Abstract
Exostoses are bony outgrowths of the external auditory canal (EAC) that can lead to cerumen entrapment, recurrent infections, and conductive hearing loss. When surgical removal is indicated, a drill or osteotome may be used via a post-auricular, endaural, or transcanal approach. Studies suggest that exostoses removed by transcanal osteotome results in decreased morbidity when compared to open, drilled approaches; however, inadvertent injury to the facial nerve or inner ear is a theoretical concern given the restrictive geometry of the EAC and challenges of visualizing the tip of the chisel through the microscope. The endoscope provides superior visualization of the canal and tympanic membrane compared to the microscope. We sought to demonstrate the efficacy and safety of endoscopic exostosis surgery with an osteotome. We find that the endoscope provides improved wide angled views without blind spots. There were no intraoperative complications. Endoscopic canaloplasty for exostoses may be readily applied.
Keywords: exostoses, endoscope, middle ear surgery, canaloplasty
Introduction
Exostoses of the external ear canal (EAC) are lamellar bony outgrowths that commonly occur as a reaction to cold-water exposure.1 Numerous studies have addressed the surgical management of exostoses and debated approaches (post-auricular versus transcanal) and operative instruments (drill versus osteotome).2,3 While the use of a high speed drill allows for precise bone removal and is believed to decrease the risk of injury to surrounding structures, it may result in sensorineural hearing loss (SNHL) due to direct transmission of sound to the cochlea.4 The osteotome may avoid the risks of tinnitus and SNHL; however, studies have expressed concerns for the risk of injury to the facial nerve, tympanic membrane, and temporomandibular joint due to lack of landmarks and visualization.5
Recently there has been increased application of endoscopes for otologic surgery as a ‘minimally invasive approach’ given that transcanal procedures avoid the need for a post-auricular incision. Advocates of endoscopic ear surgery espouse its high resolution, magnification, and wide-angle view. These features make the endoscope an ideal instrument for visualization of the EAC in osteotome-assisted exostosis removal, and address the safety concerns most often ascribed to this technique. Herein, we describe endoscopic transcanal resection of EAC exostoses.
Materials and Methods
Institutional review board approval was obtained.
Representative Operative Technique
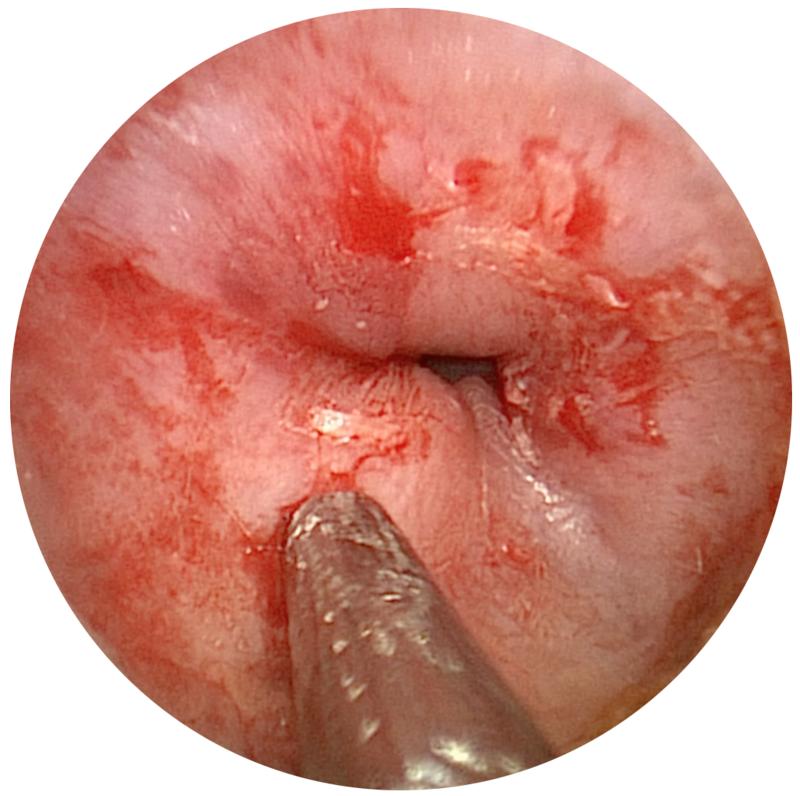
A healthy 88-year-old male had a history of left sided recurrent otitis externa and persistent aural fullness. Otologic exam revealed several large exostoses. Medial debris was difficult to remove and the tympanic membrane could not be visualized. He was taken to the operating room (OR) for removal of the exostoses where endoscopic and microscopic equipment were available. (Fig.1) Using a 3.0 mm, 14cm, 0° endoscope, three large, occlusive exostoses were identified just lateral to the tympanic ring. (Fig. 2). The remainder of the surgery was performed under endoscopic surveillance.
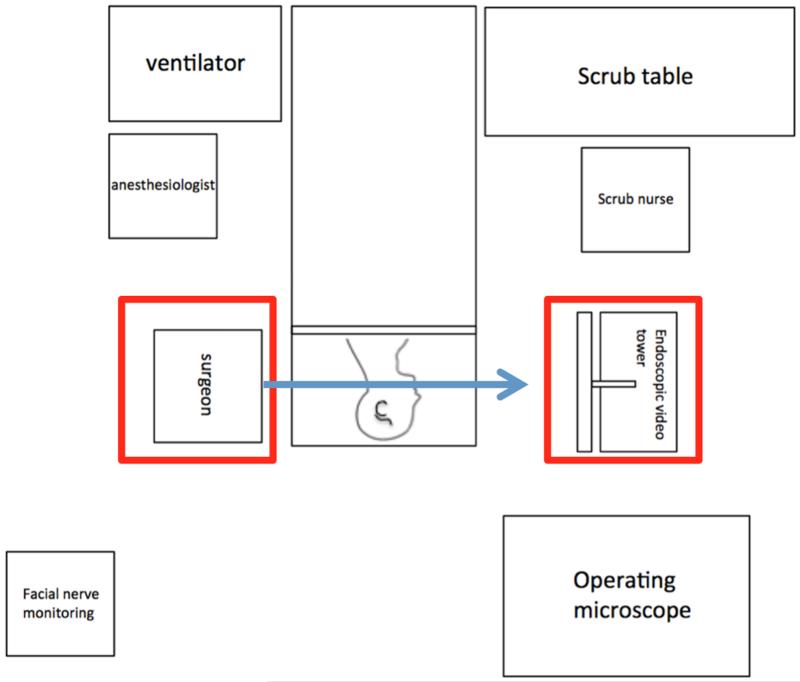
Figure 1. Endoscopic ear Surgery Room Set Up.
The high-definition video tower (or boom-mounted video screen) is placed directly opposite the surgeon for direct line of sight using rigid endoscopy.
Figure 2. Preoperative View of Ear Canal.
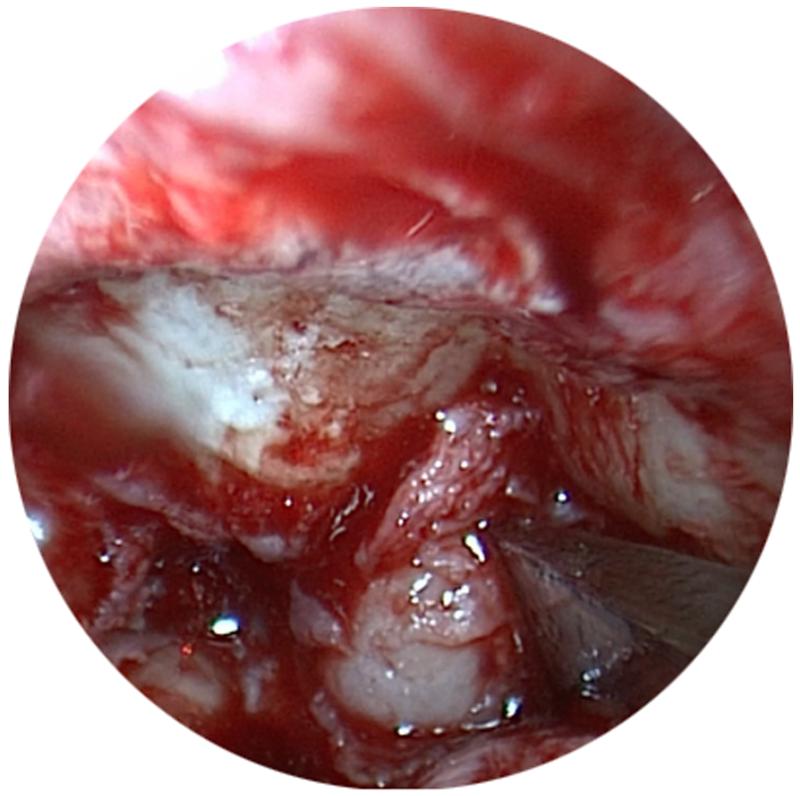
Lidocaine with Epinephrine 1:100,000 was infiltrated at the bony-cartilaginous junction. A Rosen knife was used to incise the skin crest of the first exostosis to fully expose the extent of the bony lesion. A 2.0 mm straight osteotome was applied at the base. Using a “three-handed” technique (Figure 3A), the lesion fractured with gentle tapping at its base and completely mobilized. A cup forceps was used to remove the bony mass in one piece. This allowed for removal of the remaining medial debris and afforded a complete view of the tympanic membrane using the endoscope. The 2.0 mm osteotome was again used on the remaining exostoses with the annulus in view. (Figure 3B and 3C). Epinephrine 1:1000 soaked cotton balls were used frequently to maintain hemostasis during the dissection.
Figure 3. “Three Handed” Technique of Endoscopic Removal of External Auditory Canal Exostoses.
A: Surgical assistant holds endoscope and suction in place, while surgeon uses osteotome to remove exostoses. B: Osteotome placed on base of exostosis. C: View of tympanic membrane following removal of exostoses.
The ear canal was irrigated with saline, suctioned, and then inspected using the endoscope. The tympanic annulus was intact, as the skin medial to the exostosis was not disrupted. Skin edges were then laid down with good coverage at the base of each exostosis. Gelfoam pieces were placed sequentially from the tympanic membrane out to the lateral canal. The patient was returned to the anesthesia team for postoperative care.
Results
Preoperative Patient Characteristics and Demographics
A retrospective review of patients who underwent endoscopic exostoses removal between January 2014 and August 2014 was performed. We identified four patients from two different surgeons. Preoperative history was significant for recurrent infection, entrapped epithelial debris, and hearing loss; exam demonstrated significant exostoses in all patients (Table 1).
Table.
| Patient No. |
Gender | Age (Years) |
Case Type | Surgical Approach |
Endoscope Used |
Instrument for Exostosis Removal |
Admission to Hospital? (Y/N) |
Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 88 | Exostoses alone |
Transcanal | 0 degree 3.0 mm |
2 mm osteotome | N | None |
| 2 | M | 44 | Exostoses and Stapedectomy |
Transcanal | 0 degree 3.0 mm |
2 mm Skeeter drill; 2 mm osteotome |
N | None |
| 3 | M | 30 | Exostoses alone |
Transcanal | 0 degree 3.0 mm |
2 mm osteotome | N | None |
| 4 | F | 51 | Exostoses alone |
Transcanal + Endaural |
0 degree 3.0 mm |
1.5 mm osteotome | N | None |
Intraoperative and Postoperative Outcomes
For 3 of 4 patients, the surgical approach was transcanal. One patient underwent a combined transcanal and endaural approach. At our institution, it is standard practice to use skin grafts following exotosis removal from the EAC; however, in two patients, this was not necessary due to the skin saving technique of using the osteotome and endoscope. Mean procedural time exostoses removal was 83 ± 14 minutes (SD); cases were performed with otolaryngology resident participation and facial nerve monitoring. There were no intraoperative complications. Patients were followed postoperatively for a median length of follow-up of 3.5 months. Postoperative exams showed a healing ear canal with intact canal skin without evidence of infection. Postoperative audiograms showed unchanged sensorineural thresholds.
Discussion
Removal of symptomatic exostoses may be challenging because the narrow aperture of the EAC makes visualization of landmarks challenging. While microscopes confer the ability for binocular vision and two-handed surgery, visualization is limited because an adequate amount of light must reach the surgical plane from afar. The endoscope allows for improved visualization due to the fact that the light emerges from the tip of the instrument and availability of angled lenses offer a wide perspective of the operative field.
We describe our technique and early safety profile of endoscopic canaloplasty for exostoses. OR times, including set-up and procedural time, were relatively short. There were no intraoperative complications. Postoperatively, patients demonstrated expected wound healing and minimal pain, and sustained no change in sensorineural hearing thresholds. No patients have experienced prolonged dizziness, headache, or other notable symptoms. Limitations of an endoscopic approach is need for a surgical assistant and lack of binocular view. Future studies should continue to evaluate the use of the endoscope for exostoses removal, and define the patient and disease characteristics that necessitate standard approaches.
Conclusion
We describe our early experience with endoscope-based resection of EAC exostoses. The endoscope provides improved wide angled view compared to microscope and excellent feedback on location and distance relative to the tympanic membrane. There were no intraoperative or postoperative complications. This technique is readily applied and provides discrete advantages given improved visualization over standard operative microscopy.
Acknowledgements
We would like to thanks Dr. Douglas Hetzler for sharing his insight with the senior author on the use of osteotomes for the transcanal resection of exostoses at the Practical Anatomy and Surgical Education Workshop, St. Louis University, St. Louis, Missouri.
Footnotes
Conflict of Interest: None
Disclosures: None
Works Cited
- 1.Timofeev I, Notkina N, Smith I. Exostoses of the external auditory canal: a long-term follow-up study of surgical treatment. Clin Otolaryngol. 2004;29:588–94. doi: 10.1111/j.1365-2273.2004.00865.x. [DOI] [PubMed] [Google Scholar]
- 2.Barrett G, Ronan N, Cowan E, et al. To drill or to chisel? A long-term follow-up study of 92 exostectomy procedures in the UK. The Laryngoscope. 2014 doi: 10.1002/lary.24849. [DOI] [PubMed] [Google Scholar]
- 3.Fisher E, McManus T. Surgery for external auditory canal exostoses and osteomata. The Journal of laryngology and otology. 1994;108:106–10. doi: 10.1017/s0022215100126027. [DOI] [PubMed] [Google Scholar]
- 4.Frese K, Rudert H, Maune S. Surgical Treatment of External Auditory Canal Exostoses. Laryngorhinootologie. 1999;78:538–43. doi: 10.1055/s-1999-8754. [DOI] [PubMed] [Google Scholar]
- 5.Hetzler D. Osteotome technique for removal of symptomatic ear canal exostoses. The Laryngoscope. 2007;117:1–14. doi: 10.1097/MLG.0b013e31802cbb12. [DOI] [PubMed] [Google Scholar]