Abstract
Objectives
Traditional Cox maze III is the gold standard for treatment of atrial fibrillation (AF). Because of its invasiveness, it has been replaced by a simplified procedure involving radiofrequency ablation of modified Cox maze IV. Although the modified Cox maze IV has the advantages of simplicity and less morbidity, a lower rate of sinus rhythm conversion has been reported. We try to establish a scoring system to predict the outcome of this procedure.
Methods and Results
The derivation group consisted of 287 patients with structural heart disease and chronic AF who underwent cardiac surgery and modified Cox-maze IV procedure between August 2005 and March 2013. Demographics, clinical and laboratory variables were retrospectively collected as sinus conversional predictors. Overall sinus conversion rate was 75.8%. The parameters of the Soft Markers Scoring system included AF duration, preoperative left atrial (LA) size, rheumatic pathology and postoperative LA remodeling. We compared 80 patients from another hospital between January 2004 and December 2011 as a validation group to evaluate the power of the scoring system. Soft Markers Score indicated a good discriminative power by using the areas under the receiver operating characteristic curve (AUROC: 0.759 ± 0.032). The score was further divided into three groups: low (0-2), intermediate (3-5), and high (6-10), with predicted sinus conversion rates of 92.4%, 74.2%, and 47.8%, respectively.
Conclusions
In patients with chronic AF receiving modified Cox-maze IV procedure, the Soft Markers Score demonstrated good discriminative power of predicting sinus recovery in our patients and applied well to the other validation populations.
Introduction
The gold standard treatment for atrial fibrillation (AF), Cox-Maze III procedure, successfully restores atrio-ventricular synchrony and decreases the risk of thromboembolism and stroke. [1] Because of its invasiveness, it has been replaced in most clinical practice by a simplified procedure involving radiofrequency (RF) ablation, modified Cox maze IV. Although the modified Cox maze IV has the advantages of feasibility and decreased morbidity, a lower rate of sinus rhythm recovery has been reported compared with the maze III. [2,3] According to the previous reports, preoperative left atrial (LA) size and the duration of AF are the two most important predictors of sinus conversion. [4–6] However, most reports did not incorporate postoperative LA remodeling to predict the outcome. Collecting both preoperative and postoperative parameters to establish a scoring system to predict the procedure success may be an attractive alternative. In this retrospective study, we examined the Soft Markers Score and other predictors for patients with structural heart disease and chronic AF who underwent concomitant cardiac surgery and modified Cox-Maze IV procedure, aiming to identify the relationship between the sinus rhythm recovery rate and the prognostic scoring system. Moreover, we compared with the validation group from another hospital to confirm the power of the Soft Markers Score.
Materials And Methods
Study population
This retrospective study was conducted after receiving the approval of the Institutional Review Board (IRB) both from our hospital, Chang Gung Memorial Hospital, LinKou, and the other hospital, Chang Gung Memorial Hospital, Kaohsiung, of the validation group (approval No. 102-4227B). Written informed consent for the AF ablation procedure was collected from all patients prior to surgery. The enrolled and excluded criteria in validation group were the same with the derivation group. Only patients with structural heart disease receiving concomitant cardiac surgery were enrolled. Lone AF was excluded from this study. With the aid of a RF device, AF ablation became a routine adjunct operation if patients were willing to receive the procedure and if it was not contraindicated, such as in cases of significant calcification of the left atrial wall in extreme rheumatic heart disease or redo cases with severe pericardial adhesion. The derivation group of 287 patients was collected between August 2005 and March 2013 and compared with the validation group of 80 patients who were operated on between January 2004 and December 2011.
Surgical procedure
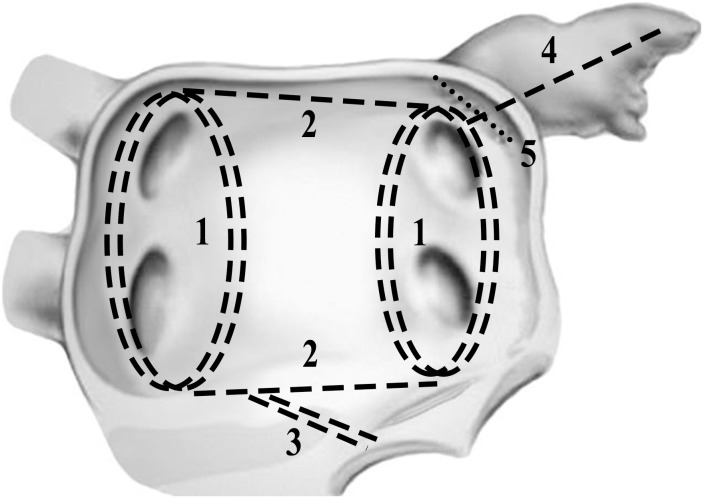
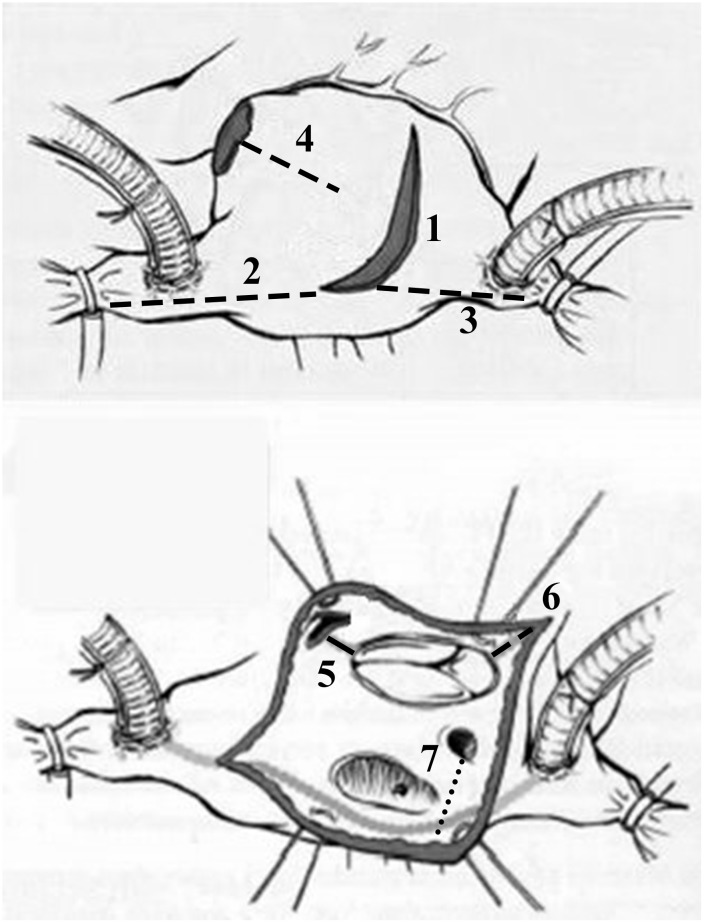
Patients of the derivation group were operated on by three senior surgeons with technical unity and the first ten cases were excluded to avoid learning curve bias. Our routine approach was standard full sternotomy with bicaval cannulations, and AF ablation lesion sets were similar to traditional Cox-Maze III except most cut-and-sew lesions were replaced by the RF ablation device and separated pulmonary vein isolation with two connecting lesions of both superior and inferior pulmonary veins. [7] The complete lesion sets were as the Fig 1 and Fig 2. Additional cryoablation of mitral isthmus was applied with cryoprobe for 2 minutes. Bi-atrial ablation was applied in most cases and left atrial ablation alone was applied solely in elderly patients with isolated aortic valve replacement. The left atrial appendage was closed from inside with 4–0 prolene double running sutures. The ligament of Marshall was divided during left pulmonary vein isolation and bilateral epicardial fats over the interatrial groove, comprised of ganglional plexi, were also resected. Left atrial volume reduction for markedly enlarged left atrium, dimensions > 60 mm by preoperative echo, was carried out with plications of posterior wall between the inferior pulmonary vein and mitral isthmus.
Fig 1. Lesion set of the modified Cox-maze IV procedure, Left atrium.
1. Pulmonary veins isolation: Twice under beating heart. 2. Connect bilateral PV: Double line. 3. Connect to mitral annulus: Twice. 4. Connect LAA to LPV. 5. Suture closure of LAA: From interior, double layers. Additional procedures: divide ligament of Marshall; LA volume reduction. (PV: Pulmonary vein, LAA: Left atrial appendix, LPV: Left pulmonary vein, LA: Left atrium)
Fig 2. Lesion set of the modified Cox-maze IV procedure, Right atrium.
1. Prepare: transverse incision, amputate RAA, loop RAA &RA atriotomy with silk for exposure, free AV groove & RA dome. 2. Connect incision to SVC, beware of SA Node & swan ganz catheter. 3. Connect incision to IVC. 4. Connect from RAA to free wall, leave 2 cm gap. 5. Connect to 10” o’clock of TV annulus. 6. Connect incision to 4” o’clock of TV annulus. 7. Ablation of coronary sinus from inside. (RAA: Right atrial appendix, RA: Right atrium, SVC: Superior vena cava, IVC: Inferior vena cava, TV: Tricuspid valve)
Postoperative medications and follow-up
Class III antiarrhythmic agent, Amiodarone, was used if AF remained postoperatively and without contraindications of junctional bradycardia or prolonged QT interval. After 3 months, if AF persisted, beta blockers were prescribed instead of anti-arrhythmics. Anticoagulant was discontinued at 3 months for patients with sinus conversion and without other lifelong mandatory indications such as receiving mechanical valve replacement. Both of the preoperative and postoperative cardiac measurements were recorded by transthoracic echocardiography. The left atrial diameter was measured in the parasternal long-axis view from the trailing edge of the posterior aortic root-anterior left atrial complex to the posterior left atrial wall at end-systolic phase. The twelve leads electrocardiograms (EKG) were checked monthly at the first three months and then every two to three months periodically at outpatient clinic visit to document atrial rhythm. No routine 24 hours Holter monitoring or event recorder was used unless patients complained of paroxysmal palpitations while resting EKG showed sinus rhythm. Failure of sinus conversion was defined as detection of an episode of AF, atrial flutter or atrial tachycardia lasting more than 30 seconds by Holter. At least one-year follow up was completed for every patient.
Establishment of Soft Markers Scoring system and Validation
Each risk factor in the derivation group was recognized by multivariate logistic regression and the cutoff point of parameters was calculated by acquiring the best Youden Index (sensitivity + specificity -1). While establishing Soft Markers Score parameters from the univariate analysis, we found that rheumatic heart disease had a wider confidence interval compared with other risk factors. We speculated this factor would represent lower power of prediction in the scoring system and defined it as a minor parameter of one score point. The other risk factors defined as intermediate and major parameters were two and three score points, respectively. This comprised of our scoring system with one minor parameter, rheumatic heart disease, three intermediate parameters including preoperative LA diameter over 60 mm, postoperative LA diameter over 50 mm and reduced LA diameter less than 10 mm in echocardiography and one major parameter of preoperative AF duration (Table 1). To test the Soft Markers Score as a powerful independent predictor of the sinus recovery in chronic AF patients, we compared the areas under the receiver operating characteristic (AUROC) curve of the Soft Markers Score both in the derivation and validation group.
Table 1. Soft Marker Scoring system.
| Point | Parameter |
|---|---|
| 1 point | Rheumatic heart disease |
| 2 points | Preoperative LA diameter > 60 mm |
| Postoperative LA diameter > 50 mm | |
| Postoperative LA reduction < 10 mm | |
| 3 points | AF duration > 4 years |
LA: left atrial
Statistical analysis
Descriptive statistics such as number of observations, mean and standard deviation will be presented for continuous variables. The primary analysis compared rates of sinus recovery with whom of persistent AF at the last follow up. All variables were tested for normal distribution using the Kolmogorov-Smirnov test. The Student’s t test was utilized to compare the means of continuous variables and normally distributed data. If assumption of normality is not satisfied, the use non-parametric analysis, the Mann-Whitney U test, will be considered. Categorical data were tested with the chi-square test or the Fisher exact test. Risk factors for sinus conversion were assessed first by univariate logistic regression, and enrolled into a multivariate analysis if statistical significance was met (p < 0.05). The multivariate analyses were assessed by applying multiple logistic regressions based on forward data eliminations. Calibration was assessed using the Hosmer-Lemeshow goodness-of-fit test (C statistic) to compare the number of observed abnormal cardiac rhythms. Discrimination was assessed using the AUROC curve. Areas under two AUROC curves were compared with a non-parametric approach. The AUROC analysis was also performed to calculate cutoff values, sensitivity, and specificity. All statistical tests were two- tailed and evaluated at 0.05 level of significance. Data were analyzed using SPSS 20.0 for Windows (SPSS, Inc., Chicago, IL, USA) and STATA 11.0 for Mac (StataCorp LP, Texas, USA).
Result
Patients’ demographics
From August 2005 to March 2013, 287 patients (age: 20.3–85.6; mean: 59.0±0.7 years old) underwent the modified Cox-maze IV ablation of AF in addition to cardiac surgery. Concomitant procedures included mitral valve replacement (n = 95), mitral repair (n = 162), aortic valve replacement (n = 53), tricuspid repair (n = 159), and coronary artery bypass graft (n = 23). There were 4.9% (n = 14) hospital mortality and follow-up was completed at 99.3% (n = 285) with a mean follow-up of 38 months (range 12–96), at least twelve months for every patient. Less than 5% of the patients underwent Holter examinations. Final sinus conversion rate without any antiarrhythmic medication was 75.8% (n = 216). Demographics and clinical characteristics of both sinus recovery and non-sinus conversion group were listed in Table 2 and different mitral valve pathology related to sinus conversion was presented in Table 3.
Table 2. Patients’ demographics and clinical characteristics according to sinus recovery.
| Postoperative rhythm | ||||
|---|---|---|---|---|
| All patient (n = 287) | Sinus (n = 216) | Non-sinus (n = 71) | p | |
| Age (years) | 59.0 ± 0.7 | 58.6 ± 0.8 | 60.3 ± 1.0 | 0.203 |
| Gender, male | 140 (48.8%) | 108 (50%) | 32 (45.1%) | 0.471 |
| BMI (kg/m2) | 23.4 ± 0.2 | 23.5 ± 0.3 | 23.2 ± 0.4 | 0.494 |
| DM | 39 (13.6%) | 27 (12.5%) | 12 (16.9%) | 0.348 |
| ESRD | 5 (1.7%) | 4 (1.9%) | 1 (1.4%) | 1.000 |
| Serum creatinine (mg/dL) | 1.09 ± 0.08 | 1.14 ± 0.10 | 0.90 ± 0.03 | 0.512 |
| AF duration (month) | 53.9 ± 3.7 | 44.9 ± 4.5 | 75.4 ± 5.3 | < 0.001 |
| PA systolic pressure (mmHg) | 55.9 ± 1.3 | 55.2 ± 1.5 | 57.6 ± 2.3 | 0.344 |
| PA diastolic pressure (mmHg) | 27.1 ± 0.6 | 27.3 ± 0.7 | 26.8 ± 1.2 | 0.739 |
| PA mean pressure (mmHg) | 38.5 ± 0.8 | 38.4 ± 1.0 | 38.8 ± 1.4 | 0.685 |
| CHADS2 score | 1.5 ± 0.1 | 1.5 ± 0.1 | 1.4 ± 0.1 | 0.446 |
| Bi-atrial ablation | 267 (93.0%) | 200 (92.7%) | 67 (94.4%) | 0.426 |
| LA reduction | 130 (45.3%) | 90 (41.7%) | 40 (56.3%) | 0.031 |
| Mitral valve repair/replacement | 276 (96.2%) | 208 (96.3%) | 68 (95.8%) | 0.736 |
| Tricuspid valve repair | 159 (55.4%) | 111 (51.4%) | 48 (67.6%) | 0.017 |
| Aortic valve replacement | 53 (18.5%) | 36 (16.7%) | 17 (23.9%) | 0.170 |
| CABG | 23 (8.0%) | 21 (9.7%) | 2 (2.8%) | 0.063 |
| Complex procedure* | 49 (17.1%) | 38 (17.6%) | 11 (15.5%) | 0.683 |
| Numbers of valve surgeries | 1.7 ± 0 | 1.7 ± 0 | 1.9 ± 0.1 | 0.008 |
| Leaving OR rhythm, sinus | 161 (71.9%) | 123 (72.4%) | 38 (70.4%) | 0.778 |
| Need mechanical support** | 13 (4.5%) | 7 (3.2%) | 6 (8.5%) | 0.095 |
| Need temporary pacing | 51 (17.8%) | 41 (19.1%) | 10 (14.1%) | 0.341 |
| Pre OP EF % | 59.5 ± 0.8 | 58.2 ± 1.0 | 63.5 ± 1.2 | 0.014 |
| Pre-OP LA diameter (mm) | 58.9 ± 0.7 | 57.4 ± 0.7 | 63.4 ± 1.4 | < 0.001 |
| Pre-OP LVEDD (mm) | 55.1 ± 0.6 | 55.6 ± 0.8 | 53.4 ± 1.0 | 0.092 |
| Pre-OP LVESD (mm) | 36.9 ± 0.6 | 37.7 ± 0.8 | 34.2 ± 0.9 | 0.003 |
| Post-OP EF % | 60.8 ± 0.8 | 60.7 ± 1.0 | 61.1 ± 1.2 | 0.649 |
| Post-OP LA diameter (mm) | 47.2 ± 0.6 | 45.5 ± 0.7 | 52.1 ± 1.1 | < 0.001 |
| Post-OP LVEDD (mm) | 48.8 ± 0.5 | 48.9 ± 0.6 | 48.5 ± 0.8 | 0.663 |
| Post-OP LVESD (mm) | 32.5 ± 0.6 | 32.6 ± 0.7 | 32.3 ± 0.8 | 0.421 |
| Post-OP LA reduced diameter (mm) | 11.9 ± 0.7 | 11.5 ± 0.8 | 11.0 ± 1.4 | 0.785 |
| Soft Marker Score | 2.8 ± 0.1 | 3.2 ± 0.2 | 5.5 ± 0.3 | < 0.001 |
AF: atrial fibrillation; BMI: body mass index; CABG: coronary artery bypass graft; DM: diabetes mellitus; EF: ejection fraction; ESRD: end stage renal disease; LVEDD: left ventricle end-diastolic diameter; LVESD: left ventricle end-systolic diameter; OP: operation; OR: operation room; PA: pulmonary artery
*Complex procedure: combined coronary artery bypass or triple valve surgeries.
**Mechanical support: Intra-aortic balloon pump (IABP) or extracorporeal membrane oxygenation (ECMO)
Table 3. Mitral valve pathology data according to sinus recovery.
| Postoperative rhythm | ||||
|---|---|---|---|---|
| All patient (n = 265) | Sinus (n = 199) | Non-sinus (n = 66) | p | |
| Degenerative | 91 (34.3%) | 71 (35.7%) | 20 (30.3%) | 0.434 |
| Ischemic | 21 (7.9%) | 17 (8.5%) | 4 (6.1%) | 0.518 |
| Rheumatic | 112 (42.3%) | 76 (38.2%) | 36 (54.5%) | 0.020 |
| Dilated | 35 (13.2%) | 30 (15.1%) | 5 (7.6%) | 0.119 |
| Endocarditis | 3 (1.1%) | 3 (1.5%) | 0 (0%) | 0.576 |
| Previous prosthesis dysfunction* | 10 (3.8%) | 6 (3.0%) | 4 (6.1%) | 0.272 |
*: bioprosthesis degeneration/endocarditis or mechanical valve thrombosis/endocarditis
Calibration and Discrimination for Risk Factor and Soft Markers Score
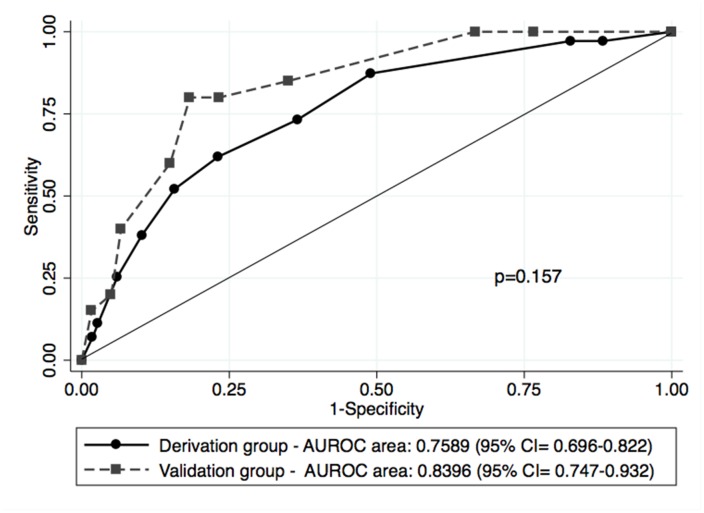
Hosmer-Lemeshow chi-square statistic of predicted non-sinus recovery risk and the AUROC were used to assess calibration and discrimination, respectively. Table 4 compares some important predictors of sinus conversion for these patients. Calibration for Soft Markers Score (Hosmer-Lemeshow chi-square 6 = 5.409; p = 0.493) was good. The AUROC curve confirmed the good discrimination power of the Soft Markers Score (AUROC, 0.759 ± 0.032; 95% confidence interval [CI], 0.695–0.822, p < 0.001) compared with preoperative, postoperative LA diameter, and AF duration.
Table 4. Comparison of calibration and discrimination of the score and risk factors in sinus recovery.
| Calibration | Discrimination | |||||
|---|---|---|---|---|---|---|
| Hosmer-Lemeshow | df | p | AUROC ± SE | 95% CI | p | |
| Soft Marker Score | 5.409 | 6 | 0.493 | 0.759 ± 0.032 | 0.695–0.822 | < 0.001 |
| AF duration | 16.811 | 8 | 0.032 | 0.708 ± 0.041 | 0.626–0.789 | < 0.001 |
| Pre-OP LA diameter | 5.296 | 8 | 0.726 | 0.650 ± 0.037 | 0.579–0.722 | < 0.001 |
| Post-OP LA diameter | 14.369 | 8 | 0.073 | 0.711 ± 0.035 | 0.642–0.780 | < 0.001 |
Long-Term Prognosis and Validation
In multivariate analysis without the Soft Markers Score, the preoperative LA size and postoperative LA size were all the independent predictors. After we included the Soft Markers Score, though several variables showing prognostic significance in univariate analysis, only Soft Markers Score was identified as independent predictor in multivariate analysis in Table 5. The logarithm of odds = -2.314 + 0.46 × Soft Markers Score. Table 6 lists the demographics, medical histories, and outcomes in the derivation and validation groups. We found the patients in the validation group had shorter AF duration, smaller LA diameters and better EF before operation, and more reduced LA diameter after operation. A comparison of the AUROC between derivation group and validation group confirms the good discrimination power of the Soft Marker Score in the validation group (AUROC, 0.840 ± 0.049; 95% confidence interval [CI], 0.747–0.932, p < 0.001). Moreover, the nonparametric comparison revealed that there was no statistically significant difference between the derivation and the validation group (Fig 3). The Soft Marker Score provided good predictor power in both groups and was divided into 3 categories: Low, intermediate and high risks. The low risk group, compromising scores from 0 to 2, intermediate risk group of 3 to 5 and high risk group of 6 to 10 points had sinus rhythm recovery rates of 92.4%, 74.2%, and 47.8%, respectively. The overall sinus recovery rate in the Soft Markers Score is shown in Table 7.
Table 5. Variables showing prognostic significance.
| Univariate logistic regression | Multivariate logistic regression | |||
|---|---|---|---|---|
| Parameter | OR (95% CI) | p | OR (95% CI) | p |
| AF duration (month) | 1.013 (1.006–1.020) | < 0.001 | ||
| LA reduction | 1.806 (1.051–3.104) | 0.032 | ||
| Tricuspid valve repair | 1.974 (1.123–3.470) | 0.018 | ||
| Numbers of valve surgeries | 1.766 (1.146–2.719) | 0.010 | ||
| Pre OP EF % | 1.031 (1.088–1.054) | 0.007 | ||
| Pre-OP LA diameter (mm) | 1.049 (1.023–1.076) | < 0.001 | ||
| Pre-OP LVESD (mm) | 0.964 (0.936–0.993) | 0.015 | ||
| Post-OP LA diameter (mm) | 1.083 (1.047–1.119) | < 0.001 | ||
| Mitral: rheumatic pathology | 1.942 (1.106–3.409) | 0.021 | ||
| Soft Marker Score | 1.444 (1.285–1.624) | < 0.001 | 1.452 (1.253–1.683) | < 0.001 |
Table 6. Patients’ demography data in Derivation and Validation groups.
| Derivation (n = 287) | Validation (n = 80) | p | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 59.0 ± 0.7 | 56.7 ± 1.5 | 0.119 |
| Gender, male | 140 (48.8%) | 38 (47.5%) | 0.839 |
| BMI (kg/m2) | 23.4 ± 0.2 | 23.1 ± 0.4 | 0.504 |
| Medical history | |||
| AF duration (months)* | 53.9 ± 3.7 | 51.8 ± 7.4 | 0.049 |
| Pre OP LA diameter (mm) | 58.9 ± 0.7 | 54.4 ± 1.1 | 0.001 |
| Pre OP EF% | 59.5 ± 0.8 | 64.6 ± 1.4 | 0.004 |
| Bi-atrial ablation | 224 (78.0%) | 67 (83.8%) | 0.073 |
| Mitral valve surgery | 276 (96.2%) | 78 (97.5%) | 0.742 |
| Rheumatic heart disease | 112 (42.3%) | 35 (43.8%) | 0.814 |
| Outcome | |||
| Sinus conversion | 216 (75.3%) | 60 (75.0%) | 0.998 |
| Post OP LA diameter | 47.2 ± 0.6 | 43.1 ± 1.1 | 0.001 |
*Compared with patient whose AF durations were known
Fig 3. AUROC curve of Derivation and Validation groups.
This is the Soft Marker Score ROC curve of the derivation and validation groups. It shows the good discrimination power of the Soft Marker Score and the p-value shows there was no statistically significant difference between the derivation and validation group. (CI: confidence interval)
Table 7. Sinus recovery rate in Soft Marker Score.
| Soft marker score | Sinus recovery rate |
|---|---|
| Low risk (score 0–2) | 92.4% |
| Intermediate risk (score 3–5) | 74.2% |
| High risk (score 6–10) | 47.8% |
Discussion
Modified Cox maze IV with RF assisted ablation has replaced the traditional cut and sew in most clinical practice because of its simplicity and less invasiveness. However, less sinus conversion drives us to pursue a better tool to predict the outcome of surgical ablation, focus more on potentially correctable factors and improve the success rate [2,3]. The Soft Markers Score that we established here comprised of four important parameters: duration of AF, preoperative LA size, pathology of the mitral valve and the postoperative LA remodeling.
The duration of AF and the size of LA were the most independent prognostic predictors for patients underwent the Cox-maze procedure. [4–6] In spite of these two factors may influence the outcome independently, they are reciprocal causation. [8] The AF would induce atrial dysfunction, which contributed to myocardial constriction function impairment and chamber dilatation. Dilatation of the atrial wall would break the normal structure of the conducting system, trigger the macro-reentry development, making the AF more persistent and developing a vicious cycle of AF begets AF. From our previous reports and others, preoperative LA size was significantly larger in patients who experienced recurrent AF after modified Cox-maze IV procedure. [5,9–11] Some further used the LA volume index or left atrial emptying fraction to predict the outcome of the operation. [12,13]
In contrast to the previous report that pathology of mitral lesion was not a predictor of AF recurrence, [14] we found that chronic AF patients associated with rheumatic etiologies had lower sinus conversion rates when compared with other mitral pathologies. These attributes of a significant predictor may echo the hypothesis that atrial extracellular matrix alternation or atrial wall fibrosis could play a role in AF maintenance. [15,16] More studies may be necessary to determine whether the lower sinus conversion rate was really caused by this particular pathology alone or just a coincidental result of the association between larger LA size and prolonged AF duration.
Not only preoperative LA size and function are important to the prognosis of modified Cox-maze IV procedure, the postoperative LA size and remodeling may also influence the outcome. [17] Structural remodeling of the pulmonary veins and LA can be reversible after successful catheter ablation without AF recurrence; however, late recurrence of AF is associated with progressive LA dilatation. [18] The LA size decreased during follow-up in patients with sustained sinus rhythm, whereas LA size increased in cases of recurrent AF.[4] This raises the tempting possibility that reducing atrial size may help to mitigate the re-entry circuits underlying AF, thus increasing the success rate of modified Cox-maze IV procedure. However, the evidence is not strong enough to draw solid conclusions since it was not randomized and cannot be generalized, owing to substantial variations in the populations. [19]
Despite the promising results of this study, several important limitations must be recognized. First, though duration of the AF was the most important parameter in our scoring system, its duration may be under estimated. We can only count it until the patient’s presentation to the hospital. Second, some missing details of data collection should be expected in this retrospective study such as the pulmonary arterial pressure or New York Heart Association functional class during the whole time span. Third, postoperative echocardiography was not performed with a tight time frame and by a core lab examiner. Therefore, the size of LA measurement may show some variations. Finally but not last, we applied our score system to the validation group from another hospital with acceptable outcome. Without propensity matched population because of the limitation of numbers, the pre-existing differences in patients’ demographics between the two groups may compromise the outcome and jeopardize the final judgment. Cooperation with multi-centers, prospective data collection and adhering to strict echo follow-up protocol with a core lab may minimize the bias and confirm the accuracy of this scoring system.
In conclusion, patients with structural heart disease combined with permanent AF who underwent cardiac surgery and concomitant modified Cox-maze IV procedure attained a sinus rhythm recovery rate of 75.8% in this study. The Soft Markers Score, including four important parameters of duration of AF, preoperative LA size, pathology of the mitral valve and postoperative LA remodeling, demonstrated a good discriminative power to predict sinus recovery in our patients as well as the other validation populations. This scoring system provides us a treatment policy in the postoperative management. In the low risk population, the anticoagulant protocol maybe modified to decrease the bleeding hazard, especially in the patients who had coagulopathy history such as liver cirrhosis or other comorbidities. However, in the high risk population, this scoring system may remind us to stick to the guideline of anticoagulant recommendations for preventing the embolic event.
Data Availability
The data cannot be made freely available because of IRB regulations. Data are available from the Department of Cardiothoracic and Vascular surgery in Chang Gung memorial hospital Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data.
Funding Statement
This study was supported by funds from the national science council in Taiwan (NMRP 99-2314-B-182A-050-MY2 and NMRP 102-2314-B-182A-049-MY2). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Feng-Chang Tsai, an expert in statistical analysis, took part in data analysis and statistical methods verification. He received the salaries from Formosa Biomedical Technology, but this commercial company did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Cox JL, Ad N, Palazzo T. Impact of the Maze procedure on the stroke rate in patients with atrial fibrillation. J Thorac Cardiovasc Surg. 1999; 118: 833–840. [DOI] [PubMed] [Google Scholar]
- 2. Khargi K, Hutten BA, Lemke B, Deneke T. Surgical treatment of atrial fibrillation; a systematic review. Eur J Cardiothorac Surg. 2005; 27: 258–265. [DOI] [PubMed] [Google Scholar]
- 3. Basu S, Nagendran M, Maruthappu M. How effective is bipolar radiofreuqency ablation for atrial fibrillation during concomitant cardiac surgery? Interact Cardiovasc Thorac Surg. 2012; 15: 741–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gaynor SL, Schuessler RB, Bailey MS, Ishii Y, Boineau JP, Gleva MJ, et al. Surgical treatment of atrial fibrillation: Predictors of late recurrence. J Thorac Cardiovasc Surg. 2005; 129: 104–111. [DOI] [PubMed] [Google Scholar]
- 5. Beukema WP, Sie HT, Misier AR, Delnoy PP, Wellens HJ, Elvan A. Predictive factors of sustained sinus rhythm and recurrent atrial fibrillation after a radiofrequency modified Maze procedure. Eur J Cardiothorac Surg. 2008; 34: 771–775. 10.1016/j.ejcts.2008.07.026 [DOI] [PubMed] [Google Scholar]
- 6. Chaiyaroj S, Ngarmukos T, Lertsithichai P. Predictors of sinus rhythm after radiofrequency maze and mitral valve surgery. Asian Cardiovasc Thorac Surg. 2008; 16: 292–297. [DOI] [PubMed] [Google Scholar]
- 7. Damiano RJ Jr, Gaynor SL. Atrial fibrillation ablation during mitral valve surgery using the Atricure device. Operat Tech Thorac Cardiovasc Surg. 2004; 9: 24–32. [Google Scholar]
- 8. Henry WL, Morganroth J, Pearlman AS, Clark CE, Redwood DR, Itscoitz SB, et al. Relation between echocardiographically determined left atrial size and atrial fibrillation. Circulation. 1976; 53: 273–279. [DOI] [PubMed] [Google Scholar]
- 9. Chen MC, Chang JP, Chang HW. Preoperative Atrial Size Predicts the Success of Radiofrequency Maze Procedure for Permanent Atrial Fibrillation in Patients Undergoing Concomitant Valvular Surgery. CHEST. 2004; 125: 2129–2134. [DOI] [PubMed] [Google Scholar]
- 10. Sunderland N, Maruthappu M, Nagendran M. What size of left atrium significantly impairs the success of maze surgery for atrial fibrillation? Interact Cardiovasc Thorac Surg. 2011; 13: 332–8. 10.1510/icvts.2011.271999 [DOI] [PubMed] [Google Scholar]
- 11. Damiano RJ Jr, Schwartz FH, Bailey MS, Maniar HS, Munfakh NA, Moon MR, et al. The Cox maze IV procedure: predictors of late recurrence. J Thorac Cardiovasc Surg. 2011; 141: 113–21. 10.1016/j.jtcvs.2010.08.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim YH, Lee SC, Her AY, Kim HJ, Choi JO, Shin DH, et al. Preoperative left atrial volume index is a predictor of successful sinus rhythm restoration and maintenance after the maze operation. J Thorac Cardiovasc Surg. 2007; 134: 448–453. [DOI] [PubMed] [Google Scholar]
- 13. Aikawa M, Watanabe H, Shimokawa T, Inoue K, Takamisawa I, Seki A, et al. Preoperative left atrial emptying fraction is a powerful predictor of successful maze procedure. Circ J, 2009; 73: 269–273. [DOI] [PubMed] [Google Scholar]
- 14. Lee JW, Park NH, Choo SJ, Jo MS, Song H, Song MG. Surgical outcome of the maze procedure for atrial fibrillation in mitral valve disease: rheumatic versus degenerative. Ann Thorac Surg. 2003; 75: 57–61. [DOI] [PubMed] [Google Scholar]
- 15. Polyakova V, Miyagawa S, Szalay Z, Risteli J, Kostin S. Atrial extracellular matrix remodeling in patients with atrial fibrillation. J Cell Mol Med. 2008; 12: 189–208. 10.1111/j.1582-4934.2008.00219.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang X, Li Y, Liu L, Hu SS, Song YH, Wang W. The role of matrix metalloproteinase-2 in the treatment of atrial fibrillation recurrence after a radiofrequency modified maze procedure. Cardiology. 2013; 126: 62–8. 10.1159/000351980 [DOI] [PubMed] [Google Scholar]
- 17. Chen MC, Chang JP, Guo GB, Chang HW Atrial size reduction as a predictor of the success of radiofrequency maze procedure for chronic atrial fibrillation in patients undergoing concomitant valvular surgery. J Cardiovasc Electrophysiol. 2001; 12: 867–74. [DOI] [PubMed] [Google Scholar]
- 18. Tsao HM, Wu MH, Huang BH, Lee SH, Lee KT, Tai CT, et al. Morphologic remodeling of plmonary veins and left atrium after catheter abaltion of atrial fibrillation: insight from long-term follow-up of three dimensional magnetic resonance imaging. J Cardiovasc Electrophysiol. 2005; 16: 7–12. [DOI] [PubMed] [Google Scholar]
- 19. Marui A, Saji Y, Nishina T, Tadamura E, Kanao S, Shimamoto T, et al. Impact of left atrial volume reduction concomitant with atrial fibrillation surgery on left atrial geometry and mechanical function. J Thoarc Cardiovasc Surg. 2008; 135:1297–305. 10.1016/j.jtcvs.2008.02.026 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data cannot be made freely available because of IRB regulations. Data are available from the Department of Cardiothoracic and Vascular surgery in Chang Gung memorial hospital Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data.