Abstract
Many cancer survivors report that fatigue is a disruptive symptom even after treatment ends. Persistent cancer-related fatigue affects quality of life, because individuals become too tired to fully participate in the roles and activities that make life meaningful. Identification and management of fatigue remains an unmet need for many cancer survivors. This section of the NCCN Guidelines for Survivorship provides screening, evaluation, and management recommendations for fatigue in survivors. Management includes education and counseling, physical activity, psychosocial interventions, and pharmacologic treatments.
NCCN defines cancer-related fatigue as “a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning.”1 Fatigue is a common symptom in patients with cancer and is nearly universal in those receiving cytotoxic chemotherapy, radiation therapy, bone marrow transplantation, or treatment with biological response modifiers.2–4 According to a survey of 1569 patients with cancer, the symptom is experienced by 80% of individuals who receive chemotherapy and/or radiotherapy.5,6 Cancer survivors report that fatigue continues to be a disruptive symptom after treatment ends,7–14 with studies showing that 17% to 29% of cancer survivors experience persistent fatigue for years after the completion of active therapy.15,16 Persistent cancer-related fatigue affects quality of life, because individuals become too tired to fully participate in the roles and activities that make life meaningful.9,17 Disability-related issues are also relevant for cancer survivors, because obtaining or retaining disability benefits from insurers is often difficult for patients with cancer-related fatigue. Identification and management of fatigue remains an unmet need for many cancer survivors.
The specific mechanisms involved in the pathophysiology of cancer-related fatigue are unknown. Proposed mechanisms include proinflammatory cytokines, hypothalamic-pituitary-adrenal axis dysregulation, circadian rhythm desynchronization, skeletal muscle wasting, and genetic dysregulation.18–23 Several studies have focused on the cause of fatigue, especially in cancer survivors with no evidence of active disease, and have suggested that persistent immune system activation and chronic inflammatory processes may be involved.7,24–26 Evidence supporting these mechanisms is limited.

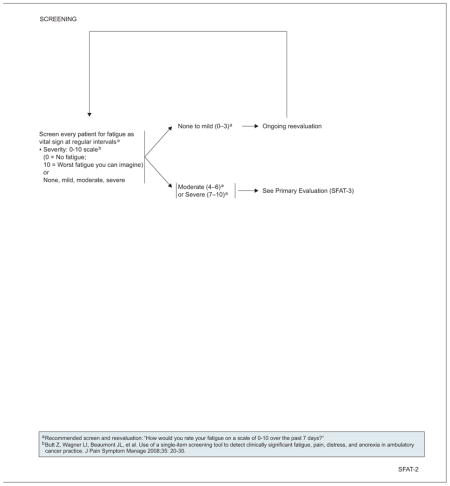



Screening for Fatigue
All survivors should be screened for fatigue to ensure that those with moderate to severe fatigue are identified and treated promptly and effectively. Because fatigue is a subjective experience, clinicians must rely on patients’ descriptions of their fatigue level. The panel recommends the use of a severity scale, with survivors being asked, “How would you rate your fatigue on a scale of 0 to 10 over the past 7 days?” Alternately, screening can be performed with patients asked to rate their fatigue as none, mild, moderate, or severe. Scores of 0 to 3 or none to mild fatigue require no further assessment or interventions; these patients should be rescreened at regular intervals. Patients with scores of 4 or greater or indicating moderate or severe fatigue should be evaluated further. Studies in patients with cancer have revealed a marked decrease in physical functioning at a reported fatigue level of 7 or higher on the 0 to 10 scale.27,28
Evaluation for Moderate to Severe Fatigue
When fatigue is rated as moderate to severe, with a score of 4 to 10, a more focused history and physical examination should be conducted. A thorough history is warranted, because the recommended workup for fatigue differs according to the timing of fatigue onset in relation to the completion of active therapy and the presence of predisposing factors and other symptoms. Fatigue has a variable natural history, with some patients complaining of only mild levels of fatigue even during active therapy and others experiencing severe fatigue for years after treatment completion.
In general, mild to moderate levels of fatigue that persist for 6 to 12 months after the completion of therapy likely do not warrant an extensive work-up, unless other symptoms are present. Conversely, when moderate to severe fatigue begins after or worsens during this period, or when other symptoms are present, such as pain, pulmonary complaints, or unintentional weight loss, a more extensive workup is warranted to screen for the presence of metastatic disease or other comorbidities.
Regardless of fatigue onset, it is always relevant to screen for common contributing factors, such as emotional distress, sleep disturbance, pain, and the use of prescriptions or over-the-counter medications or supplements. Possible medical causes of fatigue, including cardiac disease and hypothyroidism, should also be assessed. Disease and treatment considerations also affect recommendations for screening, such as the inclusion of echocardiograms for patients who received cardiotoxic treatments, and thyroid screening for patients who received radiation to the neck or thorax.
Management of Fatigue
Several interventions and strategies have been shown to help alleviate fatigue and reduce distress caused by this symptom in patients with cancer and survivors; recommended strategies and interventions are described herein. For additional information about fatigue in survivors and patients with cancer, please see the NCCN Guidelines for Cancer-Related Fatigue (to view the most recent version of these guidelines, visit NCCN.org). The following guidelines may be modified to fit the individual survivor’s circumstances.
Treatment of Contributing Factors
Management of fatigue in survivors first includes the treatment of contributing factors, such as pain, distress, anemia, and sleep disturbances (more information on treatment of pain, anxiety/depression, and sleep disorders in survivors can be found throughout the full version of these guidelines, available online at NCCN.org).
Patient and Family Education and Counseling
Education and counseling can be beneficial in helping patients cope with fatigue. Understanding typical patterns of fatigue during and after treatment can help patients set reasonable expectations regarding improvements in energy after the completion of cancer therapy and can help allay concerns that persistent fatigue after the completion of therapy is evidence of disease recurrence. Counseling can help patients develop strategies for self-monitoring of fatigue and techniques, such as energy conservation, that may be helpful in the immediate post-treatment period.29
Physical Activity
Activity enhancement is a category 1 recommendation. Improving strength, energy, and fitness through regular exercise, even a moderate walking exercise program, has been shown to facilitate the transition from patient to survivor, decrease anxiety and depression, improve body image, and increase tolerance for physical activity. Therefore, survivors with moderate to severe fatigue should be encouraged to maintain adequate levels of physical activity (category 1). Robust data support the efficacy of increased physical activity for reducing fatigue in patients with cancer and survivors.30–36 A recent meta-analysis of randomized controlled trials found that cancer survivors who participated in exercise interventions, either during or after treatment for cancer, experienced significant improvements in fatigue compared with patients randomized to the control group.37 Another meta-analysis of 44 studies, including 3254 cancer survivors, concluded that moderate-intensity resistance exercise among older cancer survivors reduced fatigue.30
Survivors at a higher risk of injury should be referred to a physical therapist or exercise specialist (also see “Physical Activity,” page 882).
Psychosocial Interventions
Psychosocial interventions, such as cognitive behavioral therapy (CBT), psychoeducational therapy, and supportive expressive therapy, including support groups, counseling, and journal writing (all category 1 recommendations), have also been shown to reduce fatigue in cancer survivors, although data are not entirely consistent.38–43 Several meta-analyses have evaluated the role of psychosocial interventions in reducing fatigue. For example, Kangas et al42 reported a weighted pooled mean effect of –0.31 for psychosocial interventions on fatigue in an analysis of 3620 patients with cancer from 41 studies. Jacobsen et al44 analyzed 30 randomized controlled trials and found a significant effect size (dw) for psychological interventions (dw, 0.10; 95% CI, 0.02–0.18), but not for activity-based programs (dw, 0.05; 95% CI, −0.08–0.19). A meta-analysis by Duijts et al38 reported that, like exercise programs, behavioral techniques, including cognitive therapy, relaxation techniques, counseling, social support, hypnosis, and biofeedback, are beneficial in improving fatigue among patients with breast cancer during and after treatment (standardized mean difference [SMD], –0.16).
Several published studies support the conclusion that CBT interventions designed to optimize sleep quality in patients with cancer may also improve fatigue.45–49 Two randomized clinical trials of patients who reported chronic insomnia in the survivorship phase demonstrated improvements in both sleep and fatigue after 4 to 5 weekly behavioral therapy sessions.39,40,49 Two smaller studies of patients with current complaints of insomnia in the survivorship phase reported improved sleep and fatigue.45,47 Two other studies found positive benefits of a behavioral intervention on sleep and fatigue that were not sustained over time.48,50 The American Academy of Sleep Medicine has recommended 3 specific therapies for chronic insomnia in healthy individuals: relaxation training, cognitive behavior therapy, and stimulus control therapy.51
Pharmacologic Interventions
Psychostimulants, such as methylphenidate and modafinil, are also used to treat fatigue, although data regarding their use to treat fatigue in cancer survivors are limited. A 54% response rate to methylphenidate was reported in a phase II trial of 37 breast cancer survivors.52 A randomized trial in 154 patients postchemotherapy also found an improvement in fatigue symptoms in the dexmethylphenidate arm.53 A recent meta-analysis of 5 randomized controlled trials of patients with cancer found limited evidence for the efficacy of 4 or more weeks of methylphenidate treatment for cancer-related fatigue (mean difference, –3.70; 95% CI, –7.03 to –0.37; P=.03).54
Modafinil also shows some promise for management of posttreatment fatigue in small trials. Morrow et al55 conducted an open-label study of modafinil for 51 breast cancer survivors with persistent fatigue. The dose was 200 mg/d for 1 month. A reduction in fatigue was reported among 86% of these survivors. In a pilot study of 30 adults with previously treated brain tumors, modafinil was associated with improvement in fatigue by 8 weeks.56 Currently, the panel agrees that methylphenidate or modafinil may be considered after ruling out other causes of fatigue, although they acknowledge the limited data supporting the use of these agents in this setting.
Small pilot studies and one recent randomized controlled trial have evaluated the impact of supplements, including ginseng and vitamin D, for cancer-related fatigue.57 The evidence to date is inconsistent, and the panel currently does not recommend the use of supplements for the treatment of fatigue.
NCCN Survivorship Panel Members
*,a,cCrystal S. Denlinger, MD/Chair†
Fox Chase Cancer Center
*,c,dJennifer A. Ligibel, MD/Vice Chair†
Dana-Farber/Brigham and Women’s Cancer Center
fMadhuri Are, MD£
Fred & Pamela Buffett Cancer Center at The Nebraska Medical Center
b,eK. Scott Baker, MD, MS€ξ
Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance
cWendy Demark-Wahnefried, PhD, RD≅
University of Alabama at Birmingham Comprehensive Cancer Center
b,dDebra L. Friedman, MD, MS€‡
Vanderbilt-Ingram Cancer Center
*,gMindy Goldman, MDΩ
UCSF Helen Diller Family Comprehensive Cancer Center
c,dLee Jones, PhDΠ
Memorial Sloan-Kettering Cancer Center
bAllison King, MD€Ψ‡
Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine
Grace H. Ku, MDξ‡
UC San Diego Moores Cancer Center
b,hElizabeth Kvale, MD£
University of Alabama at Birmingham Comprehensive Cancer Center
aTerry S. Langbaum, MAS¥
The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins
gKristin Leonardi-Warren, RN, ND#
University of Colorado Cancer Center
bMary S. McCabe, RN, BS, MS#
Memorial Sloan-Kettering Cancer Center
b,c,d,gMichelle Melisko, MD†
UCSF Helen Diller Family Comprehensive Cancer Center
eJose G. Montoya, MDΦ
Stanford Cancer Institute
a,dKathi Mooney, RN, PhD#
Huntsman Cancer Institute at the University of Utah
c,eMary Ann Morgan, PhD, FNP-BC#
Moffitt Cancer Center
Javid J. Moslehi, MD Þ
Dana-Farber/Brigham and Women’s Cancer Center
d,hTracey O’Connor, MD†
Roswell Park Cancer Institute
cLinda Overholser, MD, MPHÞ
University of Colorado Cancer Center
cElectra D. Paskett, PhDε
The Ohio State University Comprehensive Cancer Center -James Cancer Hospital and Solove Research Institute
f,hMuhammad Raza, MD‡
St. Jude Children’s Research Hospital/The University of Tennessee Health Science Center
fKaren L. Syrjala, PhDθ
Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance
*,fSusan G. Urba, MD†£
University of Michigan Comprehensive Cancer Center
gMark T. Wakabayashi, MD, MPHΩ
City of Hope Comprehensive Cancer Center
*,hPhyllis Zee, MDΨΠ
Robert H. Lurie Comprehensive Cancer Center of Northwestern University
NCCN Staff: Nicole McMillian, MS, and Deborah Freedman-Cass, PhD
KEY
*Writing Committee Member Subcommittees:
aAnxiety and Depression; bCognitive Function; cExercise; dFatigue; eImmunizations and Infections; fPain; gSexual Function; hSleep Disorders
Specialties: ξBone Marrow Transplantation; Cardiology; εEpidemiology; ΠExercise/Physiology; ΩGynecology/Gynecologic Oncology; ‡Hematology/Hematology Oncology; ΦInfectious Diseases; ÞInternal Medicine; †Medical Oncology; ΨNeurology/Neuro-Oncology; #Nursing; ; ≅Nutrition Science/Dietician; ¥Patient Advocacy; €Pediatric Oncology; θPsychiatry, Psychology, Including Health Behavior; £Supportive Care Including Palliative, Pain Management, Pastoral Care, and Oncology Social Work
Footnotes
NCCN Categories of Evidence and Consensus
Category 1: Based upon high-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2A: Based upon lower-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2B: Based upon lower-level evidence, there is NCCN consensus that the intervention is appropriate.
Category 3: Based upon any level of evidence, there is major NCCN disagreement that the intervention is appropriate.
All recommendations are category 2A unless otherwise noted.
Clinical trials: NCCN believes that the best management for any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged.
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) are a statement of consensus of the authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult the NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The National Comprehensive Cancer Network® (NCCN®) makes no representation or warranties of any kind regarding their content, use, or application and disclaims any responsibility for their applications or use in any way. The full NCCN Guidelines for Survivorship are not printed in this issue of JNCCN but can be accessed online at NCCN.org.
© National Comprehensive Cancer Network, Inc. 2014, All rights reserved. The NCCN Guidelines and the illustrations herein may not be reproduced in any form without the express written permission of NCCN.
Disclosures for the NCCN Survivorship Panel
At the beginning of each NCCN Guidelines panel meeting, panel members review all potential conflicts of interest. NCCN, in keeping with its commitment to public transparency, publishes these disclosures for panel members, staff, and NCCN itself.
Individual disclosures for the NCCN Survivorship Panel members can be found on page 887. (The most recent version of these guidelines and accompanying disclosures are available on the NCCN Web site at NCCN.org.)
These guidelines are also available on the Internet. For the latest update, visit NCCN.org.
| Panel Member | Clinical Research Support/Data Safety Monitoring Board | Advisory Boards, Speakers Bureau, Expert Witness, or Consultant | Patent, Equity, or Royalty | Other | Date Completed |
|---|---|---|---|---|---|
| Madhuri Are, MD | None | None | None | None | 5/15/13 |
| K. Scott Baker, MD, MS | None | None | None | None | 11/22/13 |
| Wendy Demark-Wahnefried, PhD, RD | National Cancer Institute; Harvest for Health Gardening Project for Breast Cancer Survivors; and Nutrigenomic Link between Alpha-Linolenic Acid and Aggressive Prostate Cancer | American Society of Clinical Oncology | None | American Society of Preventive Oncology | 11/13/13 |
| Crystal S. Denlinger, MD | Bayer HealthCare; ImClone Systems Incorporated; MedImmune Inc.; OncoMed Pharmaceuticals; Astex Pharmaceuticals; Merrimack Pharmaceuticals; and Pfizer Inc. | Eli Lilly and Company | None | None | 1/9/14 |
| Debra L. Friedman, MD, MS | None | None | None | None | 5/26/13 |
| Mindy Goldman, MD | Pending | ||||
| Lee W. Jones, PhD | None | None | None | None | 2/2/12 |
| Allison King, MD | None | None | None | None | 8/12/13 |
| Grace H. Ku, MD | None | None | None | None | 8/13/13 |
| Elizabeth Kvale, MD | None | None | None | None | 10/7/13 |
| Terry S. Langbaum, MAS | None | None | None | None | 8/13/13 |
| Kristin Leonardi-Warren, RN, ND | None | None | None | None | 1/6/14 |
| Jennifer A. Ligibel, MD | None | None | None | None | 10/3/13 |
| Mary S. McCabe, RN, BS, MS | None | None | None | None | 8/12/13 |
| Michelle Melisko, MD | Celldex Therapeutics; and Galena Biopharma | Agendia BV; Genentech, Inc.; and Novartis Pharmaceuticals Corporation | None | None | 10/11/13 |
| Jose G. Montoya, MD | None | None | None | None | 12/6/13 |
| Kathi Mooney, RN, PhD | University of Utah | None | None | None | 9/30/13 |
| Mary Ann Morgan, PhD, FNP-BC | None | None | None | None | 8/19/13 |
| Javid J. Moslehi, MD | None | ARIAD Pharmaceuticals, Inc.; Millennium Pharmaceuticals, Inc.; Novartis Pharmaceuticals Corporation; and Pfizer Inc. | None | None | 1/27/14 |
| Tracey O’Connor, MD | None | None | None | None | 6/13/13 |
| Linda Overholser, MD, MPH | None | Antigenics Inc.; and Colorado Central Cancer Registry Care Plan Project | None | None | 10/10/13 |
| Electra D. Paskett, PhD | Merck & Co., Inc. | None | None | None | 6/13/13 |
| Muhammad Raza, MD | None | None | None | None | 8/23/12 |
| Karen L. Syrjala, PhD | None | None | None | None | 10/3/13 |
| Susan G. Urba, MD | None | Eisai Inc.; and Helsinn Therapeutics (U.S.), Inc. | None | None | 10/9/13 |
| Mark T. Wakabayashi, MD, MPH | None | None | None | None | 6/19/13 |
| Phyllis Zee, MD | Philips/Respironics | Merck & Co., Inc.; Jazz Pharmaceuticals; Vanda Pharmaceuticals; and Purdue Pharma LP | None | None | 3/26/14 |
References
- 1.Berger AM, Abernethy AP, Atkinson A, et al. NCCN Clinical Practice Guidelines in Oncology for cancer-related fatigue. J Natl Compr Canc Netw. 2010;8:904–931. doi: 10.6004/jnccn.2010.0067. [DOI] [PubMed] [Google Scholar]
- 2.Ahlberg K, Ekman T, Gaston-Johansson F, Mock V. Assessment and management of cancer-related fatigue in adults. Lancet. 2003;362:640–650. doi: 10.1016/S0140-6736(03)14186-4. [DOI] [PubMed] [Google Scholar]
- 3.Collins JJ, Devine TD, Dick GS, et al. The measurement of symptoms in young children with cancer: the validation of the Memorial Symptom Assessment Scale in children aged 7–12. J Pain Symptom Manage. 2002;23:10–16. doi: 10.1016/s0885-3924(01)00375-x. [DOI] [PubMed] [Google Scholar]
- 4.Wagner LI, Cella D. Fatigue and cancer: causes, prevalence and treatment approaches. Br J Cancer. 2004;91:822–828. doi: 10.1038/sj.bjc.6602012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henry DH, Viswanathan HN, Elkin EP, et al. Symptoms and treatment burden associated with cancer treatment: results from a cross-sectional national survey in the US Support Care. Cancer. 2008;16:791–801. doi: 10.1007/s00520-007-0380-2. [DOI] [PubMed] [Google Scholar]
- 6.Hofman M, Ryan JL, Figueroa-Moseley CD, et al. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;12(Suppl 1):4–10. doi: 10.1634/theoncologist.12-S1-4. [DOI] [PubMed] [Google Scholar]
- 7.Bower JE, Ganz PA, Aziz N, et al. T-cell homeostasis in breast cancer survivors with persistent fatigue. J Natl Cancer Inst. 2003;95:1165–1168. doi: 10.1093/jnci/djg0019. [DOI] [PubMed] [Google Scholar]
- 8.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743–753. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 9.Crom DB, Hinds PS, Gattuso JS, et al. Creating the basis for a breast health program for female survivors of Hodgkin disease using a participatory research approach. Oncol Nurs Forum. 2005;32:1131–1141. doi: 10.1188/05.ONF.1131-1141. [DOI] [PubMed] [Google Scholar]
- 10.Fossa SD, Dahl AA, Loge JH. Fatigue, anxiety, and depression in long-term survivors of testicular cancer. J Clin Oncol. 2003;21:1249–1254. doi: 10.1200/JCO.2003.08.163. [DOI] [PubMed] [Google Scholar]
- 11.Haghighat S, Akbari ME, Holakouei K, et al. Factors predicting fatigue in breast cancer patients. Support Care Cancer. 2003;11:533–538. doi: 10.1007/s00520-003-0473-5. [DOI] [PubMed] [Google Scholar]
- 12.Ruffer JU, Flechtner H, Tralls P, et al. Fatigue in long-term survivors of Hodgkin’s lymphoma; a report from the German Hodgkin Lymphoma Study Group (GHSG) Eur J Cancer. 2003;39:2179–2186. doi: 10.1016/s0959-8049(03)00545-8. [DOI] [PubMed] [Google Scholar]
- 13.Servaes P, Verhagen S, Bleijenberg G. Determinants of chronic fatigue in disease-free breast cancer patients: a cross-sectional study. Ann Oncol. 2002;13:589–598. doi: 10.1093/annonc/mdf082. [DOI] [PubMed] [Google Scholar]
- 14.Servaes P, Verhagen S, Schreuder HW, et al. Fatigue after treatment for malignant and benign bone and soft tissue tumors. J Pain Symptom Manage. 2003;26:1113–1122. doi: 10.1016/j.jpainsymman.2003.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 16.Wang XS, Zhao F, Fisch MJ, et al. Prevalence and characteristics of moderate to severe fatigue: A multicenter study in cancer patients and survivors. Cancer. 2014;120:425–432. doi: 10.1002/cncr.28434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janda M, Gerstner N, Obermair A, et al. Quality of life changes during conformal radiation therapy for prostate carcinoma. Cancer. 2000;89:1322–1328. doi: 10.1002/1097-0142(20000915)89:6<1322::aid-cncr18>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 18.al-Majid S, McCarthy DO. Cancer-induced fatigue and skeletal muscle wasting: the role of exercise. Biol Res Nurs. 2001;2:186–197. doi: 10.1177/109980040100200304. [DOI] [PubMed] [Google Scholar]
- 19.Berger AM, Wielgus K, Hertzog M, et al. Patterns of circadian activity rhythms and their relationships with fatigue and anxiety/depression in women treated with breast cancer adjuvant chemotherapy. Support Care Cancer. 2009;18:105–114. doi: 10.1007/s00520-009-0636-0. [DOI] [PubMed] [Google Scholar]
- 20.Bower JE. Cancer-related fatigue: links with inflammation in cancer patients and survivors. Brain Behav Immun. 2007;21:863–871. doi: 10.1016/j.bbi.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller AH, Ancoli-Israel S, Bower JE, et al. Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol. 2008;26:971–982. doi: 10.1200/JCO.2007.10.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rich TA. Symptom clusters in cancer patients and their relation to EGFR ligand modulation of the circadian axis. J Support Oncol. 2007;5:167–174. discussion 176–167. [PubMed] [Google Scholar]
- 23.Schubert C, Hong S, Natarajan L, et al. The association between fatigue and inflammatory marker levels in cancer patients: a quantitative review. Brain Behav Immun. 2007;21:413–427. doi: 10.1016/j.bbi.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 24.Alfano CM, Imayama I, Neuhouser ML, et al. Fatigue, inflammation, and omega-3 and omega-6 fatty acid intake among breast cancer survivors. J Clin Oncol. 2012;30:1280–1287. doi: 10.1200/JCO.2011.36.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bower JE, Ganz PA, Irwin MR, et al. Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29:3517–3522. doi: 10.1200/JCO.2011.36.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bower JE, Ganz PA, Aziz N, Fahey JL. Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med. 2002;64:604–611. doi: 10.1097/00006842-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Mendoza TR, Wang XS, Cleeland CS, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 28.Piper BF, Dodd MJ, Ream E. Better health through nursing research: international state of the science. Vol. 99. Washington, DC: American Nurses Association; 1999. Improving the clinical measurement of cancer treatment-related fatigue. [Google Scholar]
- 29.Barsevick AM, Dudley W, Beck S, et al. A randomized clinical trial of energy conservation for patients with cancer-related fatigue. Cancer. 2004;100:1302–1310. doi: 10.1002/cncr.20111. [DOI] [PubMed] [Google Scholar]
- 30.Brown JC, Huedo-Medina TB, Pescatello LS, et al. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2011;20:123–133. doi: 10.1158/1055-9965.EPI-10-0988. [DOI] [PubMed] [Google Scholar]
- 31.Courneya KS, Mackey JR, Bell GJ, et al. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol. 2003;21:1660–1668. doi: 10.1200/JCO.2003.04.093. [DOI] [PubMed] [Google Scholar]
- 32.Mishra SI, Scherer RW, Geigle PM, et al. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;8:CD007566. doi: 10.1002/14651858.CD007566.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McMillan EM, Newhouse IJ. Exercise is an effective treatment modality for reducing cancer-related fatigue and improving physical capacity in cancer patients and survivors: a meta-analysis. Appl Physiol Nutr Metab. 2011;36:892–903. doi: 10.1139/h11-082. [DOI] [PubMed] [Google Scholar]
- 34.McNeely ML, Campbell KL, Rowe BH, et al. Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. CMAJ. 2006;175:34–41. doi: 10.1503/cmaj.051073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McNeely ML, Courneya KS. Exercise programs for cancer-related fatigue: evidence and clinical guidelines. J Natl Compr Canc Netw. 2010;8:945–953. doi: 10.6004/jnccn.2010.0069. [DOI] [PubMed] [Google Scholar]
- 36.Speck RM, Courneya KS, Masse LC, et al. An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2010;4:87–100. doi: 10.1007/s11764-009-0110-5. [DOI] [PubMed] [Google Scholar]
- 37.Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11:CD006145. doi: 10.1002/14651858.CD006145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duijts SF, Faber MM, Oldenburg HS, et al. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors: a meta-analysis. Psychooncology. 2011;20:115–126. doi: 10.1002/pon.1728. [DOI] [PubMed] [Google Scholar]
- 39.Espie CA, Fleming L, Cassidy J, et al. Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J Clin Oncol. 2008;26:4651–4658. doi: 10.1200/JCO.2007.13.9006. [DOI] [PubMed] [Google Scholar]
- 40.Epstein DR, Dirksen SR. Randomized trial of a cognitive-behavioral intervention for insomnia in breast cancer survivors. Oncol Nurs Forum. 2007;34:E51–59. doi: 10.1188/07.ONF.E51-E59. [DOI] [PubMed] [Google Scholar]
- 41.Gielissen MFM, Verhagen S, Witjes F, Bleijenberg G. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24:4882–4887. doi: 10.1200/JCO.2006.06.8270. [DOI] [PubMed] [Google Scholar]
- 42.Kangas M, Bovbjerg DH, Montgomery GH. Cancer-related fatigue: a systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychol Bull. 2008;134:700–741. doi: 10.1037/a0012825. [DOI] [PubMed] [Google Scholar]
- 43.Mustian KM, Morrow GR, Carroll JK, et al. Integrative nonpharmacologic behavioral interventions for the management of cancer-related fatigue. Oncologist. 2007;12(Suppl 1):52–67. doi: 10.1634/theoncologist.12-S1-52. [DOI] [PubMed] [Google Scholar]
- 44.Jacobsen PB, Donovan KA, Vadaparampil ST, Small BJ. Systematic review and meta-analysis of psychological and activity-based interventions for cancer-related fatigue. Health Psychol. 2007;26:660–667. doi: 10.1037/0278-6133.26.6.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davidson JR, Waisberg JL, Brundage MD, MacLean AW. Nonpharmacologic group treatment of insomnia: a preliminary study with cancer survivors. Psychooncology. 2001;10:389–397. doi: 10.1002/pon.525. [DOI] [PubMed] [Google Scholar]
- 46.Fleming L, Randell K, Harvey CJ, Espie CA. Does cognitive behaviour therapy for insomnia reduce clinical levels of fatigue, anxiety and depression in cancer patients? Psychooncology. doi: 10.1002/pon.3468. published online ahead of print January 23, 2014. [DOI] [PubMed] [Google Scholar]
- 47.Quesnel C, Savard J, Simard S, et al. Efficacy of cognitive-behavioral therapy for insomnia in women treated for nonmetastatic breast cancer. J Consult Clin Psychol. 2003;71:189–200. [PubMed] [Google Scholar]
- 48.Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: sleep and psychological effects. J Clin Oncol. 2005;23:6083–6096. doi: 10.1200/JCO.2005.09.548. [DOI] [PubMed] [Google Scholar]
- 49.Dirksen SR, Epstein DR. Efficacy of an insomnia intervention on fatigue, mood and quality of life in breast cancer survivors. J Adv Nurs. 2008;61:664–675. doi: 10.1111/j.1365-2648.2007.04560.x. [DOI] [PubMed] [Google Scholar]
- 50.Berger AM, VonEssen S, Khun BR, et al. Feasibilty of a sleep intervention during adjuvant breast cancer chemotherapy. Oncol Nurs Forum. 2002;29:1431–1441. doi: 10.1188/02.ONF.1431-1441. [DOI] [PubMed] [Google Scholar]
- 51.Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29:1415–1419. [PubMed] [Google Scholar]
- 52.Hanna A, Sledge G, Mayer ML, et al. A phase II study of methylphenidate for the treatment of fatigue. Support Care Cancer. 2006;14:210–215. doi: 10.1007/s00520-005-0857-9. [DOI] [PubMed] [Google Scholar]
- 53.Lower EE, Fleishman S, Cooper A, et al. Efficacy of dexmethylphenidate for the treatment of fatigue after cancer chemotherapy: a randomized clinical trial. J Pain Symptom Manage. 2009;38:650–662. doi: 10.1016/j.jpainsymman.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 54.Gong S, Sheng P, Jin H, et al. Effect of methylphenidate in patients with cancer-related fatigue: a systematic review and meta-analysis. PLoS One. 2014;9:e84391. doi: 10.1371/journal.pone.0084391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morrow GR, Gillies LJ, Hickok JT, et al. The positive effect of the psychostimulant modafinil on fatigue from cancer that persists after treatment is completed [abstract] J Clin Oncol. 2005;23(Suppl 16):Abstract 8012. [Google Scholar]
- 56.Kaleita TA, Wellisch DK, Graham CA, et al. Pilot study of modafinil for treatment of neurobehavioral dysfunction and fatigue in adult patients with brain tumors [abstract] J Clin Oncol. 2006;24(Suppl 18):Abstract 1503. [Google Scholar]
- 57.Barton DL, Liu H, Dakhil SR, et al. Wisconsin Ginseng (Panax quinquefolius) to improve cancer-related fatigue: a randomized, double-blind trial, N07C2. J Natl Cancer Inst. 2013;105:1230–1238. doi: 10.1093/jnci/djt181. [DOI] [PMC free article] [PubMed] [Google Scholar]


