Abstract
Background
Although the importance of the right ventricle (RV) involvement has been known for many years in patients with ST-elevation myocardial infarction (STEMI), it is scarce in non-ST-elevation acute coronary syndrome (NSTE-ACS).
Objectives
We aimed to investigate the effects of urgent percutaneous coronary intervention (PCI) on the RV systolic functions in patients with NSTE-ACS.
Materials and Methods
Ninety-five patients diagnosed with NSTE-ACS and who underwent urgent PCI were prospectively investigated. RV systolic functions were analyzed and compared before and after PCI in all patients by using RV index of myocardial performance (RIMP), tricuspid annular plane systolic excursion (TAPSE), two-dimensional (2D) RV fractional area change (FAC), and isovolumic acceleration (IVA) parameters with transthoracic echocardiography.
Results
Among 95 NSTE-ACS patients, 31 had impaired RIMP, 13 had impaired TAPSE, 8 had decreased 2D FAC, and 32 had impaired IVA values at baseline. There was a significant increase in 2D FAC and IVA values after PCI.
Conclusions
The right ventricular functions may also be affected in patients with NSTE-ACS, and urgent PCI has a significant effect on the recovery of right ventricular systolic functions in patients with NSTE-ACS.
Keywords: isovolumic acceleration, non-ST-elevation acute coronary syndrome, percutaneous coronary intervention, right ventricular index of myocardial performance, tricuspid annular plane systolic excursion, two-dimensional right ventricle fractional area change
Introduction
Right ventricular (RV) dysfunction may be seen as a consequence of right ventricular myocardial infarction (MI) which is seen in about 50% of patients with inferior MI and 10% of patients with anterior MI [1, 2]. Although RV involvement in acute MI usually does not attract enough attention during patient care, it may compromise hemodynamics and play an important prognostic role. Studies aiming to evaluate RV involvement in acute MI have been conducted using different diagnostic approaches including electrocardiography, echocardiography, and radionuclide techniques [1, 3–5]. Most of them aimed to define the prognostic role of RV involvement in acute MI patients who underwent thrombolytic or no reperfusion therapy. Although the importance of the right ventricle has been well known for many years [4, 6] in patients with ST-elevation myocardial infarction (STEMI), the importance of right ventricle in non-ST-elevation acute coronary syndromes (NSTE-ACS) is less known.
In this study, we aimed to investigate the right ventricle systolic functions in patients with NSTE-ACS and the effect of urgent mechanical revascularization on the right ventricle systolic functions.
Methods
Study population
In this prospective nonrandomized study, a total of 95 patients (73 male, mean ± SD age: 59 ± 12.7 years) who were diagnosed with NSTE-ACS based on clinical, laboratory, and electrocardiographic (ECG) parameters upon their admission to Kartal Kosuyolu Heart Training and Research Hospital between November 2012 and February 2013 with the complaint of chest pain and no contraindication for the conventional coronary angiography were included. Physical examination and MI-related basal risk evaluation were performed.
Biochemical assessment
Venous blood samples were taken from each patient upon their admission. Blood glucose, serum creatinine, and troponin I values of each patient were recorded.
Electrocardiographic evaluation
ST-segment depression and T-wave inversion on admission ECG of each patient were evaluated.
Echocardiographic examination
Transthoracic echocardiography was performed in all patients on admission by using Vivid 7 Dimension® (GE Vingmed Ultrasound AS N-3190 Horten, Norway) echocardiography machine. Left ventricular ejection fractions of the patients were calculated by using biplane Simpson’s method.
Evaluation of right ventricular systolic functions
RV systolic functions were analyzed in all patients by calculating right ventricular index of myocardial performance (RIMP), tricuspid annular plane systolic excursion (TAPSE), two-dimensional right ventricle fractional area change (2D RV FAC), and isovolumic acceleration (IVA) parameters.
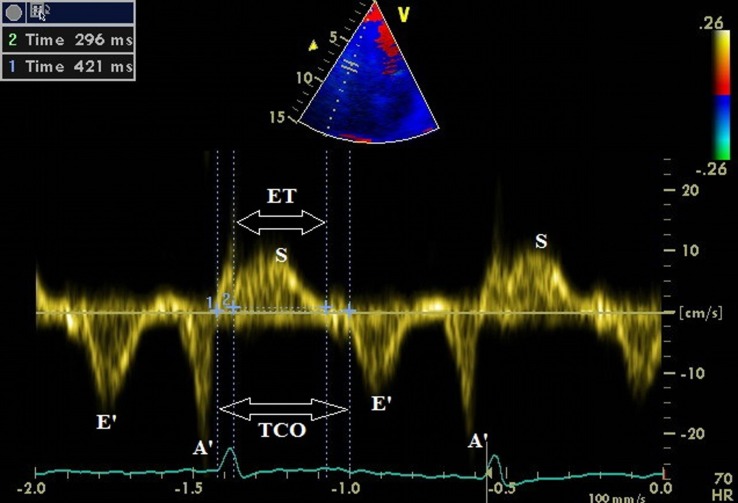
RIMP was obtained by using the pulse wave tissue Doppler method at the lateral tricuspid annulus. Tricuspid valve closure and opening time (TCO) which was measured from the cessation of the A´ wave to the beginning of the E´ wave encompasses isovolumetric contraction time (IVCT), ejection time (ET), and isovolumetric relaxation time (IVRT). Ejection time was measured from the beginning to cessation of systolic ejection wave. RIMP was calculated with the formula: RIMP = (TCO − ET) / ET (Fig. 1).
Fig. 1.
RIMP was obtained by using the pulse wave tissue Doppler method at the lateral tricuspid annulus, with the formula: RIMP = (TCO − ET) / ET
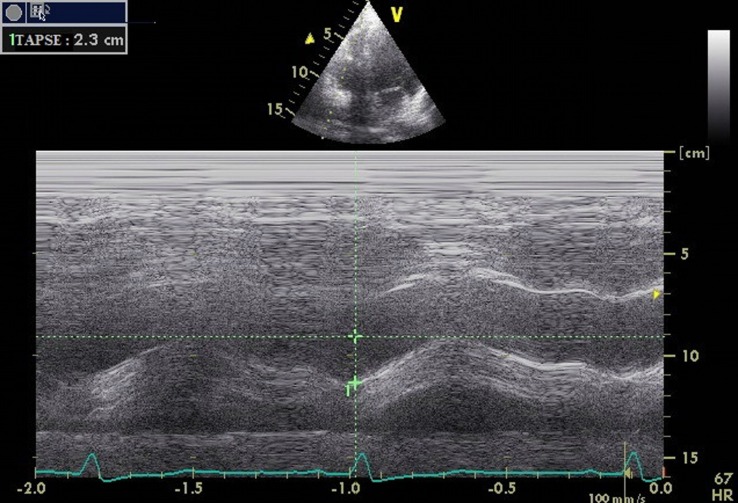
TAPSE was acquired by placing an M-mode cursor through the lateral tricuspid annulus and measuring the amount of longitudinal motion of the annulus at peak systole in the standard apical four-chamber view (Fig. 2).
Fig. 2.
TAPSE was acquired by placing an M-mode cursor through the lateral tricuspid annulus and measuring the amount of longitudinal motion of the annulus at peak systole
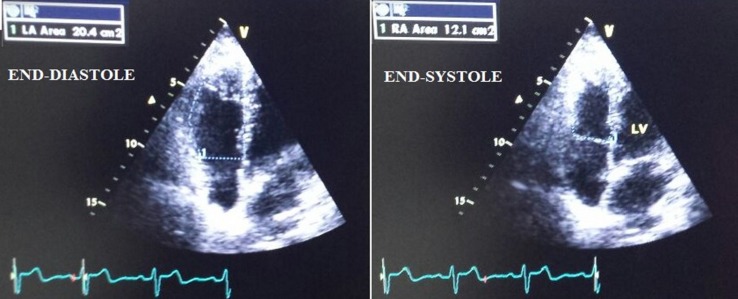
2D RV FAC was obtained by tracing the RV endocardium both in end systole and end diastole from the annulus along with the free wall to the apex and then back to the annulus along with the interventricular septum in the standard apical four-chamber view (Fig. 3).
Fig. 3.
Calculating 2D RV FAC by tracing the RV endocardium both in end systole and end diastole from the annulus along with the free wall to the apex and then back to the annulus along with the interventricular septum in the standard apical four-chamber view. FAC = 100 × (end-diastolic area − end-systolic area) / end-diastolic area
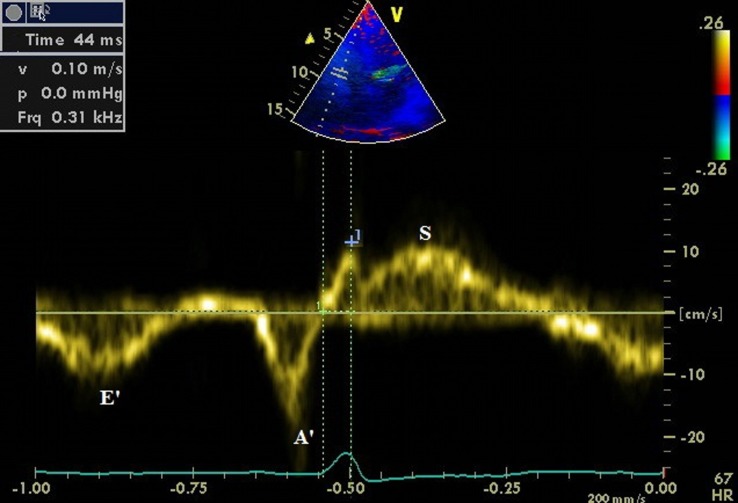
IVA was assessed during isovolumic contraction for the right ventricle by placing pulse wave tissue Doppler at the point where the tricuspid annulus joins the lateral free wall in apical four-chamber view. IVA was calculated by dividing the peak isovolumic velocity, just the wave before the systolic wave on the tissue Doppler trace, by the time to peak velocity (Fig. 4).
Fig. 4.
IVA was calculated by dividing the peak isovolumic velocity, just the wave before the systolic wave on the tissue Doppler trace, by the time to peak velocity
A RIMP value >40%, a TAPSE value <16 mm, a FAC value <35%, and an IVA value <2.2 indicate right ventricular systolic dysfunction [7].
Coronary angiography and PCI
Coronary angiography was performed via transfemoral approach using Siemens Angiocore Machine (Germany) by experienced interventional cardiologists (who perform at least 75 interventional procedures per year) to all patients within 12 h after admission. After coronary angiography, PCI was performed to 56 patients. Prior to the PCI, all patients were administered aspirin (300 mg, oral), clopidogrel (600 mg, oral), and heparin (dose adjusted to body weight).
Comparison of the right ventricular systolic functions before and after PCI
Right ventricular systolic functional analysis was performed again using RIMP, TAPSE, 2D RV FAC, and IVA parameters within 24 h after PCI. Subsequently, these parameters were compared with the baseline parameters before PCI.
Statistical analysis
Statistical analysis was made using the computer software SPSS version 13.0 (SPSS Inc. Chicago, IL, USA). Analysis of numeric variables was performed via Student t-test, Mann–Whitney U-test, while that of categorical variables was performed via chi-square test. Data were expressed as “mean ± standard deviation (SD)” and/or percentage (%). p value <0.05 was considered statistically significant.
Results
Physical examination
KILLIP status of all patients upon admission was recorded. Eighty out of 95 patients had KILLIP class I status, 14 had KILLIP class II, and one had KILLIP class III. Systolic blood pressures and heart rates of all patients were recorded on admission. The mean value of systolic blood pressure was 140.90 ± 24 mm Hg, and the mean heart rate value was 76.9 ± 14.7 beat/min (Table I).
Table I.
Baseline clinical characteristics of study population
| Characteristics | Total (n = 95) | |
|---|---|---|
| Age (year) | 59.0 ± 12.7 | |
| Male/female (n/n) | 73/22 | |
| Fasting glucose (mg/dL) | 141.45 ± 65.57 | |
| Troponin I (mg/dL) | 3.63 ± 7.33 | |
| Serum creatinine (mg/dL) | 0.85 ± 0.19 | |
| KILLIP status, n (%) | I | 80 (84.2) |
| II | 14 (14.7) | |
| III | 1 (1.1) | |
| Heart rate (beat/min) | 76.9 ± 14.7 | |
| Systolic BP (mm Hg) | 140.90 ± 24 | |
Biochemical assessment
The mean blood glucose level was 141.45 ± 65.57 mg/dL. Thirty-five patients had diabetes mellitus. The mean serum creatinine level was 0.85 ± 0.19 mg/dL, and mean troponin I level was 3.63 ± 7.33 mg/dL (Table I).
Electrocardiographic evaluation
There was no remarkable electrocardiographic change in 35 patients. ST-segment depression was present in 46, and T-wave inversion was recorded in 14 patients.
Echocardiographic examination
The mean ejection fraction (EF) of the left ventricle of the study population was calculated as 53.8 ± 10.1. In 37 patients, the left ventricular EF was between 30% and 50% and higher than 50% in remaining 58 patients (Table II).
Table II.
Data from echocardiographic examinations of the study subjects
| Characteristics | Total (n = 95) |
|---|---|
| RIMP (%) | 37.7 ± 17.2 |
| TAPSE (mm) | 19.7 ± 1.1 |
| 2D RV FAC (%) | 44.1 ± 7.6 |
| IVA (m/s2) | 2.7 ± 1.3 |
| EF-Simpson (%) | 53.8 ± 10.1 |
| ≥50% | 58 (61%) |
| <50% | 37 (39%) |
Right ventricular systolic functions of the study population
The mean RIMP value of all patients was 37.7 ± 17.2 (%), the mean value of TAPSE was calculated as 19.7 ± 1.1 mm, the mean value of 2D RV FAC of the study population was 44.1 ± 7.6 (%), and the mean value of IVA was 2.7 ± 1.3 m/s2(Table III). The RIMP values of 31 patients were higher than 40%, 13 patients had TAPSE values under 16 mm, eight patients had 2D RV FAC values <35%, and 32 patients had IVA values under 2.2 m/s2.
Table III.
Comparison of right ventricular systolic function parameters before and after PCI
| Characteristics | Total (n = 56) | ||
|---|---|---|---|
| Before PCI | After PCI | p | |
| RIMP (%) | 37.7 ± 17.2 | 36.8 ± 20.3 | 0.8 |
| TAPSE (mm) | 19.7 ± 1.1 | 20.5 ± 3.3 | 0.08 |
| 2D RV FAC (%) | 44.1 ± 7.6 | 46.3 ± 6.8 | 0.045 |
| IVA (m/s2) | 2.7 ± 1.3 | 3.2 ± 1.2 | 0.001 |
There was only a weak negative correlation between the ages and TAPSE values of the study population (p = 0.022, r = −0.236) (Table IV) during the correlation analysis of clinical and laboratory traits with the right ventricular systolic functional parameters.
Table IV.
Correlation analysis of clinical and laboratory subjects with cardiac parameters
| RIMP (%) | TAPSE (mm) | 2D RV FAC (%) | IVA (m/s2) | |
|---|---|---|---|---|
| Age (year) | ||||
| r | 0.058 | −0.236 | −0.138 | −0.069 |
| p | 0.574 | 0.022 | 0.188 | 0.508 |
| FBG (mg/dL) | ||||
| r | −0.096 | −0.022 | −0.103 | −0.166 |
| p | 0.360 | 0.831 | 0.329 | 0.112 |
| Troponin I | ||||
| r | −0.052 | −0.146 | −0.062 | 0.059 |
| p | 0.614 | −0.159 | 0.553 | 0.571 |
| Creatinine (mg/dL) | ||||
| r | 0.001 | −0.088 | −0.159 | −0.010 |
| p | 0.994 | 0.395 | 0.128 | 0.925 |
Coronary angiography and PCI
After coronary angiography, PCI was performed to 56 patients with critical lesions. Critical right coronary artery (RCA) lesion was observed in 27 patients. Seven patients had critical circumflex (Cx) artery stenosis, and 16 had critical left anterior descending (LAD) artery lesion. Five patients had both RCA and Cx artery lesions, while seven had both RCA and LAD artery lesions, and six had both LAD and Cx artery lesions. All patients had TIMI III flow in culprit artery except one who had culprit lesion on Cx artery and TIMI flow was 0 before PCI. TIMI III flow was achieved in all patients after PCI.
Comparison of the right ventricular systolic functions before and after PCI
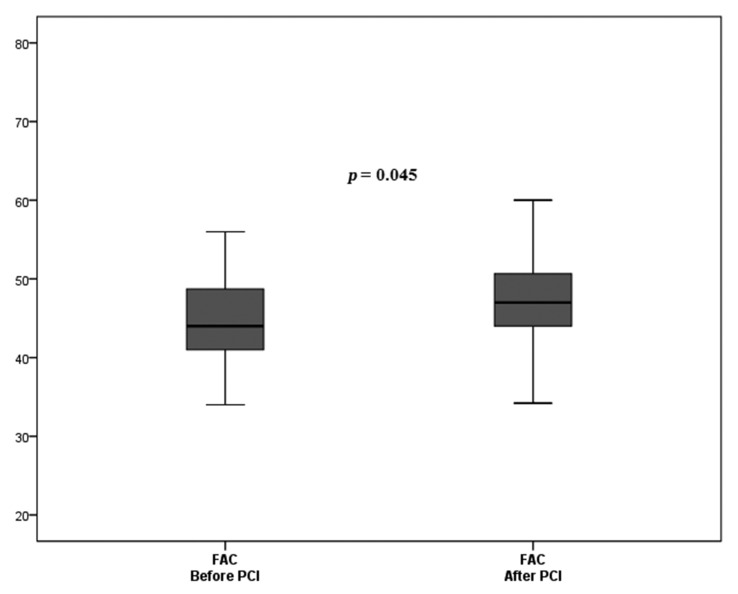
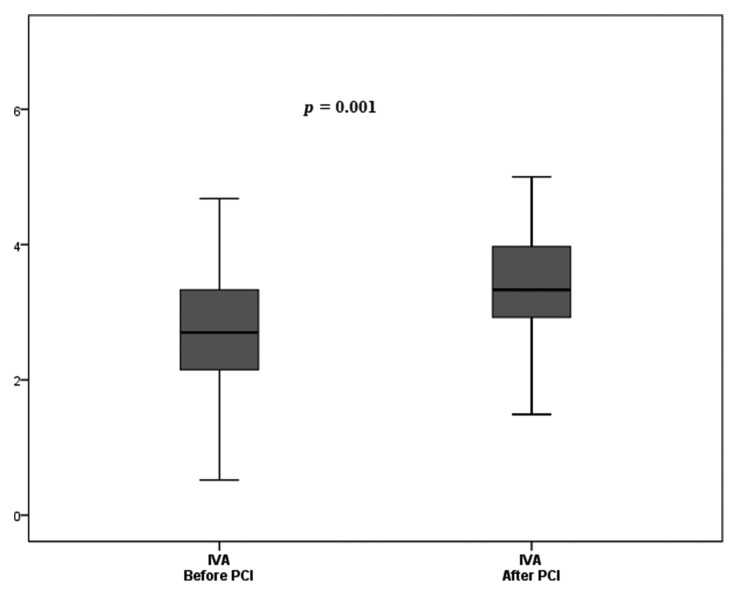
During comparison of right ventricular systolic functions, there was a significant increase in the 2D RV FAC and IVA values before and after PCI (44.1% ± 7.6% vs. 46.3% ± 6.8% [p = 0.045] [Fig. 5] and 2.7 ± 1.3 m/s2 vs. 3.2 ± 12 m/s2 [p = 0.001], respectively [Fig. 6]). TAPSE values of patients performing PCI also increased after PCI, but this increment was not statistically significant (19.7 ± 1.1mm vs. 20.5 ± 3.3 mm [p = 0.08]). However, the RIMP values of these patients did not differ significantly before and after PCI (37.7% ± 17.2% vs. 36.8% ± 20.3% [p = 0.8]) (Table III). The effect of the urgent PCI on right ventricular systolic functions was independent from culprit vessel location (Table V).
Fig. 5.
The box-plot graph comprising of FAC values of patients with NSTE-ACS before and after urgent PCI
Fig. 6.
The box-plot graph comprising of IVA values of patients with NSTE-ACS before and after urgent PCI
Table V.
Correlation analysis of clinical and laboratory subjects with cardiac parameters
| Culprit lesion: RCA | Culprit lesion: other | p** | |
|---|---|---|---|
| Before RIMP | 37.0 ± 13.9 | 35.9 ± 16.1 | 0.57 |
| After RIMP | 37.9 ± 18.8 | 35.9 ± 21.6 | 0.64 |
| Δ RIMP | 0.9 ± 12.2 | 0.001 ± 13.5 | 0.98 |
| p* | 0.95 | 0.99 | |
| Before TAPSE | 19.8 ± 3.9 | 19.5 ± 4.1 | 0.60 |
| After TAPSE | 20.9 ± 2.6 | 20.3 ± 3.7 | 0.36 |
| Δ TAPSE | 1.1 ± 3.1 | 0.8 ± 1.9 | 0.32 |
| p* | 0.02 | 0.002 | |
| Before IVA | 2.7 ± 1.2 | 2.7 ± 0.9 | 0.47 |
| After IVA | 3.5 ± 1.4 | 3.0 ± 0.9 | 0.06 |
| Δ IVA | 0.8 ± 1.3 | 0.3 ± 0.7 | 0.11 |
| p* | 0.006 | 0.008 | |
| Before 2D RV FAC | 43.8 ± 6.4 | 44.9 ± 8.1 | 0.23 |
| After 2D RV FAC | 46.4 ± 7.1 | 46.2 ± 6.6 | 0.85 |
| Δ 2D RV FAC | 2.6 ± 7.3 | 1.3 ± 6.5 | 0.35 |
| p* | 0.06 | 0.08 | |
| *Wilcoxon signed rank
test **Mann–Whitney U-test Abbreviations: systolic BP: systolic blood pressure; RIMP: right ventricular index of myocardial performance; TAPSE: tricuspid annular plane systolic excursion; 2D RV FAC: two-dimensional right ventricle fractional area change; IVA: isovolumic acceleration; PCI: percutaneous coronary intervention; EF: ejection fraction | |||
Discussion
This study showed that the right ventricular systolic functions may be impaired in patients with NSTE-ACS, and urgent PCI has beneficial effect on recovery of these impaired functions.
NSTE-ACS is an unstable coronary condition prone to ischemic recurrences and other complications that may lead to death or MI in the short and long term. The management, which includes anti-ischemic and anti-thrombotic pharmacological treatments as well as various strategies for coronary revascularization, is directed to prevent or reduce such complications and to improve outcomes [8].
Hamon et al. [9] demonstrated RV dysfunction as a predictor of an adverse prognosis in STEMI without cardiogenic shock, in a meta-analysis of data from 22 studies. On the other hand, RV dysfunction in NSTE-ACS has not been widely investigated yet.
A number of parameters such as RIMP, TAPSE, 2D RV FAC, 2D RV ejection fraction (EF), three-dimensional (3D) RV EF, tissue Doppler-derived tricuspid lateral annular systolic velocity (S0), and longitudinal strain and strain rate can be used for evaluation of RV systolic functions. Studies have shown clinical utility and value of RIMP, TAPSE, and 2D RV FAC for the assessment of the right ventricular systolic functions [2, 10, 11].
Maheshwari and Mittal [12] showed that RIMP is a more sensitive, non-geometric echocardiographic parameter than Simpson’s RVEF in detecting early RV dysfunction. In the present study, 31 patients with NSTE-ACS had impaired RIMP values.
Although TAPSE is an index of longitudinal function, it is known to be well correlated with parameters of RV global systolic function, such as radionuclide-derived RV EF, 2D RV FAC, and 2D RV EF [13]. Hoogslag et al. [14] investigated determinants of right ventricular remodeling following ST-segment elevation myocardial infarction, and they defined RV systolic dysfunction as TAPSE <16 mm. In our study, 13 patients with NSTE-ACS had TAPSE value under 16 mm.
Azevedo et al. [15] demonstrated that predictors of right ventricle dysfunction after anterior myocardial infarction by using 2D FAC and they defined 2D FAC <35% as RV systolic dysfunction. In our study population, eight of NSTE-ACS patients had FAC value under 35%.
Tayyareci et al. [16] demonstrated subclinic right ventricular dysfunction in patients with type 2 DM by using IVA. Thirty-two patients in our study had impaired IVA values.
The impairment of those parameters in our study demonstrated that RV systolic dysfunctions may be present in patients with NSTE-ACS on admission.
Revascularization for NSTE-ACS relieves symptoms, shortens hospital stay, and improves prognosis. The indications and timing for myocardial revascularization rely on many factors including the patient’s clinical traits, the presence of risk factors, comorbidities, and the severity of the lesions as identified by coronary angiography [8].
Many studies have showed that reperfusion therapy especially primary PCI restores the right ventricular systolic function in patients with STEMI [17]. However, the effects of urgent PCI on RV systolic functions in NSTE-ACS patients are less known. In our study, we compared the right ventricular systolic functions by using TAPSE, 2D FAC, IVA, and RIMP obtained before and after urgent PCI in patients with NSTE-ACS. We found that 2D FAC and IVA values of these patients increased after performing PCI. Although TAPSE and RIMP value of these patients recovered after PCI, it was not significantly different.
As the right coronary artery supplies most of the RV, studies analyzing RV infarction have evaluated those cases resulting from an acute occlusion of this vessel [4, 18–20]. The anterior wall of the RV is supplied by branches of the LAD [17], and autopsy studies had revealed that acute LAD occlusion could also cause partial RV infarction [21, 22]. This association has not been widely studied yet. More precise evaluation of RV involvement can improve our understanding of pathophysiology and allow a more thorough assessment of anterior STEMI patients.
When we analyzed the effect of culprit lesion on the right ventricular systolic functional recovery after urgent PCI, we found that the beneficial effect of the urgent PCI was independent from culprit vessel location (Table V).
Conclusions
The right ventricular functions may also be affected in patients with NSTE-ACS, and urgent PCI has a significant effect on the recovery of right ventricular systolic functions in patients with NSTE-ACS.
Abbreviations
- 2D RV FAC
two-dimensional right ventricle fractional area change
- Cx
circumflex coronary artery
- ECG
electrocardiographic
- ET
ejection time
- IVA
isovolumic acceleration
- IVCT
isovolumetric contraction time
- IVRT
isovolumetric relaxation time
- LAD
left anterior descending artery
- MI
myocardial infarction
- NSTE-ACS
non-ST-elevation acute coronary syndrome
- PCI
percutaneous coronary intervention
- RCA
right coronary artery
- RIMP
right ventricular index of myocardial performance
- RV
right ventricular
- STEMI
ST-elevation myocardial infarction
- TAPSE
tricuspid annular plane systolic excursion
- TCO
tricuspid valve closure and opening time
Funding Statement
Funding sources: No financial support was received for this study.
Footnotes
Authors’ contribution: All of the authors contributed to planning, conducting, and reporting of the work. All authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest: All of the authors have no conflict of interest.
Contributor Information
Nurşen Keleş,
Macit Kalçik,
Mustafa Çalişkan,
Hakan Çakir,
Soe Moe Aung,
Osman Köstek,
İbrahim Akin İzgi,
Cevat Kirma,
References
- 1.Zehender M, Kasper W, Kauder E, Schönthaler M, Geibel A, Olschewski M, Just H. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med. 1993;328:981–988. doi: 10.1056/NEJM199304083281401. [DOI] [PubMed] [Google Scholar]
- 2.Cabin HS, Clubb KS, Wackers FJ, Zaret BL. Right ventricular myocardial infarction with anterior wall left ventricular infarction: an autopsy study. Am Heart J. 1987;113:16–23. doi: 10.1016/0002-8703(87)90004-4. [DOI] [PubMed] [Google Scholar]
- 3.Zornoff LA, Skali H, Pfeffer MA, St John Sutton M, Rouleau JL, Lamas GA, Plappert T, Rouleau JR, Moyé LA, Lewis SJ, Braunwald E, Solomon SD, SAVE Investigators Right ventricular dysfunction and risk of heart failure and mortality after myocardial infarction. J Am Coll Cardiol. 2002;39:1450–1455. doi: 10.1016/s0735-1097(02)01804-1. [DOI] [PubMed] [Google Scholar]
- 4.Mehta SR, Eikelboom JW, Natarajan MK, Diaz R, Yi C, Gibbons RJ, Yusuf S. Impact of right ventricular involvement on mortality and morbidity in patients with inferior myocardial infarction. J Am Coll Cardiol. 2001;37:37–43. doi: 10.1016/s0735-1097(00)01089-5. [DOI] [PubMed] [Google Scholar]
- 5.Bueno H, López-Palop R, Pérez-David E, García-García J, López-Sendón JL, Delcán JL. Combined effect of age and right ventricular involvement on acute inferior myocardial infarction prognosis. Circulation. 1998;98:1714–1720. doi: 10.1161/01.cir.98.17.1714. [DOI] [PubMed] [Google Scholar]
- 6.Harvey W. An anatomical disquisition on the motion of the heart and blood in animals. In: Willius FA, Keys TE, editors. Classics of Cardiology. New York: Dover Publications; 1941. pp. 19–79. [Google Scholar]
- 7.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group. American Society of Echocardiography’s Guidelines and Standards Committee. European Association of Echocardiography Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, Petrie MC, Sonntag F, Uva MS, Storey RF, Wijns W, Zahger D, ESC Committee for Practice Guidelines ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 9.Hamon M, Agostini D, Le PO, Riddell JW, Hamon M. Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: meta-analysis. Crit Care Med. 2008;36:2023–2033. doi: 10.1097/CCM.0b013e31817d213d. [DOI] [PubMed] [Google Scholar]
- 10.Bos JM, Hagler DJ, Silvilairat S, Cabalka A, O’Leary P, Daniels O, Miller FA, Abraham TP. Right ventricular function in asymptomatic individuals with a systemic right ventricle. J Am Soc Echocardiogr. 2006;19:1033–1037. doi: 10.1016/j.echo.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Izzo A, Galderisi M, de Divitiis O. The influence of left systolic ventricular function on right ventricular function after an acute myocardial infarct. Cardiologia. 1998;43:173–180. [PubMed] [Google Scholar]
- 12.Maheshwari M, Mittal SR. Right ventricle myocardial performance index versus Simpson’s right ventricle ejection fraction in patients with isolated left ventricle anterior myocardial infarction. Heart Views. 2013;14:68–71. doi: 10.4103/1995-705X.115500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Hoogslag GE, Haeck ML, Velders MA, Joyce E, Boden H, Schalij MJ, Bax JJ, Ajmone Marsan N, Delgado V. Determinants of right ventricular remodeling following ST-segment elevation myocardial infarction. Am J Cardiol. 2014;114:1490–1496. doi: 10.1016/j.amjcard.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Azevedo PS, Cogni AL, Farah E, Minicucci MF, Okoshi K, Matsubara BB, Zanati SG, Fonseca AG, Patini BJ, Paiva SA, Zornoff LA. Predictors of right ventricle dysfunction after anterior myocardial infarction. Can J Cardiol. 2012;28:438–442. doi: 10.1016/j.cjca.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Tayyareci Y, Yurdakul S, Tayyareci G, Nisanci Y, Umman B, Buğra Z. Impact of myocardial acceleration during isovolumic contraction in evaluating subclinical right ventricular systolic dysfunction in type 2 diabetes mellitus patients. Echocardiography. 2010;27:1211–1218. doi: 10.1111/j.1540-8175.2010.01237.x. [DOI] [PubMed] [Google Scholar]
- 17.Assali AR, Teplitsky I, Ben-Dor I, Solodky A, Brosh D, Battler A, Fuchs S, Kornowski R. Prognostic importance of right ventricular infarction in an acute myocardial infarction cohort referred for contemporary percutaneous reperfusion therapy. Am Heart J. 2007;153:231–237. doi: 10.1016/j.ahj.2006.10.038. [DOI] [PubMed] [Google Scholar]
- 18.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, Part I. Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–1448. doi: 10.1161/CIRCULATIONAHA.107.653576. [DOI] [PubMed] [Google Scholar]
- 19.Pfisterer M. Right ventricular involvement in myocardial infarction and cardiogenic shock. Lancet. 2003;362:392–394. doi: 10.1016/S0140-6736(03)14028-7. [DOI] [PubMed] [Google Scholar]
- 20.Wong CK, White HD. Risk stratification of patients with right ventricular infarction: is there a need for a specific risk score? Eur Heart J. 2002;23:1642–1645. doi: 10.1053/euhj.2002.3306. [DOI] [PubMed] [Google Scholar]
- 21.Cabin HS, Clubb KS, Wackers FJ, Zaret BL. Right ventricular myocardial infarction with anterior wall left ventricular infarction: an autopsy study. Am Heart J. 1987;113:16–23. doi: 10.1016/0002-8703(87)90004-4. [DOI] [PubMed] [Google Scholar]
- 22.Andersen HR, Falk E, Nielsen D. Right ventricular infarction: frequency, size and topography in coronary heart disease: a prospective study comprising 107 consecutive autopsies from a coronary care unit. J Am Coll Cardiol. 1987;10:1223–1232. doi: 10.1016/s0735-1097(87)80122-5. [DOI] [PubMed] [Google Scholar]