Abstract
Objectives
To characterize whether single parent households are associated with pediatric asthma-related repeat healthcare utilization and to examine family-level psychosocial variables that may explain this relationship.
Methods
We analyzed a prospective cohort of 526 children aged 1–16 years hospitalized for asthma or bronchodilator-responsive wheezing whose caregivers self-reported their marital status. Those reporting being “single” were considered the at-risk category. The outcome was repeat asthma-related utilization (emergency room (ER) revisit or hospital readmission) within 12 months. We assessed, a priori, four psychosocial variables (household income, caregiver risk of psychological distress, ratio of in-home children to adults, and regular attendance at childcare or a secondary home).
Results
Among all children enrolled in the cohort, 40% returned to the ER or hospital for asthma within 12 months. Of all caregivers, 59% self-identified as single. Single status was significantly associated with each psychosocial variable. Children in households with lower incomes and higher ratios of children to adults were both more likely to return to the ER or hospital than children with higher incomes and lower ratios, respectively (each p<0.05). Patients in single parent households were significantly more likely to reutilize than those in married parent households (OR 1.44, 95% CI 1.00–2.07, p<0.05). When adjusted for income, the relationship between single parent households and reutilization became non-significant.
Conclusions
Children admitted for asthma from single parent households were more likely to have asthma-related reutilization within 12 months than children from homes with married parents. This was driven, in large part, by underlying differences in household income.
Keywords: Distress, family structure, hospitalization, income, pediatric, psychosocial factors
Introduction
In 2009, the Census Bureau reported that 40% of children in the United States were born to unmarried mothers [1]. Children living in single parent households are nearly twice as likely to have a physician diagnosis of asthma as children living in households with married parents [2,3]. Although the association between caregiver marital status and asthma prevalence has been examined, the influence of marital status on asthma-related morbidity is not well understood. One study found that children from single parent households filled fewer prescriptions for controller medications and were more likely to have their asthma rated as severe. This study also associated a higher number of children living in the home with fewer prescriptions filled and an increased likelihood of asthma exacerbations [4]. While many have examined the importance of the urban context, including poverty and race, on child asthma [5-7], no prior study has focused on caregiver marital status, specifically single parent households and asthma morbidity, particularly among children ill enough to be hospitalized.
Several psychosocial factors, such as lower household income, are more common among single parents and also play a role in asthma [3,8-10]. Indeed, poor children are more likely to have an asthma diagnosis, require hospitalization and seek care in the emergency room (ER) than children living above the poverty level [2,11-13]. Caregiver mental health has also been related to both single-parenthood and asthma morbidity. Children whose caregivers have a mental illness are roughly two times more likely to experience an asthma hospitalization [14]. Moreover, having a caregiver with major depressive disorder is associated with more lifetime asthma exacerbations [15]. We postulate that a higher ratio of children to adults in the home and variation in the child’s care environments may also shape asthma morbidity. A child who spends time outside the home may have more adults that provide asthma-related care (e.g. control their medication usage), a known risk factor for poor outcomes [16].
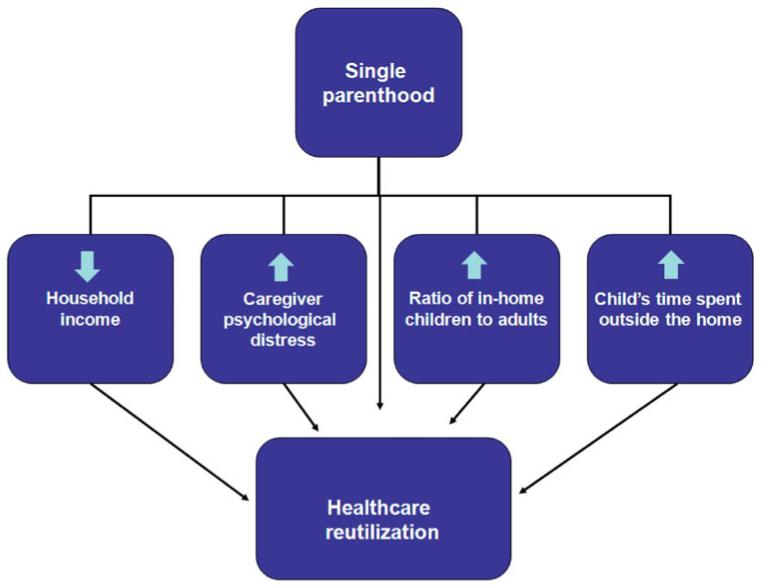
To the best of our knowledge, no study has focused on the association of living in a single parent household and subsequent asthma morbidity in an inpatient population. Furthermore, the identification of potentially explanatory underlying household factors might lead to effective interventions to support parents caring for children with chronic conditions. Therefore, our objective was to incorporate single parent status and potentially associated psychosocial factors, chosen a priori, into a single model of the stressors that may impact a child’s asthma morbidity (Figure 1). We hypothesized that children hospitalized with asthma or bronchodilator-responsive wheezing whose parents self-identify as single would have higher healthcare reutilization (asthma-related ER revisit or repeat hospitalization) within 12 months compared to children from homes with married parents. We further hypothesized that certain psychosocial characteristics of these households, including lower income, increased caregiver risk of psychological distress, increased ratio of children to adults and increased child’s time spent outside the home might explain the association between living in a single parent household and asthma-related morbidity.
Figure 1.
Conceptual model of single marital status and a proposed pathway to asthma-related healthcare reutilization. *Downward arrow indicates “decreased”, upward arrow indicates “increased”.
Methods
Study design and data collection
We analyzed data from a cohort of children, aged 1–16 years, admitted to Cincinnati Children’s Hospital Medical Center (CCHMC). Eligible children, admitted through the ER or directly to the inpatient units, were diagnosed with asthma or bronchodilator-responsive wheezing by the admitting physician and begun on CCHMC’s asthma treatment protocol. The primary caregiver of each eligible child was approached during the hospitalization at a time dependent upon availability of research staff. Children were excluded if they had comorbid pulmonary or cardiac conditions (e.g. cystic fibrosis, congenital heart disease) or were removed from the asthma treatment protocol during their hospital stay. To limit loss to follow-up, children were excluded if they lived outside of CCHMC’s 8-county primary service area.
Trained research coordinators conducted a face-to-face survey during the inpatient stay. Responses were entered into an electronic data capture system and checked for completeness following enrollment. Recruitment took place for a full year (April 2008–May 2009) to account for seasonal variation. Sixty percent of all the children eligible for the study and admitted on days staffed by research personnel were enrolled.
Outcome
The primary outcome was asthma-related reutilization, defined as any ER revisit or repeat hospitalization for asthma or bronchodilator-responsive wheezing within 12 months of the index admission. This was treated as a dichotomous outcome variable (yes/no) and was captured prospectively using the hospital’s electronic billing system. This data tracking method was validated through a review of 10% of the charts chosen randomly (kappa = 1.0).
Predictor variables
Children were categorized into three groups according to the self-identified marital status of the primary caregiver: “single”, “married”, or “other (divorced, widowed or separated)”. The data did not allow for delineation of cohabitating caregivers. Of the 601 children enrolled, we analyzed the 526 whose parents identified themselves as single or married. We excluded those in the “other (divorced, widowed or separated)” category due to the small sample (n = 68, 11%) and the inability to distinguish between the subcategories. We also excluded those whose caregiver did not respond to the question (n = 7, 1%).
Four psychosocial variables were conceptualized as potential contributors to the impact of a single parent household on asthma morbidity. Self-reported annual household income was collected as a categorical variable (<$15 000, $15 000–29 999, $30 000–59 999, $60 000–89 999 and ≥$90 000). Caregiver psychological distress was measured by parental score on the 6-item Kessler 6 (K6) scale [17,18] designed for use in the National Health Interview Survey (NHIS). The K6 has been validated to discriminate respondents at risk of psychological distress, treated as any Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) diagnosis other than a substance use disorder. The ratio of in-home children to adults was calculated based upon the number of each reported. A description of the day-to-day movement of the child was evaluated by dichotomous response (yes/no) to the question “Does the patient spend time in more than one household or regularly go to childcare for one or more days per week?”.
Statistical analyses
Distributions of the variables were examined. Associations were assessed between marital status, the four psychosocial variables and healthcare reutilization. Bivariate analyses used Chi-square statistics for categorical variables and the student’s t-test for continuous variables. Annual household income was initially analyzed in its original five categories. Analyses relating income to reutilization revealed a similar effect of the first three income categories (income <$60 000) on healthcare reutilization. We therefore dichotomized annual house-hold income to above and below $60 000 in regression analyses with income <$60 000 defined as the risk category. Caregiver psychological distress, defined by the parent’s score on the K6, was examined as a continuous variable (0–24). Higher scores on the K6 indicate higher risk for psychological distress. To aid in interpretation, we also noted that the effect size on reutilization comparing the 90th to the 10th percentile of K6 scores. The ratio of in-home children to adults was analyzed in quartiles for bivariate analysis which indicated a similar effect of the lowest three quartiles (ratio of <2:1) on the outcome. A cut-point of 2:1 was, therefore, used in regression analyses with a ratio of ≥2:1 defined as the risk category. A child’s time spent outside the home was analyzed as a dichotomous variable; having weekly childcare or a secondary household was the risk category.
Multivariable logistic regression was used to adjust for potential confounders and to determine the independent contributions of a single parent household and the psychosocial variables to the outcome. We opted not to add race as a covariate to these models given the co-linearity with income (~90% of African Americans had income <$60 000). Caregiver age was explored as a possible covariate given that it was significantly associated with marital status. It was not included in final models, however, given that it lacked a significant association with reutilization.
Marital status as a predictor of reutilization was examined first (Model 1). Each psychosocial variable significantly associated with reutilization during bivariate analyses was individually entered into a model with marital status (Models 2–4). The change in the relationship between marital status and the outcome was examined as each variable was entered. Model 5 included single marital status and each psychosocial variable; Model 6 removed household income.
Analyses were performed using Statistical Analysis System (SAS) software version 9.2 (Cary, NC.). This study was approved by the CCHMC Institutional Review Board. Each participant signed informed consent prior to enrollment.
Results
Study population
The mean age was 5.9 (SD 4.0) years. Most children were male, African American, publically insured or self-pay, and had mothers with high school and/or some college education (Table 1); 90% of caregiver respondents were female. Forty percent of the cohort either returned to the ER or was re-hospitalized for asthma within 12 months of enrollment. There were no significant differences in age, gender, race, insurance or likelihood of reutilization between eligible children that were enrolled and eligible children that were not. Of the 526 meeting our inclusion criteria, 59% of primary caregivers self-identified as single. Nearly three-quarters reported an income <$60 000 and nearly a third reported an income <$15 000. More than 30% of caregivers reported aratio of in-home children to adults of ≥2:1. Nearly half of children regularly attended childcare or spent time in a secondary household.
Table 1.
Sample population characteristics (N=526).
| Characteristic | % |
|---|---|
| Age (years) | |
| 1–4 | 54 |
| 5–10 | 36 |
| 11–16 | 10 |
| Sex | |
| Male | 64 |
| Race | |
| Black/African American | 53 |
| White/Caucasian | 39 |
| Other | 8 |
| Maternal education | |
| High school or less | 19 |
| Some college | 52 |
| College graduate or greater | 28 |
| Insurance status | |
| Public/self-pay | 60 |
| Healthcare reutilization in 12 months | |
| Yes | 40 |
| Marital status | |
| Single | 59 |
| Married | 41 |
| Annual household income ($) | |
| <15 000 | 30 |
| 15 000–29 999 | 24 |
| 30 000–59 999 | 19 |
| 60 000–89 999 | 13 |
| >90 000 | 14 |
| Caregiver psychological distress | |
| K6 Mean (SD) | 4.9 (4.6)a |
| Ratio of in-home children to adults | |
| ≥2.0 | 34 |
| <2.0 | 66 |
| Child’s time spent outside the home | |
| Yes | 49 |
Mean (SD).
Relationship between marital status and psychosocial stressors
Single parent households differed significantly from married parent households across each psychosocial variable (Table 2). Compared to married parent households, annual household income for single parent households was twice as likely to be <$60 000 (94% versus 40%, p<0.001) and six times more likely to be <$15 000 (46% versus 7%, p<0.001). Single parents also had a 34% higher mean K6 score than married parents (5.6 versus 3.7, p = 0.001). They were also more likely than married parents to have a ratio of in-home children to adults that was ≥2:1 (46% versus 18%, p<0.001). Finally, children from single parent households were more likely to regularly spend time outside the home than children from married parent households (57% versus 39%, p<0.001).
Table 2.
Relationships between marital status and psychosocial variables.
| Single | Married | p Value* | ||
|---|---|---|---|---|
| Annual household income (%<$60 000) | 73 | 94 | 40 | <0.001 |
| Caregiver risk of psychological distress [mean (SD)] | 4.9 | 5.6 (4.7) | 3.7 (4.3) | 0.001 |
| Ratio of in-home children to adults (% ≥2:1) | 35 | 46 | 18 | <0.001 |
| Child’s time spent outside the home (% yes) | 49 | 57 | 39 | <0.001 |
Chi-square analyses for each association with the exception of for risk of psychological distress (student’s t-test).
Associations between predictors and asthma-related healthcare reutilization
Table 3 shows associations between marital status and each of the psychosocial variables with asthma-related healthcare reutilization. Children from single parent households were significantly more likely to return to the ER or hospital for asthma than children from homes with married parents (43% versus 34%, p = 0.04). Children from homes with annual household incomes <$60 000 were also significantly more likely to reutilize than those with higher incomes (45% versus 26%, p<0.001). Similarly, higher K6 scores, indicating higher risk of psychological distress, were significantly associated with reutilization (p = 0.03). Children from homes with a higher ratio of in-home children to adults (≥2:1) were more likely to reutilize (46% versus 36%, p = 0.02). A child’s time spent outside the home was not associated with healthcare reutilization and was, therefore, not examined further.
Table 3.
Bivariate associations of marital status and psychosocial stressors with asthma-related healthcare reutilization within 12 months.
| Healthcare reutilization |
||
|---|---|---|
| Variable | N (%) | p Value* |
| Overall | 208 (40) | |
| Marital status | ||
| Single | 134 (43) | 0.04 |
| Married | 74 (34) | |
| Annual household income ($) | ||
| <15 000 | 70 (45) | <0.001 |
| 15 000–29 999 | 56 (45) | |
| 30 000–59 999 | 45 (45) | |
| 60 000–89 999 | 18 (28) | |
| >90 000 | 17 (24) | |
| Ratio of in-home children to adults | ||
| ≥2.0 | 82 (46) | 0.02 |
| <2.0 | 122 (36) | |
| Child’s time spent outside the home | ||
| Yes | 104 (40) | 0.5 |
| No | 100 (38) | |
| Caregiver risk of psychological distress | ||
| (K6 score mean (SD)) | ||
| Reutilization | 5.5 (5.1) | 0.03 |
| No reutilization | 4.5 (4.3) | |
Chi-square analyses for each association with the exception of for risk of psychological distress (student’s t-test).
After adjusting for child age and gender, children whose parents self-identified as single were still 1.44-fold (95% CI 1.00–2.07) more likely than children of married parents to return for an asthma-related ER visit or hospitalization (Table 4, Model 1). This relationship, after adjustment, was statistically significant. Model 2 illustrated that single parent household status was no longer significant upon adjustment for annual household income. Indeed, the association between marital status and reutilization was virtually eliminated while income remained significantly associated with the outcome (OR 2.29, 95% CI 1.38–3.82). In Model 3, caregiver risk of psychological distress, measured on a continuous 0–24 scale, was marginally associated with the outcome. To clarify this observation, a child with a caregiver with a K6 score at the 90th percentile (K6 score of >11) was 1.54-fold (95% CI, 1.00–2.33) more likely to reutilize than one with a caregiver in the 10th percentile (K6 = 0) even after adjustment for single parent household status. In Model 4, the ratio of inhome children to adults was not significantly associated with the outcome. In all three of these models (2–4), the effect of single parent household status became non-significant. A multivariable model combining single parent household status with each of the three psychosocial variables included in this analysis suggested that household income drove most of the observed effect and was the strongest independent predictor of reutilization (Model 5). Removing income from Model 5 suggested caregiver risk of psychological distress may also have had a marginal adverse effect on risk of reutilization (Model 6).
Table 4.
Associations between marital status and psychosocial variables and healthcare reutilization within 12 months using multivariable logistic regression.
| Strain variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
|---|---|---|---|---|---|---|
| Single parent | 1.44 (1.00–2.07) | 1.02 (0.66–1.58) | 1.37 (0.95–2.00) | 1.30 (0.89–1.91) | 0.96 (0.61–1.50) | 1.23 (0.83–1.81) |
| Annual household income | – | 2.29 (1.38–3.82) | – | – | 2.02 (1.20–3.41) | – |
| Caregiver psychological distress | – | – | 1.04 (0.99–1.08) | – | 1.03 (0.99–1.07) | 1.04 (1.00–1.08) |
| Ratio of in-home children to adults | – | – | – | 1.40 (0.95–2.05) | 1.33 (0.90–1.08) | 1.43 (0.97–2.12) |
All models present odds ratios adjusted for age and gender. Annual household income was categorized (<$60 000 and ≥$60 000). Caregiver psychological distress (K6 score) was analyzed as a continuous variable. Ratio of in-home children to adults was categorized (<2:1 and ≥2:1).
Discussion
Adjusting for age and gender, children with asthma whose parents self-described themselves as single had more than a 40% increase in the odds of returning to the hospital within 12 months when compared to children from homes with married parents. Lower household income appeared to explain this relationship: lower income was both more common in single parent households and also a powerful, independent predictor of healthcare reutilization. Caregiver risk of psychological distress was higher among those described as single, but was less strongly associated with healthcare reutilization in multivariable models. A higher ratio of in-home children to adults was more common in homes with caregivers self-identified as single, but was not associated with asthma-related healthcare reutilization. Single parents face substantial parenting demands and life stressors which may have particularly adverse effects on care for a child with asthma [19]. There are potentially less time, emotional and material resources available to commit to chronic asthma care. In addition, children in single parent households may experience social stressors which could contribute to the physiology of asthma and asthma morbidity [20].
Nearly 60% of children in this hospitalized asthma cohort lived in households headed by single parents. Prior research identified children of single mothers at increased risk of parent-reported asthma [19], poorer chronic care of asthma and parental rating of asthma as more severe [4]. Our study extends these findings by identifying higher rates of single parent household status in an inpatient asthma cohort than in the general population, and by linking single parenthood to increased healthcare reutilization.
Prior research has identified that children of parents with competing priorities, including concerns about relationships or paying bills, are more likely to have poor adherence to asthma controller medications and to have suboptimal asthma control [21]. We sought to identify stressors, particularly those relevant to single parent households, which may complicate a parent’s ability to care for a child with asthma. We explored four psychosocial variables hypothesized to be related to both single parent households and reutilization. Each potential stressor was more prevalent in single parent households: lower household income, increased caregiver psychological distress, higher ratio of in-home children to adults and increased child’s time spent outside the home. Lower income, and to a lesser extent, increased caregiver risk of psychological distress and higher ratio of in-home children to adults, were each associated with asthma-related reutilization. We also found that much of the effect of single parent household status on reutilization was attributable to reported household income. Caregiver psychological distress may play a lesser but still important role in the pathway between single parent household status and asthma-related reutilization.
Disparities in pediatric asthma outcomes are clearly linked to poverty, with low income associated with an increased likelihood of asthma diagnosis [12] and longer hospital stays [11]. Our findings also support the notion that households headed by single parents are at higher likelihood of living in poverty [22]. Our findings highlight that not only are children living in poverty at risk for asthma, but disproportionate healthcare reutilization is experienced by children with modest financial resources (annual household income <$60 000). Our data reveal a significant increase in reutilization as annual household income falls below $60 000 (Table 3). Although we cannot, with our data, illustrate the direct impact of income below $60 000, lower household income, in general, has been shown to translate to fewer financial resources available for quality housing, transportation to appointments or other expenses related to chronic asthma care. Lower income may also be a proxy for related factors including environmental exposures (e.g. allergens, environmental tobacco smoke and air pollution), access to healthcare, health beliefs and literacy [7,12,23]. It is also possible that single parent households experience poverty or these associated risks differently from married parent households. For example, single parents may have more difficulty scheduling follow-up appointments; hence, they may benefit from home health care services or medication home delivery programs. Further work is necessary to better understand associations and interactions between poverty and single parent households as well as to identify appropriate and targeted interventions. Knowing the situation in which a child is living may prompt a different approach to clinical or community-based interventions.
In addition to lower income, in our cohort, single parents experienced increased risk of psychological distress. Prior research demonstrates that asthmatic children of parents with poor mental health have worse outcomes [14,24,25]. It is difficult to compare the prevalence of psychological distress across studies using different instruments, but it is important to note that the National Cooperative Inner-City Asthma Study reported that greater than 50% of the caregivers had psychological distress of clinical severity on the Brief Symptom Inventory [6]. We are not able, from our data, to identify patients with a true mental health diagnosis; however, the K6 does enable us to identify those at higher risk of psychological distress. The average K6 score among those who both lived in single parent households and who were readmitted was above 5, a value found to be consistent with moderate mental, or psychological, distress, that has been associated with impairment [26]. Also, in adjusted analyses, higher caregiver risk of psychological distress was significantly associated with increased asthma-related healthcare use.
A higher ratio of in-home children to adults was associated with increased healthcare reutilization; although, this relationship was no longer significant when adjusting for age, gender and parental marital status. Still, the trend toward significance stands in contrast to what could be expected by prior research. Though our study is assessing asthma-related reutilization and not presence or absence of atopy, others have found that having more children in the home is associated with a lower likelihood of allergic disorders (consistent with the hygiene hypothesis) [27,28]. One possible inference from our data, therefore, is that dividing a parent’s resources (e.g. time, income) amongst more children may adversely affect prioritization of asthma care thereby influencing healthcare reutilization. Although the ratio was associated with both marital status and healthcare reutilization, it did not appear to mediate or explain the relationship between the two in regression analyses. Income appeared to be the more powerful explanatory factor and may be completely confounding the observed relationship. Constraints on parental time resources merit further attention in future studies, but likely needs to be measured with improved precision. Additional data on cohabitating adults may also prove useful.
Though children whose parents were single were significantly more likely to spend time outside the home, this variable was not associated with healthcare reutilization. A previous study reported that family organization and strategies around medication use, including making plans for use away from home, were associated with greater adherence to a medication regimen [29]. Transitions such as regularly sleeping in another home are more likely to significantly impact chronic asthma care, but this was not captured in our study. Future studies should focus explicitly on the number and types of transitions in caregivers experienced by children with asthma, and the potential impact of these transitions on morbidity.
The contributions of income and caregiver psychological distress to the relationship of single parent household status and healthcare reutilization represent potential opportunities for intervention. Community health workers (CHWs) might be a particularly important resource to help develop problem-solving and self-efficacy skills around disease management especially for single parents who have limited social supports. CHWs may also help to incorporate medication adherence, allergen remediation and follow-up visits in a way that is amenable to a specific family structure and routine [30-32]. Although such family centered interventions are likely to be useful for any family structure, single parents may stand to benefit the most from an intensive, family focused intervention. Further work assessing CHWs or analogous in-home or in-community interventions could assess whether interventions are more (or less) efficacious or cost-effective in one family structure over another. The effect of low income can be mitigated by ensuring that families receive all public benefits for which they qualify. Screening for and addressing the mental health and social support needs of caregivers, those who are single in particular, should be a priority even during the course of an asthma-related hospitalization. Further research is required to determine how best to implement novel yet realistic interventions that take household structure into account, context that includes parental marital status.
This study had the advantage of using a large inpatient cohort to determine prospective outcomes for children with asthma but also had important limitations. Findings from this study may not be generalizable to populations in other regions with different socio-demographic characteristics or to outpatient populations. Similarly, reutilization patterns may differ from hospitals that provide different in-hospital care [33]. Furthermore, 40% of the eligible children were not enrolled which may have potentially biased our sample. However, there were no significant differences between enrolled and unenrolled children, including in reutilization rates. Investigators did not capture healthcare use outside of the CCHMC network in this study. However, a random 25% subsample of this cohort (N 151) revealed that no children were admitted to an institution other than CCHMC. Of the 51 children revisiting an ER, eight went to an institution other than CCHMC. Of the eight, seven had available data on marital status (four were single and three were married). Thus, we do not expect this to have substantially biased our results. Still, we were unable to capture urgent care or unscheduled follow up visits. We were also limited by the lack of verifiable medication adherence data. Adherence to asthma therapies would be a useful mechanism to assess in future studies. The use of an existing cohort limited our ability to optimally define our psychosocial variables; for example, our classification of caregiver number may be inexact as physical presence in the home does not directly translate to significant contribution to caregiving. We did not have adequate information to discriminate between single-cohabitating families and single parents without the partner in the house nor were we able to assess the amount of help offered by adults living within the home. Though imperfect, we attempted to address this issue by examining the ratio of children to adults in the home. We were surprised that we did not find a stronger association for K6 with reutilization, but this may be in part due to the small number of parents in the highest category of distress (7%). Our data relied on self-report for each of the psychosocial variables. To minimize reporting bias, families were unaware of our central hypothesis and assured of confidentiality. In addition, there may be other potential confounders that we were unable to address in this analysis. For example, single parent households and lower income households may have larger numbers of environmental exposures or triggers which we did not fully capture [34]. Finally, the study could not assess causality between the psychosocial variables and the outcome.
Conclusions
Among children admitted for asthma or bronchodilator-responsive wheezing, children from single parent households had more than a 40% increased odds of returning to the ER or hospital within 12 months. This relationship was explained by lower income and increased risk of psychological distress among single parents. Future research should work to identify potential modifications in chronic asthma care to address these mediating factors and to tailor interventions to specific family contexts.
Acknowledgements
We thank Drs Marc Rothenberg, Amal Assa’ad, Denny Drotar and Carolyn Kercsmar for their mentorship, and Shawna Hottinger for the editorial assistance.
Support for this work is from the following sources: Clinical Fellowship Stipends in Allergy and Immunology from the American College of Allergy, Asthma, and Immunology and the Child Health Research Career Development Award (CHRCDA) (NIH K12 HD028827) (Moncrief). Thrasher Research Fund New Investigator Award, Cincinnati Children’s Hospital Medical Center Outcomes Research Award, National Research Service Award (1T32PE10027) (Simmons). Bureau of Health Professions (BHPr), Health Resources and Services Administration (HRSA), Department of Health and Human Services (DHHS) National Research Service Award Primary Care Research Fellowship in Child and Adolescent Health (T32HP10027) (Beck).
Footnotes
Declaration of interest
The information or content and conclusions herein are those of the authors and should neither be construed as the official position or policy of the BHPR, HRSA, DHHS or the U.S. Government, nor should any endorsements by these organizations be inferred.
References
- 1. [last accessed 30 May/2012];Census Bureau Homepage. 2012 Available at: http://www.cen-sus.gov/
- 2.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National health interview survey, 2010. Vital Health Stat 10. 2011;250:1–80. [PubMed] [Google Scholar]
- 3.Blackwell DL. Family structure and children’s health in the United States: findings from the national health interview survey, 2001-2007. Vital Health Stat 10. 2010;246:1–166. [PubMed] [Google Scholar]
- 4.Chen AY, Escarce JJ. Family structure and the treatment of childhood asthma. Med Care. 2008;46:174–184. doi: 10.1097/MLR.0b013e318156ff20. [DOI] [PubMed] [Google Scholar]
- 5.Koinis-Mitchell D, McQuaid EL, Jandasek B, Kopel SJ, Seifer R, Klein RB, Potter C, Fritz GK. Identifying individual, cultural and asthma-related risk and protective factors associated with resilient asthma outcomes in urban children and families. J Pediatr Psychol. 2012;37:424–437. doi: 10.1093/jpepsy/jss002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wade S, Weil C, Holden G, Mitchell H, Evans R, III, Kruszon-Moran D, Bauman L, et al. Psychosocial characteristics of inner-city children with asthma: a description of the NCICAS psychosocial protocol. National cooperative inner-city asthma study. Pediatr Pulmonol. 1997;24:263–276. doi: 10.1002/(sici)1099-0496(199710)24:4<263::aid-ppul5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 7.Kattan M, Mitchell H, Eggleston P, Gergen P, Crain E, Redline S, Weiss K, et al. Characteristics of inner-city children with asthma: The national cooperative inner-city asthma study. Pediatr Pulmonol. 1997;24:253–262. doi: 10.1002/(sici)1099-0496(199710)24:4<253::aid-ppul4>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 8.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National health interview survey, 2007. Vital Health Stat 10. 2009;239:1–80. [PubMed] [Google Scholar]
- 9.Ker J, Hartert TV. The atopic march: what’s the evidence? Ann Allergy Asthma Immunol. 2009;103:282–289. doi: 10.1016/S1081-1206(10)60526-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martino D, Prescott S. Epigenetics and prenatal influences on asthma and allergic airways disease. Chest. 2011;139:640–647. doi: 10.1378/chest.10-1800. [DOI] [PubMed] [Google Scholar]
- 11.Carr W, Zeitel L, Weiss K. Variations in asthma hospitalizations and deaths in new york city. Am J Public Health. 1992;82:59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halfon N, Newacheck PW. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993;91:56–61. [PubMed] [Google Scholar]
- 13.Koenig K. Pilot study of low-income parents’ perspectives of managing asthma in high-risk infants and toddlers. Pediatr Nurs. 2007;33:223–228. 242. [PMC free article] [PubMed] [Google Scholar]
- 14.Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104:1274–1280. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- 15.Feldman JM, Acosta Perez E, Canino G, McQuaid EL, Goodwin RD, Ortega AN. The role of caregiver major depression in the relationship between anxiety disorders and asthma attacks in island puerto rican youth and young adults. J Nerv Ment Dis. 2011;199:313–318. doi: 10.1097/NMD.0b013e3182174e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bauman LJ, Wright E, Leickly FE, Crain E, Kruszon-Moran D, Wade SL, Visness CM. Relationship of adherence to pediatric asthma morbidity among inner-city children. Pediatrics. 2002;110:e6. doi: 10.1542/peds.110.1.e6. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, Furukawa TA, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO world mental health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19:4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Victorino CC, Gauthier AH. The social determinants of child health: variations across health outcomes – a population-based cross-sectional analysis. BMC Pediatr. 2009;9:53. doi: 10.1186/1471-2431-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slopen N, Kubzansky LD, McLaughlin KA, Koenen KC. Childhood adversity and inflammatory processes in youth: a prospective study. Psychoneuroendocrinology. 2013;38:188–200. doi: 10.1016/j.psyneuen.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith LA, Bokhour B, Hohman KH, Miroshnik I, Kleinman KP, Cohn E, Cortés DE, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122:760–769. doi: 10.1542/peds.2007-2750. [DOI] [PubMed] [Google Scholar]
- 22.Wood RA, Bloomberg GR, Kattan M, Conroy K, Sandel MT, Dresen A, Gergen PJ, et al. Relationships among environmental exposures, cord blood cytokine responses, allergy, and wheeze at 1 year of age in an inner-city birth cohort (urban environment and childhood asthma study) J Allergy Clin Immunol. 2011;127:913–919. e6. doi: 10.1016/j.jaci.2010.12.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102:2308–2314. doi: 10.2105/AJPH.2012.300806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kilpelainen M, Koskenvuo M, Helenius H, Terho EO. Stressful life events promote the manifestation of asthma and atopic diseases. Clin Exp Allergy. 2002;32:256–263. doi: 10.1046/j.1365-2222.2002.01282.x. [DOI] [PubMed] [Google Scholar]
- 25.Scott KM, Von Korff M, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, et al. Childhood adversity, early-onset depressive/anxiety disorders, and adult-onset asthma. Psychosom Med. 2008;70:1035–1043. doi: 10.1097/PSY.0b013e318187a2fb. [DOI] [PubMed] [Google Scholar]
- 26.Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012;21:88–97. doi: 10.1002/mpr.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldberg S, Israeli E, Schwartz S, Shochat T, Izbicki G, Toker-Maimon O, Klement E, Picard E. Asthma prevalence, family size, and birth order. Chest. 2007;131:1747–1752. doi: 10.1378/chest.06-2818. [DOI] [PubMed] [Google Scholar]
- 28.Kinra S, Davey Smith G, Jeffreys M, Gunnell D, Galobardes B, McCarron P. Association between sibship size and allergic diseases in the glasgow alumni study. Thorax. 2006;61:48–53. doi: 10.1136/thx.2004.034595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McQuaid EL, Everhart RS, Seifer R, Kopel SJ, Mitchell DK, Klein RB, Esteban CA, et al. Medication adherence among latino and non-latino white children with asthma. Pediatrics. 2012;129:e1404–e1410. doi: 10.1542/peds.2011-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Postma J, Karr C, Kieckhefer G. Community health workers and environmental interventions for children with asthma: a systematic review. J Asthma. 2009;46:564–576. doi: 10.1080/02770900902912638. [DOI] [PubMed] [Google Scholar]
- 31.Krieger JW, Takaro TK, Song L, Weaver M. The seattle-king county healthy homes project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95:652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fox P, Porter PG, Lob SH, Boer JH, Rocha DA, Adelson JW. Improving asthma-related health outcomes among low-income, multiethnic, school-aged children: results of a demonstration project that combined continuous quality improvement and community health worker strategies. Pediatrics. 2007;120:e902–e911. doi: 10.1542/peds.2006-1805. [DOI] [PubMed] [Google Scholar]
- 33.Knighton AJ, Flood A, Speedie SM, Harmon B, Smith P, Crosby C, Payne NR. Does initial length of stay impact 30-day readmission risk in pediatric asthma patients? J Asthma. 2013;50:821–827. doi: 10.3109/02770903.2013.816726. [DOI] [PubMed] [Google Scholar]
- 34.Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect. 2007;115:971–975. doi: 10.1289/ehp.8989. [DOI] [PMC free article] [PubMed] [Google Scholar]