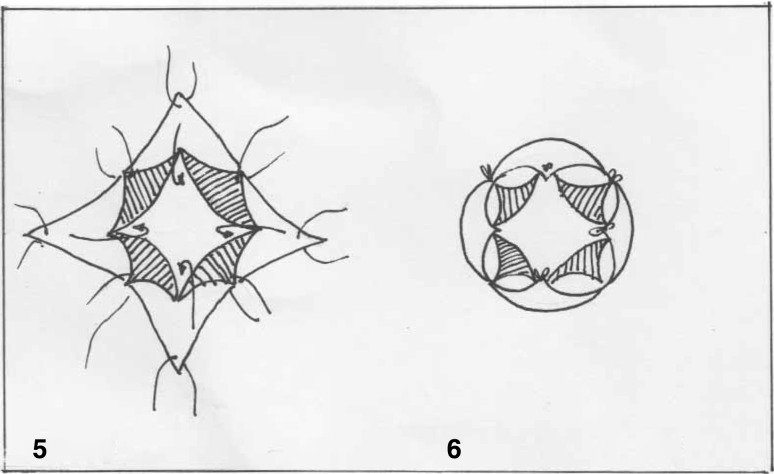
Following double cross plasty in transverse vaginal septum, the suture line is in continuous “W “pattern and hence narrowing of the vagina does not occur at suture line after healing. It results in capacious vagina even for future reproduction.
The technique of crossplasty is simple and can be adopted by Gynecologist for management of low- and middle-level transverse vaginal septae.
Acknowledgments
Compliance with ethical requirements and Conflicts of interests
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5). Informed consent was obtained from all patients for the surgery. An ethical clearance has also been taken from the institutional ethical committee. The authors of the article Dr Suman Pradeep Sardesai, Dr Raju Dabade, Dr Vinayak Chitale declare that they have no conflicts of interest.
Dr. Suman Pradeep Sardesai
graduated from Topiwala National Medical College & Nair Hospital Mumbai and did post-graduation in OBST & GYN at Nowrosjee Wadia Hospital & Seth G.S. Medical College, Mumbai in 1975. She joined Dr. Vaishampayan Govt. Medical College, Solapur, Maharashtra, and pursued her teaching career for 32 years. She has many original research projects to her credit. She was the first runner-up of “FOGSI CORION AWARD” for her research paper “Low dose MgSo4 Regime for Pre clampesia and eclampsia” in 1998 at AICOG, Hyderabad (AP). She received FOGSI CORION AWARD for her original research on “Tobacco Handling in Pregnant Bidi Workers: As Hazardous as smoking 25 cigarettes per day” in 1999 at AICOG, Lucknow (UP). She also presented poster on various conservative surgeries for prolapse at FIGO held at Washington. Her other subjects of interest are conservative surgical procedure for genital prolapse, reversal of sterilization, and surgery for genital malignancies.
References
- 1.Chitale VR, Sardesai SP, et al. The double crossplasty: a new technique for transverse vaginal septum. J Obstet Gynecol India. 1996;46(6):859–861. [Google Scholar]
- 2.John AR, Lesley LB. Surgery for anomalies of the mullerian ducts; Te Linde’s Operative Gynecology. 10. New York: Wolters Kluwer; 2010. p. 539. [Google Scholar]
- 3.Fayez GS, Ramez S, Zoury A. Transverse vaginal septum : a clinicopathologic. Eval Obstet Gynecol. 1979;54(3):278–283. [PubMed] [Google Scholar]
- 4.Bradley SH, John AR. Preoperative dilatation to facilitate repair of the high transverse vaginal septum. Fertil & Steril. 1992;57(6):1351–1353. doi: 10.1016/s0015-0282(16)55102-4. [DOI] [PubMed] [Google Scholar]
- 5.Franz W, Klaus B, Babetta S, et al. ‘Z’ plasty of the transverse vaginal septum using Garcia’s procedure and the Grunberger modification. Fertil Steril. 2003;79(3):608–612. doi: 10.1016/S0015-0282(02)04803-3. [DOI] [PubMed] [Google Scholar]
- 6.John AR, Howard AZ, et al. Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet Gynecol. 1982;59:448–451. [PubMed] [Google Scholar]