Abstract
BACKGROUND
Nursing home residents’ use of hospice has substantially increased. Whether this increase in hospice use reduces end-of-life expenditures is unknown.
METHODS
The expansion of hospice between 2004 and 2009 created a natural experiment, allowing us to conduct a difference-in-differences matched analysis to examine changes in Medicare expenditures in the last year of life that were associated with this expansion. We also assessed intensive care unit (ICU) use in the last 30 days of life and, for patients with advanced dementia, feeding-tube use and hospital transfers within the last 90 days of life. We compared a subset of hospice users from 2009, whose use of hospice was attributed to hospice expansion, with a matched subset of non–hospice users from 2004, who were considered likely to have used hospice had they died in 2009.
RESULTS
Of 786,328 nursing home decedents, 27.6% in 2004 and 39.8% in 2009 elected to use hospice. The 2004 and 2009 matched hospice and nonhospice cohorts were similar (mean age, 85 years; 35% male; 25% with cancer). The increase in hospice use was associated with significant decreases in the rates of hospital transfers (2.4 percentage-point reduction), feeding-tube use (1.2 percentage-point reduction), and ICU use (7.1 percentage-point reduction). The mean length of stay in hospice increased from 72.1 days in 2004 to 92.6 days in 2009. Between 2004 and 2009, the expansion of hospice was associated with a mean net increase in Medicare expenditures of $6,761 (95% confidence interval, 6,335 to 7,186), reflecting greater additional spending on hospice care ($10,191) than reduced spending on hospital and other care ($3,430).
CONCLUSIONS
The growth in hospice care for nursing home residents was associated with less aggressive care near death but at an overall increase in Medicare expenditures. (Funded by the Centers for Medicare and Medicaid Services and the National Institute on Aging.)
Medicare expenditures for beneficiaries in their last year of life account for a quarter of the annual payments made by Medicare.1 From its inception, hospice has been viewed as respecting patients’ goals of care with no resulting increase — or even with a resulting decrease — in health care expenditures.2–4
Between 2000 and 2012, the percentage of Medicare decedents using hospice doubled (from 23% to 47%)5 and hospice expenditures quintupled (from $2.9 billion to about $15.1 billion),5 which raised budgetary concerns.6,7 This increase was particularly large among persons with non-cancer diagnoses and those residing in nursing homes.8 The Medicare Payment Advisory Commission and the Office of Inspector General have expressed concern about hospice providers that may be selectively enrolling nursing home residents with longer hospice stays and less complex care needs, thereby generating higher profit margins.6,7 It is unknown how growth in the number of hospice patients residing in nursing homes has affected health care expenditures.
The evidence regarding the relationship between hospice and health care savings is mixed,4,6,9–12 and most studies have had important methodologic limitations.9 An important limitation is that most observational studies are not able to control for differences in preferences for aggressive care. In the present study, we address this limitation in two ways. First, we use mandatory nursing home assessment data that provide a wealth of risk adjusters not available in most other studies, including proxies for patients’ preferences for aggressive care (do-not-resuscitate [DNR] and do-not-hospitalize [DNH] orders). Second, we capitalize on the natural experiment created by the rapid expansion of hospice in the nursing home setting by using a difference-in-differences matching approach. This approach provides better adjustment for confounders than has been used in previous studies.
METHODS
OVERVIEW AND STUDY POPULATION
An important concern with observational studies is that persons who elect and those who do not elect hospice have different preferences for aggressive care. This concern regarding selection bias and the lack of information on preferences is an important threat to the validity of earlier studies that matched hospice users to persons who contemporaneously die without hospice services.
Instead of using cross-sectional matching, we used a difference-in-differences cross-temporal matching design. We took advantage of the natural experiment created by the substantial increase in hospice use between 2004 and 2009 and compared a subset of hospice users in 2009, whose use of hospice was attributed to hospice expansion between 2004 and 2009, with a matched subset of nonusers in 2004, who were considered likely to have used hospice had they died in 2009.
We studied all 2004 (baseline period) and 2009 nursing home decedents who were 67 years of age or older at death and who had fee-for-service Medicare for the last 2 years of life. We did not include 828 persons (0.1%) whose last nursing home assessment was performed more than 120 days before death. Although the use of data from later years would have been desirable, the nursing home assessment changed in 2010; the new assessment is not comparable and is missing key information, such as DNR and DNH orders.
OUTCOMES
Medicare expenditures in the last year of life9 were based on inpatient, outpatient, postacute, home health, and hospice claims. In addition, carrier-file physician-visit claims for a random 20% sample were used. Expenditures for health care services starting before the last year of life but overlapping with the last year of life were prorated. All expenditures were inflation-adjusted to 2007 prices.13 We also examined claims-based measures that characterized the aggressiveness and quality of end-of-life care. For all patients, we examined admission to an intensive care unit (ICU) in the last 30 days of life. For patients with advanced dementia (those with dementia and a Cognitive Performance Scale [CPS] score of 4, 5, or 6), we examined feeding-tube use in the last 90 days of life and “burdensome transitions” (defined as more than two hospitalizations for any reason or more than one hospitalization for pneumonia, urinary tract infection, dehydration, or sepsis) in the last 90 days of life.14 The CPS score ranges from 0 (intact) to 6 (very severe impairment), with a score of 5 corresponding to a score of 5.1 on the Mini–Mental State Examination (range, 0 to 30; <24 indicates cognitive impairment).
OTHER VARIABLES
Our main independent variable was hospice use in the last year of life. Detailed demographic and clinical information was obtained from the Minimum Data Set (MDS), a comprehensive assessment federally mandated for Medicare and Medicaid–certified nursing homes. Our analyses adjusted for demographic characteristics (age at death, sex, race [white or nonwhite], and marital status), four diagnosis groups based on the MDS assessments and Medicare claims (cancer without dementia, cancer with dementia, dementia without cancer, and other), a list of clinical coexisting conditions, measures of physical and cognitive performance impairment (activities of daily living score and CPS score, respectively), DNR and DNH orders, indicators of long (>90 days) and very short (<30 days) nursing home stays before death, and time from the last MDS assessment to death. We also adjusted for the number and mean length of stay of hospitalizations in the year before the last year of life, to control for previous health care use patterns, which are known to predict use in the last year of life.15 Our models also controlled for nursing home facility characteristics, including proprietary status; whether it was hospital-based, was part of a chain, or had any special care units; and the percentage of patients whose primary payer was Medicaid, Medicare, or other (generally private pay). Facility data were obtained from the Online Survey Certification and Reporting (OSCAR) component of the Centers for Medicare and Medicaid Services Provider of Services file.16
STATISTICAL ANALYSIS
We created three well-defined matched groups of nursing home decedents in 2004 and 2009: those who used hospice services during both periods (traditional hospice users, who used hospice before and after the expansion of hospice use; group 1); those who used hospice in 2009 whose use was attributed to hospice expansion, matched to residents who did not use hospice in 2004 but were considered likely to have been users had they died in 2009 (new users, those expected to use hospice only in the context of expanded hospice use; group 2); and those who did not use hospice in 2009 matched with 2004 nonhospice residents (nonusers, group 3).
The difference-in-differences matching model was used to estimate the association between hospice use and outcomes by comparing changes over time for decedents in group 2 (new users) with changes over time for decedents in group 3 (nonusers). This approach adjusts for changes over time other than the change in hospice status. Group 1 (hospice users in both years) offers a basis for the assessment of the secular changes among hospice users over this period and is not used in the analysis in which the association between hospice and outcomes is examined.
To account for case-mix differences between the 2004 and 2009 cohorts, we first used propensity-score matching within each of the three groups to find decedents with similar characteristics. Next, we applied a difference-in-differences multivariable regression model based on the resulting matched decedents in groups 2 and 3, to adjust for the residual person and facility characteristics that remained after matching.
Figure 1 provides a schematic depiction of the matching procedures. First, the 2004 cohort was used to calculate the propensity for hospice election in 2004, p2004 (Fig. 1, step 1). The p2004 model was applied to the 2009 cohort to predict who would have elected hospice if they had died in 2004. Persons who used hospice in 2004 were matched one-to-one with replacement to 2009 hospice users to form the first group using hospice in both years (G12004 and G12009 in Fig. 1). The 2009 hospice patients who were left unmatched (G22009) form the basis of the second group of decedents new to hospice in 2009. The propensity score based on the 2009 cohort data, p2009, is used to find one-to-one matches with replacement for them (G22004) among 2004 non-hospice decedents who were likely to have elected hospice had they died in 2009, to complete our group of “new to hospice” decedents (Fig. 1, step 2). Because matching was done with replacement, some persons in 2004 were selected as matches for more than one person in 2009. Finally, the last comparison group of decedents that never used hospice was formed with the use of the 2009 propensity score, p2009, to match each nonhospice decedent in 2009 (G32009) to one nonhospice decedent in 2004 (G32004).
Figure 1. Overview of the Analytic Difference-in-Differences Cross- Temporal Matching Approach.
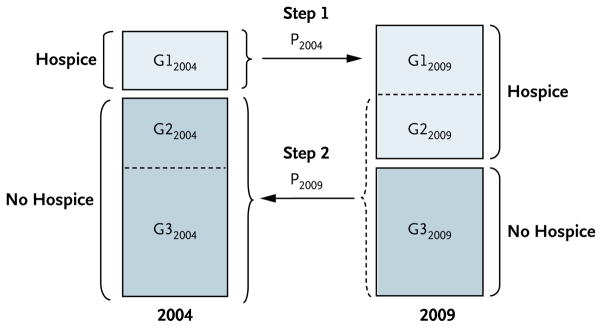
Step 1 forms group 1 of “traditional” hospice users: the propensity-score model of hospice election in 2004 (p2004) is used to match one-to-one with replacement each hospice user in 2004 (group G12004) to a hospice user in 2009 (group G12009); G12009 represents those most likely to have used hospice in 2004. In step 2, the propensity-score model of hospice election in 2009 (p2009) is used to form groups 2 and 3, used in the final analysis. Group 2 is formed from all the 2009 hospice users who remain unmatched in step 1 (G22009) and their matched (with replacement) 2004 nonhospice decedents (G22004). Similarly, group 3 consists of all the 2009 nonhospice decedents (G32009) and their matched (with replacement) 2004 nonhospice decedents (G32004). Note that because matching is done with replacement, some 2004 nonhospice decedents are not selected into G22004 or G32004 as best matches for those in G22009 or G32009 and are not used in our comparative analysis. Our difference-in-differences model calculates the effect of hospice use among new hospice users as the difference of the changes in outcomes over time for groups 2 and 3: (G22009 - G22004) − (G32009 - G32004).
The propensity-score models of hospice election were calculated with the use of multivariable logistic regression, with the patient and nursing home facility characteristics listed above as covariates. Covariate balance among matched groups was examined with standardized differences.17 The difference-in-differences models were estimated with the use of a least-squares regression for Medicare expenditures in the last year of life and a probability linear model for our clinical binary outcomes. These regressions included the same covariates as the propensity-score models to adjust for residual imbalances in our matching. We estimated robust standard errors adjusted for the clustering of persons within nursing home facilities.18 A Supplementary Appendix, available with the full text of this article at NEJM.org, contains additional details of the estimation process, the adequacy of the matching model, and sensitivity analyses.
RESULTS
CHARACTERISTICS OF THE NURSING HOME DECEDENTS AND MATCHED TREATMENT AND CONTROL GROUPS
The total number of Medicare fee-for-service beneficiaries we identified who were 67 years of age or older who died while they were nursing home residents was 786,328 (426,276 in 2004 and 360,052 in 2009). The mean age of the persons in our sample was 85 years, and 35% were male. Among the nursing home decedents in our total sample, 117,858 (27.6%) in 2004 and 143,394 (39.8%) in 2009 used hospice care. The mean length of stay in hospice increased from 72.1 days (median, 17; proportion of hospice users with a length of stay >6 months, 12.3%) in 2004 to 92.6 days (median, 21; proportion of hospice users with a length of stay >6 months, 16.7%) in 2009. Each year, approximately 15% of nursing home decedents had cancer, 46% had dementia without cancer, and 10% had both cancer and dementia. Among hospice users, these three rates changed from 18.6%, 46.6%, and 12.5%, respectively, in 2004 to 14.5%, 51.9%, and 12.4% in 2009, reflecting a reduction in the rate of cancer and a similar increase in the rate of dementia cases (Table S1 in the Supplementary Appendix).
Using our matching approach, we identified 71,003 hospice users (49.5%) in 2009 who were likely to have elected hospice in 2004 if they had died then (group G12009 in Fig. 1). The analytic comparison sample consisted of the remaining 2009 new hospice decedents (72,391 decedents, group G22009) and 2009 nonhospice decedents (216,658 decedents, group G32009) and their 2004 matches (groups G22004 and G32004 in Fig. 1). Decedent characteristics were very similar within matched groups, which indicated adequate covariate balance (Table 1). Among new hospice users and their 2004 nonhospice matched decedents (G22009 and G22004), the mean age at death was approximately 86 years, about one third were male, one quarter had a cancer diagnosis, close to 64% had Alzheimer’s disease or another form of dementia, and coexisting conditions like emphysema or chronic obstructive pulmonary disease, congestive heart failure, diabetes, and depression were common. Most of these hospice users (77%) had a DNR order, but DNH orders were uncommon (less than 10%). The largest differences were in the rates of diabetes (25.3% in 2004 vs. 29.4% in 2009) and depression (43.1% in 2004 vs. 48.4% in 2009). Nursing home decedents who did not use hospice in 2009 (group G32009) and their 2004 matches (group G32004) also shared similar characteristics, with the largest differences being in the rates of diabetes and depression.
Table 1.
Comparison of Nursing Home Decedents According to Matching Group.*
| Characteristic | Hospice Group (Group 2)† | Nonhospice Group (Group 3)† | ||||
|---|---|---|---|---|---|---|
| G22004 (N = 72,391) | G22009 (N = 72,391) | Standardized Difference‡ | G32004 (N = 216,658) | G32009 (N = 216,658) | Standardized Difference‡ | |
| Age at death (yr) | 85.9 | 86.0 | 1.2 | 85.2 | 85.4 | 2.1 |
|
| ||||||
| Male sex (%) | 30.9 | 32.0 | 2.4 | 36.0 | 37.4 | 2.9 |
|
| ||||||
| Nonwhite race (%) | 8.9 | 10.3 | 4.6 | 11.0 | 12.3 | 4.1 |
|
| ||||||
| Married (%) | 23.1 | 24.2 | 2.7 | 25.4 | 26.6 | 2.7 |
|
| ||||||
| Cancer and no dementia (%) | 13.7 | 14.2 | 2.1 | 13.4 | 13.7 | 1.0 |
|
| ||||||
| Cancer and dementia (%) | 11.2 | 12.2 | 3.2 | 7.9 | 8.3 | 1.5 |
|
| ||||||
| Dementia and no cancer (%) | 52.2 | 52.1 | −0.4 | 44.7 | 45.2 | 1.0 |
|
| ||||||
| No cancer and no dementia (%) | 22.9 | 21.5 | −3.5 | 34.0 | 32.8 | −2.7 |
|
| ||||||
| Emphysema or chronic obstructive pulmonary disease (%) | 30.5 | 32.2 | 3.6 | 35.1 | 36.3 | 2.5 |
|
| ||||||
| Congestive heart failure (%) | 46.6 | 44.5 | −3.6 | 52.6 | 50.9 | −3.5 |
|
| ||||||
| Diabetes (%) | 25.3 | 29.4 | 9.1 | 28.4 | 32.7 | 9.4 |
|
| ||||||
| Arteriosclerotic heart disease (%) | 15.4 | 15.6 | 0.7 | 16.1 | 16.9 | 2.0 |
|
| ||||||
| Peripheral vascular disease (%) | 13.0 | 13.4 | 1.1 | 13.5 | 13.9 | 1.2 |
|
| ||||||
| Cerebrovascular accident (%) | 22.5 | 19.7 | −7.0 | 22.3 | 19.5 | −7.0 |
|
| ||||||
| Depression (%) | 43.1 | 48.4 | 10.4 | 36.2 | 40.5 | 8.9 |
|
| ||||||
| Asthma (%) | 2.5 | 3.2 | 3.4 | 2.5 | 3.1 | 3.9 |
|
| ||||||
| Pneumonia (%) | 9.5 | 9.1 | −1.1 | 13.2 | 13.2 | −0.2 |
|
| ||||||
| Respiratory infection (%) | 3.9 | 3.2 | 3.5 | 4.3 | 3.7 | −3.1 |
|
| ||||||
| Septicemia (%) | 1.4 | 1.5 | 0.5 | 2.2 | 2.3 | 0.3 |
|
| ||||||
| CPS score§ | 3.66 | 3.45 | −11.4 | 3.29 | 3.09 | −10.8 |
|
| ||||||
| ADL score¶ | 22.0 | 21.8 | −2.9 | 21.1 | 21.1 | −0.5 |
|
| ||||||
| ADL score worsening since last MDS (%) | 27.3 | 25.8 | −2.9 | 16.4 | 14.5 | −5.3 |
|
| ||||||
| Do-not-hospitalize orders (%) | 8.1 | 9.2 | 4.1 | 6.5 | 7.4 | 3.8 |
|
| ||||||
| Do-not-resuscitate orders (%) | 77.0 | 77.4 | 0.8 | 66.9 | 66.4 | −1.1 |
|
| ||||||
| Nursing home stay <30 days (%) | 7.3 | 6.9 | −1.1 | 17.9 | 16.7 | −3.2 |
|
| ||||||
| Nursing home stay >90 days (%) | 80.5 | 80.3 | −1.3 | 64.0 | 64.3 | 0.7 |
|
| ||||||
| Time from last MDS to death (days) | 34.6 | 34.1 | −2.0 | 25.7 | 25.2 | −1.7 |
|
| ||||||
| No. of hospitalizations in the year before the year of death | 0.72 | 0.76 | 3.8 | 0.68 | 0.72 | 3.3 |
|
| ||||||
| Mean hospital length of stay (days) | 2.20 | 2.17 | −0.8 | 2.15 | 2.10 | −1.3 |
ADL denotes activities of daily living, CPS Cognitive Performance Scale, and MDS Minimum Data Set.
Group G22004 includes non–hospice users in 2004 considered likely to have used hospice if they had died in 2009. Group G22009 includes hospice users in 2009 considered likely not to have used hospice if they had died in 2004. Groups G32004 includes non–hospice users in 2004 who were considered likely to continue not to use hospice if they had died in 2009, and Group G32009 includes non–hospice users in 2009. Because matching was done with replacement, some persons in 2004 were selected as matches for more than one person in 2009. The number of unique persons in the two 2004 groups was 58,427 for the hospice group and 139,351 for the nonhospice group. The results in the table for the 2004 groups of matched persons are based on weighted individuals so that 2004 and 2009 have same matched sample size. See the Supplementary Appendix for further details.
Standardized differences are defined as 100 × (mean1 − mean0) ÷ [(variance1+ variance0) ÷ 2]1/2, where 1 is the 2009 subgroup and 0 is the (matched) 2004 subgroup. The range is from −100 to 100. Some studies have used a standardized difference of less than 10 percentage points (in absolute value) to indicate a negligible difference,19 but no precise agreement exists.17 For characteristics expressed as percentages, standardized differences are given as percentage points.
The CPS score ranges from 0 (intact) to 6 (very severe impairment), with a score of 5 corresponding to a score of 5.1 on the Mini–Mental State Examination (range, 0 to 30; <24 indicates cognitive impairment).
The ADL score ranges from 0 to 28, with higher values reflecting greater impairment in function.
END-OF-LIFE EXPENDITURES FOR THE MATCHED TREATMENT AND CONTROL GROUPS
Table 2 shows Medicare spending in the last year of life for decedents with or without hospice care. Nursing home decedents not electing hospice in 2009 saw a mean increase in expenditures of $3,143, as compared with a $9,906 increase among those electing hospice in 2009 (where increases are defined as relative to their matched 2004 non–hospice users), for a net adjusted increase of $6,761 (95% confidence interval [CI], 6,335 to 7,186). Analyses stratified according to diagnosis showed that patients with cancer and without dementia (14% of hospice group) had the smallest net increase, at $2,180 (95% CI, 826 to 3,534), whereas the hospice patients with dementia and without cancer (52% of the hospice group) had the largest net increase, at $8,592 (95% CI, 8,126 to 9,058). Decedents in for-profit nursing homes were slightly more likely to elect hospice (adjusted odds ratio, 1.20; 95% CI, 1.18 to 1.22) and had a net adjusted increase in expenditures of $3,461 (95% CI, 2,770 to 4,152) on average. A breakdown of total expenditures according to type of care highlights that although hospice election is indeed associated with some reduction in costs related to hospitalizations and other types of care ($3,430), the savings are lower than the cumulative costs of hospice care ($10,191) (Table 3).
Table 2.
Association of Hospice and Total Medicare Expenditures in the Last Year of Life and End-of-Life Care Outcomes.*
| Outcome | Hospice Group (Group 2) | Nonhospice Group (Group 3) | Unadjusted Difference in Differences (95% CI)† | Adjusted Difference in Differences‡ (95% CI) | ||
|---|---|---|---|---|---|---|
| G22004 | G22009 | G32004 | G32009 | |||
| All conditions combined§ | ||||||
|
| ||||||
| Mean total Medicare expenditures in the last year of life ($) | 30,636 | 40,542 | 36,745 | 39,888 | 6,763 (6,244 to 7,282) | 6,761 (6,335 to 7,186) |
|
| ||||||
| Any intensive care unit care in the last 30 days of life (%) | 14.2 | 13.1 | 21.3 | 27.2 | −7.0 (−7.4 to −6.5) | −7.1 (−7.5 to −6.6) |
|
| ||||||
| Decedents with advanced Alzheimer’s disease or other dementia¶ | ||||||
|
| ||||||
| Mean total Medicare expenditures in the last year of life ($) | 18,705 | 30,481 | 22,521 | 24,322 | 9,975 (9,243 to 10,706) | 9,717 (9,109 to 10,325) |
|
| ||||||
| Any feeding-tube insertions in the last 90 days of life (%) | 3.8 | 2.3 | 6.0 | 5.6 | −1.1 (−1.6 to −0.6) | −1.2 (−1.6 to −0.8) |
|
| ||||||
| Any multiple burdensome hospitalizations in the last 90 days of life||(%) | 8.0 | 6.5 | 11.0 | 11.7 | −2.2 (−2.9 to −1.5) | −2.4 (−3.0 to −1.8) |
All expenditures are in 2007 dollars. Differences in outcomes measured as percentages are expressed as percentage-point differences.
Values were calculated as the difference over time for the hospice group (group 2) minus the difference over time for the nonhospice control group (group 3): (G22009 - G22004) − (G32009 - G32004).
Adjustment was made for person and nursing home characteristics. Confidence intervals were adjusted for clustering of decedents within nursing home facilities.
For all conditions combined, 72,391 decedents were included in the hospice group, and 216,658 decedents were included in the nonhospice group. The unadjusted mean expenditures for groups not used in the comparisons were as follows: $40,241 for the 117,858 hospice decedents in 2004; $40,581 for the 117,858 (after weighting) 2009 hospice decedents matched to 2004 hospice decedents; and $36,844 for the 143,440 2004 nonhospice decedents left unmatched.
For advanced Alzheimer’s disease and other types of dementia, 22,735 decedents were included in the hospice group, and 51,267 decedents were included in the nonhospice group. Decedents with Alzheimer’s or other dementia who had a CPS score of 4, 5, or 6 are included. A CPS score of 5 (on a scale ranging from 0 [intact] to 6 [very severe impairment]) corresponds to a mean ± SD score of 5.1±5.3 on the Mini–Mental State Examination (on which a score below 24 indicates cognitive impairment).
Multiple burdensome hospitalizations was defined as more than two hospitalizations for any reason or more than one hospitalization for pneumonia, urinary tract infection, dehydration, or sepsis.14
Table 3.
Adjusted Net Difference in Mean Medicare Expenditures in the Last Year of Life among Hospice Patients According to Expenditure Type.*
| Expenditure Type | Hospice Group (Group 2) | Nonhospice Group (Group 3) | Net Difference† | ||
|---|---|---|---|---|---|
| G22004 | G22009 | G32004 | G32009 | ||
| dollars | |||||
|
| |||||
| Hospice | 0 | 10,191 | 0 | 0 | 10,191 |
|
| |||||
| Hospitalizations | 13,082 | 13,678 | 16,860 | 19,516 | −2,060 |
|
| |||||
| Skilled-nursing-facility care | 8,022 | 5,697 | 8,660 | 7,279 | −944 |
|
| |||||
| Physician visits or other Medicare part B expenses | 5,064 | 5,390 | 5,932 | 6,280 | −22 |
|
| |||||
| Other‡ | 4,469 | 5,586 | 5,293 | 6,814 | −404 |
|
| |||||
| Total | 30,637 | 40,542 | 36,745 | 39,889 | 6,761 |
All expenditures are in 2007 dollars.
Net differences are calculated as the difference in expenditures over time for the hospice group (group 2) minus the difference in expenditures over time for the nonhospice control group (group 3): (G22009 - G22004) − (G32009 - G32004).
Other expenditures include outpatient care (e.g., emergency department, observation days in a hospital), long-term acute care hospitalizations, psychiatric hospitalizations, inpatient rehabilitation facility post–acute care, and home health care.
CHANGES IN THE AGGRESSIVENESS OF END-OF-LIFE CARE
As compared with nursing home decedents who did not elect hospice, those who elected hospice in 2009 had a larger reduction (relative to their 2004 nonhospice matches) in their aggressive end-of-life care outcomes. Their rate of ICU admission in the last 30 days of life decreased by 1.1 percentage points, as compared with an increase of 5.9 percentage points for 2009 non–hospice users, for a net adjusted decrease of 7.1 percentage points (95% CI, 7.5 to 6.6). Similarly, among persons with advanced dementia, in the last 90 days of life, hospice users had modest net adjusted decreases in burdensome transitions of 2.4 percentage points (95% CI, 3.0 to 1.8) and decreases in feeding-tube insertions of 1.2 percentage points (95% CI, 1.6 to 0.8) (Table 2).
DISCUSSION
The landscape of hospice providers in the United States has changed, from small not-for-profit providers to increasingly for-profit hospice chains. The percentage of persons receiving hospice care in a nursing home tripled from 14% of Medicare decedents in 19998 to nearly 40% in 2009. Medicare pays a per-diem rate for routine hospice care, regardless of whether services are provided, which raises the policy concern that profit motives may be driving selective enrollment of nursing home residents without cancer, who have longer hospice lengths of stay.6,7 Recent regulations to address the growth of long hospice stays, such as the physician narrative implemented in 2009 or the face-to-face visit requirement implemented in 2011, have had a negligible effect.20 Using a difference-in-differences matching approach, we found that although hospice use was associated with a reduction in aggressive end-of-life care, it was also associated with a net increase of $6,761 in Medicare expenditures per decedent in the last year of life.
The higher level of expenditures has two primary explanations. First, an increased mean hospice length of stay led to additional Medicare expenditures. In our unmatched cohorts, the mean hospice length of stay increased from 72.1 days in 2004 to 92.6 days in 2009. This increase is largely due to the growth in the number of nursing home hospice residents without cancer (who have less accurate 6-month prognoses)21 from 16% of hospice admissions in 199022 to 68% in 2012, and 75% in nursing homes.5 Second, hospice savings arise through avoidance of hospitalizations and curative treatments. However, among 2004 nonhospice decedents, those considered likely to have elected hospice had they died in 2009 had lower end-of-life care expenditures than did those considered likely not to have used hospice had they died in 2009 ($30,636 vs. $36,745) (Table 2). These two reasons — longer hospice stays and low use among the non–hospice users most likely to elect hospice — make it hard to achieve any savings.
Previous research on the association between hospice and health care expenditures has provided mixed results and has had important limitations.9 At best, studies used cross-sectional matching approaches, relied primarily on claims-based risk factors,10,12 excluded beneficiaries with long hospice stays,4 or examined expenditures in the last month of life.11 By focusing on nursing home patients, our study addressed these limitations by including a rich array of potential confounders and accounting for selection bias with a new difference-in-differences cross-temporal matching model that controlled for time-invariant unmeasured differences between hospice and nonhospice groups. Furthermore, we examined the effect of hospice on expenditures in the last year of life from a population perspective, providing key policy information on whether the current use of hospice is cost-neutral. 9
There are certain limitations in the interpretation of this study. Our results, which are based on fee-for-service Medicare beneficiaries, may not be generalizable to nursing home residents with Medicare Advantage or to non–nursing home residents. However, Medicare Advantage nursing home decedents have characteristics similar to those of fee-for-service nursing home decedents (see Table S4 in the Supplementary Appendix). Also, our findings pertain to nursing home residents who started using hospice services in 2009. However, our findings were robust under sensitivity analyses involving nursing home facilities that had no hospice in 2004 (see Table S5 in the Supplementary Appendix). Finally, our analyses offer some measures of how hospice reduces the aggressiveness of care for dying patients, but it does not include other quality-of-care measures.23–25
Increasingly, hospice is provided in nursing homes. Our finding of an increased cost of $6,761 associated with hospice use per decedent needs to be considered in light of evidence that hospice improves the quality of care and that the decision to enter hospice services is consistent with the patient’s goals and wishes for care. Cost neutrality or savings was a policy goal of the Medicare hospice benefit at its onset. If we are to achieve this policy objective, hospice must be provided at the right time and for the right duration. Prognostication in patients without cancer is difficult. If patients improve, reconsideration of the goals of care and the appropriateness of continued hospice care is warranted. Our study raises important concerns regarding the efficiency of hospice services from a societal perspective, especially if the motivation for keeping persons on hospice services (at $159 per day in fiscal year 2015) is increasing profit margins and not improving patients’ quality of life. With the current payment policy based on a flat per-diem payment rate, and given the increase in long hospice stays, the Medicare hospice benefit may not achieve cost savings.
Supplementary Material
Acknowledgments
Supported by a subcontract from Abt Associates on a contract to the Centers for Medicare and Medicaid Services (Hospice Study and Report, HHSM-500-2005-000881) and by a grant from the National Institute on Aging (AG027296). None of the funding agencies had a role in the design, execution, or drafting steps of the study.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010;45:565–76. doi: 10.1111/j.1475-6773.2010.01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer PA, Lowy FH. Rationing, patient preferences, and cost of care at the end of life. Arch Intern Med. 1992;152:478–80. [PubMed] [Google Scholar]
- 3.Fries JF, Koop CE, Beadle CE, et al. Reducing health care costs by reducing the need and demand for medical services. N Engl J Med. 1993;329:321–5. doi: 10.1056/NEJM199307293290506. [DOI] [PubMed] [Google Scholar]
- 4.Kelley AS, Deb P, Du Q, Aldridge Carlson MD, Morrison RS. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff (Mill-wood) 2013;32:552–61. doi: 10.1377/hlthaff.2012.0851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Report to the Congress: Medicare payment policy. Washington, DC: Medicare Payment Advisory Commission; Mar, 2014. http://www.medpac.gov/documents/reports/mar14_entirereport.pdf. [Google Scholar]
- 6.Report to the Congress: reforming the delivery system. Washington, DC: Medicare Payment Advisory Commission; Jun, 2008. http://www.medpac.gov/documents/reports/Jun08_EntireReport.pdf. [Google Scholar]
- 7.Medicare hospices that focus on nursing facility residents. Washington, DC: Office of Inspector General, Department of Health and Human Services; Jul, 2011. http://oig.hhs.gov/oei/reports/oei-02-10-00070.pdf. [Google Scholar]
- 8.Miller SC, Lima J, Gozalo PL, Mor V. The growth of hospice care in U.S. nursing homes. J Am Geriatr Soc. 2010;58:1481–8. doi: 10.1111/j.1532-5415.2010.02968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emanuel EJ. Cost savings at the end of life: what do the data show? JAMA. 1996;275:1907–14. [PubMed] [Google Scholar]
- 10.Campbell DE, Lynn J, Louis TA, Shugarman LR. Medicare program expenditures associated with hospice use. Ann Intern Med. 2004;140:269–77. doi: 10.7326/0003-4819-140-4-200402170-00009. [DOI] [PubMed] [Google Scholar]
- 11.Gozalo PL, Miller SC, Intrator O, Barber JP, Mor V. Hospice effect on government expenditures among nursing home residents. Health Serv Res. 2008;43:134–53. doi: 10.1111/j.1475-6773.2007.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor DH, Jr, Ostermann J, Van Houtven CH, Tulsky JA, Steinhauser K. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare program? Soc Sci Med. 2007;65:1466–78. doi: 10.1016/j.socscimed.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 13.Bureau of Labor Statistics. Consumer price index for medical care services. 2013 http://www.bls.gov/data.
- 14.Gozalo P, Teno JM, Mitchell SL, et al. End-of-life transitions among nursing home residents with cognitive issues. N Engl J Med. 2011;365:1212–21. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newhouse JP, Manning WG, Keeler EB, Sloss EM. Adjusting capitation rates using objective health measures and prior utilization. Health Care Financ Rev. 1989;10:41–54. [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Medicare and Medicaid Services. Provider of Services Current Files. http://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/index.html.
- 17.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donald SG, Lang K. Inference with difference-in-differences and other panel data. Rev Econ Stat. 2007;89:221–33. [Google Scholar]
- 19.Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–98. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 20.Plotzke M, Christian TJ, Pozniak A, et al. Medicare hospice payment reform: analyses to support payment reform: interim report to the Centers for Medicare and Medicaid Services. Cambridge, MA: Abt Associates; May 1, 2014. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice/Downloads/May-2014-AnalysesToSupportPaymentReform.pdf. [Google Scholar]
- 21.Mitchell SL, Miller SC, Teno JM, Kiely DK, Davis RB, Shaffer ML. Prediction of 6-month survival of nursing home residents with advanced dementia using ADEPT vs hospice eligibility guidelines. JAMA. 2010;304:1929–35. doi: 10.1001/jama.2010.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Banaszak-Holl J, Mor V. Differences in patient demographics and expenditures among Medicare hospice providers. Hosp J. 1996;11:1–19. doi: 10.1080/0742-969x.1996.11882824. [DOI] [PubMed] [Google Scholar]
- 23.Baer WM, Hanson LC. Families’ perception of the added value of hospice in the nursing home. J Am Geriatr Soc. 2000;48:879–82. doi: 10.1111/j.1532-5415.2000.tb06883.x. [DOI] [PubMed] [Google Scholar]
- 24.Miller SC, Mor V, Wu N, Gozalo P, Lapane K. Does receipt of hospice care in nursing homes improve the management of pain at the end of life? J Am Geriatr Soc. 2002;50:507–15. doi: 10.1046/j.1532-5415.2002.50118.x. [DOI] [PubMed] [Google Scholar]
- 25.Teno JM, Gozalo PL, Lee IC, et al. Does hospice improve quality of care for persons dying from dementia? J Am Geriatr Soc. 2011;59:1531–6. doi: 10.1111/j.1532-5415.2011.03505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


