Abstract
Background
The Self-Management and Care of Heart Failure through Group Clinics Trial (SMAC-HF) evaluated the effects of multidisciplinary group clinic appointments on self-care skills and rehospitalizations in high risk heart failure (HF) patients.
Objective
The purpose of this article is to: (1) describe key SMAC-HF group clinic interactive learning strategies; (2) describe resources and materials used in the group clinic appointment; and (3) present results supporting this patient-centered group intervention.
Methods
This clinical trial included 198 HF patients (randomized to either group clinical appointments or to standard care). Data were collected from 72 group clinic appointments via patients’: (1) group clinic session evaluations; (2) HF Self-Care Behaviors Skills; (3) HF related discouragement and quality of life scores and (4) HF related reshopitalizations during the 12 month follow-up. Also the costs of delivery of the group clinical appointments were tabulated.
Results
Overall, patients rated group appointments as 4.8 out of 5 on the “helpfulness” in managing HF score. The statistical model showed a 33% decrease in the rate of rehospitalizations (incidence rate ratio (IRR) = 0.67) associated with the intervention over the 12-month follow-up period when compared with control patients (χ2(1) = 3.9, p = 0.04). The total cost for implementing five group appointments was $243.58 per patient.
Conclusion
The intervention was associated with improvements in HF self-care knowledge and home care behavior skills and managing their for HF care. In turn, better self-care was associated with reductions in HF related hospitalizations.
Keywords: Heart Failure, group clinic appointments, rehospitalizations
Background
The cost for heart failure (HF) in the US for 2009 was $37.2 million and is estimated increase to $69.7 billion in 2030, 80% due to hospitalizations.1 Of the 1 million HF hospital admissions in the United States (US) each year on average, 18%, 50% and 60% of these patients are readmitted within 30 days2 and 6 and 9 months respectively.3 Studies indicate that up to 70% of heart failure (HF) readmissions are preventable if patients had better self-management skills.4,5
Many hospital discharge and nursing follow-up programs are designed to improve HF knowledge without emphasis on developing patients’ daily HF self-care skills. Yet, many patients lack understanding of medication adherence and the importance of sodium intake limits, and they do not have the skills to recognize and report the symptoms of HF decompensation. 6,7 Data from 10 clinical trials of HF management programs suggested that programs employing multidisciplinary teams and in-person communication led to fewer HF hospital readmissions.8 Indeed, high risk HF patients (advanced stage, low self-care skills, elderly, and those with frequent readmissions) could benefit the most from skill-building programs.9
The Self-Management and Care of Heart Failure through Group Clinics Trial (SMAC-HF) is a randomized controlled trial evaluating the effects of nurse practitioner (NP) facilitated, multidisciplinary HF group clinic appointments among higher risk patients.10 The SMAC-HF intervention includes five clinic appointments where four to eight patients recently discharged from the hospital for HF decompensation are seen by multiple professionals. The scientific basis of this clinical trial is the Chronic Care Model (CCM),11 which emphasizes engaging patients in self-management partnerships with multiple professionals12,13,14,15 The purpose of this article is to: (1) describe key SMAC-HF group clinic interactive learning strategies; (2) describe resources used in the group clinic appointment; and (3) present results supporting this patient-centered group intervention.
In group appointments, patients who face a common health disorder are seen by multidisciplinary health professionals and, as a group, address the self-management priorities of their illness.16,17 Group appointments have been successfully used for patients with a variety of cardiovascular and other chronic diseases.18 Studies have repeatedly found significantly greater patient satisfaction ratings with their medical care in group clinics than in individual appointments.19,20 Wagner and colleagues found with frail elders and patients with diabetes; that group clinic participants had greater overall health status, and received more health education and preventive care services.21, 22,23,24 In large Kaiser Permanente randomized trials of group visits, chronically ill elder adults with heart failure and with poorly controlled diabetes had greater quality of life scores and required significantly fewer specialists or ER visits compared to controls.25,26 Research on HF group visits have shown positive patient outcomes in increased knowledge, medication adherence and care satisfaction 27,28,29,30,31,32 However, group appointment studies rarely include only NY Class III and IV patients, who are at the highest risk for rehospitalization, or measure HF-related rehospitalizations, as in this study.
Methods
This design is a classic clinical trial using random assignment to either the experimental group clinic intervention or standard care. The design complies with the CONSORT standards describing scientific processes expected in clinical trial reports33 and represents a rigorous methodology for comparing treatment to controls. Analyses used negative binomial regression to assess the magnitude of effect of the intervention on rates of post-intervention rehospitalization due to heart failure. The regression included factors posited an a priori to clinically influence rehospitalizations for HF and other group comparisons on questionnaire scores.
Measures
Measures for this analysis included patients’ HF self-management skills, HF knowledge, HF related discouragement, quality of life, and symptom severity/frequency scores. HF related rehospitalizations and Group Clinic Appointment Evaluations were summarized by reviewers blinded to group assignment. 34,35 All scores were measured at baseline, 6 and 12 months post-intervention follow-up using the empirically validated methods and rating scales in Table 1.
Table 1.
Measures1 Operational Definitions and Reliability & Validity noted
| Measures | Operational Definition (Collected 6 and 12 months post-intervention) | Reliabilitya,b,c Validityd,e,f |
|---|---|---|
| Kansas City Cardiomyopathy Questionnaire (KCCQ) 70 | HF-related quality of life, symptom frequency & severity, sense of discouragement relative to having HF. | 23-item Likert.a,c,d,e α = 0.90.a |
| The European Heart Failure Self Care Behavior Scale71,72 | HF self-care skills practiced daily (maintaining their daily medications, fluid and sodium restrictions, monitoring HF symptoms Information about HF home management |
9-item Likerta α=.81 |
| HF Knowledge Questionnaire.73 | HF knowledge (i.e., What is the sodium intake per day for HF patients?) | 8 multiple choice items, KR21 = 0.70 |
| Patients’ HF rehospitalizations. Each occurrence was classified as HF-related hospitalization or not. | Adjudicated by MDs blinded to group by using an a priori determined adjudication definition of HF (based on other NIH funded clinical trials)74 | 3-item Likerte,f |
| Group Appointment Helpfulness Evaluation Scale.75 | Participants were asked to anonymously rate their group clinic experience in helping them manage their HF. | 8-item Likertc,d,e α=.86 (1 = not helpful to 5 = very helpful) |
These measures have confirmed discriminant or construct validity, internal consistency and reliability, and established specificity from large populations of HF patients. These measures also have published scores/standard deviations that distinguish clinically significant differences and are verified to be sensitive to change over time.
Sample
All patients (n=198) enrolled in the study were adults hospitalized due to exacerbation or decompensation of HF and gave written consent to participate. Participants randomized to the group clinic intervention (N=92) compared to the standard care control group (N=106) did not vary in age (mean 62.3, SD = 13.2 years), gender (38% female), ethnicity, socioeconomic status, education, depression level, mean left ventricular EF (30%), comorbidities, or number of deaths and attrition across the 12-month follow-up. Attrition was low in both groups, less than seven per each group.
Group Clinic Appointment Intervention
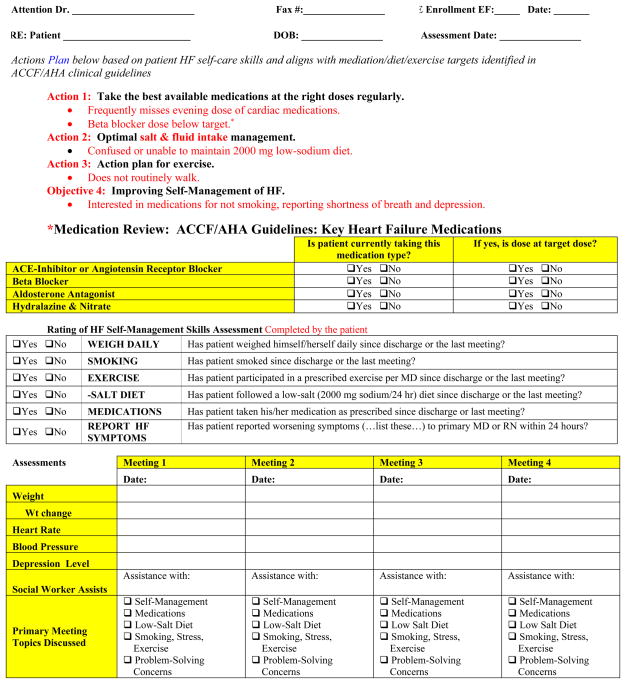
Fundamental learning strategies of this intervention are providing American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 36 self-care guidelines illustrated in DVD and supportive group facilitation to engage participants in patient-centered discussions related to daily HF management. Table 2 describes patient group discussion guidelines and training provided to the multidisciplinary professionals for facilitating the group clinic appointments. Further, during group clinics, patients practiced assessing their own HF symptoms, managing any discouragement, and establishing HF self-care skills such as adhering to daily medications using the pill box organizer. Also patients listed questions and information to discuss with their primary care providers (see Figure 1).
Table 2.
Clinic Guidelines and Staff Facilitation Training for Group Discussion.
| Discussion Guidelines | Group Facilitation Strategies Used |
|---|---|
|
Patient Group Introduction and “Ground Rules.” The multidisciplinary professionals and patients sat around a table together. Name tags (first name only) were used in the group. |
|
| The NP facilitator and health professionals were trained in motivational counseling techniques, to promote group information sharing and to refrain from lecturing to the group since the HF self-care content is presented in the DVDs. |
|
| Professionals were trained in specific protocols to manage any patient who becomes emotional, angry, or derogatory. |
|
| The health professionals provided problem-solving guidance, if the group reached an impasse or required reinforcement of problem-solving skills. |
|
Figure 1.
HF Self-Management Summary Report: Patient/Provider Action Recommandations.
Group Clinic Appointment Implementation
In this trial, each patient randomized to the intervention group was invited to a total of five, 2-hour group clinic appointments with four to eight other patients. For each clinic session, a patient-centered agenda with time allotments was used as an overall guide (Table 3). Twice in the 72 group clinic appointments, there were variations in the agenda time schedule when patients were taken to the ER due to acute symptoms or during a patient’s emotional reaction. Across the 72 group sessions in this trial, the strongest and most frequent emotions expressed were frustration, grief, and mild anger due to HF required lifestyle changes, declining physical stamina, and discouragement related to the HF diagnoses.37 Such issues were planned for and managed skillfully, and the routine agenda was resumed after a halt for the situation to be managed.
Table 3.
Group Clinic Appointment Agenda.
| Minutes | Patient-Centered Agenda Protocol |
|---|---|
| 15 | A brief HF self-management assessment exam of weight, vital signs, and a chart review of current medication orders. |
| 5 | Introductions (by first names only), name tags and HIPPA health protections and confidentiality pledge reminders. |
| 15 | View the short DVD for that week and HF home care skills identified. |
| 70 | Facilitated group discussions: Patient problem identification with solutions generated from patients and professionals practice of HF home care skills. |
| 15 | Each clinic appointment ended with completion of the HF Self-Management Summary report including the Patient/Provider Action Plan recommandations for each patient, that are then faxed to their primary care provider (see Figure 1). |
Note: The average of each clinic appointment length was 2 hours with four to eight patients participating. The first four appointments occurred weekly post hospital discharge for an exacerbation of HF, and the fifth appointment occurred approximately 6 months later as a reinforcing booster.
Four health professionals, each with HF care experience, were present at each clinic: (1) a nurse practitioner (NP) with HF outpatient care background; (2) a mental health clinical nurse specialist; (3) a social work case manager; and (4) a dietitian. Other professionals such as physical therapists (to guide exercise) and pharmacists (to discuss medications) could be invited to group sessions. However, to maintain standardization of the SMAC-HF intervention and the lower cost of these clinics, only these four professionals were included.
Resources and Materials Used in the Group Clinic Appointment
HF Self-Management DVDs were developed during a previous NIH grant according to television broadcast standards.38 Unique to the DVD series is the inclusion of 13 ethnic groups of young and older adult HF patients, the visual displays of the signs of worsening HF, and the illustration of simple memory aids that convey key skills of HF self-management. The DVDs illustrate over 20 examples of patients and professionals working together to manage the complexities of HF.
A focus group of cardiologists, registered nurses, and dieticians all evaluated the DVDs as accurately illustrating the essential ACCF/AHA HF education elements and condensing scientifically-based information into layman’s language (5th grade reading level) according to criteria for health literacy.39 Use of the audiovisual DVD method supported patients with low health literacy while also providing a standardized, replicable method of delivering HF self-management information for the trial.40
At each group clinic, following discussion of the DVD topics, the group practiced HF home-care skills using the provided HF monitoring resources and materials (Table 4). The checklists and monitoring resources, materials and strategies practiced in each group clinic appointment were given the “Innovation in Practice Award” by the American Association of Heart Failure Nurses in 2008.41 The DVDs earned the International Health and Medical Media Award42 in 2007 and then the booster DVD won the national Robert Wood Johnson ‘Innovations for Better Transitions in Care’ video award. 43
Table 4.
Resources and Materials Used in the Group Clinic Appointment.
| Resource and Materials | Description and Protocols |
|---|---|
| HF Self-Management skills illustrated in the DVDs (viewed prior to discussion) are then practiced during the clinic appointment. |
|
| Daily HF Monitoring Checklist and Early Symptom Reporting list. Daily HF self-monitoring one-page, double-sided checklist chart used for 12 weeks to establish a habit of self-monitoring. | Patients are directed to:
|
| List of common signs and symptoms associated with worsening HF and intolerance to HF medication that prompts early recognition and reporting of decompensation. |
|
| Other materials provided and used for practice in the group sessions |
|
Results
Patients’ Clinic Helpfulness Evaluations Ratings
The 92 patients randomized to the intervention group clinics attended 4.6 out of 5 appointments on average. Patients rated the group clinic appointments and the initial and booster DVDs as very helpful, generating cumulative averaged “helpfulness” scores of 4.7, 4.4, and 4.8 (out of 5), respectively. No patients rated any clinic appointment as a “1” (not helpful), and only one patient rated one appointment as a “2” (a little helpful), explaining that her decreased hearing prevented her from fully participating in the group discussions. The majority of patients wrote additional comments, indicating that “talking about” and “sharing opinions with others” were the best ways to learn how to cope and manage their HF. Each of the key elements in the American College of Cardiology Foundation/American Heart Association clinical guideline were found to be topics during the discussion sessions.
Rehospitalizations Related to Heart Failure
Factors posited a priori to affect HF rehospitalization were: (1) random assignment to intervention or not; (2) patient’s KCCQ total symptom frequency and severity score; their HF related quality of life and discouragement about HF scores and (3) patient’s HF knowledge and self-care behavior skills scores.
Due to the large number of subjects in both groups without a rehospitalization during the post-intervention follow-up period, zero-inflated Poisson regression was used to estimate the magnitude of effect of the intervention on rates of post-intervention rehospitalization due to heart failure (HF) at 1 year. The Poisson model showed a 33% decrease in the rate of rehospitalizations (incidence rate ratio (IRR) = 0.67) associated with the intervention over the follow-up period when compared with controls (χ2(1) = 3.9, p = 0.04). The zero-inflated logistic model included the predictor KCCQ total symptom score at baseline, showing baseline total symptom scores were predictive of the risk of rehospitalization for HF during the follow-up period (χ2(1) = 7, p < 0.01). Specifically, subjects with a lower total symptom score at baseline were significantly more likely to remain rehospitalization-free at 1 year—for every one-unit decrease in total symptom score, the odds of rehospitalization decreased by 3% (OR = 1.03, est = 0.03, SE = 0.009).
Patients HF Self-care Skills Use
The group clinic intervention patients as well as the standard care patients were asked to track on checklists from daily to never, which specific aspects of their own HF self-care they undertook including whether they weighed, used a low sodium diet, limited their fluids, and took all prescribed medications. At the 6-month follow-up, there was a significant improvement found in the intervention group (χ2 = 4.92, p =.03) on recognizing HF exacerbation symptoms and reporting these to their healthcare providers. At the 12-month follow-up, using t-test statistics, a significantly greater number of clinic group versus the standard care patients reported that they used a checklist/calendar to monitor their daily weight (t= 2.11, p=.04). At 6 and 12 months, a significantly greater percentage of patients in the group clinics had improved HF self-care skills of reducing salt intake, taking HF medications, and exercising than did standard care patients (χ2= 4.99, P=.03).
The results from the HF self-management knowledge data were similar in that patients were able to name: 1) the milligram/ounces limits of daily fluid and sodium intake, 2) symptoms of HF exacerbation; and 3) their HF medications. The group clinic patients had significantly greater knowledge scores than controls post SMAC-HF sessions (t=2.26, p=0.05) and again at follow-up (t=2.76, p=0.01).
KCCQ Quality of Life and Depression Scores
The HF-related quality of life scale data revealed a significant improvement (p=.000) from baseline to 12 months of one-half standard deviation in both groups, with no significant difference found between groups. Likewise, on the discouraged by HF rating (depression score), both groups had improvement from baseline to 12 months. However, at 12 months a greater percentage of patients in the group clinics (26%) scored as having no or rare feelings of discouragement versus 18 % in the control group.
Intervention Costs
All costs for administering the group clinics were tabulated to be $243.58 per participant for all five groups. Costs included time of the professionals participating for the group clinic 2 hour sessions (nurses, dietitian and social workers payroll reimbursement), the DVD series, the medication pill organizer, handout printing costs and the low sodium reference guide.
Discussion
As shown in this study, building patients’ HF self-care skills and knowledge, recognition of HF symptoms, and managing their discouragement related to HF should be intervention strategies used to reduce HF-related hospitalization.44,45,46,47, 48 It is essential for patients’ to practice HF symptom monitoring and reporting to professionals and to incorporate self-care skills in their daily routine.
Notably quality of life increased in both groups, likely due to patient’s improvements of their HF exacerbation symptoms during the index hospitalization. Also, the mental health nurse specialist guided discussion of ways to manage discouragement, frustration and grief related to reduced functional capacity and limited social activities because of their HF with all patients who had depressive scores.49, 50 Thus input from the mental health professional and encouragement from other patients in the group addressed patients discouragement with their HF. The greater reduction in frequency of discouragement in group clinic patients is likely due to their shared understanding that depression is a common and a recurring component of HF to be monitored daily. 51
Although there have been other HF group clinics described in the literature;52,53 the SMAC-HF trial intervention is unique in several ways. The SMAC-HF problem-solving approach engaged patients in actual use of self-care skills and working with professionals. This approach has been found to increase patient-professional partnerships and results in increased patient symptom self-management, improved physical status, and emotional health. Patient and health professional relationships were also maintained over time when problem-solving partnerships developed.54
Another unique strategy in SMAC-HF was the self-management report that patients completed at the end of every clinic appointment. On this report patients identified HF self-management questions for their Provider Patient Action Plans. The professionals coached patients to discuss these questions with their primary providers.55 Completing the Action Report fostered active participation and emphasized the patient’s responsibility for monitoring their HF daily and reporting untoward symptoms. This patient-centered action plan report gave patient ownership for the written details of their HF status and the “words” for talking to their primary health providers about their specific regimen.
Notably, recent national report approximately 25% of Medicare patients with HF are rehospitalized within 30 days after hospital discharge for HF,56 40 to 60% are rehospitalized within 12 months, and 12 to 31% of patients die of their HF within 12 months.57 Therefore the results of this study of reducing HF readmissions by 33% across 12 months are promising. Considering the escalating costs and the high rehospitalization rates for HF, the impact of this comprehensive, multidisciplinary intervention should be replicated and retested.58 It is possible that group clinics may “bridge the gap” in the HF self-management skill deficits that exist in the transition between hospital and home.59,60 Also, having NPs facilitate HF patients in incorporating self-care practices into their everyday lives may relieve the current and rapidly increasing physician shortage.61,62,63 This analysis assessed the impact of repeated hospitalizations for HF of all subjects during the entire follow up period. This aligns with the analyses of time till first HF related hospitalization which was significantly delayed in the intervention group for the first six 6 months.64 The cost of these patient appointments is less than the reimbursement currently provided by Medicare for group education. And the cost is certainly less than the charges for an ER visit or rehospitalization that could be avoided by patients with HF home care skills or out-of-pocket costs for HF care reported by families.65
Study Limitations
Overall, the intervention was associated with improvement in patients’ HF self-care behaviors and less discouragement about having HF. In turn, better self-care and less discouragement have been associated with reduced risk for having HF related rehospitalization.66,67,68 Study limitations were identified. First, the personnel time used for tabulating costs of the intervention were based on the recorded length of each group clinic. Yet detailed data could not be collected as to the length of time some patients spent having short discussions/referrals with clinic professionals either before or after the clinic appointments. Personnel cost is the major component of the total intervention cost. Therefore, this additional personnel time data should be collected and used in future clinic cost tabulations. We did not include any administrative costs such as personnel time for appointment scheduling of group clinic patients and reminder telephone calls for their appointments nor for the use of the office space for the clinic sessions. 69 In the future, including such administrative fees will provide a more realistic picture of group clinic resource needs and costs. Another limitation is we did not enroll family members in the SMAC-HF program. Thus an important change for SMAC-HF would be involving family caregivers in the group education and discussion sessions. The ACCF/AHA national guidelines for HF care state that close monitoring of symptoms by family members is possibly the most effective but least utilized recommendation.
Summary
The SMAC-HF trial evaluated the effects of low cost NP-facilitated multidisciplinary group clinic appointments. During these group clinics, patients practiced self-care skills of medication schedule adherence, maintaining sodium/fluid restrictions, and monitoring and reporting symptoms early as illustrated in our HF DVDs. The clinic professionals guided practice of HF self-care and patient-centered group discussions. These NPs facilitated groups clinics lead to statistically lower risk for post clinic rehospitalizations related to improved HF self-care and less discouragement about their HF. Multidisciplinary, group clinic appointments are feasible, affordable, and highly rated by HF patients.
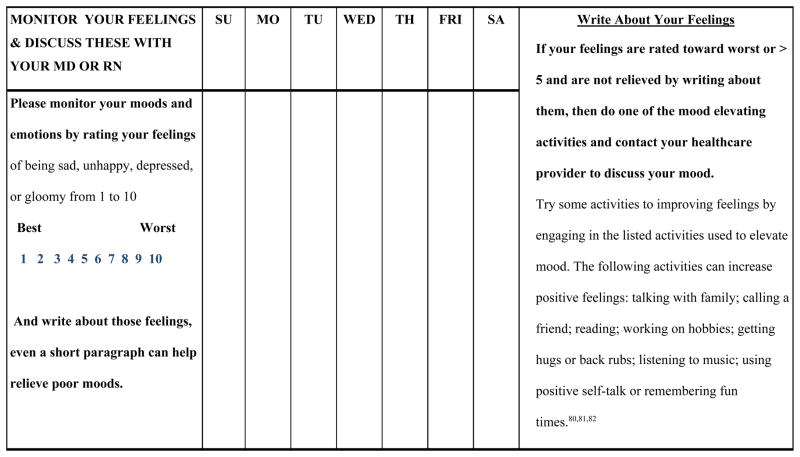
Figure 2.
Mood Monitoring Checklist for Patients to Rate Their Daily Mood and Emotions.
Acknowledgments
The authors extend their appreciation to all patients who participated in this study and to the Mid America Cardiology/University of Kansas Hospital staff for their continued advocacy of patients and their families managing lifelong complex HF home care. We are grateful for the recommendations and clinical expertise contributed to this trial by: Noreen Thompson, RN, MSN, CS; Jane Myer, LSCSW; Kara Rohleder, MS, RD, LD; Laura Motosko, MSEd, RD; Marilyn Werkowitch, RN, BSN; K. Reeder, RN, PhD; Jennifer Staley RN, BSN, CCRC; Sharon Fitzgerald, MPH; Andrea Elyachar, MA, CCRP; and Elizabeth Blachard-Hills, is acknowledged as the developer of the DVDs used in this study. James L. Vacek, MD, MS, is acknowledged for his monitoring and review of the clinical trial.
Footnotes
Conflicts of Interest and Source of Funding: None of the authors have any relationship with industry or financial associations that might pose a conflict of interest in connection with this manuscript.
Disclaimer: The project described is part of a clinical trial study supported by the National Institute of Heart, Lung and Blood (NHLBl) Grant # HL 085397. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NHLBl or the National Institutes of Health.
Contributor Information
C. E. Smith, Professor, School of Nursing & Department of Preventive Medicine, University of Kansas, Kansas City, Kansas.
U. Piamjariyakul, Research Associate Professor, School of Nursing, University of Kansas, Kansas City, Kansas.
K. M. Dalton, Cardiac Vascular Nurse Practitioner, University of Kansas Hospital, Kansas City, Kansas.
C. Russell, Heart Failure Nurse Practitioner, University of Kansas Hospital, Kansas City, Kansas.
J. Wick, Assistant Professor, Biostatistics Department, University of Kansas, Kansas City, Kansas.
E.F. Ellerbeck, Professor, Department of Preventive Medicine and Public Health, University of Kansas, Kansas City, Kansas.
References
- 1.Heidenreich PA, Albert NA, Allen LA, et al. Forecasting the impact of heart failure in the United States. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;23; 309(4):355–63. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarin D, Roger VL, et al. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dickson VV, Riegel B. Are we teaching what patients need to know? Building skills in heart failure self-care. Heart Lung. 2009;38(3):253–61. doi: 10.1016/j.hrtlng.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Coffey RM, Misra A, Barrett M, Andrews RM, Mutter R, Moy E. Congestive heart failure: who is likely to be readmitted? Medical Care Research and Review. 2012;69(5):602–16. doi: 10.1177/1077558712448467. [DOI] [PubMed] [Google Scholar]
- 6.Reeder KM, Ercole PM, Peek GM, Smith CE. Symptom perceptions and self-care behaviors in patients who self-manage heart failure. Journal of Cardiovascular Nursing. 2013 doi: 10.1097/JCN.0000000000000117. [ePub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: Problems and perspectives. J Am Coll Cardiol. 2013;61(4):391–403. doi: 10.1016/j.jacc.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 8.Sochalski J, Jaarsma T, Krumholz HM, et al. What works in chronic care management: the case of heart failure. Health Aff (Millwood) 2009;28(1):179–89. doi: 10.1377/hlthaff.28.1.179. [DOI] [PubMed] [Google Scholar]
- 9.Rich MW. Heart failure disease management programs: efficacy and limitations. Am J Med. 2001;110(5):410–2. doi: 10.1016/s0002-9343(01)00632-5. [DOI] [PubMed] [Google Scholar]
- 10.Smith CE. Nurse-led multidisciplinary heart failure group clinic appointments. American Heart Association Scientific Sessions: Late Breaking Clinical Trials. 2013 [Google Scholar]
- 11.Bodenheimer T, Wagner E, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model. JAMA. 2002;288(15):1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 12.Shortell SM, Schmittdie J, Wang MC, et al. An empirical assessment of high-performing medical groups: results from a national study. Med Care Res Rev. 2005;62(4):407–434. doi: 10.1177/1077558705277389. [DOI] [PubMed] [Google Scholar]
- 13.Levine MD, Ross TR, Balderson BH, Phelan EA. Implementing group medical visits for older adults at group health cooperative. J Am Geriatr Soc. 2010;58(1):168–72. doi: 10.1111/j.1532-5415.2009.02628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin A, Cavendish J, Boren D, Ofstad T, Seidensticker D. A pilot study: Reports of benefits from a 6-month, multidisciplinary, shared medical appointment approach for heart failure patients. Military Medicine. 2008;173(12):1210–1213. doi: 10.7205/milmed.173.12.1210. [DOI] [PubMed] [Google Scholar]
- 15.Grady KL, Dracup K, Kennedy G, et al. Team management of patients with heart failure: a statement for healthcare professionals from the Cardiovascular Nursing Council of the American Heart Association. Circulation. 2000;102(19):2443–2456. doi: 10.1161/01.cir.102.19.2443. [DOI] [PubMed] [Google Scholar]
- 16.Houck S, Kilo C, Scott J. Group Visits 101. [Accessed December 09, 2013];Family Practice Management. 2003 Available online at: http://www.aafp.org/fpm/20030500/66grou.html. [PubMed]
- 17.Glasgow RE, Davis CL, Funnell MM, Beck A. Implementing practical interventions to support chronic illness self-management. Jt Comm J Qual Saf. 2003;29(11):563–74. doi: 10.1016/s1549-3741(03)29067-5. [DOI] [PubMed] [Google Scholar]
- 18.Masley S, Phillips S, Copeland JR. Group office visits change dietary habits of patients with coronary artery disease—the dietary intervention and evaluation trial (D.I.E.T.) J of Family Practice. 2001;50(3):235–239. [PubMed] [Google Scholar]
- 19.Bartley KB, Haney R. Shared medical appointments: improving access, outcomes, and satisfaction for patients with chronic cardiac diseases. J Cardiovasc Nurs. 2010;25(1):13–19. doi: 10.1097/JCN.0b013e3181b8e82e. [DOI] [PubMed] [Google Scholar]
- 20.Watts SA, Gee J, O’Day ME, et al. Nurse practitioner-led multidisciplinary teams to improve chronic illness care: the unique strengths of nurse practitioners applied to shared medical appointments/group visits. J Acad Nurse Pract. 2009;21:167–172. doi: 10.1111/j.1745-7599.2008.00379.x. [DOI] [PubMed] [Google Scholar]
- 21.Wagner EH, Grothaus LC, Sandhu N, Galvin MS, McGregor M, Artz K, Coleman EA. Chronic care clinics for diabetes in primary care: A system-wide randomized trial. Diabetes Care. 2001;24(4):695–700. doi: 10.2337/diacare.24.4.695. [DOI] [PubMed] [Google Scholar]
- 22.Hersh AM, Masoudi FA, Allen LA. Postdischarge environment following heart failure hospitalization: Expanding the view of hospital readmission. J Am Heart Assoc. 2012;2(2):e000116. doi: 10.1161/JAHA.113.000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: A randomized controlled trial of a new model of primary care for frail older adults. J Am Geriatr Soc. 1999;47(7):775–783. doi: 10.1111/j.1532-5415.1999.tb03832.x. [DOI] [PubMed] [Google Scholar]
- 24.Scott JC, Conner DA, Venohr I, et al. Effectiveness of a group outpatient visit model for chronically ill older health maintenance organization members: A 2-year randomized trial of the cooperative health care clinic. J Am Geriatr Soc. 2004;52(9):1463–1470. doi: 10.1111/j.1532-5415.2004.52408.x. [DOI] [PubMed] [Google Scholar]
- 25.Beck A, Scott J, William P, et al. Randomized trial of group outpatient visits for chronically ill older HMO members: The cooperative health care clinic. J Am Geriatr Soc. 1997;45(5):543–549. doi: 10.1111/j.1532-5415.1997.tb03085.x. [DOI] [PubMed] [Google Scholar]
- 26.Wilkes RM, Dukes KR, Feagles LL, Leong D, Allen GL. Kaiser Permanente’s approach to congestive heart failure in South San Franciso. JCOM. 1999;6(5):37–40. [Google Scholar]
- 27.Smith CE, Piamjariyakul U, Wick J, et al. Multidisciplinary Group Clinic Appointments: The Self-Management and Care of Heart Failure (SMAC-HF) Trial. Circulation: Heart Failure. 2014;7:888–894. doi: 10.1161/CIRCHEARTFAILURE.113.001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wakefiled BH, Boren SA, Groves PS, Conn VS. Heart Failure Care Management Programs Review of Study Interventions and Meta-Analysis of Outcomes. J of Cardiovasc Nurs. 2013;28(1):8–19. doi: 10.1097/JCN.0b013e318239f9e1. [DOI] [PubMed] [Google Scholar]
- 29.Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckman V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams. Ann Behav Med. 2002;24(2):80–7. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 30.Powell LH, Calvin JE, Jr, Mendes de Leon CF, et al. The Heart Failure Adherence and Retention Trial (HART): design and rationale. Am Heart J. 2008;156(3):452–460. doi: 10.1016/j.ahj.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kasper EK, Gerstenblith G, Hefter G, Van Anden E, Brinker JA, Thiemann DR, et al. Randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol. 2002;39(3):471–80. doi: 10.1016/s0735-1097(01)01761-2. [DOI] [PubMed] [Google Scholar]
- 32.Paul S, Yehle KS, Wood K, Wingate S, Steg B. Implementing shared medical appointments for heart failure patients in a community cardiology practice: A pilot study. Heart & Lung. 2013;42(6):456–461. doi: 10.1016/j.hrtlng.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 33.Mohler D, Schultz KF, Altman D CONSORT Group (Consolidated Standards of Reporting Trials) The CONSORT Statement: Revised Recommendations for Improving the Quality of Reports of Parallel-Group Randomized Trials. JAMA. 2001;285(15):1987–91. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- 34.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35(5):1245–55. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 35.McCullough PA, Philbin EF, Spertus JA, Sandberg KR, Sullivan RA, Kaatz S. Opportunities for improvement in the diagnosis and treatment of heart failure. Clin Cardio. 2003;26(5):231–237. doi: 10.1002/clc.4960260507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;15; 62(16):e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 37.Bowden K, Fitzgerald SA, Piamjariyakul U, et al. Comparing Patient and Nurse Specialist Reports of Causative Factors of Depression Related to Heart Failure. Perspect Psychiatr Care. 2011;47(2):98–104. doi: 10.1111/j.1744-6163.2010.00279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCann J, Blanchard Hills E, Zauszniewski JA, Smith CE, Farran CJ, Wilkie DJ. NIH SBIR Project Outcomes: Home Care Self-management DVD series wins the international health media education award. WJNR. 2010;33(14):109–13. [Google Scholar]
- 39.National Institutes of Health. Turning discovery into health. Clear Communication: A NIH health literacy initiative. 2013 Available at: http://www.nih.gov/clearcommunication/
- 40.Smith CE, Koehler J, Moore J, Blanchard E, Ellerbeck E. Testing videotape education for heart failure. Clinical Nursing Research. 2005;14(2):191–205. doi: 10.1177/1054773804273276. [DOI] [PubMed] [Google Scholar]
- 41.Russell C, Smith C, Ellerbeck E, et al. Self-Management And Care of Heart Failure Through Group Clinics (SMAC-HF): A Nurse Practitioner Facilitated Multidisciplinary Group Clinic. Paper Presentation, American Association of Heart Failure Nurses (AAHFN) Conference; Boston. June 26–28, 2008. [Google Scholar]
- 42.Kumar A, Dalton K, Smith CE, et al. Methodology of Self Management and Care of Heart Failure through group trial (SMAC-HF). Poster Presentation. Quality of Care and Outcomes Research; 2007; Scientific Session American Heart Association; [Google Scholar]
- 43.Blanchard E. Robert Wood Johnson Foundation Transitions to Better Care: Innovations in Care Transitions and Discharge (Top 100 videos in national presentation on care transitions and reducing readmissions); February 13, 2013; Washington D.C: Robert Wood Johnson Foundation; Live Webcast. [Google Scholar]
- 44.Wakefield BJ, Boren SA, Groves PS, Conn VS. Heart failure care management programs: a review of study interventions and meta-analysis of outcomes. Journal of Cardiovascular Nursing. 28:8–19. doi: 10.1097/JCN.0b013e318239f9e1. [DOI] [PubMed] [Google Scholar]
- 45.Greenberg B. Acute decompensated heart failure-treatments and challenges. Circ J. 2012;76(3):532–43. doi: 10.1253/circj.cj-12-0130. [DOI] [PubMed] [Google Scholar]
- 46.Lam C, Smeltzer SC. Patterns of symptom recognition, interpretation, and response in heart failure patients: an integrative review. J of Cardiovasc Nurs. 2013;28(4):348–359. doi: 10.1097/JCN.0b013e3182531cf7. [DOI] [PubMed] [Google Scholar]
- 47.Gustafsson F, Arnold JM. Heart failure clinics and outpatient management: review of the evidence and call for quality assurance. Eur heart J. 2004;25:1596–1604. doi: 10.1016/j.ehj.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 48.Ettner SL, Kotlerman J, Afifi A, Vazirani S, Hays RD, Shapiro M, Cowan M. An alternative approach to reducing the costs of patient care? A controlled trial of the multi-disciplinary doctor-nurse practitioner (MDNP) model. Med Decis Making. 2006;26(1):9–17. doi: 10.1177/0272989X05284107. [DOI] [PubMed] [Google Scholar]
- 49.Scott LD, Setter-Kline K, Britton AS. The effects of nursing interventions enhance mental health and quality of life among individuals with heart failure. Appl Nurs Res. 2004;17:248–256. doi: 10.1016/j.apnr.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 50.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–37. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 51.Gallagher R, Luttik ML, Jaarsma T. Social support and self-care in heart failure. J Cardiovasc Nurs. 2011;26:439–445. doi: 10.1097/JCN.0b013e31820984e1. [DOI] [PubMed] [Google Scholar]
- 52.Watts SA, Gee J, O’Day ME, et al. Nurse practitioner-led multidisciplinary teams to improve chronic illness care: the unique strengths of nurse practitioners applied to shared medical appointments/group visits. J Acad Nurse Pract. 2009;21:167–172. doi: 10.1111/j.1745-7599.2008.00379.x. [DOI] [PubMed] [Google Scholar]
- 53.Yehle KS, Sands LP, Rhynders PA, Newton GD. The effect of shared medical visits on knowledge and self-care in patients with heart failure: A pilot study. Heart & Lung. 2009;38:25–33. doi: 10.1016/j.hrtlng.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 54.Roberts J, Brown GB, Streiner D, Gafni A, Pallister R, Hoxby H, Brummond-Young M, LeGris J, Meichenbaum D. Problem-solving counselling or phone-call support for outpatients with chronic illness: effective for whom? The Can J Nurs Res. 1995;27(3):111–137. [PubMed] [Google Scholar]
- 55.Piamjariyakul U, Russell C, Smith CE, Werkowitch M, Elyachar A. The feasibility of a telephone coaching program on heart failure home management for family caregivers. Heart & Lung. 2013;42(1):32–9. doi: 10.1016/j.hrtlng.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 57.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stauffer BD, Fullerton C, Fleming N, et al. Effectiveness and cost of a transitional care program for heart failure. Arch Intern Med. 2011;171(14):1238–1243. doi: 10.1001/archinternmed.2011.274. [DOI] [PubMed] [Google Scholar]
- 59.Naylor MD, Bowles KH, McCauley KM, et al. High-value transitional care: translation of research into practice [published online march 16, 2011] J Eval Clin Pract. doi: 10.1111/j.1365-2753.2011.01659.x. [DOI] [PubMed] [Google Scholar]
- 60.Alspach GJ. Slowing the revolving door of hospitalization for acute heart failure. Crit Care Nurse. 2014;34(1):8–12. doi: 10.4037/ccn2014527. [DOI] [PubMed] [Google Scholar]
- 61.Petterson SM, Liaw WR, Phillips RL, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10(6):503–509. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Falk H, Ekman I, Anderson R, Fu M, Granger B. Older patients’ experiences of heart failure: An integrative literature review. J Nurs Scholars. 2013;45 (3):247–255. doi: 10.1111/jnu.12025. [DOI] [PubMed] [Google Scholar]
- 63.Albert N, Fonarow G, Yancy C, et al. Influence of dedicated heart failure clinics on delivery of recommended therapies in outpatient cardiology practices: findings from the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF) Am Heart J. 2010;159(2):238–244. doi: 10.1016/j.ahj.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 64.Smith CE, Piamjariyakul U, Wick J, et al. Multidisciplinary Group Clinic Appointments: The Self-Management and Care of Heart Failure (SMAC-HF) Trial. Circ Heart Fail. 2014;7:888–894. doi: 10.1161/CIRCHEARTFAILURE.113.001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Piamjariyakul U, Yadrich DM, Russell C, et al. Patients’ annual income adequacy, insurance premiums and out-of-pocket expenses related to heart failure care. Heart & Lung. 2014;43(5):469–75. doi: 10.1016/j.hrtlng.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ. 2013;185(13):E635–44. doi: 10.1503/cmaj.130053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lavoie JG, Wong ST, Chongo M, Browne AJ, MacLeod ML, Ulrich C. Group medical visits can deliver on patient-centered care objectives: results from a qualitative study. BMC Health Serv Res. 2013;29(13):155. doi: 10.1186/1472-6963-13-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Litchman JH, Froelicher ES, Blumenthal JA. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014 doi: 10.1161/CIR.0000000000000019. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 69.Centers for Medicare & Medicaid Services (CMS) 2010 Reporting hospital quality data for annual payment update. U.S. Department of Health & Human Services; Available at: https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp. [Google Scholar]
- 70.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35(5):1245–55. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 71.Lee CS, Lyons KS, Gelow JM, Mudd JO, Hiatt SO, Nguyen T, Jaarsma T. Validity and reliability of the European Heart Failure Self-care Behavior Scale among adults from the United States with symptomatic heart failure. Eur J Cardiovasc Nurs. 2013;12(2):214–8. doi: 10.1177/1474515112469316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jaarsma T, Arestedt KF, Mårtensson J, Dracup K, Strömberg A. The European Heart Failure Self-care Behavior scale revised into a nine-item scale (EHFScB-9): a reliable and valid international instrument. Eur J Heart Fail. 2009;1(1):99–105. doi: 10.1093/eurjhf/hfn007. [DOI] [PubMed] [Google Scholar]
- 73.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A Multidisciplinary Intervention to Prevent the Readmission of Elderly Patients with Congestive Heart Failure. The New England Journal of Medicine. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 74.Pfeffer MA, Swedberg K, Granger CB, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet. 2003;362(9386):759–66. doi: 10.1016/s0140-6736(03)14282-1. [DOI] [PubMed] [Google Scholar]
- 75.Takeda A, Taylor SJ, Taylor RS, Khan F, Krum H, Underwood M. Clinical service organization for heart failure. Cochrane Database Syst Rev. 2012;9:CD002752. doi: 10.1002/14651858.CD002752.pub3. [DOI] [PubMed] [Google Scholar]
- 76.United States Department of Health and Human Services. Understanding HIPAA Privacy. Office for Civil Rights; [Accessed October 15, 2009]. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/index.html. [Google Scholar]
- 77.Houts PS, Nezu AM, Nezu CM, Bucher JA, Lipton A, editors. American College of Physician’s Home Care Guide for Cancer: How to Care for Family and Friends at Home. Philadelphia: American College of Physicians; 1994. [Google Scholar]
- 78.Toseland R, Rivas R. An introduction to group work practice. 5. Needham Heights, MA: Allyn & Bacon; 2005. [Google Scholar]
- 79.Roberts J, Brown GB, Streiner D, Gafni A, Pallister R, Hoxby H, Brummond-Young M, LeGris J, Meichenbaum D. Problem-solving counselling or phone-call support for outpatients with chronic illness: effective for whom? The Can J Nurs Res. 1995;27(3):111–137. [PubMed] [Google Scholar]
- 80.Heisler M, Halasyamani L, Cowen ME, Davis MD, Resnicow K, Strawderman RL, Choi H, Mase R, Piette JD. Randomized controlled effectiveness trial of reciprocal peer support in heart failure. Circ Heart Fail. 2013;6(2):246–53. doi: 10.1161/CIRCHEARTFAILURE.112.000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Smith CE, Leneerts M, Gajewski B. A Systematically Tested Intervention to Manage A Common Adverse Reactive Depression. Nurs Res. 2003;52(6):401–9. doi: 10.1097/00006199-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 82.MacMahon KH, Lip GY. Psychological factors in heart failure: a review of the literature. Archives of Internal Medicine. 2002;162:509–516. doi: 10.1001/archinte.162.5.509. [DOI] [PubMed] [Google Scholar]