Abstract
Staphylococcus aureus carriers with S. aureus bacteremia may have a reduced mortality risk compared to non-carriers. A role for the immune system is suggested. Here, we study in mice the effect of mild S. aureus skin infection prior to endogenous or exogenous S. aureus bacteremia, and evaluate protection in relation to anti-staphylococcal antibody levels. Skin infections once or twice by a clinical S. aureus isolate (isolate P) or S. aureus strain 8325-4 were induced in mice free of S. aureus and anti-staphylococcal antibodies. Five weeks later, immunoglobulin G (IgG) levels in blood against 25 S. aureus antigens were determined, and LD50 or LD100 bacteremia caused by S. aureus isolate P was induced. S. aureus skin infections led to elevated levels of anti-staphylococcal IgG in blood. One skin infection improved the course of subsequent severe endogenous bacteremia only. A second skin infection further improved animal survival rate, which was associated with increased pre-bacteremia IgG levels against Efb, IsaA, LukD, LukE, Nuc, PrsA and WTA. In conclusion, S. aureus isolate P skin infection in mice reduces the severity of subsequent endogenous S. aureus bacteremia only. Although cellular immune effects cannot be rules out, anti-staphylococcal IgG against specified antigens may contribute to this effect.
Introduction
About 20% of the healthy human population persistently carries Staphylococcus aureus in their nose [1–3]. Although carriage of S. aureus is usually asymptomatic, this bacterial species can also cause infections. These include skin and soft tissue infections such as furunculosis, and also life-threatening invasive diseases such as pneumonia and bacteremia [4]. Nasal carriage of S. aureus is a major risk factor for the development of surgical site infections caused by S. aureus [5–9]. Moreover, Wertheim et al. [10] suggested that carriers have a three-fold higher risk than non-carriers of acquiring hospital-associated S. aureus bacteremia, while the mortality risk in carriers with bacteremia might be lower [10][10].
In spite of the higher risk of acquiring nosocomial S. aureus bacteremia in S. aureus carriers, the risk of death due to bacteremia might be lower once carriers acquire bacteremia. An explanation for this has not yet been provided, although a role for the immune system has been proposed. More than 80% of health care-associated S. aureus infections are caused by an endogenous strain [10, 11]. This suggests that because of long-term exposure to the colonizing S. aureus strain, carriers may have developed antibodies or cellular immune responses that protect against endogenous bacteremia-related death. Non-carriers may have developed humoral responses that protect against colonization more than against invasive disease. Several studies have been conducted comparing anti-staphylococcal antibody levels in carriers and non-carriers. Carriers show higher immunoglobulin G (IgG) levels than non-carriers against toxic shock syndrome toxin 1 (TSST-1), staphylococcal enterotoxin A (SEA) [12] and the factor effecting methicillin resistance (FmtB) [13]. In contrast, compared to carriers, IgG levels in non-carriers are significantly higher against alpha toxin, major autolysin (Atl), iron-responsive surface determinant A and H (IsdA and IsdH), immunodominant staphylococcal antigen A (IsaA) [13], extracellular adherence protein (Eap), haptoglobin-hemoglobin binding protein A (HarA), and clumping factor B (ClfB) [14]. In addition to these descriptive studies, the prospective clinical study of Kolata et al. [15] also suggested a contribution of antibodies against the colonizing S. aureus strain in the improvement of the course and outcome of S. aureus bacteremia. In this study, S. aureus carriers who developed endogenous S. aureus bacteremia showed a stronger and broader pre-bacteremia IgG response to their own invasive, endogenous S. aureus strain compared to non-carriers, who develop an exogenous S. aureus bacteremia. Recently, Montgomery et al. [16] showed in an experimental study in mice that S. aureus skin and soft tissue infection (SSTI) protects against secondary endogenous SSTI. This protection was mediated by antibody and interleukin (IL) 17A and inhibited by interferon (IFN) γ. Conclusions regarding the antigen-specificity of these antibodies were not drawn. Their observation suggests, in addition to a role of humoral immunity, a protective role of cellular immunity. Protection against exogenous infection was not studied.
In humans, conclusive studies on the exact influence of S. aureus carriage and/or S. aureus exposure and the role of humoral and/or cellular immunity on the course and outcome of subsequent endogenous or exogenous S. aureus infection are difficult as both carriers and non-carriers harbor a diversity of anti-staphylococcal antibodies. In non-carriers, these antibodies may be induced by S. aureus carriage or (sub-)clinical infection in the past. Studies in mice initially free of S. aureus and anti-staphylococcal antibodies may provide further insight.
In the present study in mice, we investigated whether the course of S. aureus bacteremia is influenced by prior S. aureus exposure and whether this is dependent on the S. aureus strain (endogenous or exogenous) causing the initial exposure. For this purpose, a mouse model of mild S. aureus skin infection once or twice was established. We focused in this study on humoral immunity only, by analyzing the pre-bacteremia IgG levels against a broad panel of 25 S. aureus antigens following skin infection, and we assessed whether improvement in the course of S. aureus bacteremia was associated with pre-bacteremia IgG levels.
Materials and Methods
Bacteria
Bacterial strains used were a clinical S. aureus isolate and S. aureus strain 8325–4, a well-characterized laboratory strain (MSSA, ST8) [17]. S. aureus isolate P (gift from G. Buist, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands) is a clinical isolate recovered from blood of a septic patient and was previously described and analyzed by proteomics by Ziebandt et al. (community-acquired MSSA, ST7, agr-type 1) [18]. Staphylococci were grown overnight at 35°C on Colombia III blood agar (Becton Dickinson, Breda, the Netherlands). Cultures of S. aureus, grown in Brain Heart Infusion broth (Becton Dickinson, Breda, the Netherlands) until OD560 ~ 1.0, were stored with 5% glycerol at -80°C. For infection, a suspension of staphylococci was defrosted and centrifuged for 10 minutes at 14,000 x g. The S. aureus pellet was resuspended in saline, and diluted to obtain the desired inoculum.
Animals
Specified opportunistic pathogen-free (SOPF) female BALB/cBYJ mice were obtained from Charles River (Saint-Germain-sur-l’Arbresle, France). These S. aureus-free animals were 11–13 weeks old on the day of infection, and were given food and water ad libitum. Before each experiment, one mouse per group was sacrificed to confirm the S. aureus-free status in terms of cultures of fresh fecal and nasal microbiota and the absence of anti-staphylococcal IgG levels in blood (see below). The animal experimental protocols adhered to the rules laid down in the Dutch Animal Experimentation Act and the EU Animal Directive 2010/63/EU, and the Institutional Animal Care and Use Committee of the Erasmus University Medical Centre Rotterdam approved the present protocols (permit number: EMC2415).
Model of S. aureus skin infection
The method of induction of S. aureus skin infection in mice was adapted from Brown et al. [19]. In short, the lower back of the mice was shaved and cleaned with 70% ethanol under general anesthesia after using a mixture of medetomidine (Sedator®, 0.5 mg/kg; Eurovet Animal Health, Bladel, the Netherlands), midazolam (Midazolam, 5 mg/kg; Actavis, Baarn, the Netherlands) and fentanyl (Fentanyl, 0.05 mg/kg; Hameln Pharmaceuticals, Hameln, Germany). S. aureus isolate P (3–6 x 107 CFU) or S. aureus 8325–4 (5–10 x 107 CFU) was injected intradermally (50 μL) (n = 10 per group). For placebo skin infection, mice received saline. Anesthesia was antagonized to quickly awaken the mice using a mixture of atipamezole (Antisedan®, 2.5 mg/kg; Orion Corporation, Espoo, Finland), flumazenil (Flumazenil, 0.5 mg/kg; Pharmachemie, Haarlem, the Netherlands) and naloxon (Naloxon, 1.2 mg/kg; Orpha-Devel Handels und Vertriebs, Purkersdorf, Germany). Anesthetic and antagonistic agents were administered intraperitoneally, in a total volume of 175 and 250 μL, respectively. Mouse body weight was assessed three times a week. Two and five weeks after intradermal S. aureus inoculation, blood was withdrawn from the tail artery to determine anti-staphylococcal IgG levels in serum. Blood was collected in a Microvette® CB300 tube (Sarstedt, Etten-Leur, the Netherlands) and sera were prepared and stored at -80°C. At week five, mice were sacrificed by CO2 exposure. Presence of S. aureus in intestines and nasopharynx five weeks after intradermal S. aureus inoculation was determined by culturing fresh feces and nasopharyngeal lavage in phenol-red mannitol salt broth (PHMB; Becton Dickinson, Breda, the Netherlands) at 35°C for 7 days. Nasopharyngeal lavage was performed by flushing the nares with 5 mL sterile phosphate buffered saline + 0.4% Tween 20 (Sigma-Aldrich, Zwijndrecht, the Netherlands). When PHMB turned yellow, this was subcultured overnight at 35°C on Colombia III blood agar. S. aureus was identified based on colony morphology and Slidex Staph Plus agglutination testing (bioMérieux, Marcy l’Etoile, France). Multi-locus variable number of tandem repeat analysis (MLVA) of SIRU01, SIRU07, SIRU13 and SIRU15 [20] was used at regular intervals to verify that isolated S. aureus strains were the same as the strain used for infection of mice.
Model of S. aureus bacteremia
Bacteremia was induced by inoculation of 100 μL of S. aureus isolate P into the tail vein. A S. aureus inoculum at the 50% lethal dose (LD50; 1–2 x 105 CFU) or at the 100% lethal dose (LD100; 5–8 x 105 CFU) was used for establishment bacteremia. Clinical signs of illness in each mouse were evaluated twice daily during the experiment to minimize suffering as described before [21]. Mice were scored -1 directly after bacterial inoculation. Mice with bad fur were scored -2. Mice with bad fur and hunched back were scored -3. Mice with bad fur and hunched back and that showed instability were scored -4. These mice showed severe signs of illness and were euthanized by CO2 exposure. Euthanized mice were considered as deaths, as pilot experiments showed that mice with severe signs of illness die before the next time point. Animal survival rate over 14 days after infection was monitored. At day 28, S. aureus load in blood and organs of surviving animals was determined to investigate whether surviving mice next to survival also showed improved S. aureus clearance. The mice were sacrificed by CO2 exposure. A blood sample was taken via a transcutaneous cardiac puncture and collected in a vial containing Lithium Heparin (Sarstedt, Etten-Leur, the Netherlands). The lungs, spleen, liver, and kidneys were removed aseptically and homogenized (Polytron, Kinematica, Luzern, Switzerland) in 2 mL of saline for 10 seconds at 30,000 rpm at room temperature. Undiluted homogenate suspensions and blood as well as 10-fold serial dilutions in saline were plated onto Colombia III blood agar. After incubation overnight at 35°C, colonies were counted.
Experimental set-up to study the course of S. aureus bacteremia in relation to prior S. aureus skin infection
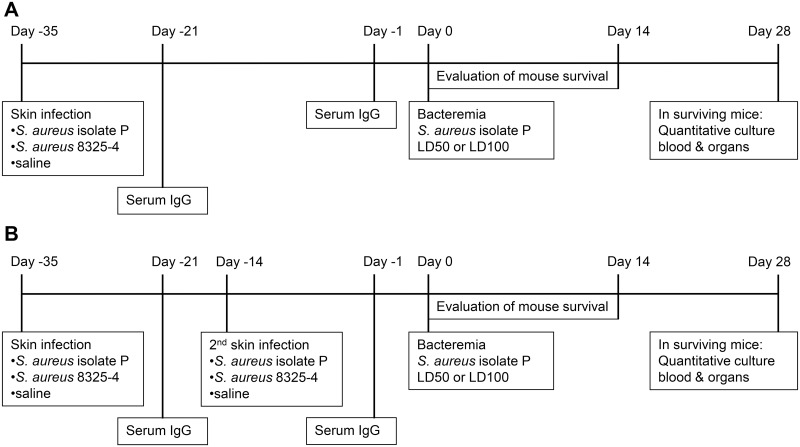
Experimental set-up is shown in Fig 1. Skin infection with S. aureus isolate P or with S. aureus 8325–4 (n = 15 per group) was induced 35 days before induction of bacteremia. Controls received intradermal inoculation of saline. In case of skin infection twice, three weeks after the first skin infection, a second skin infection using the same S. aureus strain was applied, near the inoculation site of the first skin infection. Bacteremia caused by S. aureus isolate P was always established at five weeks after the first skin infection, when mice were 16–18 weeks old (adults).
Fig 1. Experimental set-up for studying the influence of S. aureus skin infection on subsequent bacteremia.
A. Skin infection once at 35 days before S. aureus bacteremia. B. Skin infection twice at 35 days and 14 days before S. aureus bacteremia.
Quantification of serum anti-staphylococcal IgG levels
Serum IgG levels against the following antigens were semi-quantified: alpha toxin; clumping factors A and B (ClfA and ClfB); extracellular fibrinogen-binding protein (Efb); ESAT-6-like protein (EsxA) and CFP-10-like protein (EsxB); formyl peptide receptor-like1 inhibitory protein (FLIPr); fibronectin-binding protein A (FnbpA); immunodominant staphylococcal antigen A (IsaA); iron-responsive surface determinants A and H (IsdA and IsdH); lipase; leukocidins D and E (LukD and LukE); peptidoglycan hydrolase (LytM); endonuclease (Nuc); peptidoglycan (PG); a parvulin-type peptidyl-prolyl cis/trans isomerase (PrsA); hypothetical protein SA0104; serine-aspartate dipeptide repeat protein D (SdrD); staphylococcal superantigen-like proteins 1, 3, 5, and 10 (SSL1, SSL3, SSL5, and SSL10); and wall teichoic acid (WTA). Genes encoding these S. aureus antigens were all present in both S. aureus isolate P and S. aureus 8325–4.
Alpha toxin, LukD, and LukE were prepared as described previously [22]. ClfB, FnbpA, IsdA, IsdH, and SdrD were expressed and purified as described previously [12]. The constructs were kindly provided by T. Foster (Trinity College, Dublin, Ireland). All other antigens were kindly provided by other research groups, as indicated in the Acknowledgements.
IgG levels were semi-quantified simultaneously in multiplex assays using a bead-based flow cytometry technique (xMap; Luminex Corporation, Austin, TX). Methods have been described elsewhere [23–26]. Tests were performed in independent duplicates, and the median fluorescence intensity (MFI) values, reflecting semi-quantitative antibody levels, were averaged. In each experiment, control beads (no antigen coupled) were included to determine nonspecific binding. In case of nonspecific binding, the nonspecific MFI values were subtracted from the antigen-specific values.
Serum samples from mice with skin infection caused by S. aureus isolate P or S. aureus 8325–4 (n = 10 per group), and from mice with placebo skin infection were analyzed. Sera from three non-infected mice were used as negative controls.
Statistical analysis
The Mann-Whitney U test was used to compare median differences in anti-staphylococcal IgG levels in different groups. The Wilcoxon Signed Rank test was used to compare anti-staphylococcal IgG levels in paired samples. In individual mice, high IgG levels against an antigen were not correlated with high IgG levels against other antigens, or vice versa. The Bonferroni correction was applied to correct for multiple testing. As a result, P-values < 0.002 were considered to be statistically significant. These statistical analyses were performed using the Statistical Package of Social Sciences version 17.0 for Windows (SPSS Inc., Chicago, IL).
The Fisher’s exact test was used to compare differences in S. aureus colonization status. The log rank test was used to determine statistical differences in animal survival rate between groups. Differences were considered statistically significant when 2-sided P-values were < 0.05. GraphPad Prism 5 for Windows (GraphPad Software Inc., La Jolla, CA) was used for these statistical analyses.
Results
S. aureus skin infection
Mice infected with S. aureus isolate P or S. aureus 8325–4 developed a scab (area of ~1.5 cm2) at the inoculation site within 1 week. Body weight loss was only minor (maximum of 8% at week 1 after intradermal inoculation) and mice appeared healthy. Five weeks after infection, when S. aureus bacteremia was induced, the skin had healed and body weight was restored. S. aureus cultures from the inoculation site were always negative at week 5 after skin infection. However, the intestines of mice with skin infection once or twice, caused by S. aureus isolate P or S. aureus 8325–4, were always culture positive for the infecting S. aureus strain. Nasopharynges were not always culture positive: S. aureus was cultured from mice after S. aureus isolate P skin infection once (3 of 10 mice) or twice (5 of 10 mice), and after S. aureus 8325–4 skin infection once (1 of 10 mice) or twice (4 of 10 mice). No significant differences in number of nasopharynx culture positive mice were observed.
Anti-staphylococcal IgG levels following skin infection
Serum anti-staphylococcal IgG levels against a broad panel of 25 staphylococcal antigens were assessed in mice with S. aureus isolate P skin infection once or twice (Table 1) or with S. aureus 8325–4 skin infection once or twice (Table 2) (n = 10 per group). Levels were assessed at two and five weeks after the first skin infection. Antigens included immune modulators, superantigen like proteins, MSCRAMMs (microbial surface components recognizing adhesive matrix molecules), toxins, and household antigens. Before infection (week 0), IgG levels were at background values. In mice with skin infection once caused by S. aureus isolate P or S. aureus 8325–4, IgG levels against a number of S. aureus antigens were observed at week 2 and 5 after infection, but these did not change significantly over time. However, following the second skin infection with S. aureus isolate P, the IgG levels against IsaA, Nuc, PrsA, and WTA were significantly elevated at week 5 (P < 0.002), whereas the second skin infection with S. aureus 8325–4 resulted in a significant rise in IgG levels at week 5 against Efb, IsaA, and IsdA (P < 0.002).
Table 1. S. aureus isolate P skin infection.
Median fluorescence intensity (MFI) values reflecting levels of antigen-specific IgG against 25 S. aureus antigens in sera from mice (n = 10 per group) before skin infection (week 0), after skin infection once (week 2 and week 5), and after skin infection twice (week 5 after first skin infection).
| Skin infection once | Skin infection twice | |||||||
|---|---|---|---|---|---|---|---|---|
| Antigen | Median MFI week 0 (range) | Median MFI week 2 (range) | Median MFI week 5 (range) | Median MFI week 5 (range) | P-value (skin infection once) week 2 vs week 0 a | P-value (skin infection once) week 5 vs week 0 a | P-value (skin infection once) week 5 vs week 2 b | P-value (week 5) skin infection twice vs once a |
| alpha toxin | 0 (0–1) | 644 (203–1712) | 5693 (4402–6704) | 3994 (3381–5922) | 0.011 | 0.011 | 0.005 | 0.007 |
| ClfA | 0 (0–0) | 0 (0–0) | 0 (0–4) | 0 (0–5) | 1.000 | 0.584 | 0.317 | 0.304 |
| ClfB | 0 (0–0) | 0 (0–0) | 0 (0–14) | 0 (0–4) | 1.000 | 0.584 | 0.317 | 0.358 |
| Efb | 3 (1–6) | 4 (2–8) | 11 (7–1536) | 143 (33–1590) | 0.611 | 0.011 | 0.005 | 0.070 |
| EsxA | 5 (5–6) | 5 (5–6) | 6 (4–8) | 5 (3–8) | 0.661 | 0.495 | 0.313 | 0.569 |
| EsxB | 3 (3–4) | 4 (3–24) | 5 (3–46) | 4 (2–177) | 0.551 | 0.062 | 0.028 | 0.119 |
| FLIPr | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–44) | 1.000 | 1.000 | 1.000 | 0.068 |
| FnbpA | 0 (0–0) | 0 (0–3) | 0 (0–14) | 0 (0–0) | 0.584 | 0.584 | 0.317 | 0.317 |
| IsaA | 5 (4–6) | 12 (6–1504) | 8 (5–1509) | 3885 (247–8090) | 0.014 | 0.034 | 0.386 | 0.001 * |
| IsdA | 103 (3–106) | 77 (0–108) | 30 (0–94) | 70 (0–432) | 0.498 | 0.236 | 0.012 | 0.072 |
| IsdH | 63 (27–68) | 38 (21–61) | 36 (11–50) | 41 (20–1065) | 0.236 | 0.236 | 0.475 | 0.257 |
| lipase | 6 (6–6) | 9 (8–14) | 8 (7–20) | 80 (9–8188) | 0.011 | 0.011 | 0.959 | 0.002 |
| LukD | 0 (0–0) | 0 (0–0) | 103 (1–1986) | 1595 (34–5177) | 0.584 | 0.011 | 0.005 | 0.019 |
| LukE | 2 (0–2) | 235 (13–777) | 4470 (2110–6930) | 6487 (4921–7596) | 0.011 | 0.011 | 0.005 | 0.023 |
| LytM | 1 (1–3) | 2 (0–5) | 2 (1–3) | 4 (2–66) | 0.865 | 0.441 | 0.918 | 0.015 |
| Nuc | 2 (1–3) | 6 (0–270) | 405 (2–3999) | 4554 (930–5686) | 0.128 | 0.028 | 0.013 | 0.001 * |
| PG | 6 (4–6) | 6 (5–6) | 6 (5–7) | 6 (5–7) | 0.302 | 0.395 | 0.777 | 0.223 |
| PrsA | 32 (28–33) | 405 (194–900) | 3282 (1728–4490) | 4568 (3592–5838) | 0.011 | 0.011 | 0.005 | 0.0019 * |
| SA0104 | 5 (4–6) | 6 (4–19) | 6 (4–34) | 6 (5–9) | 0.125 | 0.106 | 0.574 | 0.939 |
| SdrD | 0 (0–0) | 0 (0–10) | 0 (0–22) | 0 (0–5) | 0.584 | 0.584 | 0.317 | 0.942 |
| SSL1 | 0 (0–0) | 0 (0–50) | 1 (0–63) | 21 (0–34) | 0.215 | 0.148 | 0.500 | 0.292 |
| SSL3 | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 1.000 | 1.000 | 1.000 | 1.000 |
| SSL5 | 0 (0–0) | 0 (0–2) | 3 (0–274) | 0 (0–20) | 0.584 | 0.098 | 0.028 | 0.033 |
| SSL10 | 0 (0–0) | 0 (0–2) | 1 (0–12) | 0 (0–2) | 0.147 | 0.098 | 0.324 | 0.606 |
| WTA | 1 (0–1) | 1 (0–2) | 4 (2–10) | 22 (4–78) | 0.283 | 0.011 | 0.008 | 0.0019 * |
a Mann-Whitney U test
b Wilcoxon signed ranks test
* P < 0.002
Table 2. S. aureus 8325–4 skin infection.
Median fluorescence intensity (MFI) values reflecting levels of antigen-specific IgG against 25 S. aureus antigens in sera from mice (n = 10 per group) before skin infection (week 0), after skin infection once (week 2 and week 5), and after skin infection twice (week 5 after first skin infection).
| Skin infection once | Skin infection twice | |||||||
|---|---|---|---|---|---|---|---|---|
| Antigen | Median MFI week 0 (range) | Median MFI week 2 (range) | Median MFI week 5 (range) | Median MFI week 5 (range) | P-value (skin infection once) week 2 vs week 0 a | P-value (skin infection once) week 5 vs week 0 a | P-value (skin infection once) week 5 vs week 2 b | P-value (week 5) skin infection twice vs once a |
| alpha toxin | 0 (0–1) | 1129 (354–2341) | 5545 (2110–6932) | 4401 (2878–6605) | 0.011 | 0.011 | 0.005 | 0.258 |
| ClfA | 0 (0–0) | 0 (0–0) | 0 (0–1) | 0 (0–0) | 1.000 | 0.584 | 0.317 | 0.317 |
| ClfB | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–2) | 1.000 | 1.000 | 1.000 | 0.317 |
| Efb | 3 (1–6) | 4 (2–8) | 8 (6–12) | 24 (15–80) | 0.445 | 0.017 | 0.009 | 0.0002 * |
| EsxA | 5 (5–6) | 5 (3–6) | 6 (4–6) | 6 (5–6) | 0.865 | 0.670 | 0.366 | 0.335 |
| EsxB | 3 (3–4) | 3 (3–12) | 4 (3–6) | 4 (2–39) | 0.733 | 0.351 | 0.483 | 0.731 |
| FLIPr | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 1.000 | 1.000 | 1.000 | 1.000 |
| FnbpA | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–2) | 1.000 | 1.000 | 1.000 | 0.147 |
| IsaA | 5 (4–6) | 7 (4–61) | 6 (5–166) | 186 (12–6838) | 0.235 | 0.089 | 0.918 | 0.001 * |
| IsdA | 103 (3–106) | 54 (0–129) | 82 (0–221) | 525 (120–1145) | 0.397 | 0.612 | 0.161 | 0.001 * |
| IsdH | 63 (27–68) | 34 (28–60) | 36 (14–53) | 37 (19–61) | 0.398 | 0.237 | 0.359 | 0.650 |
| lipase | 6 (6–6) | 12 (5–166) | 141 (8–1992) | 405 (8–6865) | 0.011 | 0.011 | 0.008 | 0.364 |
| LukD | 0 (0–0) | 0 (0–61) | 7 (0–112) | 11 (2–57) | 0.304 | 0.037 | 0.012 | 0.325 |
| LukE | 2 (0–2) | 5 (0–345) | 57 (5–1008) | 118 (7–1743) | 0.034 | 0.011 | 0.022 | 0.364 |
| LytM | 1 (1–3) | 2 (1–3) | 2 (1–3) | 3 (1–22) | 0.492 | 0.293 | 0.429 | 0.333 |
| Nuc | 2 (1–3) | 1 (0–13) | 2 (0–15) | 11 (1–1646) | 0.497 | 0.670 | 0.130 | 0.031 |
| PG | 6 (4–6) | 6 (5–6) | 6 (4–7) | 6 (5–7) | 0.664 | 0.389 | 0.589 | 0.373 |
| PrsA | 32 (28–33) | 190 (43–303) | 1074 (153–2502) | 3167 (264–4967) | 0.011 | 0.011 | 0.005 | 0.034 |
| SA0104 | 5 (4–6) | 6 (5–8) | 5 (4–8) | 7 (4–23) | 0.034 | 0.391 | 0.087 | 0.030 |
| SdrD | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–3) | 1.000 | 1.000 | 1.000 | 0.317 |
| SSL1 | 0 (0–0) | 1 (0–93) | 45 (0–3834) | 41 (1–4112) | 0.148 | 0.062 | 0.043 | 0.545 |
| SSL3 | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 1.000 | 1.000 | 1.000 | 1.000 |
| SSL5 | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0 (0–5) | 1.000 | 1.000 | 1.000 | 0.317 |
| SSL10 | 0 (0–0) | 0 (0–5) | 0 (0–6) | 1 (0–5) | 0.215 | 0.148 | 0.564 | 0.209 |
| WTA | 1 (0–1) | 1 (0–2) | 2 (0–7) | 3 (1–12) | 0.122 | 0.383 | 0.443 | 0.068 |
a Mann-Whitney U test
b Wilcoxon signed ranks test
* P < 0.002
Course of S. aureus bacteremia in mice with prior skin infection
Bacteremia was always induced by S. aureus isolate P irrespective of the strain used for skin infection. Animal survival rate after bacteremia was monitored over a 14-day evaluation period. After this time point, no further changes in animal survival were observed (data not shown).
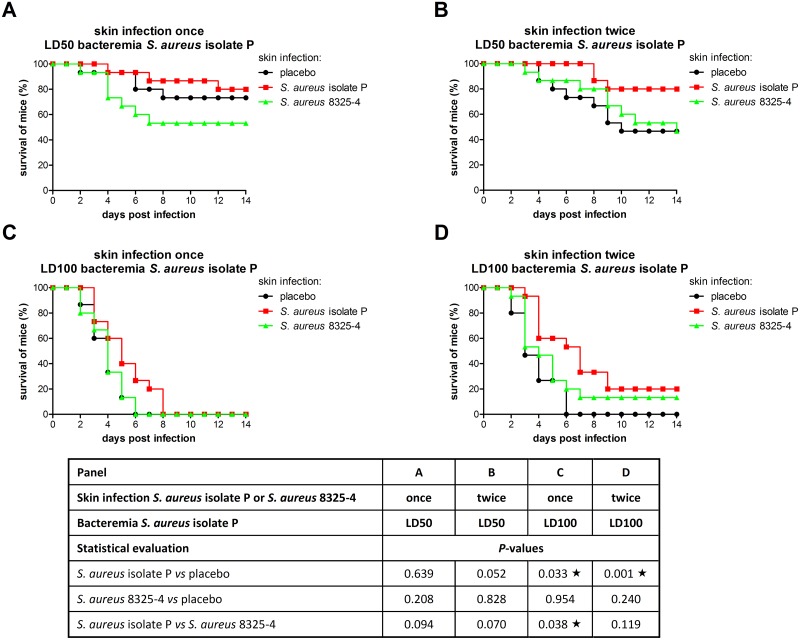
The course of LD50 S. aureus bacteremia in mice with prior skin infection is shown in Fig 2A and 2B (n = 15 per group). In mice with placebo skin infection, survival of bacteremic mice declined gradually, until 47–73% at day 14. Survival rates of mice with placebo skin infection once or twice were comparable. After skin infection once or twice with S. aureus isolate P or S. aureus 8325–4, animal survival rate of bacteremic mice was not significantly improved compared to placebo skin infection.
Fig 2. Survival rate in mice with S. aureus bacteremia.
Skin infection prior to S. aureus bacteremia was induced once or twice by S. aureus isolate P (red squares) or S. aureus 8325–4 (green triangles); placebo skin infection (black circles). LD50 or LD100 bacteremia was induced by S. aureus isolate P. Animal survival rate in different groups (n = 15 per group) was compared using the log-rank test, and P-values are indicated in the table. Stars indicate statistically significant differences (P < 0.05).
The course of LD100 S. aureus bacteremia in mice with prior skin infection is shown in Fig 2C and 2D (n = 15 per group). In mice with placebo skin infection, survival of bacteremic mice declined gradually, and at day 6 all mice had died. Survival rates of mice with placebo skin infection once or twice were comparable. An increased animal survival rate of bacteremic mice was observed only after prior skin infection with S. aureus isolate P. The time to death of bacteremic mice was increased after skin infection once (P = 0.033), and was further prolonged after the second skin infection (P = 0.001). Mouse survival at day 14 was increased from 0% to 20%. Skin infection once or twice with S. aureus 8325–4 had no effect on the course of bacteremia.
In mice that survived LD50 bacteremia (Fig 2A and 2B) or LD100 bacteremia (Fig 2D), S. aureus was never cultured from blood, lungs, spleen, and liver at day 28. In 17–60% of surviving mice, cultures from kidneys were S. aureus positive, ranging from 1 x 101–2 x 107 CFU per two kidneys, but differences in number of S. aureus positive kidneys between the mice that survived moderate bacteremia were not observed
Course of S. aureus bacteremia in association with anti-S. aureus IgG levels
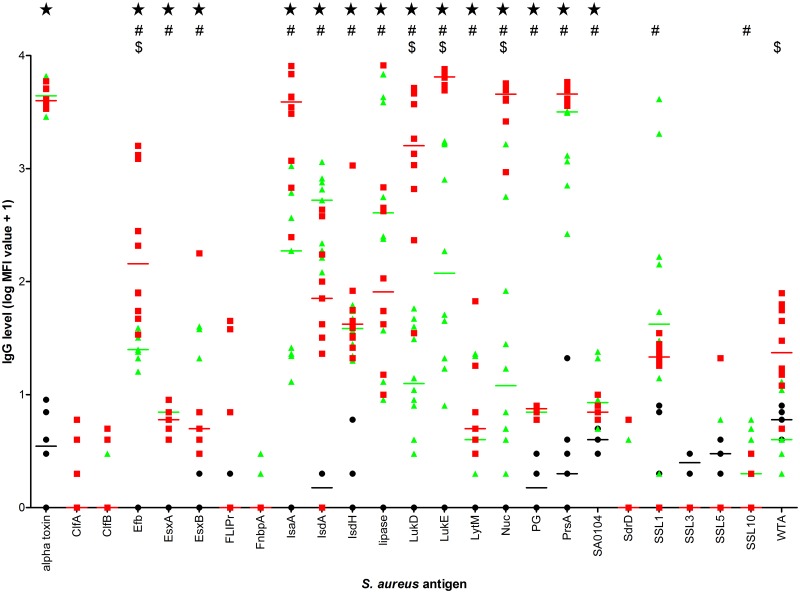
We assessed whether improvement of the course of S. aureus bacteremia was associated with increased levels of anti-staphylococcal IgG induced by S. aureus skin infection. To this aim, in mice receiving skin infection twice caused by S. aureus isolate P or S. aureus 8325–4 (n = 10 per group), serum IgG levels against a broad panel of 25 staphylococcal antigens at week 5 after skin infection, the day of induction of S. aureus isolate P bacteremia were compared. IgG levels are shown in Fig 3. In S. aureus isolate P skin infected mice, IgG levels against alpha toxin, Efb, EsxA, EsxB, IsaA, IsdA, IsdH, lipase, LukD, LukE, LytM, Nuc, PG, PrsA, and SA0104 were significantly higher than in mice with placebo skin infection. In S. aureus 8325–4 skin infected mice, IgG levels against Efb, EsxA, EsxB, IsaA, IsdA, IsdH, lipase, LukD, LukE, LytM, Nuc, PG, PrsA, SA0104, SSL1 and SSL10 were significantly higher than in mice with placebo skin infection. Comparing both IgG profiles, IgG levels against Efb, LukD, LukE, Nuc, and WTA were significantly higher in S. aureus isolate P skin infected mice than in S. aureus 8325–4 skin infected mice.
Fig 3. Antigen-specific IgG levels in mice at week 5 after S. aureus skin infection twice.
Median fluorescence intensity (MFI) values reflect levels of IgG against 25 S. aureus antigens. Skin infections were induced by S. aureus isolate P (red squares) or S. aureus 8325–4 (green triangles); placebo skin infection (black circles) (n = 10 per group). Median values are indicated by horizontal lines. Stars indicate significant differences (P < 0.002) between mice with S. aureus isolate P skin infection and mice with placebo skin infection. Number signs indicate significant differences (P < 0.002) between mice with S. aureus 8325–4 skin infection and mice with placebo skin infection. Dollar signs indicate significant differences (P < 0.002) between mice with S. aureus isolate P skin infection and mice with S. aureus 8325–4 skin infection.
Discussion
In the present study, we showed for the first time that mild S. aureus skin infection improved the course of subsequent endogenous S. aureus bacteremia. The use of S. aureus-free mice enabled us to draw conclusions in this respect. In humans, conclusive studies on the exact influence of S. aureus exposure on the outcome of S. aureus bacteremia remain difficult, as both carriers and non-carriers have been exposed to S. aureus [12–15]. Wertheim et al. [10] already showed that carriers may have a decreased risk of death due to S. aureus bacteremia compared to non-carriers, hypothesizing that anti-staphylococcal antibody levels or components of the cellular immune system that are increased in carriers, induced by prior S. aureus exposure, may play a role in protection against death due to S. aureus bacteremia. Our observations in the present study in mice are in line with the suggestions made by Wertheim et al.
We established local S. aureus skin infection caused by either S. aureus isolate P, a clinical sepsis isolate [18], or S. aureus 8325–4, a frequently used sequenced strain [17]. Subsequent bacteremia was always induced by S. aureus isolate P. Skin infection led to S. aureus colonization in intestines and nasopharynges, and with respect to the humoral immune response, anti-staphylococcal IgG in blood was found. The skin infection described above was mild and transient, simulating a mild S. aureus infection in humans. We showed that prior S. aureus skin infection improved the course of LD100 S. aureus isolate P bacteremia provided that bacteremia was caused by the endogenous S. aureus strain. This effect was not observed in exogenous bacteremia caused by S. aureus isolate P when skin infection was induced by S. aureus 8325–4. While a single prior skin infection resulted in delayed time to death and improved animal survival in our endogenous LD100 S. aureus bacteremia model, in endogenous LD50 S. aureus bacteremia prior skin infection did not. This lack of a protective effect in LD50 S. aureus bacteremia may be related to the relatively small window to detect significant differences in this respect. Whereas in the present study bacteremia was always caused by S. aureus isolate P, in future experiments it would be informative to study the effects of skin infection on the course and outcome of subsequent S. aureus 8325–4 bacteremia. S. aureus 8325–4 showed a very steep inoculum-response curve in the mouse model of bacteremia, and as a consequence unfortunately, we were not able to realize reproducible infection models with LD50 and LD100 inocula.
We also demonstrated that a second skin infection following the first skin infection further enhanced the survival rate in mice with endogenous LD100 S. aureus bacteremia. Also in the model of endogenous LD50 S. aureus bacteremia, mortality was reduced, although this difference was only borderline significant (P = 0.052), indicating a trend in improvement of survival rate in skin infected mice with subsequent endogenous bacteremia. Interestingly, following the second skin infection, pre-bacteremia serum IgG levels were elevated as well. As improved survival rates were associated with strong increases in pre-bacteremia anti-staphylococcal IgG levels, this suggests that IgG resulting from prior mild skin infection may potentially act protective against antigens determining the outcome of S. aureus bacteremia. Future studies including successful adoptive transfer of antibody purified from serum of skin infected mice to naive mice prior to S. aureus bacteremia are necessary to confirm a protective role of pre-bacteremia IgG.
Regarding the pre-bacteremia IgG levels, most striking were the IgG levels against IsaA, Nuc, PrsA, and WTA, which were further elevated following the second skin infection. These IgG levels may contribute to the delayed time to death and improved animal survival in mice with S. aureus isolate P bacteremia. Next to IgG against these S. aureus antigens, pre-bacteremia IgG against Efb, LukD, and LukE may also contribute in this respect. These IgG levels were elevated in mice with S. aureus isolate P skin infection twice and endogenous bacteremia compared to mice with S. aureus 8325–4 skin infection twice and exogenous bacteremia.
Our observation that S. aureus isolate P skin infection improved the course of subsequent endogenous S. aureus bacteremia in mice are in line with those obtained in a recently published experimental study in mice by Montgomery et al. [16]. They studied the effect of S. aureus SF8300 (USA300) skin infection (SSTI) on a secondary SSTI caused by the same S. aureus strain. It was shown that skin infection protected against the subsequent skin infection. Protection against exogenous SSTI was not studied. They demonstrated that this protection was mediated by antibody and IL-17A and inhibited by IFN-γ as shown by antibody transfer to naive mice and neutralization of IL-17A or IFN-γ prior to infection, respectively. While in their study IgG levels against Hla and IsdB were assessed, the present study in mice included IgG levels against a broad panel of 25 S. aureus antigens. Future studies in mice on the effect of immunization targeting IsaA, Nuc, PrsA, WTA, Efb, LukD and LukE prior to the induction of S. aureus bacteremia may shed further light on the protective role of these anti-staphylococcal IgGs in bacteremia. In addition to these antigens, antibodies against S. aureus antigens not included in the present study may also be associated with protection against S. aureus bacteremia. Further insight may be obtained from adoptive antibody transfer studies.
Next to the potential role of pre-bacteremia anti-staphylococcal antibodies, components of cellular immunity are expected to contribute as well to the improvement of the animal survival rate in mice with endogenous S. aureus bacteremia, as the cellular immune response has a role in S. aureus infections [16, 27, 28]. Regarding the role of cellular immunity in reduction of S. aureus bacteremia-related mortality, conclusions cannot be drawn from the present study which was focused on the humoral immune response prior to S. aureus bacteremia. However Montgomery et al. [16] showed that in their model of SSTI protection against the second skin infection in BALB/c mice was mediated by both antibody and IL-17A. It would be very interesting to investigate the role of IL-17A and other components of cellular immunity in the S. aureus bacteremia model used in the present study.
In addition to pre-bacteremia immune responses, the consequences of exposure to S. aureus in the intestines and nasopharynx following S. aureus skin infection may also contribute to the improvement of the animal survival rate. As differences in number of intestine or nasopharynx culture positive mice were not observed between the groups, no conclusions can be drawn on the immunological relevance of colonization of these sites. As quantitative cultures from the intestinal and nasopharyngeal flora were not performed, definite conclusions on the role of intestinal and nasopharyngeal colonization cannot be drawn, but this merits further investigation.
In conclusion, we show that S. aureus isolate P skin infection prior to S. aureus bacteremia improved the outcome of endogenous invasive infection. Improved animal survival rates may be associated with the elevated levels of anti-staphylococcal IgGs against specified antigens. The observation that anti-S. aureus IgG may contribute to improvement of the course and outcome of endogenous S. aureus bacteremia opens new perspectives to investigate the protective capacity of active and passive immunization as a non-antibiotic-based treatment regimen in patients with S. aureus bacteremia. Further studies using other S. aureus strains are needed to generalize and support our conclusion that S. aureus skin infection improves the course of subsequent endogenous S. aureus bacteremia. In this respect, also the role of cellular immunity should be further investigated.
Acknowledgments
We thank M.T. ten Kate and G.J. de Knegt for their technical assistance in animal experiments. We would also like to thank all research groups who kindly provided the recombinant staphylococcal antigens used for the Luminex assay described in this manuscript. T. Bosma (BiOMaDe Technology Foundation, Groningen, the Netherlands) supplied ClfA. J.I. Flock (Karolinska Institutet, Stockholm, Sweden) provided Efb [29]. EsxA, EsxB, FLIPr, lipase, PG, PrsA, SA0104, SSL10, and WTA were obtained from K.P.M. van Kessel (University Medical Center Utrecht, Utrecht, the Netherlands) [30]. G. Buist (University of Groningen, University Medical Center Groningen, Groningen, the Netherlands) supplied IsaA, LytM, and Nuc [18]. SSL1, SSL3, and SSL5 were a kind gift of J.D. Fraser (University of Auckland, Auckland, New Zealand) [31].
Data Availability
All relevant data are within the paper.
Funding Statement
bioMérieux provided support for this work in the form of salaries for author Alex van Belkum, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific role of this author is articulated in the ‘author contributions’ section.
References
- 1. Nouwen JL, Ott A, Kluytmans-Vandenbergh MF, Boelens HA, Hofman A, van Belkum A, et al. Predicting the Staphylococcus aureus nasal carrier state: derivation and validation of a "culture rule". Clin Infect Dis. 2004;39(6):806–11. Epub 2004/10/09. 10.1086/423376 . [DOI] [PubMed] [Google Scholar]
- 2. Williams RE. Healthy carriage of Staphylococcus aureus: its prevalence and importance. Bacteriol Rev. 1963;27:56–71. Epub 1963/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997;10(3):505–20. Epub 1997/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998;339(8):520–32. Epub 1998/08/26. 10.1056/NEJM199808203390806 . [DOI] [PubMed] [Google Scholar]
- 5. Kluytmans JA, Mouton JW, Ijzerman EP, Vandenbroucke-Grauls CM, Maat AW, Wagenvoort JH, et al. Nasal carriage of Staphylococcus aureus as a major risk factor for wound infections after cardiac surgery. J Infect Dis. 1995;171(1):216–9. Epub 1995/01/01. . [DOI] [PubMed] [Google Scholar]
- 6. Muñoz P, Hortal J, Giannella M, Barrio JM, Rodríguez-Créixems M, Pérez MJ, et al. Nasal carriage of S. aureus increases the risk of surgical site infection after major heart surgery. J Hosp Infect. 2008;68(1):25–31. Epub 2007/10/20. doi: S0195-6701(07)00272-1 [pii] 10.1016/j.jhin.2007.08.010 . [DOI] [PubMed] [Google Scholar]
- 7. Calia FM, Wolinsky E, Mortimer EA Jr., Abrams JS, Rammelkamp CH Jr. Importance of the carrier state as a source of Staphylococcus aureus in wound sepsis. J Hyg (Lond). 1969;67(1):49–57. Epub 1969/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weinstein HJ. The relation between the nasal-staphylococcal-carrier state and the incidence of postoperative complications. N Engl J Med. 1959;260(26):1303–8. Epub 1959/06/25. 10.1056/NEJM195906252602601 . [DOI] [PubMed] [Google Scholar]
- 9. Williams RE, Jevons MP, Shooter RA, Hunter CJ, Girling JA, Griffiths JD, et al. Nasal staphylococci and sepsis in hospital patients. Br Med J. 1959;2(5153):658–62. Epub 1959/10/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wertheim HF, Vos MC, Ott A, van Belkum A, Voss A, Kluytmans JA, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet. 2004;364(9435):703–5. . [DOI] [PubMed] [Google Scholar]
- 11. von Eiff C, Becker K, Machka K, Stammer H, Peters G. Nasal carriage as a source of Staphylococcus aureus bacteremia. N Engl J Med. 2001;344(1):11–6. Epub 2001/01/04. 10.1056/NEJM200101043440102 . [DOI] [PubMed] [Google Scholar]
- 12. Verkaik NJ, de Vogel CP, Boelens HA, Grumann D, Hoogenboezem T, Vink C, et al. Anti-staphylococcal humoral immune response in persistent nasal carriers and noncarriers of Staphylococcus aureus . J Infect Dis. 2009;199(5):625–32. 10.1086/596743 [DOI] [PubMed] [Google Scholar]
- 13. Clarke SR, Brummell KJ, Horsburgh MJ, McDowell PW, Mohamad SA, Stapleton MR, et al. Identification of in vivo-expressed antigens of Staphylococcus aureus and their use in vaccinations for protection against nasal carriage. J Infect Dis. 2006;193(8):1098–108. . [DOI] [PubMed] [Google Scholar]
- 14. Dryla A, Prustomersky S, Gelbmann D, Hanner M, Bettinger E, Kocsis B, et al. Comparison of antibody repertoires against Staphylococcus aureus in healthy individuals and in acutely infected patients. Clin Diagn Lab Immunol. 2005;12(3):387–98. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kolata J, Bode LG, Holtfreter S, Steil L, Kusch H, Holtfreter B, et al. Distinctive patterns in the human antibody response to Staphylococcus aureus bacteremia in carriers and non-carriers. Proteomics. 2011;11(19):3914–27. Epub 2011/08/02. 10.1002/pmic.201000760 . [DOI] [PubMed] [Google Scholar]
- 16. Montgomery CP, Daniels M, Zhao F, Alegre ML, Chong AS, Daum RS. Protective immunity against recurrent Staphylococcus aureus skin infection requires antibody and interleukin-17A. Infect Immun. 2014;82(5):2125–34. Epub 2014/03/13. doi: IAI.01491-14 [pii] 10.1128/IAI.01491-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Novick R. Properties of a cryptic high-frequency transducing phage in Staphylococcus aureus . Virology. 1967;33(1):155–66. Epub 1967/09/01. doi: 0042-6822(67)90105-5 [pii]. . [DOI] [PubMed] [Google Scholar]
- 18. Ziebandt AK, Kusch H, Degner M, Jaglitz S, Sibbald MJ, Arends JP, et al. Proteomics uncovers extreme heterogeneity in the Staphylococcus aureus exoproteome due to genomic plasticity and variant gene regulation. Proteomics. 2010;10(8):1634–44. 10.1002/pmic.200900313 [DOI] [PubMed] [Google Scholar]
- 19. Brown EL, Dumitrescu O, Thomas D, Badiou C, Koers EM, Choudhury P, et al. The Panton-Valentine leukocidin vaccine protects mice against lung and skin infections caused by Staphylococcus aureus USA300. Clin Microbiol Infect. 2009;15(2):156–64. 10.1111/j.1469-0691.2008.02648.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Melles DC, Schouls L, Francois P, Herzig S, Verbrugh HA, van Belkum A, et al. High-throughput typing of Staphylococcus aureus by amplified fragment length polymorphism (AFLP) or multi-locus variable number of tandem repeat analysis (MLVA) reveals consistent strain relatedness. Eur J Clin Microbiol Infect Dis. 2009;28(1):39–45. Epub 2008/07/30. 10.1007/s10096-008-0585-4 . [DOI] [PubMed] [Google Scholar]
- 21. van den Berg S, Laman JD, Boon L, ten Kate MT, de Knegt GJ, Verdijk RM, et al. Distinctive cytokines as biomarkers predicting fatal outcome of severe Staphylococcus aureus bacteremia in mice. PLoS One. 2013;8(3):e59107 Epub 2013/03/23. 10.1371/journal.pone.0059107 PONE-D-12-35263 [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Verkaik NJ, Dauwalder O, Antri K, Boubekri I, de Vogel CP, Badiou C, et al. Immunogenicity of toxins during Staphylococcus aureus infection. Clin Infect Dis. 2010;50(1):61–8. 10.1086/648673 [DOI] [PubMed] [Google Scholar]
- 23. Martins TB, Augustine NH, Hill HR. Development of a multiplexed fluorescent immunoassay for the quantitation of antibody responses to group A streptococci. J Immunol Methods. 2006;316(1–2):97–106. . [DOI] [PubMed] [Google Scholar]
- 24. van den Berg S, Bowden MG, Bosma T, Buist G, van Dijl JM, van Wamel WJ, et al. A multiplex assay for the quantification of antibody responses in Staphylococcus aureus infections in mice. J Immunol Methods. 2011;365(1–2):142–8. Epub 2010/12/28. doi: S0022-1759(10)00390-X [pii] 10.1016/j.jim.2010.12.013 . [DOI] [PubMed] [Google Scholar]
- 25. Verkaik N, Brouwer E, Hooijkaas H, van Belkum A, van Wamel W. Comparison of carboxylated and Penta-His microspheres for semi-quantitative measurement of antibody responses to His-tagged proteins. J Immunol Methods. 2008;335(1–2):121–5. Epub 2008/04/18. doi: S0022-1759(08)00085-9 [pii] 10.1016/j.jim.2008.02.022 . [DOI] [PubMed] [Google Scholar]
- 26. den Reijer PM, Lemmens-den Toom N, Kant S, Snijders SV, Boelens H, Tavakol M, et al. Characterization of the humoral immune response during Staphylococcus aureus bacteremia and global gene expression by Staphylococcus aureus in human blood. PLoS One. 2013;8(1):e53391 Epub 2013/01/12. 10.1371/journal.pone.0053391 PONE-D-12-25651 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Murphy AG, O'Keeffe KM, Lalor SJ, Maher BM, Mills KH, McLoughlin RM. Staphylococcus aureus infection of mice expands a population of memory γδ T cells that are protective against subsequent infection. J Immunol. 2014;192(8):3697–708. Epub 2014/03/14. doi: jimmunol.1303420 [pii] 10.4049/jimmunol.1303420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brown AF, Leech JM, Rogers TR, McLoughlin RM. Staphylococcus aureus colonization: Modulation of host immune response and impact on human vaccine design. Front Immunol. 2014;4:507 Epub 2014/01/11. 10.3389/fimmu.2013.00507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shannon O, Uekotter A, Flock JI. Extracellular fibrinogen binding protein, Efb, from Staphylococcus aureus as an antiplatelet agent in vivo . Thromb Haemost. 2005;93(5):927–31. . [DOI] [PubMed] [Google Scholar]
- 30. Prat C, Bestebroer J, de Haas CJ, van Strijp JA, van Kessel KP. A new staphylococcal anti-inflammatory protein that antagonizes the formyl peptide receptor-like 1. J Immunol. 2006;177(11):8017–26. Epub 2006/11/23. doi: 177/11/8017 [pii]. . [DOI] [PubMed] [Google Scholar]
- 31. Chung MC, Wines BD, Baker H, Langley RJ, Baker EN, Fraser JD. The crystal structure of staphylococcal superantigen-like protein 11 in complex with sialyl Lewis X reveals the mechanism for cell binding and immune inhibition. Mol Microbiol. 2007;66(6):1342–55. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.