Abstract
Parental substance abuse is a serious problem affecting the well-being of children and families. The co-occurrence of parental substance abuse and problematic parenting is recognized as a major public health concern. This review focuses on 21 outcome studies that tested dual treatment of substance abuse and parenting. A summary of theoretical conceptualizations of the connections between substance abuse and parenting provides a backdrop for the review. Outcomes of the dual treatment studies were generally positive with respect to reduction of parental substance use and improvement of parenting. Research in this area varied in methodological rigor and needs to overcome challenges regarding design issues, sampling frame, and complexities inherent in such a high-risk population. This area of work can be strengthened by randomized controlled trials, use of mixed-methods outcome measures, consideration of parent involvement with child protective services, involvement of significant others in treatment, provision of concrete supports for treatment attendance and facilitative public policies.
Keywords: Parental substance abuse, Child maltreatment, Parenting difficulties, Parenting interventions, Dual-treatment
The number of children in the United States living with at least one substance-abusing (S1A) parent is alarming. According to the 2012 National Survey on Drug Use, an estimated 7.5 million children, or 10.5% of the population 17 years of age and younger, live with at least one parent who abuses drugs or alcohol. More than one third of these children (35.9%) are five years of age or younger (Appleyard, Berlin, Rosanbalm, & Dodge, 2011), and nearly two thirds of adults enrolled in SA treatment programs are parents (Niccols et al., 2012).
Poor outcomes for children of SA parents can be seen across development. In infancy, prenatal drug exposure has been found to predict difficult temperament including irritability, sleep and feeding disturbances, excessive crying and physical ailments such as gastrointestinal problems, fever and seizures (Conners, Bradley, Whiteside-Mansell, & Crone, 2001; Jansson & Velez, 1999; Whiteside-Mansell, Crone, & Conners, 1999). In the first three years of life, parental SA is associated with insecure and disorganized attachment (Barnard & McKeganey, 2004; Beeghly, Frank, Rose-Jacobs, Cabral, & Tronick, 2003; Pajulo, Suchman, Kalland, & Mayes, 2006) and poor child performance on developmental measures, especially in the areas of speech and language development (Shulman, Shapira, & Hirshfield, 2000; Dunn et al., 2002). School-age children of SA parents are more likely to show aggressive behaviors, have fewer friends and experience more peer conflict (Dunn et al.), as well as show higher rates of hyperactivity and inattention (Barnard & McKeganey, 2004; Chronis et al., 2003). Adolescent offspring of SA parents show high rates of psychopathology such as depression, anxiety (Luthar, Cushing, Merikangas, & Rounsaville, 1998; Merikangas, Dierker, & Szatmari, 1998), and substance abuse (Biederman, Faraone, Monuteaux, & Feighner, 2000; Ritter, Stewart, Bernet, Coe, & Brown, 2002).
These adverse developmental outcomes associated with parental SA likely derive in part from ineffective parenting practices. Drug-involved parents are more likely to reflect demanding or coercive parenting styles, to provide less supervision, and rely more heavily on punitive forms of discipline (Kandel, 1990; Miller, Smyth, & Mudar, 1999). Parental SA is associated with problematic parenting that sometimes rises to the level of abuse. For example, in a study of over 8,000 participants asked to retrospectively report on their parents’ alcohol use, respondents who grew up with one or more alcoholic parent were twice as likely to have experienced emotional abuse, physical abuse, sexual abuse or neglect during childhood as those whose parents were not alcoholics (Dube et al., 2001). Prospective research further supports the link.
In a two-year follow-up study of more than 7,000 parents with no prior history of child maltreatment, Chaffin, Kelleher, and Hollenberg (1996) found that socioeconomic status, education, household size and social support were not strong predictors of child maltreatment, but the presence of parental SA increased the odds for child abuse by 2.9 and for child neglect by 3.24. Similar results were found in a representative community survey of more than 11,000 parents conducted by Kelleher, Chaffin, Hollenberg and Fisher (1994). Of the approximately 300 parents who self-reported child maltreatment, 40% of those reporting child abuse and 56% percent of those reporting child neglect also met criteria for SA based on a structured diagnostic interview. By comparison, 16% of the non-maltreating respondents qualified for SA. These studies likely underestimated the true prevalence of both maltreatment and SA because self-report data is subject to presentation bias.
SA mothers in the U.S. are more than twice as likely to lose custody of their children than non-SA mothers (Suchman, DeCoste, Leigh, & Borelli., 2010) and when children are taken into protective services, SA mothers are least likely to comply with court orders and most likely to lose custody permanently (Barnard & McKeganey, 2004; Grella, Needell, Shi, & Hser, 2009). Parents with SUD often do not seek out SA treatment or leave treatment early for fear that they will lose custody of their children or face criminal prosecution (Niccols & Sword, 2005). Child services agencies are financially and politically pressured to find permanent placements for children who have been removed from the home within an expedited time-frame, but successful SA treatment requires a sufficient amount of time to devote to recovery (Dauber, Neighbors, Dasaro, Riordan, & Morgenstern, 2012). Policies that require mothers to decide between caring for their children and completing drug treatment represent significant barriers that place mothers in the unfortunate situation where either choice may be considered wrong by influential authority figures on who’s opinion both the mother and child’s futures depend (Jansson & Velez, 1999). Participating in services that address both SA and parenting difficulties simultaneously enables parents to have both needs addressed, without their having to choose to prioritize one over the other.
Rationale for Review
Given the pervasiveness of parental SA in CPS cases and the huge cost of the dual problems (National Institute on Drug Abuse, 2008; PEW Charitable Trust, 2008), interest in evaluating progress and outcomes associated with the integration of parenting interventions into SA treatment programs has grown. The current review examines research on dual-treatment studies reporting both kinds of outcomes, namely parenting practices and parental SA. This review departs from prior reviews published in this general area. Niccols et al. (2012) reported on parenting outcomes of programs that provided SA treatment and some other family-focused intervention, only a portion of which included parenting-specific content. Similarly, Milligan et al. (2010) reviewed treatment studies that integrated SA treatment with some sort of parent or child intervention, but reviewed SA outcomes only.
The main purpose of the current review is to take stock of progress in this critical and challenging area, with respect to how well the research is being undertaken and what levels of success are being achieved. The review considers dual-treatment studies that include outcome measurement for both parenting and parental SA. Study characteristics reviewed include research design, sampling issues, data sources, assessment timing, treatment fidelity, and participant retention and attrition. Intervention outcomes for parenting and parental SA were evaluated. Finally, the review takes a preliminary look at emerging conceptualizations about the pathways connecting SA and parenting difficulties and characterizes how these conceptualizations are addressed, either implicitly or explicitly, by the treatments provided in the studies. While a unifying conceptual model has not yet been embraced by the field, it is important to keep (or increase) the spotlight on underlying theory and to describe progress and constraints in this regard.
Pathways of Influence Linking Substance Abuse and Child Maltreatment Risk
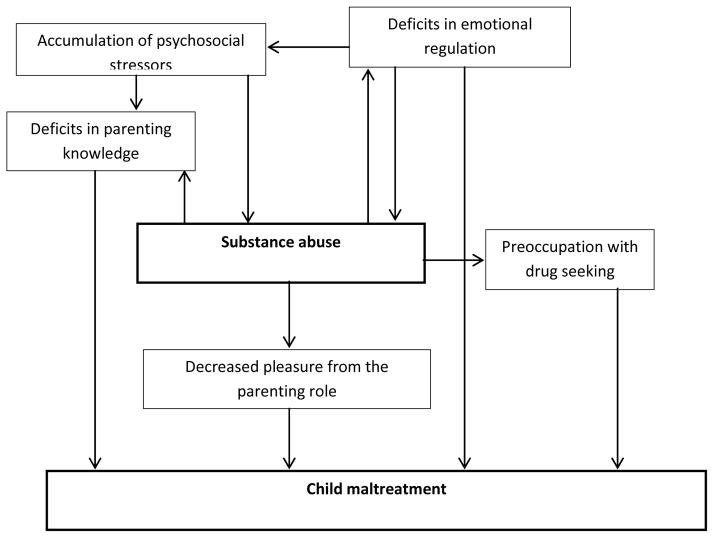
At this early stage, in this challenging intervention area, there is not yet a consensus as to a single conceptual model that captures the interrelationship between parental SA and parenting difficulties. A number of different conceptualizations could reasonably be postulated to describe the pathways of influence between parental SA and parenting difficulties including shared putative underlying causes as well as an established reciprocal relationship in which SA compromises effective parenting and child behavior difficulties may cause parents to cope with frustrations by turning to SA. The following five pathways are based on an interpretation of data from the literature and are not meant to be mutually exclusive but rather interacting ways of conceptualizing the connections between SA and parenting difficulties from multiple angles within the ecological system. An overview of how the pathways relate to each other is presented in Figure 1.
Figure 1.
Conceptual frameworks connecting substance abuse and child maltreatment.
Deficits in emotional regulation predict both SA and risk for child maltreatment
Individual deficits in emotional regulation among parents have been shown to predict both SA and poor parenting (Borelli, West, DeCoste, & Suchman, 2012). Such deficits manifest as poor impulse control and decreased frustration tolerance as well as an inability to cope with negative emotional states in adaptive ways. Under such circumstances, substance use is often initiated as a self-medicating or emotion-avoidance strategy (Suchman, DeCoste, Castiglioni, Legow, & Mayes, 2008) and parenting is often harsh and violent when parents act out feelings of anger and frustration without thought of consequences.
Parents who have difficulty regulating their own negative affective states also have difficulty accurately assessing and attending to their children’s emotions. Slade (2005) labeled these empathetic skills “reflective functioning” and described parents who are able to conceptualize, regulate and experience their own emotions while simultaneously reflecting on their child’s emotions and responding to their needs as being high in reflective functioning. Reflective functioning is generally low in SA parents as they struggle to separate their feelings of anger towards their situation from anger towards their child (Borelli et al., 2012). Such parents are more likely to attribute negative intentionality towards their children and respond with hostility (Dunn et al., 2002; Suchman, DeCoste, Leigh et al., 2010). Lack of emotional regulation combined with drug states limit parents’ abilities to focus on alternative explanations for their children’s negative behavior or anticipate the negative consequences of their own violent reactions (Kelley, 1998; Jansson & Velez, 1999; Miller et al., 1999).
Psychosocial factors predict both SA and risk for child maltreatment
Psychosocial stress has been conceptualized as a common cause of both parental SA and parenting difficulties (Hillson & Kuiper, 1994). SA parents experience a greater number of stressors based on life histories, compromised employability and limited social support. In a 2004 study looking at over 2,000 mothers seeking treatment at 50 SA rehabilitation programs between 1993 and 2000, Conners et al. found that 88% of the women were unemployed, 51.7% lacked a high school degree and 70.6% received public assistance. One-third of the sample had been homeless during the previous two years and two-thirds had been arrested. Fifty-seven percent reported having been abused by their parents and 73.6% reported being abused by a non-parent. Comorbid psychopathology was found in more than half of the subjects, with the most prevalent conditions being depression, trauma and bipolar disorder.
When parents with SA appraise these stressors and recognize the mismatch between their needs and their resources, their reactions are often maladaptive, such as engaging in additional drug use as an escape mechanism, as well as taking frustrations out on children (Kelley, 1998). Nair, Schuler, Black, Kettinger, and Harrington (2003) performed a survey on a sample of 161 mothers with SA and looked for factors that differentiated those who were involved with CPS for accusations of abuse and those who were not. Results showed that involvement with CPS was predicted by an accumulation of psychosocial stressors rather than any type of stressor in particular. Specifically, mothers with five or more life stressors were at significantly greater risk for maltreatment than those with four or fewer risks. Additional factors predicting CPS involvement for SA mothers found by Lussier, Laventure, and Bertrand (2010) included younger age, decreased interpersonal resources, less supportive family members, and less time to devote to relationship building.
Deficits in knowledge of parenting and child developmental predict risk for child maltreatment
SA parents show diminished knowledge of appropriate child-care practices and expected child developmental milestones. In a 2004 study Velez et al. developed a questionnaire regarding parenting practices and child development and administered it to a sample of 73 pregnant women in their first week of SA treatment. Results showed a mean total score of only 57.3%, a failing grade. Similarly, Pajulo et al. (2006) found that SA mothers had difficulty identifying what skills their children were and were not capable of and could not accurately anticipate their next developmental stage. In such cases, parents may expect too much of their children, and attribute misbehavior to malicious intentions that the child is not developmentally capable of having (Kerwin, 2005). Lack of proper expectations and alternative strategies for dealing with child behavior problems can result in use of unwarranted and inappropriate discipline, (Kelley, 1998; Magura, Laudet, Kang, & Whitney, 1999). Such knowledge deficits have been hypothesized to stem from parents’ cognitive impairments and compromised attention brought on by either drug or withdrawal states (Clausen, Aguilar, & Ludwig, 2012), as well as reduced access to parenting education resources.
Preoccupation with drug-seeking leads to risk for child maltreatment
The addictive nature of alcohol and illicit substances lend themselves to an increased risk for child neglect when one considers the psychological and financial costs of maintaining a drug habit. For many families, time, effort and money that would otherwise be spent on fulfilling the child’s needs are instead spent on procuring drugs (Barnard & McKeganey, 2004; Lussier et al., 2010; Dunn et al., 2002).
On a cognitive level, drug acquisition and child care compete for parents’ attention such that a parent cannot invest fully in one or the other. This results in compromised care of the child during times of severe craving and withdrawal, as well as during times of acute drug use.
Neurologically, drug states have been shown to corrupt the motivational center of the brain through altering the sensitivity of dopamine receptors in the nucleus accumbens. Robinson and Berridge (2003) have shown that with repeated drug use, the nucleus accumbens becomes so sensitized to the drug stimulus that its activity interferes with the user’s ability to override the motivation to continue to take the drugs via logic or rationality. This sensitization can be triggered subconsciously by any relevant environmental drug cue, such as the street corner where a parent has procured drugs in the past, or a stressful event such as a child crying that the parent has previously coped with via drugs (Robinson & Berridge). While parents may consciously want to provide and care for their children, in the sensitized state, motivation for increased drug taking out-competes this drive (Pajulo et al., 2006; Robinson & Berridge).
Decreased pleasure in parenting leads to risk for child maltreatment
Parents with SA derive less pleasure from the parenting role than non-SA parents. Studies have shown that parents with SA spend less time interacting with their children (Clausen et al., 2012; Suchman, De Cosete, Leigh et al., 2010), report lower levels of satisfaction in their parental relationships (Lussier et al., 2010), initiate fewer interactions with their children in behavioral observation paradigms (Pajulo et al., 2006) and exhibit diminished bonding behaviors towards their children starting in infancy (Dunn et al., 2002). Furthermore, when mother-child dyads do interact, their exchanges are characterized by less enthusiasm or mutual enjoyment, and more conflict (Pajulo et al.).
Researchers have hypothesized that the tolerance-building effects of illicit drugs reduce the ability of parents with SA to experience joy from non-drug sources. As tolerance escalates such that greater and greater amounts of drug are needed to achieve desired feelings of pleasure, a process known as allostatic loading, the threshold for experiencing pleasure on a neurological level increases. Naturally-rewarding activities such as interacting with one’s child are no longer enjoyable enough to provide sufficient mood elevation (George, Le Moal, & Koob, 2012). Decreased pleasure garnered from the parent-child relationship may decrease parents’ motivation to interact with and care for their children.
Summary
The five preceding conceptualizations begin to describe the complex connections between SA and parenting difficulties and provide theoretical support for their concurrent treatment. Treating SA without addressing parenting leaves parents with insufficient skills for handling child behavior issues and makes them more vulnerable to drug relapse as a coping mechanism (Belt & Punamäki, 2007; Suchman et al., 2008; Whiteside-Mansell et al., 1999). Additionally, addressing parenting without addressing SA is likely futile as effective parenting requires a significant amount of emotional-regulation and intrinsic motivation, both of which are incompatible with drug and withdrawal states (Robinson & Berridge, 2003; George et al., 2012). The combined treatment of substance abuse and parenting difficulties has the potential to act synergistically to enhance outcomes in both areas by increasing self-regulation skills. The current review examines methodologies and outcomes of published dual-treatment studies, and makes recommendations for future research, practice and policy changes in this area.
Method
A literature search of PsychINFO, Google Scholar and Medline (Ovid) included keyword terms “substance use,” “substance abuse,” “addiction,” “alcoholism,” “treatment,” “intervention,” “rehabilitation,” “child abuse,” “child maltreatment,” “child neglect,” “parenting,” “parental,” “parent education,” and “parenting skills,” and yielded 290 studies. From these, 21 studies were identified that met the following criteria: (1) publication in English between 1993 and 2014, (2) concurrent (dual) SA and parenting interventions, and (3) quantitative outcome data on both parental SA and parenting. Studies with either randomized or non-randomized designs were included to capture trends in this growing but still emerging area of research, however case trials were excluded due to their predominantly qualitative nature. Readers interested in reviewing case studies are encouraged to reference Romero, Donohue & Allen (2010), Romero et al. (2010) and Donohue et al. (2010).
Review of Intervention Studies
Design
The 21 studies included 9 randomized-control trials (RCTs). In these studies, all parents received SA treatment and were randomly assigned to either a parenting intervention or control condition. Control groups ranged from treatment as usual, consisting of SA treatment and some form of case management (Catalano, Gainey, Flemming, Haggerty, & Johnson, 1999; Luthar, Suchman & Altomare, 2007; Dakof et al., 2010; Donohue et al., 2014) to alternative treatment controls, such as Behavioral Couple’s Therapy (Lam, Fals-Steward, & Kelley, 2009) or Parenting Education brochures (Suchman, DeCoste, Castiglioni et al., 2010; Suchman, DeCoste, McMahon, Rounsaville, & Mayes, 2011). Analyses compared outcomes between groups using baseline data as a covariate when available. All but two (Berlin et al., 2014; Luthar & Suchman, 2000) of the nine RCT studies conducted intent-to-treat analyses and when appropriate, all RCT studies used assessors who were blind to participants’ study condition with the exception of Lam et al. (2009) and Dawe & Harnett (2007) which looked at self-report data only.
Of the 12 non-RCT studies, 3 used quasi-experimental designs in which participant outcomes were compared to outcomes for non-participant control groups made up of families who did not sign up for, or were not offered the chance to enroll in the studies. Five studies employed dose-response analyses, assessing outcomes for families based on time in treatment, while the remaining four studies used single-group pre-post repeated measures analyses with no comparison group (see Table 1).
Table 1.
Study Design and Methodology
| Study | Design | Treatment setting | Treatment timing | Treatment fidelity | Data sources | Longest follow-up |
|---|---|---|---|---|---|---|
| Donohue et al., 2014 | RCT | H | C | Yes | SR; US | 10 mos. PE |
| Berlin et al., 2014 | RCT | I | SA first | No | SR; US; PCO | PT only |
| Suchman et al., 2010; 2011 | RCT | O | C, PMH first | Yes | SR; US; PCO | 6 wks. PT |
| Dakof et al., 2010 | RCT | O | C | No | SR; US; Rec | 18 mos. PE |
| Lam et al., 2009 | RCT | O | C | Yes | SR | 12 mos. PT |
| Dawe & Harnett, 2007 | RCT | H | SA first | No | SR | 6 mos. PT |
| Luthar et al., 2007 | RCT | O | C, PMH first | Yes | SR | 6 mos. PT |
| Luthar & Suchman, 2000 | RCT | O | C, PMH first | Yes | SR, US | 6 mos. PT. |
| Catalano et al. 1999 | RCT | O | SA first | No | SR | 12 mos. PT |
| Schaeffer et al., 2013 | Quasi | H | C | No | SR; US; Rec | PT only |
| McComish et al., 2003 | Quasi | I | C | No | SR | 6 mos. PT |
| Field et al., 1998 | Quasi | S | C | No | SR; US; PCO | 12 mos. PE |
| Conners et al., 2006 | OGPP, DR | I | C | No | SR | 12 mos. PT |
| Conners et al., 2001 | OGPP, DR | I | C | No | SR | 12 mos. PT |
| Killeen & Brady, 2000 | OGPP, DR | I | C | No | SR | 12 mos. PT |
| Magura, et al., 1999 | OGPP, DR | O | C | No | SR; HS | 12 mos. PE |
| Camp & Finkelstein, 1997; Moore et al., 2001 | OGPP, DR | I | Mixed | No | SR; PCO | 9 mos. PE |
| Suchman et al., 2008 | OGPP | O | C, PMH first | No | SR; PCO | PT only |
| Belcher et al. 2005 (Project Strive) | OGPP | O | NR | No | SR; PCO | PT only |
| Niccols & Sword, 2005 | OGPP | O | C | No | SR | 6 mos. PT |
| Dawe et al., 2003 | OGPP | O | SA first | No | SR | 3 mos. PT |
Note. Design: RCT = randomized controlled trial; Quasi= quasi-experimental; OGPP= one group pre/post comparison; DR = dose response analyses. Intervention setting: I=impatient; O=outpatient; H=home-based; S=school-based; Intervention Timing: C= concurrent SA and parenting interventions started at enrollment; PMH= parent mental health addressed first in parenting intervention component; NR= not reported; Data sources: SR=self-report; PCO= observation of parent-child interaction; US= urine toxicology screen; HS= hair toxicology screen; Rec= Records collected from Child Protective Service agencies; Longest follow-up; PE= post-enrollment; PT= post-treatment
Sample
Parent demographics
Demographic data on parent race and education attainment are presented in Table 2. Nine studies reported that the majority of participants were non-Hispanic Whites while eight studies reported the majority of participants were Black and four studies did not provide the racial breakdown of participants (Dawe & Harnett, 2007; Conners et al., 2001; Niccols & Sword, 2005; Dawe, Harnett, Rendalls, & Staiger, 2003). Level of educational attainment was low across samples with the majority of studies reporting a large proportion of their participants had less than high school education, and only Suchman et al. (2008) reporting that more than 12% of participants attended any college.
Table 2.
Study Samples
| Study | N | Parent race % | Parent education % | Child Welfare involvement % | Substance type | Child age | Treatment retention % | Study retention % |
|---|---|---|---|---|---|---|---|---|
| Donohue et al., 2014 | 72 | 47 W; 25 B; 17 O; 11 H | 50< HS; 44 HS; 6 SC | 100 | IS | Average 3.9 years | 75 | 74 |
| Berlin et al., 2014 | 21 | 86 W; 14 non-W | 86 HS+ | NR | NR | 1–20 months | 76 | 76 |
| Suchman et al., 2010; 2011 | 47 | 70 W; 30 non-W | Mean 12 yrs. | 60 | IS + A | 0–36 months | 72 T; 78 C | 72 T; 78 C |
| Dakof et al., 2010 | 62 | 42 B; 35 H; 23 W | 57 < HS; 37 HS; 6 SC | 100 | IS + A | 0- 18 years | 61 | 93 |
| Lam et al., 2009 | 30 | 63 W; 23 B; 7 H; 7 O | Mean 13 yrs. | 40 | A | 8–12 years | 84 T; 86 couples’ therapy; 83 standard | 83 |
| Dawe & Harnett., 2007 | 64 | NR | NR | NR | IS + A | 2–8 years | 77 T | 83 |
| Luthar et al., 2007 | 127 | 44 B; 40 W; 16 H | 35 <HS; 39 HS; 1.5 SC | 0 | IS | 0–16 years | 58 T; 63 C | 75 T; 87 C |
| Luthar & Suchman, 2000 | 61 | 72 W; 20 B; 8 H | NR | NR | IS | 0–16 years | 86 T; 83 C | 76 T; 79 C |
| Catalano et al. 1999 | 130 | 77 W; 18 B; 5 O | 95 HS; 5 SC | 0 | IS | 3–14 years | 51 | 93 |
| Schaeffer et al., 2013 | 25 | 79 W; 16 H; 5 B | NR | 100 | IS + A | 6–17 years | 92 | 92 |
| McComish et al., 2003 | 39 | 78 B; 17 W; 5 O | 63 HS+ | 49 | NR | 0–3 years | 75 > 6 mos; 50 > 10 mos | 72 |
| Field et al., 1998 | 126 | 64 B; 27 H; 10 W | Mean 10yrs. | NR | IS | Infants | NR | NR |
| Conners et al., 2006 | 305 | 64 W, 36 B | NR | 34 | IS + A | 0–15 years | 43 | 76 |
| Conners et al., 2001 | 72 | NR | NR | NR | IS + A | 0–15 years | 42 grads; 42 > 30 days; 16 < 30 days | 86 |
| Killeen & Brady., 2000 | 63 | 70 B; 29 W; 1 H | NR | NR | IS + A | 0–12 years | 38 | 75 |
| Magura, et al., 1999 | 173 | 65 B; 27 H; 8 W | 61 < HS; 27 HS; 12 HS+ | 70% | IS + A | 1–9 years | 28 | 82 SR; 66 Tox |
| Camp & Finkelstein, 1997; Moore et al., 2001 | 66 | 72 B; 22 W; 4 H; 2 NA | 60 < HS; 40 HS+ | NR | IS + A | Infants | Program A 35; Program B 55 | Program A 33; Program B 44 |
| Suchman et al., 2008 | 14 | 72 W; 14 H; 14 B | 14 <HS; 57 HS; 29 SC | NR | IS | 12–36 months | 57 | 57 |
| Belcher et al. 2005 (Project Strive) | 80 | 63 B; W 30; 4 H; 3 O | 66 < HS | NR | IS + A | Infants | 20 | 88 |
| Niccols & Sword, 2005 | 13 | NR | NR | 69 | IS + A | 0–6 years | 54 | 69 |
| Dawe et al., 2003 | 7 | NR | NR | 11 | IS + A | 2–6 years | 100 | 89 |
Note. W= non-Hispanic White; B= Black/African American; H= Hispanic; NA= Native American; O = Other; NR = not reported; HS= high school; SC= some college; A=alcohol; IS= illicit substances; T=treatment group; C=control group SR= self-report data; Tox= toxicology screen data; Treatment Retention = % of participants successfully participating in interventions as defined by the authors; Study Retention = % of participants who provided at-least post-treatment data.
Types of abused substances
For twelve of the studies, to be included parents had to abuse at least one substance that could include opiates, narcotics, cannabis or alcohol. Six studies included parents who abused at least one illicit substance, excluding parents who only abused alcohol, and one study focused exclusively on parents who abused alcohol (see Table 2). Berlin et al. (2014) did not specify the type of substances participants abused, and McComish et al. (2003) reported that 85% of participants were cocaine users but did not provide further information. On the individual level, five studies reported that the majority of participants were poly-substance abusers, reporting more than one substance of abuse (Dakof et al., 2010; Camp & Finkelstein, 1997; Killeen & Brady, 2000; Conners et al., 2001; Belcher et al., 2005) while six included majority heroin or other opiate abusers (Catalano et al., 1999; Luthar et al., 2007; Luthar & Suchman, 2000; Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al., 2011; Dawe & Harnett, 2007; Dawe et al., 2003) and five included majority crack/cocaine abusers (Conners, Grant, Crone, & Whiteside-Mansell, 2006; Conners et al., 2001; Magura et al., 1999; McComish et al., 2003; Belcher et al., 2005). Only Donohue et al. (2014) and Lam et al. (2009) reported conducting DSM-based assessments to independently verify participants qualified for SA disorder diagnoses. Other studies based inclusion criteria off of parents’ enrollment in SA treatment, involvement in drug courts or attendance at methadone maintenance clinics.
Child age
Samples varied greatly with respect to the ages of the parents’ children (see Table 2). Some studies addressed children from infancy through adolescence while others focused on more specific age ranges such as infants, children under three, or eight to twelve year-olds. The majority (12) focused on children under ten years of age, with four studies addressing adolescents over the age of fifteen.
Child welfare involvement
Samples were mixed with regard to child welfare involvement. Three studies required parents to have open CPS cases for child abuse or neglect as inclusion criteria. Seven studies included some families with CPS involvement and nine studies did not specify parents’ involvement with CPS. Two studies excluded parents with CPS involvement, which might have yielded a lower-risk sample (see Table 2). None of the studies with mixed samples examined CPS involvement as a covariate or moderator in outcome analyses.
Parent gender
Seventeen studies included mothers only, while three studies also included some fathers (Dawe et al., 2003; Dawe & Harnett, 2007; Catalano et al., 1999) and one study focused exclusively on fathers (Lam et al., 2009).
Timing of Interventions
The sequence of interventions also differed across studies. Eleven studies were designed such that both the SA and parenting components of the intervention began concurrently upon enrollment in the program (see Table 1). Four studies included participants in the parenting intervention only if they had already been involved in SA treatment for at least a few months (Catalano et al., 1999; Dawe et al., 2003; Dawe & Harnett, 2007; Berlin et al., 2014).
Four studies used a hybrid model wherein the first half of the parenting program addressed the mothers’ psychological well-being generally, focusing on developing coping mechanisms, challenging dysfunctional attributions and anger management, while the second half addressed specific parenting skills (Luthar et al., 2007; Luthar & Suchman, 2000; Suchman et al., 2008; Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al., 2011).
Camp and Finkelstein’s (1997) study qualifies as both simultaneous and delayed parenting interventions as one study site provided parents with both services immediately upon entering treatment, while the other provided parenting services 3–6 months after SA treatment began. Comparison of the two sites was compromised, however, by significant demographic differences between participants at the different locations.
Data Sources and Timing of Outcome Variables
Across all of the studies, baseline and outcome data on parental SA relied heavily on self-report measures (see Table 1). The most commonly used self-report measure was the Addiction Severity Index (McLellan, Luborsky, Woody & O’Brien, 1980). For an extended consideration of substance abuse outcomes measures the reader is referred to (Carroll, 1995). Nine studies also used biological analyses of substance use including urine or hair toxicology screens. Such multi-method analyses strengthen the validity of the findings, especially when the drug screens occurred randomly.
Parenting outcomes were assessed primarily with self-report measures as well. There was no consistency across the studies in terms of choice of self-report measures related to parenting. The measures varied from ones solely focused on parenting style or practices such as the Parenting Scale (Arnold, O’Leary, Wolff, & Acker, 1993), to measures reflecting a broader set of constructs that include parenting, such as the Parenting Stress Index (Abidin, 1997) or the Child Abuse Potential Inventory (Milner, 1994). Additionally, Berlin et al. (2014), Field, Scafidi, and Pickens (1998), Camp and Finkelstein (1997) and studies testing the Mothers and Toddlers Program (Suchman et al., 2008; Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al., 2011) and Project Strive (Belcher et al., 2005) conducted coded observations of parent-child interactions.
Longitudinal follow-up assessments were conducted for 17 of the 21 studies. Time frames ranged from six weeks post-treatment (Suchman et al., 2011) to 18 months post-enrollment (Dakof et al., 2010) with five studies conducting six-month follow-up assessments and seven studies conducting 12-month follow-up assessments (see Table 1).
Treatment Fidelity
Treatment fidelity was assessed for five of the nine RCT studies and for none of the non-controlled studies (see Table 1).
Treatment Retention and Study Attrition
Premature departure from SA treatment is common among parents in the child welfare system. When individuals in the general population enroll in SA treatment, the majority (55–60%) attends at least half of treatment appointments, while only 20% of mothers in the child welfare system attend at this rate (Schaeffer, Swenson, Tuerk, & Henggeler, 2013). Authors of the reviewed studies described that many parents reported histories of SA treatment failures and pointed to child care concerns and difficulty managing the disparate demands of SA treatment programs and CPS as the main barriers to program completion (Killeen & Brady, 2000).
Across the studies, retention in treatment varied as a function of study design, intervention timing, sample size, treatment location and the tangible supports provided by program staff. Studies that utilized RCT designs reported the highest attendance rates with at least 50% of participants attending at least 50% of sessions (see Table 2). Two RCTs provided the parenting intervention only after the parents had been involved in SA services for a few months, and four RCTs used the hybrid model, addressing parent’s psychological functioning generally before addressing specific parenting practices (see Table 1). Delaying the parenting content appeared to increase treatment retention rates in these studies compared to the studies that provided parenting content immediately (see Table 2). Two RCTs also addressed environmental barriers to treatment attendance such as financial problems and lack of transportation. Catalano et al. (1999) provided three dollars per session to parents and small toys for the children. Suchman, DeCoste, Castiglioni et al. (2010) and Suchman et al. (2011) provided parents with food, transportation vouchers, and child care during sessions. Both of these programs reported retention rates above 50%, significantly higher than many of the non-randomized studies.
While rates of treatment completion varied substantially, retention in study activities was higher across studies (see Table 2). In the 20 studies that reported on study retention, at least 70% of participants provided post-treatment data in all studies except for Suchman et al. (2008) in which 57% of parents provided follow-up data, and Camp and Finkelstein (1997) for which approximately 40% of parents provided follow-up data. Field et al. (1998) did not provided data on study retention rates. Short follow-up duration combined with the use of financial incentives to complete study measures likely contributed to success in this area.
Conceptual Pathways Associated with the Parenting Interventions
The 21 studies encompassed 17 different parenting interventions. The Mothers and Toddler’s Program (Suchman et al., 2008; Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al., 2011), the Parents Under Pressure program (Dawe et al., 2003; Dawe & Harnett, 2007), the Relational Psychotherapy Mother’s Group (RPMG) (Luthar et al., 2007; Luthar & Suchman, 2000) and the Arkansas CARES program (Conners et al., 2001; Conners et al., 2006) were each evaluated by two studies. Across the interventions, it was common for an intervention to address more than one pathway of influence connecting parental SA and parenting difficulties (see Table 4). However, the most frequent conceptual pathway was the connection between psychosocial stressors and the dual-problems of SA and poor parenting. Fifteen of the 17 programs provided parents with services aimed at increasing psychosocial resources such as employment, housing and increased support from family and friends. Four programs, the Arkansas CARES program (Conners et al., 2001; Conners et al., 2006), The Nurturing Program (Camp & Finkelstein, 1997; Moore et al., 2001) the Flint Odyssey House (McComish et al., 2003) and Killeen & Brady’s (2003) program were all are comprehensive, integrated residential programs that provided parents with additional services beyond SA treatment and parenting education such as vocational trainings, medical care, life skills training and psychiatric treatment. Unfortunately, assessment of the relative benefits of these comprehensive programs is limited based on the uncontrolled nature of their study designs (see Table 1).
Table 4.
Conceptualizations: Pathways of Influence Addressed by the Parenting Interventions
| Parenting Intervention (Study) | Conceptual Pathways
|
|||
|---|---|---|---|---|
| Emotional regulation | Psychosocial functioning | Parenting knowledge | Drug preoccupation | |
| Parents Under Pressure (Dawe et al., 2003; Dawe & Harnett., 2007) | x | x | x | x |
| Focus on Families (Catalano et al. 1999) | x | x | x | x |
| Mothers and Toddlers Program (Suchman et al., 2008; 2010; 2011) | x | x | x | |
| Engaging Mom’s Program (Dakof et al., 2010) | x | x | x | |
| School-based program for young mothers (Field et al., 1998) | x | x | x | |
| Family Behavior Therapy (Donohue et al., 2014) | x | x | x | |
| The Nurturing Program (Camp & Finkelstein, 1997; Moore et al., 2001) | x | x | x | |
| Multisystemic Therapy – Building Stronger Families (Schaeffer et al., 2013) | x | x | x | |
| Relational Psychotherapy Mother’s Group (Luthar et al., 2007; Luthar & Suchman, 2000) | x | x | ||
| Flint Odyssey House Family Focused program (McComish et al., 2003) | x | x | ||
| Parenting Skills & Behavioral Couples Therapy (Lam et al., 2009) | x | x | ||
| Arkansas CARES (Conners et al., 2001; Conners et al., 2006) | x | x | ||
| Family Rehabilitation Program (Magura, et al., 1999) | x | x | ||
| New Choices Program (Niccols & Sword, 2005) | x | x | ||
| Attachment and Biobehavioral Catch-up (Berlin et al., 2014) | x | |||
| Killeen & Brady., 2000 | x | |||
| Project Strive (Belcher et al. 2005) | x | |||
No intervention directly addressed reduced pleasure from parenting as a conceptual pathway.
The second most commonly addressed pathway was the connection between parental SA and deficits in parent knowledge of child development and appropriate parenting practices. Thirteen of the 17 interventions provided parents with information regarding child development and specific parenting skills. Nine of the 17 interventions addressed deficits in parents’ emotional regulation and reflective functioning by helping parents focus on increasing sensitivity to their children’s emotions and needs and developing cognitive-behavioral coping mechanisms of managing their own negative affect. Five of the seventeen interventions addressed ways in which preoccupation with drug seeking interferes with child care practices by reinforcing parents for engaging in child care activities that are incompatible with drug use. No study directly addressed the decreased pleasure that parents with SA garner from interacting with their children.
Outcomes
The RCTs permitted comparisons regarding the relative contributions of combined parenting and SA treatment to SA treatment alone. All of the RCTs revealed that dual treatment reduced SA as much as SA treatment alone, and in five studies (Catalano et al., 1999 & Luthar et al., 2007; Luthar & Suchman, 2000; Lam et al., 2009; Donohue et al., 2014), parents who received the parenting intervention showed better SA outcomes than those who did not receive parenting help.
As anticipated, results of the RCTs indicated that combined SA treatment and parenting intervention improved parenting above and beyond SA treatment alone (see Table 3). With respect to adverse outcomes, risk for child maltreatment in two studies increased for the parents who received SA treatment only (Dawe & Harnett, 2007; Luthar et al., 2007).
Table 3.
Study Outcomes
| Study | Improvement Substance abuse | Improvement Parenting | Child adjustment |
|---|---|---|---|
| Donohue et al., 2014 | * T > C | T > C | |
| Berlin et al., 2014 | T = C | T > C | |
| Suchman et al., 2010; 2011 | T = C | T > C | T > C |
| Dakof et al., 2010 | T > C | T > C | |
| Lam et al., 2009 | T > C | T > C | |
| Dawe & Harnett., 2007 | T > C | T > C | T > C |
| Luthar et al., 2007 | T > C | T > C | T > C |
| Luther & Suchman, 2000 | T > C | T > C | |
| Catalano et al. 1999 | T > C | T > C | C > T |
| Schaeffer et al., 2013 | PrePost | QT> QC | PrePost |
| McComish et al., 2003 | QT > QC | PrePost | |
| Field et al., 1998 | QT > QC | QT > QC | QT> QC |
| Conners et al., 2006 | Com > NCom | Com > NCom | |
| Conners et al., 2001 | Com > NCom | Com > NCom | NC |
| Killeen & Brady, 2000 | Com > NCom | Com > NCom | Com > NCom |
| Magura, et al., 1999 | Com > NCom | Com > NCom | |
| Camp & Finkelstein 1997; Moore et al., 2001 | Com > NCom | PrePost | |
| Suchman et al., 2008 | PrePost | PrePost | |
| Belcher et al. 2005 (Project Strive) | PrePost | PrePost | |
| Niccols & Sword., 2005 | PrePost | PrePost | PrePost |
| Dawe et al., 2003 | PrePost | PrePost | PrePost |
Note. T=treatment group (randomized); C=control group (randomized); QT=treatment group (quasi-exp.); QC=control group (quasi-exp); Com=treatment completers; NCom=treatment non-completers; PrePost= single group repeated measures comparison; NC = no change;
The overall sample showed equal reduction in drug use across groups, however, mothers in the treatment condition who were referred for child neglect rather than in-utero drug exposure showed greater reduction in hard-drug use than their counterparts in the control condition.
Among the RCTs, only Luthar et al. (2007) stood out for its less promising results. Outcomes showed that the parenting intervention group showed just a marginal decrease in risk for maltreatment, and no treatment gains in either SA or parenting remained at six month follow-up. Researchers hypothesized that such regression may have occurred because mothers had become overly dependent on program services and were unable to transfer skills to life after treatment.
Results of the studies with quasi-experimental, dose-response, or single-group designs supported the conclusions of the RCTs, namely that the addition of parenting intervention in conjunction with SA treatment might have benefits above and beyond SA treatment alone. Camp and Finkelstein (1997) and McComish et al. (2003) found that participation in parent training correlated with longer mean stays in residential facilities compared to non-participants, suggesting that the addition of parent-specific programming may have increased parents’ motivation to remain in treatment. Conners et al. (2001), Conners et al. (2006), Killeen and Brady (2000) and Magura et al. (1999) all found that SA decreased and parenting improved at post-treatment for program completers as compared to non-completers and Niccols and Sword (2005), Dawe et al. (2003), Suchman et al. (2008) and Schaeffer et al. (2013) found significant reductions in substance abuse as well as improved parent functioning in repeated measures analyses for study participants. Such results suggest that the addition of the parenting components to treatment did not detract from or interfere with the SA interventions, and in some cases, enhanced it. Additionally, SA parents may be able to benefit from and absorb the content of parenting interventions.
Discussion
The 21 studies on dual treatment of parental SA and poor parenting included nine RCTs and three quasi-experimental designs. The other, less controlled studies contribute some breadth to the literature by piloting explorations of interventions that could graduate to more rigorous trials. Across studies, samples differed in regard to the age of the target children, parents’ involvement with the child welfare system, the types of outcome measures collected, the timing of intervention components, as well as treatment settings and conceptual pathways addressed.
Difficulty recruiting sufficient numbers of families and the desire to provide services to all families in need contribute to a literature that is made up mostly of non-randomized designs. The nine randomized controlled trials allow us to make stronger inferences regarding internal and external validity of results, however, some of these studies ensured that the treatment and control conditions received equal intervention contact hours, (Luthar et al., 2007; Luthar & Suchman, 2000; Dakof et al., 2010), while others did not (Catalano et al., 1999; Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al., 2011; Dawe & Harnett, 2007; Donohue et al., 2014; Berlin et al., 2014). In the cases where the experimental group had a greater number of treatment hours, it is difficult to determine if treatment changes are attributable to the specific type of treatment provided or to the increased dosage of clinical contact. Two studies, Berlin et al. (2014) and Luthar and Suchman (2000) did not perform intent-to-treat analyses and thus we cannot be sure that treatment completers did not differ from treatment non-completers in important yet unmeasured ways. Additionally, only five of the nine RCTs provided data on treatment fidelity. For the remaining four studies we cannot know how closely providers followed treatment guidelines or how consistently treatment was implemented across subjects randomized to the same condition.
In the three studies that utilized quasi-experimental control groups, external validity is compromised as it is impossible to know if individuals who volunteer to participate in such dual-treatment studies differ from those who do not. Validity for the five studies that assessed outcomes for families based on time in treatment is similarly threatened as individuals who remain in treatment may differ from those who drop out in significant but unmeasured ways, such as in level of motivation. Finally, for the four studies that looked only at change over time for a single cohort, validity is threatened as it is impossible to assess whether treatment effects are attributable to the interventions themselves, or would have occurred naturally over time.
Only two studies, Donohue et al. (2014) and Lam et al. (2009) performed independent diagnostic assessments to verify the presence of SA disorders in participants. It is possible that participants enrolled other studies would not meet DSM diagnostic criteria for a SA disorder. That being said, attendance in SA treatment is a likely indicator of at least a moderate level of dysfunctional substance use as individuals often resist attending treatment until they or someone else recognizes the problem as severe enough to warrant intervention.
In five studies that looked at outcome data on child adjustment, internal validity was diminished as these programs provided services such as enriched or therapeutic daycare directly to the children (Field et al., 1998; Conners et al., 2001; Conners et al., 2006; Killeen & Brady, 2000 and Niccols & Sword, 2005). It is impossible to determine whether the improvements in child outcomes seen in these studies were attributable to changes in parenting, or were the result of the direct clinical contact children received.
In terms of child age, programs that provide services to parents of children of all ages lend themselves to greater generalizability. However, it is questionable whether such interventions can adequately address the specific needs of parents of children in different stages of development. Demands on parents change dramatically as children age. Infants require intensive and sustained attention and near constant parental availability to fulfill needs. Toddlers and young children require parents to teach daily life skills, provide enriching and stimulating environments and use effective limit setting to establish behavioral expectations. Older children and adolescents require parents to act as role models, attend to academic and emotional needs, monitor peer groups and prevent risky behavior. Programs that focus on parents’ immediate needs based on their children’s current ages may have the greatest immediate impact, yet focusing only on a small age-range may leave parents without comparable knowledge of what to do as their children age into other phases of development. The majority of literature supports the notion that the earlier one intervenes the better however, there is likely value, and certainly need for interventions with parents of older children as well. The ideal timing of interventions for parents remains a question and without longitudinal follow-ups it is not possible to evaluate best practices in this area.
Child welfare status is another important variable that should be considered when evaluating study participation and outcome data. No study that included CPS or mixed samples described the nature of the parents’ CPS involvement such as how much contact they had with their children or their custody statuses. This information is vital to assessing the validity of outcomes as parents who have limited or no contact with their children cannot practice newly learned skills or accurately report on behavioral changes. They may answer outcome measures that ask about the use of specific parenting strategies based on what they think they would do, but do not have the chance to actually use the skills.
Complicating the issue further are mixed findings on the effect removing children from the home has on parents’ motivation to engage in treatment. Some research has found that removal of children from a parents’ care is a motivating factor for parents to participate in treatment, while other research has found that mothers who have restricted contact with their children may have reduced motivation for participation in the dual treatment studies. Some data suggest that mothers may actually increase their drug use when children are removed as a method of coping with their loss, and because of lessened maternal demands, while mothers who remain with their children are more likely to attempt to limit their drug use to times when the children are not around (Lam, Wechsburg & Zule, 2004). Future research is needed to clarify the extent to which the child’s placement out of home predicts treatment participation (Magura et al., 1999; Donohue et al., 2014) and to determine what is best practice, both for parents and their children.
Interpretation of study outcomes is also affected by the researchers’ choice of outcome measures. Studies relied heavily on self-report measures which are subject to inaccurate recall and dishonest reporting, especially if respondents’ cognitive capacities are diminished by drug states (Conners et al., 2004). Inclusion of observational assessments increases reliability and validity of data and helps researchers to determine the degree to which parents with SA can accurately report on their parenting.
Three studies assessed parenting outcomes only via the self-report measure, the Parenting Stress Index (Conners et al., 2001; Killeen & Brady, 2000; Magura et al., 1999). While these studies found significant reductions in parental stress, improvements in this area do not necessarily tell us about changes in parents’ use of different parenting skills. Inclusion of more behaviorally-based measures or observational data in these studies would have helped determine program impact more directly.
Timing of intervention components differed across studies and this is an important variable to consider when designing future treatments. Simultaneous participation in SA treatment and parenting interventions maximizes efficiency and takes advantage of parents’ engagement in the treatment process. Given the time pressures placed on parents by most CPS offices, simultaneous dual-treatment provides parents with the best chance of successfully completing child welfare mandates for SA recovery and parenting intervention in a timely manner. On the other hand, some researchers theorize that parents are not able to successfully address parenting and parent-child relationship concerns until they have made progress in SA treatment and have addressed their own underlying psychological needs (Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al., 2011). Four studies included participants in the parenting intervention only if they had already been involved in drug treatment for at least a few months (Catalano et al., 1999; Dawe et al., 2003; Dawe & Harnett, 2007; Berlin et al., 2014). Offering parenting interventions only after successful participation in SA treatment skews the sample towards those who have already demonstrated motivation and commitment to change, limiting generalizability.
Four studies utilized a hybrid model in which parents participated in SA treatment and a parenting intervention simultaneously, but the first half of the parenting program addressed parents’ psychological wellbeing and emotional coping generally before the second half taught specific parenting skills (Luthar et al., 2007; Luthar & Suchamn, 2000; Suchman et al., 2008; Suchman, DeCoste, Castiglioni et al., 2010; Suchman et al. 2011). The resulting beneficial outcomes of these four hybrid-model studies point to the potential need to address emotion regulation as the primary and most important of the pathways linking SA and parenting difficulties. Learning emotional coping strategies may help parents build a foundation from which they can learn to manage the psychosocial stressors, child behavior problems and triggers of prior drug use that they are bound to face.
Notably, only two studies, Camp and Finkelstein (1999) and Belcher et al. (2005), mentioned taking cultural considerations into account in implementing their interventions. Given the great degree of racial and ethnic diversity among the parents who abuse substances and struggle with parenting difficulties, this was surprising. A large body of research on parenting interventions has consistently revealed that parenting is a highly culturally-mediated endeavor. Parents’ expectations for their children and the values and skills they seek to instill in them differ markedly based on cultural background. For low-income families and racial minorities in particular, parents must help their children achieve success in the face of limited resources and the prospect of prejudice and hostility. For these children, emotional adjustment is not just a matter of parents’ discipline strategies and family rules, but also how parents socialize their children to see themselves and their culture in the context of the world (Coard, Wallace, Stevenson, & Brotman, 2004; Coard, Foy-Watson, Zimmer, & Wallace, 2007). Lack of recognition or acknowledgement of cultural diversity in choosing or designing interventions that help parents improve their parenting is an oversight that should be addressed in future intervention studies.
Finally, study setting played a role in treatment retention and effectiveness. Studies that took place at inpatient treatment facilities might be expected to result in superior retention rates as these settings provide safe and secure living arrangements, often allow children to stay with their parents and let parents focus on recovery without the distraction and pressures of life outside the facility’s walls. Surprisingly, retention rates in such programs were not better than their outpatient counterparts (see Table 2). It is possible that parents in inpatient services struggle with the reduced independence and intense demands of residential treatment, and that a higher risk sample is referred to these inpatient settings to begin with. Studies that took place in participants’ homes had the highest retention rates (Schaeffer et al., 2013; Donohue et al., 2014; Field et al., 1998; Catalano et al., 1999) as parents did not have to take initiative to arrange for transportation or child care to attend outpatient treatment and did not have to give up their independence to attend residential treatment (Schaeffer et al.).
Recommendations
The review yielded several recommendations described below, for dual treatment research, strengthening of interventions, and for public policy.
Study Methodology and Research
-
1
Internal validity can be improved by greater use of randomized controlled designs, by utilizing stratification on important variables like CPS involvement, and by equating experimental and control conditions with respect to number of hours of clinical contact. External validity can be improved by consistent use of intent-to-treat analyses. RCT designs might fit better in outpatient SA treatment centers where there is a high volume of clients and intervention protocols can be integrated into the ecology of the setting. Furthermore, assessment of treatment fidelity should be done to insure quality implementation of interventions.
-
2
Mixed-methods outcome assessments such as biological assays of substance use and independent evaluations of parenting skills would enhance accuracy and validity, and might also mitigate the presentation bias inherent in self-report measures. With respect to parenting, assessments of specific parenting practices might be preferable over focusing only on parenting stress.
-
3
Studies that involve parents with open CPS cases would be better served by taking into account the amount of contact parents have with their children as a potential covariate or moderator of parenting outcomes.
-
4
Increasing the number and duration of follow-up time points may help to elucidate the long-term effects of dual treatment, and may help to pinpoint the conditions under which treatment effects are sustained.
Intervention Strategies
-
5
It makes sense to enroll parents concurrently in SA treatment and parenting intervention, as opposed to delaying the parenting intervention for months. However, there is a caveat. Parents seem to benefit most when the parenting intervention begins with fundamental psychological processes such as developing emotional regulation mechanisms, before teaching specific parenting techniques such as effective discipline strategies.
-
6
Interventions might be more successful when family members and significant others are involved in treatment. Including families might help parents avoid regression associated with the abrupt termination of services. It is recognized that some individuals are markedly isolated, which might necessitate yoking these parents with treatment partners. Additionally, cultural considerations should be taken into account when choosing or designing interventions for this diverse population.
-
7
Common obstacles to session attendance include lack of transportation, hunger, unsupervised children and stigma. Interventions need planned strategies for addressing each of these such as providing vouchers or courtesy rides, meals, child care and a safe, supportive and non-judgmental environment.
Policy
-
8
Parents who are involved with CPS while struggling with substance abuse face conflicting demands. Child welfare agencies are financially and politically pressured to find permanent placements for children who have been removed from their homes within an expedited time-frame, but successful SA treatment requires parents to devote a sufficient amount of time to recovery (Dauber et al., 2012). Policies that require parents to decide between fulfilling child care goals and completing drug treatment place them in the unfortunate situation where either choice may be considered wrong by influential authority figures (Jansson & Velez, 1999).
Policy changes are needed for example, to improve communication and cooperation between CPS workers and intervention staff. In this realm, some of the shared goals include structuring child visitation to optimize parenting interventions, overcoming obstacles to treatment participation, and promoting a safe environment for parents to progress.
Highlights.
Parental substance abuse and parenting difficulties dually threaten public health.
The nature and quality of dual-treatment outcome studies are reviewed.
Multiple pathways and conceptual frameworks inform this area.
Methodological rigor varied but positive outcomes were observed.
Methodology, interventions, and public policy can and should be strengthened.
Acknowledgments
Work on this article was supported in part by NIGMS and NIDA of the National Institutes of health under award numbers T32GM081740 and R01DA031780. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Glossary
- SA
Substance Abuse
- CPS
Child Protective Services
Footnotes
Author Disclosure
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome. Study sponsors had no role in the design, collection, analysis, interpretation of any data included in this manuscript nor did they have any role in the writing of this report or the decision to submit the paper for publication.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abidin RR. Parenting Stress Index: A measure of the parent–child system. In: Zalaquett CP, Wood RJ, editors. Evaluating stress: A book of resources (277–291) xvii. Lanham, MD, US: Scarecrow Education; 1997. p. 474. [Google Scholar]
- Appleyard K, Berlin LJ, Rosanbalm KD, Dodge KA. Preventing early child maltreatment: Implications from a longitudinal study of maternal abuse history, substance use problems, and offspring victimization. Prevention Science. 2011;12(2):139–149. doi: 10.1007/s11121-010-0193-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold DS, O’Leary SG, Wolff LS, Acker MM. The Parenting Scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment. 1993;5:137–144. [Google Scholar]
- Barnard M, McKeganey N. The impact of parental problem drug use on children: what is the problem and what can be done to help? Addiction. 2004;99(5):552–559. doi: 10.1111/j.1360-0443.2003.00664.x. [DOI] [PubMed] [Google Scholar]
- Beeghly M, Frank DA, Rose-Jacobs R, Cabral H, Tronick E. Level of prenatal cocaine exposure and infant–caregiver attachment behavior. Neurotoxicology and Teratology. 2003;25(1):23–38. doi: 10.1016/s0892-0362(02)00323-9. http://dx.doi.org/10.1016/S0892-0362(02)00323-9. [DOI] [PubMed] [Google Scholar]
- Belcher HME, Butz AM, Wallace P, Hoon AH, Reinhardt E, Reeves SA, Pulsifer MB. Spectrum of early intervention services for children with intrauterine drug exposure. Infants & Young Children: An Interdisciplinary Journal of Special Care Practices. 2005;18(1):2–15. [Google Scholar]
- Belt R, Punamäki RL. Mother-infant group psychotherapy as an intensive treatment in early interaction among mothers with substance abuse problems. Journal of Child Psychotherapy. 2007;33(2):202–220. doi: 10.1080/00754170701437096. [DOI] [Google Scholar]
- Berlin LJ, Shanahan M, Carmody KA. Promoting supportive parenting in new mothers with substance-use problems: A pilot randomized trial of residential treatment plus an attachment-based parenting program. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Monuteaux MC, Feighner JA. Patterns of Alcohol and Drug Use in Adolescents Can Be Predicted by Parental Substance Use Disorders. Pediatrics. 2000;106(4):792. doi: 10.1542/peds.106.4.792. [DOI] [PubMed] [Google Scholar]; Infant Mental Health Journal. 35(1):81–85. doi: 10.1002/imhj.21427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borelli JL, West JL, Decoste C, Suchman NE. Emotionally avoidant language in the parenting interviews of substance-dependent mothers: Associations with reflective functioning, recent substance use, and parenting behavior. Infant Mental Health Journal. 2012;33(5):506–519. doi: 10.1002/imhj.21340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camp JM, Finkelstein N. Parenting training for women in residential substance abuse treatment: Results of a demonstration project. Journal of Substance Abuse Treatment. 1997;14(5):411–422. doi: 10.1016/s0740-5472(97)00004-4. http://dx.doi.org/10.1016/S0740-5472(97)00004-4. [DOI] [PubMed] [Google Scholar]
- Carroll KM. Methodological issues and problems in the assessment of substance use. Psychological Assessment. 1995;7(3):349–358. http://dx.doi.org/10.1037/1040-3590.7.3.349. [Google Scholar]
- Catalano RF, Gainey RR, Fleming CB, Haggerty KP, Johnson NO. An experimental intervention with families of substance abusers: one-year follow-up of the focus on families project. Addiction. 1999;94(2):241–254. doi: 10.1046/j.1360-0443.1999.9422418.x. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20(3):191–203. doi: 10.1016/s0145-2134(95)00144-1. http://dx.doi.org/10.1016/S0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Kipp HL, Baumann BL, Lee SS. Psychopathology and Substance Abuse in Parents of Young Children With Attention-Deficit/Hyperactivity Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(12):1424–1432. doi: 10.1097/00004583-200312000-00009. [DOI] [PubMed] [Google Scholar]
- Clausen JM, Aguilar RM, Ludwig ME. Fostering healthy attachment between substance dependent parents and their infant children. Journal of Infant, Child & Adolescent Psychotherapy. 2012;11(4):376–386. doi: 10.1080/15289168.2012.735183. [DOI] [Google Scholar]
- Coard S, Wallace S, Stevenson H, Jr, Brotman L. Towards Culturally Relevant Preventive Interventions: The Consideration of Racial Socialization in Parent Training with African American Families. Journal of Child and Family Studies. 2004;13(3):277–293. doi: 10.1023/B:JCFS.0000022035.07171.f8. [DOI] [Google Scholar]
- Coard SI, Foy-Watson S, Zimmer C, Wallace A. Considering Culturally Relevant Parenting Practices in Intervention Development and Adaptation: A Randomized Controlled Trial of the Black Parenting Strengths and Strategies (BPSS) Program. The Counseling Psychologist. 2007;35(6):797–820. doi: 10.1177/0011000007304592. [DOI] [Google Scholar]
- Conners NA, Bradley RH, Mansell LW, Liu JY, Roberts TJ, Burgdorf K, Herrell JM. Children of Mothers with Serious Substance Abuse Problems: An Accumulation of Risks. American Journal of Drug & Alcohol Abuse. 2004;30(1):85–100. doi: 10.1081/ADA-120029867. [DOI] [PubMed] [Google Scholar]
- Conners NA, Bradley RH, Whiteside-Mansell L, Crone CC. A comprehensive substance abuse treatment program for women and their children: an initial evaluation. Journal of Substance Abuse Treatment. 2001;21(2):67–75. doi: 10.1016/s0740-5472(01)00186-6. http://dx.doi.org/10.1016/S0740-5472(01)001866. [DOI] [PubMed] [Google Scholar]
- Conners NA, Grant A, Crone CC, Whiteside-Mansell L. Substance abuse treatment for mothers: Treatment outcomes and the impact of length of stay. Journal of Substance Abuse Treatment. 2006;31(4):447–456. doi: 10.1016/j.jsat.2006.06.001. http://dx.doi.org/10.1016/j.jsat.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Dakof GA, Cohen JB, Henderson CE, Duarte E, Boustani M, Blackburn A, Hawes S. A randomized pilot study of the engaging moms program for family drug court. Journal of Substance Abuse Treatment. 2010;38(3):263–274. doi: 10.1016/j.jsat.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauber S, Neighbors C, Dasaro C, Riordan A, Morgenstern J. Impact of intensive case management on child welfare system involvement for substance-dependent parenting women on public assistance. Children and Youth Services Review. 2012;34(7):1359–1366. doi: 10.1016/j.childyouth.2012.03.020. http://dx.doi.org/10.1016/j.childyouth.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawe S, Harnett P. Reducing potential for child abuse among methadone-maintained parents: Results from a randomized controlled trial. Journal of Substance Abuse Treatment. 2007;32(4):381–390. doi: 10.1016/j.jsat.2006.10.003. http://dx.doi.org/10.1016/j.jsat.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Dawe S, Harnett PH, Rendalls V, Staiger P. Improving family functioning and child outcome in methadone maintained families: The Parents Under Pressure programme. Drug and Alcohol Review. 2003;22(3):299–307. doi: 10.1080/0959523031000154445. [DOI] [PubMed] [Google Scholar]
- Donohue B, Azrin NH, Bradshaw K, Van Hasselt VB, Cross CL, Urgelles J, et al. A controlled evaluation of Family Behavior Therapy in concurrent child neglect and drug abuse. Journal of Consulting and Clinical Psychology. 2014 doi: 10.1037/a0036920. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue BC, Romero V, Herdzik K, Lapota H, Al RA, Allen DN, Van Hasselt VB. Concurrent treatment of substance abuse, child neglect, bipolar disorder, post-traumatic stress disorder, and domestic violence: a case examination involving family behavior therapy. Clinical case studies. 2010;9(2):106–124. doi: 10.1177/1534650109351928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Feletti VJ, Croft JB, Edwards VJ, Giles WH. Growing up with parental alcohol abuse: exposure to childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2001;25:1627–1640. doi: 10.1016/s0145-2134(01)00293-9. [DOI] [PubMed] [Google Scholar]
- Dunn MG, Tarter RE, Mezzich AC, Vanyukov M, Kirisci L, Kirillova G. Origins and consequences of child neglect in substance abuse families. Clinical Psychology Review. 2002;22:1063–1090. doi: 10.1016/s0272-7358(02)00132-0. [DOI] [PubMed] [Google Scholar]
- Field T, Scafidi FA, Pickens J. Polydrug-using adolescent mothers and their infants receiving early intervention. Adolescence. 1998;33(129):111–43. [PubMed] [Google Scholar]
- George O, Le Moal M, Koob GF. Allostasis and addiction: Role of the Dopamine and corticotropin-releasing factor system. Physiology and Behavior. 2012;106:58–64. doi: 10.1016/j.physbeh.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Needell B, Shi Y, Hser Y. Do drug treatment services predict reunification outcomes of mothers and their children in child welfare? J Subst Abuse Trea. 2009;36(3):278–293. doi: 10.1016/j.jsat.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillson JMC, Kuiper NA. A stress and coping model of child maltreatment. Clinical Psychology Review. 1994;14(4):261–285. http://dx.doi.org/10.1016/0272-7358(94)90025-6. [Google Scholar]
- Jansson LM, Velez M. Understanding and Treating Substance Abusers and Their Infants. Infants and Young Children. 1999:79–89. [Google Scholar]
- Kandel DB. Parenting Styles, Drug Use, and Children’s Adjustment in Families of Young Adults. Journal of Marriage and Family. 1990;52(1):183–196. doi: 10.2307/352849. [DOI] [Google Scholar]
- Kelley SJ. Stress and Coping Behaviors of Substance-Abusing Mothers. JSPN. 1998;3(3):103–110. doi: 10.1111/j.1744-6155.1998.tb00215.x. [DOI] [PubMed] [Google Scholar]
- Kelleher K, Chaffin M, Hollenberg MS, Fischer E. Alcohol and Drug Disorders among Physical Abusive and Neglectful Parents in a Community-Based Sample. American Journal of Public Health. 1994;84(10) doi: 10.2105/ajph.84.10.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerwin ME. Collaboration between Child Welfare and Substance-Abuse Fields: Combined Treatment Programs for Mothers. Journal of Pediatric Psychology. 2005;30(7):581–597. doi: 10.1093/jpepsy/jsi045. [DOI] [PubMed] [Google Scholar]
- Killeen TCS, Brady KT. Parental stress and child behavioral outcomes following substance abuse residential treatment: Follow-up at 6 and 12 months. Journal of Substance Abuse Treatment. 2000;19(1):23–29. doi: 10.1016/s0740-5472(99)00078-1. http://dx.doi.org/10.1016/S0740-5472(99)00078-1. [DOI] [PubMed] [Google Scholar]
- Lam WKK, Fals-Stewart W, Kelley ML. Parent training with behavioral couples therapy for fathers’ alcohol abuse: Effects on substance use, parental relationship, parenting, and CPS involvement. Child Maltreatment. 2009;14(3):243–254. doi: 10.1177/1077559509334091. [DOI] [PubMed] [Google Scholar]
- Lam WK, Wechsberg W, Zule W. African–American women who use crack cocaine: A comparison of mothers who live with and have been separated from their children. Child Abuse & Neglect. 2004;28(11):1229–1247. doi: 10.1016/j.chiabu.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Lussier K, Laventure M, Bertrand K. Parenting and maternal substance addiction: Factors affecting utilization of child protective services. Substance Use & Misuse. 2010;45(10):1572–1588. doi: 10.3109/10826081003682123. [DOI] [PubMed] [Google Scholar]
- Luthar S, Cushing G, Merikangas KR, Rounsaville BJ. Multiple jeopardy: Risk and protective factors among addicted mothers’ offspring. Development and Psychopathology. 1998;10:117–136. doi: 10.1017/s0954579498001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S, Suchamn NE. Relatioanl Psychothearpy Mothers’ Group: A developmentally informed intervention for at-risk mothers. Development and Psychopathology. 2000;12(2):235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S, Suchman NE, Altomare M. Relational Psychotherapy Mothers’ Group: A randomized clinical trial for substance abusing mothers. Development and Psychopathology. 2007;19:243–261. doi: 10.1017/S0954579407070137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Laudet A, Kang SY, Whitney SA. Effectiveness of comprehensive services for crack-dependent mothers with newborns and young children. Journal of Psychoactive Drugs. 1999;31(4):321–338. doi: 10.1080/02791072.1999.10471763. [DOI] [PubMed] [Google Scholar]
- McComish JF, Greenberg R, Ager J, Essenmacher L, Orgain LS, Bacik WJ., Jr Family-Focused Substance Abuse Treatment: A Program Evaluation. Journal of Psychoactive. 2003 doi: 10.1080/02791072.2003.10400015. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. Journal of Nervous and Mental Disorders. 1980;168(1):26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Dierker LC, Szatmari P. Psychopathology among Offspring of Parents with Substance Abuse and/or Anxiety Disorders: A High–risk Study. Journal of Child Psychology and Psychiatry. 1998;39(5):711–720. doi: 10.1111/1469-7610.00370. [DOI] [PubMed] [Google Scholar]
- Miller BA, Smyth NJ, Mudar PJ. Mothers’ Alcohol and Other Drug Problems and Their Punitiveness toward Their Children. Journal of Studies on Alcohol. 1999:632–642. doi: 10.15288/jsa.1999.60.632. [DOI] [PubMed] [Google Scholar]
- Milligan K, Niccols A, Sword W, Thabane L, Henderson J, Smith A, Liu J. Maternal substance use and integrated treatment programs for women with substance abuse issues and their children: A meta-analysis. Substance Abuse Treatment, Prevention, and Policy. 2010;5 doi: 10.1186/1747-597X-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner JS. Assessing physical child abuse risk: The child abuse potential inventory. Clinical Psychology Review. 1994;14(6):547–583. [Google Scholar]
- Moore J, Finkelstein N. Parenting services for families affected by substance abuse. Child Welfare. 2001;80(2):221–238. [PubMed] [Google Scholar]
- Nair P, Schuler ME, Black MM, Kettinger L, Harrington D. Cumulative environmental risk in substance abusing women: Early intervention, parenting stress, child abuse potential and child development. Child Abuse & Neglect. 2003;27(9):997–1017. doi: 10.1016/S0145-2134(03)00169-8. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse Addiction Science: From Molecules to Managed Care series. Drug abuse costs the United States economy hundreds of billions of dollars in increased health care costs, crime and lost productivity. 2008 Retrieved from: http://www.drugabuse.gov/publications/addiction-science-molecules-to-managed-care/introduction/drug-abuse-costs-united-states-economy-hundreds-billions-dollars-in-increased-health.
- Niccols A, Milligan K, Sword W, Thabane L, Henderson J, Smith A. Integrated programs for mothers with substance abuse issues: A systematic review of studies reporting on parenting outcomes. Harm Reduction Journal. 2012;9 doi: 10.1186/1477-7517-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niccols A, Sword W. “New Choices” for substance-using mothers and their children: preliminary evaluation. Journal of Substance Use. 2005;10(4):239–251. [Google Scholar]
- Pajulo M, Suchman N, Kalland M, Mayes L. Enhancing the effectiveness of residential treatment for substance abusing pregnant and parenting women: Focus on maternal reflective functioning and mother-child relationship. Infant Mental Health Journal. 2006;27(5):448–465. doi: 10.1002/imhj.20100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PEW Charitable Trust. Child Abuse and Neglect Cost Nation over $100 Billion per Year. 2008 Retrieved from: http://www.pewtrusts.org/news_room_detail.aspx?id=34676.
- Ritter J, Stewart M, Bernet C, Coe M, Brown SA. Effects of Childhood Exposure to Familial Alcoholism and Family Violence on Adolescent Substance Use, Conduct Problems, and Self-Esteem. Journal of Traumatic Stress. 2002;15(2):113–122. doi: 10.1023/A:1014803907234. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Addiction. Annual Review of Psychology. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- Romero V, Donohue B, Allen DN. Treatment of concurrent substance dependence, child neglect and domestic violence: a single case examination involving family behavior therapy. Journal of Family Violence. 2010;25(3):287–295. doi: 10.1007/s10896-009-9291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero V, Donohue BC, Hill HH, et al. Family behavior therapy for use in child welfare: results of a case study involving an abused woman fomrally diagnosed with alcohol dependence, bipolar disorder and several anxiety disorders. Clinical Case Studies. 2010;9(5):353–368. doi: 10.1177/1534650110383306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeffer CM, Swenson CC, Tuerk EH, Henggeler SW. Comprehensive treatment for co-occurring child maltreatment and parental substance abuse: Outcomes from a 24-month pilot study of the MST-Building Stronger Families program. Child Abuse & Neglect. 2013;37(8):596–607. doi: 10.1016/j.chiabu.2013.04.004. [DOI] [PubMed] [Google Scholar]
- Shulman L, Shapira SA, Hirshfield S. Outreach Developmental Services to Children of Patients in Treatment for Substance Abuse. American Journal of Public Health. 2000;90(12):1930–1933. doi: 10.2105/ajph.90.12.1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade A. Parental reflective functioning: An introduction. Attachment & Human Development. 2005;7(3):269–281. doi: 10.1080/14616730500245906. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- Suchman NP, DeCoste C, Castiglioni N, Legow N, Mayes L. The Mothers and Toddlers program: Preliminary Findings From an Attachment-Based Parenting Intervention for Substance-Abusing Mothers. Psychoanal Psychol. 2008;25(3):499–517. doi: 10.1037/0736-9735.25.3.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, DeCoste C, Castiglioni N, McMahon TJ, Rounsaville B, Mayes L. The Mothers and Toddlers Program, an attachment-based parenting intervention for substance using women: Post-treatment results from a randomized clinical pilot. Attachment & Human Development. 2010;12(5):483–504. doi: 10.1080/14616734.2010.501983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, DeCoste C, Leigh D, Borelli J. Reflective functioning in mothers with drug use disorders: Implications for dyadic interactions with infants and toddlers. Attachment & Human Development. 2010;12(6):567–585. doi: 10.1080/14616734.2010.501988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Decoste C, McMahon TJ, Rounsaville B, Mayes L. The mothers and toddlers program, an attachment-based parenting intervention for substance-using women: Results at 6-week follow-up in a randomized clinical pilot. Infant Mental Health Journal. 2011;32(4):427–449. doi: 10.1002/imhj.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velez ML, Jansson LM, Montoya ID, Schweitzer W, Golden A, Svikis D. Parenting knowledge among substance abusing women in treatment. Journal of Substance Abuse Treatment. 2004;27(3):215–222. doi: 10.1016/j.jsat.2004.07.004. http://dx.doi.org/10.1016/j.jsat.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Whiteside-Mansell L, Crone CC, Conners NA. The Development and Evaluation of an Alcohol and Drug Prevention and Treatment Program for Women and Children: The AR-CARES Program. Journal of Substance Abuse Treatment. 1999;16(3):265–275. doi: 10.1016/s0740-5472(98)00049-x. http://dx.doi.org/10. [DOI] [PubMed] [Google Scholar]