Abstract
Background
Breast cancer is a troublesome health problem, particularly among underserved and minority women. Early detection through screening mammography can reduce the impact of this disease, yet it remains underused.
Objective
We examined cost as a barrier to screening mammography and studied the accuracy of women’s perceptions of the cost of a mammogram among a rural, low-income, tri-racial (white, Native American and African American) population in need of a mammogram.
Design
We interviewed 897 women age 40 and older, asking about cost as a barrier to mammography and perceptions about the actual costs of a screening mammogram. Face-to-face interviews were conducted between 1998 and 2000 among women participating in a randomized, controlled study to evaluate a health education intervention to improve mammography screening rates in an underserved population. All data used in these analyses were from the baseline interviews.
Results
Cost acted as a barrier to screening mammography for a majority of the participants (53%). More than half of these women (52%), however, overestimated the cost of a screening mammogram, and overestimation of the cost was significantly related to mentioning cost as a barrier (OR 1.56, 95% CI 1.04–2.33). Higher estimates of out-of-pocket costs were associated with reporting cost as a barrier to mammography (OR 2.25, 95% CI 1.43–3.52 for $1–50 and OR 12.64, 95% CI 6.61–24.17 for > $50). Factors such as race, income and employment status were not related to reporting cost as a barrier to screening mammography.
Conclusions
Among a group of tri-racial, low-income, rural women who were in need of a mammogram, cost was a common barrier. Overestimating the cost, however, was significantly and positively associated with reporting cost as a barrier. Providing information about the actual cost women have to pay for mammograms may lessen the role of cost as a barrier to mammography screening, especially for underserved women, potentially improving utilization rates.
Keywords: Mammography, Screening, Rural, Cost, Barriers, Access to care
Introduction
Despite considerable advances in scientific understanding of the disease, breast cancer remains a significant health problem for women. In the USA alone, the American Cancer Society estimated that breast cancer claimed the lives of 40,580 women in 2004, while another 215,990 women were diagnosed with the disease (American Cancer Society 2004). Among African Americans, breast cancer is the most common cancer among women, and African American women are 30% more likely to die of breast cancer than white women (American Cancer Society 2005). It is generally accepted that mammography represents the best opportunity for early detection of breast cancer (Adams et al. 2001; Schwartz et al. 2004), and the American Cancer Society currently recommends annual mammograms for women over the age of 40 (American Cancer Society 2003).
Mammography utilization has increased in the past decade, but in 2002, one-quarter of US women over the age of 40 had not had a mammogram within the past two years (Centers for Disease Control and Prevention 2004). Among underserved women, non-compliance with screening recommendations is especially problematic. Racial and ethnic disparities in mammography utilization persist (National Center for Health Statistics 2004), with white women more likely to be adherent than minority women, and African American women more likely to be diagnosed at a later stage of cancer than whites (American Cancer Society 2005). Recent data have also shown that women with lower incomes and lower education levels are consistently less likely to have had a mammogram within the past year compared to their wealthier and better educated counterparts (National Center for Health Statistics 2004). Similarly, women who live in rural areas reportedly receive screening mammograms at a significantly lower rate compared to women who live in urban areas (Coughlin et al. 2002).
Various explanations for lack of compliance with recommendations for screening mammography have been proposed, but perhaps one of the most tangible is the barrier of cost (Stein et al. 1991; Kiefe et al. 1994; Urban et al. 1994; Miller & Champion 1997; Adams et al. 2001). In general, perceived cost has been shown to be a substantial barrier to medical care, and presents a greater burden to people who are black or Hispanic, younger, unemployed, or have lower income or education levels (Weissman et al. 1991; Blendon et al. 1995; Himmelstein & Woolhandler 1995; Nelson et al. 1999). With respect to screening mammography, studies have shown that income level is related to concerns about cost and receipt of mammography (Lane et al. 1992), and that such financial concerns are especially salient for rural women (Zhang et al. 2000; Adams et al. 2001). The impact of cost as a barrier is quite significant, even among women whose insurance provides some level of coverage for a mammogram (Urban et al. 1994; Gordon et al. 1998; Friedman et al. 2002; Suter et al. 2002). As cost is an important barrier to women who have received mammograms, it is likely to also be a reason for lack of compliance with mammography screening guidelines. Further, knowledge and attitudes regarding mammography as well as barriers to receiving a screening mammogram have been shown to vary among ethnic groups (Glanz et al. 1996; McGarvey et al. 2003). It is thus important to investigate how cost may act as a barrier to mammography among women of different races and ethnicities.
Few studies have evaluated the various factors associated with women reporting cost as a barrier to screening mammography, and scant research has studied the appropriateness of women’s perceptions of that cost barrier (Urban et al. 1994), especially among underserved women. We have previously examined women’s perceptions of insurance coverage for screening mammography (McAlearney et al. 2005), but we did not focus specifically on women’s self-report of cost as a barrier. In this report we investigated cost as a barrier to mammography in a tri-racial population of low-income, underserved women in need of a mammogram. We then explored whether or not inappropriate perceptions of the cost of mammography influenced reporting cost as a barrier to screening, and whether there were any differences by race. Our results have important implications for researchers and providers seeking to understand why underserved women do not obtain mammograms as recommended.
Conceptual Framework
Theory in the area of health behavior change and health promotion was used as a conceptual framework to guide our study of the importance of cost as a barrier to screening mammography. The Health Belief Model (Rosenstock 1966; Becker 1974; Rosenstock 1974; Janz & Becker 1984) relies on the notion that an individual’s health behaviors depend on both knowledge and motivation. When a person decides to seek care, the individual’s perceptions about factors such as vulnerability to illness and effectiveness of medical care become important. In the case of screening mammography, if women believe that they are vulnerable to breast cancer, that cancer is a serious problem, and that screening will be effective and not excessively expensive, they will then interpret a screening opportunity as a cue to act and obtain a screening mammogram (Elder 1994). However, variability in any of these factors, including women’s perceptions of the cost of a screening mammogram, may affect their motivation to seek a mammogram, resulting in lower mammography rates. Further, variability by race or by ethnicity might be particularly telling, contributing to low rates for screening mammography among underserved women.
Given this crucial link between individuals’ beliefs and their behaviors, our research was designed to study women’s perceptions of cost as a potential barrier to screening mammography. If women reported that high costs present a barrier to screening, yet their perceptions about screening expenses were inaccurate, interventions that improve knowledge about actual screening costs may help remove these misconceptions. In contrast, if perceptions of costs were accurate, efforts to improve screening rates must focus first on reducing the actual cost barrier to screening mammography. Finally, if perceptions differed by race or other demographic factors, these differences must be taken into account when designing appropriate tailored interventions to improve screening rates.
Methods
Population Studied
Women interviewed in this study resided in Robeson County, North Carolina which is characterized by a large concentration of Native Americans (Lumbee) as well as a considerable population of African Americans. This rural county is consistently ranked among the poorest counties in North Carolina, and at the time of this study, was ranked eighth poorest in the state with a poverty rate of 24.7% (US Department of Commerce 2001). Less than half of the adults were high school graduates.
Within Robeson County, the Robeson Health Care Corporation (RHCC) is a major health care provider, and the Bureau of Primary Care provides funding for four sites funded through a Community Health Center program. At the time of the study, Lumberton Radiological Associates (LRA) was the primary provider of mammography services in the county, and for the Breast and Cervical Cancer Control Program (BCCCP). All participants in our study used RHCC services. Overall, one-third of RHCC users had no health insurance, 32% were covered by Medicaid and 63% had incomes below the poverty level. The standard of care at RHCC at the time of this study was to recommend annual mammograms for women starting at age 40. The cost of a mammogram through LRA could be billed to any private insurance, Medicare or Medicaid.
Sample Selection
This manuscript uses baseline data from the Robeson County Outreach, Screening and Education (ROSE) Project, a randomized, controlled trial of an intervention designed to improve breast cancer screening rates among rural, poor and minority women in Robeson County, North Carolina. This study has been described elsewhere (Paskett et al. 2004) and is briefly described here. Charts of 2,954 women were randomly selected for review, and 51% of these women (1,503) were determined to be eligible to participate in the trial (patients of RHCC for at least the past two years, age 40 and older, and in need of a mammogram). Upon a telephone screening interview, the eligibility of 1,150 women was confirmed; the other 353 women were deemed ineligible to participate (i.e. moved, deceased, mentally/physically unable, etc.). A total of 1,022 (89%) were able to be contacted, and 901 of these women were enrolled for a participation rate of 81%. Four women were later found to have had a recent mammogram and were not included in the ongoing study; the remaining 897 women were included in our analyses. All women provided written informed consent, and this study was approved by the Institutional Review Boards at Wake Forest University and The Ohio State University.
Measures
The baseline interview collected information such as demographics, knowledge of breast cancer and awareness of screening services for breast cancer. Multiple items on the survey were aimed at identifying whether cost was a barrier to mammography for women in the study population. Women were asked if cost made it hard for them to get a mammogram and whether they felt they could not afford to go to the doctor for tests. They were also asked to give reasons for not having had a mammogram, and could mention problems with cost or insurance in their responses. The number of affirmative responses to these items was used to determine the number of times women identified cost as a barrier to mammography, with a possible range of zero to four. Women were also asked how much a screening mammogram cost in their community, and were probed to choose from seven price ranges if they did not know. At the time of the baseline interview (1998–2000), the cost of a mammogram at LRA was $60. Those women whose answers fell in the range of $51–75 were determined to have an ‘appropriate’ perception of the cost of a mammogram. Women who reported the cost to be $50 or less were considered to ‘underestimate’ the cost of a mammogram, while women who reported the cost to be higher than $75 were determined to ‘overestimate’ the actual cost.
Statistical Analysis
All data for these analyses came from the baseline interview, prior to randomization and administration of the intervention. Univariate analyses were conducted to describe the demographic characteristics of the baseline study population (n=897) and chi-square tests of homogeneity were used to investigate bivariate relationships between independent variables and the dependent variables related to cost. Using logistic regression analysis, odds ratios and 95% confidence intervals (CI) for multivariable associations were calculated. Dummy variables were created as appropriate for categorical variables including race (i.e. white, African American, Native American, other), and age was used as a categorical variable in all models (ages 40–49, 50–64 and ≥65). Multinomial logistic regression was performed to assess predictors of the level of appropriateness of perception of cost, using ‘appropriate’ as the referent category and controlling for all other independent variables included in the regression analysis. Subjects missing data for any of the variables in the regression were excluded (3.65%), leaving 866 women for this analysis. STATA version 8.0 was used for the multinomial logistic regression analysis (Stata Corporation, College Station, TX). All other analyses were performed using SAS version 8.2 (SAS Institute Inc., Cary, NC).
Results
Study Population
The study population (n=897) was representative of the population of Robeson County, North Carolina, as one-third (33%) of our participants were African American, 41% were Native American, and 25% were white; five women were mixed race. Women were predominantly low income, with nearly three-quarters (74%) of all women, and 78% of African American women in particular, reporting incomes of less than $20,000. Over one-quarter (28%) of the participants were uninsured, while 42% were covered by some form of public insurance (Medicaid, Medicare or a combination). One in five women (20%) completed only eighth grade or less, and another one-quarter (24%) reported that they had some high school education but had not graduated. Demographic characteristics for the total study population and by racial group are shown in Table 1.
Table 1.
Demographic Characteristics of Study Participants, by Race (n = 892)a
| TOTAL (N = 892) |
White (N = 226) |
African American (N = 295) |
Native American (N= 3 71) |
p-Valueb | |
|---|---|---|---|---|---|
| Age, N (%) | 0.002 | ||||
| 40–49 | 377 (42.3) | 81 (35.8) | 146 (49.5) | 150 (40.4) | W vs AA: 0.008 |
| 50–64 | 325 (36.4) | 86 (38.1) | 86 (29.2) | 153 (41.2) | W vs NA: 0.078 |
| ≥65 | 190 (21.3) | 59 (26.1) | 63 (21.4) | 68 (18.3) | AA vs NA: 0.005 |
| Income, N (%) | 0.069 | ||||
| < $20,000 | 635 (73.8) | 148 (68.8) | 223 (78.0) | 264 (73.3) | W vs AA: 0.021 |
| ≥ $20,000 | 226 (26.2) | 67 (31.2) | 63 (22.0) | 96 (26.7) | W vs NA: 0.247 |
| AA vs NA: 0.174 | |||||
| Insurance status, N (%) | 0.005 | ||||
| Private only | 267 (30.0) | 77 (34.1) | 87 (29.6) | 103 (27.8) | W vs AA: 0.026 |
| Medicaid only | 114 (12.8) | 30 (13.3) | 45 (15.3) | 39 (10.5) | W vs NA: 0.002 |
| Medicare/Medicaid | 114 (12.8) | 22 (9.7) | 42 (14.3) | 50 (13.5) | AA vs NA: 0.387 |
| Medicare/private | 52 (5.8) | 24 (10.6) | 12 (4.1) | 16 (4.3) | |
| Medicare only | 95 (10.7) | 24 (10.6) | 29 (9.9) | 42 (11.4) | |
| No insurance | 248 (27.9) | 49 (21.7) | 79 (26.9) | 120 (32.4) | |
| Education, N (%) | <0.001 | ||||
| 8th grade or less | 181 (20.3) | 45 (19.9) | 38 (12.9) | 98 (26.4) | W vs AA: 0.081 |
| Some high school | 211 (23.7) | 47 (20.8) | 73 (24.8) | 91 (24.5) | W vs NA: 0.047 |
| High school graduate | 500 (56.0) | 134 (59.3) | 184 (62.4) | 182 (49.1) | AA vs NA: <0.001 |
| Working status, N (%) | 0.257 | ||||
| Full/part time | 374 (41.9) | 95 (42.0) | 134 (45.4) | 145 (39.1) | W vs AA: 0.44 |
| Other | 518 (58.1) | 131 (58.0) | 161 (54.6) | 226 (60.9) | W vs NA: 0.476 |
| AA vs NA: 0.099 | |||||
| Marital status, N (%) | <0.001 | ||||
| Married/living together | 397 (44.5) | 119 (52.7) | 98 (33.2) | 180 (48.5) | W vs AA: <0.001 |
| Other | 495 (55.5) | 107 (47.4) | 197 (66.8) | 191 (51.5) | W vs NA: 0.327 |
| AA vs NA: <0.001 |
Five women were of mixed race and thus are not included in this table.
From chi-square test over all categories of race and then paired comparisons; W=White, AA=African American, NA=Native American.
Cost as a Barrier to Screening Mammography
Women who had never had a mammogram (n=209) or had not had one within the past two years (n=298) were asked to give reasons for not getting a mammogram. Cost was the most frequently cited reason by both groups, with one-quarter of former-users and one-fifth of never-users reporting cost as a reason. Over half (53%) of the 897 women interviewed identified cost as a barrier to mammography at least once. Further, 19% identified cost as a barrier three or four times. Among women who identified cost as a barrier to mammography at least once (n=478), 77% specifically said that cost made it hard for them to get a mammogram and 70% agreed that they could only afford to go to the doctor if they were sick.
Appropriateness of Cost Perceptions
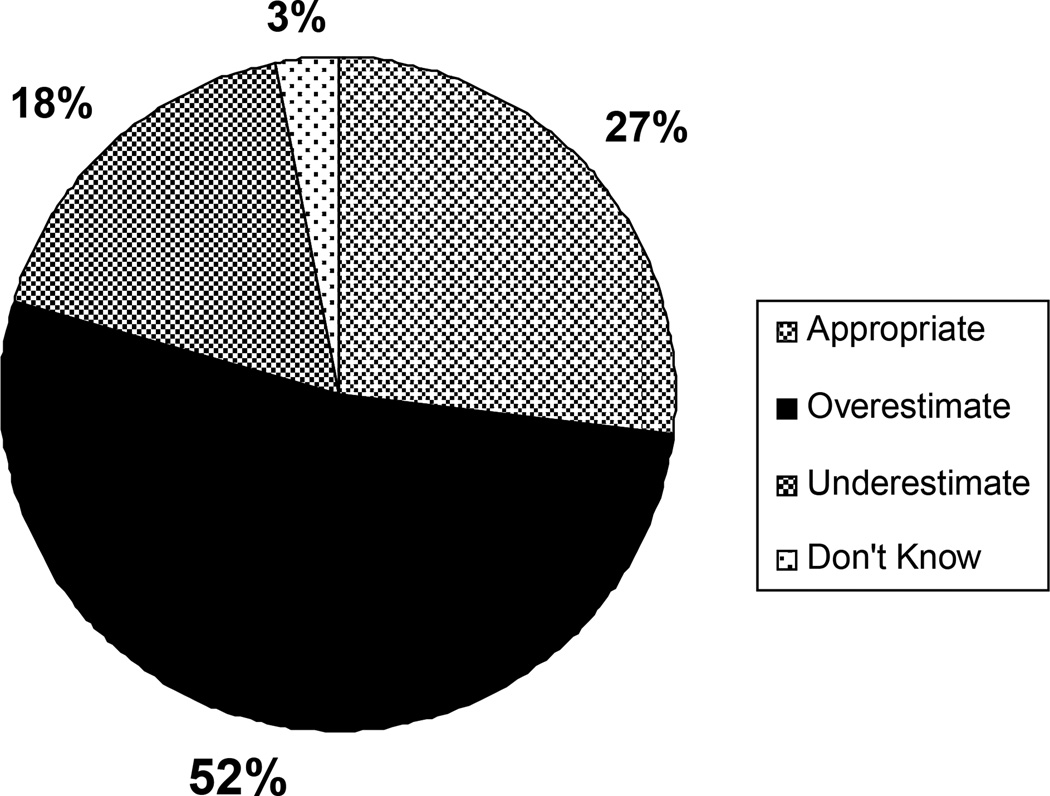
As cost was reportedly a significant barrier for this population, women’s knowledge of the true cost of screening mammography was explored. Figure 1 presents the distribution of the appropriateness of women’s perception of the cost of a screening mammogram. Overall, 52% of the women in our study overestimated the cost of a mammogram in their community. In contrast, only 27% of these women had an appropriate perception of this cost.
Figure 1.
Distribution of Appropriateness of Perception of Cost of a Screening Mammogram (n=897).
Identifying Cost as a Barrier
Logistic regression analysis was used to determine what factors were related to identifying cost as a barrier (Table 2). Insurance status was related to whether or not women reported that cost was a barrier. Women without insurance had three times the odds of identifying cost as a barrier to mammography (OR 3.27, 95% CI 1.71–6.25) compared to privately insured women. Additionally, women dually covered by Medicare and private insurance had one-third the odds of reporting cost as a barrier (OR 0.34, 95% CI 0.13–0.91) compared to women with only private insurance. There were no significant associations with income, race, marital status or work status.
Table 2.
Associations between Independent Variables and Identification of Cost as a Barrier to Mammography (n = 866)a
| Identified cost as a barrier to mammography |
||||
|---|---|---|---|---|
| No (n) | Yes (n) | OR | 95% CI | |
| Race | ||||
| White | 107 | 119 | 1.00 | – |
| African American | 147 | 148 | 0.82 | 0.52–1.29 |
| Native American | 163 | 208 | 0.83 | 0.54–1.28 |
| Other | 2 | 3 | 1.31 | 0.17–10.46 |
| Insurance status | ||||
| Private only | 155 | 117 | 1.00 | – |
| Medicaid only | 73 | 42 | 0.71 | 0.35–1.43 |
| Medicare/Medicaid | 75 | 39 | 0.52 | 0.23–1.19 |
| Medicare/private | 41 | 11 | 0.34b | 0.13–0.91 |
| Medicare only | 50 | 45 | 0.88 | 0.40–1.90 |
| No insurance | 25 | 224 | 3.27c | 1.71–6.25 |
| Perceived health | ||||
| Fair/poor | 127 | 163 | 1.00 | – |
| Good | 127 | 149 | 0.96 | 0.62–1.48 |
| Very good/excellent | 165 | 166 | 0.65 | 0.42–1.02 |
| Regular check-up in past 12 months | ||||
| No | 98 | 177 | 1.00 | – |
| Yes | 321 | 301 | 0.57c | 0.39–0.82 |
| Appropriateness of perception of cost | ||||
| Appropriate | 116 | 126 | 1.00 | – |
| Underestimate | 90 | 67 | 0.79 | 0.47–1.32 |
| Overestimate | 197 | 274 | 1.56b | 1.04–2.33 |
| Don’t know | 16 | 11 | 1.31 | 0.45–3.79 |
| Out-of-pocket costd | ||||
| $0 | 245 | 102 | 1.00 | – |
| $1–50 | 108 | 93 | 2.25c | 1.43–3.52 |
| >$50 | 22 | 225 | 12.64c | 6.61–24.17 |
| Don’t know | 44 | 58 | 2.68c | 1.56–4.60 |
Adjusted for age (40–49, 50–64, ≥65), marital status (married/living together vs other), educational level (8th grade or less, some high school, high school graduate), employment status (full time vs other), income (≥$20,000 vs <$20,000), family history of breast cancer (no vs yes), believe doctor wants you to get a mammogram (no vs yes), doctor has recommended a mammogram (no vs yes), worry about breast cancer (not at all/slightly, moderately, quite a bit/extremely) and history of mammography (no vs yes).
p ≤ 0.05.
p ≤ 0.01.
For $0 to > $50 categories ptrend<0.001.
Women who reported having had a regular check-up in the 12 months before the interview had lower odds of noting cost as a barrier (OR 0.57, 95% CI 0.39–0.82) than women who had not had a check-up. Women who perceived their health to be ‘excellent’ or ‘very good’ had marginally significantly lower odds of reporting cost was a barrier (OR 0.65, 95% CI 0.42–1.02) compared to those who reported their health to be ‘poor’ or ‘fair’.
Underestimating or not knowing the cost of a mammogram was not related to reporting cost as a barrier. In contrast, women who overestimated cost had significantly greater odds of noting cost as a barrier to getting a mammogram (OR 1.56, 95% CI 1.04–2.33) compared to women with an appropriate perception of the cost.
A significant linear relationship was observed between women’s reported level of out-of-pocket cost for a mammogram and their assessment of cost as a barrier to mammography (ptrend<0.001). Compared to women who reported that they had no out-of-pocket costs for a mammogram, women who reported having to pay $1–50 had twice the odds of noting cost as a barrier (OR 2.26, 95% CI 1.43–3.52). Women who reported out-of-pocket costs of more than $50 for a mammogram had nearly 13 times the odds of noting cost as a barrier (OR 12.64, 95% CI 6.61–24.17). Women who did not know how much they would have to pay out-of-pocket for a mammogram had almost three times the odds of stating that cost was a barrier to obtaining a mammogram (OR 2.68, 95% CI 1.568–4.60).
Predictors of Perceptions of Cost
Multinomial logistic regression was used to determine what characteristics were related to the different levels of appropriateness of perceived cost of a mammogram. None of the variables were significantly associated with having underestimated the cost of a mammogram, and small numbers of women in the ‘don’t know’ category led to unstable odds ratio estimates for that model; thus the models for underestimating and reporting ‘don’t know’ for cost are not shown.
Table 3 presents the model for overestimate (n=691). Insurance status was significantly related to the appropriateness of the perception of the cost of a mammogram. Women reporting Medicaid as their only source of health insurance had twice the odds (OR 2.10, 95% CI 1.05–4.19) and women covered by both Medicaid and Medicare had greater than twice the odds (OR 2.44, 95% CI 1.05–5.70) of overestimating the cost of a mammogram than to have an appropriate perception of the cost, compared to privately insured women. Also, those women with moderate levels of worry about their risk of getting breast cancer had twice the odds of overestimating the cost as compared to women who were not or only slightly worried (OR 2.04, 95% CI 1.22–3.39).
Table 3.
Associations between Independent Variables and Overestimating Compared to Appropriately Estimating the Cost of a Mammogram (n = 691)a
| Model: Overestimate of true cost vs appropriate estimate of true cost | OR | 95% CI |
|---|---|---|
| Race | ||
| White | 1.00 | – |
| African American | 1.17 | 0.74–1.83 |
| Native American | 1.21 | 0.79–1.84 |
| Other | 2.62 | 0.27–25.66 |
| Insurance status | ||
| Private only | 1.00 | – |
| Medicaid only | 2.10b | 1.05–4.19 |
| Medicare/Medicaid | 2.44b | 1.05–5.70 |
| Medicare/private | 1.01 | 0.39–2.58 |
| Medicare only | 1.37 | 0.61–3.08 |
| No insurance | 0.99 | 0.59–1.67 |
| Number of times cost identified as a barrier | ||
| 0 | 1.00 | – |
| 1 | 1.15 | 0.75–1.76 |
| ≥2 | 2.08c | 1.29–3.35 |
| Level of worry about breast cancer | ||
| Not at all/slightly | 1.00 | – |
| Moderately | 2.04c | 1.22–3.39 |
| Quite a bit/extremely | 1.38 | 0.88–2.16 |
Model is adjusted for age (40–49, 50–64, ≥65), marital status (married/living together vs other), educational level (8th grade or less, some high school, high school graduate), employment status (full time vs other), income (≥$20,000 vs <$20,000), family history of breast cancer (no vs yes), perceived health (fair/poor, good, very good/excellent), regular check-up within past 12 months (no vs yes), believe doctor wants you to get a mammogram (no vs yes), doctor has recommended a mammogram (no vs yes) and history of mammography (no vs yes).
p ≤ 0.05.
p ≤ 0.01.
Women who identified cost as a barrier to mammography more than once had twice the odds of overestimating the cost of a mammogram (OR 2.08, 95% CI 1.29–3.35) instead of giving an appropriate response, compared to those who did not report cost as a barrier to mammography. Race, income and employment status were not associated with the appropriateness of cost perceptions.
Discussion
Cost was cited as a barrier to mammography screening by over half of a population of underserved, tri-racial, rural women in need of a mammogram. Our findings are consistent with prior research demonstrating that cost concerns create a barrier for many individuals to access needed medical services, especially low-income, minority and uninsured persons (Weissman et al. 1991; Harvey & Faber 1993; Braveman et al. 1994; Himmelstein & Woolhandler 1995). In particular, our population of low-income women most frequently cited cost as the reason for not having had a mammogram.
Yet, these women’s perceptions of the cost of a mammogram in their county were often inaccurate. While the true cost of a mammogram at the time of the study (1998–2000) was approximately $60, over half of the women believed a mammogram cost more than $75. In comparison to our previous study where we found that 40% of these women had an inappropriate perception of their insurance coverage (McAlearney et al. 2005), here we found that nearly three-quarters (73%) of the women had an inappropriate perception of the cost of a mammogram, with over half (52%) overestimating the cost. Inappropriate perceptions of the cost of services may not be surprising. However, our findings revealed that these perceptions were distinctly related to women’s reports of cost as a barrier to screening mammography. We found that women who reported cost as a barrier to mammography multiple times during the course of the interview had increased odds of overestimating the cost of a mammogram. Additionally, our analyses showed a significant relationship between perceived levels of out-of-pocket costs and women’s assessments of cost as a barrier to receiving a mammogram. As such, higher estimated cost levels, whether accurate or not, were associated with greater perceived cost burden across our study population. We found that women who reported higher estimates of out-of-pocket costs had nearly 13 times the odds of noting cost as a barrier, highlighting a potential problem associated with inappropriate cost perceptions. As women’s perceptions may affect their care-seeking behaviors, our findings that both higher estimates of out-of-pocket costs and overestimation of the true mammography cost being associated with reports of cost as a barrier to mammography screening are troublesome.
It is of particular interest to note that factors such as income, race and employment status were not related to reporting a cost barrier. We might expect that individuals with lower incomes and without full- or part-time jobs might be more likely to report a barrier to mammography due to cost, yet this was not the case in our population. Overestimation of mammography cost and high estimates of out-of-pocket costs were independently and strongly related to reported cost barriers. Thus, perceptions of what a mammogram would cost were important, even in situations in which lack of money is likely an real issue (i.e. among women with low incomes or without jobs). This provides further evidence that the barrier of cost may be meaningfully influenced by perceptions as well as by reality.
While we were unable to test the association between perceptual accuracy and actual screening practices, the Health Belief Model provides compelling theoretical support for our concern. According to this theoretical framework, a woman who believes that the cost of a mammogram is too high may be less motivated to seek out screening and therefore less likely to receive a mammogram. Admittedly, cost is truly a barrier for many women (Stein et al. 1991; Kiefe et al. 1994; Urban et al. 1994; Miller & Champion 1997; Adams et al. 2001); however, our study found that women who overestimated the cost of a mammogram were significantly more likely to report cost as a barrier. Thus, educating women about the actual costs of mammography should improve their understanding of this expense and, theoretically, increase their motivation to receive a mammogram. This will be an important area for future research.
Several potential limitations of this study should be considered when interpreting our findings. First, the racial and ethnic composition of this area makes the study population somewhat unusual. Our finding of no racial differences in cost perceptions may reflect a unique characteristic of our study population wherein the numbers of African Americans and Native Americans studied are both larger than the number of Caucasians, and all women were low income. However, our results are strengthened considerably by our control for multiple demographic and health characteristics. Second, because our information was gathered through a single interview, a causal relation between appropriateness of cost perceptions and receipt of screening mammograms could not be investigated. Third, our sample population is admittedly biased because all women participating needed a mammogram and had self-selected to participate in the study. We believe, however, that our findings about the barrier of cost within a population of underserved women needing a screening mammogram remain striking despite this bias.
The cost of a mammogram is a concern for low-income women and can present a seemingly insurmountable barrier to needed screening. This is the first study, however, to investigate the appropriateness of women’s perceptions of cost among women in need of a mammogram, and we found that a majority of women overestimated the cost of a mammogram. The barrier of cost may thus seem inappropriately burdensome rather than reflect women’s understanding of the true costs they would be responsible to pay. According to the Health Belief Model which guided our investigation, these inaccurate perceptions of cost may negatively influence a woman’s motivation to receive a mammogram.
Various interventions designed to improve breast cancer screening have focused on reducing or eliminating cost as a barrier (Kiefe et al. 1994; Skaer et al. 1996; Stoner et al. 1998), and the success of such programs is likely associated with reducing the reality of cost as a barrier. However, programs designed to increase appropriate use of screening mammograms would appear to benefit substantially by educating women about the actual cost of a screening mammogram, as well as the levels of coverage available (McAlearney et al. 2005) to pay for the test, or refer to the CDC Breast and Cervical Cancer Detection Program (BCCDP). We hypothesize that providing accurate cost information would help reduce the cost barrier to screening mammography, but we were not able to study this effect. Future studies will be needed to investigate if improving the appropriateness of women’s perceptions of cost can lead to receipt of screening mammography.
Providing cost information to patients, or directing them to it, may substantially reduce the impact of perceived cost as a barrier to screening mammography. As the true cost of a mammogram continues to increase (e.g. the charge at LRA is now $163), the perceived cost will likely increase as well. Thus, providing women with accurate information about the cost of screening mammography, and ways to pay for a mammogram when cost is a barrier, will be important.
Acknowledgements
This research was supported by NIH NCI Grant Nos. CA72022-04 and CA57707-08. An earlier version of this paper was presented as a poster at the Academy Health Annual Research Meeting, San Diego, California, 6 June 2004.
References
- Adams ML, Becker H, Colbert A. African-American women’s perceptions of mammography screening. Journal of National Black Nurses Association: JNBNA. 2001;12:44–48. [PubMed] [Google Scholar]
- American Cancer Society. Cancer prevention & early detection: facts & figures 2003. Atlanta, GA: American Cancer Society; 2003. [Google Scholar]
- American Cancer Society. Cancer facts & figures 2004. Atlanta, GA: American Cancer Society; 2004. [Google Scholar]
- American Cancer Society. Cancer facts & figures for African Americans 2005–2006. Atlanta, GA: American Cancer Society; 2005. [Google Scholar]
- Becker M. The Health Belief Model and personal health behavior. Health Education Monographs. 1974;2:324–473. [Google Scholar]
- Blendon RJ, Scheck AC, Donelan K, Hill CA, Smith M, Beatrice D, Altman D. How white and African Americans view their health and social problems. Different experiences, different expectations. JAMA: The Journal of the American Medical Association. 1995;273:341–346. [PubMed] [Google Scholar]
- Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. The New England Journal of Medicine. 1994;331:444–449. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [accessed 8 December 2004];BRFSS trends data, nationwide, no mammogram within 2 years, 2002. 2004 Available at: http://apps.nccd.cdc.gov/brfss/Trends/trendchart.asp?qkey=10060&state=US.
- Coughlin SS, Thompson TD, Hall HI, Logan P, Uhler RJ. Breast and cervical carcinoma screening practices among women in rural and nonrural areas of the United States, 1998–1999. Cancer. 2002;94:2801–2812. doi: 10.1002/cncr.10577. [DOI] [PubMed] [Google Scholar]
- Elder JP. Motivating Health Behavior. Delmar, Albany, NY: 1994. [Google Scholar]
- Friedman C, Ahmed F, Franks A, Weatherup T, Manning M, Vance A, Thompson BL. Association between health insurance coverage of office visit and cancer screening among women. Medical Care. 2002;40:1060–1067. doi: 10.1097/00005650-200211000-00007. [DOI] [PubMed] [Google Scholar]
- Glanz K, Resch N, Lerman C, Rimer BK. Black–white differences in factors influencing mammography use among employed female health maintenance organization members. Ethnicity & Health. 1996;1:207–220. doi: 10.1080/13557858.1996.9961789. [DOI] [PubMed] [Google Scholar]
- Gordon NP, Rundall TG, Parker L. Type of health care coverage and the likelihood of being screened for cancer. Medical Care. 1998;36:636–645. doi: 10.1097/00005650-199805000-00004. [DOI] [PubMed] [Google Scholar]
- Harvey SM, Faber KS. Obstacles to prenatal care following implementation of a community-based program to reduce financial barriers. Family Planning Perspectives. 1993;25:32–36. [PubMed] [Google Scholar]
- Himmelstein DU, Woolhandler S. Care denied: US residents who are unable to obtain needed medical services. American Journal of Public Health. 1995;85:341–344. doi: 10.2105/ajph.85.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz N, Becker M. The Health Belief Model: a decade later. Health Education Quarterly. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Kiefe CI, Mckay SV, Halevy A, Brody BA. Is cost a barrier to screening mammography for low-income women receiving Medicare benefits? A randomized trial. Archives of Internal Medicine. 1994;154:1217–1224. [PubMed] [Google Scholar]
- Lane DS, Polednak AP, Burg MA. Breast cancer screening practices among users of county-funded health centers vs women in the entire community. American Journal of Public Health. 1992;82:199–203. doi: 10.2105/ajph.82.2.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlearney AS, Reeves KW, Tatum C, Paskett ED. Perceptions of insurance coverage for screening mammography among women in need of screening. Cancer. 2005;103:2473–2480. doi: 10.1002/cncr.21068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarvey EL, Clavet GJ, Johnson JB, Butler A, Cook KO, Pennino B. Cancer screening practices and attitudes: comparison of low-income women in three ethnic groups. Ethnicity & Health. 2003;8:71–82. doi: 10.1080/13557850303556. [DOI] [PubMed] [Google Scholar]
- Miller AM, Champion VL. Attitudes about breast cancer and mammography: racial, income, and educational differences. Women and Health. 1997;26:41–63. doi: 10.1300/J013v26n01_04. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2004 with chartbook on trends in the health of Americans. Hyattsville, MD: 2004. [PubMed] [Google Scholar]
- Nelson DE, Thompson BL, Bland SD, Rubinson R. Trends in perceived cost as a barrier to medical care, 1991–1996. American Journal of Public Health. 1999;89:1410–1413. doi: 10.2105/ajph.89.9.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paskett ED, Tatum C, Rushing J, Michielutte R, Bell R, Foley KL, Bittoni M, Dickinson S. Racial differences in knowledge, attitudes, and cancer screening practices among a triracial rural population. Cancer. 2004;101:2650–2659. doi: 10.1002/cncr.20671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM. Why people use health services. Milbank Memorial Fund Quarterly. 1966;44:9–124. [PubMed] [Google Scholar]
- Rosenstock IM. Historical origins of the Health Belief Model. Health Education Monographs. 1974;2:328–355. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Fowler FJ, Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA: The Journal of the American Medical Association. 2004;291:71–78. doi: 10.1001/jama.291.1.71. [DOI] [PubMed] [Google Scholar]
- Skaer TL, Robison LM, Sclar DA, Harding GH. Financial incentive and the use of mammography among Hispanic migrants to the United States. Health Care for Women International. 1996;17:281–291. doi: 10.1080/07399339609516245. [DOI] [PubMed] [Google Scholar]
- Stein JA, Fox SA, Murata PJ. The influence of ethnicity, socioeconomic status, and psychological barriers on use of mammography. Journal of Health and Social Behavior. 1991;32:101–113. [PubMed] [Google Scholar]
- Stoner TJ, Dowd B, Carr WP, Maldonado G, Church TR, Mandel J. Do vouchers improve breast cancer screening rates? Results from a randomized trial. Health Services Research. 1998;33:11–28. [PMC free article] [PubMed] [Google Scholar]
- Suter LG, Nakano CY, Elmore JG. The personal costs and convenience of screening mammography. Journal of Women’s Health and Gender-Based Medicine. 2002;11:667–672. doi: 10.1089/152460902760360603. [DOI] [PubMed] [Google Scholar]
- Urban N, Anderson GL, Peacock S. Mammography screening: how important is cost as a barrier to use? American Journal of Public Health. 1994;84:50–55. doi: 10.2105/ajph.84.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Commerce, Bureau of the Census. United States Census 2000. Washington, DC: US Government Printing Office; 2001. [Google Scholar]
- Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, and consequences. Annals of Internal Medicine. 1991;114:325–331. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- Zhang P, Tao G, Irwin KL. Utilization of preventive medical services in the United States: a comparison between rural and urban populations. The Journal of Rural Health. 2000;16:349–356. doi: 10.1111/j.1748-0361.2000.tb00485.x. [DOI] [PubMed] [Google Scholar]