Abstract
Background
Achieving and sustaining high levels of healthcare worker (HCW) compliance with contact isolation precautions is challenging. The aim of this study was to determine HCW work system barriers to, and facilitators of, adherence to contact isolation for patients with suspected or confirmed Clostridium difficile infection (CDI) using a human factors and systems engineering approach.
Methods
Prospective cohort study from September 2013 to November 2013 at a large academic medical center (hospital A) and an affiliated Veterans Administration (VA) hospital (hospital B). A human factors engineering (HFE) model for patient safety – the Systems Engineering Initiative for Patient Safety (SEIPS) model – was used to guide work system analysis and direct observation data collection. 288 observations were conducted. HCWs and visitors were assessed for compliance with all components of contact isolation precautions (hand hygiene, gowning, and gloving) before and after patient contact. Time required to complete contact isolation precautions was measured and adequacy of contact isolation supplies was assessed.
Results
Full compliance with contact isolation precautions was low at both hospitals: hospital A, 7%; hospital B, 22%. Lack of appropriate hand hygiene prior to room entry (Compliance: hospital A, 18%; hospital B, 29%) was the most common reason for lack of full compliance. More time was required for full compliance as compared to compliance with no components of contact isolation precautions before patient room entry, inside patient room, and after patient room exit (59.9 sec vs. 3.2 sec; P < .001; 507.3 sec vs. 149.7 sec; P = .006; 15.2 sec vs. 1.3 sec; P < .001). Compliance was lower when contact isolation supplies were inadequate (4% vs. 16%; P = .005).
Conclusions
Adherence to contact isolation precautions for CDI is a complex, time-consuming process. HFE analysis indicates multiple work system components serve as barriers and facilitators to full compliance with contact isolation precautions and should be addressed further to prevent CDI.
Keywords: Clostridium difficile, contact precautions, infection control, human factors, systems engineering
Background
Clostridium difficile is the major infectious etiology of nosocomial diarrhea causing as many as 25% of cases of nosocomial diarrhea.1 C. difficile infection (CDI) affects 500,000 Americans each year, is responsible for 20,000 deaths annually, and has an annual cost approaching $2 billion in the United States.2,3 The incidence and severity of C. difficile infection is rising.4 Prevention of C. difficile is essential and is a critical patient safety issue.5
C. difficile infection is considered largely preventable if optimal infection control practices are consistently and regularly deployed. However, there is significant variability across institutions regarding adherence to and implementation of C. difficile infection prevention practices6,7 Despite widespread knowledge that consistent adherence to contact isolation precautions is a cornerstone of CDI prevention, recent studies continue to demonstrate poor healthcare worker (HCW) compliance with these basic yet crucial infection prevention interventions.8 Novel investigation into the underlying causes of poor guideline adherence suggests there are myriad, often subtle reasons for nonadherence, and increasingly complex infection prevention interventions themselves are a source of ambiguity, that is, uncertainty or vagueness which prevents a system or process from achieving its purpose.9 This combination of complexity and ambiguity argues for a new systems based and user centered approach to infection prevention.10
Conceptual Model
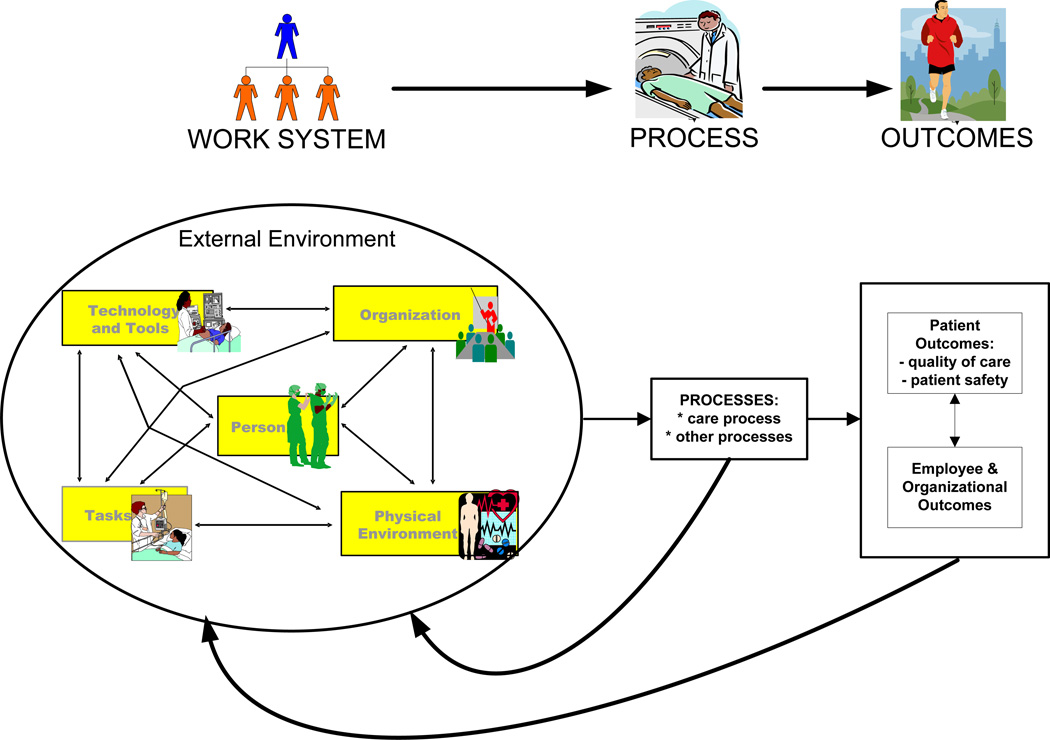
Human factors engineering (HFE) is the science of understanding interactions among humans and other elements of a system and designing systems for optimal performance and human well-being. The Systems Engineering Initiative for Patient Safety (SEIPS) model is an innovative HFE approach to patient safety originally described by Carayon and colleagues in 2006.11 The SEIPS model has been applied broadly in health care to improve patient safety in operating rooms, ICUs, ambulatory surgery centers, and outpatient clinics.12
At the center of the SEIPS model is the work system, which includes a person, tasks, tools and technologies, the physical environment, and organizational conditions (Figure 1). This work system approach guides a detailed and granular yet flexible analysis of multiple patient safety issues. Employing the SEIPS model to guide checklist generation and data collection, we performed a work-system analysis of contact isolation precautions for patients with suspected or confirmed CDI at two hospitals. We hypothesized that multiple work system barriers would pose challenges to successful HCW adherence to contact isolation precautions.
Figure 1.
Systems Engineering Initiative for Patient Safety (SEIPS) model.
Methods
Setting
Direct observations to collect data on the current practices of HCW caring for patients with CDI were conducted at a large academic medical center, henceforth known as hospital A and an affiliated Veterans Administration (VA) hospital, henceforth known as hospital B. Hospital A is a 586-bed tertiary care facility with active transplant, infection control, and antimicrobial stewardship programs with a closed intensive care unit (ICU). Hospital B is an 87-bed tertiary care hospital also with active transplant, infection control, and antimicrobial stewardship programs with an open ICU. Practices on general medicine, oncology, palliative care, intensive care, surgical, and transplant wards were observed.
Hospitals A and B are physically connected with overlapping medical staff, resident trainees, and medical students. There is no staff overlap of nursing, environmental services, physical/occupational therapy, food service, and laboratory technicians. Nursing and support staff at hospitals A and B are similarly trained in infection prevention procedures: All hospital staff at both hospitals are required to complete an annual safety and infection control online training module with a posttest. Both hospitals provide unit-level feedback on healthcare-associated infection rates and hand hygiene compliance. At any point in time, 10–15% of patients at both hospitals are in contact isolation precautions.
Contact isolation precautions are initiated and door signs posted for patients at both hospitals known or suspected to have gastrointestinal illness that is easily transmitted by direct patient contact or contact with patient environmental items. Frequent loose stools (3 or more in a 24 hour period), test ordering for CDI, or a positive CDI test result are objective triggers for initiating contact isolation precautions at both hospitals. C. difficile is the most common infection associated with contact isolation precautions at both hospitals, and both hospitals provide dedicated medical equipment (e.g. stethoscopes) for contact isolation rooms.
Work System Analysis
Tasks
Completing individual elements of contact isolation precautions were the tasks being performed. At hospital A, full compliance with contact isolation tasks requires completion of the following components in order: 1. Use of alcohol-based hand sanitizer or hand washing with soap and water. 2. Donning of gown and gloves. 3. Room entry. 4. Room exit. 5. Removal of gown and gloves. 6. Hand washing with soap and water (inside or outside the room). Hospital B has the same requirements for full compliance with the exception of gown use. Gowns must be worn in hospital B only if the individual comes in direct, physical contact with the patient or the patient environment.
Timing of contact isolation precaution tasks was also measured. Time elapsed from first use of alcohol-based hand sanitizer or first contact with personal protective equipment until patient room entry was defined as time “before room entry.” Time elapsed from entering patient room until exiting patient room was defined as “time in room.” Time elapsed from room exit until completion of hand hygiene, if performed, was defined as “time after room exit.” Timing data were obtained for contact isolation rooms and non-contact isolation rooms.
Process
Completion of all contact isolation tasks in the correct order was considered full compliance and was the main process measure. Completing at least one, but not all, contact isolation tasks was considered partial compliance. Failure to complete any contact isolation tasks was considered non-compliance. When adherence to one component of the protocol was unable to be determined, compliance was assumed. If adherence to more than one component was unable to be determined, the entire observation was excluded from the data set.
Tools and technologies
The supplies necessary to complete contact isolation precaution tasks were the tools in use. Supply adequacy of gowns, gloves, alcohol-based hand sanitizer, and soap was measured. Adequate sink access was also considered a necessary tool for completion of contact isolation tasks. Inadequate supplies were defined as lack of gowns, appropriate sized gloves, alcohol-based hand sanitizer, soap, or sink access.
Person
HCWs and visitors were considered the persons involved. The group identity (e.g. physical therapist) of each person entering a contact isolation room was recorded.
Organization
Hospitals A and B were considered two different organizations, and compliance data were compared between the two hospitals. ICU and non-ICU rooms were functionally considered two different “organizations” within hospital B as they are located in physically separated areas of the hospital and each has dedicated nursing, support, and management staff. Compliance data were compared between ICU and non-ICU rooms at hospital B. Work schedules are also considered an element of the organization component, which were evaluated by comparing weekday and weekend compliance data.
Environment
Room layout and locaton of gowns, gloves, alcohol-based hand sanitizer, soap, and sinks (room and hallway locations) were the main environmental features related to contact isolation precautions. Room and hallway blueprints were obtained from clinical engineering at both hospitals and used to draw and analyze representative room layouts. Distances to hallway sinks outside of patient rooms were also measured.
Instruments
We used the above SEIPS work system analysis to guide development of a checklist used to record time and measure compliance with each hospital’s contact isolation precautions. The checklist was also designed to ensure systematic observation and documentation of components of the SEIPS work system. It operationalized work system factors and standardized elements for observation.
Observations were performed from September 18, 2013 to November 11, 2013 at varied times throughout the day including weekdays and weekends. All people entering patient rooms under contact isolation precautions were observed. Individual identities of persons entering contact precaution rooms were not recorded, and there were no limits on the number of observations per person. A single, trained observer performed direct observation outside of patient rooms under contact isolation precautions for no longer than three consecutive hours.
Each episode of direct observation could include multiple rooms (range: 1–10 different rooms) on multiple hospital units (range: 1–5 different units). ICU observations were only performed at hospital B, which has an open ICU. Since many components of contact isolation precautions were present inside patient rooms, the observer attempted to maximize visibility into patient rooms, although this was not always possible. HCWs caring for patients under contact isolation precautions were not informed of our observations, and the observer was not a member of either hospital’s infection control team.
Data Analysis
Fisher’s two-tailed exact test was used for testing differences in proportions. Continuous data were analyzed using Student’s independent t-test. P value < .05 was the threshold for statistical significance. GraphPad Prism (GraphPad Software; La Jolla, CA) was used for statistical analysis. This project was considered a quality improvement project.
Results
There were a total of 288 observations; 237 at hospital A and 51 at hospital B. 175 observations were of nurses, 59 observations were of physicians, 17 observations were of visitors, 10 observations were of environmental staff, and 27 observations were distributed among other HCWs (physical therapists, occupational therapists, pharmacists, laboratory technicians, and food service).
The observer was unable to determine compliance with one component of the contact isolation protocol in 70 observations (24%), and compliance was assumed. Since appropriate hand hygiene could be performed inside patient rooms, and complete visibility into patient rooms was not always possible, all indeterminate data points resulted from the observer’s inability to accurately observe hand hygiene inside patient rooms. Four observations were completely excluded as compliance with more than one component of the contact isolation protocol was unable to be determined.
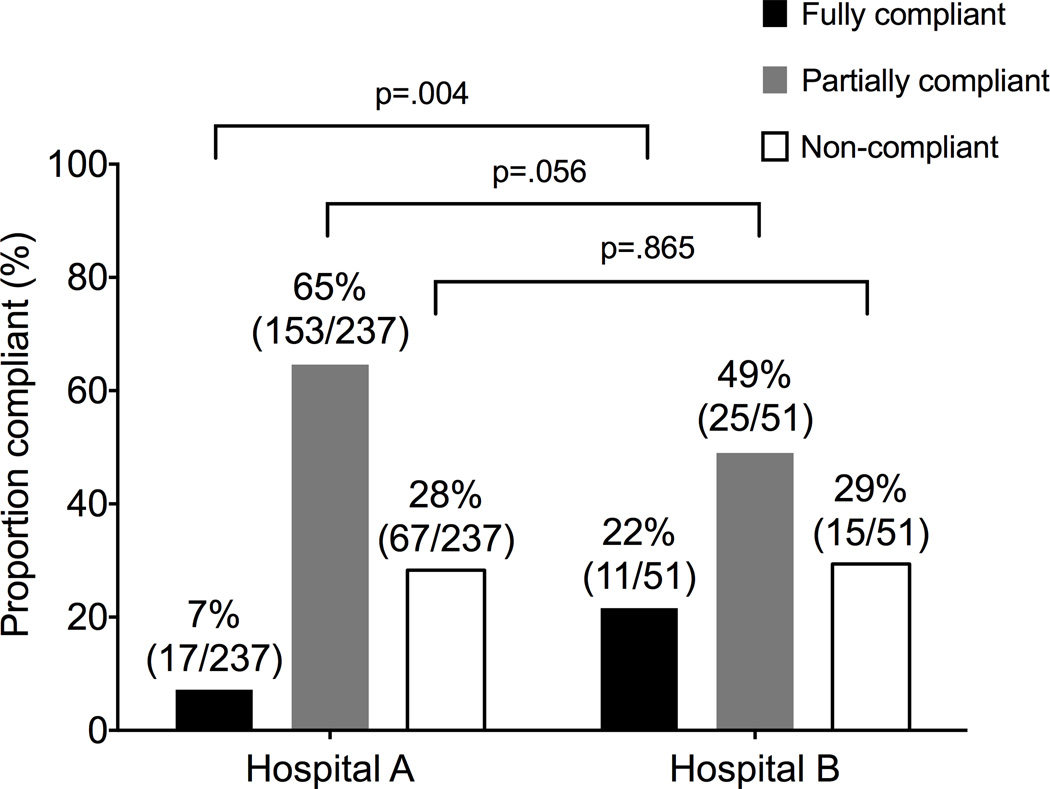
Full compliance with contact isolation precautions was low at both hospitals, the main SEIPS process measure. At hospital A, 17 persons (7%) fully complied with contact isolation precautions. Full compliance in hospital B was significantly higher and observed for 11 persons (22%) (P = .004). A comparison of rates of contact isolation precaution compliance between the two institutions is shown in Figure 2.
Figure 2.
Comparison of compliance with contact isolation precautions between two hospitals. Completion of all contact isolation precaution tasks in the correct order before room entry and after room exit was considered full compliance. Completing at least one, but not all, contact isolation tasks was considered partial compliance. Failure to complete any contact isolation tasks was considered non-compliance.
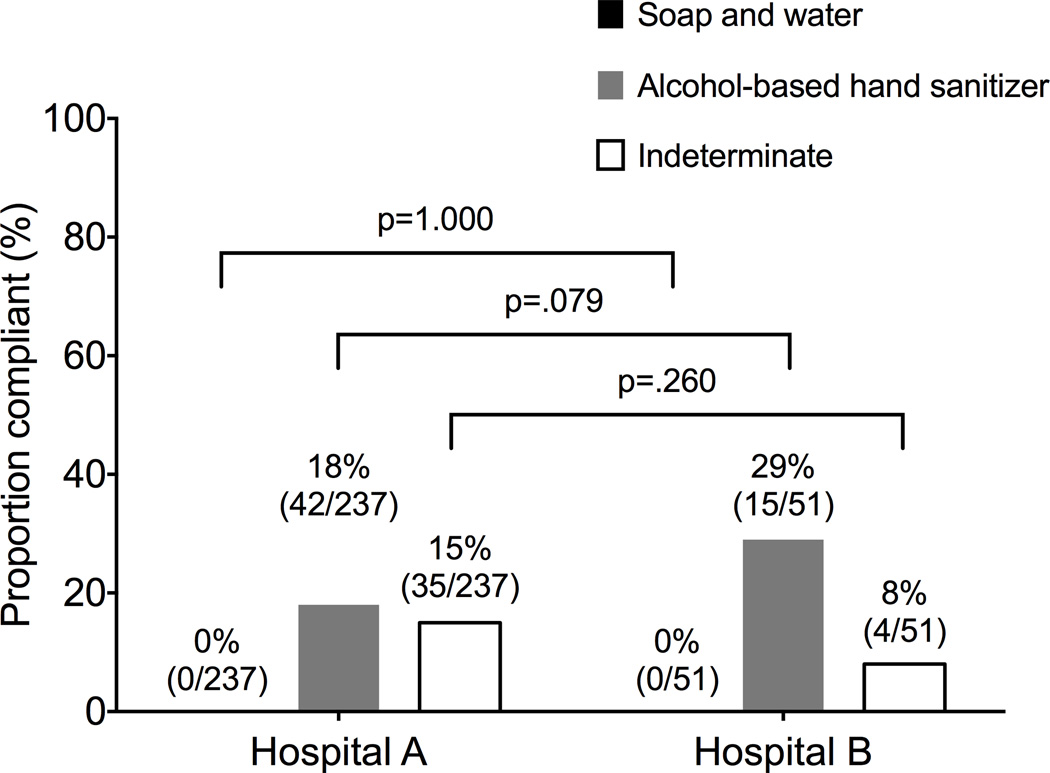
Rates of compliance with individual components of contact isolation precautions, representing the SEIPS work system task components, were also overall low. Rates of gown and glove use were not significantly different between hospitals A and B (63% vs. 71%; P = .337; 52% vs. 61%; P = .283). The rate of hand hygiene use before room entry was very low at both hospital A and B (18% vs. 29%; P = .079) shown in Figure 3. After room exit, use of soap and water for hand hygiene was significantly higher at hospital B (23% vs. 55%; P <.001).
Figure 3.
Comparison of compliance with hand hygiene prior to entry of contact isolation rooms at two hospitals. Use of soap and water or alcohol-based hand sanitizer prior to room entry was considered appropriate hand hygiene at both hospitals.
There were several differences in the environment related to contact isolation precautions at hospital A and B.
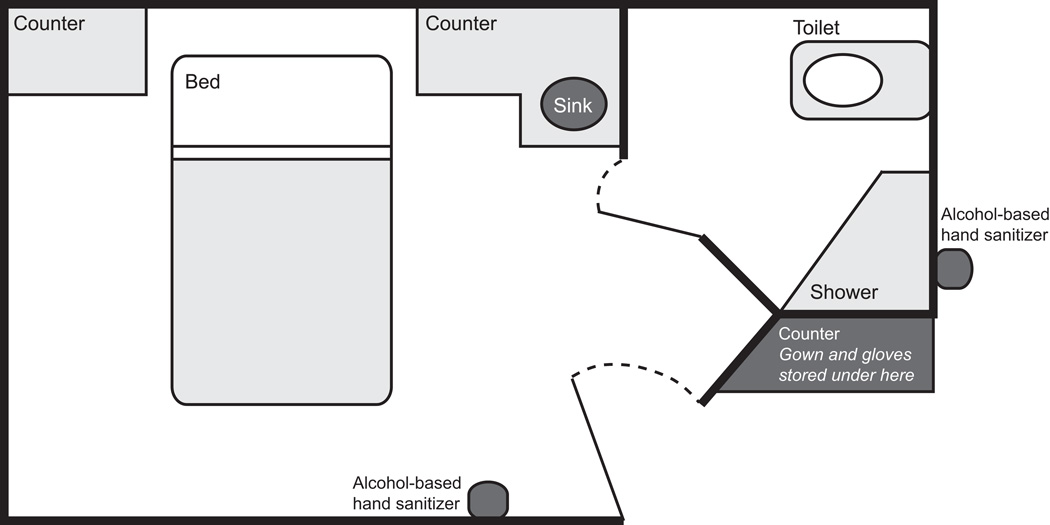
Hospital A: Gowns and gloves are located in a cabinet under a counter outside patient rooms. Alcohol based hand sanitizer is located both inside and outside patient rooms. Sinks and soap are located both inside patient rooms and at variable distances outside of patient rooms. The layout of a typical room at hospital A is shown in Figure 4. The average distance to the closest sink with soap outside the most commonly observed unit at hospital A was 9.5 ± 1.2 meters.
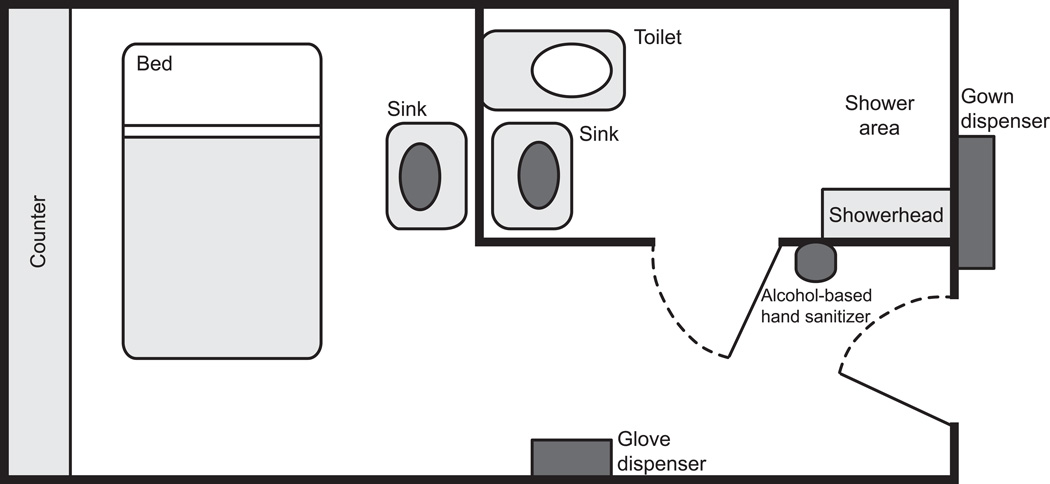
Figure 4.
Layout of a representative patient room in hospital A.
Hospital B: Gowns are supplied in a wall dispenser outside the patient room. Alcohol based hand sanitizer and a glove dispenser are mounted on the wall inside the patient room. Sinks and soap are located inside patient rooms in two locations (room and bathroom) and at variable distances outside of patient rooms. The layout of a typical non-ICU room at hospital B is shown in Figure 5. The average distance to the closest sink with soap outside of non-ICU rooms observed at hospital B was 10.9 ± 2.1 meters. Sinks were only present inside ICU rooms at hospital B.
Figure 5.
Layout of a representative patient room in hospital B.
Time required to comply with contact isolation precautions before room entry, time spent inside room, and time required after room exit were measured and compared with timing data from rooms not under isolation precautions (Table 1), which also addressed the SEIPS work system task component. Full compliance with contact isolation precautions as compared to non-compliance required a significantly greater amount of time before room entry, inside the room, and after room exit (59.9 sec vs. 3.2 sec; P < .001; 507.3 sec vs. 149.7 sec; P = .006; 15.2 sec vs. 1.3 sec; P < .001). Time required for full and partial compliance was not significantly different. Significantly less time was required before room entry and inside the room in non-isolation rooms as compared to full compliance (59.9 sec vs. 0 sec; P < .001, 507.3 sec vs. 28.4 sec; P = .027).
Table 1.
Relationship between compliance with contact isolation precautions and time required, relative to full compliance.
| Time | Mean (sec) | N | SEM | P |
|---|---|---|---|---|
| Before room entry | ||||
| Fully compliant | 59.9 | 21 | 7.15 | 1.000 |
| Partially compliant | 43.2 | 103 | 6.92 | .288 |
| Non-compliant | 3.2 | 56 | 2.16 | <.001 |
| Non-isolation room | 0.0 | 9 | 0 | <.001 |
| In room | ||||
| Fully compliant | 507.3 | 23 | 82.26 | 1.000 |
| Partially compliant | 375.0 | 108 | 37.18 | .140 |
| Non-compliant | 149.7 | 54 | 73.72 | .006 |
| Non-isolation room | 28.4 | 7 | 50.29 | .027 |
| After room exit | ||||
| Fully compliant | 15.2 | 21 | 6.33 | 1.000 |
| Partially compliant | 12.6 | 127 | 2.74 | .722 |
| Non-compliant | 1.3 | 89 | 0.81 | <.001 |
| Non-isolation room | 0.5 | 9 | 0.38 | .145 |
Note. Completion of all contact isolation precaution tasks in the correct order before room entry and after room exit was considered full compliance. Completing at least one, but not all, contact isolation tasks was considered partial compliance. Failure to complete any contact isolation tasks was considered non-compliance.
We compared rates of isolation precaution compliance among various types of HCWs and visitors, representing the SEIPS work-system persons. Physicians had a significantly higher rate of full compliance compared to nursing staff (17% vs. 7%; P = .043). Although not statistically significant, there was a trend toward a lower rate of compliance among visitors; none were in full compliance with contact isolation precautions.
Compliance with contact isolation precautions was compared between ICU and non-ICU rooms at hospital B, which reflected different organizations within hospital B. The rate of full compliance was significantly higher in the ICU (64% vs 10%; P = .001). Contact isolation compliance between weekdays and weekends was also compared. Full compliance with contact isolation precautions was significantly higher during the week as compared to the weekend (12% vs. 4%; P = .043).
At least one supply item for contact isolation precautions was observed as inadequate at hospital A in 83 of 184 (45%) observations. There were no supply inadequacies observed at hospital B. Contact isolation supplies included gowns, gloves, alcohol-based hand sanitizer, soap, and adequate sink access; these were considered the SEIPS work-system tools. Rates of compliance with contact isolation precautions were compared between rooms with adequate supplies and rooms with at least one supply inadequacy. The rate of full compliance was significantly lower with at least one supply inadequacy as compared to all supplies adequate (4% vs. 16%; P = .005). Full compliance was noted during 3 observations despite supply inadequacy. This occurred when HCWs obtained necessary supplies from nearby, adequately supplied rooms. Rates of full compliance based on healthcare worker type, ICU status, day of the week, and supply adequacy are summarized in Table 2.
Table 2.
Rates of full compliance with contact isolation precautions based on healthcare worker type, ICU status, day of week, and supply adequacy.
| Proportion (%) with full compliance |
P | |
|---|---|---|
| Occupation | ||
| Physicians | 10/59 (17%) | 1.000 |
| Nursing Staff | 13/175 (7%) | .043 |
| Visitors | 0/17 (0%) | .105 |
| Environmental Staff | 2/10 (20%) | 1.000 |
| Other Healthcare Worker* | 3/27 (11%) | .747 |
| ICU status† | ||
| ICU | 7/11 (64%) | 1.000 |
| Non-ICU | 4/40 (10%) | .001 |
| Day of week | ||
| Weekday | 24/204 (12%) | 1.000 |
| Weekend | 3/84 (4%) | .043 |
| Supply adequacy | ||
| All supplies adequate | 24/152 (16%) | 1.000 |
| Any supply item inadequate | 3/83 (4%) | .005 |
Includes physical therapists, occupational therapists, pharmacists, laboratory technicians, and food service.
ICU status compliance data were obtained only at hospital B.
Discussion
Prevention of CDI in healthcare settings relies on consistent, high adherence to contact isolation precautions by HCWs. However, in practice, this is difficult to achieve because of the changes in workflow necessitated by this intervention. Previous studies have demonstrated poor compliance with both individual and grouped components of contact isolation precautions.8,13–16 However, to our knowledge, this is the first study to apply a human factors and systems engineering approach to examine barriers to, and facilitators of, compliance with contact isolation precautions for CDI. We now examine our findings in the context of the SEIPS model.
The main process measure was compliance with contact isolation precautions. Full compliance with contact isolation precautions was very low across both institutions. Full compliance was higher at hospital B than hospital A, suggesting the presence of additional facilitators or absence of barriers at hospital B. The SEIPS model proposes these findings result from an interplay of all work system components (person, organization, technologies and tools, tasks, and environment), which we evaluate next with an emphasis on actionable interventions to improve contact isolation precaution adherence.
Among the many sequential tasks required to fully comply with contact isolation precautions, hand hygiene prior to glove use was the most commonly missed component. This is similar to previous findings demonstrating lower rates of hand hygiene compliance when wearing gloves, possibly the result of erroneous HCW perception that wearing gloves completely protects them from both pathogens on the patient and pathogens on the caregiver.17
To promote hand hygiene with soap and water following care of the patient with CDI, a possible approach may be to cover or inactivate alcohol-based hand sanitizer dispensers in CDI patient rooms. However, our findings suggest this may be counterproductive by discouraging appropriate hand sanitizer use before gloving. Hospital B has subsequently developed standalone alcohol-based hand sanitizer dispensers with signs stating “Gel In – Wash Out” that are placed outside of CDI patient rooms.
Time required to complete contact precautions is an essential part of work system task analysis. As expected, full compliance required more time before room entry, more time in the room, and more time after room exit compared to non-compliance. No significant time difference between partial and full compliance was observed, and full compliance required more time before room entry and in the room compared to non-contact isolation rooms. This may reflect that patient care tasks take longer to complete when wearing personal protective equipment or may be an adaptation to the previously described phenomenon of fewer HCW visits to contact precaution rooms.18 Regardless, these findings suggest all HCWs (i.e. physicians, nurses, and support staff) may need to be provided with more time or given fewer patients when caring for a large proportion of patients under contact isolation precautions.
The work system technologies and tools component was evaluated by assessing supply adequacy of personal protective equipment and hand hygiene products (i.e. gowns, gloves, alcohol-based hand sanitizer, soap, and sinks). These were considered the main tools used by HCWs to complete individual contact precaution tasks. Hospital A had at least one supply item inadequacy during nearly half of observations while hospital B had no observed supply inadequacies. Given hospital B’s overall higher rate of full compliance, this suggests supply inadequacy may be a significant barrier to CDI contact isolation precaution compliance. Since full compliance was still quite low at hospital B despite consistently adequate supplies, this further suggests adequate supplies are necessary but not sufficient for full compliance. These findings emphasize the need for adequate supplies of personal protective equipment near contact isolation precaution rooms.
Closely related to tasks and technologies and tools is the pervasive environment in which tasks are completed and tools are used. Evaluating the above results in the context of the patient room layouts suggests several specific recommendations related to the built environment of care. The presence of multiple sinks inside patient rooms (as at hospital B) may increase the rate of appropriate hand hygiene (i.e. soap and water) upon room exit, especially in the academic setting with larger medical teams of residents and students. Gown and glove dispensing locations were very different between hospitals A and B, yet there was no significant difference between their rates of use. One possible explanation is that separate locations of gown and gloves (i.e. hospital B) has no effect on their overall use as part of contact isolation precautions. Alternatively, the highly visible gown dispenser outside of every room at hospital B (as compared to inside a cabinet at hospital A) may have prompted HCWs to use gowns when they otherwise would not have, particularly since hospital B only required gown use when anticipating direct contact with the patient or patient environment.
Comparison of contact isolation compliance rates among various HCWs evaluated the multiple persons at the center of the SEIPS work system. In our study, physicians were more likely to be fully compliant with contact isolation precautions as compared with nurses, although both groups’ full compliance rates remained low. This is in contrast to several previous studies demonstrating superior contact isolation compliance among nursing staff.14–15,19 Hospital visitors were never fully compliant at both hospitals. This is consistent with earlier findings and may be the result of perceived immunity to C. difficile as visitors were exposed to the patient outside of the hospital and did not acquire C. difficile.20 Although visitors are less likely to visit multiple patient rooms as HCWs would, they may represent a vector for nosocomial spread of C. difficile into common areas. Neither hospital A nor hospital B has a consistently implemented infection prevention policy addressing visitors of patients under contact isolation precautions, and this represents a gap in CDI infection prevention.
Organizational elements of the work system are diverse and address less tangible areas of HFE such as teamwork, culture, social relationships, and management style. Hospitals A and B clearly reflect two different organizations, and such organizational factors may explain hospital B’s (a VA hospital) overall higher rate of full compliance. C. difficile prevention is a national VA priority culminating in a C. difficile bundle which has been implemented at every VA hospital nationwide since early 2012. In addition to contact isolation precautions, the VA C. difficile bundle includes directives for environmental management and cultural transformation. While organizational culture consists of more than policy content, using the VA C. difficile bundle as a model may be beneficial to non-VA health care organizations.
Within hospital B, the ICU and non-ICU patient care areas can be considered two different “organizations” as well. Compliance with contact isolation precautions was significantly higher in hospital B’s ICU compared to the general wards. This may be a consequence of greater emphasis on contact isolation precautions in critically ill patients or possibly the result of higher nurse to patient ratios. Higher hand hygiene compliance rates described previously in the ICU were attributed to HCW perception of higher patient risk in the ICU.21 Identification of these internal organizations (e.g. individual wards, teams, or services) can serve to highlight so-called “bright spots” or top performers and share best practices.
Synthesizing these findings in the context of the SEIPS indicates the entire work system must be addressed when designing interventions to improve compliance with C. difficile infection prevention practices. Traditional infection prevention interventions limited to a single group or intervention (e.g. improving physician hand hygiene) will be inadequate to address complex healthcare-associated infections like C. difficile. Indeed, poor infection prevention compliance may persist even after thoughtful but isolated interventions to improve adherence22, while many of the more effective contemporary interventions to improve infection prevention compliance have been multidimensional.23
The SEIPS model’s emphasis on multiple persons (e.g. physician, nurse, visitor, environmental services) at the center of the work system is particularly relevant to C. difficile infection prevention. Our findings strongly suggest optimal contact isolation precaution adherence requires multidisciplinary involvement and must engage all relevant stakeholders, in particular hospital visitors and environmental services.
Previous models of health care quality (e.g. Donabedian’s structure-process-outcome model) implied tight linkage between individual HCWs, individual care process, and individual care outcomes. This focus on the individual often assumed poor outcomes were solely a consequence of poor performance or behaviors. The SEIPS model, in contrast, recognizes processes and outcomes originate in the work system, which better reflects contemporary patient safety concepts with emphasis on the patient care system as opposed to individual providers.10
Several limitations warrant discussion. First, the same individual conducted all observations, potentially resulting in the Hawthorne effect. However, assuming HCWs improved their behavior in response to observation, this still suggests low compliance with contact isolation precautions. Second, our study took place in two academic teaching hospitals, limiting the generalizability of our findings. Third, there were several barriers at hospital B that made conducting observations more challenging than hospital A. Gloves were located in the patient room behind a curtain at hospital B. Consequently, if a healthcare worker entered a contact isolation room and closed the door, gathering complete compliance data was not possible. Fourth, contact isolation protocols differed slightly between the two hospitals: At hospital B, HCWs were only required to don gowns if they anticipated contact with the patient or patient environment, and it was not always possible for the observer to determine if HCW contact with the patient or environment occurred. This limited the number of total observations at Hospital B as inability to determine compliance with more than one component of contact isolation precautions resulted in exclusion of the entire observation from the data set. Finally, we did not assess provider perceptions of barriers to compliance as our main focus was on understanding the current practices at the facilities.
This study also has several strengths. Examining two institutions, one university and one VA, broadens the applicability of our findings. In addition, differences between these two facilities provide insight into very specific work system barriers and facilitators (e.g. number of sinks per room). Lastly, our multifaceted approach to direct observation by collecting compliance data, timing data, and evaluating supply adequacy allowed for a systematic interpretation of barriers and facilitators to contact isolation precautions compliance through use of an innovative HFE model designed for patient safety.
In conclusion, we found low compliance rates with C. difficile contact isolation precautions across two institutions, one an academic, tertiary care hospital, the other a VA hospital. The most common reason for noncompliance was lack of hand hygiene prior to room entry. While inadequate supplies partially explain non-compliant behavior, a HFE approach (SEIPS model) suggests multiple work system components serve as both barriers and facilitators to full compliance.
Acknowledgments
Financial support. Dr. Safar is supported by a Veterans Affairs MERIT award. The contents do not represent views of the Department of Veterans Affairs or the U.S. Government. Dr. Carayon is supported by the University of Wisconsin Institute for Clinical and Translational Research and by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021.
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article.
Contributor Information
Eric Yanke, Department of Medicine, William S. Middleton Memorial Veterans Hospital, Madison, Wisconsin..
Caroline Zellmer, College of Agricultural & Life Sciences, University of Wisconsin-Madison, Madison, Wisconsin..
Sarah Van Hoof, Department of Infection Control, University of Wisconsin Hospital and Clinics, Madison, Wisconsin..
Helene Moriarty, Villanova University College of Nursing, Villanova, Pennsylvania and Philadelphia Veterans Affairs Medical Center, Philadelphia, Pennsylvania..
Pascale Carayon, Department of Industrial and Systems Engineering, Center for Quality and Productivity Improvement, University of Wisconsin-Madison, Madison, Wisconsin..
Nasia Safdar, William S. Middleton Memorial Veterans Hospital and Division of Infectious Diseases, Department of Medicine, University of Wisconsin Medical School and Infection Control Department, University of Wisconsin-Madison, Madison, Wisconsin..
References
(PMID has been substituted at end of citation when DOI unavailable)
- 1.Mylonakis E, Ryan ET, Calderwood SB. Clostridium difficile--Associated diarrhea: A review. Arch Intern Med. 2001;161:525–533. doi: 10.1001/archinte.161.4.525. PMID: 11252111. [DOI] [PubMed] [Google Scholar]
- 2.Bouza E. Consequences of Clostridium difficile infection: understanding the healthcare burden. Clin Microbiol Infect. 2012;18(Suppl 6):5–12. doi: 10.1111/1469-0691.12064. [DOI] [PubMed] [Google Scholar]
- 3.McGlone SM, Bailey RR, Zimmer SM, et al. The economic burden of Clostridium difficile. Clin Microbiol Infect. 2012;18:282–289. doi: 10.1111/j.1469-0691.2011.03571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loo VG, Poirier L, Miller MA, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med. 2005;353:2442–2449. doi: 10.1056/NEJMoa051639. [DOI] [PubMed] [Google Scholar]
- 5.Vonberg RP, Kuijper EJ, Wilcox MH, et al. Infection control measures to limit the spread of Clostridium difficile. Clin Microbiol Infect. 2008;14(Suppl 5):2–20. doi: 10.1111/j.1469-0691.2008.01992.x. [DOI] [PubMed] [Google Scholar]
- 6.Dubberke ER, Reske KA, Noble-Wang J, et al. Prevalence of Clostridium difficile environmental contamination and strain variability in multiple health care facilities. Am J Infect Control. 2007;35:315–318. doi: 10.1016/j.ajic.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Murphy CR, Avery TR, Dubberke ER, Huang SS. Frequent hospital readmissions for Clostridium difficile infection and the impact on estimates of hospital-associated C. difficile burden. Infect Control Hosp Epidemiol. 2012;33:20–28. doi: 10.1086/663209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhar S, Marchaim D, Tansek R, et al. Contact precautions: more is not necessarily better. Infect Control Hosp Epidemiol. 2014;35:213–221. doi: 10.1086/675294. [DOI] [PubMed] [Google Scholar]
- 9.Gurses AP, Seidl KL, Vaidya V, et al. Systems ambiguity and guideline compliance: a qualitative study of how intensive care units follow evidence-based guidelines to reduce healthcare-associated infections. Qual Saf Health Care. 2008;17:351–359. doi: 10.1136/qshc.2006.021709. [DOI] [PubMed] [Google Scholar]
- 10.Yanke E, Carayon P, Safdar N. Translating Evidence into Practice Using a Systems Engineering Framework for Infection Prevention. Infect Control Hosp Epidemiol. 2014;35:1176–1182. doi: 10.1086/677638. [DOI] [PubMed] [Google Scholar]
- 11.Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(Suppl 1):50–58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon. 2014;45:14–25. doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afif W, Huor P, Brassard P, Loo VG. Compliance with methicillin-resistant Staphylococcus aureus precautions in a teaching hospital. Am J Infect Control. 2002;30:430–333. doi: 10.1067/mic.2002.125174. PMID: 12410221. [DOI] [PubMed] [Google Scholar]
- 14.Manian FA, Ponzillo JJ. Compliance with routine use of gowns by healthcare workers (HCWs) and non-HCW visitors on entry into the rooms of patients under contact precautions. Infect Control Hosp Epidemiol. 2007;28:337–340. doi: 10.1086/510811. [DOI] [PubMed] [Google Scholar]
- 15.Weber DJ, Sickbert-Bennett EE, Brown VM, et al. Compliance with isolation precautions at a university hospital. Infect Control Hosp Epidemiol. 2007;28:358–361. doi: 10.1086/510871. [DOI] [PubMed] [Google Scholar]
- 16.Bergsbaken J, Schulz LT, Trapskin PJ, Marx J, Safdar N. Pharmacist participation in infection prevention: an innovative approach to monitoring compliance with the Five Moments for Hand Hygiene in a large academic medical center. Am J Infect Control. 2014;42:331–332. doi: 10.1016/j.ajic.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 17.Fuller C, Savage J, Besser S, et al. “The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32:1194–1199. doi: 10.1086/662619. [DOI] [PubMed] [Google Scholar]
- 18.Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with Contact Precautions: a review of the literature. Am J Infect Control. 2009;37:85–93. doi: 10.1016/j.ajic.2008.04.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pittet D, Mourouga P, Perneger TV. Compliance with handwashing in a teaching hospital. Infection Control Program. Ann Intern Med. 1999;130:126–130. doi: 10.7326/0003-4819-130-2-199901190-00006. PMID: 10068358. [DOI] [PubMed] [Google Scholar]
- 20.Birnbach DJ, Nevo I, Barnes S, et al. Do hospital visitors wash their hands? Assessing the use of alcohol-based hand sanitizer in a hospital lobby. Am J Infect Control. 2012;40:340–343. doi: 10.1016/j.ajic.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Novoa AM, Pi-Sunyer T, Sala M, Molins E, Castells X. Evaluation of hand hygiene adherence in a tertiary hospital. Am J Infect Control. 2007;35:676–683. doi: 10.1016/j.ajic.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Whitby M, McLaws ML. Handwashing in healthcare workers: accessibility of sink location does not improve compliance. J Hosp Infect. 2004;58:247–253. doi: 10.1016/j.jhin.2004.07.024. [DOI] [PubMed] [Google Scholar]
- 23.Kowitt B, Jefferson J, Mermel LA. Factors associated with hand hygiene compliance at a tertiary care teaching hospital. Infect Control Hosp Epidemiol. 2013;34:1146–1152. doi: 10.1086/673465. [DOI] [PubMed] [Google Scholar]