Abstract
Cognitive impairment is a common complaint among cancer survivors and may be a consequence of the tumors themselves or direct effects of cancer-related treatment (eg, chemotherapy, endocrine therapy, radiation). For some survivors, symptoms persist over the long term and, when more severe, can impact quality of life and function. This section of the NCCN Guidelines for Survivorship provides assessment, evaluation, and management recommendations for cognitive dysfunction in survivors. Nonpharmacologic interventions (eg, instruction in coping strategies; management of distress, pain, sleep disturbances, and fatigue; occupational therapy) are recommended, with pharmacologic interventions as a last line of therapy in survivors for whom other interventions have been insufficient.
Cognitive impairment is a common complaint among cancer survivors and may be a consequence of the tumors themselves or direct effects of cancer-related treatment (eg, radiation therapy). This symptom may be especially prominent in survivors of primary central nervous system (CNS) cancers or those with brain metastases. In addition, survivors who never had brain involvement may also report difficulties in cognition.1 For some survivors, symptoms persist over the long term.2 When more severe, the presence of cognitive dysfunction can impact quality of life and function. Cognitive dysfunction is most commonly connected with chemotherapy (sometimes referred to as “chemobrain”), but evidence suggests that therapies other than chemotherapy, such as endocrine therapy and radiation, may be associated with cognitive impairments.3–9 A recent national cross-sectional study found that a history of cancer is independently associated with a 40% increase of the likelihood of self-reported memory problems.10
Cancer-related cognitive changes have primarily been studied in patients with CNS and breast cancers and lymphoma, and those who have undergone hematopoietic stem cell transplant (HSCT), with a wide incidence ranging from 19% to 78%.2,11–24 Deficits commonly occur in the domains of executive function, learning and memory, attention, and processing speed.2,23
Growing evidence supports the patient experience of cognitive dysfunction associated with cancer and its treatment. In one meta-analysis of 17 studies, women treated with chemotherapy for breast cancer 6 or more months previously (n=807) had lower functional abilities than those not treated with chemotherapy (n=291).14 These deficits were limited to verbal (eg, word-finding) and visuospatial (eg, copying complex images) abilities. However, when compared with their prechemotherapy baseline, no differences were noted among patients complaining of cognitive dysfunction. In another study, cognitive function was compared among 196 long-term survivors of breast cancer treated with cyclophosphamide, methotrexate, and fluorouracil (CMF) who were, on average, 21 years out from diagnosis, and 1509 control patients with no history of cancer.25 The chemotherapy group did significantly worse on several neuropsychological tests (eg, immediate and delayed verbal memory, executive functioning, psychomotor speed). Finally, one study compared 101 patients who underwent an HSCT with 82 patients treated with a nonmyeloablative therapy; both groups showed mild cognitive impairments at baseline.26 Although no significant differences in cognitive dysfunction were identified at 2-year follow-up, patients who underwent HSCT had poorer performances in several areas, including attention and executive and psychomotor functions.


The correlation between patient reports of cognitive decline and results of neuropsychological testing has not been consistently demonstrated, possibly because of various definitions of cognitive dysfunction and differences in the statistical analyses across studies.23 However, a recent study of 189 breast cancer survivors found that memory and executive function complaints, present in approximately 20% of the cohort, showed a statistically significant association with results of domain-specific neuropsychological tests.27
The underlying mechanisms that might increase the risk for chemotherapy-induced cognitive changes are not known. Studies have reported elevated levels of cytokines or DNA damage as some of the possible mechanisms.28 Structural studies have supported the hypothesis that neurotoxicity resulting in damage to white matter of the brain may play an important role in cognitive deficits after chemotherapy treatment.2,5,13,29,30 In addition, fatigue and depression, common in cancer survivors, may negatively influence cognitive function, although several studies have found that cognitive dysfunction does not correlate with mood.25,31 Psychosomatic effects can also contribute, as evidenced by a recent study of patients to be treated with chemotherapy, which found that those who were informed of the possible cognitive side effects were more likely to report cognitive dysfunction and perform worse on neuropsychological testing than uninformed patients.32 A better understanding of the mechanisms that cause cancer-related cognitive impairment is essential for the development of treatments to improve cognitive function and quality of life in patients with cancer and survivors.1,33,34
In October 2006, the International Cognition and Cancer Taskforce (ICCTF) was formed, comprising a multidisciplinary group of health professionals and health advocates. The mission of ICCTF is to advance understanding of the impact of treatment-related cognitive and behavioral functioning in patients with non-CNS cancers.35 The group recently published recommendations regarding neuropsychological testing, defining cognitive impairment/changes, and future study design.34 ICCTF also has a Web site (www.icctf.com) to provide up-to-date information to both physicians and patients seeking assistance in the management of cognitive symptoms associated with cancer treatment.
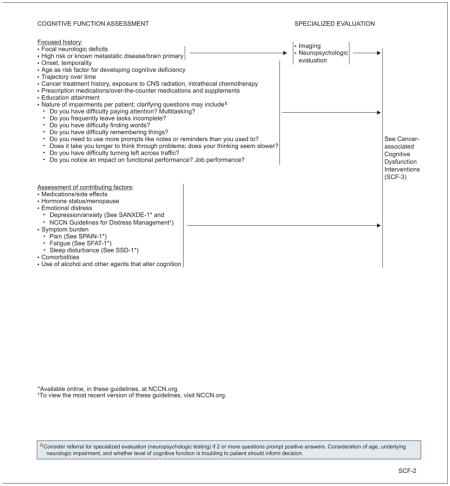
Assessment and Evaluation for Cognitive Dysfunction
Patients who present with symptoms of cognitive impairment should be screened for potentially reversible factors that may contribute to cognitive impairment, including depression, pain, fatigue, and sleep disturbance. Some medications can also contribute to cognitive impairment. Therefore, current medications, including over-the-counter medications and supplements, should be reviewed. Any potentially contributing factor should be addressed.
For those who present with concomitant focal neurologic deficits and those whose symptoms evolve to include these findings, imaging is indicated to rule out brain or CNS disease. In addition, imaging in the absence of focal findings may be appropriate for patients deemed to be at high risk for recurrence or metastatic disease involving the CNS.
Unfortunately, no effective brief screening tool currently exists for cancer-associated cognitive dysfunction in the asymptomatic cancer survivor. The Mini-Mental State Examination (MMSE36) and similar screening tools lack adequate sensitivity to detect a subtle decline in cognitive performance. Instead, the panel listed several questions that can help clarify the nature of the impairment, including inquiries about the ability to pay attention, find words, remember things, think clearly, and perform functions. The time of onset and the trajectory over time should also be assessed.
Neuropsychological evaluation may be helpful when individuals perceive cognitive impairment in a nonspecific way and clarity is needed about the nature of impairments to guide rehabilitative efforts. Neuropsychological evaluation itself can be therapeutic and validating. Evaluation may also be necessary if an individual is pursuing disability benefits and cognitive impairment is a contributing factor to work limitation.
Management of Cognitive Dysfunction
Survivors benefit from validation of their symptom experience and should be reassured that, in most patients, cognitive dysfunction does not worsen over time. In fact, data from breast cancer survivors suggest that symptoms may improve over time.4 The panel recommends the use of nonpharmacologic interventions whenever possible, with pharmacologic interventions as a last line of therapy in survivors for whom other interventions have been insufficient, as discussed in the following sections. Additional recommendations for cognitive dysfunction in older adults can be found in the cognitive function section of the NCCN Guidelines for Senior Adult Oncology (to view the most recent version of these guidelines, visit NCCN.org).
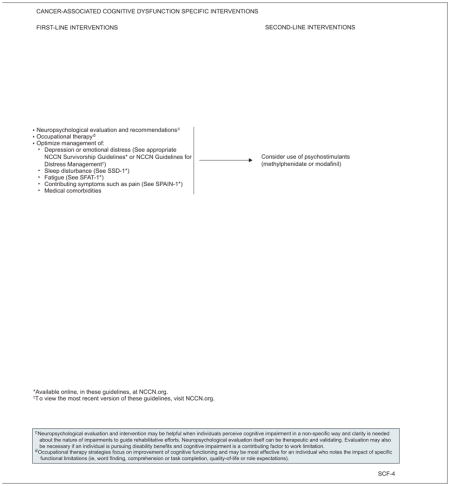
Nonpharmacologic Interventions for Cognitive Dysfunction
Prospective data are lacking to inform the use or potential benefits of nonpharmacologic interventions for cancer survivors who complain of cognitive dysfunction. In one small study, cognitive behavioral therapy was evaluated in 40 breast cancer survivors using a waitlist control trial design.37 Although overall quality of life improved with the intervention, statistically significant improvement was noted only with verbal memory, not with self-reports of daily cognitive complaints.
Practical suggestions include instruction in self-management and coping strategies (eg, using planners and reminder notes, keeping items in the same place, minimizing distractions, avoiding multitasking), which the panel believes can be very helpful to patients. Discontinuation or limitation of use of medications known to cause or contribute to cognitive impairment should be attempted. Management of distress, pain, sleep disturbances, and fatigue should be provided. In fact, a recent study showed that cognitive behavioral therapy for fatigue was effective at reducing self-reported cognitive disability and concentration problems in 98 severely fatigued cancer survivors.38 Finally, relaxation, stress management, and routine exercise should all be encouraged. Substantial evidence shows that physical activity enhances cognitive function in elderly people in general, although only few studies specific to cancer survivors have been reported.39–41
Occupational therapy strategies focus on improvement of cognitive functioning and may be most effective for individuals who note the impact of specific functional limitations, such as word finding, comprehension, task completion, work performance, quality of life, or role expectations.42
Pharmacologic Interventions for Cognitive Dysfunction
If nonpharmacologic interventions have been insufficient, consideration of psychostimulants such as methylphenidate or modafinil is reasonable, although data informing the efficacy of these agents are lacking. Trials assessing the effects of methylphenidate have reported mixed results.43 For example, a randomized, placebo-controlled, double-blind trial found that d-methylphenidate had no effect on neuropsychological test scores.44 In contrast, a randomized, double-blind, crossover trial of child survivors of acute lymphoblastic leukemia or brain tumors showed that methylphenidate was more effective than placebo at improving attention, cognitive flexibility, and processing speed.45
Results of studies on modafinil are more consistent. A randomized controlled trial assessing the efficacy of modafinil for fatigue and cognitive function in breast cancer survivors found significantly greater improvement in memory and attention among patients receiving modafinil than in the placebo group.46 Similarly, a double-blind, randomized, crossover trial also in breast cancer survivors found that participants receiving modafinil performed significantly better on cognitive tests of attention and psychomotor speed.47 Benefits with treatment were also noted among patients with a primary brain tumor.48
NCCN Survivorship Panel Members
*,a,cCrystal S. Denlinger, MD/Chair†
Fox Chase Cancer Center
*,c,dJennifer A. Ligibel, MD/Vice Chair†
Dana-Farber/Brigham and Women’s Cancer Center
fMadhuri Are, MD£
Fred & Pamela Buffett Cancer Center at The Nebraska Medical Center
b,eK. Scott Baker, MD, MS€ξ
Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance
cWendy Demark-Wahnefried, PhD, RD≅
University of Alabama at Birmingham Comprehensive Cancer Center
b,dDebra L. Friedman, MD, MS€‡
Vanderbilt-Ingram Cancer Center
*,gMindy Goldman, MDΩ
UCSF Helen Diller Family Comprehensive Cancer Center
c,dLee Jones, PhDΠ
Memorial Sloan Kettering Cancer Center
bAllison King, MD€Ψ‡
Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine
Grace H. Ku, MDξ‡
UC San Diego Moores Cancer Center
b,hElizabeth Kvale, MD£
University of Alabama at Birmingham Comprehensive Cancer Center
aTerry S. Langbaum, MAS¥
The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins
gKristin Leonardi-Warren, RN, ND#
University of Colorado Cancer Center
bMary S. McCabe, RN, BS, MS#
Memorial Sloan Kettering Cancer Center
b,c,d,gMichelle Melisko, MD†
UCSF Helen Diller Family Comprehensive Cancer Center
eJose G. Montoya, MDΦ
Stanford Cancer Institute
a,dKathi Mooney, RN, PhD#
Huntsman Cancer Institute at the University of Utah
c,eMary Ann Morgan, PhD, FNP-BC#
Moffitt Cancer Center
Javid J. Moslehi, MDλÞ
Dana-Farber/Brigham and Women’s Cancer Center
d,hTracey O’Connor, MD†
Roswell Park Cancer Institute
cLinda Overholser, MD, MPHÞ
University of Colorado Cancer Center
cElectra D. Paskett, PhDε
The Ohio State University Comprehensive Cancer Center - James Cancer Hospital and Solove Research Institute
f,hMuhammad Raza, MD‡
St. Jude Children’s Research Hospital/The University of Tennessee Health Science Center
fKaren L. Syrjala, PhDθ
Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance
*,fSusan G. Urba, MD†£
University of Michigan Comprehensive Cancer Center
gMark T. Wakabayashi, MD, MPHΩ
City of Hope Comprehensive Cancer Center
*,hPhyllis Zee, MDΨΠ
Robert H. Lurie Comprehensive Cancer Center of Northwestern University
NCCN Staff: Nicole R. McMillian, MS, and Deborah A. Freedman-Cass, PhD
KEY:
*Writing Committee Member
Subcommittees: aAnxiety and Depression; bCognitive Function; cExercise; dFatigue; eImmunizations and Infections; fPain; gSexual Function; hSleep Disorders
Specialties: ξBone Marrow Transplantation; λCardiology; εEpidemiology; ΠExercise/Physiology; ΩGynecology/Gynecologic Oncology; ‡Hematology/Hematology Oncology; ΦInfectious Diseases; ÞInternal Medicine; †Medical Oncology; ΨNeurology/Neuro-Oncology; #Nursing; ; ≅Nutrition Science/Dietician; ¥Patient Advocacy; €Pediatric Oncology; θPsychiatry, Psychology, Including Health Behavior; £Supportive Care Including Palliative, Pain Management, Pastoral Care, and Oncology Social Work; ¶Surgery/Surgical Oncology; ωUrology
Footnotes
NCCN Categories of Evidence and Consensus
Category 1: Based upon high-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2A: Based upon lower-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2B: Based upon lower-level evidence, there is NCCN consensus that the intervention is appropriate.
Category 3: Based upon any level of evidence, there is major NCCN disagreement that the intervention is appropriate.
All recommendations are category 2A unless otherwise noted.
Clinical trials: NCCN believes that the best management for any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged.
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) are a statement of consensus of the authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult the NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The National Comprehensive Cancer Network® (NCCN®) makes no representation or warranties of any kind regarding their content, use, or application and disclaims any responsibility for their applications or use in any way. The full NCCN Guidelines for Survivorship are not printed in this issue of JNCCN but can be accessed online at NCCN.org.
© National Comprehensive Cancer Network, Inc. 2014, All rights reserved. The NCCN Guidelines and the illustrations herein may not be reproduced in any form without the express written permission of NCCN.
Disclosures for the NCCN Survivorship Panel
At the beginning of each NCCN Guidelines panel meeting, panel members review all potential conflicts of interest. NCCN, in keeping with its commitment to public transparency, publishes these disclosures for panel members, staff, and NCCN itself.
Individual disclosures for the NCCN Survivorship Panel members can be found on page 986. (The most recent version of these guidelines and accompanying disclosures are available on the NCCN Web site at NCCN.org.)
These guidelines are also available on the Internet. For the latest update, visit NCCN.org.
| Panel Member | Clinical Research Support/Data Safety Monitoring Board | Advisory Boards, Speakers Bureau, Expert Witness, or Consultant | Patent, Equity, or Royalty | Other | Date Completed |
|---|---|---|---|---|---|
| Madhuri Are, MD | None | None | None | None | 5/15/13 |
| K. Scott Baker, MD, MS | None | None | None | None | 11/22/13 |
| Wendy Demark-Wahnefried, PhD, RD | National Cancer Institute; Harvest for Health Gardening Project for Breast Cancer Survivors; and Nutrigenomic Link between Alpha-Linolenic Acid and Aggressive Prostate Cancer | American Society of Clinical Oncology | None | American Society of Preventive Oncology | 11/13/13 |
| Crystal S. Denlinger, MD | Bayer HealthCare; ImClone Systems Incorporated; MedImmune Inc.; OncoMed Pharmaceuticals; Astex Pharmaceuticals; Merrimack Pharmaceuticals; and Pfizer Inc. | Eli Lilly and Company | None | None | 1/9/14 |
| Debra L. Friedman, MD, MS | None | None | None | None | 5/26/13 |
| Mindy Goldman, MD | Pending | ||||
| Lee W. Jones, PhD | None | None | None | None | 2/2/12 |
| Allison King, MD | None | None | None | None | 8/12/13 |
| Grace H. Ku, MD | None | Seattle Genetics, Inc. | None | None | 5/6/14 |
| Elizabeth Kvale, MD | None | None | None | None | 10/7/13 |
| Terry S. Langbaum, MAS | None | None | None | None | 8/13/13 |
| Kristin Leonardi-Warren, RN, ND | None | None | None | None | 1/6/14 |
| Jennifer A. Ligibel, MD | None | None | None | None | 10/3/13 |
| Mary S. McCabe, RN, BS, MS | None | National Cancer Institute | None | None | 5/6/14 |
| Michelle Melisko, MD | Celldex Therapeutics; and Galena Biopharma | Agendia BV; Genentech, Inc.; and Novartis Pharmaceuticals Corporation | None | None | 10/11/13 |
| Jose G. Montoya, MD | None | None | None | None | 12/6/13 |
| Kathi Mooney, RN, PhD | University of Utah | None | None | None | 9/30/13 |
| Mary Ann Morgan, PhD, FNP-BC | None | None | None | None | 5/5/14 |
| Javid J. Moslehi, MD | None | ARIAD Pharmaceuticals, Inc.; Millennium Pharmaceuticals, Inc.; Novartis Pharmaceuticals Corporation; and Pfizer Inc. | None | None | 1/27/14 |
| Tracey O’Connor, MD | None | None | None | None | 6/13/13 |
| Linda Overholser, MD, MPH | None | Antigenics Inc.; and Colorado Central Cancer Registry Care Plan Project | None | None | 10/10/13 |
| Electra D. Paskett, PhD | Merck & Co., Inc. | None | Pfizer Inc. | None | 5/7/14 |
| Muhammad Raza, MD | None | None | None | None | 8/23/12 |
| Karen L. Syrjala, PhD | None | None | None | None | 5/1/14 |
| Susan G. Urba, MD | None | Eisai Inc.; and Helsinn Therapeutics (U.S.), Inc. | None | None | 10/9/13 |
| Mark T. Wakabayashi, MD, MPH | None | None | None | None | 6/19/13 |
| Phyllis Zee, MD | Philips/Respironics | Merck & Co., Inc.; Jazz Pharmaceuticals; Vanda Pharmaceuticals; and Purdue Pharma LP | None | None | 3/26/14 |
References
- 1.Janelsins MC, Kohli S, Mohile SG, et al. An update on cancer- and chemotherapy-related cognitive dysfunction: current status. Semin Oncol. 2011;38:431–438. doi: 10.1053/j.seminoncol.2011.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wefel JS, Schagen SB. Chemotherapy-related cognitive dysfunction. Curr Neurol Neurosci Rep. 2012;12:267–275. doi: 10.1007/s11910-012-0264-9. [DOI] [PubMed] [Google Scholar]
- 3.Ahles TA, Saykin AJ, McDonald BC, et al. Cognitive function in breast cancer patients prior to adjuvant treatment. Breast Cancer Res Treat. 2008;110:143–152. doi: 10.1007/s10549-007-9686-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahles TA, Saykin AJ, McDonald BC, et al. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. J Clin Oncol. 2010;28:4434–4440. doi: 10.1200/JCO.2009.27.0827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahles TA, Root JC, Ryan EL. Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol. 2012;30:3675–3686. doi: 10.1200/JCO.2012.43.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hodgson KD, Hutchinson AD, Wilson CJ, Nettelbeck T. A meta-analysis of the effects of chemotherapy on cognition in patients with cancer. Cancer Treat Rev. 2012;39:297–304. doi: 10.1016/j.ctrv.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Phillips KM, Jim HS, Small BJ, et al. Cognitive functioning after cancer treatment: a 3-year longitudinal comparison of breast cancer survivors treated with chemotherapy or radiation and noncancer controls. Cancer. 2012;118:1925–1932. doi: 10.1002/cncr.26432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wefel JS, Lenzi R, Theriault RL, et al. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;100:2292–2299. doi: 10.1002/cncr.20272. [DOI] [PubMed] [Google Scholar]
- 9.Wefel JS, Lenzi R, Theriault R, et al. ‘Chemobrain’ in breast carcinoma?: a prologue. Cancer. 2004;101:466–475. doi: 10.1002/cncr.20393. [DOI] [PubMed] [Google Scholar]
- 10.Jean-Pierre P, Winters PC, Ahles TA, et al. Prevalence of self-reported memory problems in adult cancer survivors: a national cross-sectional study. J Oncol Pract. 2012;8:30–34. doi: 10.1200/JOP.2011.000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahles TA, Saykin AJ, Furstenberg CT, et al. Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol. 2002;20:485–493. doi: 10.1200/JCO.2002.20.2.485. [DOI] [PubMed] [Google Scholar]
- 12.Anderson-Hanley C, Sherman ML, Riggs R, et al. Neuropsychological effects of treatments for adults with cancer: A meta-analysis and review of the literature. J Int Neuropsychol Soc. 2003;9:967–982. doi: 10.1017/S1355617703970019. [DOI] [PubMed] [Google Scholar]
- 13.Deprez S, Amant F, Smeets A, et al. Longitudinal assessment of chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning. J Clin Oncol. 2012;30:274–281. doi: 10.1200/JCO.2011.36.8571. [DOI] [PubMed] [Google Scholar]
- 14.Jim HS, Phillips KM, Chait S, et al. Meta-analysis of cognitive functioning in breast cancer survivors previously treated with standard-dose chemotherapy. J Clin Oncol. 2012;30:3578–3587. doi: 10.1200/JCO.2011.39.5640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jim HS, Small B, Hartman S, et al. Clinical predictors of cognitive function in adults treated with hematopoietic cell transplantation. Cancer. 2012;118:3407–3416. doi: 10.1002/cncr.26645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meadows ME, Chang G, Jones JA, et al. Predictors of neuropsychological change in patients with chronic myelogenous leukemia and myelodysplastic syndrome. Arch Clin Neuropsychol. 2013;28:363–374. doi: 10.1093/arclin/acs141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santini B, Talacchi A, Squintani G, et al. Cognitive outcome after awake surgery for tumors in language areas. J Neurooncol. 2012;108:319–326. doi: 10.1007/s11060-012-0817-4. [DOI] [PubMed] [Google Scholar]
- 18.Satoer D, Vork J, Visch-Brink E, et al. Cognitive functioning early after surgery of gliomas in eloquent areas. J Neurosurg. 2012;117:831–838. doi: 10.3171/2012.7.JNS12263. [DOI] [PubMed] [Google Scholar]
- 19.Scherwath A, Schirmer L, Kruse M, et al. Cognitive functioning in allogeneic hematopoietic stem cell transplantation recipients and its medical correlates: a prospective multicenter study. Psychooncology. 2013;22:1509–1516. doi: 10.1002/pon.3159. [DOI] [PubMed] [Google Scholar]
- 20.Scoccianti S, Detti B, Cipressi S, et al. Changes in neurocognitive functioning and quality of life in adult patients with brain tumors treated with radiotherapy. J Neurooncol. 2012;108:291–308. doi: 10.1007/s11060-012-0821-8. [DOI] [PubMed] [Google Scholar]
- 21.Stewart A, Bielajew C, Collins B, et al. A meta-analysis of the neuropsychological effects of adjuvant chemotherapy treatment in women treated for breast cancer. Clin Neuropsychol. 2006;20:76–89. doi: 10.1080/138540491005875. [DOI] [PubMed] [Google Scholar]
- 22.Syrjala KL, Artherholt SB, Kurland BF, et al. Prospective neurocognitive function over 5 years after allogeneic hematopoietic cell transplantation for cancer survivors compared with matched controls at 5 years. J Clin Oncol. 2011;29:2397–2404. doi: 10.1200/JCO.2010.33.9119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vardy J, Rourke S, Tannock IF. Evaluation of cognitive function associated with chemotherapy: a review of published studies and recommendations for future research. J Clin Oncol. 2007;25:2455–2463. doi: 10.1200/JCO.2006.08.1604. [DOI] [PubMed] [Google Scholar]
- 24.Zucchella C, Bartolo M, Di Lorenzo C, et al. Cognitive impairment in primary brain tumors outpatients: a prospective cross-sectional survey. J Neurooncol. 2013;112:455–460. doi: 10.1007/s11060-013-1076-8. [DOI] [PubMed] [Google Scholar]
- 25.Koppelmans V, Breteler MM, Boogerd W, et al. Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. J Clin Oncol. 2012;30:1080–1086. doi: 10.1200/JCO.2011.37.0189. [DOI] [PubMed] [Google Scholar]
- 26.Harder H, Van Gool AR, Duivenvoorden HJ, et al. Case-referent comparison of cognitive functions in patients receiving haematopoietic stem-cell transplantation for haematological malignancies: two-year follow-up results. Eur J Cancer. 2007;43:2052–2059. doi: 10.1016/j.ejca.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Ganz PA, Kwan L, Castellon SA, et al. Cognitive complaints after breast cancer treatments: examining the relationship with neuropsychological test performance. J Natl Cancer Inst. 2013;105:791–801. doi: 10.1093/jnci/djt073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer. 2007;7:192–201. doi: 10.1038/nrc2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deprez S, Billiet T, Sunaert S, Leemans A. Diffusion tensor MRI of chemotherapy-induced cognitive impairment in non-CNS cancer patients: a review. Brain Imaging Behav. 2013;7:409–435. doi: 10.1007/s11682-012-9220-1. [DOI] [PubMed] [Google Scholar]
- 30.Simo M, Rifa-Ros X, Rodriguez-Fornells A, Bruna J. Chemobrain: a systematic review of structural and functional neuroimaging studies. Neurosci Biobehav Rev. 2013;37:1311–1321. doi: 10.1016/j.neubiorev.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 31.Wefel JS, Saleeba AK, Buzdar AU, Meyers CA. Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer. 2010;116:3348–3356. doi: 10.1002/cncr.25098. [DOI] [PubMed] [Google Scholar]
- 32.Schagen SB, Das E, Vermeulen I. Information about chemotherapy-associated cognitive problems contributes to cognitive problems in cancer patients. Psychooncology. 2012;21:1132–1135. doi: 10.1002/pon.2011. [DOI] [PubMed] [Google Scholar]
- 33.Nelson CJ, Nandy N, Roth AJ. Chemotherapy and cognitive deficits: mechanisms, findings, and potential interventions. Palliat Support Care. 2007;5:273–280. doi: 10.1017/s1478951507000442. [DOI] [PubMed] [Google Scholar]
- 34.Wefel JS, Vardy J, Ahles T, Schagen SB. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011;12:703–708. doi: 10.1016/S1470-2045(10)70294-1. [DOI] [PubMed] [Google Scholar]
- 35.Vardy J, Wefel JS, Ahles T, et al. Cancer and cancer-therapy related cognitive dysfunction: an international perspective from the Venice cognitive workshop. Ann Oncol. 2008;19:623–629. doi: 10.1093/annonc/mdm500. [DOI] [PubMed] [Google Scholar]
- 36.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 37.Ferguson RJ, McDonald BC, Rocque MA, et al. Development of CBT for chemotherapy-related cognitive change: results of a waitlist control trial. Psychooncology. 2012;21:176–186. doi: 10.1002/pon.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goedendorp MM, Knoop H, Gielissen MF, et al. The effects of cognitive behavioral therapy for postcancer fatigue on perceived cognitive disabilities and neuropsychological test performance. J Pain Symptom Manage. 2014;47:35–44. doi: 10.1016/j.jpainsymman.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 39.Angevaren M, Aufdemkampe G, Verhaar HJ, et al. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2008:CD005381. doi: 10.1002/14651858.CD005381.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Fitzpatrick TR, Edgar L, Holcroft C. Assessing the relationship between physical fitness activities, cognitive health, and quality of life among older cancer survivors. J Psychosoc Oncol. 2012;30:556–572. doi: 10.1080/07347332.2012.703768. [DOI] [PubMed] [Google Scholar]
- 41.Kramer AF, Erickson KI. Capitalizing on cortical plasticity: influence of physical activity on cognition and brain function. Trends Cogn Sci. 2007;11:342–348. doi: 10.1016/j.tics.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 42.Player L, Mackenzie L, Willis K, Loh SY. Women’s experiences of cognitive changes or ‘chemobrain’ following treatment for breast cancer: a role for occupational therapy? Aust Occup Ther J. doi: 10.1111/1440-1630.12113. published online ahead of print February 6, 2014. [DOI] [PubMed] [Google Scholar]
- 43.Gehring K, Roukema JA, Sitskoorn MM. Review of recent studies on interventions for cognitive deficits in patients with cancer. Expert Rev Anticancer Ther. 2012;12:255–269. doi: 10.1586/era.11.202. [DOI] [PubMed] [Google Scholar]
- 44.Mar Fan HG, Clemons M, Xu W, et al. A randomised, placebo-controlled, double-blind trial of the effects of d-methylphenidate on fatigue and cognitive dysfunction in women undergoing adjuvant chemotherapy for breast cancer. Support Care Cancer. 2008;16:577–583. doi: 10.1007/s00520-007-0341-9. [DOI] [PubMed] [Google Scholar]
- 45.Conklin HM, Khan RB, Reddick WE, et al. Acute neurocognitive response to methylphenidate among survivors of childhood cancer: a randomized, double-blind, cross-over trial. J Pediatr Psychol. 2007;32:1127–1139. doi: 10.1093/jpepsy/jsm045. [DOI] [PubMed] [Google Scholar]
- 46.Kohli S, Fisher SG, Tra Y, et al. The effect of modafinil on cognitive function in breast cancer survivors. Cancer. 2009;115:2605–2616. doi: 10.1002/cncr.24287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lundorff LE, Jonsson BH, Sjogren P. Modafinil for attentional and psychomotor dysfunction in advanced cancer: a double-blind, randomised, cross-over trial. Palliat Med. 2009;23:731–738. doi: 10.1177/0269216309106872. [DOI] [PubMed] [Google Scholar]
- 48.Gehring K, Patwardhan SY, Collins R, et al. A randomized trial on the efficacy of methylphenidate and modafinil for improving cognitive functioning and symptoms in patients with a primary brain tumor. J Neurooncol. 2012;107:165–174. doi: 10.1007/s11060-011-0723-1. [DOI] [PubMed] [Google Scholar]


