Abstract
Introduction
Parenteral lipid emulsions (LEs) are commonly rich in long-chain triglycerides (LCT) derived from soybean oil (SO). SO containing emulsions may promote systemic inflammation and therefore may adversely affect clinical outcomes. We hypothesized that alternative oil-based LEs (SO-sparing strategies) may improve clinical outcomes in critically ill adult patients compared to SO emulsion only products. The purpose of this systematic review was to evaluate the effect of parenteral SO-sparing strategies on clinical outcomes in intensive care unit (ICU) patients.
Methods
We searched computerized databases from 1980 to 2013. We included randomized controlled trials (RCTs) conducted in critically ill adult patients that evaluated SO-sparing strategies versus SO-based LEs in the context of parenteral nutrition (PN).
Results
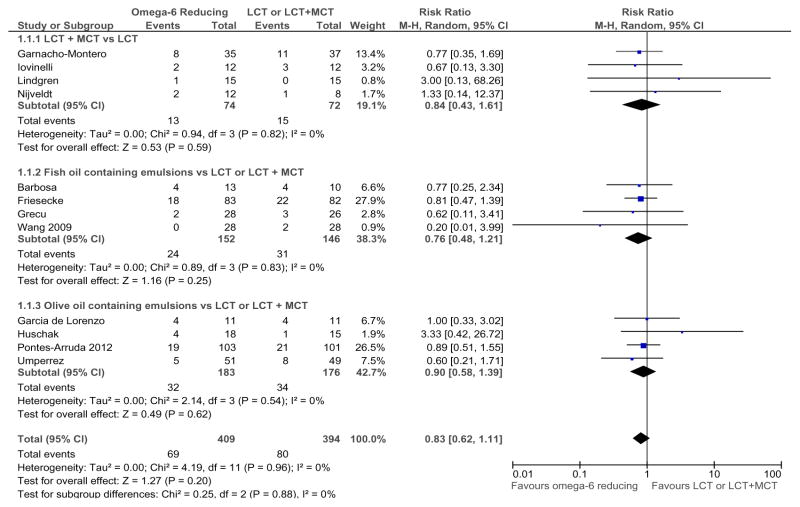
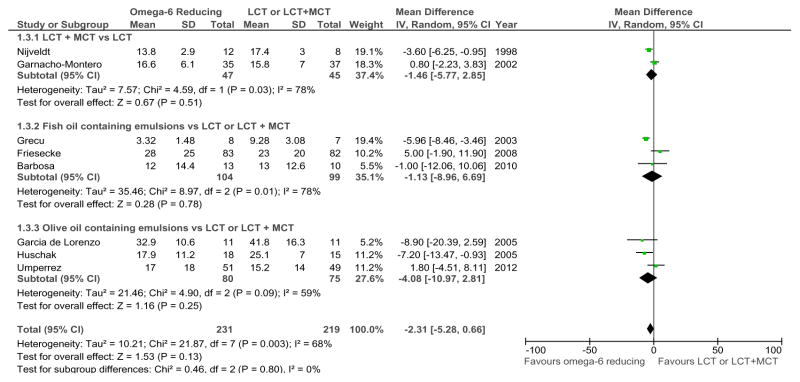
A total of 12 RCTs met inclusion criteria. When the results of these RCTs that were statistically aggregated, SO-sparing strategies were associated with clinically important reductions in mortality (risk ratio RR= 0.83, 95% confidence intervals CI 0.62, 1.11, P = 0.20), in duration of ventilation (weighted mean difference, WMD −2.57, 95% CI −5.51, 0.37, P= 0.09), and in ICU length of stay (WMD −2.31, 95% CI −5.28, 0.66, P= 0.13) but none of these differences were statistically significant. SO-sparing strategies had no effect on infectious complications (RR=1.13, 95% CI 0.87, 1.46, P=0.35).
Conclusion
Alternative oil-based LEs may be associated with clinically important reductions in mortality, duration of ventilation, and ICU LOS but lack of statistical precision precludes any clinical recommendations at this time. Further research is warranted to confirm these potential positive treatment effects.
Keywords: alternative lipid emulsions, soybean oil reducing strategies, critically ill
Introduction
Lipid emulsions (LEs) are an essential constituent of parenteral nutrition (PN) [1] and are considered an important source of energy, essential fatty acids (FA) and vitamins E and K [2,3,4]. However, the current literature suggests that soy-bean oil (SO) and safflower-based LEs which are rich in the ω−6 fatty acid linoleic acid, might promote production of pro-inflammatory prostanoids and leukotrienes resulting in increased oxidative stress and systemic inflammation[5,6] and may be associated with worse clinical outcomes [7].
Over the past three decades, different generations of alternative oil-based LEs have been developed, which could have less proinflammatory effects, less immune suppression, and more antioxidant effects than the standard SO-based LEs [8,9]. These SO-sparing strategies consist of different formulations of SO combined with medium-chain triglycerides (MCTs), olive oil (OO) which contains the ω-9 monounsaturated FA (MUFA) oleic acid, and fish oil (FO) which contains ω-3 FA eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). The purpose of the current study was to provide an up-to-date systematic review and meta-analysis of all randomized clinical trials (RCTs) of alternative oil-based LEs, compared to SO emulsion products evaluating clinically relevant outcomes in the critically ill.
Methods
Study Identification
We conducted a systematic review of the published literature to identify all relevant clinical trials using a strategy found in Appendix 1. We included studies if they met all the following eligibility criteria:
Study design: randomized controlled trials (RCTs).
Population: critically ill adult patients (>18 years old).
Intervention: parenteral strategies to reduce the overall load of ω-6 FA (alternative ω6-sparing LEs) versus ω6 oil-based LEs (LCT in the control group).
Study outcomes: mortality was the primary outcome for this meta-analysis. Secondary outcomes were: intensive care unit (ICU) and hospital LOS, infections, and mechanical ventilation (MV) days. We excluded the clinical studies that reported only biochemical, metabolic, immunologic or nutritional outcomes. Critically ill patients were defined as patients admitted to an ICU who had an urgent or life-threatening complication (high baseline mortality rate ≥5%) to distinguish them from patients with elective surgery who are also cared for in some ICUs but have a low baseline mortality rate (<5%).
Data Extraction and Risk of Bias Assessment
Two reviewers independently extracted data using a data abstraction form with a scoring system [10]. We scored the methodological quality of individual trials according to key methodological features outlined in the Appendix 2. Disagreement was resolved by consensus between both reviewers. We attempted to contact the authors of included trials and requested missing or unclear information. We designated as a level 1 study if all of the following criteria are fulfilled: concealed randomization, blinded outcome adjudication and an intention to treat analysis. A study was considered as level 2 study if any one of the above characteristics was unfulfilled.
Data synthesis
The primary outcome of the systematic review was overall mortality. From all trials, we combined hospital mortality where reported. If hospital mortality was not reported, we used ICU mortality or 28-day mortality. Secondary outcomes included infections, MV days, and ICU LOS. We used definitions of infections as defined by the authors in their original papers. We analyzed data using RevMan 5.1 [11] with a random effect model. We calculated pooled relative risks using the Mantel-Haenszel estimator for dichotomous outcomes and weighted mean differences (WMDs) were estimated by the inverse variance approach for continuous outcomes, with associated 95% CIs. The random effects model of DerSimonian and Laird was used to estimate variances for the Mantel-Haenszel and inverse variance estimators [12]. The possibility of publication bias was assessed by generating funnel plots and testing asymmetry of outcomes using methods proposed by Rucker and colleagues [13]. Statistical heterogeneity was assessed by the I2 statistic. We considered P< 0.05 to be statistically significant and P< 0.20 as indicator of trend.
A priori hypotheses testing
Given the different ω-6 FA sparing strategies and the heterogeneity of trial design, we performed pre-specified, hypothesis-generating subgroup analyses to attempt to elucidate potentially more beneficial treatment strategies. We compared the results of trials that provided a) LCTs plus MCT to a LCT emulsion; b) ω-3 oil-based LEs to a LCT or LCT/MCT mixture, and c) ω-9 oil-based LEs to a LCT or LCT + MCT mixture.
Results
Study identification and selection
A total of 52 potentially eligible RCTs were identified. Of these, we excluded 40 trials due to the following reasons: 22 trials [14,15,16,17,18,19,20,21,22,23,24,25,26,27, 28,29,30,31,32,33,34,35] trials did not include ICU patients (mostly elective surgery and cancer patients), 12 trials [36,37,38,39,40,41,42,43,44,45,46,47] did not evaluate clinically important outcomes; 2 trials [48,49] did not include SO-based LE in the control group; 1 trial [50] compared LCT vs. another LCT emulsion without reduction in SO; 1 trial [51] was conducted in a pediatric population; 1 trial[52] had a short duration of intervention (12 hour of lipid emulsion infusion during the first day); 1 trial included patients with poisoning and not representative of ICU patients[53]. In the end, 12 RCTs [54,55,56,57,58,59,60,61,62,63,64,65] enrolling a total of 806 patients met the inclusion criteria and were included in this systematic review (see Table 1 and 2). The authors reached 100% agreement for inclusion of relevant trials in this review. The mean methodological score of all trials was 9.8 (6 to 14). Randomization was concealed in 8/12 (67 %) trials, ITT analysis was performed in 11/12 (92 %) trials and 8/12 (67 %) trials were double blinded. There were 5 level 1 studies and 7 level 2 studies.
Table 1.
Randomized clinical trial evaluating type of lipids (PN) in critically ill patients
| Study | Population | Methods (score) | Intervention | Mortality # (%)† | Infections # (%)‡ | ||
|---|---|---|---|---|---|---|---|
| Long Chain Triglyceride (LCT) plus Medium Chain Triglycerides (MCT) vs. LCT | |||||||
| Nijveldt 1998 | ICU, septic surgical patients, trauma N = 20 |
C. Random: not sure ITT: yes Blinding: double (10) |
PN + Lipofundin (50% LCT+ 50% MCT) vs. PN + Intralipid (100% LCT, soybean) |
LCT + MCT ICU 2/12 (17) |
LCT ICU 1/8 (13) |
LCT + MCT NR |
LCT NR |
| Lindgren 2001 | ICU patients, sepsis, multitrauma N = 30 |
C. Random: yes ITT: yes Blinding: yes (12) |
PN + Structolipid (64% LCT + 36% MCT) vs. PN + Intralipid (100% LCT, soybean) |
LCT + MCT 1/15 (7) |
LCT 0/15 (0) |
LCT + MCT 6/15 (40) |
LCT 4/15 (27) |
| Garnacho-Montero. 2002 | Surgical ICU Patients with peritonitis and abdominal sepsis N = 72 |
C. Random: not sure ITT: no Blinding: no (6) |
PN + Lipofundin (50% LCT + 50% MCT) vs. PN with Intralipid (100% LCT, soybean) Both groups received PN with 45 % Branched chain amino acids |
LCT + MCT ICU 8/35 (23) Hospital 11/35 (31) |
LCT ICU 11/37 (30) Hospital 13/37 (35) |
LCT + MCT NR |
LCT NR |
| Iovinelli 2007 | Patients with COPD requiring ventilation N = 24 |
CRandom: yes ITT: yes Blinding: no (7) |
PN + Lipofundin (50% LCT + 50% MCT) vs. 100% LCT (100% LCT, soybean). In both received 50% of non-protein calories given as lipids |
LCT + MCT ICU 2/12 (17) |
LCT ICU 3/12 (25) |
LCT + MCT Catheter- related 1/12 (8) |
LCT Catheter-related 2/12 (17) |
| Fish oil (ω 3) containing emulsions in PN fed patients vs. LCT or LCT+MCT | |||||||
| Grecu 2003 | Patients with abdominal sepsis N = 54 (15/54 in ICU) |
C. Random: yes ITT: yes Blinding: double (12) |
PN + Omegaven (10% fish oils) plus LCTs vs. PN with LCT |
Omegaven + LCT ICU 2/28 (7) |
LCT ICU 3/26 (12) |
Omegaven VAP 0/8* |
LCT VAP 1/7* (14) |
| Friesecke 2008 | Medical ICU patients N= 166 |
CRandom: yes ITT: yes Blinding: double (10) |
PN + Lipofundin MCT (50% LCT + 50% MCT) + Omegaven (10% fish oil) vs. Lipofundin MCT (50% LCT + 50% MCT) |
LCT + MCT + FO 28 day 18/83 (22) |
LCT+MCT 28 day 22/82 (27) |
LCT+ MCT+ FO 10/83 (12) |
LCT + MCT 11/82 (13) |
| Wang 2009 | Severe acute pancreatitis patients in ICU N = 56 |
C. Random: no ITT: yes Blinding: double (11) |
PN + Omegaven (10% fish oils) plus Lipovenos (LCTs, soybean oil) (ω3:ω6 ratio was 1:4) vs. PN with Lipovenos (LCTs, soybean oil). Both received same amounts of lipids (1 gm/kg/day) |
Omegaven ICU 0/28 (0) |
LCT ICU 2/28 (7) |
Omegaven 6/28 (21) |
LCT 9/28 (32) |
| Barbosa 2010 | ICU patients with SIRS or sepsis requiring PN N=25 |
CRandom: yes ITT: yes Blinding: single (10) |
PN + Lipoplus (50% MCT, 40% LCTs soybean oil, 10% FOl) vs. Nutriflex LipidSpecial (50% MCT, 50% LCT, soybean oil). Both received same amounts of lipids (~1 gm/kg/day) |
MCT+LCT+FO 5 day 2/13 (15) 28 day 4/13 (31) |
MCT+LCT 5 day 1/10 (10) 28 day 4/10 (40) |
MCT+LCT+FO NA |
MCT+LCT NA |
| Olive oil containing emulsions vs. LCT or LCT+MCT | |||||||
| Garcia-de-Lorenzo 2005 | Severe burn patients, burn severity index ≥7, TBSA > 30 % N = 22 |
C. Random: not sure ITT: yes Blinding: double (10) |
PN with ClinOleic 20% (80% olive oil, 20% soybean oil, (63% ω9, 37% ω6= restricted linoleic acid {ω6} content) vs. Lipofundin (50% LCT+ 50% MCT). |
Clinoleic ICU 4/11 (36) |
Lipofundin ICU 4/11 (36) |
Clinoleic 6/11 (55) |
Lipofundin 6/11 (55) |
| Huschak 2005** | ICU trauma patients N = 33 |
CRandom: yes ITT: yes Blinding: None (7) |
PN high fat (lipid:glucose 75:25) + Clinoleic (80% olive oil, 20% soybean oil) + EN Glucerrna (lipid:glucose 60:40) vs. PN high carbohydrate (lipid: glucose 37:63) + Lipofundin (50% LCT + 50% MCT) + EN Fresubin HP Energy (lipid:glucose 44:56) |
High fat + Clinoleic ICU 4/18 (22) |
Low fat + LCT + MCT ICU 1/15 (7) |
High fat + Clinoleic Low fat +LCT+MCT Data Not reported. |
|
| Umperrez 2012 | Medical surgical ICU pts post op (88% emergency surgeries) N =100 |
C. Random: yes ITT: yes Blinding: double (14) |
PN with ClinOleic 20% (80% olive oil, 20% soybean oil, ω6:ω3=9:1) vs. Intralipid (100% soybean oil, ω6:ω3=7:1) |
Clinoleic Hospital 5/51 (10) |
Intralipid Hospital 8/49 (16) |
Clinoleic 29/51 (57) |
Intralipid 21/49 (43) |
| Pneumonia | |||||||
| 7/51 (14) | 5/49 (10) | ||||||
| Pontes-Arruda 2012 | ICU pts requiring PN from 8 ICUs and 3 countries N=204 |
C. Random: yes ITT: yes Blinding: no (9) |
PN with ClinOleic (n=103) vs PN with a MCT/LCT based IVLE (n=101) |
ClinOleic ICU 19/103 (24) 28-day 24/103 (27) |
MCT/LCT ICU 21/101 (21) 28-day 26/101 (26) |
ClinOleic | MCT/LCT |
| All infections | |||||||
| 39/103 (38) | 35/101 (35) | ||||||
| ICU acquired infections | |||||||
| 28/103 (27) | 23/101 (23) | ||||||
| VAP/lower respiratory infections | |||||||
| 9/103 (9) | 11/101 (11) | ||||||
Abbreviations: ARDS: acute respiratory distress syndrome; C. Random: concealed randomization; DHA: docosahexaenoic acid; EN: enteral nutrition; EPA: eicosapentaenoic acid; C. Random: concealed randomization; EN: enteral nutrition; FO: fish oil; ICU: intensive care unit; ITT: intention to treat; IV: intravenous; LCT: long chain triglycerides; MCT: medium chain triglycerides; N: number of patients; NA: non attribuible; NR: non referred; PN: parenteral nutrition; SIRS: systemic inflammatory response syndrome; VAP: ventilator associated pneumonia; ω-3: omega 3; ω-6: omega 6; ω-9: omega 9.
hospital mortality unless specified;
number of patients with infections unless specified;
data obtained from author, 8 out of 28 in Omegaven and 7 out of 26 in LCT group were in ICU;
intervention includes high fat low carbohydrates PN plus fish oil;
converted Standard Error Mean (SEM) to Standard deviation (SD)
Table 2.
Outcomes of included trials on omega 6 reducing strategies lipid emulsions
| Study | LOS days | Ventilator days | Other | |||
|---|---|---|---|---|---|---|
| Long Chain Triglyceride (LCT) plus Medium Chain Triglycerides (MCT) vs. LCT | ||||||
| Nijveldt 1998 |
LCT + MCT 13.8 ± 2.9 (12) |
LCT 17.4 ± 3.0 (8) |
LCT + MCT NR |
LCT NR |
NR | |
| Lindgren 2001 |
LCT + MCT NR |
LCT NR |
LCT + MCT NR |
LCT NR |
LCT + MCT | LCT |
| Adverse effects | ||||||
| 5/15 (33) | 4/15 (27) | |||||
| Nitrogen balance at day 3 | ||||||
| 2.6 ± 5.6 gms | −11.7 ± 4.8 gms | |||||
| Garnacho-Montero 2002 |
LCT + MCT ICU 16.6 ± 6.1 (35) |
LCT ICU 15.8 ± 7 (37) |
LCT + MCT NR |
LCT NR |
LCT + MCT | LCT |
| Retinol binding protein | ||||||
| 1.7 ± 1 | 0.8 ± 0.6 | |||||
| Nitrogen balance | ||||||
| 14.2 ± 2.9 | 11.6 ± 4 | |||||
| Iovinelli 2007 |
LCT + MCT NR |
LCT NR |
LCT + MCT 10.6 ± 3.0 (12) |
LCT 13.4 ± 3.5 (12) |
LCT + MCT | LCT |
| Time before weaning | ||||||
| 52 ± 36 hrs | 127 ± 73 hrs | |||||
| Fish oil (ω 3) containing emulsions in PN fed patients vs. LCT or LCT+MCT | ||||||
| Grecu 2003* |
Omegaven ICU 3.32 ± 1.48 (8) Hospital 11.68 ± 2.04 (28) |
LCT ICU 9.28 ± 3.08 (7) Hospital 20.46 ± 3.27 (26) |
Omegaven 2.83 ± 1.62 (8) |
LCT 5.23 ± 2.80 (7) |
Omegaven | LCT |
| Patients undergoing reoperation for septic episode | ||||||
| 2/28 (7) | 8/26 (31) | |||||
| Friesecke 2008 |
FO ICU 28 ± 25 (83) |
LCT ICU 23 ± 20 (82) |
LCT + MCT + FO 22.8 ± 22.9 (83) |
LCT+MCT 20.5 ± 19.0 (82) |
LCT + MCT + FO | LCT+MCT |
| Urinary Tract Infections | ||||||
| 6/83 (7) | 4/82 (5) | |||||
| Catheter-related infections | ||||||
| 1/83 (1) | 3/83 (4) | |||||
| Total EN Energy Intake (kcal/kg) | ||||||
| 22.2 ± 5.5 | 21.6 ± 5.6 | |||||
| Wang 2009 | NA | NA | NA | NA | Omegaven | LCT |
| Surgery of infected pancreatic necrosis | ||||||
| 3/28 (11) | 6/28 (21) | |||||
| Barbosa 2010 |
MCT+LCT+FO ICU 12 ± 14.4a (13) Hospital 22 ± 25.2 a (13) |
MCT+LCT ICU 13 ± 12.6 a (10) Hospital 55 ± 50 a.6 (10) |
MCT+LCT+FO 10 ± 14.4 (13) |
MCT+LCT 11 ± 12.64 (10) |
MCT+LCT+ FO 2057± 418 kcals |
MCT+LCT 1857 ± 255 kcals |
| Olive oil containing emulsions vs. LCT or LCT+MCT | ||||||
| Garcia-de-Lorenzo 2005 |
Clinoleic ICU 32.9 ± 10.6a (11) Hospital 57 ± 15.3a (11) |
Lipofundin ICU 41.8 ± 16.3a (11) Hospital 64.9 ± 27.2a (11) |
Clinoleic 11.0 ± 11.93a (11) |
Lipofundin 13.0 ± 16.25a (11) |
Clinoleic | Lipofundin |
| Multiple organ dysfunction score | ||||||
| 11.0 ± 3.6 | 13.0 ± 4.9 | |||||
| Huschak 2005** |
High fat + Clinoleic ICU 17.9 ± 11.2 (18) |
Low fat + LCT+MCT ICU 25.1 ± 7.0 (15) |
High fat + Clinoleic 13.0 ± 8.9 (18) |
Low fat + LCT+MCT 20.4 ± 7.0 (15) |
High fat + Clinoleic | Low fat + LCT + MCT |
| Total Energy Intake (kcal/kg) | ||||||
| 17.9 ± 6.3 | 22.3 ± 4.2 | |||||
| Umperrez 2012 |
Clinoleic ICU 17 ± 18 (51) Hospital 40.8 ± 36 (51) |
Intralipid ICU 15.2 ± 14 (49) Hospital 46.7 ± 48 (51) |
Clinoleic NR |
Intralipid NR |
Clinoleic | Intralipid |
| Total Energy Intake (kcal/kg) | ||||||
| 22 ± 6 | 22 ±5 | |||||
| Pontes-Arruda 2013 |
Clinoleic ICU 12 (7–17) Hospital 21 (15–25) |
MCT/LCT ICU 11 (5–14) Hospital 18 (13–23) |
NA | NA | Clinoleic | MCT/LCT |
| Nutritional Intake | ||||||
| Lipids (g/day) | ||||||
| 66 (61–73) | 61 (54–67) | |||||
| Days on PN | ||||||
| 12 (8–15) | 11 (7–15) | |||||
| Dextrose (g/day) | ||||||
| 288 (275–303) | 281 (273–301) | |||||
| AAs (g/day) | ||||||
| 87 (84–90) | 87 (83–92) | |||||
Abbreviations: EN: enteral nutrition; FO: fish oil; ICU: intensive care unit; LCT: long chain triglycerides; LOS: length of stay; MCT: medium chain triglycerides; NA: non attribuible; NR: not reported; PN: parenteral nutrition;
hospital mortality unless specified;
number of patients with infections unless specified;
data obtained from author, 8 out of 28 in Omegaven and 7 out of 26 in LCT group were in ICU;
intervention includes high fat low carbohydrates PN plus fish oil;
converted Standard Error Mean (SEM) to Standard deviation (SD)
Meta-Analysis of Primary Outcome
When the results of 12 RCTs [54–65] that evaluated mortality were statistically aggregated, ω-6-sparing strategies were associated with a reduction in mortality that was not statistically significant (risk ratio [RR]= 0.83, 95 % confidence intervals [CI] 0.62, 1.11, P= 0.20, heterogeneity I2 =0% see Figure 1).
Figure 1.
Overall effect on Mortality of LCT (Omega-6 reducing strategy) vs. LCT
Abbreviations: LCT: long chain triglycerides; MCT: medium chain triglycerides; 95% CI: 95% confidence intervals
Secondary Outcomes
Compared to LCT, when the RCTs reporting ventilator days were aggregated [58,60,61,62,64], overall ω-6 FA-sparing strategies were consistent with a -reduction in duration of MV but differences were not statistically significant (WMD −2.57, 95% CI −5.51, 0.37, P=0.09, heterogeneity I2=25%) (Figure 2). There was a trend towards a reduction in ICU LOS associated with the use of ω-6-sparing strategies when compared to LCT [54,56,58,59,60,61,62,64] (WMD −2.31, 95% CI −5.28, 0.66, P=0.13, I2=68%, P< 0.003) (Figure 3). When the data from 5 RCTs [58,60,62,63,65] that reported ICU-acquired infections were aggregated, ω-6-sparing strategy had no effect (RR= 1.13, 95% CI 0.87, 1.46, P=0.35, heterogeneity I2=0%).
Figure 2.
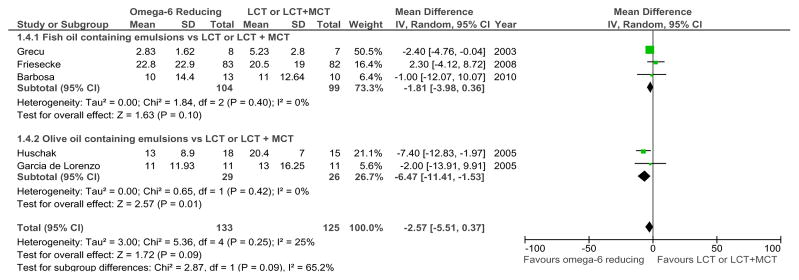
Overall effect on ventilation days of Omega 6 reducing strategy vs. LCT
Abbreviations: LCT: long chain triglycerides; 95% CI: 95% confidence intervals; SD: standard deviation
Figure 3.
Overall effect on ICU LOS of Omega 6 reducing strategy vs. LCT
Abbreviations: LCT: long chain triglycerides; MCT: medium chain triglycerides; 95% CI: 95% confidence intervals; SD: standard deviation
Subgroup analysis
LCTs plus MCT versus LCT emulsion
Four RCTs [54–57] compared LCTs plus MCT to a LCT emulsion. When statistically aggregated, these studies showed no difference in mortality (RR= 0.84, 95 % CI 0.43, 1.61, P=0.59, heterogeneity I2=0%) (Figure 1). Only one trial [57] compared LCT+MCT to LCT that reported duration of ventilation and no significant differences were seen between the two groups. When the data from the two trials [54,56] that report ICU LOS were aggregated, there were no differences in ICU LOS (WMD −1.46, 95 % CI −5.77, 2.85, P= 0.51, heterogeneity was present I2= 78%, P=0.03) (Figure 3).
Fish oil containing emulsions vs. LCT or LCT +MCT
Four RCTs [61–64] comparing ω-3 oil-based LEs to a LCT or LCT+MCT reported mortality. When these data were aggregated, this strategy was not associated with a reduction in mortality (RR= 0.76, 95% CI 0.48, 1.21, P = 0.25 heterogeneity I2=0%) (Figure 1). We found a trend towards a reduction in the duration of mechanical ventilation (WMD −1.81, 95% CI −3.98, 0.36, P= 0.10, heterogeneity I2=0%) (Figure 2). There were no differences between the groups in ICU LOS (WMD −1.13, 95% CI −8.96, 6.69, P = 0.78; heterogeneity I2= 78%, P= 0.01) (Figure 3) and infections (RR= 0.79, 95% CI 0.43, 1.43, P = 0.43, heterogeneity I2= 0%).
ω9 oil-based LEs versus a LCT + MCT mixture
Four RCTs [58,59,64,65] compared a ω-9 oil-based LE to a LCT + MCT mixture. We did not find any difference between the groups in mortality (RR= 0.90, 95% CI 0.58, 1.39, P=0.62, heterogeneity I2= 0%) (Figure 1), however we found a significant reduction in the duration of MV (WMD −6.47, 95% CI −11.41, −1.53, P= 0.01, heterogeneity I2=0%) (Figure 2) but no effect on ICU LOS (WMD −4.08, 95 % CI −10.97, 2.81, P=0.25, heterogeneity I2=59%) (Figure 3). When 3 RCTs [58,60,65] that reported on ICU-acquired infections were aggregated, this strategy showed a tendency towards an increase in infections (RR= 1.23, 95% CI 0.92, 1.63, P= 0.16, heterogeneity I2=0%).
Risk of publication bias
There was no indication that publication bias influenced the observed aggregated results. Funnel plots were created for each study outcome (data not shown) and the tests of asymmetry were not significant for any outcome measure (mortality, P= 0.48; ICU LOS, P= 0.88, and mechanical ventilation days P= 0.78).
Discussion
Our systematic review and meta-analysis is the first in evaluating the overall effects of parenteral ω-6 reducing strategies in the critically ill. When 12 eligible trials were statistically aggregated, we did not find statistically significant effects. However, the magnitude of the potential treatment effect, in terms of a reduction in mortality (relative risk reduction 17%) and reduction in ICU LOS (more than 2 days less), if realized, would be consistent with a large and clinically and economically important difference. The lack of statistical precision is likely due to the small number of studies and the small sample size of each study. Given the heterogeneous population of ICU patients included in this systematic review (sepsis, severe sepsis/septic shock, surgery, trauma, burns, and SIRS), the conclusions of our systematic review could be applied to a broad group of ICU patients. However, given the heterogeneity of alternative LEs, we explored several subgroups to evaluate if the treatment effect was different across different commercial preparations. There are no head-to-head comparisons of these different alternative LEs strategies. Indirectly, by examining the risk ratios of the different alternatives, there does not appear to be any difference in the treatment effects. Therefore, we are unable to define the best ω-6 sparing strategy in the critically ill as available evidence on the differential effects of LEs in ICU patients remains limited after our meta-analysis.
The anti-inflammatory properties of EPA and DHA have been described and exhaustively studied in different experimental and clinical studies [66,67]. Two RCTs included in our systematic review found a significant reduction of the proinflammatory cytokine interleukin 6 and an increase in the HLA-DR expression. However, we were unable to demonstrate any significant effect with FO based LEs rich in EPA and DHA. Recently, two meta-analyses on parenteral FO have been published. Pradelli et al [68] demonstrated that parenteral FO enriched LE were associated with a statistically and clinically significant reduction in infections (P= 0.002) and the LOS, both in the ICU (P= 0.005) and in hospital (P= 0.0005) [68]. Nonetheless, these results cannot be compared with our findings because our meta-analysis included only RCTs evaluating clinical outcomes in the critically ill and excluded RCTs performed in non ICU surgical patients.
More recently, Palmer et al [69] concluded that parenteral FO does not improve mortality, infectious complications, and ICU LOS in comparison with standard PN. These results are similar to our findings. However, we found a tendency toward a reduction in mechanical ventilation days. We believe that this difference was largely due to the difference in the papers included in the different reviews. In fact, Palmer et al [69] have included two papers published by Wang et al in 2008 [28] and 2009 [63]. However, we have decided to include the study published in 2009 [63] and exclude the previous study because it did not include ICU patients and did not report on relevant clinical outcomes. In addition, we excluded two unpublished studies by Liderman et al [70] and Ignatenko et al [71], as both are published as abstracts and we have not had any response from the investigators, which was needed to complete our data abstraction form.
The strength of our meta-analysis includes the fact that we used several methods to reduce bias (comprehensive literature search, duplicate data abstraction, specific criteria for searching and analysis) and have focused on clinically important primary outcomes for ICU patients. The major limitation of our meta-analysis was the small number of trials included which resulted in statistical imprecision. Furthermore, the presence of heterogeneity, both clinical and statistical, weakens any inferences we can make from these data.
In spite of these limitations, we have demonstrated that alternative oil-based LEs in the critically ill could be able to reduce overall mortality, shorten ventilation days and ICU LOS. Further research is warranted and should define the best mixture of lipids, target patient population, best timing, and duration of therapy to optimize the effects on underlying systemic inflammation, immune status, and metabolic processes while at the same time achieving an acceptable safety and tolerance profile.
Acknowledgments
Daren Heyland received speaking honorarium and research grants from Fresenius Kabi and Baxter.
Appendix 1
“omega-6 sparing”, “omega-6 reducing”, “alternative fat emulsions”, “fish oil lipid emulsions”, “omega-3”, “omega 9”, “olive oil lipid emulsions”, “medium chain triglycerides (MCT) lipid emulsions”, “randomized,” “blind,” “clinical trial,” “nutritional support”, “parenteral nutrition”, “lipid emulsions”, “critical illness” and “critically ill”.
Appendix 2: Methodological Quality Assessment
We scored the methodological quality of individual trials considering the following key features of high-quality studies: a) extent to which randomization was concealed, b) blinding, c) analysis was based on the intention-to-treat (ITT) principle, d) comparability of groups at baseline, e) extent of follow-up, f) description of treatment protocol and co-interventions, and g) definition of clinical outcomes. Each individual study was scored from 0 to 14.
Footnotes
Competing interests
The other authors declare that they have no competing interests.
Contributor Information
William Manzanares, Email: wmanzanares@adinet.com.uy.
Rupinder Dhaliwal, Email: dhaliwar@KGH.KARI.NET.
Brian Jurewitsch, Email: jurewitschb@smh.ca.
Renee D. Stapleton, Email: renee.stapleton@uvm.edu.
Khursheed N. Jeejeebhoy, Email: khushjeejeebhoy@compuserve.com.
Daren K. Heyland, Email: dkh2@queensu.ca.
References
- 1.Vanek VW, Seidner DL, Allen P, Bistrian B, Collier S, Gura K, Miles JM, Valentine CJ, Kochevar M Novel Nutrient Task Force, Intravenous Fat Emulsions Workgroup; and the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. Position Paper: Clinical role for alternative intravenous fat emulsions. Nutr Clin Pract. 2012;27:150–192. doi: 10.1177/0884533612439896. [DOI] [PubMed] [Google Scholar]
- 2.Vinnars E, Wilmore D. Jonathan Roads Symposium Papers. History of parenteral nutrition. JPEN J Parenter Enteral Nutr. 2003;27:225–231. doi: 10.1177/0148607103027003225. [DOI] [PubMed] [Google Scholar]
- 3.Hippalgaonkar K, Majumdar S, Kansara V. Injectable Lipid Emulsions: advancements, opportunities and challenges. AAPS Pharm Sci Tech. 2010;11:1526–1540. doi: 10.1208/s12249-010-9526-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carpentier YA, Dupont IE. Advances in intravenous lipid emulsions. World J Surg. 2000;24:1493–1497. doi: 10.1007/s002680010267. [DOI] [PubMed] [Google Scholar]
- 5.Wanten GJA, Calder P. Immune modulation by parenteral lipid emulsions. Am J Clin Nutr. 2007;85:1171–1184. doi: 10.1093/ajcn/85.5.1171. [DOI] [PubMed] [Google Scholar]
- 6.Furukawa K, Yamamori H, Takagi K, Hayashi N, Suzuki R, Nakajima N, Tashiro T. Influences of soybean oil emulsion on stress response and cell-mediated immune function in moderately or severely stressed patients. Nutrition. 2002;18:235–240. doi: 10.1016/s0899-9007(01)00784-5. [DOI] [PubMed] [Google Scholar]
- 7.Heyland DK, MacDonald S, Keefe L, Drover JW. Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA. 1998;280:2013–2019. doi: 10.1001/jama.280.23.2013. [DOI] [PubMed] [Google Scholar]
- 8.Bannenberg G, Serhan CN. Specialized pro-resolving lipid mediators in the inflammatory response: an update. Biochim Biophys Acta. 2010;1801:1260–1273. doi: 10.1016/j.bbalip.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serhan CN, Yacoubian S, Yang R. Anti-inflammatory and proresolving lipid mediators. Annu Rev Pathol. 2008;3:279–312. doi: 10.1146/annurev.pathmechdis.3.121806.151409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heyland DK, MacDonald S, Keefe L, Drover JW. Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA. 1998;280:2013–2019. doi: 10.1001/jama.280.23.2013. [DOI] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 13.Rucker G, Schwarzer G, Carpenter J. Arcsine test for publication bias in meta-analyses with binary outcomes. Statistics in Medicine. 2008;27:746–763. doi: 10.1002/sim.2971. [DOI] [PubMed] [Google Scholar]
- 14.Wachtler P, König W, Senkal M, Kemen M, Köller M. Influence of a total parenteral nutrition enriched with omega-3 fatty acids on leukotriene synthesis of peripheral leukocytes and systemic cytokine levels in patients with major surgery. J Trauma. 1997;42:191–8. doi: 10.1097/00005373-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Gogos CA, Ginopoulos P, Salsa B, Apostolidou E, Zoumbos NC, Kalfarentzos F. Dietary omega-3 polyunsaturated fatty acids plus vitamin E restore immunodeficiency and prolong survival for severely ill patients with generalized malignancy: a randomized control trial. Cancer. 1998;82:395–402. doi: 10.1002/(sici)1097-0142(19980115)82:2<403::aid-cncr21>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 16.Furukawa K, Tashiro T, Yamamori H, Takagi K, Morishima Y, Sugiura T, Otsubo Y, Hayashi N, Itabashi T, Sano W, Toyoda Y, Nitta H, Nakajima N. Effects of soybean oil emulsion and eicosapentaenoic acid on stress response and immune function after a severely stressful operation. Ann Surg. 1999;229:255–61. doi: 10.1097/00000658-199902000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linseisen J, Hoffmann J, Lienhard S, Jauch KW, Wolfram G. Antioxidant status of surgical patients receiving TPN with an omega-3-fatty acid-containing lipid emulsion supplemented with alpha-tocopherol. Clin Nutr. 2000;19:177–84. doi: 10.1054/clnu.1999.0096. [DOI] [PubMed] [Google Scholar]
- 18.Heller AR, Fischer S, Rossel T, Geiger S, Siegert G, Ragaller M, Zimmermann T, Koch T. Impact of n-3 fatty acid supplemented parenteral nutrition on haemostasis patterns after major abdominal surgery. Br J Nutr. 2002;87 (Suppl 1):S95–101. doi: 10.1079/bjn2001462. [DOI] [PubMed] [Google Scholar]
- 19.Heller AR, Rössel T, Gottschlich B, Tiebel O, Menschikowski M, Litz RJ, Zimmermann T, Koch T. Omega-3 fatty acids improve liver and pancreas function in postoperative cancer patients. Int J Cancer. 2004;111:611–6. doi: 10.1002/ijc.20291. [DOI] [PubMed] [Google Scholar]
- 20.Kłek S, Kulig J, Szczepanik AM, Jedrys J, Kołodziejczyk P. The clinical value of parenteral immunonutrition in surgical patients. Acta Chir Belg. 2005;105:175–9. [PubMed] [Google Scholar]
- 21.Grimm H, Mertes N, Goeters C, Schlotzer E, Mayer K, Grimminger F, Fürst P. Improved fatty acid and leukotriene pattern with a novel lipid emulsion in surgical patients. Eur J Nutr. 2006;45:55–60. doi: 10.1007/s00394-005-0573-8. [DOI] [PubMed] [Google Scholar]
- 22.Mertes N, Grimm H, Fürst P, Stehle P. Safety and efficacy of a new parenteral lipid emulsion (SMOF lipid) in surgical patients: a randomized, double-blind, multicenter study. Ann Nutr Metab. 2006;50:253–9. doi: 10.1159/000091683. [DOI] [PubMed] [Google Scholar]
- 23.Senkal M, Geier B, Hannemann M, Deska T, Linseisen J, Wolfram G, Adolph M. Supplementation of omega-3 fatty acids in parenteral nutrition beneficially alters phospholipid fatty acid pattern. JPEN J Parenter Enteral Nutr. 2007;31:12–7. doi: 10.1177/014860710703100112. [DOI] [PubMed] [Google Scholar]
- 24.Wendel M, Rössel T, Bergmann S, Otto S, Ragaller M, Zimmermann T, Konopke R, Koch T, Heller AR. Impact of total parenteral nutrition including omega-3 fatty acids on the regulation of plasma lipoproteins and glycemic control after major abdominal surgery. E-SPEN. 2007;2:e103–e110. [Google Scholar]
- 25.Wichmann MW, Thul P, Czarnetzki HD, Morlion BJ, Kemen M, Jauch KW. Evaluation of clinical safety and beneficial effects of a fish oil containing lipid emulsion (Lipoplus, MLF541): data from a prospective, randomized, multicenter trial. Crit Care Med. 2007;35:700–6. doi: 10.1097/01.CCM.0000257465.60287.AC. [DOI] [PubMed] [Google Scholar]
- 26.Berger MM, Tappy L, Revelly JP, Koletzko BV, Gepert J, Corpataux JM, Cayeux MC, Chiolero RL. Fish oil after abdominal aorta aneurysm surgery. Eur J Clin Nutr. 2008;62:1116–22. doi: 10.1038/sj.ejcn.1602817. [DOI] [PubMed] [Google Scholar]
- 27.Liang B, Wang S, Ye YJ, Yang XD, Wang YL, Qu J, Xie QW, Yin MJ. Impact of postoperative omega-3 fatty acid-supplemented parenteral nutrition on clinical outcomes and immunomodulations in colorectal cancer patients. World J Gastroenterol. 2008;14:2434–9. doi: 10.3748/wjg.14.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang X, Li W, Li N, Li J. Omega-3 fatty acids-supplemented parenteral nutrition decreases hyperinflammatory response and attenuates systemic disease sequelae in severe acute pancreatitis: a randomized and controlled study. JPEN J Parenter Enteral Nutr. 2008;32:236–41. doi: 10.1177/0148607108316189. [DOI] [PubMed] [Google Scholar]
- 29.Heidt MC, Vician M, Stracke SK, Stadlbauer T, Grebe MT, Boening A, Vogt PR, Erdogan A. Beneficial effects of intravenously administered N-3 fatty acids for the prevention of atrial fibrillation after coronary artery bypass surgery: a prospective randomized study. Thorac Cardiovasc Surg. 2009;57:276–80. doi: 10.1055/s-0029-1185301. [DOI] [PubMed] [Google Scholar]
- 30.Piper SN, Schade I, Beschmann R, Maleck W, Boldt J, Rohm KD. Hepatocellular integrity after parenteral nutrition: comparison of a fish-oil-containing lipid emulsion with an olive-soybean oil-based lipid emulsion. Eur J Anaesthesiol. 2009;26:1076–82. doi: 10.1097/eja.0b013e32832e08e0. [DOI] [PubMed] [Google Scholar]
- 31.Puiggròs C, Sánchez J, Chacón P, Sabín P, Roselló J, Bou R, Planas M. Evolution of lipid profile, liver function, and pattern of plasma fatty acids according to the type of lipid emulsion administered in parenteral nutrition in the early postoperative period after digestive surgery. JPEN J Parenter Enteral Nutr. 2009;33:501–12. doi: 10.1177/0148607109333001. [DOI] [PubMed] [Google Scholar]
- 32.Badía-Tahull MB, Llop-Talaverón JM, Leiva-Badosa E, Biondo S, Farran-Teixidó L, Ramón-Torrell JM, Jódar-Masanes R. A randomised study on the clinical progress of high-risk elective major gastrointestinal surgery patients treated with olive oil-based parenteral nutrition with or without a fish oil supplement. Br J Nutr. 2010;104:737–41. doi: 10.1017/S0007114510001066. [DOI] [PubMed] [Google Scholar]
- 33.Jiang ZM, Wilmore DW, Wang XR, Wei JM, Zhang ZT, Gu ZY, Wang S, Han SM, Jiang H, Yu K. Randomized clinical trial of intravenous soybean oil alone versus soybean oil plus fish oil emulsion after gastrointestinal cancer surgery. Br J Surg. 2010;97:804–9. doi: 10.1002/bjs.6999. [DOI] [PubMed] [Google Scholar]
- 34.Han YY, Lai SL, Ko WJ, Chou CH, Lai HS. Effects of fish oil on inflammatory modulation in surgical intensive care unit patients. Nutr Clin Pract. 2012;27:91–8. doi: 10.1177/0884533611429796. [DOI] [PubMed] [Google Scholar]
- 35.Zhu MW, Tang DN, Hou J, Wei JM, Hua B, Sun JH, Chui HY. Impact of fish oil enriched total parenteral nutrition on elderly patients after colorectal cancer surgery. Chin Med J. 2012;125:178–81. [PubMed] [Google Scholar]
- 36.Adams S, Yeh YY, Jensen GL. Changes in plasma and erythrocyte fatty acids in patients fed enteral formulas containing different fats. JPEN J Parenter Enteral Nutr. 1993;17:30–4. doi: 10.1177/014860719301700130. [DOI] [PubMed] [Google Scholar]
- 37.Schauder P, Rohn U, Schafer G, Korff G, Schenk HD. Impact of fish oil enriched total parenteral nutrition on DNA synthesis, cytokine release and receptor expression by lymphocytes in the postoperative period. Br J Nutr. 2002;87(Suppl 1):S103–10. doi: 10.1079/bjn2001463. [DOI] [PubMed] [Google Scholar]
- 38.Koller M, Senkal M, Kemen M, Konig W, Zumtobel V, Muhr G. Impact of omega-3 fatty acid enriched TPN on leukotriene synthesis by leukocytes after major surgery. Clin Nutr. 2003;22:59–64. doi: 10.1054/clnu.2002.0592. [DOI] [PubMed] [Google Scholar]
- 39.Mayer K, Meyer S, Reinholz-Muhly M, Maus U, Merfels M, Lohmeyer J, Grimminger F, Seeger W. Short-time infusion of fish oil-based lipid emulsions, approved for parenteral nutrition, reduces monocyte proinflammatory cytokine generation and adhesive interaction with endothelium in humans. J Immunol. 2003;171:4837–4843. doi: 10.4049/jimmunol.171.9.4837. [DOI] [PubMed] [Google Scholar]
- 40.Mayer K, Fegbeutel C, Hattar K, Sibelius U, Krämer HJ, Heuer KU, Temmesfeld-Wollbrück B, Gokorsch S, Grimminger F, Seeger W. Omega-3 vs. omega-6 lipid emulsions exert differential influence on neutrophils in septic shock patients: impact on plasma fatty acids and lipid mediator generation. Intensive Care Med. 2003;29:1472–1481. doi: 10.1007/s00134-003-1900-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mayer K, Gokorsch S, Fegbeutel C, Hattar K, Rosseau S, Walmrath D, Seeger W, Grimminger F. Parenteral nutrition with fish oil modulates cytokine response in patients with sepsis. Am J Respir Crit Care Med. 2003;15(167):1321–1328. doi: 10.1164/rccm.200207-674OC. [DOI] [PubMed] [Google Scholar]
- 42.Mayer K, Meyer S, Reinholz-Muhly M, Maus U, Merfels M, Lohmeyer J, Grimminger F, Seeger W. Short-time infusion of fish oil-based lipid emulsions, approved for parenteral nutrition, reduces monocyte proinflammatory cytokine generation and adhesive interaction with endothelium in humans. J Immunol. 2003;171:4837–43. doi: 10.4049/jimmunol.171.9.4837. [DOI] [PubMed] [Google Scholar]
- 43.Antébi H, Mansoor O, Ferrier C, Tétégan M, Morvan C, Rangaraj J, Alcindor LG. Liver function and plasma antioxidant status in intensive care unit patients requiring total parenteral nutrition: comparison of 2 fat emulsions. JPEN J Parenter Enteral Nutr. 2004;28:142–8. doi: 10.1177/0148607104028003142. [DOI] [PubMed] [Google Scholar]
- 44.Tappy L, Berger MM, Schwarz JM, Schneiter P, Kim S, Revelly JP, Chioléro R. Metabolic effects of parenteral nutrition enriched with n-3 polyunsaturated fatty acids in critically ill patients. Clin Nutr. 2006;25:588–95. doi: 10.1016/j.clnu.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 45.Piper SN, Schade I, Beschmann RB, Maleck WH, Boldt J, Röhm KD. Hepatocellular integrity after parenteral nutrition: comparison of a fish-oil-containing lipid emulsion with an olive-soybean oil-based lipid emulsion. Eur J Anaesthesiol. 2009;26:1076–82. doi: 10.1097/eja.0b013e32832e08e0. [DOI] [PubMed] [Google Scholar]
- 46.Xiong J, Zhu S, Zhou Y, Wu H, Wang C. Regulation of omega-3 fish oil emulsion on the SIRS during the initial stage of severe acute pancreatitis. J Huazhong Univ Sci Technolog Med Sci. 2009;29:35–8. doi: 10.1007/s11596-009-0107-3. [DOI] [PubMed] [Google Scholar]
- 47.Sungurtekin H, Değirmenci S, Sungurtekin U, Oguz BE, Sabir N, Kaptanoglu B. Comparison of the effects of different intravenous fat emulsions in patients with systemic inflammatory response syndrome and sepsis. Nutr Clin Pract. 2011;26:665–71. doi: 10.1177/0884533611418783. [DOI] [PubMed] [Google Scholar]
- 48.Khor BS, Liaw SJ, Shih HC, Wang LS. Randomized, double blind, placebo-controlled trial of fish-oil-based lipid emulsion infusion for treatment of critically ill patients with severe sepsis. Asian J Surg. 2011;34:1–10. doi: 10.1016/S1015-9584(11)60011-0. [DOI] [PubMed] [Google Scholar]
- 49.Gupta A, Govil D, Bhatnagar S, Gupta S, Goyal J, Patel S, Baweja H. Efficacy and safety of parenteral omega-3 fatty acids in ventilated patients with acute lung injury. Indian J Crit Care Med. 2011;15:108–113. doi: 10.4103/0972-5229.83019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kari A, Hersio K, Takala J, Penttila I. Comparison of two long-chain triglyceride fat emulsions in parenteral nutrition of critically ill patients. Current Therap Res. 1989;45:1077–1087. [Google Scholar]
- 51.Larsen BM, Goonewardene LA, Joffe AR, Van Aerde JE, Field CJ, Olstad DL, Clandinin MT. Pre-treatment with an intravenous lipid emulsion containing fish oil (eicosapentaenoic and docosahexaenoic acid) decreases inflammatory markers after open-heart surgery in infants: A randomized, controlled trial. Clin Nutr. 2012;31:322–329. doi: 10.1016/j.clnu.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 52.Sabater J, Masclans JP, Sacanell J, Chacon P, Sabin P, Planas M. Effects on hemodynamics and gas exchange of omega-3 fatty acid-enriched lipid emulsion in acute respiratory distress syndrome (ARDS): a prospective, randomized, double-blind, parallel group study. Lipids Health Dis. 2008;7:39. doi: 10.1186/1476-511X-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taftachi F, Sanaei-Zadeh H, Sepehrian B, Zamani N. Lipid emulsion improves Glasgow coma scale and decreases blood glucose level in the setting of acute non-local anesthetic drug poisoning--a randomized controlled trial. Eur Rev Med Pharmacol Sci. 2012;16(Suppl 1):38–42. [PubMed] [Google Scholar]
- 54.Nijveldt RJ, Tan AM, Prins HA, de Jong D, van Rij GL, Wesdorp RI, van Leeuwen PA. Use of a mixture of medium-chain triglycerides and longchain triglycerides versus long-chain triglycerides in critically ill surgical patients: a randomized prospective double-blind study. Clin Nutr. 1998;17:23–9. doi: 10.1016/s0261-5614(98)80039-3. [DOI] [PubMed] [Google Scholar]
- 55.Lindgren BF, Ruokonen E, Magnusson-Borg K, Takala J. Nitrogen sparing effect of structured triglycerides containing both medium-and long-chain fatty acids in critically ill patients; a double blind randomized controlled trial. Clin Nutr. 2001;20:43–48. doi: 10.1054/clnu.2000.0156. [DOI] [PubMed] [Google Scholar]
- 56.Garnacho-Montero J, Ortiz-Leyba C, Jiménez-Jiménez FJ, Garcia-Garmendia JL, Jiménez-Jiménez LM, Garnacho-Montero MC, Barrero-Almodóvar A. Clinical and metabolic effects of two lipid emulsions on the parenteral nutrition of septic patients. Nutrition. 2002;18:134–138. doi: 10.1016/s0899-9007(01)00716-x. [DOI] [PubMed] [Google Scholar]
- 57.Iovinelli G, Marinangeli F, Ciccone A, Ciccozzi A, Leonardis M, Paladini A, Varrassi G. Parenteral nutrition in ventilated patients with chronic obstructive pulmonary disease: long chain vs. medium chain triglycerides. Minerva Anestesiol. 2007;73:65–76. [PubMed] [Google Scholar]
- 58.García-de-Lorenzo A, Denia R, Atlan P, Martinez-Ratero S, Le Brun A, Evard D, Bereziat G. Parenteral nutrition providing a restricted amount of linoleic acid in severely burned patients: a randomised double-blind study of an olive oil-based lipid emulsion v. medium/long-chain triacylglycerols. Br J Nutr. 2005;94:221–230. doi: 10.1079/bjn20051467. [DOI] [PubMed] [Google Scholar]
- 59.Huschak G, Zur Nieden K, Hoell T, Riemann D, Mast H, Stuttmann R. Olive oil based nutrition in multiple trauma patients: a pilot study. Intensive Care Med. 2005;31:1202–1208. doi: 10.1007/s00134-005-2727-9. [DOI] [PubMed] [Google Scholar]
- 60.Umpierrez GE, Spiegelman R, Zhao V, Smiley DD, Pinzon I, Griffith DP, Peng L, Morris T, Luo M, Garcia H, Thomas C, Newton CA, Ziegler TR. A double-blind, randomized clinical trial comparing soybean oil-based versus olive oil-based lipid emulsions in adult medical-surgical intensive care unit patients requiring parenteral nutrition. Crit Care Med. 2012;40:1792–1798. doi: 10.1097/CCM.0b013e3182474bf9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Grecu I, Mirea L, Grintescu I. Parenteral fish oil supplementation in patients with abdominal sepsis. Clin Nutr. 2003 abstract. [Google Scholar]
- 62.Friesecke S, Lotze C, Köhler J, Heinrich A, Felix SB, Abel P. Fish oil supplementation in the parenteral nutrition of critically ill medical patients: a randomised controlled trial. Intensive Care Med. 2008;34:1411–1420. doi: 10.1007/s00134-008-1072-1. [DOI] [PubMed] [Google Scholar]
- 63.Wang X, Li W, Zhang F, Pan L, Li N, Li J. Fish oil-supplemented parenteral nutrition in severe acute pancreatitis patients and effects on immune function and infectious risk: a randomized controlled trial. Inflammation. 2009;32:304–309. doi: 10.1007/s10753-009-9136-0. [DOI] [PubMed] [Google Scholar]
- 64.Barbosa VM, Miles EA, Calhau C, Lafuente E, Calder PC. Effects of fish oil containing lipid emulsion on plasma phospholipid fatty acids, inflammatory markers, and clinical outcomes in septic patients: a randomized, controlled clinical trial. Crit Care. 2010;14:R5. doi: 10.1186/cc8844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pontes-Arruda A, Dos Santos MC, Martins LF, González ER, Kliger RG, Maia M, Magnan GB EPICOS Study Group. Influence of parenteral nutrition delivery system on the development of bloodstream infections in critically ill patients: an international, multicenter, prospective, open-label, controlled study--EPICOS study. JPEN J Parenter Enteral Nutr. 2012;36:574–586. doi: 10.1177/0148607111427040. [DOI] [PubMed] [Google Scholar]
- 66.Singer P, Shapiro H, Theilla M, Anbar R, Singer J, Cohen J. Antiinflammatory properties of omega-3 fatty acids in critical illness: novel mechanisms and an integrative perspective. Intensive Care Med. 2008;34:1580–1592. doi: 10.1007/s00134-008-1142-4. [DOI] [PubMed] [Google Scholar]
- 67.Calder PC. Long-chain n-3 fatty acids and inflammation: potential application in surgical and trauma patients. Braz J Med Biol Res. 2003;36:433–446. doi: 10.1590/s0100-879x2003000400004. [DOI] [PubMed] [Google Scholar]
- 68.Pradelli l, Mayer K, Muscaritoli M, Heller AR. n-3 fatty acid-enriched parenteral nutrition regimens in elective surgical and ICU patients: a meta-analysis. Crit Care. 2012;16:R184. doi: 10.1186/cc11668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Palmer AJ, Ho CKM, Ajibola O, Avenell A. The role of ω-3 fatty acid supplemented parenteral nutrition in critical illness in adults: a systematic review and meta-analysis. Crit Care Med. 2013;41:307–316. doi: 10.1097/CCM.0b013e3182657578. [DOI] [PubMed] [Google Scholar]
- 70.Leiderman I, Malkova O, Levit A. Omega 3 enriched lipid emulsion decreases APACHE II and SOFA scores values in abdominal sepsis patients. Clin Nutr Suppl. 2010;5:30. [Google Scholar]
- 71.Ignatenko O, Yaroshetskiy A, Masolitin S, Protsenko D, Gelfand B. Fish oil treatment in severe trauma patients. Intensive Care Med. 2010;36:S316. [Google Scholar]