Abstract
BACKGROUND
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is associated with sudden cardiac death. However, the selection of patients for implanted cardioverter-defibrillators (ICDs), as well as programming of the ICD, is unclear.
OBJECTIVES
The objective of this study was to identify predictors, characteristics, and treatment of ventricular arrhythmias in patients with ARVC.
METHODS
The Multidisciplinary Study of Right Ventricular Cardiomyopathy established the North American ARVC Registry and enrolled patients with a diagnosis of ARVC. Patients were followed prospectively.
RESULTS
Of 137 patients enrolled, 108 received ICDs. Forty-eight patients had 502 sustained episodes of ventricular arrhythmias, including 489 that were monomorphic and 13 that were polymorphic. In the patients with ICDs, independent predictors of ventricular arrhythmias in follow-up included spontaneous sustained ventricular arrhythmias before ICD implantation and T-wave inversions inferiorly. The only independent predictor for life-threatening arrhythmias, defined as sustained ventricular tachycardia (VT) ≥240 beats/min or ventricular fibrillation, was a younger age at enrollment. Anti-tachycardia pacing (ATP), independent of the cycle length of the VT, was successful in terminating 92% of VT episodes.
CONCLUSIONS
In the North American ARVC Registry, the majority of ventricular arrhythmias in follow-up are monomorphic. Risk factors for ventricular arrhythmias were spontaneous ventricular arrhythmias before enrollment and a younger age at ICD implantation. ATP is highly successful in terminating VT, and all ICDs should be programmed for ATP, even for rapid VT.
Keywords: arrhythmogenic right ventricular cardiomyopathy, implantable cardioverter-defibrillator, ventricular arrhythmia, ventricular tachycardia
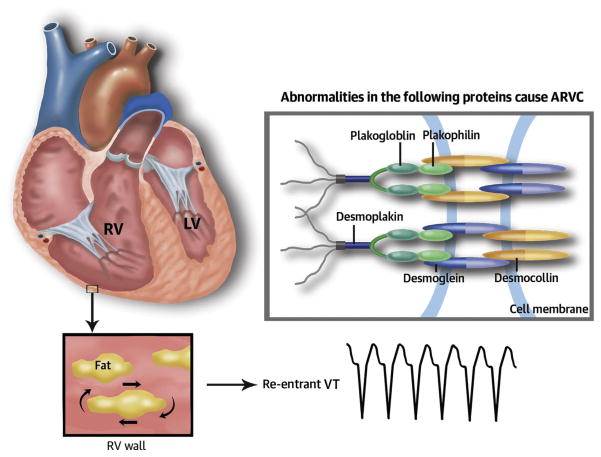
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a cardiomyopathy associated with sudden cardiac death (SCD) (Central Illustration) (1–3). Selection of patients for implantable cardioverter-defibrillators (ICDs) is controversial. Natural history studies have suggested risk factors for sudden cardiac death, including marked right ventricular (RV) dilatation, left ventricular (LV) involvement, hemodynamically unstable rapid sustained monomorphic ventricular tachycardia (SMVT), and history of syncope (4–8). However, these risk factors have not been consistent from study to study. In addition, guidelines for appropriate ICD programming are lacking. The North American Multidisciplinary Study of Right Ventricular Cardiomyopathy/Dysplasia was initiated in 2000 to clarify diagnostic criteria and assess treatment of ARVC (2,9,10). The focus of the current study is to review the experience in this prospective ARVC Registry.
METHODS
PATIENT POPULATION
At the enrolling centers, patients were subject to 12-lead electrocardiography (ECG), signal-averaged electrocardiography (SAECG), 24-h Holter monitoring, electrophysiology study with programmed ventricular stimulation, echocardiography, RV angiography, RV free-wall and septal biopsies, magnetic resonance imaging, and blood work for a genetic analysis. The decision to implant an ICD and all programming decisions were left to the discretion of the individual physician and patient. Stored elec-trograms were reviewed after any device therapy and with each scheduled follow-up. All electrograms were sent to the ICD core laboratory (Tufts Medical Center, Boston, Massachusetts), where all therapies were independently reviewed and classified by 2 electrophysiologists. Ventricular tachycardias were characterized as monomorphic or polymorphic and by cycle length.
STATISTICAL ANALYSIS
Descriptive characteristics are provided as mean ± SD and were compared by means of the Student t test. Continuous variables that were not normally distributed were reported as median and interquartile range and were compared with the use of the Wilcoxon rank-sum test. Categorical variables were compared by means of the chi-square analysis. The Cox proportional hazard model was used to examine the 2 primary arrhythmic endpoints: 1) ICD-treated ventricular arrhythmia, death, or transplantation; and 2) potentially life-threatening arrhythmia (defined as ventricular tachycardia >240 beats/min or ventricular fibrillation), using only those patients who had an ICD implanted. Univariate variables of significance were subject to multivariate stepwise models. Values of p < 0.05 were considered significant.
RESULTS
PATIENT POPULATION
A total 137 patients were enrolled in the ARVC registry. The mean age at enrollment was 40 ± 14 years. The presentation of the patients included SMVT or cardiac arrest (n = 56; 41%), and syncope without documented sustained arrhythmias (n = 17; 12%). Of these 137, 108 (78%) underwent an ICD implantation. Implant complications occurred in 2 patients, including an RV perforation and an infection that did not require ICD removal. During 3.3 ± 1.7 years of follow-up, 48 patients with an ICD had the combined endpoint of any ventricular arrhythmia, death, or transplantation, including 22 with the endpoint of life-threatening arrhythmias. In the patients not undergoing ICD implantation, there were no SCDs or documented sustained ventricular arrhythmia during a mean of 2.4 ± 1.5 years of follow-up.
CHARACTERISTICS OF PATIENTS BEFORE RECEIVING AN ICD VERSUS NO ICD
There was no difference in the mean age or sex of those who did or did not receive an ICD (Table 1). Fifty-two of the 108 (48%) patients with ICDs had spontaneous SMVT or sustained polymorphic ventricular fibrillation (SPVF) before ICD implantation, compared with 4 in the non-ICD group (p < 0.001). An additional 14 (13%) had syncope in the group implanted with ICDs, compared with 3 (10%) in the non-ICD group (p = 0.07). Other differences between the ICD patients and the non-ICD patients included a definitive diagnosis of ARVC, number of Task Force Criteria points, and T-wave inversions in leads V1 to V3.
TABLE 1.
Clinical and Electrophysiological Factors in Patients With ARVC Who Were or Were Not Implanted With an ICD
| Clinical Characteristics | ICD (n = 108) | No ICD (n = 29) | p Value |
|---|---|---|---|
| Age at enrollment, yrs | 40 ± 14 | 39 ± 14 | NS |
| Female | 43 (40) | 13 (45) | NS |
| Sustained VT or cardiac arrest | 52 (48) | 4 (14) | <0.001 |
| Syncope (without sustained VT/CA) | 14 (13) | 3 (10) | 0.07 |
| Sustained VT or CA or syncope | 66 (61) | 7 (24) | <0.001 |
| Inducibility at EPS | 46 (43) | 5 (17) | 0.01 |
| Inducibility at EPS without history of sustained VT/CA | 16 (15) | 4 (14) | NS |
| Inducibility at EPS without history of sustained VT/CA/syncope | 11 (10) | 4 (14) | NS |
| Nonsustained VT | 17 (16) | 2 (7) | NS |
| Definite diagnosis of ARVC by original Task Force Criteria | 77 (71) | 14 (48) | 0.02 |
| Diagnostic criteria points (1994 criteria) | 4.3 ± 1.1 | 3.7 ± 1.0 | 0.05 |
| Family history of ARVC | 21 (21) | 5 (21) | NS |
| Antiarrhythmic agents after enrollment | 53 (55) | 8 (42) | NS |
| Beta-blockers | 80 (83) | 14 (74) | NS |
| RVEF (%), mean by MRI | 43 ± 12 | 46 ± 8 | 0.79 |
| LVEF (%), mean by MRI | 58.1 ± 6.1 | 57.7 ± 4.1 | NS |
| T-wave inversion V1 to V3 | 82 (76) | 15 (52) | 0.011 |
| Abnormal SAECG | 53 (62) | 15 (65) | NS |
Values are mean ± SD or n (%). Differences between the 2 groups were observed in prior sustained ventricular arrhythmias, any prior sustained ventricular arrhythmia or syncope, inducibility at EPS, definite diagnosis of ARVC by original Task Force Criteria, diagnostic criteria points (1994 criteria), and T-wave inversion V1 to V3.
ARVC = arrhythmogenic right ventricular cardiomyopathy; CA = cardiac arrest; EPS = electrophysiologic study; ICD = implantable cardioverter-defibrillator; LVEF = left ventricular ejection fraction; MRI = magnetic resonance imaging; RVEF = right ventricular ejection fraction; SAECG = signal-averaged electrocardiogram; VT = ventricular tachycardia.
ENDPOINTS OF VENTRICULAR ARRHYTHMIA AFTER ICD IMPLANTATION
Of the 108 patients who received an ICD, 48 had ventricular arrhythmias treated by the ICD during follow-up (Table 2, Fig. 1). In a multivariate analysis, the only 2 predictors of ICD treatment of ventricular arrhythmias were pre-implantation SMVT or SPVF (p = 0.0029) and T-wave inversions inferiorly (p = 0.0159). There were no sudden deaths in the cohort with ICDs or in the cohort who did not receive ICDs.
TABLE 2.
Predictors of Ventricular Arrhythmias in the 108 Patients With ICDs
| Clinical Characteristics | No Arrhythmia (n = 60) | Arrhythmia (n = 48) | p Value |
|---|---|---|---|
| Age at enrollment, yrs | 41 ± 14 | 38 ± 14 | 0.413 |
| Age at earliest symptom, yrs | 37 ± 14 | 35 ± 15 | 0.609 |
| Female | 27 (45) | 16 (33) | 0.218 |
| Affected (by Task Force Criteria) | 37 (62) | 40 (83) | 0.013 |
| Diagnostic criteria points (1994 criteria) | 4.2 ± 1.0 | 4.3 ± 1.2 | 0.84 |
| Arrhythmic events (VT/VF) before enrollment | 34 (57) | 45 (94) | <0.001 |
| Syncope before enrollment | 14 (23) | 14 (29) | 0.492 |
| Syncope or VT/VF before enrollment | 36 (60) | 46 (96) | <0.001 |
| Family history of sudden death | 22 (42) | 16 (36) | 0.960 |
| Follow-up, yrs | 3.0 ± 1.8 | 3.5 ± 1.5 | 0.114 |
| Heart transplant | 2 (3) | 1 (2) | 1.000 |
| Death | 1 (2) | 1 (2) | 1.000 |
| Antiarrhythmic drug treatment | 19 (39) | 34 (72) | <0.001 |
| Beta-blockers | 41 (84) | 39 (83) | 0.927 |
| RVEF (%) by MRI, mean | 43 ± 11 | 43 ± 13 | 0.334 |
| LVEF (%) by MRI, mean | 59.74 ± 6.42 | 55.65 ± 4.79 | 0.009 |
| Negative T-wave in leads II, III, aVF | 19 (32) | 33 (69) | <0.001 |
| QRS duration in V2, mean | 0.103 ± 0.023 | 0.108 ± 0.021 | 0.055 |
| fQRS40, mean | 116.9 | 126.5 | 0.011 |
| fQRS40 >120 | 16 (33) | 21 (55) | 0.041 |
| VPBs (ventricular total >1,000/24 h) | 25 (58) | 18 (51) | 0.553 |
| Any induced VT or VF | 30 (50) | 33 (69) | 0.050 |
Values are mean ± SD or n (%). Predictors of arrhythmias after ICD implantation included definite diagnosis of ARVC, VT/VF before enrollment, syncope or VT/VF before enrollment, antiarrhythmic drug treatment, negative T-wave in leads II, III, aVF, abnormal SAECG by fQRS40 mean and >140 ms, induced VT/VF. The 2 independent predictors of ICD treatment of ventricular arrhythmias were pre-implantation sustained VT/VF (p = 0.0029) and T-wave inversions inferiorly (p = 0.0159).
EPS = electrophysiologic study; VPB = ventricular premature beat; VF = ventricular fibrillation; other abbreviations as in Table 1.
FIGURE 1. Time to Cardiac Arrhythmia.
Kaplan-Meier graph of time to first cardiac arrhythmia with the groups divided according to their clinical presentation; sustained ventricular tachycardia (VT) or cardiac arrest (CA), syncope without documented sustained arrhythmias, or palpitations/asymptomatic. Event rates in those with sustained VT or CA was 3.91 per year compared with 1.48 per year in those with syncope and 0.79 per year in those asymptomatic or with palpitations. Asymt = asymptomatic; ICD = implantable cardioverter-defibrillator; Palp = palpitations; Sust = sustained; VF = ventricular fibrillation.
ENDPOINT OF LIFE-THREATENING ARRHYTHMIAS (VENTRICULAR TACHYCARDIA ≥240 BEATS/MIN, VENTRICULAR FIBRILLATION, OR SCD)
Twenty-two individuals had the occurrence of rapid SMVT (≥240 beats/min) or SPVF after ICD implantation (Table 3). In a multivariate analysis, only younger age at the time of ICD implantation was predictive of life-threatening ventricular arrhythmias (p = 0.032).
TABLE 3.
Predictors of Life-Threatening VT/VF in the Patients With ICDs
| Clinical Characteristics | No Arrhythmia (n = 60) | Fast Arrhythmia VT/VF (n = 22) | p Value | |
|---|---|---|---|---|
| No Arrhythmia Vs. Fast Arrhythmias | No Fast Arrhythmia Vs. Fast Arrhythmias | |||
| Age at enrollment | 41 ± 14 | 33 ± 15 | 0.036 | 0.032 |
| Age at earliest symptom, yrs | 37 ± 14 | 31 ± 17 | 0.140 | 0.130 |
| Female | 27 (45) | 5 (25) | 0.114 | 0.132 |
| Affected | 37 (62) | 18 (90) | 0.018 | 0.066 |
| Arrhythmic events (VT/VF) before enrollment | 34 (57) | 19 (95) | 0.002 | 0.020 |
| Syncope before enrollment | 14 (23) | 8 (40) | 0.148 | 0.151 |
| Syncope or VT/VF | 36 (60) | 19 (95) | 0.003 | .040 |
| Family history of sudden death | 22 (42) | 7 (37) | 1.000 | 0.970 |
| Follow-up, yrs | 3.0 ± 1.8 | 3.8 ± 1.1 | 0.074 | 0.185 |
| Heart transplant | 2 (3) | 0 (0) | 1.000 | 1.000 |
| Death | 1 (2) | 0 (0) | 1.000 | 1.000 |
| Antiarrhythmic agents | 19 (39) | 14 (70) | 0.018 | 0.169 |
| Beta-blockers | 41 (84) | 17 (85) | 1.000 | 1.000 |
| RVEF (%), mean, MRI | 43 ± 8 | 41 ± 13 | 0.237 | 0.284 |
| LVEF (%), mean, MRI | 59.74 ± 6.42 | 55.67 ± 4.69 | 0.041 | 0.131 |
| Negative T-wave in leads II, III, aVF | 19 (32) | 12 (60) | 0.024 | 0.296 |
| QRS duration in V2 | 0.103 ± 0.023 | 0.106 ± 0.023 | 0.292 | 0.693 |
| Filtered QRS40, mean | 116.9 | 123.4 | 0.172 | 0.552 |
| fQRS40 >120 | 16 (33) | 8 (53) | 0.164 | 0.451 |
| VPBs (ventricular total >1,000/24 h) | 25 (58) | 9 (64) | 0.684 | 0.560 |
| Any induced VT or VF | 30 (50) | 13 (65) | 0.244 | 0.625 |
Values are mean ± SD or n (%). The fourth column compares those with no ventricular arrhythmia with those with only fast ventricular arrhythmias; the fifth column compares those without fast VT/VF with those with fast VT/VF. Predictors of life-threatening VT/VF included younger age at enrollment, VT/VF before enrollment, and syncope or VT/VF before enrollment. The only independent predictor was younger age at the time of ICD implantation (p = 0.032).
ICD TREATMENT OF VENTRICULAR ARRHYTHMIAS DURING FOLLOW-UP
Forty-eight patients had 502 sustained episodes of ventricular arrhythmias, including 489 SMVT and 13 SPVF. The mean cycle length of the SMVT was 317 ± 39 ms and the mean cycle length of the SPVF was 216 ± 40 ms. Of the 489 monomorphic ventricular arrhythmias, 450 were treated with anti-tachycardia pacing (ATP) and 412 (92%) were successfully terminated with ATP. Thirty-eight arrhythmias did not respond to ATP and were treated with a shock. There was no difference in the cycle length of the SMVT successfully treated (320 ± 36 ms) versus those unsuccessfully treated with ATP (320 ± 45 ms) (Fig. 2). Of the SMVT cycle lengths from 200 to 250 ms, 11 of 12 (92%) were successfully treated with ATP, compared with 27 of 32 (84%) with cycle lengths from 251 to 275 ms, 90 of 97 (93%) with cycle lengths of 276 to 300 ms, 115 of 125 (92%) with cycle lengths of 301 to 320 ms, and 159 of 174 (91%) with cycle lengths of >320 ms. Fifty VTs were treated with a shock initially (cycle lengths of 256 ± 40 ms) because of the lack of ATP programming for the rate of the VT. All episodes of SMVT and VF were successfully terminated with a shock.
FIGURE 2. Success of Anti-Tachycardia Pacing in the Termination of Ventricular Tachycardia Stratified by Cycle Length of Arrhythmia in Milliseconds.
Even rapid ventricular tachycardias had a high likelihood of termination with anti-tachycardia pacing.
INAPPROPRIATE THERAPY WITH THE ICD
Seventeen individuals had inappropriate ICD therapy, including 2 for nonsustained ventricular tachycardia, 14 for sinus tachycardia, 7 for atrial fibrillation, 16 for other supraventricular tachycardias, 1 for lead noise, and 3 for oversensing. There was no difference in these groups with regard to age at enrollment, age with earlier symptom(s), sex, appropriate arrhythmic events, history of syncope, use of antiarrhythmic drugs, or beta-blockers.
DISCUSSION
In this analysis of the North American ARVC Registry, ventricular arrhythmias, including those defined as life-threatening, occurred in nearly 50% of patients who received an ICD. Predictors of ICD-treated ventricular arrhythmias were predominantly the occurrence of prior SMVT or SPVF, although T-wave inversions were a predictor of any ventricular arrhythmia in follow-up and a younger age predicted for SPVF. These data support the use of ICDs in ARVC. The observation that there were no deaths in the 29 patients without ICDs indicates that patients without spontaneous ventricular arrhythmias or syncope may have a reasonable prognosis without ICDs. This study also offers guidance for programming an ICD. In patients with ARVC, the arrhythmias were predominantly monomorphic VT. ATP was successful in terminating 92% of the SMVTs, and its success did not depend on the rapidity of the SMVT.
PRIOR STUDIES ON PREDICTORS OF SCD AND ARRHYTHMIAS IN ARVC
Previous studies that evaluated predictors of arrhythmias in ARVC were based on retrospective analyses (11). In a multi-center trial of 132 ICD patients (13 [10%] of whom had prior cardiac arrest, 82 [62%] had sustained ventricular tachycardia, and 21 [16%] had syncope), nearly one-half had ventricular arrhythmias in a follow-up of 39 ± 25 months (8). Predictors of life-threatening arrhythmias (SMVT >240 beats/min or SPVF) were a history of either cardiac arrest or SMVT with hemodynamic compromise, younger age, and left ventricular involvement. Inducible SMVT did not predict SMVT in follow-up. In 42 ICD patients followed for 42 ± 26 months, 33 had ventricular arrhythmias (92% SMVT) (6). Predictors of arrhythmias in the study included spontaneous or induced ventricular arrhythmias. Syncope and family history of ARVC did not predict SMVT or SPVF. Another 60 ICD patients (most with SMVT, SPVF, or syncope) followed for 80 ± 43 months had no predictors of ventricular arrhythmias (5).
In a more recent publication of 106 ICD patients without prior sustained ventricular arrhythmias or SCD (Darvin II), only unexplained syncope was a predictor of ventricular arrhythmias (4).
In a study that included patients without ICDs, 313 patients were followed for 8.5 years, with an annual mortality rate of 0.3% (12). The major risk for death was reduced left ventricular function. In another cohort of ARVC patients, including 61 patients not treated with ICDs, congestive heart failure and left ventricular involvement were predictors for SCD (13). Finally, in a study that included 84 patients with ARVC who did not have clinical SMVT or SPVF, inducibility at electrophysiologic study and non-sustained ventricular tachycardia were independent predictors of ICD therapy for ventricular arrhythmias (14).
APPROPRIATE ENDPOINTS
In most of the ARVC studies, the primary endpoint has been that of ventricular arrhythmias treated by an ICD. However, treated ventricular arrhythmias do not necessarily equate with SCD in the absence of an ICD. In an analysis of randomized, controlled trials in which patients with idiopathic heart failure with ICDs were compared with patients without ICDs, the number of ICD-treated arrhythmias was 2- to 3-fold the SCD risk in the control arm (15). Thus, the life-saving benefit of the ICD is overestimated if equated with any ventricular arrhythmia treated by the ICD.
Although we attempted to more closely approximate SCD by including an analysis restricted to potential life-threatening arrhythmias defined as ≥240 beats/min, this definition may overestimate the incidence of SCD, especially in patients with ARVC who frequently have normal LV function and can tolerate rapid VT for hours or longer. In addition, rapid VT may terminate spontaneously if left untreated.
IMPLICATIONS FOR THE PROGRAMMING OF ICDS
The vast majority of ventricular arrhythmias in ARVC patients in this registry were SMVT (97%), some with very rapid rates. However, in this study, even rapid SMVT (at 200 to 250 ms cycle length) was terminated with ATP. Of those arrhythmias in which ATP was attempted, most patients were successfully treated with ATP, and the success of ATP was not dependent on the cycle length. Thus, ATP should be programmed for all patients with ARVC and should include ATP, even for rapid VT.
CONCLUSIONS
The North American Multidisciplinary Study in Right Ventricular Cardiomyopathy is the first prospectively defined registry to evaluate the risk factors of ar-rhythmias and sudden death in patients with ARVC. Most of the individuals in this registry were treated with an ICD, and approximately one-half received ICD therapy for SMVT, whereas one-fifth of patients were treated for rapid SMVT or SPVF. Risk factors for ventricular arrhythmias were spontaneous ventricular arrhythmias before enrollment and a younger age at time of ICD implantation. When an ICD is placed, ATP is highly successful in terminating SMVT and should be programmed for all SMVT, regardless of heart rate.
Figure 3. CENTRAL ILLUSTRATION.
Arrhythmogenic Right Ventricular Cardiomyopathy Arrhythmogenic right ventricle dysplasia, an inherited disease of the desmosomal proteins, causes sudden cardiac death as a result of re-entrant arrhythmias. ARVC = arrhythmogenic right ventricular cardiomyopathy.
PERSPECTIVES.
COMPETENCY IN MEDICAL KNOWLEDGE 1
VT in patients with ARVC is more often monomorphic than polymorphic.
COMPETENCY IN MEDICAL KNOWLEDGE 2
In patients with ARVC with ICDs, sustained ventricular arrhythmias before device implantation and T-wave inversions in the inferior electrocardiographic leads are independent predictors of ventricular arrhythmias.
COMPETENCY IN PATIENT CARE
Anti-tachycardia pacing successfully terminated most VT episodes regardless of the heart rate and should be programmed for all patients.
TRANSLATIONAL OUTLOOK 1
Additional studies are needed to identify predictors of less common polymorphic VT in patients with ARVC.
TRANSLATIONAL OUTLOOK 2
The efficacy of anti-tachycardia pacing and optimum device settings for patients with ARVC should be evaluated in prospective studies.
Acknowledgments
This research was funded by National Institutes of Health grant U01-HL65594.
ABBREVIATIONS AND ACRONYMS
- ARVC
arrhythmogenic right ventricular cardiomyopathy
- ATP
anti-tachycardia pacing
- ECG
electrocardiogram/ electrocardiography
- ICD
implantable cardioverter-defibrillator
- LV
left ventricular
- RV
right ventricular
- SAECG
signal-averaged electrocardiogram/ electrocardiography
- SCD
sudden cardiac death
- SMVT
sustained monomorphic ventricular tachycardia
- SPVF
sustained polymorphic ventricular fibrillation
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Basso C, Corrado D, Marcus FI, et al. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373:1289–300. doi: 10.1016/S0140-6736(09)60256-7. [DOI] [PubMed] [Google Scholar]
- 2.Marcus FI, Zareba W, Calkins H, et al. Arrhythmogenic right ventricular cardiomyopathy/dysplasia clinical presentation and diagnostic evaluation: results from the North American Multidisciplinary Study. Heart Rhythm. 2009;6:984–92. doi: 10.1016/j.hrthm.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marcus FI, Fontaine G. Arrhythmogenic right ventricular dysplasia/cardiomyopathy: a review. Pacing Clin Electrophysiol. 1995;18:1298–314. doi: 10.1111/j.1540-8159.1995.tb06971.x. [DOI] [PubMed] [Google Scholar]
- 4.Corrado D, Calkins H, Link MS, et al. Prophylactic implantable defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia and no prior ventricular fibrillation or sustained ventricular tachycardia. Circulation. 2010;122:1144–52. doi: 10.1161/CIRCULATIONAHA.109.913871. [DOI] [PubMed] [Google Scholar]
- 5.Wichter T, Paul M, Wollmann C, et al. Implantable cardioverter/defibrillator therapy in arrhythmogenic right ventricular cardiomyopathy: single-center experience of long-term follow-up and complications in 60 patients. Circulation. 2004;109:1503–8. doi: 10.1161/01.CIR.0000121738.88273.43. [DOI] [PubMed] [Google Scholar]
- 6.Roguin A, Bomma CS, Nasir K, et al. Implantable cardioverter-defibrillators in patients with arrhythmogenic right ventricular dysplasia/ cardiomyopathy. J Am Coll Cardiol. 2004;43:1843–52. doi: 10.1016/j.jacc.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 7.Nava A, Bauce B, Basso C, et al. Clinical profile and long-term follow-up of 37 families with arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2000;36:2226–33. doi: 10.1016/s0735-1097(00)00997-9. [DOI] [PubMed] [Google Scholar]
- 8.Corrado D, Leoni L, Link MS, et al. Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2003;108:3084–91. doi: 10.1161/01.CIR.0000103130.33451.D2. [DOI] [PubMed] [Google Scholar]
- 9.Marcus F, Towbin JA, Zareba W, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C): a multidisciplinary study: design and protocol. Circulation. 2003;107:2975–8. doi: 10.1161/01.CIR.0000071380.43086.29. [DOI] [PubMed] [Google Scholar]
- 10.Marcus GM, Glidden DV, Polonsky B, et al. Efficacy of antiarrhythmic drugs in arrhythmogenic right ventricular cardiomyopathy: a report from the North American ARVC Registry. J Am Coll Cardiol. 2009;54:609–15. doi: 10.1016/j.jacc.2009.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Link MS, Wang PJ, Haugh CJ, et al. Arrhythmogenic right ventricular dysplasia: clinical results with implantable cardioverter defibrillators. J Interv Card Electrophysiol. 1997;1:41–8. doi: 10.1023/a:1009714718034. [DOI] [PubMed] [Google Scholar]
- 12.Peters S. Long-term follow-up and risk assessment of arrhythmogenic right ventricular dysplasia/cardiomyopathy: personal experience from different primary and tertiary centres. J Cardiovasc Med. 2007;8:521–6. doi: 10.2459/01.JCM.0000278450.35107.b3. [DOI] [PubMed] [Google Scholar]
- 13.Lemola K, Brunckhorst C, Helfenstein U, et al. Predictors of adverse outcome in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy: long term experience of a tertiary care centre. Heart. 2005;91:1167–72. doi: 10.1136/hrt.2004.038620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhonsale A, James CA, Tichnell C, et al. Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol. 2011;58:1485–96. doi: 10.1016/j.jacc.2011.06.043. [DOI] [PubMed] [Google Scholar]
- 15.Ellenbogen KA, Levine JH, Berger RD, et al. Are implantable cardioverter-defibrillator shocks a surrogate for sudden cardiac death in patients with nonischemic cardiomyopathy? Circulation. 2006;113:776–82. doi: 10.1161/CIRCULATIONAHA.105.561571. [DOI] [PubMed] [Google Scholar]