Abstract
This systematic review synthesizes data published between 1988 and 2009 on mean BMI and prevalence of overweight, obesity, and type 2 diabetes among Asian subgroups in the U.S. We conducted systematic searches in PubMed for peer-reviewed, English-language citations that reported mean BMI and percent overweight, obesity, and diabetes among South Asians/Asian Indians, Chinese, Filipinos, Koreans, and Vietnamese. We identified 647 database citations and 23 additional citations from hand-searching. After screening titles, abstracts, and full-text publications, 97 citations remained. None were published between 1988 and 1992, 28 between 1993 and 2003, and 69 between 2004 and 2009. Publications were identified for the following Asian subgroups: South Asian (n=8), Asian Indian (n=20), Chinese (n=44), Filipino (n=22), Korean (n= 8), and Vietnamese (n=3). The observed sample sizes ranged from 32 to 4245 subjects with mean ages from 24 to 78 years. Among samples of men and women, the lowest reported mean BMI was in South Asians (22.1 kg/m2), and the highest was in Filipinos (26.8 kg/m2). Estimates for overweight (12.8 - 46.7%) and obesity (2.1 – 59.0%) were variable. Among men and women, the highest rate of diabetes was reported in Asian Indians with BMI ≥ 30 kg/m2 (32.9%, age and sex standardized). This review suggests heterogeneity among U.S. Asian populations in cardiometabolic risk factors, yet comparisons are limited due to variability in study populations, methods, and definitions used in published reports. Future efforts should adopt standardized methods to understand overweight, obesity and diabetes in this growing U.S. ethnic population.
Keywords: Asian, BMI, diabetes, ethnicity, obesity, overweight
INTRODUCTION
Between 2000 and 2010, the United States (U.S.) Asian population grew by 46%, to 17.3 million, the highest percentage growth of any racial group during that time period. The three largest Asian American subgroups are Chinese (3.8 million), Filipino (3.2 million), and Asian Indian (2.8 million) [1]. Despite continued growth of general and specific Asian American sub-populations, studies still group them into one large category, potentially missing important heterogeneity in disease burden and risk. This is especially true with regard to overweight, obesity and diabetes, chronic conditions of increasing public health significance due to increasing prevalence worldwide. However, the estimated burden of these conditions across Asian American subgroups in the U.S. is difficult to quantify because data disaggregated by Asian American subgroups are fragmented in the literature. The aim of this review is to systematically synthesize data about overweight, obesity, and diabetes among specific Asian American groups. The resulting synthesis will qualitatively summarize available estimates on the prevalence of overweight, obesity, and diabetes among those specific Asian American subgroups with high immigration rates to the U.S. over the past 20 years, specifically South Asians (Asian Indian, Bangladeshi, Bhutanese, Pakistani, Nepalese, and Sri Lankan), Chinese, Filipino, Korean, and Vietnamese.
METHODS
We performed a systematic search for peer-reviewed studies published in English using PubMed (1988 – 2009). Search strategies included Medical Subject Heading (MeSH) terms and keywords. For overweight, obesity, and diabetes, search terms included “body mass index,” “overweight,” “obesity,” “diabetes mellitus,” and “diabetes mellitus, Type 2.” The search terms for Asian groups included country ethnology, “emigrant,” “immigrant,” and “United States.” Because South Asia and South Asian are both commonly used and capture some of the subgroups of interest, we decided to search for South Asia by keyword (“South Asian*”). Additional studies were retrieved through a hand search of the citations listed in the publications of PubMed search results and from recent review articles on the topics of interest.
Inclusion And Exclusion Criteria
An article was eligible for inclusion if it presented original research in English language collected in the U.S. or a U.S. territory between 1988 and 2009, including 2009 electronic publications ahead of 2010 print. Inclusion criteria were designed to retrieve studies that reported prevalence of obesity, overweight, and diabetes among various Asian American subgroups (South Asians, Asian Indian, Pakistani, Bangladeshi, Sri Lankan, Chinese, Filipino, Korean, and Vietnamese). Articles containing study samples with origin from two or more South Asian countries were exclusively categorized into the South Asian subgroup. Given that Asian Indians, Pakistanis, etc. are part of South Asian ancestry, these categories could be combined for a more generalized analysis, however, for the purpose of this review, South Asian was treated as a separate category in accordance with database search strategies. Articles were included if they contained data on mean body mass index (BMI), percent overweight, percent obesity, or percent diabetes. Only articles with samples sizes of at least 30 participants in the specific Asian American subgroups of interest were included. Studies that included individuals less than 18 years of age, living outside the U.S., or participating in data collection outside the time period of interest (1988-2009) were excluded. Other exclusion criteria are listed as follows: studies that only selected for people with diabetes or other poor health conditions; studies using non-representative samples matched by BMI or diabetes; and studies examining gestational diabetes mellitus or weight change during pregnancy.
Study Selection
The selection of articles for inclusion was conducted through two screening phases. The first phase included a review of abstracts for inclusion and exclusion criteria. All abstracts were reviewed by the first reviewer (LRS) and by an independent second reviewer (MBW or ROF). Discrepancies about inclusion of studies were resolved through consensus with a third person serving as a non-reviewing arbitrator (MBW or ROF). Remaining abstracts were included in the second screening phase in which each reviewer applied inclusion and exclusion criteria to full-text articles.
Data Extraction
For each publication retrieved and meeting inclusion and exclusion criteria, data were extracted using a standardized form. Key measures extracted included mean BMI, percent overweight or obese defined by BMI strata, and percent diabetes defined by self-report, fasting blood glucose, random (non-fasting) blood glucose, or two-hour, post challenge blood glucose. Percent overweight and percent obesity were defined as mutually exclusive ranges of BMI. Publications that defined overweight using a BMI range that lacked an upper BMI bound (e.g., BMI ≥25 kg/m2) were included in this review, with data categorized into combined overweight and obesity. Other extracted data included study cohort, year(s) of data collection, study design, characteristics of the study population (ethnicity/nationality, sex, age range, etc.), sample size, and measurement methods (e.g., self-report, fasting blood glucose).
RESULTS
Literature Search
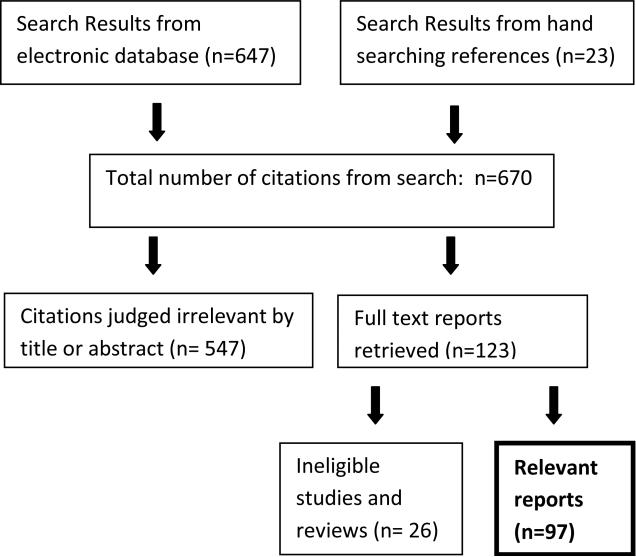
Our searches yielded 647 citations from PubMed and 23 citations from hand searching of references. After the first screening phase of titles and abstracts, 547 citations were excluded, leaving 123 articles for full-text review. The second screening phase of the full-text articles resulted in the exclusion of 26 additional articles, and 97 articles remained for data extraction (Figure 1). Disagreement between reviewers occurred for only nine citations (1.3%).
Figure 1. Systematic review flow chart: report selection.
Studies were ineligible for the following reasons: BMI and percent overweight/obese and percent diabetes not provided (n=13); participant age (n=6); study dates (n=2); sample size (n=1); review paper (n=1); other (n=3)
Study Characteristics
Articles were identified for the following Asian subgroups: South Asian (n=8), Asian Indian (n=20), Chinese (n=44), Filipino (n=22), Korean (n= 8), and Vietnamese (n=3). Most articles reported on one Asian subgroup, however six reported on two or more Asian subgroups as defined for this review [2-7], hence the summation of articles by subgroup was greater than 97. In all studies, ethnicity was defined by participant self-report of ethnicity, origin, or ancestral origin. Although searches were conducted for studies with Bangladeshi, Bhutanese, Nepalese, Pakistani, or Sri Lankan individuals, no articles were found for these groups. Of the 97 articles in the systematic review, nearly half (n=46) were analyses of one of the following seven studies: Multi-Ethnic Study of Atherosclerosis [8-25] (MESA, n=18), Study of Women's Health Across the Nation [26-37] (SWAN, n=12), Filipino Women's Health Study [38-44] (n=7), Kōhala Health Research Project/Native Hawaiian Health Research Project [41, 45, 46] (NHHR, n=3), Behavioral Risk Factor Survey in Guam [47, 48] (BRFS, n=2), University of California San Diego (UCSD) Rancho Bernardo Study [49, 50] (n=2), and National Health Interview Survey [5, 7] (NHIS, n=2). Almost all articles reported cross-sectional data for the variables of interest; only two SWAN studies [27, 33] provided longitudinal data. Nationally representative data were sparse and limited to articles reporting NHIS data; however, several articles reported on studies with multi-center recruitment, including MESA (six centers throughout the U.S.: Baltimore, MD; Chicago, IL; Forsythe County, NC; Los Angeles, CA; New York City, NY; and St. Paul, MN) and the Diabetes Among Indian Americans (DIA) study [51] (seven urban sites: Houston, TX; Phoenix, AZ; Washington, DC; Boston, MA; San Diego, CA; Edison, NJ; and Parsippany, NJ). A quarter of all studies utilized random sampling methods (n=26).
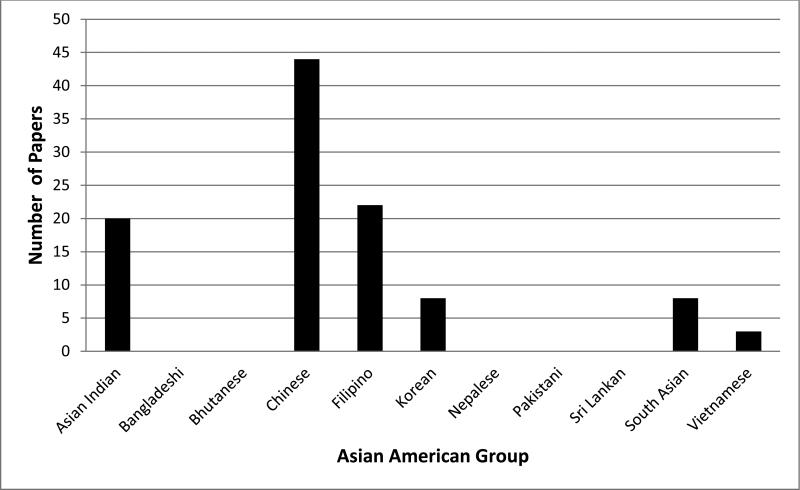
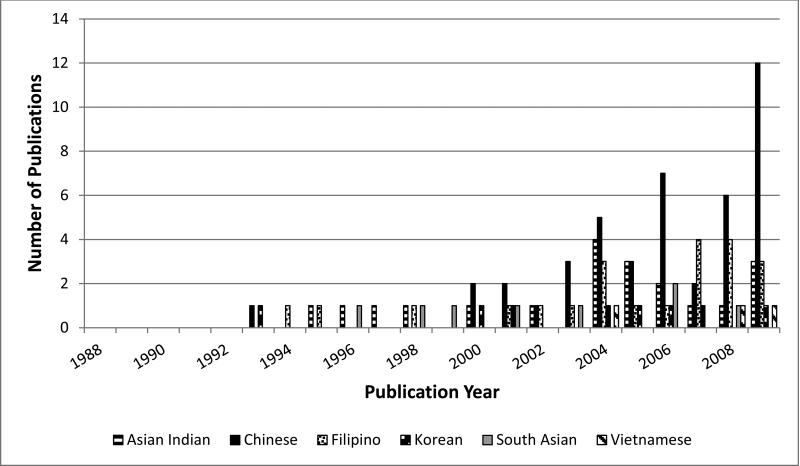
The number of studies representing specific Asian subgroups is proportional to the population sizes of Asian subgroups in the U.S.; Chinese were represented in the most studies (47% of all studies, largest U.S. Asian subgroup) followed by South Asians and Filipinos (27% and 24%, respectively, the 3rd and 2nd largest U.S. Asian subgroups) (Figure 2). Additionally, the number of studies reporting data on Asian-specific subgroups increased from 1988-2009 (Figure 3), with the greatest number of publications with Chinese participants apparent after 2002. The observed sample sizes in the 97 articles ranged from 32 subjects to 4245 subjects. The mean age reported across studies ranged from 24 to 78 years. The ages of participants in the most common studies were 45-84 years in MESA, 40-55 in SWAN, 18 years and older in NHIS, 18 to 95 years in NHHR, and 40-76 years in the Filipino Women's Health Study. Prevalence estimates of interest were variable and wide-ranging across all subgroups. Only 20% of all articles reported prevalence data that were adjusted for age, sex, and/or other factors in the study sample or that were standardized for age, sex, and/or other factors to another population. Such data were provided for five Asian Indian [5, 51-54] articles, two Chinese [2, 5] articles, nine Filipino [2, 5, 38-41, 47, 50, 55] articles, two Korean [56, 57] articles, and one Vietnamese [58] article. None were reported for the South Asian category. Hereafter, reported values are crude unless otherwise noted. Of 32 articles providing prevalence of overweight and/or obesity, 63% (n=20) reported only conventional definitions for overweight or obesity (i.e., 25≤BMI<30, BMI ≥30 kg/m2) or similarly (e.g., 26≤BMI≤30 kg/m2). Five articles defined overweight and obesity according to 2004 WHO Asian-specific cut-points [59] (BMI 23.0 – 27.4 kg/m2 and BMI ≥ 27.5 kg/m2, respectively) or similarly (obesity as BMI ≥ 27.8 kg/m2) [5, 51, 53, 60, 61]. Six studies defined overweight without an upper BMI bound (i.e., as BMI ≥ 23; BMI > 23; BMI >25; or BMI ≥ 25 kg/m2) [4, 62-66]. Over half (n=52) of all articles reported prevalence of diabetes, defining diabetes by one or more of the following methods: self-report (n=42, includes self-report of diagnosis or diabetes medication usage), fasting blood glucose (n= 32), two-hour glucose tolerance (n=11), or random (nonfasting) blood glucose (n=1). Five articles did not provide the method used to assess diabetes [23, 67-70].
Figure 2. Number of publications reporting on Asian groups, 1988 – 2009,* by Asian American sub-population.
*Reports with electronic publication in 2009 and paper publication in 2010 were included
Figure 3. Number of peer-reviewed publications reporting data on specific Asian groups by year*.
*Reports with electronic publication in 2009 and paper publication in 2010 were included.
Summary of BMI, Overweight, Obesity, and Diabetes across Asian Subgroups
Among men and women combined, the lowest mean BMI reported was 22.1 kg/m2 in South Asians [71], whereas the highest mean was reported in Filipino adults (26.8 kg/m2) [46]. Among men, the lowest mean BMI was reported among young, Asian Indian men (22.8 kg/m2) [54]; the highest mean was 25.9 kg/m2 among Asian Indian immigrants to the San Francisco area [72, 73] and 25.7 kg/m2 among Filipino men from Guam [48]. Among women, the lowest mean BMI was reported in Chinese community college students (19.4 kg/m2) [6], and the highest mean was among Korean elderly women age 65 and greater (26.3 kg/m2) [74].
According to NHIS data, which included Asian Indian, Chinese, and Filipino Asian subgroups, the highest proportions of overweight (23.0 ≤ BMI ≤ 27.4 kg/m2) and obesity (BMI ≥ 27.5 kg/m2) adjusted for age and sex were among Filipinos (46.5% overweight, 20.8% obese) and Asian Indians (46.7% overweight, 16.6% obese) [5]. Across all other studies combining men and women, the highest percent overweight (BMI 23-27.4 kg/m2) was reported among Koreans (38.4%) [60] and the highest percent obesity (defined as BMI ≥ 25 kg/m2) was reported among Filipinos (59%) [4]. Among studies reporting on both men and women, the lowest rate of overweight (25≤BMI≤29.9 kg/m2) was among Asian Indians (12.8%) [75] and the lowest rate of obesity (BMI ≥ 30 kg/m2) was reported for Vietnamese (2.1%) [58].
The prevalence of diabetes varied widely across articles. The lowest prevalence of diabetes was reported in South Asians (1%) [68], Chinese (3.96%) [64], and Vietnamese (5.3%, age-standardized) [58]. Reports for the greatest percent of diabetes included those for Filipinos (e.g., 36.4%, women in the Filipino Women's Health Study [42]) and Chinese (28%, 45 years or older with at least one CVD risk factor [4]). According to NHIS results, percent diabetes increased in overweight and even more in obesity across ethnicities studied. Comparing Asian subgroups (i.e., Asian Indian, Chinese, and Filipino) in a pooled NHIS analysis from 1997 to 2005, Asian Indians had the highest rates of diabetes in every category of BMI (age- and sex- standardized), compared to Chinese or Filipinos [5].
BMI, Overweight, Obesity, and Diabetes by specific Asian Subgroup
South Asians
Across the eight publications of South Asian samples, data were cross-sectional and unadjusted (Table 1). The mean BMI for analyses of men and women combined ranged from 22.1-25.8 kg/m2 [71, 76, 77]. Other studies provided mean BMI of 22-25 kg/m2 for males [69, 71, 78] and 22.3- 25 kg/m2 for females [69, 78, 79]. Percent diabetes ranged from 1-11.6% [53, 68, 76]. Ivey and colleagues reported two studies (the California Health Interview Survey, CHIS, and the Cardiovascular Health Among Asian Indians Survey, CHAI) of South Asians in one publication [76]. CHIS recruited participants from a random-digit dial of households drawn from every county in California plus households from surname lists. Mean BMI was 24.5 kg/m2, and 4% (n=37) reported diabetes. CHAI included South Asian adults from one of three areas within northern California using list-driven, surname-based recruitment (n=252 telephone participants; n=52 in-person participants). Here, mean BMI was 25.6 kg/m2 (telephone participants) and 25.8 kg/m2 (in-person participants). Self-reported diabetes was 11% (n= 27) for telephone participants and 10% (n=5) for in-person participants. All other studies about South Asians used convenience samples. The largest of these studies examined South Asians living in Dallas; this study reported mean BMI at 24.9 kg/m2 (n=616 participant without diabetes, mean age 42 years) [77]. In another study of South Asians aged 18-30 years, mean BMI (22.1 kg/ m2) was similar to European Americans (23.7 kg/m2); however South Asians had statistically higher (p<0.05) mean fasting blood glucose and family history of diabetes [71]. These findings are supported by another study among females with no history of diabetes, where mean fasting glucose was elevated (102.7 mg/dl) [79].
Table 1.
Results of a Systematic Review of Mean BMI, Percent Overweight (ov)/Obese (ob), and Prevalence of Diabetes in Asians: South Asian References (n=8)
| Reference | City, State | Sample Size | Mean Age in Years ± SD | Mean BMI in kg/m2 ± SD | Definition of ov, ob by BMI (kg/m2) | Ov, ob, % | Diabetes, % |
|---|---|---|---|---|---|---|---|
| Anand 1998 [68] | ***a | 141a | 47a | *** | *** | *** | 1a, c |
| Chicago, ILb | 255b | 46b | *** | *** | *** | 11.3b, c | |
| Chandalia 2008 [69] | Dallas, TX | 418 (men) 331 (women) |
42 ± 15 (men) 42 ± 14 (women) |
25 ± 15 (men) 25 ± 4 (women) |
*** | *** | *** |
| Chandalia 2003 [78] | Dallas, TX | 82 (men) | 31 ± 12 (men) | 23.9 ±3.1 (men) | *** | *** | *** |
| Enas 1996 [53] | *** | 1688 (total) 1131 (men) 557 (women) |
46.4 ± 7.5 (men) 42.9 ± 7.4 (women) 48.0 ± 5.5 (men ≥ 40 years) |
*** | ob: BMI≥27.8 | ob: 6.7 (men≥40 years) | 7.6 (total)d 9.0(men)d, e 6.1(women)d,e |
| Ivey 2006 [76] | CA counties / northern CA | 769f | *** | 24.5 ± 5.5f | *** | *** | 4f,g |
| CA counties / northern CA | 257b 52i |
*** | 25.6 ± 5.2h 25.8 ± 6.0i |
*** | *** | 11h,g 10i,g |
|
| Kalhan 2001 [71] | Cleveland area, OH | 32 | 23.8 ± 2.0 | 22.1 ± 3.0 | *** | *** | *** |
| Kamath 1999 [79] | Chicago, IL | 47 (women) | 27.5 ± 5.6 (women) | 22.6 ± 3.2 (women) | *** | *** | *** |
| Radha 2006 [77] | Dallas, TX | 616 j | 42 ± 13j | 24.9 ± 3.7j | *** | *** | *** |
data not included or specified
The first of two studies reported in Anand 1998 of the Coronary Artery Disease in Asian Indians (CADI) study
The second of two studies reported in Anand 1998
Estimate method not specified
Based on previous diagnosis or use of insulin or oral hypoglycaemic agents
Adjusted for age
The first of two studies reported in Ivey 2006, the California Health Interview Study (CHIS) which used population-based random sampling
Based on self-report
The second of two studies reported in Ivey 2006, the phone portion of the Cardiovascular Health Among Asian Indians Survey (CHAI) which used population-based sampling
The second of two studies reported in Ivey 2006, the in-person interview of the Cardiovascular Health Among Asian Indians Survey (CHAI) which used population-based sampling
Portion of total sample without diabetes
Asian Indians
All 20 articles identified for the Asian Indian subgroup were cross-sectional studies (Table 2). Oza-Frank, et al. 2009 [5] provided the largest sample of Asian Indians (n= 1357) with NHIS representing 1,234,233 individuals in the U.S.. The DIA study reported on 1038 Asian Indian adults (18 years and older) residing in seven U.S. urban sites [51]. While NHIS studies did not provide mean BMI, the DIA study reported a mean of 25.4 kg/m2, adjusted for age and sex. In addition to the DIA study, eleven articles reported mean BMI for men and women combined with estimates ranging from 22.4 - 26.1 kg/m2 [54, 61, 70, 72, 73, 75, 80-84]. The lower and upper values of this range were estimated by convenience samples, with the lower value among young, healthy volunteers (n=49) [54] and the upper value reported both among Asian Indians originally from the state of Gujarat living in Atlanta, Georgia (n=1046) [83] and among Asian Indian immigrants aged 29-59 in the San Francisco Bay area (n = 56) [72, 73]. Some articles stratified BMI by sex or studied only one gender, and the reported estimates for men and for women were similar, ranging from 22.8 to 25.9 kg/m2 for men [51, 52, 54, 72, 73, 75, 82, 85-87] and 21.7 to 26.5 kg/m2 for women [51, 52, 75, 82, 88].
Table 2.
Results of a Systematic Review of Mean BMI, Percent Overweight (ov)/Obese (ob), and Prevalence of Diabetes in Asians: Asian Indian references (n=20)
| Reference | City, State | Sample Size | Mean Age in Years ± SD | Mean BMI in kg/m2 ± SD | Definition of ov, ob by BMI (kg/m2) | Ov, ob, % | Diabetes, % |
|---|---|---|---|---|---|---|---|
| Abate 2004 [85] | *** | 79 (men) | 31 ± 12 (men) | 24 ± 3 (men) | *** | *** | *** |
| Abate 1995 [86] | *** | 93 (men) | 47 ± 6 (men) | 24.8 ± 3.1 (men) | *** | *** | *** |
| Balasubramanyam 2008 [80] | Houston, TX | 143 | 50.3 ± 13.8 | 25 ± 5.00 | ov: 25<BMI<30 obi: BMI≥30 ob2: BMI≥25 |
ov: 31 ob1: 11 ob2: 43 |
18a |
| Bhalodkar 2005 [88] | *** | 119 (women) | 47.9 ± 11.2 (women) | 24.0 ± 4.7 (women) | *** | *** | *** |
| Chuang 1998 [52] | *** | 110 (total) 64 (men) 46 (women) |
45.9 ± 8.7 (men) 44.3 ± 8.6 (women) |
24.0 ± 2.7 (men) 23.7 ± 3.1 (women) |
*** | *** | 7.5(total)b 6.6(men)b 8.9 (women)b |
| Ivey 2004 [84] | Northern CA cities | 304 | 40 | 25.7 | ov & ob: BMI>25c | ov & ob: 46.4 | 10.6b |
| Jonnalagadda 2007 [82] | Canton, MI | 101 (total) 44 (men) 57 (women) |
53 ± 13 (men) 55 ± 11 (women) |
25.5 (total) 25.1 ± 3.1 (men) 25.8 ± 4.4 (women) |
*** | *** | *** |
| Jonnalagadda 2005 [81] | Metropolitan Atlanta, GA | 226 | 58 ± 6 | 24.9 ± 3.3 | ov: 25≤BMI≤29.9 ob: BMI>30 |
ov: 35 ob: 5 |
18b |
| Jonnalagadda 2002 [89] | Metropolitan Atlanta, GA | 237 | *** | *** | ov & ob: BMI>25c | ov & ob: 43 | *** |
| Kamath 1997 [87] | *** | 187 (men) | 46 ± 9.3 (men) | 23.6 (men) | ov: 26≤BMI≤30 ob: BMI>30 |
ov: 24 (men) ob: 2.2 (men) |
8.8 (men)b |
| Misra 2010 [51] | 7 suburba sites in United States | 1038 (total)d 609 (men) 429 (women) |
45.7 ± 1 2.8 (total) | 25.4 ± 3.7 (total) 25.3 ± 3.3 (men) 25.6 ± 4.4 (women) |
ov1: 25<BMI <30 ov2: 23.0≤BMI≤27.4 obi: BMI≥30 ob2: BMI≥27.5 |
ov1: 38 (total) ov2: 25 (total) ob1: 11 (total) ob2: 49.8 (total) |
17.4 (total)e 20.0 (male) e 13.8 (female)e 14.0 (known)e |
| 3.4 (newly diagnosed)e 3.9 (among 20-39 years)e 17.1(among 40-59 years)e 31.2(among ≥ 60 years)e |
|||||||
| Misra 2006 [73] | San Francisco Bay Area, CA | 56 (total) 31 (men) |
43.4 ± 6.9 (total) 43.7 ± 7.1 (men) |
26.1 ± 3.7 (total) 25.9 ± 3.1 (men) |
*** | *** | *** |
| Misra 2005 [72] | San Francisco Bay Area, CA | 56 (total) 31 (men) |
43.4 ± 6.9 (total) 43.7 ± 7.1 (men) |
26.1 ± 3.7 (total) 25.9 ± 3.1 (men) |
*** | *** | *** |
| Misra 2000 [75] | *** f | 261 (total) | 46.1 ± 7.4 (total) | 24.0 (total) 24.3 (men) 23.3 (women) |
ov: 25≤BMI≤29.9 ob: BMI>30 |
ov: 12.8 (total) ov: 14.2 (men) ov: 9.4 (women) ob: 7.4 (total) ob: 8.9 (men) ob: 4.1 (women) |
*** |
| Mooteri 2004 [70] | *** | 489g | 49 ± 12 | 24.0 ± 3.5 | ob: BMI>30 | ob: 6 | 9h |
| Oza-Frank 2009 [5] | United States, 1997-2005 i | 1357 | 37.6 (SE 0.4) | *** | ovl: 23.0≤BMI≤27.4 ov2: 25.0≤BMI≤29.9 obl: BMI≥27.5 ob2: BMI≥30 |
ov1: 46.7, SE 1.8 ov2: 34.1, SE 1.6 ob1: 16.6, SE 1.4j ob2: 6.7, SE 0.9j |
6.5, SE 1.9b, j, k 8.3, SE 1.7 (ov1)b, j 8.8, SE 1.8 (ov2)b, j 19.4, SE 3.5 (ob1)b, j 32.9, SE 4.4 (ob2)b, j |
| Petersen 2006 [54] | *** | 49 (total) 31 (men) |
28.7 ± 8.3 (total) 30.0 ± 8.7 (men) |
22.4 ± 2.3 (total) 22.8 ± 2.2 (men) |
*** | *** | *** |
| Venkataraman 2004 [83] | Atlanta, GA | 1046 | 52.8 ± 11.3 | 26.1 ± 4.7 | *** | *** | 18.1b |
| Yagalla 1996 [61] | *** | 153 | 47.4 ± 6.4 | 24.6 ± 2.7 | ob: BMI≥27.8 | ob: 8 | *** |
| Ye 2009 [7] | United States, 2003-2005i | 534 | *** | *** | ob: BMI≥30 | ob: 6.1 | 8.2b |
Data not included or specified
Based on fasting overnight blood glucose >100mg/dl - or - self diagnosed
Based on self-report
Reported as overweight in publication
Sample from the Diabetes among Indian Americans (DIA) study. Directories for random sampling were created at each site through compilations of several sources. Five thousand were selected from this database (n=43,150)
Diabetes diagnosed by fasting blood glucose ≥ 126 mg/dl or self-report of previously diagnosed diabetes
Survey participants were invited from a directory of a national Gujarati Association in the United States
Portion of total sample without coronary artery disease
Estimate method not specified
Participants from the National Health Interview Survey, a U.S. nationally representative survey of non-institutionalized adults (18 and older)
Age and sex standardized to the 2000 U.S. population
Among those with BMI 18.5-22.9 kg/m2
Two articles reported the prevalence of overweight using Asian-specific cut-points. In NHIS, 46.7% (age- and sex- standardized) were overweight [5]. Misra, et al. 2010 reported 25% overweight among DIA participants (age- and sex- adjusted) [51]. The prevalence of overweight in men and women combined using other definitions for overweight ranged from 12.8-43.0% [7, 51, 70, 75, 80, 81, 89]. Three studies reported prevalence of obesity using WHO criteria for Asian populations; obesity prevalence in these studies ranged from 8% to 49.8% [5, 51, 61].
The prevalence of diabetes was reported in eleven articles (Table 2). In the DIA study, prevalence of diabetes for adults aged ≥20 was 17.4% (n=181), where 13.9% were known cases and 3.5% were previously undiagnosed (estimates age- and sex-adjusted) [51]. Stratifying by WHO Asian-specific BMI categories, NHIS diabetes estimates (age- and sex- standardized) were 6.5% among normal weight participants (BMI 18.5-22.9 kg/m2); 8.3% among overweight participants (BMI 23.0-27.4 kg/m2); and 19.4% among obese participants (BMI ≥ 27.5 kg/m2) [5]. The lowest prevalence of diabetes was reported among a sample of 110 physicians and their adult family members aged 20 to 62 years (men: 6.6%; women: 8.9%; total: 7.5%) [52]. The largest reported prevalence of diabetes for men and women (32.9%, age- and sex- standardized) was reported in NHIS among Asian Indians with BMI ≥ 30 kg/m2 [5].
Chinese
More articles (n=44) presented information about the Chinese subgroup compared to any other Asian subgroup in this systematic review (Table 3). The only nationally representative samples identified in the systematic search for Chinese were NHIS samples [5, 7]. In the pooled (1997-2005) NHIS analysis, mean overweight was 38.2% (age- and sex-standardized), and mean obesity was 8.8% (age- and sex- standardized) as per WHO Asian-specific definitions [5]. This was the only study of Chinese Americans that used WHO definitions for overweight and obesity. In MESA, percent overweight (BMI 25-29.9 kg/m2) was between 25-40% depending on age [13]. Furthermore, 4.5% were obese (BMI ≥ 30 kg/m2) [10], an estimate similar to NHIS results when using non-Asian specific cut-points (NHIS 4.2%, age- and sex- standardized) [5]. In Hawaii, the Kidney Early Evaluation Program (KEEP-2) study contained 15% overweight and 47% obese volunteers as defined by the WHO International Obesity Task Force in 2000 (BMI≥23 kg/m2 and BMI≥25 kg/m2 respectively) [4].
Table 3.
Results of a Systematic Review of Mean BMI, Percent Overweight (ov)/Obese (ob), and Prevalence of Diabetes in Asians: Chinese References (n=44)
| Reference | City, State | Sample Size | Mean Age in Years ± SD | Mean BMI in kg/m2 ± SD | Definition of ov, ob by BMI (kg/m2) | Ov, ob, % | Diabetes, % |
|---|---|---|---|---|---|---|---|
| Multi-Ethnic Study of Atherosclerosis | |||||||
| Allison 2009 [9] | a | 803 | 62.3 ± 10.3 | 24.0 ± 3.3 | *** | *** | 15.2b |
| Allison 2009 [8] | a | 258 | 65 ± 10 | 24 ± 3 | *** | *** | 15b |
| Bahrami 2008 [10] | a | 803 | 62.3 ± 10.3 | 24.0 ± 3.3 | ob: BMI≥30 | ob: 4.5 | 15.2b |
| Bertoni 2006 [11] | a | 651 | *** | *** | *** | *** | 14.4c |
| Bild 2005 [12] | a | 803 | 62.9 ± 10.3 | 24.0 ± 3.3 | *** | *** | 15.7d |
| Burke 2008 [13] | a | 803 | *** | 23.9 (women) 24.1 (men) |
ov: 25.0≤BMI≤29.9 ob: BMI>30.0 |
ov: 33 (total)e ob: 5 (total)e |
*** |
| Colangelo 2009 [14] | a | 388 (men) | *** | *** | *** | *** | 15 (men)b |
| Diez Roux 2005 [15] | a | 768 (non-U.S.-born) | 62.3 (non-U.S.-born) | 23.9 (non-U.S.-born) | *** | *** | 14.3 (non-U.S.-born)d |
| Duprez 2009 [16] | a | 374 (men) 395 (women) |
62.3 ± 10.2 (men) 62.2 ± 10.4 (women) |
24.0 ± 3.1 (men) 23.9 ± 3.5 (women) |
*** | *** | 16 (men)b 15 (women)b |
| Gao 2008 [17] | a | 790 | 62.9 | 24.0 | *** | *** | *** |
| Kandula 2008 [18] | a | 737 | 62.8 ± 10.2 | 23.9 ± 3.3 | *** | *** | 13.3b |
| Katz 2006 [19] | a | 801 (total) 388 (men) 413 (women) |
*** | *** | *** | *** | 15.7 (total)b, f 16.5 (men)v, f 15.0 (women)b, f |
| Klein 2006 [20] | a | 727 | 62.4 ± 10.2 | 24.1 ± 3.3 | *** | *** | 15.3c |
| Kramer 2004 [21] | a | 803 | 62.9 ± 10.3 | 24.0 ± 3.3 | *** | *** | 14c |
| Ouyang 2009 [22] | a | 272 | 65.6 ± 9.1 | 24.1 ± 3.7 | *** | *** | 18.4b |
| Palmas 2008 [23] | a | 790 | 62.3 ± 10.3 | 23.9 ± 3.3 | *** | *** | 14.7g |
| Paramsothy 2009 [24] | a | 695 | 61.8 ± 10.4 | 23.8 ± 3.3 | *** | *** | *** |
| Wong 2006 [25] | a | 724 | 61.8 ± 10.2 | 24.1 ± 3.3 | *** | *** | 14.5b |
| Study of Women's Health Across the Nation | |||||||
| Everson-Rose, 2004 [27] h | Oakland, CA area | 210 (women) | 46.5 ± 2.6 (women) | 23.2 ± 3.8 (women) | *** | *** | 2.9 (incident diabetes, women)i |
| Gold, 2000 [28] | Oakland, CA area | 546 (women) | *** | *** | ob: BMI≥27j | ob: 9.5 (women) | *** |
| Greendale, 2003 [29] | Oakland, CA area | 250 (women) | 46.5 ± 2.6 (women) | 23.3 ± 3.9 (women) | *** | *** | *** |
| Habel, 2007 [30] | Oakland, CA area | 179 (women) | *** | *** | ov: 24.2≤BMI≤28.2 ob:28.3≤BMI≤55.8j |
ov: 23 (women) ob: 11 (women) |
*** |
| Kelley-Hedgepeth, 2008 [31] | Oakland, CA area | 244 (women) | 46.7 (women) | 22.5 (women) | *** | *** | 2.2 (women)b |
| Lasley, 2002 [32] | Oakland, CA area | 228 (women) | 46.43 ± 2.54 (women) | 23.17 ± 3.94 (women) | *** | *** | *** |
| Lo, 2006 [33] h | Oakland, CA area | 151 (women) | *** | *** | *** | *** | 3 (women)b |
| Matthews, 2005 [34] | Oakland, CA area | 231 (women) | 46.6 ± 2.6 (women) | 23.2 ± 3.9 (women) | ov: 25≤ BMI<30 ob: BMI≥30 |
ov: 17.0 (women) ob: 4.4 (women) |
*** |
| Matthews, 2001 [26] | Oakland, CA area | 562 (women) | *** | 22.90, SE 0.15 (women) | ob: BMI ≥ 30 | ob: 3.56 (women) | *** |
| Sowers, 2006 [36] | Oakland, CA area | 151 (women) | 46.0 ± 2.4 (women) | 23.4 ± 4.2 (women) | *** | *** | *** |
| Sowers, 2003 [35] | Oakland, CA area | 220 (women) | 47 ± 2.7 (women) | 23.1 ± 3.9 (women) | *** | *** | *** |
| Torrens, 2004 [37] | Oakland, CA area | 210 (women) | 46 ± 2.7 (women) | 23.1 ± 3.8 (women) | *** | *** | *** |
| National Health Interview Surveyj | |||||||
| Oza-Frank, 2009 [5] | United States, 1997-2005 | 1510 | 40.7 (SE 0.6) | *** | ovl: 23.0≤BMI≤27.4 ov2: 25.0≤BMI≤29.9 obl: BMI≥27.5 ob2: BMI≥30 |
ov1: 38.2, SE 1.3l ov2: 20.6, SE 1.1l ob1: 8.8, SE 0.8l ob2: 4.2, SE 0.6l |
2.2, SE 0.7 l, m, n 3.8, SE 0.8 (ov1)l, m 5.2, SE 1.5 (ov2)l, m 11.2, SE 3.2 (ob1)l, m 16.8, SE 4.3 (ob2)l, m |
| Ye, 2009 [7] | United States, 2003-2005 | 559 | *** | *** | ob: BMI≥30 | ob: 4.2 | 5.5m |
| Other studies with Chinese participants | |||||||
| Babbar, 2006 [91] | New York City, NY | 300 (women) | 63.0 ± 8.2 (women) | 24.7 ± 4.0 (women) | *** | *** | *** |
| Chen, 2009 [63] | San Francisco Bay Area, CA | 65 (women) | *** | 23.1 ± 4.2 (women) | ov & ob: BMI>25o | ov & ob: 23.3 (women) | *** |
| Cotler, 2009 [67] | Chicago, IL | 2,457 | 55 ± 18 | 24 ± 4 | ob: BMI>25 | ob: 36 | 12g |
| Gomez, 2004 [2] | San Francisco, CAp | 263 (total) | *** | *** | ov: 26≤BMI≤30 ob: BMI>30j |
ov: 18.4q ob: 4.7q |
6.4m, q |
| Hung, 2009 [64] | New York City, NY | 2537 (total) | *** | *** | ov & ob: BMI>23r | ov & ob: 5.93, SE 0.61 | 3.96, SE 0.53m |
| Kim KK, 1993 [3] | Chicago, IL | 169 (total) 59 (men) 110 (women) |
74.6 (total) | 23.2± 3.7 (men) 23.3± 3.9 (women) |
ob: BMI>30.0 | ob: 3.6 (men) ob: 4.7 (women) |
*** |
| Lauderdale, 2003 [108] | Chicago, IL | 469 | 71 | *** | ov: 24.0≤BMI<26.5 ob: BMI≥26.5j |
ov: 26 ob: 23 |
*** |
| Maskarinec, 2001 [109] | Island of Oahu, HI | 73 (women) | 56.7 (women) | 22.8 (women) | *** | *** | *** |
| Maskarinec, 2000 [110] | Island of Oahu, HI | 73 (women) | 56.7 (women) | 22.8 (women) | *** | *** | *** |
| Mau, 2007 [4] | HIs | 81 | *** | *** | ov: 23≤BMI≤25t ob: BMI≥25 |
ov: 15 ob: 47 |
28u |
| Parikh, 2009 [90] | New York City, NY | 517 (total)v 336 (men) 181 (women) |
63.5, SE .38 (total) 64.3,SE .40 (men) 62.4,SE .61 (women) |
23.3 (total) 23.5 (men) 23.1 (women) |
ov: BMI 25.0-29.9 ob: BMI≥30 |
ov: 30.8 (total) ov: 33.0 (men) ov: 27.9 (women) ob: 2.4 (total) ob: 3.5 (men) ob: 0.9 (women) |
*** |
| Yates, 2004 [6] | HI | 45 (women) | *** | 19.35 ± 3.51 (women) | ob: BMI>30 | ob: 2 (women) | *** |
Data not included or specified.
Baltimore, MD; Chicago, IL; Forsythe County, N.C.; Los Angeles, CA; New York, NY; and St. Paul, MN
Based fasting glucose ≥ 126 mg/dl, or use of hypoglycemic medication
Based on self-report, fasting glucose ≥ 126 mg/dl, or use of hypoglycemic medication
Based fasting glucose > 126 mg/dl, or use of hypoglycemic medication
Estimates based on figure
Percent diabetes calculated by reviewer
Estimation method not specified
Longitudinal analysis
Based on self-report of diabetes treatment at any annual follow-up visit or based on a fasting glucose level of ≥ 126 mg/dl at the first and/or third follow-up
Authors reported a distribution of BMI rather than overweight or obesity explicitly
k U.S. nationally representative survey of non-institutionalized adults (18 and older)
Age and sex standardized to the 2000 U.S. population
Based on self-report
Among those with BMI 18.5-22.9 kg/m2
Reported as overweight in the publication
Hayward, Oakland, San Francisco, Santa Clara, and South San Francisco, CA
Adjusted for age and sex
Reported as BMI >23 kg/m2 for overweight and BMI >25 kg/m2 for obesity in the publication
Hawaii site for the Kidney Early Evaluation Program (KEEP-2)
Overweight was reported as BMI ≥23 in the publication with a prevalence of 15%
Based on self-reported history or a random blood glucose value ≥ 200 mg/dl (nonfasting)
Sample from New York City Chinese Health Study (NYC CHS), which used a complex multi-stage systematic stratified sampling design. May not be representative of frail elderly and the oldest old
Sex-specific estimates of percent overweight and obese were provided in a variety of ways across studies [3, 6, 34, 63, 90]. The highest estimates for overweight were from a subset of the New York City Chinese Health Study (NYC CHS), a population-based study of 55-75 year olds; the study reported 33% overweight (BMI = 25-29.9 kg/m2) among men and 27.9% overweight among women [90]. This was the only study that reported prevalence of overweight for men alone. The lowest estimates for overweight among women were reported in the SWAN study; 17.0% of women in this study were overweight (25≤ BMI >30 kg/m2) [34]. Only two estimates for percent obesity were found, and both were similar (3.5%, BMI ≥ 30 kg/m2) and 3.6%, BMI >30.0) [3, 90]. In women, obesity ranged from 0.9% to 11% [3, 6, 26, 28, 30, 34, 90].
Mean BMI ranged from 23.3 kg/m2 (Chinese participants aged 55-75 years subset from the NYC CHS) [90] to 25.8 kg/m2 (U.S.-born Chinese aged 45-84 years at baseline from the MESA study) among men and women [15]. Among men only, mean BMI ranged from 23.2 kg/m2 in elderly Chicago residents [3] to 24.1 kg/m2 in MESA participants [13]. Among women, the lowest mean BMI (19.4 kg/m2) was reported in a convenience sample of community college students [6] and the greatest (24.7 kg/m2) in a convenience sample of postmenopausal women from New York City's Chinatown [91]. Mean BMI in SWAN was 22.5 - 23.4 kg/m2 [3, 26, 27, 29, 31, 32, 35-37].
Diabetes prevalence estimates varied across studies. In a pooled NHIS analysis (1997-2005), 2.2% of normal weight Chinese (BMI 18.5-22.9 kg/m2), 3.8% of overweight Chinese (BMI 23.0-27.4 kg/m2), and 11.2% of obese Chinese (BMI ≥ 27.5 kg/m2) had self-reported diabetes (all data age- and sex-standardized to the 2000 U.S. population) [5]. Those with BMI ≥ 30 kg/m2 had 16.8% diabetes. Across all articles in the Chinese subgroup, the greatest prevalence diabetes was reported at 28% among Chinese participants in Hawaii, based on self-report or random, nonfasting blood glucose levels at 200 mg/dl or greater [4]. In MESA, 15.2% had diabetes based on a definition that included self-report, fasting glucose ≥ 126 mg/dl, or by use of hypoglycemic medication [9, 10].
Filipino
Among the 22 publications with Filipinos, all data were cross-sectional (Table 4). Seven publications reported population-based data from NHIS [5, 7], BRFS in Guam [47, 48], or the Kōhala Health Research Study/Native Hawaiian Health Research Project (NHHR) in rural North Kōhala, Hawaii [41, 45, 46]. In NHIS (1997-2005), 46.5% of individuals were overweight and 20.8% of individuals were obese (n = 1485, age- and sex- standardized) using WHO Asian specific definitions for overweight and obesity [5]. While data from NHIS 2003-2005 indicate that 13.2% of Filipinos were obese (BMI ≥ 30 kg/m2) [7], pooled NHIS data from 1997 – 2005 show that 10.2% were obese [5], reflecting the increase in obesity over time. The lowest mean BMI among Filipinos was reported in Guam at 23.1 kg/m2 (age-adjusted) for men and women combined, 25.7 kg/m2 for men only, and 22.8 kg/m2 for women only [47, 48]. Mean BMI among men and women from the NHHR project ranged from 26.0 kg/m2 to 26.8 kg/m2, with the latter estimate as the greatest estimate in the Filipino subgroup [41, 45, 46]. Among women, mean BMI was 21.7 kg/m2 among community college students in Hawaii [6], between 24.3 kg/m2 (age-adjusted) to 25.6 kg/m2 among 40 to 86 year olds from San Diego county [38-44], 25.4 kg/m2 (age-adjusted) among postmenopausal women in northern San Diego County [49, 50], and 26.0-26.8 kg/m2 in the NHHR project [41, 45, 46]. Only one estimate was provided for men (mean BMI 25.7 kg/m2) [48].
Table 4.
Results of a Systematic Review of Mean BMI, Percent Overweight (ov)/Obese (ob), and Prevalence of Diabetes in Asians: Filipino References (n=22)
| Reference | City, State | Sample Size | Mean Age in Years ± SD | Mean BMI in kg/m2 ± SD | Definition of ov, ob by BMI (kg/m2) | Ov, ob, % | Diabetes, % |
|---|---|---|---|---|---|---|---|
| The University of California San Diego Filipino Women's Health Study | |||||||
| Araneta 2007 [40] | San Diego area, CA | 136 (women) | 54.2 (women) | 24.3 (women)a | *** | *** | *** |
| Araneta 2006 [41]b | San Diego, CA | 446 (women) | 57.6, 95% CI: 56.7, 58.5 (women) | 25.4, 95% CI: 25.0, 25.8 (women)a | ob1: BMI≥25 ob2: BMI≥30 |
ob1: 49.2 (women)a ob2: 9.3 (women)a |
31.6 (women)a, c 24.9 (women)a, c |
| Araneta 2005 [39] | San Diego area, CA | 181 (women) | 64.4 (women) | 25.5 (women)a | *** | *** | 32.1 (women) c |
| Araneta 2004 [38] | San Diego area, CA | 181 (women) | 64.4 ± 6.0 (women) | 25.6 ± 3.4 (women)a | *** | *** | 32.6 (women)a, c |
| Araneta 2002 [42] | San Diego area, CA | 294 (women) | 59.7 ± 5.2 (women) | 25.6 ± 3.5 (women) | *** | *** | 36.4 (women)c |
| Magno 2008 [43] | San Diego area, CA | 211 (women)d | 57.3, SE 0.68 (women) | 25.1, SE0.23 (women) | *** | *** | 27.5 (women)c |
| Wong 2008 [44] | San Diego area, CA | 163 (women) | 59.3 - 60 (women)e | 25.1 - 26.3 (women))e, a | *** | *** | 34.4 (women)c |
| Kohala Health Research Project / Native Hawaiian Health Research Project | |||||||
| Araneta 2006 [41]b | North Kohala, HI | 109 (women) | 57.9, 95% CI: 56.0, 59.8 (women) | 26.0, 95% CI: 24.8, 26.5 (women)a | ob1: BMI≥25 ob2: BMI≥30 |
ob1: 50.5 (women)a ob2: 20.1 (women)a |
24.9 (women)a,c |
| Grandinetti 2007 [45] | North Kohala, HI | 186 | 53.7 ± 16.2 | 26.1 ± 5.8 | *** | *** | 19.35f |
| Kim 2008 [46] | North Kohala, HI | 261 | 50.0 ± 16.3 | 26.8 ± 5.7 | *** | *** | 20.3g 30.9 g (among those with age ≥50 years) 8.3g (among those with age <50 years) |
| The University of California San Diego (UCSD) Rancho Bernardo Study | |||||||
| Araneta 2010 [49] | San Diego, CA | 152 (women) | 59.5 (women) | 25.4 (women) | *** | *** | 33.6 (women)c |
| Morton 2003 [50] | San Diego, CA | 285 (women) | 59.9, 95% CI 59.3, 60.5 (women) | 25.4, 95% CI: 24.0 - 25.9 (women)a | *** | *** | *** |
| Behavioral Risk Factor Survey (BRFS)h - Guam | |||||||
| Pinhey 1995 [47] | Guam | 342i | *** j | 23.09a | *** | *** | *** |
| Pinhey 1994 [48] | Guam | 115 (total) 49 (men) 66 (women) |
48.1 ± 15.9 (men) 41.6 ± 12.6 (women) |
25.7± 3.8 (men) 22.8± 4.4 (women) |
ob: BMI ≥ 27 | Ob: 21.2 (total) | *** |
| National Health Interview Survey (NHIS)k | |||||||
| Oza-Frank 2009 [5] | United States, 1997-2005 | 1485 | 41.2, SE 0.4 | *** | ovl: 23.0≤BMI≤27.4 ov2: 25.0≤BMI≤29.9 obl: BMI≥27.5 ob2: BMI≥30 |
ov1: 46.5, SE 1.7l ov2: 34.5, SE 1.4l ob1: 20.8, SE 1.3l ob2: 10.2, SE 1.0l |
5.9, SE 3.7 l, m
n 3.7, SE 0.7 (ov1)l, m 6.2, SE 1.1 (ov2)l, m 11.3, SE 2.0 (ob1)l, m 10.9, SE 3.0 (ob2)l, m |
| Ye 2009 [7] | United States, 2003-2005 | 633 | *** | *** | ob: BMI≥ 30 | Ob: 13.2 | 6.1m |
| Other studies with Filipino participants | |||||||
| Cuasay 2001 [55] | Metropolitan Houston, TX | 831 | 46.1 ± 12.0 | 24.6 ± 3.6 | *** | *** | 16.1. 95% CI: 13.5, 18.7 (total)o, p 13.1, 95% CI: 10.0, 16.2(womenp, q 19.7, 95% CI: 15.1, 24.3(men)p, q 15.1, 95% CI: 12.4-17.8 (among BMI≤30)p, q 30.0, 95% CI: 16.6-43.4 (among BMI>30)p, q |
| Gomez 2004 [2] | San Francisco, CAr | 268 (total) | *** | *** | ov: 26≤BMI≤30s ob: BMI > 30s |
ov: 29.2 ob: 8.6 |
21.2 m, t |
| Guerrero 2008 [111] | Guam | 61 (total) 33 (women) |
*** | 25.9 (total) 24.4 ± 3.6 (women) |
ov: 25.0≤BMI≤29.9 ob: BMI ≥ 30 |
ov: 30.3 (female) ob: 9.1 (female) ob: 20 (total) |
*** |
| Langenberg 2007 [112] | North San Diego, CA | 389 (women) | 58.7 ± 9.4 (women) | 25.3, 95% CI: 24.9, 25.6 (women) | ob: not defined | ob: 9.8, 95% CI: 6.8, 12.7 (women) | 31.4, 95% CI: 26.7, 36.0 (women)c |
| Mau 2007 [4] | HIu | 134 | *** | *** | ov: 23≤BMI≤25v ob: BMI≥25 |
ov: 15 ob: 59 |
20w |
| Novotny 1998 [113] | HI | 74 (women) | *** x | 23.8 ± 4.5 (women) | *** | *** | *** |
| Yates 2004 [6] | HI | 59 (women) | *** | 21.71 ± 3.86 (women) | *** | *** | *** |
Data not included or specified
Adjusted for age
Araneta 2006 provides separate estimates from two studies (in California and in Hawaii) and it is listed under two sections: The University of California San Diego Filipino Women's Health Study and the Kōhala Health Research Project / Native Hawaiian Health Research Project
Based on 1999 World Health Organization criteria: fasting plasma glucose ≥ 126 mg/dl; 2-hour postchallenge glucose ≥ 200 mg/dL; history of type 2 diabetes diagnosed by a physician; or history of treatment with oral hypoglycemic agent or insulin
Study reported additional data on 55 women with cardiovascular disease but these data are not included here due to exclusion criteria
Mean age/BMI stratified by those with and without diabetes
Based on 1998 WHO criteria for diabetes and abnormalities of glucose regulation
Based on 1998 WHO criteria for diabetes: 2-hour plasma glucose 200 mg/dl; or fasting plasma glucose ≥ 126 mg/dl
Survey representative of the non-institutionalized, adult (18 and older) population in Guam
Portion of total sample without hypertension
Aged 30 years and older
U.S., nationally representative survey of non-institutionalized, adults (18 and older)
Age and sex standardized to the 2000 U.S. population
Based on self-report
Among those with BMI 18.5-22.9 kg/m2
Unweighted, unadjusted prevalence
Based on subjects' self-report. Presence of diabetes confirmed with questions on the questionnaire regarding the year and/or individuals age at diagnosis of diabetes, blood and OGTT, therapy used, frequency of blood tests, and doctors’ visits
Weighted prevalence
Hayward, Oakland, San Francisco, Santa Clara, & South San Francisco, CA
Authors reported a distribution of BMI rather than overweight or obesity explicitly
Adjusted for age and sex
Hawaii site for Kidney Early Evaluation Program (KEEP-2)
Overweight was reported as BMI ≥ 23 in publication with a prevalence of 15%
Based on prior history or a random blood glucose value ≥ 200mg/dL (non-fasting)
Women were between 25 and 35 years of age, mean age not provided
From 2003-2005, 6.1% Filipinos had diabetes in NHIS [7]. Pooled NHIS estimates of 1997 – 2005 diabetes prevalence (age- and sex- standardized) were as follows: 5.9% for normal weight (BMI 18.5-22.9 kg/m2) Filipinos, 3.7% for overweight (BMI 23.0-27.4 kg/m2), and 11.3% for obese (BMI ≥ 27.5 kg/m2) [5]. Among Filipinos with BMI ≥ 30 kg/m2,10.9% had diabetes [5]. Articles using other data sources estimated higher prevalence rates. In a study of men and women from five northern California Kaiser Permanente Medical Care Program centers, 21.2% had diabetes (age- and sex- adjusted) [2]. Across three publications on the NHHR project, 19.4-24.9% total diabetes prevalence was reported [41, 45, 46], with a higher prevalence (30.9%) among individuals 50 years and older [46]. Publications on the UCSD Filipino Women's Health Study reported 27.5 - 36.4% diabetes.
Korean
Two of the eight cross-sectional studies reporting on Koreans contained population-based samples (Table 5): the California Health Interview Survey (CHIS) randomly selected 492 Korean American adults, representing 330,000 Korean American adults in California in 2003 [60], and the Hypertension Screening Project for Korean Americans in Maryland (HSP) used a stratified sampling method to include 76 Korean Americans between 1998 and 1999 [66]. The CHIS study [60] reported percent overweight (defined by 2004 WHO definitions for Asians) as 38.4% for the entire sample, 49.0% among men, and 30.7% among women. Percent obese in the total sample was 7.5%, or 10.7% of men and 5.2% of women. The Multiethnic Cohort Study in Hawaii and Los Angeles reported that percent overweight or obese (BMI ≥ 25 kg/m2) was 31.4% for U.S.-born women and 9.4% for Korea-born women [56]. Finally, another study of Korean elderly (age 60-95, n=90) in Chicago found 6.3% obesity in men and 5.0% obesity in women, defined as BMI ≥ 30 kg/m2 [3]. BMI for Korean men ranged from 23.3 kg/m2 for elderly men living in Chicago to 24.9 kg/m2 among acculturated men in California [3, 92]. Reports of mean BMI for women ranged from 22.1 kg/m2 among Korean-born women and traditional Korean women [56, 92] to 26.3 kg/m2 among elderly Koreans in Washington State [74].
Table 5.
Results of a Systematic Review of Mean BMI, Percent Overweight (ov)/Obese (ob), and Prevalence of Diabetes in Asians: Korean references (n=8)
| Reference | City, State | Sample Size | Mean Age in Years ± SD | Mean BMI in kg/m2 ± SD | Definition of ov, ob by BMI (kg/m2) | Ov, ob, % | Diabetes, % |
|---|---|---|---|---|---|---|---|
| Cho 2006 [60] | CAa | 492 | 48.5 | *** | ov: BMI 23-27.4 ob: BMI ≥ 27.5 |
ov: 38.38, SE 2.95 (total) ov: 49.03, SE 4.99 (men) ov: 30.69, SE 3.82 (women) ob: 7.51, SE 1.36 (total) ob: 10.67, SE 2.82 (men) ob: 5.22, SE 1.31 (women) |
*** |
| Kim KK 1993 [3] | Chicago, IL | 90 (total) 30 (men) 60 (women) |
72.1 (total) | 23.3 ± 4.5 (men) 24.2 ± 3.6 (women) |
ob: BMI>30.0 | ob: 6.3 (men) ob: 5.0 (women) |
*** |
| Kim, MT 2001 [65] | Baltimore, MD | 205 (total) 75 (men) 130 (women) |
69.9 ± 6.5 (total) 69.2 ± 5.9 (men) 69.9 ± 6.8 (women) |
24.5± 3.5 (total) 24.3 ± 3.8 (men) 24.6± 3.3 (women) |
ov & ob: BMI ≥ 25b | ov & ob: 43.3 (total) ov & ob: 45.3 (men) ov & ob: 42.3 (women) |
18.1 (total)c 22.7 (men)c 15.4 (women)c |
| Kim, MT 2000 [66] | MD | 761 | 50.5 | *** | ov & ob: BMI ≥ 25b | ov & ob: 28 | *** |
| Park 2005 [56] | Los Angeles, CA & HI | 274 (U.S.-born) 218 (Korea-born) |
62.5 ± 8.4 (women, U.S.-born) 53.5 ± 6.6 (women, Korea-born) |
23.6 ± 4.1 (women, U.S.-born)d 22.1 ± 4.2 (women, Korea-born)d |
ov or ob: BMI≥25 | ov or ob:31.4 (women, U.S.-born) d ov or ob: 9.4 (women, Korea-born) d |
*** |
| Sin 2009 [74] | WAe | 87 (total) 49 (men) 38 (women) |
78 ± 6.58 (men) 73 ± 5.39 (women) |
25.4 (total) 24.6 ± 2.44 (men) 26.3 ± 4.58 (women) |
*** | *** | *** |
| Song 2004 [92] | CAf | 1026 (traditional males) 211 (bicultural males) 97 (acculturated males) 1220 (traditional females) 205 (bicultural females) 71 (acculturated females) |
*** | 24.2,SE 0.1 (traditional males) 24.4, SE 0.2 (bicultural males) 24.9, SE 4.1 (acculturated males) 22.1, SE 0.1 (traditional female) 21.6, SE 0.2 (bicultural females) 21.3,SE0.4 (acculturated females) |
*** | *** | *** |
| Yang 2007 [57] | MI | 263 (men) 234 (women) |
53.8 ± 11.2 (men) 49.0 ± 11.0 (women) |
24.0 ± 0.2 (men)g 22.4 ± 0.2 (women)g |
*** | *** | 11 (men)g, h 10 (women)g, h |
Data not included or specified
Data from the California Health Interview Survey, a statewide survey representative of non-institutionalized adults 18 and older
Reported as overweight in this publication
Based on 1997 National Diabetes Data Group's diagnostic criteria of fasting glucose ≥ 126 mg/dl
Adjusted for age and education
King County, Snohomish County, and Pierce County, WA
Representative sample of Korean adults living in CA with telephones and Korean surnames
Adjusted for age
Based on self-report
Only two studies reported percent diabetes among Koreans in the U.S.. Among 497 Korean Americans residing in Michigan, 11% of men and 10% of women had self-reported diabetes (age-adjusted) [57]. Among elderly Koreans from Maryland, 22.7% of males and 15.4% of females had diabetes (fasting glucose ≥ 126 mg/dl) [65].
Vietnamese
Limited information was published for Vietnamese Americans (Table 6). A population sample from the Centers for Disease Control and Prevention (CDC) Racial and Ethnic Approaches to Community Health (REACH) 2010 program was collected, surveying Vietnamese residents of Santa Clara County, CA who were 18 years of age and older. Among Vietnamese, 17.3% were overweight (BMI ≥ 25.0 and <30 kg/m2) and 2.1% (95% CI: 1.6, 2.7) were obese (BMI ≥ 30 kg/m2) [58]. Among Vietnamese refugees who arrived to one Texas city and were screened, 12.3% were overweight (BMI ≥25 kg/m2) [62]. Mean BMI was not reported. Two publications reported percent self-reported diabetes, ranging from 5.3% (age-standardized) to 15.6% (adjusted for age, sex, and education) [58, 93].
Table 6.
Results of a Systematic Review of Mean BMI, Percent Overweight (ov)/Obese (ob), and Prevalence of Diabetes in Asians: Vietnamese References (n=3)
| Reference | City, State | Sample Size | Mean Age in Years ± SD | Mean BMI in kg/m2 ± SD | Definition of ov, ob by BMI (kg/m2) | Ov, ob, % | Diabetes, % |
|---|---|---|---|---|---|---|---|
| Barnes 2004 [62] | TX | 114a | *** | *** | ov & ob: BMI ≥ 25b | ov & ob: 12.3 | *** |
| Nguyen 2009 [58] | 4254c | 18-34 years = 26.7%, 95% CI: 25.1, 28.3 35-54 years = 43.8% 95% CI: 42.2, 45.4 55+ years = 29.5% 95% CI: 28.0, 30.9 |
*** | ov: 25.0 ≤ BMI < 30 ob: BMI ≥ 30 |
ov: 17.3, 95% CI: 16.0, 18.7d ob: 2.1, 95% CI: 1.6, 2.7d |
5.3, 95% CI: 4.7, 6.0d,e | |
| Sorkin 2008 [93] | CA | 359f | 64.6 | *** | *** | *** | 15.6e,g |
Data not included or specified
Population-based survey of refugees in a city in TX
Reported as overweight in publication
From the CDC Racial and Ethnic Approaches to Community Health 2010 program
Age-standardized
Based on self-report
Data from the California Health Interview Survey, a statewide survey representative of non-institutionalized adults 18 and older
Adjusted for age, sex, and education
DISCUSSION
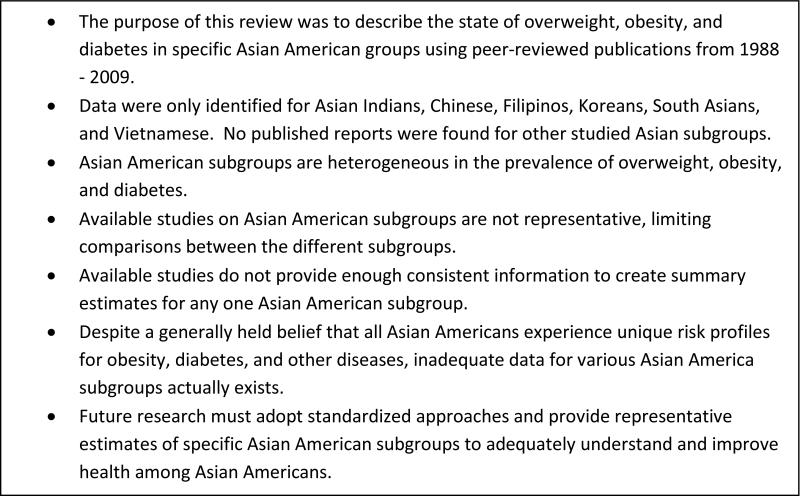
The purpose of this review was to systematically describe the state of overweight, obesity, and diabetes in specific Asian American subgroups. Our findings and key discussion points are summarized in Figure 4. Contrary to common approaches that generalize across Asians, the results of this review suggest that Asian American subgroups are vastly heterogeneous for these conditions, and generalizing them into one “Asian” group may be inappropriate. Also, despite the high volume of published reports on these conditions, this review reveals that representative studies are sorely lacking, exposing the inability to create summary estimates for specific Asian America subgroups, thereby prohibiting between-group comparisons of disease prevalence and risk factor associations. Among reported estimates for men and women, prevalence of overweight varied from 12.8 – 46.7% in Asian Indians, 15.0 – 38.2% in Chinese, and 15.0 – 46.5% in Filipinos; similarly, reports of obesity varied from 5.0 – 49.8% in Asian Indians, 2.4 – 47.0% in Chinese, and 8.6 – 59.0% in Filipinos. Only one or no estimate was provided for men and women in the other Asian subgroups. Reported prevalence of diabetes in samples of men and women ranged from 3.9 – 32.9% in Asian Indians, 1.0 - 11.3% in the South Asian category, 2.2 - 28% in Chinese, 3.7 – 30.9% in Filipinos, and 5.3 - 15.6% in Vietnamese, with one estimate for Koreans (18.1%).
Figure 4.
Key Messages
A major finding of this review was that most studies about Asian American subgroups utilize designs that prohibit between-subgroup and within-subgroup comparisons. Many of the studies drew convenience samples from specific geographic regions, defined unique inclusion/exclusion criteria, and employed different definitions of overweight, obesity, and diabetes, limiting generalizability of data. In addition, studies did not always provide measures of overweight and obesity alongside measures of diabetes, making it difficult to study the relationship between overweight and diabetes. Approximately half of all articles were from seven studies: MESA, SWAN, Filipino Women's Health Study, HHR, BRFS in Guam, Rancho Bernardo Study, and NHIS, of which only NHIS was nationally representative. For the 20% of all studies that accounted for confounding factors (i.e., age, sex) in their estimates, differing approaches were employed (e.g., age adjustment using study sample versus age-standardization to external population), also impacting comparability. Ultimately, these results provide conclusive evidence that standardized approaches to surveying Asian American subgroups are needed.
This systematic review has several limitations. All studies defined individuals based on country of origin rather than by genotypes of ethnicity, which could also play a role in prevalence differences. Additionally, the review covers a 20-year period that coincides with the rapid increases in the overall BMI among U.S. adults, making it difficult to distinguish overweight associated with ethnicity compared to overweight associated with the time period. Another limitation of this review is the ability to account for immigration and generation. First or second generation immigrants experience different obesity and disease rates compared to their ancestors [94]. Immigrants tend to have lower BMI upon migration, and foreign-born Asian Americans are significantly less overweight and obese than U.S.-born Asian Americans, though increased duration of residence in the U.S. is correlated with increased obesity [95-98]. Studies of Asian Americans by immigrant generational status also have observed a trend of increasing obesity and diabetes with later generations [99]. For example, the prevalence of diabetes is approximately 4 times higher among second-generation Japanese-Americans than among native Japanese [100].
Despite these limitations, the strengths of this review include the rigorous search for publications, which was systematic and thorough. With professional consultation in biomedical database searching and management from an experienced university librarian, the results of the PubMed search and the hand searches identified those publications which the authors expected to find based on their expertise in chronic disease epidemiology, medicine, and Asian American culture, attitudes, and beliefs. The searches also identified additional publications relevant to the review topic. In addition to the rigorous search, another strength is that the Asian American population is particularly well-suited to study differences in the relationship between overweight, obesity, and diabetes because the relationship in this population seems to be unique and may assist in unveiling underlying mechanisms of these health conditions [101]. Historically, data presenting the prevalence of diabetes, overweight, and obesity among Asian American populations have included them as a one collective group, but more recently, literature has emerged showing variations in diabetes and obesity risk when comparing specific Asian American subgroups to whites or blacks. Since 1960, the U.S. Asian population has increased almost fivefold, with more than 14 million Asians in the U.S. in 2009 and accounting for nearly 28% of the nation's foreign-born population [102]. Continued research on the heterogeneity in diabetes occurrence and risks among Asian Americans is necessary considering that this population is projected to comprise 9% of the total U.S. population by 2050 [103] and that the number of people living with diabetes is projected to increase from 366 million in 2011 to 552 million by 2030 [104]. It is of critical importance to study the relationship between ethnicity and chronic disease now, before extensive intermarriages between Asians and non-Asians makes it more difficult to identify and recruit specific Asian subgroups for studies.
Given the rapid recent and projected growth of the Asian American population, national surveys can improve surveillance and monitoring of this group through integration into existing systems [105] (i.e., BRFS, NHIS, NHANES) and through oversampling of Asian American subgroups. This would enhance national data and could be used to establish better prevalence estimates across Asian subgroups in the U.S. [106]. This includes Japanese Americans, a subgroup that was excluded from this study because Japanese migration to the U.S. occurred before the 20-year period of interest and Japanese Americans (1st, 2nd, and 3rd generation) have been extensively studied previously, unlike the Asian subgroups included in this review. In addition, large-scale population based analyses addressing more complex disease determinants of obesity and diabetes (beyond single gene polymorphisms) might improve the understanding of the relative impact of genetic and environmental factors linking them. Identifying the key risk factors and pathophysiolgical mechanism that lead to disease is essential to understanding the etiology of the disease and for the development of sound policies, including prevention and treatment strategies, for improved health among Asians.
In summary, this review summarized and synthesized data published in the past 20 years on the prevalence of diabetes, overweight, and obesity among Asian American sub-populations in the U.S. Although this review showed there are differences across Asian American subgroups, quantifying these differences is challenging because of the lack of nationally representative, standardized data within the Asian American group, a large, growing, and heterogeneous population. Future efforts to estimate levels of overweight, obesity, and diabetes must standardize approaches and include specific subgroups of Asian Americans to better understand and improve the health of these minorities in the United States.
Acknowledgements
The authors’ contributions are as follows: LRS designed and conducted literature searches, coordinated abstract and full-text review, extracted data, analyzed results, and contributed to drafting and editing the manuscript. MBW: contributed to drafting and editing the manuscript, reviewed abstracts and full-text articles, and extracted data. KMVN: provided guidance and edited the manuscript. ROF: conceptualized project, reviewed abstracts and full-text articles, extracted data, and contributed to drafting and editing the manuscript. Other contributors: Barbara Abu-Zeid assisted with search strategy design, biomedical database searching, and management; Aaron Gregg and Sumathee Selvaraj assisted with data management. LRS is supported by the Molecules to Mankind Program of the Burroughs Wellcome Fund. MBW is supported by an NIH T32 post-doctoral training grant (5T32DK007298-33). These results were presented in part at the 72nd Annual Scientific Sessions of the American Diabetes Association, June 8-12, 2012, Philadelphia, PA [107].
Footnotes
Conflict of Interest
The authors have no conflict of interest.
References
- 1.United States Census Bureau [12 December 2011];Profile America: Facts for Features - Asian/Pacific American Heritage Month: May 2011 (CB11-FF.06) 2011 Available from: http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb11-ff06.html.
- 2.Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S. Immigration and acculturation in relation to health and health-related risk factors among specific Asian subgroups in a health maintenance organization. Am J Public Health. 2004;94:1977–84. doi: 10.2105/ajph.94.11.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim KK, Yu ES, Liu WT, Kim J, Kohrs MB. Nutritional status of Chinese-, Korean-, and Japanese-American elderly. J Am Diet Assoc. 1993;93:1416–22. doi: 10.1016/0002-8223(93)92245-s. [DOI] [PubMed] [Google Scholar]
- 4.Mau MK, West MR, Shara NM, et al. Epidemiologic and clinical factors associated with chronic kidney disease among Asian Americans and Native Hawaiians. Ethn Health. 2007;12:111–27. doi: 10.1080/13557850601081720. [DOI] [PubMed] [Google Scholar]
- 5.Oza-Frank R, Ali MK, Vaccarino V, Narayan KM. Asian Americans: diabetes prevalence across U.S. and World Health Organization weight classifications. Diabetes Care. 2009;32:1644–6. doi: 10.2337/dc09-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yates A, Edman J, Aruguete M. Ethnic differences in BMI and body/self-dissatisfaction among Whites, Asian subgroups, Pacific Islanders, and African-Americans. J Adolesc Health. 2004;34:300–7. doi: 10.1016/j.jadohealth.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Ye J, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol. 2009;19:718–23. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allison MA, Budoff MJ, Nasir K, et al. Ethnic-specific risks for atherosclerotic calcification of the thoracic and abdominal aorta (from the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol. 2009;104:812–7. doi: 10.1016/j.amjcard.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allison MA, Cushman M, Solomon C, et al. Ethnicity and risk factors for change in the ankle-brachial index: the Multi-Ethnic Study of Atherosclerosis. J Vasc Surg. 2009;50:1049–56. doi: 10.1016/j.jvs.2009.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:2138–45. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bertoni AG, Goff DC, Jr., D'Agostino RB, Jr., et al. Diabetic cardiomyopathy and subclinical cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2006;29:588–94. doi: 10.2337/diacare.29.03.06.dc05-1501. [DOI] [PubMed] [Google Scholar]
- 12.Bild DE, Detrano R, Peterson D, et al. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2005;111:1313–20. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 13.Burke GL, Bertoni AG, Shea S, et al. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:928–35. doi: 10.1001/archinte.168.9.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colangelo LA, Ouyang P, Liu K, et al. Association of endogenous sex hormones with diabetes and impaired fasting glucose in men: multi-ethnic study of atherosclerosis. Diabetes Care. 2009;32:1049–51. doi: 10.2337/dc08-2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diez Roux AV, Detrano R, Jackson S, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112:1557–65. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 16.Duprez DA, Jacobs DR, Jr., Lutsey PL, et al. Race/ethnic and sex differences in large and small artery elasticity--results of the multi-ethnic study of atherosclerosis (MESA). Ethn Dis. 2009;19:243–50. [PMC free article] [PubMed] [Google Scholar]
- 17.Gao SK, Beresford SA, Frank LL, Schreiner PJ, Burke GL, Fitzpatrick AL. Modifications to the Healthy Eating Index and its ability to predict obesity: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2008;88:64–9. doi: 10.1093/ajcn/88.1.64. [DOI] [PubMed] [Google Scholar]
- 18.Kandula NR, Diez-Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA). Diabetes Care. 2008;31:1621–8. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz R, Wong ND, Kronmal R, et al. Features of the metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the Multi-Ethnic Study of Atherosclerosis. Circulation. 2006;113:2113–9. doi: 10.1161/CIRCULATIONAHA.105.598086. [DOI] [PubMed] [Google Scholar]
- 20.Klein R, Klein BE, Knudtson MD, et al. Prevalence of age-related macular degeneration in 4 racial/ethnic groups in the multi-ethnic study of atherosclerosis. Ophthalmology. 2006;113:373–80. doi: 10.1016/j.ophtha.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 21.Kramer H, Han C, Post W, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA). Am J Hypertens. 2004;17:963–70. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Ouyang P, Vaidya D, Dobs A, et al. Sex hormone levels and subclinical atherosclerosis in postmenopausal women: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2009;204:255–61. doi: 10.1016/j.atherosclerosis.2008.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palmas W, Ma S, Jacobs DR, Jr., et al. Ethnicity and sex modify the association of serum c-reactive protein with microalbuminuria. Ethn Dis. 2008;18:324–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Paramsothy P, Knopp R, Bertoni AG, Tsai MY, Rue T, Heckbert SR. Combined hyperlipidemia in relation to race/ethnicity, obesity, and insulin resistance in the Multi-Ethnic Study of Atherosclerosis. Metabolism. 2009;58:212–9. doi: 10.1016/j.metabol.2008.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong TY, Islam FM, Klein R, et al. Retinal vascular caliber, cardiovascular risk factors, and inflammation: the multi-ethnic study of atherosclerosis (MESA). Invest Ophthalmol Vis Sci. 2006;47:2341–50. doi: 10.1167/iovs.05-1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matthews KA, Abrams B, Crawford S, et al. Body mass index in mid-life women: relative influence of menopause, hormone use, and ethnicity. Int J Obes Relat Metab Disord. 2001;25:863–73. doi: 10.1038/sj.ijo.0801618. [DOI] [PubMed] [Google Scholar]
- 27.Everson-Rose SA, Meyer PM, Powell LH, et al. Depressive symptoms, insulin resistance, and risk of diabetes in women at midlife. Diabetes Care. 2004;27:2856–62. doi: 10.2337/diacare.27.12.2856. [DOI] [PubMed] [Google Scholar]
- 28.Gold EB, Sternfeld B, Kelsey JL, et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. Am J Epidemiol. 2000;152:463–73. doi: 10.1093/aje/152.5.463. [DOI] [PubMed] [Google Scholar]
- 29.Greendale GA, Huang MH, Wang Y, Finkelstein JS, Danielson ME, Sternfeld B. Sport and home physical activity are independently associated with bone density. Med Sci Sports Exerc. 2003;35:506–12. doi: 10.1249/01.MSS.0000056725.64347.C9. [DOI] [PubMed] [Google Scholar]
- 30.Habel LA, Capra AM, Oestreicher N, et al. Mammographic density in a multiethnic cohort. Menopause. 2007;14:891–9. doi: 10.1097/gme.0b013e318032569c. [DOI] [PubMed] [Google Scholar]
- 31.Kelley-Hedgepeth A, Lloyd-Jones DM, Colvin A, et al. Ethnic differences in C-reactive protein concentrations. Clin Chem. 2008;54:1027–37. doi: 10.1373/clinchem.2007.098996. [DOI] [PubMed] [Google Scholar]
- 32.Lasley BL, Santoro N, Randolf JF, et al. The relationship of circulating dehydroepiandrosterone, testosterone, and estradiol to stages of the menopausal transition and ethnicity. J Clin Endocrinol Metab. 2002;87:3760–7. doi: 10.1210/jcem.87.8.8741. [DOI] [PubMed] [Google Scholar]
- 33.Lo JC, Zhao X, Scuteri A, Brockwell S, Sowers MR. The association of genetic polymorphisms in sex hormone biosynthesis and action with insulin sensitivity and diabetes mellitus in women at midlife. Am J Med. 2006;119:S69–78. doi: 10.1016/j.amjmed.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 34.Matthews KA, Sowers MF, Derby CA, et al. Ethnic differences in cardiovascular risk factor burden among middle-aged women: Study of Women's Health Across the Nation (SWAN). Am Heart J. 2005;149:1066–73. doi: 10.1016/j.ahj.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 35.Sowers M, Crawford SL, Cauley JA, Stein E. Association of lipoprotein(a), insulin resistance, and reproductive hormones in a multiethnic cohort of pre- and perimenopausal women (The SWAN Study). Am J Cardiol. 2003;92:533–7. doi: 10.1016/s0002-9149(03)00720-3. [DOI] [PubMed] [Google Scholar]
- 36.Sowers MR, Wilson AL, Karvonen-Gutierrez CA, Kardia SR. Sex steroid hormone pathway genes and health-related measures in women of 4 races/ethnicities: the Study of Women's Health Across the Nation (SWAN). Am J Med. 2006;119:S103–10. doi: 10.1016/j.amjmed.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 37.Torrens JI, Skurnick J, Davidow AL, et al. Ethnic differences in insulin sensitivity and beta-cell function in premenopausal or early perimenopausal women without diabetes: the Study of Women's Health Across the Nation (SWAN). Diabetes Care. 2004;27:354–61. doi: 10.2337/diacare.27.2.354. [DOI] [PubMed] [Google Scholar]
- 38.Araneta MR, Barrett-Connor E. Subclinical coronary atherosclerosis in asymptomatic Filipino and white women. Circulation. 2004;110:2817–23. doi: 10.1161/01.CIR.0000146377.15057.CC. [DOI] [PubMed] [Google Scholar]
- 39.Araneta MR, Barrett-Connor E. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and white women. Obes Res. 2005;13:1458–65. doi: 10.1038/oby.2005.176. [DOI] [PubMed] [Google Scholar]
- 40.Araneta MR, Barrett-Connor E. Adiponectin and ghrelin levels and body size in normoglycemic Filipino, African-American, and white women. Obesity (Silver Spring) 2007;15:2454–62. doi: 10.1038/oby.2007.291. [DOI] [PubMed] [Google Scholar]
- 41.Araneta MR, Morton DJ, Lantion-Ang L, et al. Hyperglycemia and type 2 diabetes among Filipino women in the Philippines, Hawaii, and San Diego. Diabetes Res Clin Pract. 2006;71:306–12. doi: 10.1016/j.diabres.2005.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Araneta MR, Wingard DL, Barrett-Connor E. Type 2 diabetes and metabolic syndrome in Filipina-American women : a high-risk nonobese population. Diabetes Care. 2002;25:494–9. doi: 10.2337/diacare.25.3.494. [DOI] [PubMed] [Google Scholar]
- 43.Magno CP, Araneta MR, Macera CA, Anderson GW. Cardiovascular disease prevalence, associated risk factors, and plasma adiponectin levels among Filipino American women. Ethn Dis. 2008;18:458–63. [PubMed] [Google Scholar]
- 44.Wong CA, Araneta MR, Barrett-Connor E, Alcaraz J, Castaneda D, Macera C. Probable NAFLD, by ALT levels, and diabetes among Filipino-American women. Diabetes Res Clin Pract. 2008;79:133–40. doi: 10.1016/j.diabres.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grandinetti A, Kaholokula JK, Theriault AG, Mor JM, Chang HK, Waslien C. Prevalence of diabetes and glucose intolerance in an ethnically diverse rural community of Hawaii. Ethn Dis. 2007;17:250–5. [PubMed] [Google Scholar]
- 46.Kim HS, Park SY, Grandinetti A, Holck PS, Waslien C. Major dietary patterns, ethnicity, and prevalence of type 2 diabetes in rural Hawaii. Nutrition. 2008;24:1065–72. doi: 10.1016/j.nut.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pinhey TK. The health status and characteristics of hypertensives in Guam. Asia Pac J Public Health. 1995;8:177–80. doi: 10.1177/101053959500800306. [DOI] [PubMed] [Google Scholar]
- 48.Pinhey TK, Heathcote GM, Rarick J. The Influence of Obesity on the Self-Reported Health Status of Chamorros and other Residents of Guam. Asian Am Pac Isl J Health. 1994;2:195–211. [PubMed] [Google Scholar]
- 49.Araneta MR, Barrett-Connor E. Grand multiparity is associated with type 2 diabetes in Filipino American women, independent of visceral fat and adiponectin. Diabetes Care. 2010;33:385–9. doi: 10.2337/dc09-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morton DJ, Barrett-Connor E, Kritz-Silverstein D, Wingard DL, Schneider DL. Bone mineral density in postmenopausal Caucasian, Filipina, and Hispanic women. Int J Epidemiol. 2003;32:150–6. doi: 10.1093/ije/dyg024. [DOI] [PubMed] [Google Scholar]
- 51.Misra R, Patel T, Kotha P, et al. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: results from a national study. J Diabetes Complications. 2010;24:145–53. doi: 10.1016/j.jdiacomp.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 52.Chuang CZ, Subramaniam PN, LeGardeur BY, Lopez A. Risk factors for coronary artery disease and levels of lipoprotein(a) and fat-soluble antioxidant vitamins in Asian Indians of USA. Indian Heart J. 1998;50:285–91. [PubMed] [Google Scholar]
- 53.Enas EA, Garg A, Davidson MA, Nair VM, Huet BA, Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1996;48:343–53. [PubMed] [Google Scholar]
- 54.Petersen KF, Dufour S, Feng J, et al. Increased prevalence of insulin resistance and nonalcoholic fatty liver disease in Asian-Indian men. Proc Natl Acad Sci U S A. 2006;103:18273–7. doi: 10.1073/pnas.0608537103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cuasay LC, Lee ES, Orlander PP, Steffen-Batey L, Hanis CL. Prevalence and determinants of type 2 diabetes among Filipino-Americans in the Houston, Texas metropolitan statistical area. Diabetes Care. 2001;24:2054–8. doi: 10.2337/diacare.24.12.2054. [DOI] [PubMed] [Google Scholar]
- 56.Park SY, Murphy SP, Sharma S, Kolonel LN. Dietary intakes and health-related behaviours of Korean American women born in the USA and Korea: the Multiethnic Cohort Study. Public Health Nutr. 2005;8:904–11. doi: 10.1079/phn2005740. [DOI] [PubMed] [Google Scholar]
- 57.Yang EJ, Chung HK, Kim WY, Bianchi L, Song WO. Chronic diseases and dietary changes in relation to Korean Americans' length of residence in the United States. J Am Diet Assoc. 2007;107:942–50. doi: 10.1016/j.jada.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 58.Nguyen TT, Liao Y, Gildengorin G, Tsoh J, Bui-Tong N, McPhee SJ. Cardiovascular risk factors and knowledge of symptoms among Vietnamese Americans. J Gen Intern Med. 2009;24:238–43. doi: 10.1007/s11606-008-0889-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.World Health Organization Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 60.Cho J, Juon HS. Assessing overweight and obesity risk among Korean Americans in California using World Health Organization body mass index criteria for Asians. Prev Chronic Dis. 2006;3:A79. [PMC free article] [PubMed] [Google Scholar]
- 61.Yagalla MV, Hoerr SL, Song WO, Enas E, Garg A. Relationship of diet, abdominal obesity, and physical activity to plasma lipoprotein levels in Asian Indian physicians residing in the United States. J Am Diet Assoc. 1996;96:257–61. doi: 10.1016/S0002-8223(96)00077-6. [DOI] [PubMed] [Google Scholar]
- 62.Barnes DM, Harrison C, Heneghan R. Health risk and promotion behaviors in refugee populations. J Health Care Poor Underserved. 2004;15:347–56. doi: 10.1353/hpu.2004.0034. [DOI] [PubMed] [Google Scholar]
- 63.Chen JL. Household income, maternal acculturation, maternal education level and health behaviors of Chinese-American children and mothers. J Immigr Minor Health. 2009;11:198–204. doi: 10.1007/s10903-008-9124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hung DY, Lubetkin EI, Fahs MC, Shelley DR. Assessing the impact of behavioral risk factors and known-groups validity of the SF-12 in a US Chinese immigrant population. Med Care. 2009;47:262–7. doi: 10.1097/MLR.0b013e3181844de4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim MT, Juon HS, Hill MN, Post W, Kim KB. Cardiovascular disease risk factors in Korean American elderly. West J Nurs Res. 2001;23:269–82. doi: 10.1177/01939450122045140. [DOI] [PubMed] [Google Scholar]
- 66.Kim MT, Kim KB, Juon HS, Hill MN. Prevalence and factors associated with high blood pressure in Korean Americans. Ethn Dis. 2000;10:364–74. [PubMed] [Google Scholar]
- 67.Cotler SJ, Dhamija MK, Luc BJ, et al. The prevalence and clinical correlates of elevated ALT levels in an urban Chinatown community. J Viral Hepat. 2010;17:148–52. doi: 10.1111/j.1365-2893.2009.01162.x. [DOI] [PubMed] [Google Scholar]
- 68.Anand SS, Enas EA, Pogue J, Haffner S, Pearson T, Yusuf S. Elevated lipoprotein(a) levels in South Asians in North America. Metabolism. 1998;47:182–4. doi: 10.1016/s0026-0495(98)90217-7. [DOI] [PubMed] [Google Scholar]
- 69.Chandalia M, Mohan V, Adams-Huet B, Deepa R, Abate N. Ethnic difference in sex gap in high-density lipoprotein cholesterol between Asian Indians and Whites. J Investig Med. 2008;56:574–80. doi: 10.2310/JIM.0b013e31816716fd. [DOI] [PubMed] [Google Scholar]
- 70.Mooteri SN, Petersen F, Dagubati R, Pai RG. Duration of residence in the United States as a new risk factor for coronary artery disease (The Konkani Heart Study). Am J Cardiol. 2004;93:359–61. doi: 10.1016/j.amjcard.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 71.Kalhan R, Puthawala K, Agarwal S, Amini SB, Kalhan SC. Altered lipid profile, leptin, insulin, and anthropometry in offspring of South Asian immigrants in the United States. Metabolism. 2001;50:1197–202. doi: 10.1053/meta.2001.26704. [DOI] [PubMed] [Google Scholar]
- 72.Misra KB, Endemann SW, Ayer M. Leisure time physical activity and metabolic syndrome in Asian Indian immigrants residing in northern California. Ethn Dis. 2005;15:627–34. [PubMed] [Google Scholar]
- 73.Misra KB, Endemann SW, Ayer M. Measures of obesity and metabolic syndrome in Indian Americans in northern California. Ethn Dis. 2006;16:331–7. [PubMed] [Google Scholar]
- 74.Sin MK, Choe MA, Kim J, Chae YR, Jeon MY, Vezeau T. Comparison of body composition, handgrip strength, functional capacity, and physical activity in elderly Koreans and Korean immigrants. Res Gerontol Nurs. 2009;2:20–9. doi: 10.3928/19404921-20090101-11. [DOI] [PubMed] [Google Scholar]
- 75.Misra R, Patel TG, Davies D, Russo T. Health promotion behaviors of Gujurati Asian Indian immigrants in the United States. J Immigr Health. 2000;2:223–30. doi: 10.1023/A:1009544414050. [DOI] [PubMed] [Google Scholar]
- 76.Ivey SL, Mehta KM, Fyr CL, Kanaya AM. Prevalence and correlates of cardiovascular risk factors in South Asians: population-based data from two California surveys. Ethn Dis. 2006;16:886–93. [PubMed] [Google Scholar]
- 77.Radha V, Vimaleswaran KS, Babu HN, et al. Role of genetic polymorphism peroxisome proliferator-activated receptor-gamma2 Pro12Ala on ethnic susceptibility to diabetes in South-Asian and Caucasian subjects: Evidence for heterogeneity. Diabetes Care. 2006;29:1046–51. doi: 10.2337/diacare.2951046. [DOI] [PubMed] [Google Scholar]
- 78.Chandalia M, Cabo-Chan AV, Jr., Devaraj S, Jialal I, Grundy SM, Abate N. Elevated plasma high-sensitivity C-reactive protein concentrations in Asian Indians living in the United States. J Clin Endocrinol Metab. 2003;88:3773–6. doi: 10.1210/jc.2003-030301. [DOI] [PubMed] [Google Scholar]
- 79.Kamath SK, Hussain EA, Amin D, et al. Cardiovascular disease risk factors in 2 distinct ethnic groups: Indian and Pakistani compared with American premenopausal women. Am J Clin Nutr. 1999;69:621–31. doi: 10.1093/ajcn/69.4.621. [DOI] [PubMed] [Google Scholar]
- 80.Balasubramanyam A, Rao S, Misra R, Sekhar RV, Ballantyne CM. Prevalence of metabolic syndrome and associated risk factors in Asian Indians. J Immigr Minor Health. 2008;10:313–23. doi: 10.1007/s10903-007-9092-4. [DOI] [PubMed] [Google Scholar]
- 81.Jonnalagadda SS, Diwan S. Health behaviors, chronic disease prevalence and self-rated health of older Asian Indian immigrants in the U.S. J Immigr Health. 2005;7:75–83. doi: 10.1007/s10903-005-2640-x. [DOI] [PubMed] [Google Scholar]
- 82.Jonnalagadda SS, Khosla P. Nutrient intake, body composition, blood cholesterol and glucose levels among adult Asian Indians in the United States. J Immigr Minor Health. 2007;9:171–8. doi: 10.1007/s10903-006-9027-5. [DOI] [PubMed] [Google Scholar]
- 83.Venkataraman R, Nanda NC, Baweja G, Parikh N, Bhatia V. Prevalence of diabetes mellitus and related conditions in Asian Indians living in the United States. Am J Cardiol. 2004;94:977–80. doi: 10.1016/j.amjcard.2004.06.048. [DOI] [PubMed] [Google Scholar]
- 84.Ivey SL, Patel S, Kalra P, Greenlund K, Srinivasan S, Grewal D. Cardiovascular health among Asian Indians (CHAI): a community research project. J Interprof Care. 2004;18:391–402. doi: 10.1080/13561820400011800. [DOI] [PubMed] [Google Scholar]
- 85.Abate N, Chandalia M, Snell PG, Grundy SM. Adipose tissue metabolites and insulin resistance in nondiabetic Asian Indian men. J Clin Endocrinol Metab. 2004;89:2750–5. doi: 10.1210/jc.2003-031843. [DOI] [PubMed] [Google Scholar]
- 86.Abate N, Garg A, Enas EA. Physico-chemical properties of low density lipoproteins in normolipidemic Asian Indian men. Horm Metab Res. 1995;27:326–31. doi: 10.1055/s-2007-979971. [DOI] [PubMed] [Google Scholar]
- 87.Kamath SK, Ravishanker C, Briones E, Chen EH. Macronutrient intake and blood cholesterol level of a community of Asian Indians living in the United States. J Am Diet Assoc. 1997;97:299–301. doi: 10.1016/S0002-8223(97)00078-3. [DOI] [PubMed] [Google Scholar]
- 88.Bhalodkar NC, Blum S, Rana T, Kitchappa R, Bhalodkar AN, Enas EA. Comparison of high-density and low-density lipoprotein cholesterol subclasses and sizes in Asian Indian women with Caucasian women from the Framingham Offspring Study. Clin Cardiol. 2005;28:247–51. doi: 10.1002/clc.4960280510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jonnalagadda SS, Diwan S. Regional variations in dietary intake and body mass index of first-generation Asian-Indian immigrants in the United States. J Am Diet Assoc. 2002;102:1286–9. doi: 10.1016/s0002-8223(02)90283-x. [DOI] [PubMed] [Google Scholar]
- 90.Parikh NS, Fahs MC, Shelley D, Yerneni R. Health behaviors of older Chinese adults living in New York City. J Community Health. 2009;34:6–15. doi: 10.1007/s10900-008-9125-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Babbar RK, Handa AB, Lo CM, et al. Bone health of immigrant Chinese women living in New York City. J Community Health. 2006;31:7–23. doi: 10.1007/s10900-005-8186-y. [DOI] [PubMed] [Google Scholar]
- 92.Song YJ, Hofstetter CR, Hovell MF, et al. Acculturation and health risk behaviors among Californians of Korean descent. Prev Med. 2004;39:147–56. doi: 10.1016/j.ypmed.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 93.Sorkin D, Tan AL, Hays RD, Mangione CM, Ngo-Metzger Q. Self-reported health status of vietnamese and non-Hispanic white older adults in california. J Am Geriatr Soc. 2008;56:1543–8. doi: 10.1111/j.1532-5415.2008.01805.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wandell PE, Carlsson A, Steiner KH. Prevalence of diabetes among immigrants in the Nordic countries. Curr Diabetes Rev. 2010;6:126–33. doi: 10.2174/157339910790909404. [DOI] [PubMed] [Google Scholar]
- 95.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292:2860–7. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- 96.Kaushal N. Adversities of acculturation? Prevalence of obesity among immigrants. Health Econ. 2009;18:291–303. doi: 10.1002/hec.1368. [DOI] [PubMed] [Google Scholar]
- 97.Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes Relat Metab Disord. 2000;24:1188–94. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- 98.Sanchez-Vaznaugh EV, Kawachi I, Subramanian SV, Sanchez BN, Acevedo-Garcia D. Do socioeconomic gradients in body mass index vary by race/ethnicity, gender, and birthplace? Am J Epidemiol. 2009;169:1102–12. doi: 10.1093/aje/kwp027. [DOI] [PubMed] [Google Scholar]
- 99.Bates LM, Acevedo-Garcia D, Alegria M, Krieger N. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002-2003. Am J Public Health. 2008;98:70–7. doi: 10.2105/AJPH.2006.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fujimoto WY, Leonetti DL, Kinyoun JL, et al. Prevalence of diabetes mellitus and impaired glucose tolerance among second-generation Japanese-American men. Diabetes. 1987;36:721–9. doi: 10.2337/diab.36.6.721. [DOI] [PubMed] [Google Scholar]
- 101.Eckel RH, Kahn SE, Ferrannini E, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? Diabetes Care. 2011;34:1424–30. doi: 10.2337/dc11-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Migration Policy Institute [11 December 2011];US in Focus: Asian Immigrants in the United States. 2011 Available from: http://www.migrationinformation.org/USfocus/display.cfm?ID=841.
- 103.Passel J, Cohn D. Immigration to Play Lead Role In Future U.S. Growth: U.S. Population Projects: 2005-2050 Pew Research Center Publications. 2008 Available from: http://pewresearch.org/pubs/729/united-states-population-projections.
- 104.International Diabetes Federation [1 June 2012];The Diabetes Atlas, e-Atlas. (5th Edition). 2011 Available from: http://www.eatlas.idf.org/Incidence/
- 105.Ebrahim S. Surveillance and monitoring: a vital investment for the changing burdens of disease. Int J Epidemiol. 2011;40:1139–43. doi: 10.1093/ije/dyr144. [DOI] [PubMed] [Google Scholar]
- 106.Kanaya AM, Karter AJ. Type 2 Diabetes in Asian American and Pacific Islander Populations: a View from California. [12 January 2012];California Diabetes Program. Center for Vulnerable Populations. 2010 Available from: http://www.caldiabetes.org/content_display.cfm?contentID=1253&CategoriesID=30.
- 107.Staimez L, Weber MB, Narayan KMV, Oza-Frank R. Overweight and Diabetes Among Asian Americans: A Systematic Review (abstract). Diabetes. 2012;61(Suppl 1):A–40. [Google Scholar]
- 108.Lauderdale DS, Kuohung V, Chang SL, Chin MH. Identifying older Chinese immigrants at high risk for osteoporosis. J Gen Intern Med. 2003;18:508–15. doi: 10.1046/j.1525-1497.2003.20331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Maskarinec G, Meng L, Ursin G. Ethnic differences in mammographic densities. Int J Epidemiol. 2001;30:959–65. doi: 10.1093/ije/30.5.959. [DOI] [PubMed] [Google Scholar]
- 110.Maskarinec G, Novotny R, Tasaki K. Dietary patterns are associated with body mass index in multiethnic women. J Nutr. 2000;130:3068–72. doi: 10.1093/jn/130.12.3068. [DOI] [PubMed] [Google Scholar]
- 111.Guerrero RT, Paulino YC, Novotny R, Murphy SP. Diet and obesity among Chamorro and Filipino adults on Guam. Asia Pac J Clin Nutr. 2008;17:216–22. [PMC free article] [PubMed] [Google Scholar]
- 112.Langenberg C, Araneta MR, Bergstrom J, Marmot M, Barrett-Connor E. Diabetes and coronary heart disease in Filipino-American women: role of growth and life-course socioeconomic factors. Diabetes Care. 2007;30:535–41. doi: 10.2337/dc06-1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Novotny R, Davis J, Ross P, Wasnich R. Adiposity and blood pressure in a multiethnic population of women in Hawaii. Ethn Health. 1998;3:167–73. doi: 10.1080/13557858.1998.9961859. [DOI] [PubMed] [Google Scholar]