Abstract
Major cardiovascular disease (CVD) risk factors begin development in childhood and adolescence. Project HeartBeat! studied early development of these risk factors as growth processes. Growth, body composition, sexual maturation, major CVD risk factors, and cardiac structure and function were monitored every 4 months for up to 4 years among 678 children and adolescents (49.1% girls; 20.1% blacks) aged 8, 11, or 14 years at study entry. All resided in The Woodlands or Conroe TX. Interviews were conducted at entry and annually on diet, physical activity, and health history of participants and their families. Data were collected from 1991 to 1995, and study investigators continue data analysis and reporting. Overlap in ages at examination among three cohorts (aged 8–12, 11–15, and 14–18 years at baseline) and use of multilevel modeling methods permit analysis of some 5500 observations on each principal variable for the synthetic cohort from ages 8 to 18 years.
The mixed-longitudinal design provides trajectories of change with age, for total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides; systolic, and fourth-phase and fifth-phase diastolic blood pressure, and left ventricular mass. These trajectories are then related to concurrent measures of multiple indices of body composition and sexual maturation and adjusted for energy intake and physical activity. The data provide valuable insights into risk factor development and suggest a fresh approach to understanding influences on blood lipids, blood pressure, and left ventricular mass during the period of childhood and adolescence, a period of dynamic change in these risk factors.
Introduction
This paper provides the rationale and design of Project HeartBeat! as background to the reports that follow in this supplement to the American Journal of Preventive Medicine.1–13 The concept of a longitudinal study of “growth” of risk factors, as well as development of the research proposal and design and methods of the study, are highlighted.
Concept
Decreasing the public health impact of coronary heart disease, stroke, and other forms of atherosclerotic and hypertensive diseases is widely recognized as an immense global public health challenge.14 The major risk factors—adverse blood lipid profile, high blood pressure, tobacco use, and diabetes—with their behavioral determinants, including dietary imbalance, physical inactivity, and consequent obesity, are themselves epidemic.15 Prevention of the risk factors in the population as a whole depends fundamentally on interventions that begin in childhood and adolescence. Such intervention has been seen as a singularly promising approach to preventing the major cardiovascular diseases (CVDs) of contemporary society.16,17 Public health intervention is needed on an unprecedented scale of scope, intensity, and sustainability if the mounting burden, disparities, and costs related to CVDs are to be contained and ultimately reduced.
Knowledge from epidemiologic studies about blood lipids, blood pressure, and body composition in childhood and adolescence, accumulated in the 1970s and since, was highlighted in this supplement to the American Journal of Preventive Medicine.13 The article noted a strong focus of this research on patterns of variation by age in these risk factors as well as BMI (kg/m2). This work revealed differences among risk factors in their development with age from childhood through and beyond puberty, especially when data were examined across single year-of-age categories rather than broader age groups. Many of these factors (e.g., blood total cholesterol concentration) fluctuate markedly with age during childhood and adolescence, and the true dynamics of change are revealed only when year-to-year or even shorter-term variation can be observed.18 Therefore, understanding of risk factor development, and the opportunities for preventing adverse changes, might be advanced through close monitoring of many individuals over time, from childhood through adolescence.
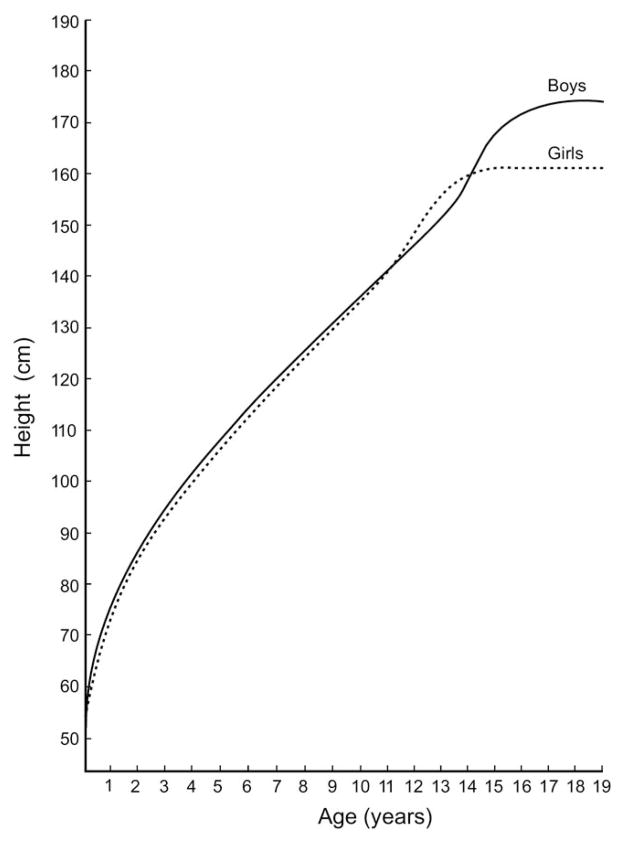
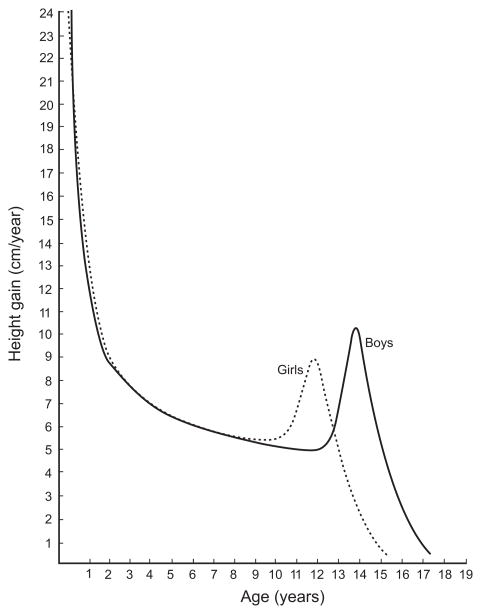
Precedent for such an approach is found in research on human growth, within which auxological anthropometry provides the measurement techniques that underlie the well-recognized standard growth curves for attained height (Figure 1), weight, and BMI by age.19,20 Further, auxology offers deeper insight into growth processes through derivation of the corresponding velocity curves, such as the curve for height velocity, which strikingly demonstrates the adolescent growth spurt (Figure 2).21
Figure 1.
Attained height curves for boys and girls from birth to age 18 years; adapted from Tanner21
Figure 2.
Height velocity curves for boys and girls from birth to age 18 years; adapted from Tanner21
Exploring this approach inspires several important questions: What could be learned from this perspective about the dynamics of change in major CVD risk factors and the possible determinants of change, such as concurrent changes in body size and composition, or sexual maturation? How might such changes be influenced by extrinsic factors, such as nutrition and physical activity? And would the period of the “growth spurt” in CVD risk factors represent a better opportunity for intervention than other times?22 The ideal study design would require observation of subjects frequently enough, for a sufficient period, and over a wide enough range of ages that peak height velocity could be determined for each individual, as well as possible peak velocities, not yet well established, for each of the major risk factors. For the current large-scale epidemiologic study, a more practical goal was adopted, as described below.
Bringing the fields of auxology and cardiovascular epidemiology together in a new approach to the study of risk factor development seemed a potentially fruitful direction toward the ultimate goal of risk factor prevention. Investigators centered in the School of Public Health at the University of Texas Health Science Center at Houston and the Department of Pediatrics at Baylor College of Medicine were joined in the late 1980s by Professor James M. Tanner, a pre-eminent authority in studies of growth and development and Visiting Professor at the School of Public Health, in designing and conducting a study applying this concept.21
Development of the Proposal
In the mid-1980s, a series of school surveys began in the community of The Woodlands TX, some 25 miles north of Houston. The population of 19,146 in 1985 was 91% Caucasian, 6% Hispanic, 1% black, and 2% other race/ethnicity groups. The Woodlands is a planned community with schools, businesses, healthcare facilities, and amenities designed to attract and retain a predominantly middle- to upper-income resident population. Housing was primarily single-family units, although some apartments and Housing and Urban Development program units were included. As part of the development plan, research facilities linked to the Texas Medical Center in Houston were offered inducements to locate in The Woodlands, and in 1982 an Epidemiology Research Center (the EpiCenter) was established there.
By 1985, the EpiCenter began planning a series of general health surveys in The Woodlands schools, with the collaboration of the Conroe Independent School District and The Woodlands Corporation. Impetus for these surveys came from the interest of Reuel A. Stallones, Dean of the School of Public Health and Director of the EpiCenter. This interest was stimulated by the 1954 Kent Paediatric Society report,23 which concluded that:
Although not yet proved, it is possible, or even probable, that Health, no less than disease, may have its specific as well as its predisposing causes and that the true promotion of Health may depend, in the long run, on our acquiring a fuller knowledge concerning them.
Preparatory work over several months laid the groundwork for the first survey. The community became engaged, and the survey protocol was completed, with detailed attention to data collection procedures that included physical and laboratory examination and parental questionnaires. This protocol became the starting point for the procedure manuals of Project HeartBeat!.
The first survey, called the Health Challenge Project, was conducted in Spring 1986 in Sally K. Ride Elementary School and embraced the theme of the National Aeronautics and Space Administration (NASA), with its Houston-area space center. Participation included completing a “Challenger” health coloring book and the opportunity to “draw a picture of health.” Subsequent surveys took place in intermediate, junior high, and high schools in The Woodlands through Spring 1988. These surveys provided a broad picture of health characteristics of the school-aged population of The Woodlands as background for the anticipated proposal.24 Participation rates in the school surveys had been high, especially in the pre–high school grade levels, and an advisory committee representing parents, schools, community management, and healthcare facilities had engaged actively in the work. Together, these assets provided a good foundation for proposing a long-term community-based study with high expectations of successful implementation. In addition, in mid-1986, the school surveys became integrated into the activities of the newly established Southwest Center for Prevention Research, part of the Prevention Research Centers Program newly initiated by the CDC. The center provided funding for the subsequent surveys.
Design and Methods
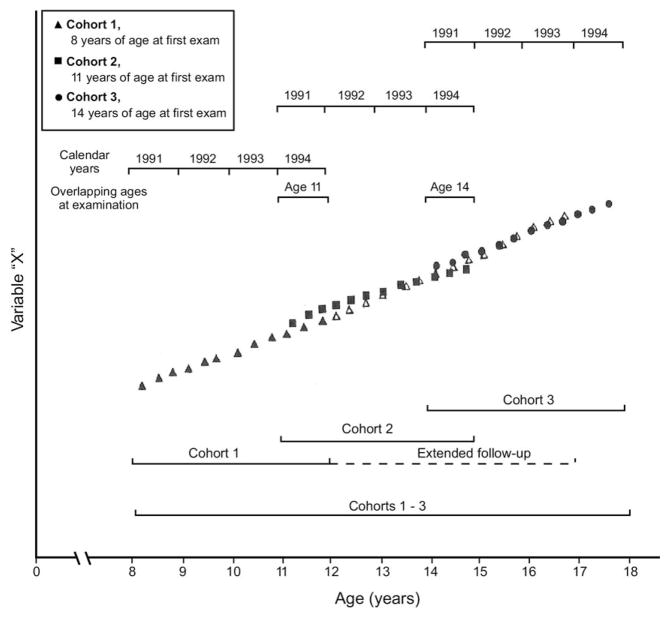
The concept of a growth study from childhood through adolescence required special consideration of the age range of participants and the planned frequency of follow-up examinations. To estimate long-term (e.g., 10-year) patterns or “trajectories” of risk factor change with age within a conventional funding period, the following approach was adopted: Multiple age cohorts would be observed, with starting ages 3 years apart, and at least 4 years of observation for each participant (e.g., observation over ages 8–12, 11–15, and 14–18 years). Overlap in ages at examination between successive cohorts and use of multilevel analytic methods would allow estimation of trajectories for each measure from ages 8 to 18 years within a 4-year period of follow-up assessment.
Practical feasibility dictated a maximum number of three examinations per year, at 4-month intervals, for all participants. Only those aspects of data collection that were especially demanding of participants’ or parents’ time—such as interview questionnaires regarding diet, physical activity, and general health history—would be limited to baseline and anniversary assessments. All other variables, including blood samples and echocardiographs, would be recorded at each examination at intervals of 4 months. This mixed-longitudinal design is schematically represented in Figure 3, and the plan of data collection is shown in Table 1.
Figure 3.
Schematic view of repeated measures in successive age cohorts of a hypothetical variable X, in the synthetic cohort from ages 8 to 18 years, Project HeartBeat!, 1991–1995
Table 1.
Data collection: study variables and frequency of assessment, Project HeartBeat!, 1991–1995
| Dependent variables | |
|---|---|
| Hemodynamics | |
| Blood pressurea | Three times per year |
| Heart ratea | Three times per year |
| Echocardiography | Three times per year |
| Blood lipids | |
| Total cholesterol | Three times per year |
| LDL-cholesterol | Three times per year |
| HDL-cholesterol | Three times per year |
| Triglycerides | Three times per year |
|
| |
| Independent variables | |
|
| |
| Growth | |
| Anthropometry | Three times per year |
| Body composition | Three times per year |
| Bone age | Three times per year |
| Endocrine function | Three times per year |
| Maturation | |
| Tanner stage | Three times per year |
| Menarche | Three times per year |
| Diet and nutrition | |
| Food frequency | Once per year |
| Dietary behavior | Once per year |
| Urinary electrolytes | Once per year |
| Physical activity/fitness | |
| Habits | Once per year |
| VO2 max, aerobic capacity | Once per year |
| Tobacco use | |
| Personal history | Three times per year |
| Family and environmental history | Once per year |
| Cotinine | Once per year |
| Personal history | |
| Health habits | Three times per year |
| Psychosocial characteristics | Once per year |
| Family history | |
| CVD and other health problems in parents, grandparents, others | Once per year |
| Demographics | |
| Household/family composition | Once per year |
| Family characteristics | Once per year |
Blood pressure and heart rate were initially recorded two times per visit, at each of three closely scheduled visits (generally within 2 weeks), on three occasions per year; frequency was later reduced to two closely scheduled visits on three occasions per year (see Design and Methods).
CVD, cardiovascular disease; HDL, high-density lipoprotein; LDL, low-density lipoprotein
It should be noted that the approach to assessment of sexual maturation was as described by Marshall and Tanner, in 1986, a method typically termed Tanner staging.25 Earlier development of this approach is credited to Reynolds and Wines,26,27 writing in 1948 and 1951, on staging methods for girls and boys, respectively. In addition, not all of the variables recorded, and indicated in Table 1, are addressed in this supplement to the American Journal of Preventive Medicine.1–13 For example, VO2 max could not be implemented at the time of entry examination because of technical complications, so no true baseline values were available.
As originally conceived, the study would address the following four specific aims:
to describe and estimate for each individual the “growth curves” (spanning 4 years) for blood lipids, blood pressure, and cardiac structure and function, to include the age-specific levels and the velocity and acceleration of each attribute, analogous to the curves conventionally used in auxology to describe physical growth;
to describe the patterns of change in each of these attributes for the grouped data in multiple successive cohorts with overlapping ages at examination, each consisting of at least 50 boys and 50 girls at each starting age, and combined through multilevel analysis to constitute the “synthetic cohort” from the earliest age at entry to the latest age at follow-up assessment;
to evaluate, for each risk factor, the relationship between age-related change and indicators of physical growth and maturation;
to assess the strength of the independent contributions, if any, of specific nutrient intakes, body composition, or other factors to the observed risk factor changes.
In the course of review of the research proposal, the National Heart, Lung, and Blood Advisory Committee determined that a second component of the study should be provided by expanding representation of black participants. This led to further planning with the Conroe Independent School District to include recruitment from schools located in Conroe TX, some 10 miles north of The Woodlands, where a larger number of minority students were enrolled. With a 13% black population, it was possible to meet the target of enrolling 20% of the Project HeartBeat! study population from this group. Because of budgetary constraints, it was unfortunately not possible to include a Hispanic group as well, which the Conroe population could have provided.
To support the needed recruitment of blacks, the background school surveys previously conducted in The Woodlands were repeated in new target schools in Conroe. For this reason, recruitment of this component of the study population was extended by approximately 1 year. Therefore, at any calendar date, follow-up assessment of these participants would cover a shorter time period than for others. Because of the relatively small sample for this component, distributed in six age–gender strata, analysis of data for blacks would necessarily be limited in comparison with that for nonblacks.
Recruitment of participants for Project HeartBeat! met the intended numbers overall, as described in a previous report.28 Ultimately, in Project HeartBeat!, three cohorts of participants were first examined at ages 8, 11, or 14 years at entry in 1991–1993 and contained a total of 678 individuals with an average of more than eight follow-up examinations each, at 4-month intervals (Table 2). Of the total, 49.1% of the participants were girls; 20.1% (n=136) were blacks, the majority of whom resided in Conroe.
Table 2.
Numbers and percentages of participants at baseline by ethnicity, gender, and cohort (N=678), Project HeartBeat!, 1991–1995a
| Black n (%) | White n (%) | Hispanic n (%) | Asian n (%) | American Indian n (%) | Total n (%) | |
|---|---|---|---|---|---|---|
| Girls | ||||||
| Cohort 1 | 41 (26.5) | 109 (70.3) | 3 (1.9) | 2 (1.3) | 0 (—) | 155 (100) |
| Cohort 2 | 17 (18.3) | 72 (77.4) | 4 (4.3) | 0 (—) | 0 (—) | 93 (100) |
| Cohort 3 | 12 (14.1) | 69 (81.2) | 3 (3.5) | 0 (—) | 1 (1.2) | 85 (100) |
| Boys | ||||||
| Cohort 1 | 38 (23.9) | 113 (71.1) | 4 (2.5) | 3 (1.9) | 1 (0.6) | 159 (100) |
| Cohort 2 | 21 (20.2) | 77 (74.0) | 4 (3.8) | 1 (1.0) | 1 (1.0) | 104 (100) |
| Cohort 3 | 7 (8.5) | 66 (80.5) | 7 (8.5) | 1 (1.2) | 1 (1.2) | 82 (100) |
| Total | 136 (20.1) | 506 (74.6) | 25 (3.7) | 7 (1.0) | 4 (0.6) | 678 (100) |
Mean age in years at baseline examination: Cohort 1, 8.5; Cohort 2, 11.5; Cohort 3, 14.4
Attrition from the intensive follow-up schedule was anticipated to be 10% of participants per year. Some attrition occurred as a result of population mobility, but very few refusals of follow-up assessment occurred. Interruption of follow-up assessments began when closure of data collection approached, so that decreasing numbers of people became eligible for greater numbers of examinations (Table 3). Among people remaining in the community and eligible for as many as nine examinations, for example, more than 90% completed them, and this represented two thirds of the total study population. The mean number of examinations completed was 8.3. Overall retention was especially high among black participants (80.1% compared with 76.8% among nonblacks).
Table 3.
Participation rates in baseline and follow-up examinations, excluding withdrawals,a Project HeartBeat!, 1991–1995
| (1)
|
(2)
|
(3)
|
(4)
|
(5)
|
|
|---|---|---|---|---|---|
| Eligibles
|
Eligibles examined
|
Eligibles examined
|
Eligibles examined
|
||
| Number of examinations | n | % | n | % of (2) | % of total |
| 1+ | 678 | 100.0 | 678 | 100.0 | 100.0 |
| 2+ | 650 | 95.9 | 650 | 100.0 | 95.9 |
| 3+ | 628 | 92.6 | 623 | 99.2 | 91.9 |
| 4+ | 609 | 89.8 | 599 | 98.4 | 88.3 |
| 5+ | 583 | 86.0 | 577 | 99.0 | 85.1 |
| 6+ | 572 | 84.4 | 559 | 97.7 | 82.4 |
| 7+ | 553 | 81.6 | 537 | 97.1 | 79.2 |
| 8+ | 512 | 75.5 | 493 | 96.3 | 72.7 |
| 9+ | 466 | 68.7 | 440 | 94.4 | 64.9 |
| 10+ | 396 | 58.4 | 350 | 88.4 | 51.6 |
| 11+ | 159 | 23.5 | 129 | 81.1 | 19.0 |
| 12+ | 3 | 0.4 | 2 | 66.7 | 0.3 |
| Total | 5809 | 100.0 | 5637 | 97.0 | |
Withdrawals are participants electively discontinuing follow-up assessment because of relocation or refusal.
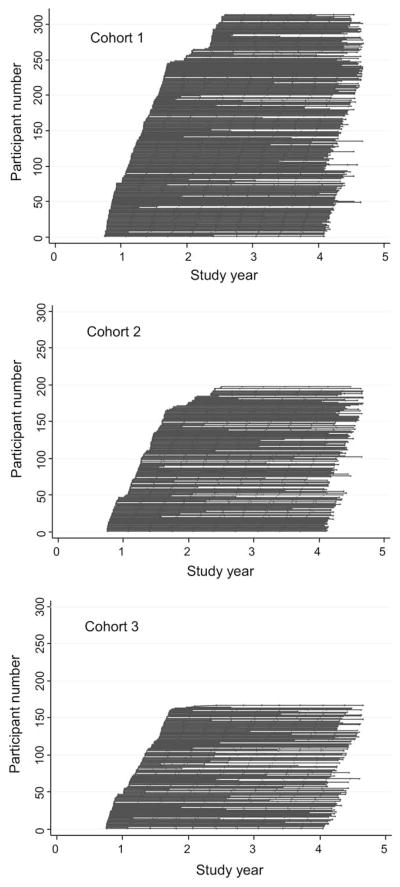
More than 5500 observations had been recorded over the course of follow-up assessment for each of the major variables in the synthetic cohort aged 8–18 years; a graphic summary of the follow-up experience of each cohort up to that date is presented in Figure 4. Each figure presents a history of examination experience by each participant in Project HeartBeat! The linear path over study years for each individual participant is marked by a vertical tick corresponding to each examination. The left contour represents the range of entry examination dates. Censoring of observations (involuntary termination of individual followup assessment) between Years 3 and 4 represents the close of data collection. A striking feature of the graphs is that the great majority of participants remained active with the study until the close of data collection.
Figure 4.
Illustration of follow-up experience of each participant in Cohort 1 (aged 8 years); Cohort 2 (aged 11 years); and Cohort 3 (aged 14 years) at entry, by study year, in Project HeartBeat!, 1991–1995. Each horizontal line represents one participant; each vertical tick represents one completed examination, from entry to the close of data collection.
Following extensive data editing and review for quality assurance, Project HeartBeat! investigators have continued to collaborate in data analysis and reporting to the present, and their work to date culminates in the present series of articles.1–13 The data elements recorded in Project HeartBeat! and their scheduled frequencies are indicated in Table 1. Methods of data collection, management, and analysis are extensively documented in Project HeartBeat! study manuals and are described in the accompanying reports as appropriate. The manuals are available on request from the corresponding author. General approaches to data collection included standardized training and certification of observers, coupled with steering committee review of all outlying values, and other measures to assure a high level of data quality.
Data collected at baseline and at each examination at 4-month intervals included the variables shown in Table 1. The original plan for blood pressure and heart rate measurement called for three visits in rapid succession (all within 2 weeks) with two readings per visit, in order to obtain the best practical estimate of blood pressure and heart rate for each examination. Early in the study, a report29 demonstrated that precision of blood pressure estimates was greatly improved by having two visits rather than one, but not by having three visits rather than two. Accordingly, the original protocol was continued for baseline visits only thereafter, and all follow-up visits were limited to two occasions, within 2 weeks.
Models to describe change in risk factors and other measures, as well as relationships among the variables of interest, are estimated by means of a multilevel statistical modeling approach and the use of MLwiN software, which accommodates the features of repeated measurements at the individual level and multiple age cohorts in this study.30–32 Methodologic aspects of data analysis are described in detail in a companion report.1 The results of these analyses for each of the major risk factors, alone and in combination with related variables, are the main focus of the subsequent articles in this supplement to the American Journal of Preventive Medicine.1–13
Both the University of Texas Health Science Center at Houston and Baylor College of Medicine IRBs reviewed and approved the resulting research proposal. The CDC approved the continuing analysis of the data. Consent of parents and assent of their children to participate in Project HeartBeat! were also obtained and documented.
Conclusion
Project HeartBeat! was successful in bridging cardiovascular epidemiology and auxology to study development of blood lipids, blood pressure, and cardiac structure and function as growth processes. The study design was effective in compressing observation time to 4 years while generating a synthetic cohort spanning ages 8 to 18 years. A subsequent report in this supplement to the American Journal of Preventive Medicine1 describes the analytic approach to achieving this goal, including testing for cohort differences in measurement data, which in general support pooling data across cohorts.
The process of establishing the background information for the study community and engaging the support of parents, participants, and community organizations, especially the schools, assured the feasibility of conducting a study highly demanding of participant time. Through these efforts and very close rapport of staff with participants and their parents, a high level of retention was achieved.16 Participation was rewarding for them in terms of very warm relationships among participants and staff and the participants’ sense of satisfaction in contributing to science and studying their own growth.
Limitations of the project include lack of data for the tri-ethnic population that Texas, and the Conroe community in particular, could have provided. The original concept of a tri-ethnic study was discouraged by the funding agency on the basis of cost. Numbers of blacks at the older school ages were insufficient to permit rigorous comparative analysis with the non-Hispanic whites in the study population. However, all age-eligible students in the targeted schools, whatever their race or ethnicity, were recruited and enrolled, subject to willingness to participate.
In addition, funds were not initially available for genetic studies or for certain biochemical determinations of interest, such as blood glucose and insulin. Subsequently, genotyping of girls was supported through a grant from the Women’s Fund, and more recently, of boys also, with support from NIH. Self-report on interview items may entail reporting error, but this was thought to be limited to some degree by parental participation in child and adolescent interviews. Data were evaluated for reliability as, for example, when improbable values of caloric intake were calculated on the basis of the dietary recall interview; in such circumstances, infrequent though they were, the data were excluded from analysis.
All study data remain available, as are buffy coat samples from the baseline examination and both plasma aliquots and videotaped echocardiographs from each of some 5500 examinations in all. The investigators remain active and engaged in the continuing work with the data. Further analyses will address predictive models in which changes in body size and composition are related to subsequent changes in both levels and rates of change, or growth velocities, of blood lipids, blood pressure, and measures of cardiac structure and function. New research proposals for use of existing data and materials are in various stages of preparation, and the possibility remains of further follow-up assessments of Project HeartBeat! participants, who are now aged approximately 25–30 years.
Acknowledgments
Project HeartBeat! has been supported by the following research awards from NIH and the CDC: UO1 HL41166; 1 RO3 HL57101; 1 RO3 HL59223 (cardiac development); and CDC contract PO# 0009966385, Intergovernmental Personnel Agreement 00IPA24501, and Cooperative Agreement U48/CCU609653. Additional support from the Compaq Computer Corporation and the University of Texas Health Science Center at Houston, School of Public Health, is also gratefully acknowledged.
The authors wish to recognize the invaluable contributions of each Project HeartBeat! participant and family. Cooperation of the Conroe Independent School District and the generous support of The Woodlands Corporation are deeply appreciated. The Woodlands and Conroe Advisory Committees have assisted greatly in the planning and conduct of the project. The many co-investigators, consultants, and staff who have contributed to the project from its inception are also recognized with deep appreciation, especially Professor James M. Tanner.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC.
No financial disclosures were reported by the authors of this paper.
References
- 1.Harrist RB, Dai S. Analytic methods in Project HeartBeat! Am J Prev Med. 2009;37(1S):S17–S24. doi: 10.1016/j.amepre.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dai S, Fulton JE, Harrist RB, Grunbaum JA, Steffen LM, Labarthe DR. Blood lipids in children: age-related patterns and association with body-fat indices: Project HeartBeat! Am J Prev Med. 2009;37(1S):S56–S64. doi: 10.1016/j.amepre.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Fulton JE, Dai S, Grunbaum JA, Boerwinkle E, Labarthe DR. Effects of apolipoprotein E genotype on blood cholesterol in adolescent girls. Am J Prev Med. 2009;37(1S):S78–S85. doi: 10.1016/j.amepre.2009.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai S, Harrist RB, Rosenthal GL, Labarthe DR. Effects of body size and body fatness on left ventricular mass in children and adolescents: Project HeartBeat! Am J Prev Med. 2009;37(1S):S97–S104. doi: 10.1016/j.amepre.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eissa MA, Wen E, Mihalopoulos NL, Grunbaum JA, Labarthe DR. Evaluation of AAP guidelines for cholesterol screening in youth: Project HeartBeat! Am J Prev Med. 2009;37(1S):S71–S77. doi: 10.1016/j.amepre.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Labarthe DR, Dai S, Day RS, Fulton JE, Grunbaum JA. Findings from Project HeartBeat!: their importance for CVD prevention. Am J Prev Med. 2009;37(1S):S105–S115. doi: 10.1016/j.amepre.2009.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Day RS, Fulton JE, Dai S, Mihalopoulos NL, Barradas DT. Nutrient intake, physical activity, and CVD risk factors in children: Project HeartBeat! Am J Prev Med. 2009;37(1S):S25–S33. doi: 10.1016/j.amepre.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steffen LM, Dai S, Fulton JE, Labarthe DR. Overweight in children and adolescents associated with TV viewing and parental weight: Project HeartBeat! Am J Prev Med. 2009;37(1S):S50–S55. doi: 10.1016/j.amepre.2009.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fulton JE, Dai S, Steffen LM, Grunbaum JA, Shah SM, Labarthe DR. Physical activity, energy intake, sedentary behavior, and adiposity in youth. Am J Prev Med. 2009;37(1S):S40–S49. doi: 10.1016/j.amepre.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altwaijri YA, Day RS, Harrist RB, Dwyer JT, Ausman LM, Labarthe DR. Sexual maturation affects diet–blood total cholesterol association in children: Project HeartBeat! Am J Prev Med. 2009;37(1S):S65–S70. doi: 10.1016/j.amepre.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Labarthe DR, Dai S, Fulton JE, Harrist RB, Shah SM, Eissa MA. Systolic and fourth- and fifth-phase diastolic blood pressure from ages 8 to 18 years: Project HeartBeat! Am J Prev Med. 2009;37(1S):S86–S96. doi: 10.1016/j.amepre.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Eissa MA, Dai S, Mihalopoulos NL, Day RS, Harrist RB, Labarthe DR. Trajectories of fat mass index, fat free–mass index, and waist circumference in children: Project HeartBeat! Am J Prev Med. 2009;37(1S):S34–S39. doi: 10.1016/j.amepre.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labarthe DR, Dai S, Harrist RB. Blood lipids, blood pressure, and BMI in childhood and adolescence: background to Project HeartBeat! Am J Prev Med. 2009;37(1S):S3–S8. doi: 10.1016/j.amepre.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 14.Labarthe DR. Epidemiology and prevention of cardiovascular diseases: a global challenge. Gaithersburg MD: Aspen Publishers, Inc; 1998. [Google Scholar]
- 15.Stamler J, Neaton JD, Garside DB, Daviglus ML. Current status: six established major risk factors—and low risk. In: Marmot M, Elliott P, editors. Coronary heart disease epidemiology: from aetiology to public health. 2. Oxford: Oxford University Press; 2005. pp. 32–70. [Google Scholar]
- 16.WHO Expert Committee. Prevention in childhood and youth of adult cardiovascular diseases: time for action. Geneva: WHO; 1990. Technical Report Series 792. [PubMed] [Google Scholar]
- 17.National Heart, Lung, and Blood Institute. Report of the Task Force on Research in Epidemiology and Prevention of Cardiovascular Diseases. Bethesda MD: USDHHS, Public Health Service, NIH; 1994. [Google Scholar]
- 18.Labarthe DR, Nichaman MZ, Harrist RB, Grunbaum JA, Dai S. The development of cardiovascular risk factors from ages 8 to 18 in Project HeartBeat!: study design and patterns of change in plasma total cholesterol concentration. Circulation. 1997;95:2636–42. doi: 10.1161/01.cir.95.12.2636. [DOI] [PubMed] [Google Scholar]
- 19.Eveleth PB, Tanner JM. Worldwide variation in human growth. 2. Cambridge: Cambridge University Press; 1990. [Google Scholar]
- 20.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 21.Tanner JM. Foetus into man. Physical growth from conception to maturity. London: Open Books Publishing, Ltd; 1978. [Google Scholar]
- 22.Aboderin I, Kalache A, Ben-Shlomo Y, et al. Life course perspectives on coronary heart disease, stroke and diabetes: key issues and implications for policy and research. Geneva: WHO; 2002. [Google Scholar]
- 23.Kent Paediatric Society. A study in the epidemiology of health. Being an investigation into the epidemiology and causation of health among 10–11 year old schoolchildren in the Borough of Bexley, Kent. Buxleyheath Kent: The Health Department; 1954. [Google Scholar]
- 24.McPherson RS, Nichaman MZ, Kohl HW, Reed DB, Labarthe DR. Intake and food sources of dietary fat among schoolchildren in The Woodlands, Texas. Pediatrics. 1990;86:520–6. [PubMed] [Google Scholar]
- 25.Marshall WA, Tanner JM. Puberty. In: Falkner F, Tanner JM, editors. Human growth. 2. Vol. 2. New York: Plenum; 1986. [Google Scholar]
- 26.Reynolds EL, Wines JV. Individual differences in physical changes associated with adolescence in girls. Am J Dis Child. 1948;75:329–50. doi: 10.1001/archpedi.1948.02030020341006. [DOI] [PubMed] [Google Scholar]
- 27.Reynolds EL, Wines JV. Physical changes associated with adolescence in boys. Am J Dis Child. 1951;82:529–47. doi: 10.1001/archpedi.1951.02040040549002. [DOI] [PubMed] [Google Scholar]
- 28.Grunbaum JA, Labarthe DR, Ayars C, Harrist R, Nichaman MZ. Recruitment and enrollment for Project HeartBeat!: achieving the goals of minority inclusion. Ethn Dis. 1996;6(3–4):203–12. [PubMed] [Google Scholar]
- 29.Gillman MW, Cook NR. Blood pressure measurement in childhood epidemiological studies. Circulation. 1995;92:1049–57. doi: 10.1161/01.cir.92.4.1049. [DOI] [PubMed] [Google Scholar]
- 30.Goldstein H. Multilevel statistical models. 2. London: Edward Arnold; 1995. [Google Scholar]
- 31.Harrist RB, Kimball KT. Multilevel analysis for a mixed longitudinal design. In: Hauspie R, Lindgren G, Falkner F, editors. Essays on auxology. Welwyn Garden City UK: Castlemead Publications; 1995. pp. 53–68. [Google Scholar]
- 32.Rabash J, Woodhouse G. MLn command reference, version 1.0. London: Multilevel Models Project, Institute of Education, University of London; 1995. [Google Scholar]