Abstract
This article provides a description of the Maternal and Child Health Epidemiology Program housed in the Division of Reproductive Health at the Centers for Disease Control and Prevention. The article highlights programmatic efforts to build capacity and increase infrastructure within states, localities, and among tribes in the field of maternal and child health by leveraging partnerships with other federal, nonprofit, private, and academic agencies.
Introduction
The Maternal and Child Health Epidemiology Program (MCHEP) at the Centers for Disease Control and Prevention (CDC) has been in existence for more than 25 years. In 1986, CDC and the Health Resources and Services Administration/Maternal and Child Health Bureau (HRSA/MCHB) developed the MCHEP and released a Request for Applications offering to provide direct epidemiologic assistance to states' MCH programs through time-limited assignments of MCH epidemiologists. The program was originally envisioned as a way to promote collaboration between federal agencies and states and has evolved into a long-term, well-developed partnership among CDC, HRSA, and affiliated states.
The mission of the MCHEP is to promote and improve the health and well-being of women, children, and families by building capacity at state, local, and tribal levels and to use and apply sound epidemiologic research to impact MCH programs and policies. In MCH, capacity building is defined as an agency's ability to implement, support, and maintain programs and policies focused on the MCH population. In the context of this article, capacity refers to an agency's ability to support and expand MCH epidemiology efforts.
Since its inception, the MCHEP has assigned more than 35 senior CDC epidemiologists focused on MCH epidemiology capacity building and applied research to 20 states, to agencies in Washington, DC, Puerto Rico, and the U.S.-Mexico Border Region, and to organizations including CityMatCH, the Northwest Portland Area Indian Health Board, and the Indian Health Service (Table 1). The program has also sponsored 17 national scientific conferences, numerous fellowships, and many training initiatives. Activities of the MCHEP include the development, improvement, and maintenance of comprehensive MCH surveillance systems; state program coordination in the areas of intervention research, healthcare financing, human resource and database development; data analysis for program development and implementation; training and capacity building to effectively implement surveillance and intervention research findings; and program evaluation. The foundation of these capacity-building efforts is collaboration both with states and with other agencies.
Table 1. States, Territories, and Agencies That Have Hosted Maternal and Child Health Epidemiology Program Assignees Through September 2011.
Current host sites
|
Previous host sites
|
This article describes the structure, role, and impact of the MCHEP, defines how partnership and collaboration have moved the program forward, provides examples of successful projects and outcomes produced from partnerships, and discusses the future of continued collaboration in a time of shrinking resources.
Justification, Framework, and Structure of the Program
The Council of State and Territorial Epidemiologists' 2009 assessment of MCH capacity indicates that as a field, MCH epidemiology has increased substantially over the past decade among U.S. states, a promising trend.1 However, this success has been based on long-term development of capacity-building programs. The Council report also concludes that the percentages of states with minimal to no MCH capacity has decreased from 25% in 2004 to 12% in 2009. The overall percentage of states with a substantial level of MCH capacity in 2009 was 55%; in comparison, other programs with high percentages of near full capacity include infectious diseases 92%, bioterrorism/emergency response 73%, and chronic diseases 53%.2,3 Although the MCHEP cannot claim responsibility for the capacity increases in MCH epidemiology, the program has provided senior-level epidemiologists to numerous states and regions and supported epidemiology fellowships to build capacity. A 1999 evaluation conducted by the University of Illinois at Chicago indicated that states with a MCHEP assignee scored higher in capacity ratings than did states that had never participated in the MCHEP. A 2006 follow-up assessment by the same group of researchers found that access to a MCHEP assignee was related to higher MCH epidemiology functioning in states.4,5
The MCHEP is a model for capacity building in states, tribes, localities, and territories. The placement process is similar to that of the CDC Epidemic Intelligence Service program, with MCHEP applicants and state-proposed assignments evaluated concurrently. For a potential applicant, a selection committee rigorously reviews each MCHEP applicant's materials. Applicants are either recommended or rejected for interview and, if interviewed, are either recommended or not recommended to candidacy. When the MCHEP receives the recommendations from the committee, the program lead reviews the interview and application materials and makes a final decision on candidacy. Once approved, applicants and assignments are matched based on assignment priorities and candidate qualifications.
The MCHEP maintains a set of eligibility criteria for an assignee position:
Doctoral degree or medical doctor with a master's degree in epidemiology or a related field
Intermediate knowledge and experience in epidemiology, statistics (e.g., multivariable modeling), and statistical programming experience or training in a related field
Experience working in MCH or on MCH issues
Intermediate knowledge and experience in communicating effectively both orally and in writing to public health leaders, public health staff, the health community, colleagues, fellow members of a team, and public health audiences
Intermediate knowledge and experience working on a multidisciplinary team to accomplish common goals and projects
Potential to become a MCH epidemiology leader
To qualify as a potential host site, the MCHEP requires a state or agency to submit a proposal to obtain an assignee. The proposal is used to facilitate the matching process and outlines the assignment and priority areas of focus for the assignee, including:
The purpose of the request for the assignment
Funding mechanisms for the assignment (CDC funds a percentage of the assignee salary; the host state/agency must provide the remaining percentage)
Justification for the assignment (e.g., public health concerns/statistical support of high rates/disparities)
Assignment structure, including the assignee's placement in the organizational chart and physical location of the assignee
First-year projects to be completed by the assignee
Partnerships include strong relationships with multiple agencies, academic institutions, hospitals, state health departments, local health departments, nonprofit agencies, and medical schools. The MCHEP assignees develop, coordinate, and maintain partnerships and programs within their assigned states and agencies. Assignees are also responsible for increasing the use of evidence-based science in the field and using the applied science process to advance state programs and policies.6 Assignees spend the first year of the assignment establishing rapport and developing a reputation for creditable scientific work in their respective states and agencies. By placing assignees in senior leadership positions within each state health department or agency, the MCHEP ensures access to officials with decision-making capabilities; facilitates the ability of an assignee to work across bureaus, divisions, and programs; and supports access to data sources available within the state or agency. After the first 2 years of assignment, the MCHEP assignees are expected to recruit and mentor young MCH professionals.
Depending on state needs, an assignee may develop a research center; supervise the scientific work of multiple state staff; provide scientific oversight for programs, data collection, and surveillance; develop and maintain program budgets; work with state legislatures to develop policies; link data systems; participate in primary data collection; provide analytic support; use public health theory to enhance programs; or become an expert in a specific field of research. These assignment activities culminate in the development of collaborative partnerships both internal and external to the states.
Partnership and Collaboration
The MCHEP has a long history of working with partners that provide direct services to women and children throughout the nation. Program goals include supporting partners as they increase MCH epidemiology capacity and building infrastructure, such as a qualified workforce through training, up-to-date data and information systems, and enhanced ability to respond to public health needs in MCH. Early and sustained partnerships with the HRSA/MCHB and state health departments provide the foundation of the MCHEP. The vision of the program—to build MCH epidemiology capacity and infrastructure in states—was conceived at program inception in partnership with the HRSA/MCHB. The HRSA/MCHB and the MCHEP have maintained a strong partnership over the past 25 years, and this relationship has burgeoned into in-kind support for multiple conferences, trainings, and fellowships in MCH epidemiology. In fact, states no longer supported by the MCHEP direct assistance assignments have continued to collaborate with the program even though formal agreements may have ended. Currently, there are 12 MCH epidemiologists assigned to states and agencies engaged in capacity-building efforts throughout the United States (Table 1 and Fig. 1).
Fig. 1.
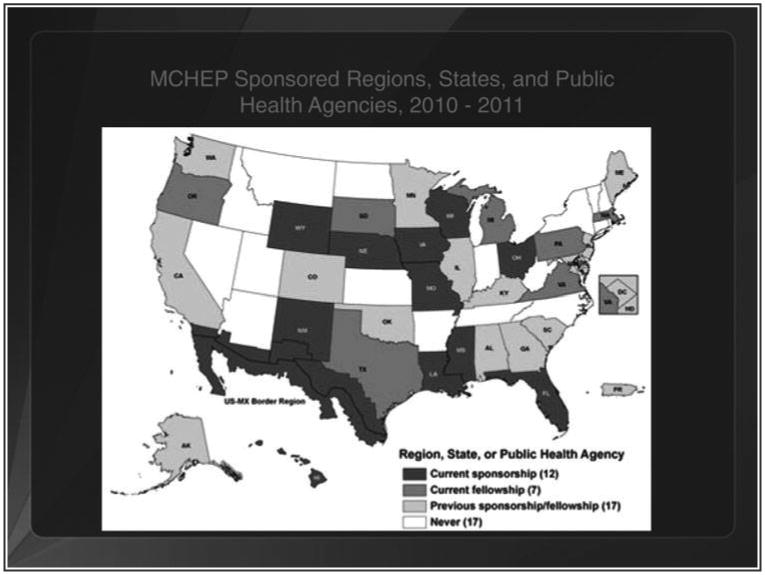
Location of current and previously Maternal and Child Health Epidemiology Program-sponsored states, regions, or agencies, October 2010–September 2011.
The MCHEP also has connected states with other federal, national, and not-for-profit agencies (Table 2) to increase capacity in MCH epidemiology. For example, the program has worked with the Association of Maternal and Child Health Programs, the Council of State and Territorial Epidemiologists, and CityMatCH to distribute information on best practices; to conduct methodology-focused trainings for MCH epidemiologists working in states, communities, tribes, and localities; and to support fellows in varied field experiences. The program has partnered with the national March of Dimes Foundation to provide universal access to MCH data by supplementing PeriStats (a web-based data query system providing free access to U.S., state, county, and city maternal and infant health data) with state-level information from the Pregnancy Risk Assessment Monitoring System (PRAMS).7 These partnerships continue to have an impact on the field of MCH epidemiology in the United States.
Table 2. Partner Organizations.
Federal agencies, state, and tribal programs
|
National organizations
|
Journal
|
University partners
|
Additionally, the MCHEP maintains partnerships with a number of universities, professional organizations, and academic organizations. A long-term partnership with the University of Illinois at Chicago has enabled MCHEP to provide training to a number of state health department staff on complex survey methodology, multivariable modeling, and development of data reports to support grant applications. A strong collaborative partnership recently developed between the MCHEP and Harvard University has provided an opportunity for Master of Public Health graduate students to obtain field experience in program evaluation by traveling to a state health department and developing an evaluation framework for a MCH program. During this time of limited resources, this new program provides invaluable support for states. Faculty at Emory University also work closely with the MCHEP to support research on populations in the U.S.-Mexico Border Region and in urban communities throughout the United States. Finally, the MCHEP maintains partnerships with organizations that support national recognition of MCH professionals whose work contributes to the field of MCH by supporting the National MCH Epidemiology Awards at the annual conference. These partnerships increase capacity for MCH epidemiology from the community levels to state levels, as well as at universities, through in-kind and joint support of training activities and recognition of professional contributions to the field of MCH.
Public Health Impacts of Capacity Building and Increased Infrastructure in MCH Epidemiology
Partnership and collaboration continue to have an impact on the reach and influence of the MCHEP. Partnership activities propel the program and promote sharing of knowledge and resources across MCH-related programs in the United States. From these partnerships, the MCHEP has hosted national and regional conferences, provided national and local trainings, promoted peer exchange and leadership in states, and increased partnership between states and other agencies. The MCHEP promotes partnership within state programs by supporting assignments with multiple foci, such as assignments that provide integration of MCH with chronic disease and injury prevention (e.g., two current assignments are hybrid: MCH, diabetes, and injury; MCH and infectious disease). The program also provides direct support to tribes, the Indian Health Service, and U.S.-Mexico Border communities. The biggest impact of the MCHEP, however, is connecting regions, states, tribes, and communities with nonmonetary resources and in-kind support from MCH agencies.
Each year, with support from partnering agencies, the MCHEP cosponsors the National MCH Epidemiology Con-ference.8 The goal of this conference is to provide a forum for training on new and innovative MCH epidemiologic methodologies; discussion of new research being conducted in states, localities, communities, other agencies, and at universities; and promoting peer exchange among junior, intermediate, and seasoned professionals in MCH epidemiology. In recent years, major conference topics have included the life course perspective, preconception care, translating epidemiologic findings to programs and policies, and the practice of MCH epidemiology. The conference is evaluated annually to ensure that the needs of partners and attendees are addressed. Additionally, in 2011, the MCHEP cosponsored a Western Regional MCH Epidemiology Conference in San Francisco, California.9 The conference provided the same workshops and sessions as the national conference, but tailored to MCH epidemiologists in the West Coast region, where travel restrictions have recently affected attendance at the national conference.
Leveraging partnerships, the MCHEP is able to support a multitude of trainings each year. Specifically, trainings on multiple topics are provided to an average of 60 participants before the annual conference. Annually, in partnership with HRSA/MCHB, training in MCH epidemiology is offered to about 45 participants from state and local health departments. The MCHEP also offers a year-long course for field assignees and participating state staff (n=60 in 2010) hosted by the faculty of the University of Illinois at Chicago. This training focuses on new methodologies or statistical techniques. Finally, the MCHEP sponsors seven web-based MCH Epidemiology Grand Rounds per year on current research and issues in the MCH field for up to 100 participants. Participants include professionals in the field of MCH, from scientists to program directors and clinicians.
The MCHEP supports leadership and workforce development of staff and professionals in the field of MCH epidemiology. While the program requires staff to supervise and engage fellows and interns in MCH epidemiology work, it also supports the mentoring and training of young professionals in other states, including fellows of the Council of State and Territorial Epidemiologists (n=13 in states for 2009– 2010), officers in the Epidemic Intelligence Service (n=3 in 2010), the Graduate Student Internship Program (n= 5 in 2010), medical students, graduate students, and student interns from various university medical and public health programs. Support of these junior professionals provides the foundation for their future work in MCH epidemiology.
To promote leadership, the MCHEP and 15 other national organizations and agencies (Table 2) sponsor the National MCH Epidemiology Awards each year.10 The National Awards highlight contributions to MCH epidemiology and provide recognition in six categories: advancing knowledge, effective practice, outstanding leadership, excellence in teaching, young professional achievement, and lifetime achievement. These categories provide a framework for promoting collaborative work in MCH epidemiology.
Through partnerships with states, the MCHEP has contributed to multiple activities, including development of the Massachusetts Pregnancy to Early Life Longitudinal data system, which links birth certificates, death certificates, and hospital discharge records; examination of decreasing trends in infant mortality in Wisconsin; initiation of a research center at the Division of Public Health in Delaware; development of a department-wide strategic planning effort in Ohio; examination of regionalized systems of care for high-risk neonates in Georgia; and coordination of scientific support for programmatic efforts to integrate MCH, diabetes, and injury in Wyoming.
Conclusion: Collaboration in a Time of Limited Resources
To achieve outcomes in a time of shrinking monetary resources, programs and agencies that previously were unaffected by decreases in funding must consider alternative strategies. One strategy to achieve these outcomes is through partnership and collaboration, specifically through nonmonetary contributions, such as in-kind support and cosponsorship of activities. As MCH programs move forward in this new environment, it is expected that collaboration will become the preferred method of increasing the ability to implement, support, and maintain programs and policies focused on this population. The MCHEP has focused on such activities since its inception 25 years ago, and partnership will continue to play a key role in these efforts. As the MCHEP moves forward, this strategy will greatly impact the program's ability to increase capacity and build infrastructure in MCH epidemiology throughout states, regions, tribes, and localities.
Acknowledgments
The author would like to acknowledge all partners for supporting the work of the MCHEP, including the Association of Maternal and Child Health Programs, American Public Health Association, CityMatCH, American Academy of Pediatrics, Association of Schools of Public Health, Association of Teachers of Maternal and Child Health, American College of Obstetricians and Gynecologists, Council of State and Territorial Epidemiologists, National Association of City and County Health Officials, Association of State and Territorial Health Officials, Health Resources and Services Administration, Maternal and Child Health Bureau, Maternal and Child Health Journal, National Association for Public Health Statistics and Information Systems, National Birth Defects Prevention Network, National March of Dimes Foundation, National Institutes of Health Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Pediatric and Perinatal Epidemiologic Research, University of Illinois at Chicago, Emory University, Harvard University, tribal epidemiology centers, and all state health departments that work closely with our program.
The findings and conclusions in this article are those of the author and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosure Statement: No competing financial interests exist.
References
- 1.Council of State and Territorial Epidemiologists. 2009 National assessment of epidemiology capacity: Supplemental report: Maternal and child health epidemiology capacity: Findings and recommendations. Atlanta: Council of State and Territorial Epidemiologists; 2010. [Google Scholar]
- 2.Council of State and Territorial Epidemiologists. 2009 National assessment of epidemiology capacity: Findings and recommendations. Atlanta: Council of State and Territorial Epidemiologists; 2009. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Assessment of epidemiology capacity in state health departments—United States, 2009. MMWR. 2009;58:1373–1377. [PubMed] [Google Scholar]
- 4.Handler A, Gellar S, Kennelly J. Effective MCH epidemiology in state health agencies: Lessons from an evaluation of the Maternal and Child Health Epidemiology Program (MCHEP) Matern Child Health J. 1999;3:217–224. doi: 10.1023/a:1022329522752. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg D, Herman-Roloff A, Kennelly J, Handler A. Factors associated with improved MCH epidemiology functioning in state health agencies. Matern Child Health J. 2011;15:1143–1152. doi: 10.1007/s10995-010-0680-x. 0680-x. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. [Accessed July 15, 2011];Maternal and Child Health Epidemiology Program. 2011 Available at: www.cdc.gov/reproductivehealth/MCHEpi/index.htm.
- 7.March of Dimes. [Accessed July 15, 2011];PeriStats: Your online source for perinatal statistics. 2011 Available at www.marchofdimes.com/peristats/
- 8. [Accessed July 15, 2011];17th Annual Maternal and Child Health Epidemiology Conference. 2011 Available at www.cdc.gov/reproductivehealth/MCHEpi/Conference/AboutConference.htm.
- 9. [Accessed July 15, 2011];2011 Western Regional Maternal and Child Health Epidemiology Conference. 2011 Available at mchepi.org/sites/default/files/Invitation_2011_Western_MCH_Epi_Conf.pdf.
- 10.Kroelinger C. Recognizing excellence in maternal and child health epidemiology: The 2010 National MCH Epidemiology Awards. Matern Child Health J. 2011;14:822–826. doi: 10.1007/s10995-011-0790-0. [DOI] [PubMed] [Google Scholar]


