Abstract
Objective
To assess the surgeon factors influencing the surgical treatment decisions for symptomatic stone disease. The factors influencing the selection of shock wave lithotripsy (SWL), ureteroscopy, or percutaneous nephrolithotomy to treat symptomatic stone disease are not well studied.
Methods
Electronic surveys were sent to urologists with American Medical Association membership. Information on training, practice, and ideal treatment of common stone scenarios was obtained and statistically analyzed.
Results
In November 2009, 600 surveys were sent and 180 were completed. High-volume SWL practices (>100 cases annually) were more common in community practice (P < .01), and high-volume ureteroscopy and percutaneous nephrolithotomy practices were more common in academic practice (P = .03). Community practice was associated with SWL selection for proximal urolithiasis and upper pole nephrolithiasis (P < .005). An increasing time since urologic training was associated with SWL selection for proximal urolithiasis and upper pole nephrolithiasis (P < .01). Urologists reporting shock wave lithotriptor ownership were 3-4 times more likely to select SWL for urolithiasis or nephrolithiasis compared with urologists who did not own a lithotripter (P < .01). Routine concern for stent pain and rigid ureteroscope preference (vs flexible) were associated with SWL selection (P < .03).
Conclusion
Surgeon factors significantly affected urolithiasis treatment selection. SWL was associated with community urology practice, increasing time since training, shock wave lithotriptor ownership, concern for stent pain, and ureteroscope preference.
Stone treatment options have improved during the past 3 decades, with a significant evolution in management away from traditional open lithotomy to minimally invasive procedures, including shock wave lithotripsy (SWL), ureteroscopy, and percutaneous nephrolithotomy (PCNL). In 2007, the American Urological Association published guidelines for urolithiasis management and recommended SWL and ureteroscopy as the first-line surgical therapies for urolithiasis.1 Although ureteroscopy and SWL are considered first-line therapy for most stones, PCNL has been advocated instead of ureteroscopy and SWL for larger renal stones (>1-2 cm), lower pole renal stones, and stones with unfavorable composition (ie, cysteine, brushite, calcium oxalate monohydrate).2 Despite the availability of multiple acceptable treatment options for common stone scenarios, SWL is the most commonly performed procedure for stone treatment.3-5 SWL is an appealing treatment option because of its low morbidity, noninvasiveness, and acceptable efficacy. SWL, however, is associated with a lower stone-free rate and greater retreatment rate compared with ureteroscopy or PCNL and ureteroscopy is a more cost-effective treatment strategy for symptomatic urolithiasis compared with SWL.6-9 Furthermore, SWL and ureteroscopy have similar overall rates of complications; however, the type of complication can differ for each treatment.10
The factors influencing the selection of SWL, ureteroscopy, or PCNL for stone treatment are not well understood.4 Patient-specific and physician-specific factors likely influence the treatment choice. Although none have been proved to affect treatment selection, some have theorized that certain factors could be influential, including equipment availability, training level, cost, reimbursement, and concerns over patient discomfort. Our objective was to assess the urologic surgeon factors influencing surgical treatment decisions for commonly encountered symptomatic urolithiasis.
Material and Methods
The Mayo Clinic Department of Urology Research Committee reviewed and approved the present study. Because the study did not involve a patient population, institutional review board approval was not required. After study approval, electronic surveys were sent to urologists with membership in the American Medical Association. The survey was designed to assess the surgical training background, characteristics of the surgeons' stone practice, and importance of common clinical variables in the assessment and treatment of a patient with symptomatic stone disease. High-volume practices were those with >100 procedures annually. Specific clinical scenarios were then presented, and the surgeons were asked to identify the surgical treatment modality of preference. In the clinical scenarios, the respondents were to assume an uncomplicated patient without other comorbidities and were given a stone size and location (ie, proximal ureter, distal ureter, lower pole of the kidney, upper pole of the kidney, and renal pelvis). They were then asked to choose the 1 best treatment, including ureteroscopy, SWL, PCNL, or stent placement. The final portion of the survey collected demographic information about the respondent. The survey also asked the respondents to determine the importance of the following subjective variables when selecting an appropriate urolithiasis treatment: stone size, stone location, stone composition, patient age, comorbidity, bilateral stones, hospital resources, surgical schedule availability, and payer status. The survey is presented in Appendix 1.
Comparisons between categorical variables were performed using Pearson's chi-square or Fisher's exact test, as appropriate. Comparisons involving ordinal variables were performed using the Cochran-Mantel-Haenszel test or its exact version, as appropriate. Odds ratios were estimated using logistic regression analysis. All tests were 2-sided, and P ≤ .05 was considered significant. Statistical analyses were done using the SAS, version 9.1.3, software package (SAS Institute, Cary, NC).
Results
Of 600 electronic surveys sent to urologists with American Medical Association membership, 200 surveys were initiated and 180 completed. Nine additional surveys were incomplete and were included in the analysis when possible. The median age of the respondents was 45 years (range 30-60). Additional endourologic training beyond residency was reported by 55 (29%) of the 189 respondents. Fellowship training was reported by 18 (10%), a minifellowship by 10 (5%), and formal endourologic course training by 27 (14%) of the 189 respondents. Of the 189 respondents, 63 (33%) reported academic practice and 121 (64%) reported community practice. Practice location was identified by American Urological Association section: New England, 17 (9%); Northeast, 8 (4%), New York, 8 (4%); Southeast, 41 (22%); South Central, 25 (13%); North Central, 41 (22%); Mid-Atlantic, 14 (7%); and Western, 34 (18%). No significant preference differences were found for any treatment modality according to geographic region when the practice patterns of the different American Urological Association sections were compared (P > .05).
The academic and community practice were stratified, and we found that high-volume stone practices (>100 procedures annually) were more common in the community setting (P < .001). When assessed by surgical treatment type, we found that high-volume ureteroscopy and PCNL practices were more common in the academic practice (P = .03 and P < .001 respectively), and high-volume SWL practices were more common in community practice (P < .001). When the patient variables important in clinical decision making were subjectively assessed, stone composition was consider significantly more often in academic practice (P < .001). The consideration of stone size, stone location, patient age and comorbidities, bilateral stone status, hospital resources, surgical schedule availability, and payer status did not vary between the academic and community practice urologists (P > .05). When the influence of practice setting was assessed in specific clinical scenarios, community urologists were more likely to choose SWL over other treatments in the following scenarios: proximal urolithiasis <5 mm to ≤15 mm, renal pelvis and lower pole nephrolithiasis <5 mm to >20 mm, and upper pole nephrolithiasis <5-15 mm (P < .005).
Treatment selection was significantly associated with time since urologic training for clinical scenarios involving urolithiasis <5-15 mm in the proximal ureter, nephrolithiasis <5-15 mm in the upper renal pole, and nephrolithiasis <5 mm to >20 mm in the renal pelvis and in the lower renal pole (P < .001). The time since urologic training was not associated with treatment selection for distal urolithiasis <15 mm (P > .05). With increasing time since urologic training, urologists were significantly more likely to select SWL for proximal urolithiasis, renal pelvis nephrolithiasis, and upper and lower renal pole nephrolithiasis, and ureteroscopy or PCNL was more likely to be selected with less time since urologic training (P < .01). The odds ratios for urologist selection of SWL over ureteroscopy or PCNL with greater time since training are listed in Table 1. When the variables important in clinical decision making were subjectively assessed (ie, stone size, stone location, stone composition, patient age, comorbidity, bilateral stone status, hospital resources, surgical schedule availability, and payer status), the response did not vary by the time since urologic training (P > .05).
Table 1. Odds ratios for urologist selection of SWL treatment of symptomatic stone disease.
| Variable | OR (URS Reference) (95% CI) | P Value | OR (PCNL Reference) (95% CI) | P Value |
|---|---|---|---|---|
| Increasing time since training | ||||
| Proximal ureter | ||||
| 15 mm | 1.6 (1.3-2.1) | < .001 | 1.1 (0.6-2.2) | .77 |
| 5-10 mm | 1.4 (1.1-1.8) | .003 | NA | |
| ≤5 mm | 1.4 (1.1-1.8) | .005 | NA | |
| Renal pelvis | ||||
| ≥2 cm | NA | 2.3 (1.5-3.7) | < .001 | |
| 15 mm | 2.2 (1.5-3.1) | < .001 | 1.6 (1.1-2.2) | .006 |
| 5-10 mm | 1.7 (1.3-2.3) | < .001 | 1.8 (0.7-4.6) | .24 |
| Lower pole | ||||
| ≥2 cm | 4.4 (1.3-14.8) | .02 | 4.1 (1.6-10.5) | .003 |
| 15 mm | 1.9 (1.3-2.7) | .002 | 1.6 (1.2-2.0) | < .001 |
| 5-10 mm | 2.2 (1.7-2.9) | < .001 | NA | |
| Upper pole | ||||
| 15 mm | 1.6 (1.3-2.0) | < .001 | 1.3 (1.0-1.7) | .10 |
| 5-10 mm | 1.4 (1.1-1.8) | .003 | NA | |
| ≤5 mm | 1.4 (1.1-1.8) | .005 | NA | |
| Shock wave lithotriptor ownership | ||||
| Distal ureter | ||||
| 15 mm | 4.9 (1.1-22.4) | .04 | NA | |
| 5-10 mm | 2.4 (0.7-7.6) | .15 | NA | |
| 5 mm | 1.5 (0.4-6.0) | .59 | NA | |
| Proximal ureter | ||||
| 15 mm | 3.6 (1.9-7.1) | < .001 | 2.6 (0.5-13.5) | .27 |
| 5-10 mm | 4.4 (2.3-8.5) | < .001 | NA | |
| ≤5 mm | 4.0 (2.0-8.1) | < .001 | NA | |
| Shock wave lithotriptor ownership | ||||
| Renal pelvis | ||||
| >2 cm | 1.6 (0.9-3.0) | .86 | 0.6 (0.3-1.3) | .21 |
| 15 mm | 3.0 (1.1-8.4) | .04 | 2.6 (1.1-6.6) | .04 |
| 5-10 mm | 3.4 (1.4-8.0) | .005 | NA | |
| Lower pole | ||||
| >2 cm | 1.2 (0.1-15.9) | .87 | 0.5 (0.2-1.1) | .07 |
| 15 mm | 2.0 (0.7-5.9) | .19 | 1.2 (0.6-2.2) | .57 |
| 5-10 mm | 3.3 (1.4-5.6) | .003 | NA | |
| ≤5 mm | 3.4 (1.4-8.0) | .005 | NA | |
| Upper pole | ||||
| 15 mm | 3.1 (1.1-8.4) | .03 | 2.2 (1.1-4.9) | .06 |
| 5-10 mm | 3.9 (1.7-9.0) | .79 | NA | |
| ≤5 mm | 3.0 (1.4-6.3) | .005 | NA |
OR, odds ratio; URS, ureteroscopy; CI, confidence interval; PCNL, percutaneous nephrolithotomy.
In the subgroup of 55 respondents with additional endourologic training, the time since urologic training did not affect the treatment selection to the extent that it did for urologists without additional endourologic training. The preference for SWL over ureteroscopy with increasing time since training and ureteroscopy over SWL with less time since training was limited to the scenarios with 5-10-mm renal pelvis nephrolithiasis, upper pole nephrolithiasis <10 mm and lower pole nephrolithiasis <10 mm (P < .05). Additional endourologic training did not affect the subjective responses to the variables important in clinical decision making (P > .05).
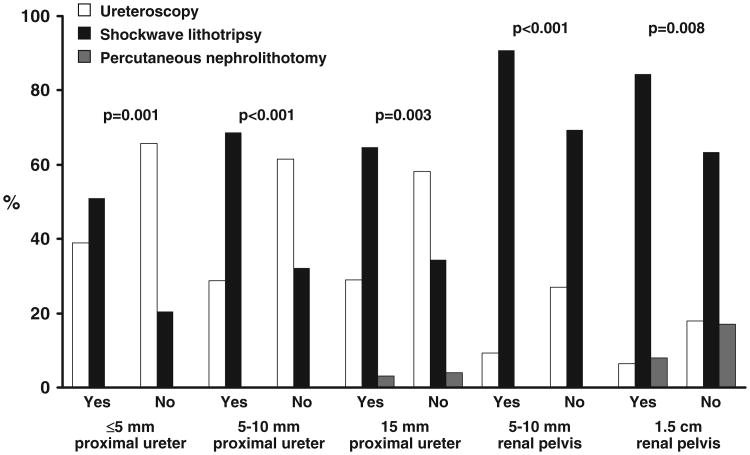
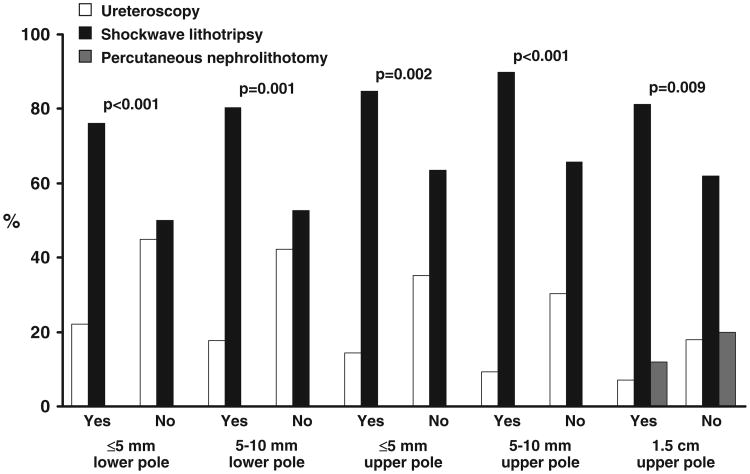
In addition to practice setting and time since urologic training, ownership of a shock wave lithotriptor was significantly associated with stone treatment selection. Urologists reporting shock wave lithotriptor ownership were significantly more likely to select SWL over ureteroscopy or PCNL for the following treatment scenarios: 15-mm distal urolithiasis, proximal urolithiasis <5-15 mm, renal pelvis and upper renal pole nephrolithiasis <5-15 mm, and lower pole nephrolithiasis <5-10 mm (P < .01). Ownership was not associated with treatment selection for renal pelvis nephrolithiasis >20 mm, lower renal pole nephrolithiasis >15 mm, or distal urolithiasis <10 mm (P < .05). The treatment preferences for urolithiasis and nephrolithiasis stratified by shock wave lithotriptor ownership are listed in Table 2. Figures 1 and 2 illustrate the SWL preference for proximal ureteral, renal pelvis, and upper and lower renal pole urolithiasis over ureteroscopy stratified by shock wave lithotriptor ownership. The association of SWL treatment selection with shock wave lithotriptor ownership remained after controlling for the influence of urologist age. The odds ratios for urologist selection of SWL over ureteroscopy or PCNL when shock wave lithotriptor ownership was reported are listed in Table 1. In clinical scenarios, shock wave lithotriptor availability (ie, hospital owned or availability of a mobile shock wave lithotriptor) did not influence treatment selection, and no preference was seen for SWL over ureteroscopy or PCNL (P > .05). The availability or ownership of a holmium laser (for ureteroscopic or percutaneous laser lithotripsy) did not influence the treatment selection for any clinical scenario (P > .05).
Table 2. Treatment selection preferences for urolithiasis and nephrolithiasis by lithotriptor ownership.
| Yes (n = 109) | No (n = 80) | Total (n = 189) | P Value | |
|---|---|---|---|---|
| Distal ureter | ||||
| 15 mm | .04 | |||
| URS | 93 (86.1) | 74 (93.7) | 167 (89.3) | |
| SWL | 13 (12) | 2 (2.5) | 15 (8) | |
| 5-10 mm | .30 | |||
| URS | 93 (86.1) | 73 (92.4) | 166 (88.8) | |
| SWL | 13 (12) | 4 (5.1) | 17 (9.1) | |
| ≤5 mm | .06 | |||
| URS | 96 (89.7) | 66 (83.5) | 162 (87.1) | |
| SWL | 7 (6.5) | 3 (3.8) | 10 (5.4) | |
| Proximal ureter | ||||
| 15 mm | < .001 | |||
| URS | 31 (29) | 46 (58.2) | 77 (41.4) | |
| SWL | 69 (64.5) | 27 (34.2) | 96 (51.6) | |
| PCNL | 3 (2.8) | 3 (3.8) | 6 (3.2) | |
| 5-10 mm | < .001 | |||
| URS | 31 (28.7) | 48 (61.5) | 79 (42.5) | |
| SWL | 74 (68.5) | 25 (32.1) | 99 (53.2) | |
| PCNL | 0 (0) | 1 (1.3) | 1 (0.5) | |
| ≤5 mm | < .001 | |||
| URS | 42 (38.9) | 52 (65.8) | 94 (50.3) | |
| SWL | 55 (50.9) | 16 (20.3) | 71 (38) | |
| Renal pelvis | ||||
| >2 cm | .62 | |||
| URS | 3 (2.8) | 3 (3.8) | 6 (3.2) | |
| SWL | 21 (19.4) | 21 (26.9) | 42 (22.6) | |
| PCNL | 83 (76.9) | 53 (67.9) | 136 (73.1) | |
| 15 mm | .008 | |||
| URS | 7 (6.5) | 14 (17.7) | 21 (11.2) | |
| SWL | 91 (84.3) | 50 (63.3) | 141 (75.4) | |
| PCNL | 9 (8.3) | 13 (16.5) | 22 (11.8) | |
| 5-10 mm | < .001 | |||
| URS | 10 (9.3) | 21 (26.9) | 31 (16.8) | |
| SWL | 97 (90.7) | 54 (69.2) | 151 (81.6) | |
| PCNL | 0 (0) | 2 (2.6) | 2 (1.1) | |
| Upper pole | ||||
| 15 mm | .009 | |||
| URS | 7 (6.5) | 14 (17.7) | 21 (11.3) | |
| SWL | 87 (81.3) | 49 (62) | 136 (73.1) | |
| PCNL | 13 (12.1) | 16 (20.3) | 29 (15.6) | |
| 5-10 mm | < .001 | |||
| URS | 10 (9.3) | 24 (30.4) | 34 (18.2) | |
| SWL | 97 (89.8) | 52 (65.8) | 149 (79.7) | |
| PCNL | 0 (0) | 3 (3.8) | 3 (1.6) | |
| ≤5 mm | .002 | |||
| Ureteral stent | 1 (1) | 1 (1.3) | 2 (1.1) | |
| URS | 15 (14.3) | 27 (35.1) | 42 (23.1) | |
| SWL | 89 (84.8) | 49 (63.6) | 138 (75.8) | |
| Lower pole | ||||
| >2 cm | .14 | |||
| URS | 1 (0.9) | 2 (2.6) | 3 (1.6) | |
| SWL | 12 (11.1) | 16 (20.5) | 28 (15.1) | |
| PCNL | 95 (88) | 60 (76.9) | 155 (83.3) | |
| 15 mm | .32 | |||
| URS | 7 (6.5) | 10 (12.7) | 17 (9.1) | |
| SWL | 58 (54.2) | 37 (46.8) | 95 (51.1) | |
| PCNL | 42 (39.3) | 32 (40.5) | 74 (39.8) | |
| 5-10 mm | < .001 | |||
| URS | 19 (17.8) | 33 (42.3) | 52 (28.1) | |
| SWL | 86 (80.4) | 41 (52.6) | 127 (68.6) | |
| PCNL | 1 (0.9) | 4 (5.1) | 5 (2.7) | |
| ≤5 mm | < .001 | |||
| URS | 23 (22.1) | 35 (44.9) | 58 (31.9) | |
| SWL | 79 (76) | 39 (50) | 118 (64.8) | |
| PCNL | 0 (0) | 2 (2.6) | 2 (1.1) |
URS, ureteroscopy; SWL, shock wave lithotripsy; PCNL, percutaneous nephrolithotomy.
Data presented as numbers, with percentages in parentheses.
Figure 1.
Surgeon treatment preferences for proximal and renal pelvis stratified by shock wave lithotriptor ownership.
Figure 2.
Surgeon treatment preferences for upper and lower renal pole stones stratified by shock wave lithotriptor ownership.
Stent pain and ureteroscope preference were associated with treatment selection. The influence of stent pain was assessed by grouping the concern for stent pain into none/rare concern, some concern, and routine/always concern. Routine concern for stent pain was reported by 22 (12%), some concern by 90 (47%), and no concern by 77 (41%). A routine concern for stent pain was associated with the selection of SWL over ureteroscopy for distal urolithiasis and for proximal urolithiasis <5 mm (P < .03). A subjective preference for the type of ureteroscope (ie, rigid or flexible, or both) was obtained. The preference for rigid ureteroscopy rather than flexible ureteroscopy, or both, was associated with SWL treatment preference over ureteroscopy or PCNL for the following treatment scenarios: distal urolithiasis <5 mm, proximal urolithiasis <5-15 mm, renal pelvis nephrolithiasis <5-15 mm, lower pole nephrolithiasis <5 mm to >2 cm, and upper pole nephrolithiasis <5-15 mm (P < .04).
Comment
The patient and surgeon factors influencing treatment selection in the urologic community are not well understood. An understanding of the factors influencing the selection of surgical treatment is important in discussing strategies for cost-efficient treatment in a modern healthcare system. Our objective was to assess the urologic surgeon factors influencing treatment selection decisions for commonly encountered urinary calculi scenarios.
The preference for SWL over ureteroscopy or PCNL for common urinary calculi scenarios was associated with community-based urologic practice, increasing time since urologic training, shock wave lithotriptor ownership, preference for rigid ureteroscopy and concern for stent pain. High-volume (>100 cases annually) SWL practice was more common in community practice, and high-volume ureteroscopy or PCNL practice was more common in academic practice. SWL was preferred more often in community practice for proximal ureteral, renal pelvis, and renal calculi. The stone composition was more frequently considered in academic practice compared with community practice, which is significant because the stone composition was associated with treatment response to shock wave or laser lithotripsy.11,13 Increasing time since training was associated with SWL selection, and less time since training was associated ureteroscopy or PCNL selection. In assessing the influence of ownership, we found that holmium laser ownership and shock wave lithotriptor availability was not associated with treatment selection. However, ownership of a shock wave lithotriptor was associated with SWL selection for treatment of most stone scenarios compared with urologists without shock wave lithotriptor ownership. The preference for SWL selection with lithotriptor ownership was independent of urologist age. We also identified the preference for SWL when the urologists reported routine concern for stent pain or when they had a preference for rigid ureteroscopy rather than both flexible and rigid ureteroscopy. Subjective variables, including stone size, location, bilateral stone status, patient age or comorbidity, surgical schedule, hospital resource/equipment availability, and payer status, did not influence treatment selection.
An increased preference for SWL has been reported in several previous studies. Pearle et al5 and the Urologic Diseases of America Project found SWL was the most commonly performed stone treatment procedure in commercially insured patients. SWL accounted for 54% of procedures, ureteroscopy 42% of procedures, and PCNL 6% of the procedures.5 However, this analysis did not assess provider-specific characteristics, which might have influenced the use of certain surgical treatment options. Matlaga et al4 recognized an increasing preference for SWL and a decreasing preference for ureteroscopy and PCNL in candidates seeking board certification. From 2004 to 2008, initial certification candidates used ureteroscopy in 52% of stone cases compared with the first and second recertification candidates who used SWL in 57.4% and 60.5% of stone cases.4 PCNL use decreased from 6.8% for the initial certification candidates to 4.5% and 2.6% for the first and second recertification candidates.4 Although their data described contemporary stone practices, potential factors influencing stone management could not be assessed owing to the descriptive nature of the American Board of Urology database. Bandi et al3 observed similar trends in stone management practices in a regional cohort of urologists and observed that fellowship-trained endourologists, academic urologists, and urologists in practice <5 years performed ureteroscopy, PCNL, and medical expulsion therapy more frequently than those who were in practice >5 years and performed SWL more often. Their regional study was also descriptive and did not analyze the effects of surgeon or patient factors on the selection of stone treatment modality.
Multiple factors could be associated with SWL preference, such as the low morbidity and noninvasiveness nature of SWL, surgeon schedule availability, concern for stent pain, equipment costs, training background, and favorable physician reimbursement. We attempted to assess surgeon time availability as a factor because ureteroscopy can be more time-consuming compared with SWL, particularly for larger stones.14,15 We found that the subjective influence of surgeon schedule on stone treatment selection was reported by few urologists and did not vary by practice type, time since training, or equipment ownership or preference, suggesting that surgeon schedule was not a significant factor. We also assessed concerns over stent-related pain as an influencing factor affecting the selection of treatment modalities, because ureteral stenting is more commonly used after ureteroscopy compared with after SWL. Because stent-related pain produces significant morbidity, we theorized that concerns over stent pain might drive urologists to choose SWL over ureteroscopy.16 A very low percentage (12%) of urologists in our survey cited stent-related pain as a major treatment concern. This low concern for stent pain is possibly because of the routine ureteral stent placement in patients with stones, including patients undergoing SWL. However, urologists with routine concern for stent pain selected SWL more often for all distal urolithiasis scenarios and proximal urolithiasis <5 mm. In all other clinical scenarios, routine concern for stent pain did not appear to affect clinical decision making. These findings support the theory that some urologists choose SWL over ureteroscopy for distal urolithiasis and small proximal urolithiasis in an attempt to avoid poststent-induced pain.
Our findings validate and elaborate on the observations and conclusions of Matlaga et al4 and Bandi et al3 and suggest that stone treatment preference is associated with training background. The association of treatment preference and training was suggested by the SWL preference with increasing time since training, the ureteroscopy and PCNL preference with less time since training, and the SWL preference by urologists with rigid ureteroscopy preference. The influence of training was also suggested by our finding that urologists with additional endourologic training selected SWL less frequently with increasing time since training. The influence of training background on treatment selection was intuitive and might be related to the evolution of stone management. During the past several decades, the use of PCNL and flexible ureteroscopy have become increasingly more common, secondary to advancements in endoscopic technology and the development of smaller, more agile and flexible ureteroscopes.17 Before these technological advancements, rigid ureteroscopy, SWL, and open stone surgery were more commonly practiced. Flexible ureteroscopy requires a different skill set than rigid ureteroscopy and was used less often in the 1980s before the development of smaller, more agile and flexible ureteroscopes.17 In contrast, the skill set required to perform SWL has remained stable if not decreased because lithotripter technicians are now highly involved in the setup and function of the lithotripter. The increased use of PCNL and flexible ureteroscopy from the limited use in the 1980s might explain the treatment preference trends for SWL with increasing time in practice and the treatment preference trends for ureteroscopy and PCNL with less time in practice.
Our study design also assessed the influence of equipment ownership on treatment selection. We did not find ureteroscopy preference associated with holmium laser ownership; however, we did find significant SWL preference associated with shock wave lithotriptor ownership. To assess the possible confounding influence of training background and length of clinical practice, we assessed the influence of surgeon age on the association of SWL preference and shock wave lithotriptor ownership. After controlling for surgeon age, the association of shock wave lithotriptor ownership and SWL preference remained, suggesting lithotriptor ownership is significantly associated with SWL use for stone management. Although physician conflict of interest in comparable aspects of care, such as in-office imaging, have been identified in a growing body of data, the conflict of interest in lithotripter ownership and SWL use has not been studied.18,19 The conflict of interest in lithotriptor ownership and use could potentially be further confounded by reimbursement issues because insurance reimbursement can be greater for SWL than ureteroscopy or PCNL (available from: http://aua.codingtoday.com). Although favorable reimbursement could be a possible confounding factor, we did not see an association with lithotriptor availability and lithotriptor use, further supporting the finding that it is ownership driving the lithotriptor use.
The primary limitations of the present study were the limited study participation and selection bias. Because participants were self-selected and were limited to urologists with membership in the American Medical Association, it might not be possible to generalize our findings to the general urologic community. As of September 2011, the American Urologic Association member profile reported 13 089 US members (available from: http://www.auanet.org). Compared with the number of practicing urologists, our survey assessed the practice preferences of <2% and, therefore, might not reflect more general practice patterns. Despite these limitations, however, our findings confirm previously observed trends and offer new insight into surgeon-related factors influencing the selection of stone treatment modality.
Conclusions
Surgeon factors influenced the selection of surgical treatment modality for common clinical stone scenarios. SWL use was associated with community urology practices, increasing time since urologic training, shock wave lithotriptor ownership, routine concern for stent pain, and when preference for rigid ureteroscopy was reported. PCNL and ureteroscopy use were associated with academic urology practices, less time since urologic training and not with holmium laser or lithotripter ownership. Additional research efforts to assess surgeon factors influencing stone treatment are necessary and will be important in developing cost-effective healthcare delivery strategies.
Supplementary Material
Acknowledgments
Funding Support: This study was supported by the Department of Urology, Mayo Clinic, Rochester, Minnesota.
Footnotes
Financial Disclosure: J. E. Lingeman is a consultant/adviser, meeting participant/lecturer for Lumenis, consultant/adviser, investor, meeting participant/lecturer, scientific study/trial investigator for Boston Scientific, consultant/adviser for Olympus, meeting participant/lecturer for Karl Storz Medical, owner, medical director of Beck Analytic, owner of and investor in Midwest Mobile Lithotripsy, and owner of and investor in Midstate Mobile Lithotriptor.
Appendix: Supplementary data: Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j. urology.2011.11.024.
References
- 1.Preminger GM, Tiselius HG, Assimos DG, et al. Guideline for the management of ureteral calculi. J Urol. 2007;178:2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 2.Wignall GR, Canales BK, Denstedt JD, et al. Minimally invasive approaches to upper urinary tract urolithiasis. Urol Clin North Am. 2008;35:441–454. viii. doi: 10.1016/j.ucl.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Bandi G, Best SL, Nakada SY. Current practice patterns in the management of upper urinary tract calculi in the north central United States. J Endourol. 2008;22:631–636. doi: 10.1089/end.2007.0186. [DOI] [PubMed] [Google Scholar]
- 4.Matlaga BR American Board of Urology. Contemporary surgical management of upper urinary tract calculi. J Urol. 2009;181:2152–2156. doi: 10.1016/j.juro.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Pearle MS, Calhoun EA, Curhan GC, et al. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848–857. doi: 10.1097/01.ju.0000152082.14384.d7. [DOI] [PubMed] [Google Scholar]
- 6.Lotan Y, Gettman MT, Roehrborn CG, et al. Management of ureteral calculi: a cost comparison and decision making analysis. J Urol. 2002;167:1621–1629. [PubMed] [Google Scholar]
- 7.Parker BD, Frederick RW, Reilly TP, et al. Efficiency and cost of treating proximal ureteral stones: shock wave lithotripsy versus ureteroscopy plus holmium:yttrium-aluminum-garnet laser. Urology. 2004;64:1102–1106. doi: 10.1016/j.urology.2004.07.040. [DOI] [PubMed] [Google Scholar]
- 8.Nabi G, Downey P, Keeley F, et al. Extra-corporeal shock wave lithotripsy (ESWL) versus ureteroscopic management for ureteric calculi. Cochrane Database Syst Rev CD. 2007;006029 doi: 10.1002/14651858.CD006029.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Srisubat A, Potisat S, Lojanapiwat B, et al. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev CD. 2009;007044 doi: 10.1002/14651858.CD007044.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Wolf JS., Jr Treatment selection and outcomes: ureteral calculi. Urol Clin North Am. 2007;34:421–430. doi: 10.1016/j.ucl.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 11.El-Nahas AR, El-Assmy AM, Mansour O, et al. A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: the value of high-resolution noncontrast computed tomography. Eur Urol. 2007;51:1688–1694. doi: 10.1016/j.eururo.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 12.Perks AE, Schuler TD, Lee J, et al. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology. 2008;72:765–769. doi: 10.1016/j.urology.2008.05.046. [DOI] [PubMed] [Google Scholar]
- 13.Wiesenthal JD, Ghiculete D, D'A Honey RJ, et al. Evaluating the importance of mean stone density and skin-to-stone distance in predicting successful shock wave lithotripsy of renal and ureteric calculi. Urol Res. 2010;38:307–313. doi: 10.1007/s00240-010-0295-0. [DOI] [PubMed] [Google Scholar]
- 14.Pearle MS, Lingeman JE, Leveillee R, et al. Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol. 2005;173:2005–2009. doi: 10.1097/01.ju.0000158458.51706.56. [DOI] [PubMed] [Google Scholar]
- 15.Salem HK. A prospective randomized study comparing shock wave lithotripsy and semirigid ureteroscopy for the management of proximal ureteral calculi. Urology. 2009;74:1216–1221. doi: 10.1016/j.urology.2009.06.076. [DOI] [PubMed] [Google Scholar]
- 16.Joshi HB, Stainthorpe A, MacDonagh RP, et al. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol. 2003;169:1065–1069. doi: 10.1097/01.ju.0000048980.33855.90. [DOI] [PubMed] [Google Scholar]
- 17.Kijvikai K, Haleblian GE, Preminger GM, et al. Shock wave lithotripsy or ureteroscopy for the management of proximal ureteral calculi: an old discussion revisited. J Urol. 2007;178:1157–1163. doi: 10.1016/j.juro.2007.05.132. [DOI] [PubMed] [Google Scholar]
- 18.Hollingsworth JM, Birkmeyer JD, Zhang YS, et al. Imaging use among employed and self-employed urologists. J Urol. 2010;184:2480–2484. doi: 10.1016/j.juro.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 19.Moser JW. Getting at the facts on imaging utilization growth. J Am Coll Radiol. 2005;2:720–724. doi: 10.1016/j.jacr.2005.07.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.