Abstract
Background
A growing literature addresses the need to reduce cigarette smoking prevalence by increasing the use of assistance when quitting. A key focus is to identify strategies for enhancing adoption of effective interventions in order to increase utilization of evidence-based treatments.
Purpose
To examine the effect of beliefs regarding ability to quit on utilization of assistance for smoking cessation. A mediation model was hypothesized whereby the relationship between smoking and use of assistance is influenced by beliefs in ability to quit.
Methods
The present study includes 474 of 1000 respondents to baseline and follow-up California Smokers Cohort surveys conducted from 2011 to 2013. Included were baseline smokers who reported a 24-h quit attempt at follow-up. Baseline variables were used to predict use of assistance when quitting. Results: The hypothesized model was tested using a product of coefficients method, controlling for demographics. Greater heaviness of smoking and lower belief in ability to quit were significantly related to use of assistance. Quitting beliefs significantly mediated the relationship between nicotine dependence and use of assistance.
Conclusions
The present data support a mechanism whereby the effect of smoking rate on treatment utilization is mediated by beliefs in ability to quit. Greater belief in one's ability to quit may represent an obstacle to treatment utilization by reducing the likelihood of successful cessation. The present findings suggest the value of targeted messages from health care providers that normalize the need for assistance when attempting to change an addictive behavior and emphasize the difficulty of quitting without assistance.
Keywords: Tobacco treatment, Smoking cessation, Tobacco control, Treatment utilization
1. Introduction
1.1. Smoking cessation treatment utilization
A growing literature addresses the need to reduce cigarette smoking prevalence by increasing the use of assistance when attempting to quit (Abrams et al., 2010; Backinger et al., 2010; Orleans et al., 2010). A key focus is to identify strategies for enhancing adoption of effective interventions in order to increase the proportion of quitters who employ evidence-based treatments during cessation attempts. Assisted quitting refers to utilization of evidence-based strategies such as medication or behavioral counseling (Fiore et al., 2008; Kotz et al., 2009) when trying to quit smoking. Studies addressing treatment utilization indicate that the majority of quit attempts are unassisted, with a small minority employing behavioral and pharmaceutical assistance simultaneously (Edwards et al., 2014; Shiffman et al., 2008a; Zhu et al., 2000). Unassisted quitting, where the smoker does not employ any evidence-based treatment, is thus the norm, despite better cessation outcomes when using smoking cessation assistance (Fiore et al., 2008; Mottillo et al., 2009; Piper et al., 2009). Highlighting the potential value of assisted quitting, a recent observational study found that smokers in England who used both pharmaceutical and behavioral assistance had significantly better outcomes than those who did not use any assistance or used only one form of treatment (Kotz et al., 2014). This finding is consonant with current clinical treatment guidelines (Fiore et al., 2008) and prior evidence for improved outcomes when treatment involves a combination of medication and behavioral counseling (Stead and Lancaster, 2012a,b).
1.2. Characteristics of smokers using assistance
At this time, little is known regarding smoker characteristics associated with the use of assistance when attempting to quit smoking. Such knowledge may serve to guide strategies for increasing smoking cessation treatment utilization. Relatively consistent findings emerge indicating that use of assistance is associated with higher levels of dependence, female sex, increasing age and White ethnicity (Kotz et al., 2009; Shiffman et al., 2008b; Zhu et al., 2000). In addition, cognitions and beliefs have been found related with treatment utilization. Lack of accurate knowledge regarding the effectiveness for various forms of treatment has been identified as a barrier in studies of attitudes toward using assistance (Carpenter et al., 2011; Foulds et al., 2009; Narayanan et al., 2009; Vogt et al., 2010). For example, beliefs that nicotine replacement medications (NRT) may be harmful, and overestimates of ability to quit successfully without assistance have been cited as reasons smokers may not utilize medications for quitting (Foulds et al., 2009). On the other hand, use of assistance has been found to be associated with lower self-efficacy for quitting and positive beliefs regarding the usefulness of treatment (Weber et al., 2007). However, beliefs as barriers to treatment have been examined only in relation to attitudes toward assistance (e.g., self-reported likelihood of utilizing assistance) rather than with actual behaviors.
1.3. Present study
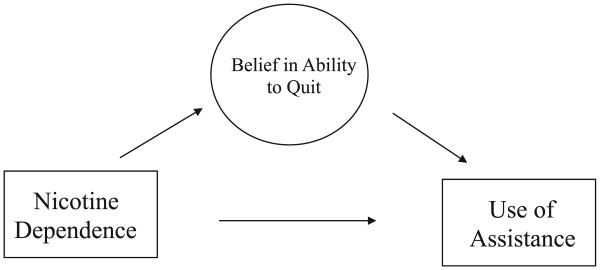
Despite the acknowledged importance of this issue, no longitudinal studies predicting use of assistance during smoking cessation attempts were identified. To address this issue, the present study examined baseline predictors of utilizing assistance in a subsequent smoking cessation attempt in a sample of California smokers. Based on evidence from cross-sectional research, it was hypothesized that, after accounting for demographic variables, more heavily dependent smokers would be more likely to utilize assistance. Based on findings regarding influences on attitudes toward treatment (Foulds et al., 2009; Weber et al., 2007) it was also predicted that beliefs regarding one's ability to quit would mediate the relationship between heaviness of smoking and use of assistance (see Fig. 1). Specifically, it was hypothesized that the relationship between heavy smoking and increased utilization reflects lower belief in ability to quit.
Fig.1.
Hypothesized mediating model for relationship of nicotine dependence with use of assistance during a quit attempt.
2. Materials and methods
2.1. Sample
The data for the present study are from the California Smokers Cohort (CSC) conducted from 2011 to 2013. The CSC was a population-based survey of a sample of adults in California who reported smoking 100 cigarettes in their lifetime. The study included a baseline survey (conducted from July, 2011 to April, 2012) to establish a cohort o f current and former smokers, and a follow-up survey (conducted from November, 2012 to January, 2013) to examine changes in smoking behaviors. The sample was identified through a random-digit-dial (RDD) survey of California households to screen for tobacco use; respondents who had smoked at least 100 cigarettes in their lifetime were administered the baseline survey (n = 4350). Of the 1745 eligible smokers and former smokers from the CSC baseline survey cohort who also completed a follow-up survey, 1000 adults were smokers at baseline. Analyses in the current study included 474 of the 1000 respondents who completed both the baseline and follow-up surveys and reported a 24-h quit attempt during the prior year at the follow-up survey. Interviews were conducted in both English and Spanish over landline and cellular telephones. Survey procedures were approved by the University of California, San Diego Human Research Protection Program. Participants provided free and informed consent for their participation.
2.2. Survey items
2.2.1. Baseline predictors
2.2.1.1. Quit attempt
Included in the present sample were respondents who at follow-up reported quitting smoking intentionally for one day or longer in the past year. The 24-h duration is commonly used in the literature to define a quit attempt (USDHS, 1999) and was employed here to denote an intentional effort to stop smoking.
2.2.1.2. The Heavy Smoking Index
(HSI; Heatherton et al., 1989). The Heavy Smoking Index (HSI; Heatherton et al., 1989) was used to represent nicotine dependence. The index is composed of two items, number of cigarettes per day and time to first cigarette, each scored from 0 to 3 based on the Fagerstrom Test for Nicotine Dependence criteria (Heatherton et al., 1991). The HSI is found to have high concordance with the Fagerstom Test for Nicotine Dependence (Chabrol et al., 2005) and is considered a good brief screen for high nicotine dependence (Perez-Rios et al., 2009).
2.2.1.3. Quitting attitudes/belief variables
Four items representing beliefs regarding ability to quit smoking, behavioral and addiction impediments to quitting, and belief in ability to quit without pharmaceuticals were selected from the survey based on content reflecting an aspect of beliefs in quitting. Each item was scored as a dichotomy reflecting more belief in one's ability to quit. The first item was a standard self-efficacy question: “How sure are you that you [could/can] refrain from smoking for at least [one/one more] month?” This item had 4 response items (very sure, somewhat sure, somewhat unsure, very unsure). Responses were dichotomized to conform to the scaling of other belief items(very sure/somewhat sure = 1;somewhat unsure/unsure = 0).
The second item was drawn from a set of 6 questions designed to assess smokers beliefs regarding NRT's: “Smokers can quit on their own without any pharmaceutical aids.” This item presented two options and was scored as ‘agree’ = 1 or ‘disagree’ = 0. The final 2 items were drawn from a scale examining perceived reasons for why respondents are still smoking and were scored ‘yes’ = 0 or ‘no’ = 1: “You’re still smoking because: Your cravings for cigarettes are too strong.” “…It has become a routine that would be really hard for you to break.” These items were selected to represent difficulty quitting attributed to physical and psychological addiction.
A nonparametric item response model (Ramsay, 1991) was employed to evaluate the assumption that the probability of higher scores increased along with greater belief in ability to quit. Option characteristic curves suggested that when item scores were dichotomized the probability of endorsing each item grew consistently with increasing levels of total beliefs. Point-biserial item-total correlations ranged from 0.53 to 0.71 and supported the strength of each items' association with a common construct. With support for the construct validity and adequate reliability for this brief scale these four items were summed into a quitting beliefs scale, with higher scores reflecting greater belief in one's ability to quit.
2.2.2. Baseline covariates
Gender, ethnicity, age, and education were employed as demographic control variables given evidence in prior studies for differences in utilization rates. Because of the small sample size ethnicity was dichotomized to reflect non-Hispanic White in one category and Hispanic plus other non-White ethnic groups in the other. Age and education were each recoded into three categories (respectively: 18–24, 25–44, 45 and older; high school or less, some college and college; and postgraduate).
2.2.3. Dependent variable
A composite variable was created to indicate use of any type of assistance during the follow-up quit attempt. The assistance items were asked for their most recent quit attempt. Respondents were coded as having used assistance in their most recent quit attempt if they responded “yes” to any of the following 3 items:
For this last quit attempt, did you use a nicotine replacement therapy such as nicotine patch, nicotine gum, nicotine inhaler, nicotine lozenge.
For this last quit attempt, did you use a prescription pill to help you to quit such as Zyban, Prozac, Chantix.
Did you use counseling advice or self-help materials to adjust to life without cigarettes?
2.3. Analysis
Univariate analyses were conducted to examine whether (a) covariates were related to use of assistance, and (b) whether hypothesized relationships were evident between predictor, mediator and use of assistance.
The hypothesized mediating model was tested using regression models, controlling for covariates. Using a product of coefficients method (MacKinnon et al., 2007, 2002) first, the relationship between level of dependence and quitting beliefs (path ‘a’) was estimated and second, the association between level of quitting belief and the likelihood of using assistance (path ‘b’) was estimated. The product of path ‘a’ and path ‘b’ provided an estimate of the indirect or mediating effect of beliefs in explaining an association between dependence and use of assistance.
3. Results
The sample of 474 California smokers was comprised of 53.4% female; 11.4% Hispanic, 66.7% non-Hispanic White, 10.1% African American, 3.2% Asian, and 8.6% mixed/other ethnicity. Age of participants ranged from 18 to 59, average = 46.02 (11.49).
Of the survey participants who reported a quit attempt at follow-up, 208 (43.9%) reported use of any form of assistance during their most recent attempt. Use of assistance was distributed as follows: 31.9% NRT, 13.3% other medications, and 19.4% counseling or self-help. Collectively, 25.1% used NRT or medications only, 13.9% used medications and counseling or self-help and 5.5% used counseling or self-help only.
As shown in Table 1, gender was the only demographic variable that differed significantly across use of assistance, with females more likely than males to use assistance (X2(df = 1)=6.17, p = .013). There was a trend whereby a greater proportion of older smokers used assistance during their most recent quit attempt (p = .099). No differences were observed for ethnicity or education. As predicted, greater heaviness of smoking and lower beliefs in ability to quit were significantly related with the use of assistance during a quit attempt (p's < .001).
Table 1.
Baseline characteristics comparing those who did use versus did not use assistance for quitting.
| Used assistance | Did not use assistance | p | |
|---|---|---|---|
| Gender (N = 464) | |||
| %female | 59.6 | 48.0 | .013 |
| Ethnicity (N = 464) | |||
| % non-Hispanic White | 34.4 | 31.3 | .476 |
| Age (N = 464) | .099 | ||
| % 18–24 | 4.3 | 7.4 | |
| % 25–44 | 25.0 | 30.9 | |
| % 45–59 | 70.7 | 61.7 | |
| Education (N = 464) | .818 | ||
| % high school or less | 31.3 | 32.8 | |
| % some college | 62.0 | 59.4 | |
| % postgraduate | 6.7 | 7.8 | |
| HSI score (N = 463) | 2.37 (1.37) | 1.62 (1.38) | <.001 |
| Quitting beliefs score (N = 448) | 1.58 (1.10) | 2.31 (1.30) | <.001 |
The hypothesized mediating model was tested (see Table 2), controlling for gender, age, ethnicity and education. In a linear regression model, higher scores on the HSI were significantly related to lower beliefs in ability to quit (b = −0.11, SE =.05). Similarly, lower beliefs in ability to quit were significantly related to an increased likelihood of using assistance (b = −0.51, SE = 0.09) after adjusting for levels of dependence. A bootstrap confidence interval for the product of coefficients (PRODCLIN; To fighi and MacKinnon, 2011) was used to test the mediation effect(a * b = 0.06, 95%CI = ;−0.12 to −0.01)indicating that quitting beliefs significantly mediated the relationship between nicotine dependence and use of assistance. Thus, the relationship where by higher nicotine dependence is associated with greater likelihood of using assistance is in part explained by lower perceived ability to quit smoking.
Table 2.
Associations between baseline level of beliefs in ability to quit and likelihood of using assistance during subsequent quit attempt (N = 448).
| Level of beliefs | Likelihood of using assistance | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Coef. | S.E. | Pr (>|t|) | Coef. | S.E. | Pr (>|t|) | |
| Age 18–24 | – | – | – | – | ||
| Age 25–44 | −0.55 | 0.25 | 0.03 | -0.10 | 0.47 | 0.83 |
| Age 45–59 | −0.60 | 0.24 | 0.01 | 0.18 | 0.45 | 0.69 |
| Male | – | – | – | |||
| Female | −0.20 | 0.11 | 0.08 | 0.34 | 0.21 | 0.10 |
| White | – | – | – | – | ||
| Non-White | 0.05 | 0.12 | 0.68 | 0.06 | 0.22 | 0.79 |
| Less than college | – | – | – | – | ||
| Some college/college | 0.19 | 0.12 | 0.12 | 0.37 | 0.23 | 0.11 |
| Graduate | 0.39 | 0.23 | 0.09 | 0.44 | 0.43 | 0.31 |
| Heaviness of smoking (HIS) | −0.11 | 0.05 | 0.034 | 0.20 | 0.97 | 0.04 |
| Beliefs about quitting | – | – | -0.51 | 0.09 | <0.0001 | |
4. Discussion
4.1. Findings
The present longitudinal study examined a hypothesized mechanism whereby the relationship between heaviness of smoking and use of assistance when quitting is mediated by beliefs in ability to quit. Heavier smoking and lower belief in ability to quit predicted use of assistance. Beliefs in ability to quit mediated the relationship between heavy smoking and assistance, providing evidence for the role of these cognitions in treatment utilization.
That heavier smokers are more likely to utilize treatment is consonant with previous research (Kotz et al., 2009; Shiffman et al., 2008a,b; Zhu et al., 2000). Higher dependence on nicotineis consistently associated with smoking cessation failure (Fiore et al., 2008; Ip et al., 2012; Vangeli et al., 2011), suggesting that heavier smokers are more likely to have made previous, unsuccessful, cessation attempts. Existing evidence indicates that a lapse to smoking after attempting cessation results in decreased self-efficacy for quitting (Shiffman et al., 1997). Accordingly, previous failures at cessation may increase receptivity to assistance in subsequent attempts through decreased self-efficacy for quitting and diminished belief in ability to quit without assistance.
The belief in ability to quit scale constructed for this study includes items that capturea range of cognitions related to quitting ability. The self-efficacy item and belief in ability to quit without medications directly tap into confidence in ability to quit. In addition, the items assessing continued smoking because of cravings and behavioral routines may capture perceptions of greater physical and behavioral addiction to tobacco, thus less perceived control over the behavior. The fact that scale scores indicating lower belief in ability to quit predict use of assistance when quitting is consistent with the few previous studies that have examined these factors in relation to attitudes toward treatment (Foulds et al., 2009; Weber et al., 2007). Conversely, smokers with greater beliefs in their ability to quit are less likely to utilize assistance. This longitudinal analysis provides empirical evidence for this mechanism and thus adds support to the importance of directly challenging beliefs that may impede use of assistance. For example, while less dependent smokers may be more likely to succeed quitting unassisted than those more heavily addicted, evidence indicates better outcomes for assisted quitting efforts across levels of dependence (Kotz et al., 2014). As such, messages that normalize the need for assistance when attempting to change an addictive behavior, and emphasize the difficulty of quitting without assistance may serve to increase treatment utilization.
As in previous studies (Edwards et al., 2014; Shiffman et al., 2008a,b; Zhu et al., 2000), only a small proportion of the sample reported using medication in combination with counseling or self-help assistance. Among medications, NRTs are most widely used because of their over-the-counter availability the U.S. and other countries (Walsh, 2008). However, findings regarding the efficacy of NRTs in population-based studies are equivocal (Alpert et al., 2013; West and Zhou, 2007), with some suggesting a lack of “real world” efficacy may reflect that smokers use NRTs without additional supports for quitting (Walsh, 2008). Consistent with the former assertion, a recent population-based study found use of NRTs without behavioral assistance was comparable to unassisted quitting, and both were significantly inferior to combined use of pharmacological and behavioral assistance (Kotz et al., 2014). The present findings highlight the need for health care providers to educate and encourage smokers to utilize combined behavioral and pharmacological assistance when quitting.
Previous, larger scale studies have identified men, younger and non-White smokers as less likely to use assistance when quitting (Kotz et al., 2009; Shiffman et al., 2008a,b; Zhu et al., 2000). In the present sample, only gender differed significantly between those who did and did not utilize assistance. The failure to identify other demographic differences may reflect the small sample size or other characteristics of the present study. Further work to identify subgroups disproportionately less likely to use quitting assistance is needed to guide health care provider efforts to combat beliefs and attitudes that inhibit the use of assistance when quitting.
4.2. Limitations
Limitations to the present study include sample and survey item content. Participants in the present study were not selected to represent the population, limiting generalizability of these findings. The small sample size precluded more fine-grained analyses, such as evaluation of this model in relation to different types of assistance. In addition, a combined “Hispanic and non-White” category was utilized that may obscure ethnic and cultural differences. However, the longitudinal design increases confidence in the findings. A single item was used to assess counseling and self-help strategies, thus limiting the ability to determine the extent to which affirmative responses reflected use of behavioral counseling. Use of assistance was assessed only in relation to the most recent quit attempt at follow-up. Thus, participants who made multiple attempts could have made other assisted or unassisted attempts. However, the robust effects observed in the analyses suggest this is not a significant concern. Having ever previously used quitting assistance may have influenced use of assistance for the quit attempts examined in the analyses, however this was not assessed as part of the baseline questionnaire. Similarly, we were unable to ascertain the number of prior failed attempts for participants, another factor that may influence the observed relationships. The belief in ability to quit scale was composed of items originally designed for other purposes. However, the items address a range of factors relevant to this construct, and the analytic basis for creating the scale supports its validity. The present study evaluated a mediating model, yet other relationships may also exist between the variables examined. To this end post hoc analyses were conducted (not reported) to examine moderating effects for which no significant interactions emerged. Finally, other factors found to serve as barriers to treatment utilization, such as cost and availability of medications (Foulds et al., 2009) were not considered in the present study.
4.3. Conclusions
In summary, results of the present study provide information regarding the complex factors that influence whether smokers choose to employ assistance during a quit attempt. To date few studies have examined individual characteristics that distinguish those who do or do not use assistance, and this may be the first longitudinal study to do so. The present data provide support for a mechanism whereby beliefs in ability to quit play a key role in predicting the use of assistance. It appears that smokers with greater belief in their ability to quit are less likely to utilize assistance. Individualized messages by health care providers targeted to counter these beliefs may prove a useful strategy for enhancing utilization of assistance.
Acknowledgments
The authors would like to thank the California Department of Health for supporting this research.
Role of funding source: The California Department of Health had a role in selection of survey items. The study sponsor had no role in any other aspect of the present report.
Footnotes
Conflict of interest: No financial disclosures were reported by the authors of this paper
Contributors: Mark Myers conceived of and drafted the manuscript, guided the data analysis and interpretation of findings. David Strong contributed to study conceptualization, conducted the data analyses contributed to interpretation of findings and writing. Sarah Linke and Richard Hofstetter contributed to interpretation of findings and writing. Wael Al Delaimy guided the study design contributed to study conceptualization, interpretation and writing.
References
- Abrams DB, Graham AL, Levy DT, Mabry PL, Orleans CT. Boosting population quits through evidence-based cessation treatment and policy. Am J Prev Med. 2010;38:S351–S363. doi: 10.1016/j.amepre.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpert HR, Connolly GN, Biener L. A prospective cohort study challenging the effectiveness of population-based medical intervention for smoking cessation. Tob Control. 2013;22:32–37. doi: 10.1136/tobaccocontrol-2011-050129. [DOI] [PubMed] [Google Scholar]
- Backinger CL, Thornton-Bullock A, Miner C, Orleans CT, Siener K, DiClemente CC, Phillips TM, Rowden JN, Arkin E. Building consumer demand for tobacco-cessation products and services: the National Tobacco Cessation Collaborative's Consumer Demand Roundtable. Am J Prev Med. 2010;38:S307–S311. doi: 10.1016/j.amepre.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Carpenter MJ, Ford ME, Cartmell K, Alberg AJ. Misperceptions of nicotine replacement therapy within racially and ethnically diverse smokers. J Natl Med Assoc. 2011;103:885–894. doi: 10.1016/s0027-9684(15)30444-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabrol H, Niezborala M, Chastan E, de Leon J. Comparison of the Heavy Smoking Index and of the Fagerstrom Test for Nicotine Dependence in a sample of 749 cigarette smokers. Addict Behav. 2005;30:1474–1477. doi: 10.1016/j.addbeh.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Edwards S, Bondy SJ, Callaghan RC, Mann RE. Prevalence of unassisted quit attempts in population-based studies: a systematic review of the literature. Addict Behav. 2014;39:512–519. doi: 10.1016/j.addbeh.2013.10.036. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, Dorfman SF, Froelicher ES, Goldstein MG, Healton CG, Henderson PN, Heyman RB, Koh HK, Lando HA, Mecklenburg RE, Mermelstein RJ, Mullen PD, Orleans CT, Robinson L, Stitzer ML, Tommasello AC, Villejo L, Wewers ME. Treating Tobacco Use and Dependence: 2008 Update Clinical Practice Guideline. U.S. Department of Health and Human Services, Public Health Service; Rockville, MD: 2008. [Google Scholar]
- Foulds J, Hughes J, Hyland A, Le Houezec J, McNeill A, Melvin C, Okuyemi K, Shiffman S, Wassum K, Williams LN, Zeller M. Barriers to use of FDA-approved smoking cessation medications:implications for policy action. Society for Research on Nicotine and Tobacco; 2009. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84:791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fager-strom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Ip DT, Cohen JE, Bondy SJ, Chaiton MO, Selby P, Schwartz R, McDonald P, Garcia J, Ferrence R. Do components of current ‘hardcore smoker’ definitions predict quitting behaviour? Addiction. 2012;107:434–440. doi: 10.1111/j.1360-0443.2011.03674.x. [DOI] [PubMed] [Google Scholar]
- Kotz D, Fidler J, West R. Factors associated with the use of aids to cessation in English smokers. Addiction. 2009;104:1403–1410. doi: 10.1111/j.1360-0443.2009.02639.x. [DOI] [PubMed] [Google Scholar]
- Kotz D, Brown J, West R. ‘Real-world’ effectiveness of smoking cessation treatments: a population study. Addiction. 2014;109:491–499. doi: 10.1111/add.12429. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottillo S, Filion KB, Belisle P, Joseph L, Gervais A, O'Loughlin J, Paradis G, Pihl R, Pilote L, Rinfret S, Tremblay M, Eisenberg MJ. Behavioural interventions for smoking cessation: a meta-analysis of randomized controlled trials. Eur Heart J. 2009;30:718–730. doi: 10.1093/eurheartj/ehn552. [DOI] [PubMed] [Google Scholar]
- Narayanan S, Ebbert JO, Sood A. Gender differences in self-reported use, perceived efficacy, and interest in future use of nicotine-dependence treatments: a cross-sectional survey in adults at a tertiary care center for nicotine dependence. Gender Med. 2009;6:362–368. doi: 10.1016/j.genm.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Orleans CT, Mabry PL, Abrams DB. Increasing tobacco cessation in America: a consumer demand perspective. Am J Prev Med. 2010;38:S303–S306. doi: 10.1016/j.amepre.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Perez-Rios M, Santiago-Perez MI, Alonso B, Malvar A, Hervada X, de Leon J. Fagerstrom test for nicotine dependence vs heavy smoking index in a general population survey. BMC Public Health. 2009;9:493. doi: 10.1186/1471-2458-9-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fiore MC, Jorenby DE, Fraser D, Baker TB. A randomized placebo-controlled clinical trial of 5 smoking cessation pharmacotherapies. Arch Gen Psychiatry. 2009;66:1253–1262. doi: 10.1001/archgenpsychiatry.2009.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsay JO. Kernel smoothing approaches to nonparametric item characteristic curve estimation. Psykometrica. 1991;56:611–630. [Google Scholar]
- Shiffman S, Hickcox M, Paty JA, Gnys M, Richards T, Kassel JD. Individual differences in the context of smoking lapse episodes. Addict Behav. 1997;22:797–811. doi: 10.1016/s0306-4603(97)00063-4. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. Am J Prev Med. 2008a;34:102–111. doi: 10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Individual differences in adoption of treatment for smoking cessation: demographic and smoking history characteristics. Drug Alcohol Depend. 2008b;93:121–131. doi: 10.1016/j.drugalcdep.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Stead LF, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. CDS Rev. 2012a;10:CD008286. doi: 10.1002/14651858.CD008286.pub2. [DOI] [PubMed] [Google Scholar]
- Stead LF, Lancaster T. Behavioural interventions as adjuncts to pharmacotherapy for smoking cessation. CDS Rev. 2012b;12:CD009670. doi: 10.1002/14651858.CD009670.pub2. [DOI] [PubMed] [Google Scholar]
- Tofighi D, MacKinnon DP. Mediation: an R package for mediation analysis confidence intervals. Behav Res Methods. 2011;43:692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDHS. Cigarette smoking among adults – United States, 1999. Morb Mortal Wkly Rep. 1999;50:869–873. [PubMed] [Google Scholar]
- Vangeli E, Stapleton J, Smit ES, Borland R, West R. Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review. Addiction. 2011;106:2110–2121. doi: 10.1111/j.1360-0443.2011.03565.x. [DOI] [PubMed] [Google Scholar]
- Vogt F, Hall S, Marteau TM. Examining why smokers do not want behavioral support with stopping smoking. Patient Educ Couns. 2010;79:160–166. doi: 10.1016/j.pec.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Walsh RA. Over-the-counter nicotine replacement therapy: a methodological review of the evidence supporting its effectiveness. Drug Alcohol Rev. 2008;27:529–547. doi: 10.1080/09595230802245527. [DOI] [PubMed] [Google Scholar]
- Weber D, Wolff LS, Orleans T, Mockenhaupt RE, Massett HA, Vose KK. Smokers' attitudes and behaviors related to consumer demand for cessation counseling in the medical care setting. Nicotine Tob Res. 2007;9:571–580. doi: 10.1080/14622200701189024. [DOI] [PubMed] [Google Scholar]
- West R, Zhou X. Is nicotine replacement therapy for smoking cessation effective in the real world? Findings from a prospective multinational cohort study. Thorax. 2007;62:998–1002. doi: 10.1136/thx.2007.078758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000;18:305–311. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]