Abstract
An institutional-based care system in mental health has been replaced by a network of community-based services with different levels of structure and support. This poses both an opportunity and a challenge to provide appropriate and effective care to persons with serious mental illnesses. This paper describes a simulation-based approach for mental health system planning, focused on hospital and residential service components that can be used as a decision support tool. A key feature of this approach is the ability to represent the current service configuration of psychiatric care and the client flow pattern within that framework. The strength of the simulation model is to help mental health service managers and planners visualize the interconnected nature of client flow in their mental health system and understand possible impacts of changes in arrival rates, service times, and bed capacity on overall system performance. The planning model will assist state mental health agencies to respond to requirements of the Olmstead decision to ensure that individuals with serious mental illness receive care in the least restrictive setting. Future plans for refining the model and its application to other service systems is discussed.
Keywords: planning model, decision making, individuals with serious mental illness, discrete event simulation
Consensus exists today that the majority of individuals with serious mental illness (SMI) do not require long-term hospitalization if alternative residential and support services are available (e.g., Clifford, Charman, Webb, Craig, & Cowan, 1991; Durbin, Cochrane, Goering, & Macfarlane, 2001; Rothbard, Kuno, Schinnar, Hadley, & Turk, 1999; Seling & Johnson, 1990). As the number of state hospital beds has decreased over the past several decades, an array of residential programs have been developed with varying degrees of staffing support (Budson, 1990; Randolph, Ridgway, & Carling, 1991). Additionally, assertive community treatment teams (ACT), intensive case management (ICM), as well as psychosocial rehabilitation programs, have become increasingly available for people with serious mental illness. The importance of implementing community-based services has been further highlighted by the recent Supreme Court decision in Olmstead v. L.C., 119 S.Ct. 2176 (1999), which affirmed that unnecessary institutionalization of individuals with disabilities is discrimination under the Americans with Disabilities Act (ADA). States are now required to have a comprehensive, effective working plan to establish compliance with the ADA (Fox-Grage, Folkemer, & Lewis, 2003).
In this era of advanced deinstitutionalization, mental health administrators and planners are faced with the challenge of providing an appropriate and effective mix of residential, ambulatory treatment and support services for persons with serious mental illness. This requires the ability to estimate demand for different levels of care given that severity of illness and accompanying social and instrumental disabilities vary across individuals and change over an individual's lifetime (Group for the Advancement of Psychiatry, 1992; Herman & Mowbray, 1991; Tessler, Bernstein, Rosen, & Goldman, 1982). Shifting away from an institutional-based care system has been a significant step toward implementing an optimal service system. However, considerable advancement in the use of planning technologies is required to assist administrators and policy makers in visualizing, designing, and implementing such a system.
In this paper we describe a simulation-based model that can be used as a decision support tool for mental health system planning with a focus on persons with serious mental disorders. A key feature of this approach is the ability to construct a representation of the current service configuration of psychiatric care and the client flow pattern within that framework. Clients can have diverse patterns of care with some moving from acute to subacute care; others from acute to community or residential care settings, etc. Simulation is a powerful tool for describing the performance of the system with respect to client admissions, discharges, waiting time, length of stay, etc., within the treatment network. Once the basic flow model is described, different policy scenarios regarding service capacity or hypothetical client transition patterns can be used to project what would transpire if capacity were increased or length of stay decreased, for example. Furthermore, estimates based on needs assessment of appropriate treatment time and site for patients can be used to determine if the system shows congestion at entry into certain types of treatment settings and empty beds in others. Parameters can be adjusted to decrease the congestion, should that occur.
With the development of increasingly powerful computer hardware and the greater availability of individual level service history data, the use of simulation-based techniques has become feasible, albeit underutilized for most health service planning purposes. The objective of this paper is to present a case study using a simulation-based approach and to encourage mental health policy makers and other stakeholders to consider using model-based decision support tools in the future. The case study is based on the Philadelphia mental health system where a close collaboration with the City of Philadelphia mental health authority enabled researchers to develop a longitudinal database on all public mental health consumers in Philadelphia (1987–current) (Rothbard, Kuno, Hadley, & Dogin, 2003). This provided an excellent platform for advancing a data based planning approach for decision-making.
CASE STUDY: THE PHILADELPHIA MENTAL HEALTH SYSTEM
The Philadelphia County Mental Health System treats approximately 15,000 adult patients with serious mental illnesses on an annual basis. The 1990 closure of a 500-bed state hospital serving Philadelphia residents marked a significant shift away from long-term institutionalized care. Sixty (60) extended acute care (EAC) beds were created in a general hospital setting at the time of the state hospital closure to provide a place for extended stays of 90 days or more. An additional 100 beds were provided in highly structured long-term care facilities for seriously disabled clients. In conjunction, the residential system consisted of 1200 beds with varying degrees of staffing and service support. During the year preceding the closure, the Office of Mental Heath was awarded a special grant program from the US Department of Housing and Urban Development (HUD) to provide for the expansion of a supported independent living program, which had 540 beds in 1999. The number of acute beds utilized by public sector patients in general hospitals was consistent before and after the state hospital closure, with a daily census ranging between 350 and 400 patients with schizophrenia or major affective disorders.
In response to the closure of the state hospital, multidisciplinary community treatment teams (CTTs) were created, modeled after the ACT program, and staffed by members of the state hospital. Initially, CTTs only provided care to patients discharged from the state hospital, however, as the former state hospital patients integrated into the community requiring less support, CTT's began to accept new clients. In addition, ICM, which were implemented in Philadelphia in 1989, targeted individuals with serious mental illness who were heavy users of emergency and acute inpatient care. Less intensive forms of case management with larger caseloads than ICM called resource coordination (RC) programs were subsequently implemented as well. The number of clients served by these programs in 1999 was approximately 7500 patients annually out of 15,000 individuals who were treated for a serious mental health disorder [500-CTTs; 4000-ICMs; and 3000-RC] (Hadley, Turk, Vasko, & McGurrin, 1997; Rothbard, Richman, & Hadley, 1997).
In the Philadelphia system, the County Office of Mental Health (OMH) funds five crisis response centers (CRC). Psychiatric emergency patients are seen at one of the CRCs prior to acute hospital admission. The monthly number of treated CRC patients in 1999 was 2000, and the annual unduplicated number of patients was approximately 18,000. A variety of ambulatory mental health care programs such as partial hospitalization, psychosocial rehabilitation, outpatient therapy, etc., are provided by the mental health system that includes 12 community mental health centers, other specialty mental health agencies, and outpatient clinics in hospital settings. There are also several consumer-operated programs including ICM and self-help groups as well (Rothbard et al., 2003) (Table 1).
Table 1.
Summary of Philadelphia Mental Health Services (1999)
| Service type | Capacity |
|---|---|
| Hospital beds | |
| Acute hospital beds (daily census) | 350 |
| Extended acute care hospital beds | 60 |
| Residential beds | |
| Long-term structured residential beds | 100 |
| Transitional residences and group homes | 1200 |
| Supported housing | 540 |
| Intensive case management clients | |
| Community treatment team | 500 |
| Intensive case management | 4000 |
| Resource coordination | 3000 |
A significant feature of the Philadelphia system is a centralized management approach that controls the flow of clients into and out of high intensity services such as inpatient, residential, and intensive case management programs. The emergency crisis service programs (CRC's) provide the gate-keeping function to acute hospitals. Triage activities are coordinated with the CRCs and the county OMH and the Medicaid behavioral health managed care organization (CBH) using prior authorization mechanisms to monitor admission patterns to acute care beds. The Access to Alternative Service (AAS) program, a quasi-public entity, has gate-keeping authority over residential beds of various care levels managed by the Office of Mental Health (Rothbard, Schinnar, Hadley, Foley, & Kuno, 1998). The AAS makes residential placement decisions for applicants on whether and what type of setting they should be placed in based on clinical and functional factors. As in the residential service referral system, patient transfer from a general acute hospital to extended psychiatric treatment units is assessed and authorized by another quasi-public entity named ADAPT (Admission, Discharge, and Planning Treatment). Furthermore, the management of admissions to the intensive case management programs (i.e., CTT, ICM, and RC) is made by the Targeted Case Management (TCM) unit that authorizes and assigns clients to these case management programs based on application information sent by referring persons from hospitals, outpatient clinics, CMHCs, families, etc. The centralized nature of referrals and placements by the AAS, ADAPT, and TCM enables comprehensive data to be collected on relevant measures of utilization required for developing the planning model.
GRAPHICAL REPRESENTATION OF THE SERVICE SYSTEM
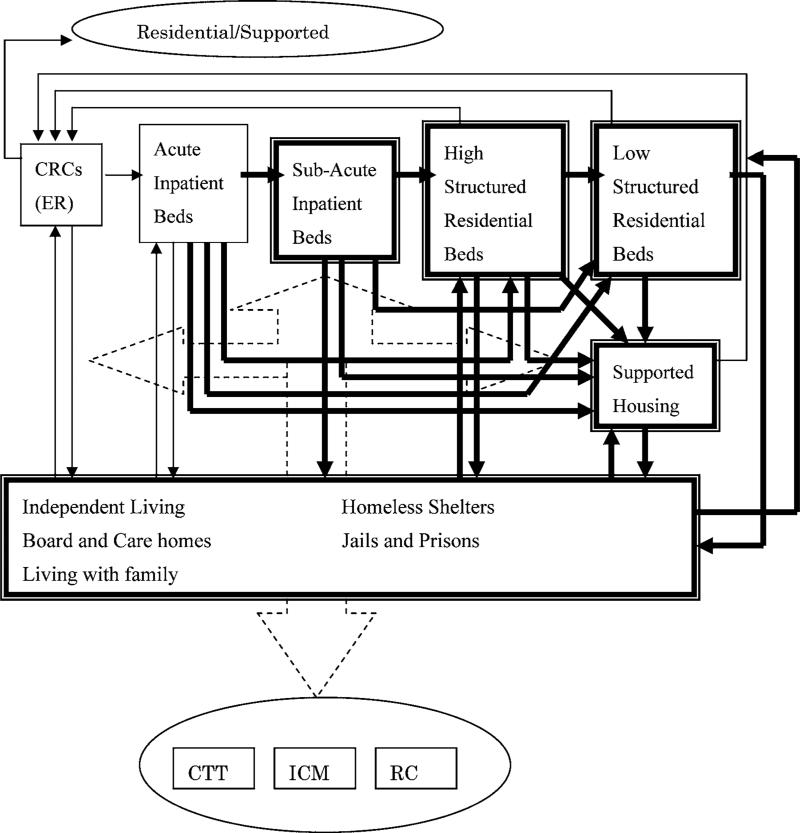
A graphical representation of the County mental health service system was constructed by identifying all relevant system components and linkages or connections among the components. A system component represents a category of service with similar structure and function (i.e., acute care hospital). Connections or links between system components represent client flows, or possible transition routes from one service system to another. The links are based on observed data on actual service use patterns as well as logical expectations. Figure 1 depicts how service components are connected in the Philadelphia mental health system.
Fig. 1.
Philadelphia mental health system.
The system consists of three major parts representing flows or movement of clients. The first component consists of the admission and discharge of clients to and from the emergency CRC system. Incoming patients to the crisis centers are from community living settings and residential care settings. Discharge dispositions from the CRCs include acute hospitals or the return to community living arrangements. The second component depicts the client flow through acute/subacute hospital beds to various residential settings. This part is modeled as a continuum of care network, although individual clients do not have to move from a higher to lower level of care setting in specific stages. Some clients discharged from subacute hospital settings move to highly structured residential settings, while others go to lower structured residential settings or back to independent living arrangements. Incoming clients to supported housing settings are largely from other residential settings or homeless shelters in Philadelphia. For other types of residential services, clients come from acute or subacute hospitals, other residential and community settings. The third component of the graphic model is related to CTT, ICM, and RC programs. It is expected that these programs influence admission and discharge rates to CRCs and hospital/residential settings. For example, some clients in structured residential settings may be capable of living in supported housing settings if CTT or ICM services are available. CTT and ICM programs are also expected to reduce acute hospital admissions or shorten length of stays among those who have been frequent users of acute inpatient care.
The above conceptual model represents a comprehensive system of care framework. This framework allows us to define boundaries or domains of the system to be modeled and clarifies relationships between parts of the system. The hospital/residential domain (subacute to long-term hospital and community residential components) is placed at its core, and the focus of this simulation case study. Client flow patterns in the CRC to acute hospital beds and the CTT/ICM/RC system can be modeled in the same way as the residential components. The CRC and hospital/residential system models can be combined after an acceptable model for each system is constructed, however, each component adds complexity to the modeling effort. In the following section, a simplified model of the hospital/residential system is presented to demonstrate how a simulation model could assist mental health system planners to understand the interdependent nature of client flows
ILLUSTRATION OF SIMULATION MODEL
Methodology
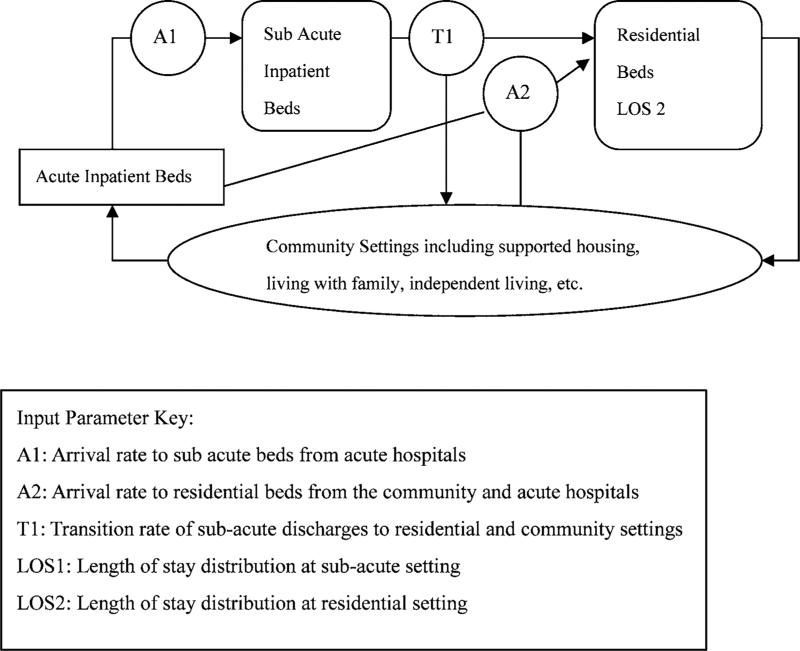
Since details in service configuration and client movement patterns differ from one system to the other, a general model of hospital/residential system was constructed. The system consists of two service components: 1) subacute hospital beds, and 2) structured residential beds. A computerized simulation model was constructed according to the following diagram (Fig. 2).
Fig. 2.
Simulation model diagram.
One of the interesting characteristics of client flow in the hospital/residential system is a phenomenon called “blocking.” The blocking occurs, in this case, when a subacute patient is ready to be transferred to the residential setting and the move is delayed because residential beds are not available. The client has to stay in the subacute setting although he or she does not require a hospital level of care environment. In turn, blocking of a subacute bed prevents an incoming patient from the acute hospital to be admitted to the subacute setting. Thus, the blocking has a ripple effect on the client flow in the hosptial and residential system. A queueing network framework is applicable to model this common phenomemon.
The type of simulation employed in this case study was “discrete event simulation.” The method is used to model event behavior that causes a change from one state to another at discrete points in time. In the case of the mental health service system, an event is associated with an individual client, e.g., an admission or arrival of a client to the system, a transition of a client from one setting to another, and a departure or discharge of a client from the system. Thus, a core undertaking of discrete event simulation is to track arrival and departure events of clients to and from each system component. In our model, clients arrive according to the calculated arrival patterns based on observational data and the pattern is assumed to follow a Poisson distribution. Each of the admitted clients is assigned a length of stay (LOS), which is sampled from the appropriate probabilistic distribution that most closely represents the empirical LOS distribution. Each of the discharged clients from the subacute setting is assigned a transfer to a residential setting or a discharge from the hospital/residential system according to the observed transition rate.
The rules regarding movement of clients waiting for service are the following: 1) “first come first serve principle” to determine which client is admitted first among those waiting for service, 2) “blocking after service,” i.e., clients occupy currently assigned beds while waiting, and 3) clients are not turned away if waiting gets long. Different rules can be applied in simulation, based on realistic movements of clients waiting for service. Simulation outputs include system performance indicators such as average number of occupied beds, average number of clients waiting, and average number of “blocked beds” in the suba-cute setting.
A computer simulation model was constructed using Visual C++ 6.0 (MicroSoft Corp.). The model was run 10 times to simulate a period of 50 years. The average outputs from all the simulation runs were calculated. The simulation results derived from observed service use data were compared with actual system statistics to examine whether the model adequately replicates the system behavior. Then, a series of “what-if” analyses were carried out. We considered a scenario where a higher proportion of suba-cute clients required placement in the residential setting. This is based on an analysis of referral records to the residential facilities maintained by AAS that showed nearly 50% of referrals deferred admission due to various reasons including lack of bed availability. Under the increased demand scenario, potential policy options to meet unmet need were compared, i.e., different parameter values for bed capacities and LOS were plugged in the model.
Description of the Data
The data used in the simulation analyses included Medicaid claims records that provide information on acute and subacute hospitalization, and monthly residential facility data from the OMH. These administrative data files were integrated to construct service use histories on individual clients. An algorithm was employed to create a composite identifier for each person and all other identifiers of a personal nature in the record are removed. Once data was linked, a random number identifier that replaced the composite identifier was attached to each person. Simulation input parameters were constructed from this “de-identified” data file.
Admission and discharge records from inpatient and residential facilities were obtained during the fiscal year of 1999 (July 1, 1999 to June 30, 2000). Arrival rates were constructed by examining the monthly number of admissions to subacute units and residential facilities. Records of clients who were admitted to each setting during the time period were pooled to estimate LOS distribution. For the admission episodes, discharge records were available until the end of June 2002, allowing at least 2-year follow-up after admissions. In estimating LOS distribution for the residential setting, the survival function technique was used to construct an empirical distribution function in order to account for censored observations. The transition rate was calculated as the number of the subacute discharges moving into the residential setting divided by the total number of subacute discharges during the observation period.
Results
Model Parameters of the Observed Client Flow
The arrival rates were approximately two admissions per 3 days to the subacute units (i.e., 0.61 per day), and four admissions per 3 days to the residential facilities (i.e., 1.36 per day). The mean LOS at the subacute units was 89.3 days (SD = 75.9), and the estimated mean LOS at the residential facilities was 433.6 days (SD = 429.6), based on the observation data. The Weibull distribution6 was found to fit best with the empirical LOS distribution for both the sub-acute units (α = 1.24, β= 95.96) and the residential facilities (α = 0.60, β = 461.31). The transition rate from the subacute to residential settings was 0.26, that is, 26% of discharges from the subacute units were transferred to the residential facilities. The observation data showed that the average daily census of subacute inpatient beds was 52. The number did not reach the capacity of 60 subacute beds, since the observation data captured only bed use by Medicaid recipients, i.e., private pay and Medicare patients in subacute beds were not in the data set. An observed average daily census of clients in residential facilities was 1097. The simulation results showed that on average 55 patients were served in the subacute setting and 970 clients in the residential setting, given the arrival and LOS patterns under the condition that beds were always available for incoming clients. The model adequately represented the client flow with a small overestimation of subacute patients and a small underestimation of residential clients.
What-if Analyses
The following what-if analyses were carried out under the hypothetical scenario of greater demand for residential placement among the subacute clients. Example 1 demonstrated the extent to which congestion would occur in association with increased demand for residential placement under the fixed bed capacity. For this exercise, the numbers of subacute and residential beds were set as 63 beds and 1115 beds, respectively, 15% above the average daily census. This was done to prevent congestion from occurring at the observed transition rate of 0.26. Example 2 compared the results of policy options designed to reduce the congestion caused by increased demand for residential placement.
As shown in Table 2, at the transition rate of 0.35 (i.e., 35% of subacute discharges are assigned to be transferred to the residential setting), clients waiting for residential placement block 4 beds on average in the subacute setting. The number of blocked beds increases to 5.3 beds and 7.4 beds, as the transition rate increases to 0.40 and 0.45. The extent of acute care patients waiting for subacute admission grows exponentially as the number of blocked subacute beds increases. It highlights the importance of efficient client flow management to prevent bed blocking.
Table 2.
Number of Patients Waiting for Residential and Subacute Care Placement by Transition Rate
| Transition rate |
||||
|---|---|---|---|---|
| Simulation outputs | 0.26 | 0.35 | 0.40 | 0.45 |
| N of subacute patients waiting for residential placement | 0.1 | 4.1 | 5.3 | 7.4 |
| N of acute patients waiting for subacute placement | 1.3 | 98.3 | 216.3 | 460.4 |
Tables 3 and 4 present the effects of policy options to alleviate the congestion from waiting for beds in the subacute setting (blocking) and in the acute hospital (waiting) (Example 2). The scenario with the transition rate of 0.35 was used for this policy scenario analyses. In this exercise, different values for one of the input parameters were plugged in, while other parameters were held constant.
Table 3.
Impact of Increase in Bed Capacity on the Number of Patients Waiting
| Subacute beds |
Residential beds |
||||
|---|---|---|---|---|---|
| Simulation outputs | a | 68 | 73 | 1125 | 1135 |
| N of subacute patients waiting for residential placement | 4.1 | 4.2 | 4.3 | 2.5 | 0.8 |
| N of acute patients waiting for subacute placement | 98.3 | 44.4 | 15.6 | 36.5 | 6.2 |
Subacute beds = 63; Residential beds = 1115; LOS estimates based on the observation data.
Table 4.
Impact of Reduction in LOS on the Number of Patients Waiting
| Subacute LOS |
Residential LOS |
||||
|---|---|---|---|---|---|
| Simulation outputs | a | 12 days | 15 days | 7 days | 14 days |
| N of subacute patients waiting for residential placement | 4.1 | 4.1 | 3.9 | 1.1 | 0.5 |
| N of acute patients waiting for subacute placement | 98.3 | 46.7 | 19.2 | 8.5 | 1.9 |
Subacute beds = 63; Residential beds = 1115; LOS estimates based on the observation data.
Table 3 demonstrates an option that enables reduced waiting in the acute hospital by increasing bed capacity. The number of acute patients waiting for subacute transfer was reduced to 16 from 98 by adding 10 subacute beds. Obviously, this option does not solve the blocking problem in the subacute setting. The scenario was examined, since it is likely to be one of proposed options, where a shortage in acute care bed capacity and acute hospital bed blocking is observed. Another option to reduce the extent of congestion would be to increase the residential bed capacity. Adding 20 residential beds would resolve the blocking problem, and, as a consequence, the problem of acute inpatients waiting for transfer to the subacute care setting.
Alternatively, reducing LOS at the subacute and residential settings would also contribute to easing congestion. We considered a policy scenario of reducing LOS among the long stay clients (60 days and longer for the subacute, and 180 days for the residential clients). On average, LOS was reduced by 12 days and 15 days among the subacute clients, and 7 days and 14 days among the residential clients. The simulation results were presented in Table 4. Shortening LOS of long-stay clients at the subacute setting by 12 and 15 days produced similar effects as increasing the number of subacute beds by 5 and 10. Reducing residential LOS by 14 days would resolve the waiting problem of acute care patients into subacute beds without increasing bed capacity or reducing LOS of subacute clients.
DISCUSSION
In this paper we provided a simulation-based approach to service system planning, focused on hospital and residential service components. The strength of the simulation model is its capability to allow planners to see possible impacts of changes in input parameters (i.e., arrival rates, service times, and bed capacity) on overall system performance. Using the hypothetical scenario of increased demand for residential placement among subacute hospital patients, we illustrated how bed blocking might occur and how it would affect the flow of acute hospital patients into the subacute setting. It demonstrated that delayed transfer of subacute patients to the residential setting caused a large number of acute patients to wait for transfer to the subacute setting. The simulation results suggest that an increase in the residential bed capacity or a reduction in the LOS of clients in the residential setting would be an efficient way to reduce congestion. Residential capacity planning has a profound effect in improving the efficiency of service delivery, where congestion in the client flow is expected.
The findings of the simulation “what-if” analyses support the fact that shortening residential and subacute hospital LOS would reduce the level of congestion. They point out the importance of integrating client flow management into bed capacity planning. For example, expanding housing options and availability, including supported housing sites, can be advocated in reference to its projected effect on the client flow in the hospital and residential system. As well, ICM/ACT can expect to reduce the subacute and residential LOS by efficiently coordinating support services and assisting clients to live in more independent settings than in structured residential setting. Availability of ICM/ACT may have a significant impact for system planning not only because of the expected effect on preventing hospital admissions but also because of expected reduction in LOS. Furthermore, the simulation results showed the importance of improving administrative efficiency. Mental health administrators will see the benefit of implementing a centralized referral and placement mechanism to reduce time spent on matching clients with available resources. The simulation model is useful in quantifying the impact of these measures on required hospital and residential bed capacity under explicitly stated assumptions. Thus, the utility of a simulation model is to assist mental health administrators and other stakeholders to better understand the interconnected nature of service demand and gain insights in possible causes and solutions to the problem. This will facilitate coordinated, rational planning efforts.
The simulation model described in this paper does not necessarily represent “true” demand for services since data used to construct input parameters are derived from the actual system and are confounded by supply issues and contextual factors. By estimating service demand based on client needs as opposed to current use, i.e., how many new clients require treatment at each component and for how long, a simulation model representing the “ideal” system could be constructed. For example, routinely collected data on clinical outcome measurements (i.e., case mix variables presented at the beginning of the treatment episode and concurrent evaluation of outcomes at regular intervals during treatment) is an excellent data source for constructing need-based input parameters.
The application of modeling technologies to real world problems is challenging. The model validation is an ongoing process involving end-users of the model, model developers, and experts in the field. Questions to be addressed include whether the model appropriately represents an actual service system, and to what extent estimated input parameters and model outputs are consistent with perceptions of experts in the field. Continuous refinement of the model in collaboration with mental health administrators is necessary to improve the utility of the model.
A well recognized limitation in modeling is the difficulty in establishing predictive validity, the concordance between model outputs and actual events in the future. No widely accepted practices and techniques yet exist to help validate complex network models (Heidemann, Mills, & Kumar, 2001). It is difficult since “ground truth” to which model outputs are compared is not always available, where real world experiments are infeasible and systems and their interaction with the outside world are constantly changing. The model projections are contingent upon assumptions and data inputs. When the conditions under which the model was constructed (e.g., system configuration, practice pattern, social circumstances) change, the assumptions and data inputs may not hold, and the model needs to be revised to incorporate the changes. For example, in this case study, the simulation suggested adding 20 residential beds would resolve the blocking and waiting problems. However, in reality, when more residential beds become available, a new group of clients from outside of the system are likely to be admitted, and adding new residential beds may not produce an expected reduction in blocking in the subacute setting. In the future, modeling efforts should be directed to document a level of confidence in projected outputs and input parameters, and to identify sources of uncertainty. The currently presented simulation model does not predict the effects of changes in policy with accuracy, rather it presents quantified comparison of policy options under the same set of assumptions, which, we believe, have a great value in bed capacity decision making.
Despite of the limitation of predictive validity, the simulation based modeling approach has tremendous potential to improve service system planning. What is essential in developing a model is to make it as transparent as possible so that the logical connection between inputs and outputs can be grasped at an intuitive level (Weinstein et al., 2003). The model can be used to monitor the system systematically over time to evaluate effects of policy decisions. The longitudinal data on the systematic evaluation of the system will improve our understanding of relationships between changes in policy and practice and the client flow, and our ability to predict the effects of future policy decisions.
As demonstrated in the study, the simplified hospital and residential system model does not require extensive data to derive simulation input parameters, nonetheless, provides valuable insights to decision makers. Since many states have developed an information management system containing basic information on client, provider, and service use, the simulation model will be applicable to settings other than Philadelphia. Where sufficient data is not available, the model can still be constructed using local expert opinions and can help them in visualizing overall system configurations and interconnections between system components as well as guide administrative data collection efforts in the future.
ACKNOWLEDGMENTS
This research was supported by a grant from NIMH (R21 #MH065307). The authors thank staff members in Access to Alternative Services unit, Philadelphia Mental Health Care Corporation, Philadelphia County Office of Mental Health for their input to this paper.
Footnotes
Weibull pdf = αβ−αxα−1e−(x/β)α
REFERENCES
- Budson R. Models of supportive living: Community residential care. In: Herz SJ, Docherty JP, editors. Handbook of schizophrenia, Vol. 4: Psychosocial treatment of schizophrenia. Elsevier Science; Amsterdam: 1990. pp. 317–338. [Google Scholar]
- Clifford P, Charman A, Webb Y, Craig TJK, Cowan D. Planning for community care: The community placement questionnaire. British Journal of Clinical Psychology. 1991;30:193–211. doi: 10.1111/j.2044-8260.1991.tb00938.x. [DOI] [PubMed] [Google Scholar]
- Durbin J, Cochrane J, Goering P, Macfarlane D. Needs based planning: Evaluation of a level of care planning model. Journal of Behavioral Health Services and Research. 2001;28(1):67–80. doi: 10.1007/BF02287235. [DOI] [PubMed] [Google Scholar]
- Fox-Grage W, Folkemer D, Lewis J. The States’ response to the Olmstead decision: How are States complying? [April 24, 2004];Forum for State Health Policy Leadership, National Conference of State Legislatures. 2003 from http://www.ncsl.org/programs/health/forum/olmsreport.pdf.
- Group for the Advancement of Psychiatry [GAP] Beyond symptom suppression: Improving long-term outcomes of schizophrenia. American Psychiatric; Washington, DC: 1992. [PubMed] [Google Scholar]
- Hadley TR, Turk R, Vasko S, McGurrin C. Community treatment teams: An alternative to state hospital. Psychiatric Quarterly. 1997;68(1):77–90. doi: 10.1023/a:1025461206155. [DOI] [PubMed] [Google Scholar]
- Heidemann J, Mills K, Kumar S. Expanding confidence in network simulations. IEEE Network. 2001:58–63. Spring/October. [Google Scholar]
- Herman SE, Mowbray CT. Client typology based on functioning level assessments: Utility for service planning and monitoring. The Journal of Mental Health Administration. 1991;18(2):101–115. doi: 10.1007/BF02518604. [DOI] [PubMed] [Google Scholar]
- Microsoft Visual C++ 6.0 (Professional Ed.) (2003). Microsoft.
- Randolph FL, Ridgway P, Carling PJ. Residential programs for persons with severe mental illness: A nation wide survey of state-affiliated agencies. Hospital and Community Psychiatry. 1991;42(11):1111–1115. doi: 10.1176/ps.42.11.1111. [DOI] [PubMed] [Google Scholar]
- Rothbard AB, Kuno E, Hadley T, Dogin J. Psychiatric service utilization and cost for persons with schizophrenia in a Medicaid managed care program. Journal of Behavioral Health Services and Research. 2003;31(1):1–12. doi: 10.1007/BF02287334. [DOI] [PubMed] [Google Scholar]
- Rothbard AB, Schinnar AP, Foley K, Hadley TR, Kuno E. A cost comparison of state hospital vs. community-based care for an admission population of seriously mentally ill adults. American Journal of Psychiatry. 1998;155(4):523–529. doi: 10.1176/ajp.155.4.523. [DOI] [PubMed] [Google Scholar]
- Rothbard AB, Kuno E, Schinnar A, Hadley TR, Turk R. Service utilization and cost of community care for discharged state hospital patients: A 3-year follow-up study. American Journal of Psychiatry. 1999;156(6):920–927. doi: 10.1176/ajp.156.6.920. [DOI] [PubMed] [Google Scholar]
- Rothbard AB, Richman E, Hadley T. “Unbundling” of state hospital services in the community: The Philadelphia state hospital story. Administration and Policy in Mental Health. 1997;24(5):391–398. doi: 10.1007/BF02042721. [DOI] [PubMed] [Google Scholar]
- Seling MJ, Johnson GW. A bridge to the community for extended-care state hospital patients. Hospital and Community Psychiatry. 1990;41(2):180–183. doi: 10.1176/ps.41.2.180. [DOI] [PubMed] [Google Scholar]
- Tessler RC, Bernstein AG, Rosen BM, Goldman HH. The chronically mentally ill in community support systems. Hospital and Community Psychiatry. 1982;33(3):208–211. doi: 10.1176/ps.33.3.208. [DOI] [PubMed] [Google Scholar]
- Weinstein MC, O'Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, et al. Principles of good practice for decision analytic modeling in health-care evaluation: Report of the ISPOR Task Force on good research practices—modeling studies. Value in Health. 2003;6(1):9–17. doi: 10.1046/j.1524-4733.2003.00234.x. [DOI] [PubMed] [Google Scholar]