Abstract
Objective
To evaluate the impact of the 2006 Massachusetts (MA) health reform on disparities in the management of acute cholecystitis (AC).
Summary Background Data
Immediate cholecystectomy has been shown to be the optimal treatment for AC, yet variation in care persists depending upon insurance status and patient race. How increased insurance coverage impacts these disparities in surgical care is not known.
Methods
A cohort study of patients admitted with AC in MA and three control states from 2001 through 2009 was performed using the Hospital Cost and Utilization Project State Inpatient Databases. We examined all non-elderly White, black, or Latino patients by insurance type and patient race, evaluating changes in the probability of undergoing immediate cholecystectomy and disparities in receiving immediate cholecystectomy before and after Massachusetts health reform.
Results
Data from 141,344 patients hospitalized for AC were analyzed. Prior to the 2006 reform, government-subsidized/self-pay (GS/SP) patients had a 6.6 to 9.9 percentage-point lower (p<0.001) probability of immediate cholecystectomy in both MA control states. The MA insurance expansion was independently associated with a 2.5 percentage-point increased probability of immediate cholecystectomy for all GS/SP patients in MA (p=0.049) and a 5.0 percentage-point increased probability (p=0.011) for non-white, GS/SP patients compared to control states. Racial disparities in the probability of immediate cholecystectomy seen prior to health care reform were no longer statistically significant after reform in MA while persisting in control states.
Conclusions
The MA health reform was associated with increased probability of undergoing immediate cholecystectomy for AC and reduced disparities in undergoing cholecystectomy by insurance status and patient race.
INTRODUCTION
Combating disparities in surgery has remained challenging given complex interrelated factors such as socioeconomic status, geography, education, patient race, and insurance coverage. In contrast to financing in other countries, health care for the non-elderly adult population in the United States is funded predominately through employer-sponsored or privately-purchased health insurance plans. Federal and state programs assist low-income residents, but even as the Affordable Care Act (ACA) begins to expand coverage, over 30-million Americans today remain without health insurance. This lack of insurance has been linked with disparities in the morbidity, mortality, and overall rates of surgery for a range of diagnoses.1,2 Recent health reform efforts have been implemented at state and federal levels in an attempt to increase access to and utilization of appropriate health care services. The most public of these efforts is the ACA modeled after the 2006 coverage expansion in Massachusetts. While overall rates of insurance grew across the Massachusetts population, non-white residents saw particularly striking gains in coverage with uninsurance rates falling from around 18% for black and Latino residents at the time of enactment to less than 5% currently.3,4 However, few studies have shown how expanded health insurance coverage impacts disparities surgical care by insurance status or patient race. Massachusetts therefore serves as a unique natural experiment to evaluate how expanded health insurance coverage affects disparities in surgical care delivery.
Acute cholecystitis has been one such diagnosis associated persistent disparities. Immediate cholecystectomy for acute cholecystitis is associated with improved medical and economic outcomes compared to delayed cholecystectomy.5–7 However, uninsured or underinsured individuals are less likely than their better-insured peers to receive surgery when diagnosed with acute cholecystitis.8 Similarly, low-income minorities are less likely than low-income whites to receive immediate cholecystectomy for other benign biliary pathology.9,10 Acute cholecystitis therefore presents an context in which to study the impact of insurance expansion—such as that achieved in Massachusetts—on disparities in surgical care.
Studies of the Massachusetts reform suggest that the increased insurance coverage is associated with increased access to primary care providers, increased use of preventative health, and improved self-reported health status.11–16 There have been increased referrals for surgical management of certain pathologies, but little is known regarding impacts on the surgical management of acute diseases such as cholecystitis.17,18 The primary objective of this study is to determine how the 2006 Massachusetts health reform impacted disparities in the management of acute cholecystitis, by both insurance status and patient race. We hypothesized that expanded health insurance would 1) increase the rates of immediate cholecystectomy for acute cholecystitis in government-subsidized/self-pay patients and 2) decrease disparities in immediate cholecystectomy for acute cholecystitis by insurance status and patient race.
METHODS
Data from the Hospital Cost and Utilization Project State Inpatient Databases (SID) for Massachusetts and three control states (Maryland, New York, and New Jersey) were used to capture all discharges of patients with acute cholecystitis between January 1, 2001 and December 31, 2009. The SID capture approximately 98% of all inpatient discharges from respective states and are validated annually. Control states were selected based on data set availability and cohesiveness over the entire study period, similar ratios of surgeons to residents, similar rates of cholecystectomy within the consistently insured population, and similar racial composition among residents who are uninsured or covered by government-subsidized plans.19,20 Each patient record represents a unique hospital discharge and includes age, sex, race, primary payer, diagnoses, procedures, admission type (emergent, urgent, elective), and hospital type (urban vs. rural, private vs. not-for-profit, and total hospital beds). The study was deemed by the institutional review board review to be exempt, as patients are not identifiable in this aggregated data set.
The study population included all white, Black, or Hispanic patients, between the ages of 18 and 64 years who were discharged with an International Classification of Diseases, Ninth Revision diagnosis code for acute cholecystitis (574.00, 574.01, 574.30, 574.31, 574.60, 574.61, 574.80, 574.81, 575.0, or 575.12). International Classification of Diseases, Ninth Revision procedure codes were used to determine whether patients underwent a cholecystectomy (512.1–512.4) during hospitalization. Patients with Medicare coverage were excluded from analysis as their insurance status was unlikely to have been affected by the 2006 insurance expansion.
Indicator variables were created for insurance coverage (government-subsidized/self-pay vs. private insurance), white vs. non-white race (Black or Hispanic), pre-reform vs. post-reform, and Massachusetts vs. control states. Government-subsidized/self-pay patients included all patients with Medicaid, Commonwealth Care (in Massachusetts), in addition to patients who were uninsured or self-pay. Privately-insured patients included all individuals in either an individually or employer-sponsored insurance plan. Given this population did not change significantly as a result of reform, it also serves as a second, internal control group to account for alternative state-specific changes in practice independent of insurance expansion. Pre-Reform was defined as before the third quarter of 2006 while post-reform was defined as discharge during or after the third quarter of 2006. Elixhauser comorbidity indices were calculated using diagnosis codes and were included in all adjusted analyses.21 To further control for complicated presentation with cholecystitis, an additional indicator variable defined complicated cholecystitis for patients carrying an associated diagnosis code for perforation of gallbladder, cholangititis, perforation or fistula of the bile duct, sepsis, septic shock, or severe sepsis. Secular trends were accounted for with the use of an additional linear time variable starting in the first quarter of 2001 and advancing at quarter-year intervals through the fourth quarter of 2009.
Our primary outcome was the probability of having an immediate cholecystectomy during the hospitalization for acute cholecystitis. Secondary outcomes included assessing if patients changed where they received their care and the cost of hospitalization. To identify the impact of the coverage expansion on these outcomes, we used a difference-in-differences analysis. This methodology is routinely used by economists and others who do policy analyses. It compares changes in outcomes in groups exposed to a policy change to a control group not exposed to the policy.22 All patient and hospital factors as well as secular trends were included in the adjusted model. Sensitivity analyses were performed to measure differences in pre-intervention trends in admission rates with acute cholecystitis and the probability of immediate cholecystectomy, by insurance status and patient race. Our results for these sensitivity models were unchanged from original models with the exception of difference-in-difference analysis of all government-subsidized/self-pay patients which showed mild sensitivity (results discussed below).
We used ordinary least squares (OLS) regression models to predict the probability of receiving a cholecystectomy depending upon both payer status and patient race. For disparities by insurance status, we compared the probability of immediate cholecystectomy for government-subsidized/self-pay patients with the probability for privately-insured patients, controlling for patient race in the adjusted analysis. To evaluate for racial disparities, we looked specifically at government-subsidized/self-pay non-white relative to government-subsidized/self-pay white patients, as this was the sub-group most directly impacted by the insurance expansion. All models were adjusted for patient and hospital factors as well as secular trends. As an additional sensitivity analysis, we also fit the data to logistic models. Results from these models did not significantly change the interpretation of our results.
Secondary analyses were done to evaluate changes in type of hospital and the cost of care after reform in Massachusetts. Site of care was examined by trending overall admissions and surgeries by hospital type. Additional evaluation in Massachusetts examined trends at safety-net vs. non-safety-net hospitals. Safety-net facilities were defined as those receiving greater than 25% of net-patient services revenue from Medicaid or self-pay patients at the time of the law’s enactment. This definition was based on criteria by the Department of Health and Human Services and availability of hospital financial records in Massachusetts. As such, we classified eight hospitals as safety-net facilities which represent approximately 12% of all hospitals in the state.23,24 Cost of care was evaluated using the HCUP cost-to-charge ratios with all costs inflation-adjusted to 2012 dollars.25 Data were analyzed using STATA version 12 (College Station, Texas). Results are reported with 95% confidence intervals or P-values as appropriate. The threshold for significance was a 2-tailed P ≤ 0.05.
RESULTS
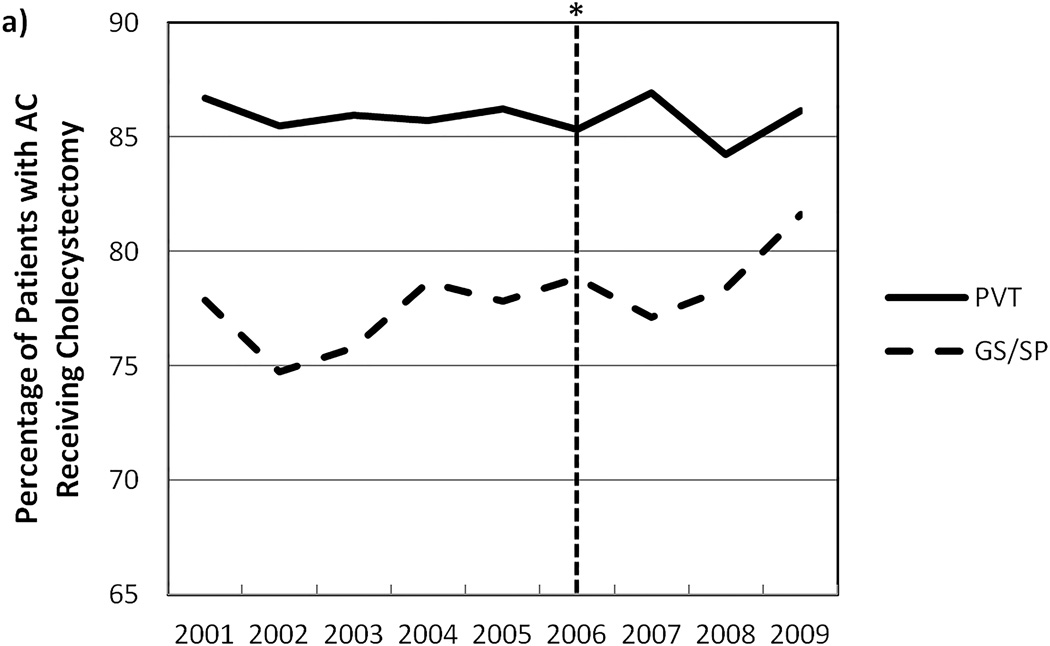
We identified 141,344 non-elderly adults who were admitted with acute cholecystitis and met additional inclusion criteria (Table 1). Compared to the control states, patients in Massachusetts tended to be older, have fewer comorbid conditions, and were less likely to be female, black or Hispanic. Patients in Massachusetts were less likely to be admitted under emergent status and less likely to be admitted to large, urban, not-for-profit hospitals. The percentage of immediate cholecystectomies performed laparoscopically was lower in Massachusetts compared to control states. Unadjusted trends in percentage of patients receiving cholecystectomy by intervention group and insurance status are shown in Figure 1.
Table 1.
Demographic characteristics of patients admitted with acute cholecystitis
| Massachusetts N (%) |
Control States N (%) |
|
|---|---|---|
| Total Patients | 20,066 | 121,278 |
| State | ||
| MA | 20,066 (100.0) | --- |
| MD | --- | 22,703 (18.7) |
| NJ | --- | 34,334 (28.3) |
| NY | --- | 64,241 (53.0) |
| Cholecystectomy | 17,261 (86.0) | 101,552 (81.9) |
| Laparoscopic | 14,549 (84.3) | 87,591 (83.7) |
| Government-subsidized/self-pay | 5,801 (28.9) | 42,575 (35.1) |
| Age mean (std) | 44.40 (12.6) | 43.17 (12.6) |
| Female | 13,328 (66.4) | 82,699 (68.2) |
| Race | ||
| White | 16,835 (83.9) | 76,367 (63.0) |
| Non-White | 3,793 (18.9) | 47,568 (39.2) |
| Comorbidity Index mean (std) | 0.98 (1.2) | 1.05 (1.1) |
| Hospital Type | ||
| NFP, Rural 100+ beds | 501 (2.5) | 4,470 (3.7) |
| NFP, Urban <100 beds | 1,275 (6.4) | 2,101 (1.7) |
| NFP, Urban 100–299 beds | 9,298 (46.3) | 45,139 (37.2) |
| NFP, Urban 300+ beds | 8,318 (41.5) | 69,143 (57.0) |
| Admission Type | ||
| Emergent | 14,250 (71.0) | 103,906 (85.7) |
| Urgent | 5,360 (26.7) | 10,152 (8.4) |
| Elective | 1,017 (5.1) | 9,698 (8.0) |
| Complicated Presentation | 746 (3.7) | 4,308 (3.6) |
MA Massachusetts
MD Maryland
NJ New Jersey
NY New York
NFP: Not-for-profit hospital
Figure 1.
Unadjusted trends in cholecystectomy for AC by insurance status in a) Massachusetts and b) control states
* Implementation of Massachusetts Insurance Expansion
AC Acute cholecystitis
PVT Private insurance coverage
GS/SP Government-subsidized/self-pay coverage
There was no differential change in annual admissions of government-subsidized/self-pay patients with acute cholecystitis between Massachusetts and control states (P=0.458). Sensitivity analyses also revealed no differences in the pre-reform trends in the probability of immediate cholecystectomy between government-subsidized/self-pay and privately-insured patients in Massachusetts (P=0.170) or control states (P=0447). Similarly, there was no differential pre-reform trend in probability of cholecystectomy for government-subsidized/self-pay non-white and government-subsidized/self-pay white patients within Massachusetts (P=0.583) or between Massachusetts and control states (P=0.878).
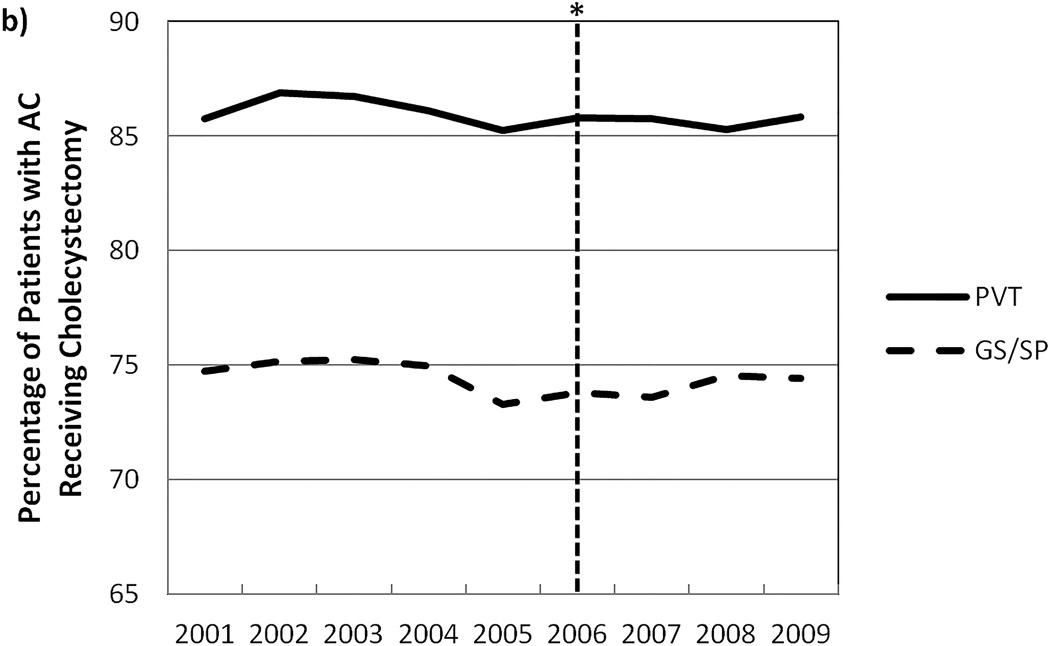
Disparities by Insurance Status
Prior to the 2006 reform, the unadjusted probability of government-subsidized/self-pay patients in Massachusetts receiving cholecystectomy was 76.8%, compared to 85.9% for privately-insured patients (Figure 1). Similarly, government-subsidized/self-pay patients in control states had a 74.0% probability of receiving immediate cholecystectomy relative to 86.1% of privately-insured patients. Adjusted analysis found that government-subsidized/self-pay patients in Massachusetts had a 6.6 percentage-point lower (p<0.001) probability of receiving cholecystectomy compared to privately-insured patients (Figure 2) prior to reform. In control states, government-subsidized/self-pay patients had a 9.9 percentage-point lower (p<0.001) probability of receiving immediate cholecystectomy relative to privately-insured patients in these states.
Figure 2.
Effect of being government-subsidized/self-pay patient on the probability of receiving immediate cholecystectomy
* Absolute difference in probability of receiving a cholecystectomy between government-subsidized/self-pay and privately insured patients, controlling for patient age, sex, race, comorbidities, hospital type, admission type, and complicated presentation.
Adjusting for confounding factors, the 2006 Massachusetts health reform was independently associated with a 2.5 percentage-point increase (P=0.049) in the probability of immediate cholecystectomy for government-subsidized/self-pay patients in Massachusetts relative to control states (Table 2). There was no differential change in the probability of immediate cholecystectomy for privately-insured patients in Massachusetts compared to control states (P=0.680). Results were mildly sensitive to the omission of 2006 quarters 1 and 2. In this sensitivity analysis, the coverage expansion was associated with a 2.29 percentage-point increased probability (P=0.075) of immediate cholecystectomy for government-subsidized/self-pay patients in Massachusetts as compared to similar patients in control states.
Table 2.
Difference-in-difference estimates for rates of cholecystectomy for government-subsidized/self-pay and privately-insured patients
| Massachusetts (% Patients with Surgery) |
Control States (% Patients with Surgery) |
Difference-in-Difference (% Patients with Surgery) |
||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Diff | Pre | Post | Diff | Unadjusted | Adjusted | |
| Government- subsidized/self-pay |
76.78 | 79.38 | +2.6 | 74.04 | 73.66 | −0.38 | +2.98 |
+2.46 (p=0.049) |
| Private Insurance | 85.94 | 85.79 | −0.15 | 86.06 | 85.71 | −0.35 | +0.20 |
−0.26 (p=0.680) |
After 2006, disparities in the probability of immediate cholecystectomy based on insurance status decreased in Massachusetts while persisting in control states. Within Massachusetts, government-subsidized/self-pay patients had a 4.3 percentage-point lower (p<0.001) probability of cholecystectomy relative to privately insured patients. In control states, government-subsidized/self-pay patients had a 10.3 percentage-point lower (p<0.001) probability of receiving cholecystectomy relative to privately-insured patients after 2006.
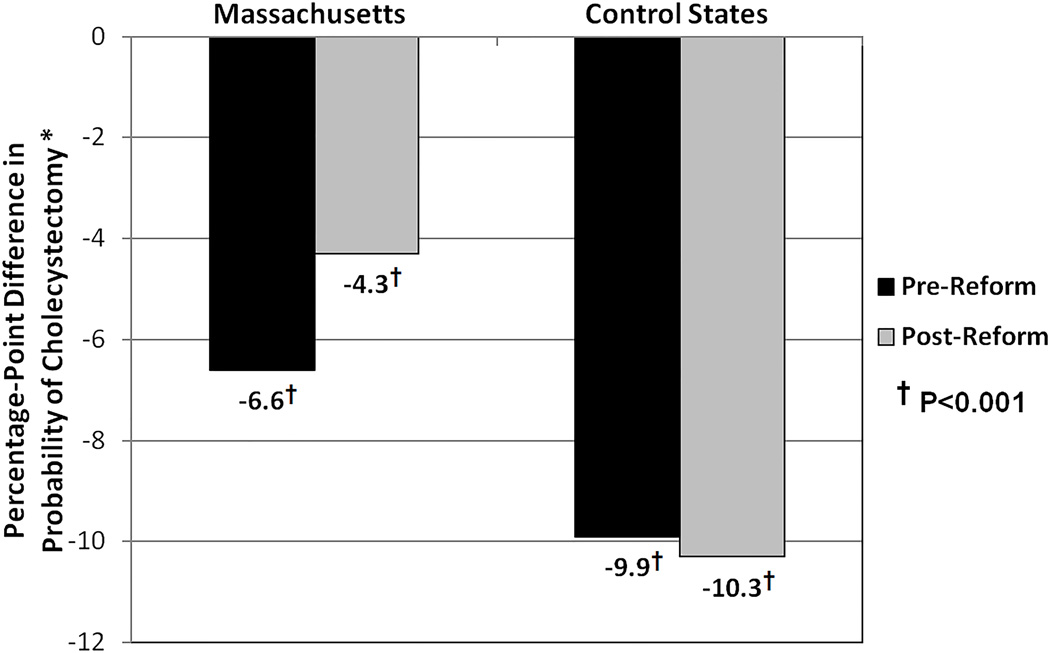
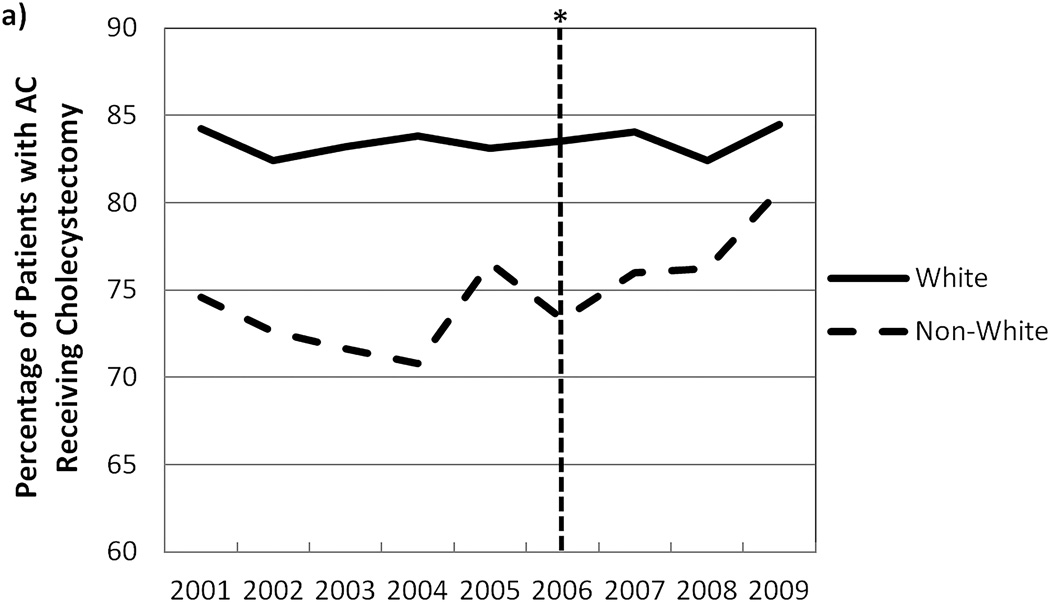
Disparities by Patient Race
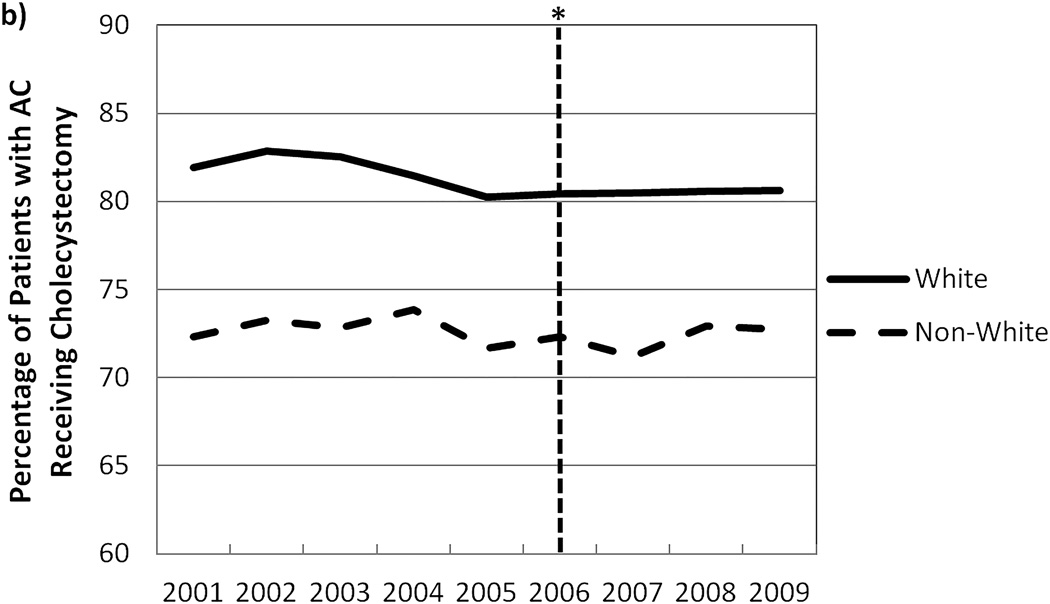
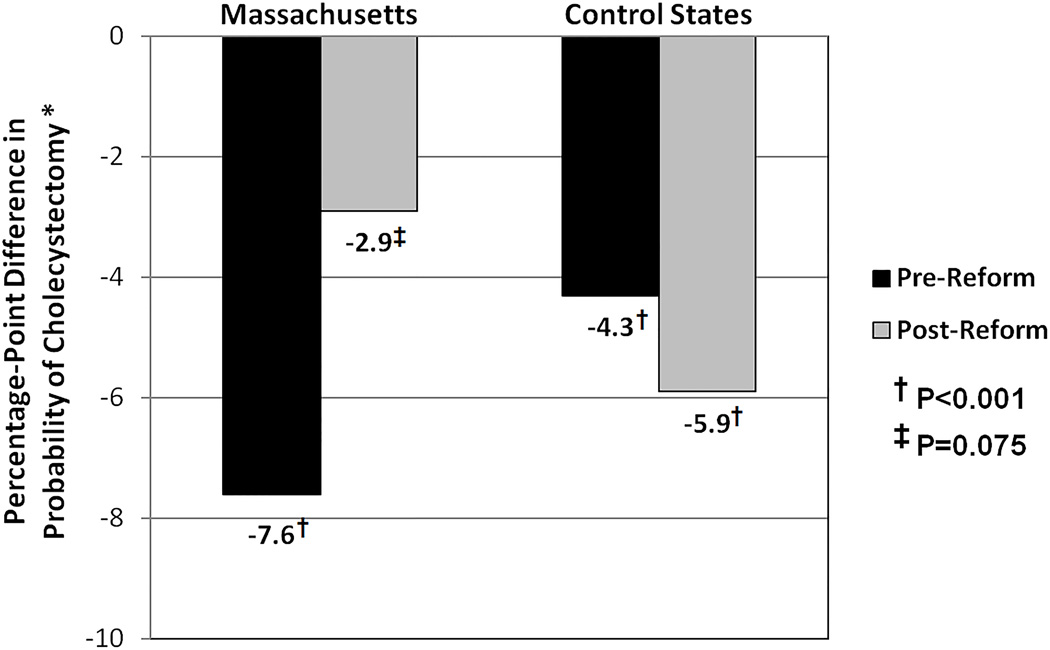
Unadjusted trends in immediate cholecystectomy by patient race and cohort are seen in Figure 3. Prior to 2006, government-subsidized/self-pay non-white patients in Massachusetts had a 72.8% unadjusted probability of receiving immediate cholecystectomy compared to 79.3% for government-subsidized/self-pay white patients in the state. Within control states, non-white patients had a 72.5% probability of undergoing immediate cholecystectomy relative to 76.5% of white patients (Table 3). Adjusting for confounding factors, non-white patients in Massachusetts had a 7.6 percentage-point lower (p<0.001) probability of cholecystectomy compared with white patients in the state (Figure 4). Non-white patients in control states had a 4.3 percentage-point lower (p<0.001) probability of cholecystectomy than white patients in control states.
Figure 3.
Unadjusted trends in immediate cholecystectomy for AC in GS/SP patients by patient race in a) Massachusetts and b) control states
* Implementation of Massachusetts Insurance Expansion
AC Acute cholecystitis
W White patients
NW Non-white patients
Table 3.
Difference-in-difference estimates of cholecystectomy for government-subsidized/self-pay patients
| Massachusetts (% Patients with Surgery) |
Control States (% Patients with Surgery) |
Difference-in-Difference (% Patients with Surgery) |
||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Diff | Pre | Post | Diff | Unadjusted | Adjusted | |
| Non-White Patients | 72.82 | 77.43 | +4.61 | 72.52 | 72.10 | −0.42 | +5.03 |
+5.00 (p=0.011) |
| White Patients | 79.32 | 80.77 | +1.45 | 76.50 | 76.41 | −0.09 | +1.54 |
+0.56 (p=0.730) |
Figure 4.
Effect of non-white race on probability of receiving immediate cholecystectomy
* Absolute difference in probability of receiving a cholecystectomy between government-subsidized/self-pay non-white and white patients, controlling for age, sex, comorbidities, hospital type, admission type, and complicated presentation.
The 2006 Massachusetts health reform was independently associated with a 5.0 percentage-point increase (P=0.011) in probability of immediate cholecystectomy for non-white patients in Massachusetts compared to similar patients in control states (Table 3). There was no statistically significant change in the probability of cholecystectomy for white patients in Massachusetts relative to white patients in control states.
After the insurance expansion, non-white patients in Massachusetts had a 77.4% probability of undergoing immediate surgery compared to 80.8% for white patients. Non-white patients in control states had 72.1% probability of cholecystectomy relative to a 76.4% probability for white patients. Again adjusting for patient, hospital, geographic, and secular covariates, non-white patients in Massachusetts had a 2.9 percentage-point lower (p=0.075) probability of immediate surgery relative to white patients within the state. For control states, non-white patients had a 5.9 percentage-point lower (p<0.001) probability of cholecystectomy compared to white patients.
Site of Care and Costs
Changes in the type of hospital were analyzed within Massachusetts, comparing safety-net to non-safety-net hospitals. Prior to reform, 19.9 % of government-subsidized/self-pay patients in Massachusetts were admitted to safety-net hospitals. After insurance expansion, safety-net hospitals admitted 22.2% of government-subsidized/self-pay patients. The 2006 reform was associated a 3.1 percentage-point increased (P=0.004) probability of low-income patients being admitted to a safety-net facility compared to privately-insured patients. There was no change in the probability of immediate cholecystectomy for privately-insured patients admitted to safety-net hospitals.
The mean inflation-adjusted cost of admission with acute cholecystitis for government-subsidized/self-pay patients was $US 12,062.64 in Massachusetts before expansion while admission of government-subsidized/self-pay patients in control states was $US 11,741.65. After 2006, the mean inflation-adjusted cost of admission for government-subsidized/self-pay patients was $US 12,763.18 in Massachusetts and $US 12,228.70 in control states. In the adjusted model, the 2006 reform was associated with no significant change in costs for government-subsidized/self-pay patients in Massachusetts relative to concurrent trends in control state (+ $US 332.90, P=0.592).
Subset Analyses (government subsidized vs. self-pay)
Subset analysis was also conducted to look at trends in immediate cholecystectomy for government-subsidized patients separate from self-pay patients. We found a significant change being for government-subsidized, non-white patients in Massachusetts. The increased probability of immediate cholecystectomy for all government-subsidized patients in Massachusetts failed to reach statistical significance (+2.6 percentage-point, P=0.101). However, the reform was associated with a 6.2 percentage-point increased probability (P=0.010) of immediate cholecystectomy for non-white patients with government-subsidized coverage in Massachusetts relative to concurrent trends in control states. Disparities in receipt of immediate cholecystectomy by patient race decreased and were no longer significant within government-subsidized patients in Massachusetts after reform while racial disparities persisted within similar patients in control states. There was no differential change in the rate of immediate cholecystectomy for self-pay in Massachusetts relative to control states, either as a whole or when stratified by patient race.
Subset Analyses (Complicated vs. uncomplicated cholecystitis)
Subset analyses by severity of presentation with AC found that the increased rates of immediate cholecystectomy were for patients presenting with uncomplicated disease. The law was associated with a 3.0 percentage-point increased probability of immediate cholecystectomy (P=0.017) for all government-subsidized/self-pay patients presenting with uncomplicated acute cholecystitis and a 5.8 percentage-point increased probability of immediate cholecystectomy (P=0.004) for non-white patients relative to concurrent trends in control states. There was no differential change in the rate patient presentation with complicated acute cholecystitis. There was also no differential change in immediate cholecystectomy for patients presenting with complicated cholecystitis.
DISCUSSION
Growing evidence suggests that surgery during initial hospitalization for acute cholecystitis improves outcomes with significantly shorter length of hospitalization and lower overall costs. Our findings highlight similar variation by insurance status and patient race prior to the 2006 reform. However, we found that the 2006 Massachusetts health law was associated with a 2.5 percentage-point increased probability of immediate cholecystectomy for all government-subsidized/self-pay patients in Massachusetts and a 4.6 percentage-point increased probability of cholecystectomy for non-white patients. Furthermore, racial disparities decreased and were no longer statistically significant for non-white patients in Massachusetts after insurance expansion while such disparities persisted in control states. These findings suggest that insurance expansion, including increased enrollment in Medicaid and government-subsidized insurance programs, may help mitigate disparities in surgical care by both insurance status and patient race.
Our findings have implications for similar expansion of insurance coverage within other states as a part of the ACA. Prior to the 2006 reform, Massachusetts had one of the smallest uninsured populations in the country. Since implementation, Massachusetts has seen a significant decrease in the number of uninsured from around 550,000 residents in 2006 to less than 250,000 individuals in 2009, with the majority of newly-insured individuals enrolling in either Medicaid or the newly created Commonwealth Care.26 Although it is challenging to generalize the Massachusetts experience across the country, other states with significantly higher baseline uninsurance rates have the potential to expand coverage to an even greater volume of residents. A recent study estimates that uninsurance rates by 2016 to be 19.6 percent without the Affordable Care Act as compared to 8.2 percent with the law.27 Within three states alone (Texas, Louisiana, and Florida), an estimated 2.3 million additional residents could gain coverage with expansion of Medicaid which is roughly ten times the volume as Massachusetts.
The interplay between race, insurance status, and receipt of optimal care has been described throughout the literature though it is often difficult to untangle. Our data suggest that a portion of such disparities in management of acute cholecystitis might be mitigated by the expansion of insurance across a population. Why patients are more likely to receive immediate cholecystectomy after health care reform is not entirely clear. One possibility is that changes in severity of patient presentation with acute cholecystitis impacts who is eligible for immediate cholecystectomy. Previous reports from Massachusetts have documented not only increased insurance coverage after reform but also improved access to primary care, greater use of preventative health services, increased outpatient referrals for certain surgical procedures, and decreased mortaility.3,4,11–13,16,17 Similarly, the Oregon Medicaid Study found increased utilization of inpatient, outpatient, and emergency department services after expanding insurance coverage to previously uninsured populations.28,29, 30
Our findings in Massachusetts could possibly be due not to changes in the overarching delivery system, but rather decreased variability in patient presentation with acute cholecystitis. Our subset analyses suggest that primary changes in the rate of immediate cholecystectomy were seen in government-subsidized patients, particularly non-white patients, who presented with uncomplicated acute cholecystitis. While we attempted to control both for patient comorbidities and severity of cholecystitis at the time of presentation, subtle changes not captured in our adjustments may have influenced the clinical decision to proceed with cholecystectomy rather than opting for nonoperative management. However, such changes would still suggest that expanding insurance coverage across a population might help mitigate disparities in care by both insurance status and patient race.
The cost of health care is also coming under increasing scrutiny. Major differences in market power, cost of living, and other economic factors confound cost comparisons between Massachusetts and other states. However, our data found no significant changes in the cost of admission for patients with acute cholecystitis after reform in Massachusetts relative to the changes in control states. Previous studies have found that immediate cholecystectomy for acute cholecystitis is associated with lower overall cost of care as compared to interval cholecystectomy. Though challenging to reach a definitive conclusion, these findings at least suggest that the increased receipt of cholecystectomy after expansion was not concurrently associated with significant increases in the cost of care for management of cholecystitis in Massachusetts as compared to our control states.
One limitation that must be considered is that practice patterns may have differentially changed for surgeons across Massachusetts or at Massachusetts safety-net hospitals for reasons independent of the reform such as recent publications on the superiority of immediate cholecystectomy or increased evidence on the cost-effectiveness of immediate cholecystectomy. However, such a change would need to be within a subsegment of surgeons within the state operating primarily on government-subsidized or self-pay patients. We used a privately-insured population as an internal, state control and did not see a concurrent rise in immediate cholecystectomy either across the state or within safety-net facilities.
Moreover, the control states used in this study may not provide a true counterfactual for Massachusetts. Each of these states was selected based on availability of data, relative geographic proximity, similar distribution of insurance coverage among non-white populations, similar rates of cholecystectomy within a consistently insured population, and similar volumes of surgeons.19 Furthermore, each state is at or below the national average in terms of health care needs met in health professional shortage areas.20 Sensitivity analyses also revealed no differential pre-reform trend in overall admissions with AC or outcomes for Massachusetts relative to control states. Nonetheless, Massachusetts is unique in many ways from other states and as such our findings may not be generalizable outside the state. As the Affordable Care Act rolls out in other states over the coming months and years, future studies may better elucidate short and long-term impacts of insurance coverage expansion on disparities in surgical care delivery.
Beyond timing and severity of presentation with acute disease, many additional factors are known to contribute to disparities in surgical care and should also be considered when contextualizing our findings. Low-income and minority communities have documented differences in health beliefs, health literacy, and trust in medical system at large. Furthermore, these populations are also disproportionately impacted by other social determinants of health, including socioeconomic status, education levels, and employment status.31,32 Changes in such confounding factors, independent of reform, could have differentially influenced healthcare seeking behavior in Massachusetts relative to the control states used in this study. To our knowledge, however, there have been few population-wide initiatives during this time period that would broadly influence health care or health seeking behavior. Furthermore, such a dramatic shift in behavior is unlikely to have occurred over the short post-reform period. Similarly, provider bias or challenges in patient-provider communication have been shown to be associated with disparities in surgical care, but are unlikely to have differentially changed over such a short period.33,34 The economic recession of 2008 has the potential to have affected Massachusetts differentially. However, data from the United States Bureau of Labor Statistics suggest that trends in unemployment were similar across all states included in this study.35 As an observational study, however, additional ecological factors unknown to authors cannot be excluded as possible influences our results.
Increasing attention has been given to the site of care as a major contributor to disparities in surgical care.36–38 Data from Massachusetts suggest that the majority of newly insured patients are preferentially maintaining care at a cluster of safety-net hospitals.39 Our data is consistent with these findings in as much as government-subsidized/self pay patients continued to be disproportionately admitted to safety-net facilities with the diagnosis of cholecystitis. Yet, we also found a reduction in disparities by race and insurance status despite government-subsidized and non-white patients receiving care at the same facilities. Our findings therefore contrast previous reports identifying site of care as a primary driver of disparities, at least in regards to the management of acute cholecystitis.
Given that the study was retrospective and used administrative data, we must also consider additional limitations of data. ICD-9 diagnosis and procedure codes were used to select patients and define outcomes. Therefore, errors in coding could have influenced our findings. However, the HCUP-SID capture approximately 98% of all discharges from respective states annually and are validated on an annual basis, significantly minimizing directional sampling bias or errors in coding.
Overall, we found the 2006 Massachusetts health reform to be associated with reduced disparities in the management of acute cholecystitis. Amidst a rapidly changing health care landscape, ongoing evaluation of major policy changes is crucial to ensure the extension of optimal care across populations, regardless or insurance status or patient race. Additional studies are needed to more comprehensively dissect the multifactorial drivers of disparities in surgical care and evaluate the impact of ongoing health reforms on disparities at state and national levels.
ACKNOWLEDGEMENTS
We would like to acknowledge the National Bureau of Economic Research, through whom data were made available. Additionally, the State Inpatient Databases are maintained through Hospital Cost and Utilization Project Data Partners, including the Massachusetts Center for Health Information and Analysis, the Maryland Health Services Cost Review Commission, the New Jersey Department of Health, and the New York State Department of Health.
Financial Support
Study supported by Department of Surgery, Massachusetts General Hospital, Boston, Massachusetts
Footnotes
Abstract Presented at: American College of Surgeons Clinical Congress, Surgical Forum, Washington D.C, U.S.A, 7 October 2013
Disclosures
No disclosures to report
REFERENCES
- 1.Lidor AO, Gearhart SL, Wu AW, et al. Effect of race and insurance status on presentation, treatment and mortality in patients undergoing surgery for diverticulitis. Arch Surg. 2008;143:1160–1165. doi: 10.1001/archsurg.143.12.1160. [DOI] [PubMed] [Google Scholar]
- 2.LaPar DJ, Castigliano MB, Mery CM, et al. Primary payer status affects mortality for major surgical operations. Ann Surg. 2010;252:544–551. doi: 10.1097/SLA.0b013e3181e8fd75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boston, MA: Division of Health Care Finance and Policy; 2010. [Accessed 13 May 2012]. Health Insurance Coverage in Massachusetts: Results from the 2008–2010 Massachusetts Health Insurance Surveys. Available at: http://www.mass.gov/chia/docs/r/pubs/10/mhis-report-12-2010.pdf. [Google Scholar]
- 4.Long SK, Stockley K. Health Reform in Massachusetts: An update as of fall 2009. [Accessed 13 May 2012];Urban Institute. 2010 Available at: http://bluecrossmafoundation.org/~/media/Files/Publications/Policy%20Publications/060810MHRS2009FINAL.pdf. [Google Scholar]
- 5.Lo CM, Liu CL, Fan ST, et al. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1998;227:461–467. doi: 10.1097/00000658-199804000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siddiqui T, MacDonald A, Chong PS, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. 2008;195:40–47. doi: 10.1016/j.amjsurg.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Gurusamy K, Samraj K, Gluud C, et al. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010;97:141–150. doi: 10.1002/bjs.6870. [DOI] [PubMed] [Google Scholar]
- 8.Greenstein AJ, Moskowitz A, Gelijns AC, et al. Payer status and treatment paradigm for acute cholecystitis. Arch Surg. 2012;147:453–458. doi: 10.1001/archsurg.2011.1702. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen GC, Tuskey A, Jagannath SB. Racial disparities in cholecystectomy rates during hospitalizations for acute gallstone pancreatitis: A national survey. Am J Gastroenterol. 2008;103:2301–2307. doi: 10.1111/j.1572-0241.2008.01949.x. [DOI] [PubMed] [Google Scholar]
- 10.Arozullah AM, Ferreira MR, Bennett RL, et al. Racial variation in the use of laparoscopic cholecystectomy in the Department of Veterans Affairs medical system. JACS. 1999;188:604–622. doi: 10.1016/s1072-7515(99)00047-2. [DOI] [PubMed] [Google Scholar]
- 11.Long SK, Masi PB. Access and affordability: An update on health reform in Massachusetts, Fall 2008. Health Aff. 2009;28:w578–w587. doi: 10.1377/hlthaff.28.4.w578. [DOI] [PubMed] [Google Scholar]
- 12.Finkelstein A, Taubman S, Wright B, et al. The Oregon health insurance experiment: evidence from the first year. NBER Working Paper No. 17190. 2011 Jul; doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolstad JT, Kowalski AE. The impact of health care reform on hospital and preventative care: Evidence from Massachusetts. NBER Working Paper No. 16012. 2010 May [Google Scholar]
- 14.Pande AH, Ross-Degnan D, Zaslavsky AM, et al. Effects of healthcare reforms on coverage, access, and disparities. Am J Prev Med. 2011;41:1–8. doi: 10.1016/j.amepre.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Smulowitz PB, Lipton R, Wharam JF, et al. Emergency department utilization after the implementation of Massachusetts health reform. Ann Emerg Med. 2011;58:225–234. doi: 10.1016/j.annemergmed.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 16.Sommers BD, Long SK, Baicker K. Changes in Mortality After Massachusetts Health Care Reform: A Quasi-experimental Study. Ann Intern Med. 2014;160:585–593. doi: 10.7326/M13-2275. [DOI] [PubMed] [Google Scholar]
- 17.Hanchate AD, Lasser KE, Kapoor A, et al. Massachusetts reform and disparities in inpatient care utilization. Med Care. 2012;50:569–577. doi: 10.1097/MLR.0b013e31824e319f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loerher AP, Song Z, Auchincloss HG, et al. Massachusetts health care reform and reduced racial disparities in minimally invasive surgery. JAMA Surg. 2013;148:1116–1122. doi: 10.1001/jamasurg.2013.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dartmouth Atlas of Health Care. [Accessed 13 May 2012]; Available at: http://www.dartmouthatlas.org/. [Google Scholar]
- 20.Kaiser Family Foundation State Health Facts. Sources from Urban Institute and Kaiser Commission on Medicaid and the Uninsured estimates based on the Census Bureau's March 2010 and 2011 Current Population Survey (CPS: Annual Social and Economic Supplements) [Accessed 13 May 2012]; Available at: http://www.statehealthfacts.org/index.jsp. [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: The MIT Press; 2001. [Google Scholar]
- 23.Wynn B, Coughlin T, Bondarenko S, et al. Analysis of the joint distribution of disproportionate share hospital payments. [Accessed 25 April 2013];Report for the Assistant Secretary of Planning and Evaluation, Department of Health and Human Services by RAND under contract with the Urban Institute. 2002 Available at: http://www.urban.org/UploadedPDF/410975_ASPEDSH_final.pdf. [Google Scholar]
- 24.Study of the reserves, endowments, and surpluses of hospitals in Massachusetts. Massachusetts Division of Health Care Finance and Policy; 2009. [Google Scholar]
- 25.Bureau of Labor Statistics, Consumer Price Index Calculator. [Accessed 24 May 2014]; Available at: http://www.bls.gov/data/inflation_calculator.htm.
- 26.United States Census Bureau. Current Population Survey Annual Social and Economic Supplement (CPS) [Accessed 13 May 2012]; Available at: http://www.census.gov/hhes/www/hlthins/data/historical/HIB_tables.html.
- 27.Eibner C, Cordova A, Nowak SA, et al. The Affordable Care Act and health insurance markets: Simulating the effects of regulation. Santa Monica, CA: RAND Corporation; 2013. [Accessed on 5 April 2014]. Available at: http://www.rand.org/content/dam/rand/pubs/research_reports/RR100/RR189/RAND_RR189.pdf. [PMC free article] [PubMed] [Google Scholar]
- 28.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment – Effects of Medicaid on clinical outcomes. N Engl J Med. 368:1713–1722. doi: 10.1056/NEJMsa1212321. 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taubman SL, Allen HL, Wright BJ, et al. Medicaid increases emergency-department use: Evidence from Oregon’s health insurance experiment. [Accessed on 4 January 2014];Science. doi: 10.1126/science.1246183. Published online 2 January 2014. Available at: http://www.sciencemag.org/content/early/2014/01/02/science.1246183.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finkelstein A, Taubman S, Wright B, et al. The Oregon health insurance experiment: Evidence from the first year. Q J Econ. 2012;127:1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams DR, Braboy Jackson P. Social sources of racial disparities in health. Health Affairs. 2005;24:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 32.Graham H. Social determinants and their unequal distribution: Clarifying policy understandings. Milbank Q. 2004;82:101–124. doi: 10.1111/j.0887-378X.2004.00303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 34.Fajah F, Wood DE, Yanez D, III, et al. Racial disparities among patients with lung cancer who were recommended operative therapy. Arch Surg. 2009;144:14–18. doi: 10.1001/archsurg.2008.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.United States Bureau of Labor Statistics. Local Area Unemployment Statistics. [Accessed on 2/1/2013]; at: http://www.bls.gov/lau/#tables.
- 36.Liu JH, Zingmond DS, McGory MI, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA. 2006;296:1973–1980. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- 37.Dimick J, Ruhter J, Vaughan Sarrazin M, et al. Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Affairs. 2013;32:1046–1053. doi: 10.1377/hlthaff.2011.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality. Arch Surg. 2012;147:63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ku L, Jones E, Shin P, et al. Safety-net providers after health care reform: Lessons from Massachusetts. Arch Intern Med. 2011;171:1379–1384. doi: 10.1001/archinternmed.2011.317. [DOI] [PubMed] [Google Scholar]