Abstract
Conflicting data on the relationship between antihypertensive medications and falls in elderly people may lead to inappropriate under-treatment of hypertension in an effort to prevent falls. We aimed to clarify the relationships between the chronic use of different classes of antihypertensive medications and different types of falls, determine the effect of medication dose, and assess whether falls risk is associated with differences in cerebral blood flow.
We assessed demographics, clinical characteristics, and chronic antihypertensive medication use in 598 community-dwelling people with hypertension, aged 70 to 97, then followed them prospectively for self-reported falls using monthly calendar postcards and telephone interviews.
Antihypertensive medication use was not associated with an increased risk of falls. Participants reporting use of Angiotensin Converting Enzyme Inhibitors (ACEI) had a significanty decreased one-year risk of injurious falls (Odds Ratio = 0.62, 95% confidence interval = 0.39-0.96), while those using Calcium Channel Blockers had a decreased risk of all falls (OR = 0.62, 95% CI = 0.42 - 0.91) and indoor falls (OR = 0.57, 95% CI = 0.36-0.91), compared to participants not taking these drugs. Larger doses of these classes were associated with a lower falls risk. Participants taking calcium channel blockers had higher cerebral blood flow than those not taking these medications.
In relatively healthy community-dwelling elderly people, high doses of antihypertensive agents are not associated with an increased risk of falls.
Keywords: Antihypertensive agents, calcium channel blockers, ACE inhibitors, aged, blood flow velocity
INTRODUCTION
Several studies have suggested that there is an increased risk of falls in elderly people taking antihypertensive medications1, 2. A recent observational study of 4961 hypertensive community-dwelling participants in the Medicare Current Beneficiary Survey showed an increased risk of injurious falls in those who received moderately intense antihypertensive therapy compared to those on no treatment, but no particular drug class was implicated3. The acute administration of antihypertensive medications such as diuretics can produce significant hypotension in elderly people4, which may threaten cerebral perfusion and produce falls and syncope. However, this may be a short-term effect that wanes after prolonged drug administration5.
In contrast, other studies have suggested that chronic blood pressure lowering with regimens that include angiotensin system-blocking medications may preserve cerebral hemodynamics6, increase cerebral perfusion7-10, and reduce the progression of cerebral white matter hyperintensities11, which are associated with abnormal gait and falls.12, 13 Consistent with these reports, a recent prospective cohort study by Wong et al14 showed a lower risk of falls among elderly community-dwelling participants taking angiotensin converting enzyme inhibitors (ACEIs) and/or angiotensin receptor blockers (ARBs).
The conflicting data on the relationship between antihypertensive medications and falls may be due not only to the duration of use or effect on cerebral perfusion, but also a dose effect. Lower doses of certain antihypertensive medications may be protective, while higher doses may be associated with falls.3, 15 We examined one-year fall risk in a population-based cohort of hypertensive elderly people to help clarify the relationships between the chronic use of different classes of antihypertensive medications and falls. We also examined the effect of medication dose and whether antihypertensive agents are associated with an increase in cerebral blood flow.
METHODS
Study Design and Sample
We conducted a one-year prospective observational study of falls after the collection of baseline data in 598 people aged 70 to 97 with hypertension who were enrolled in the Maintenance of Balance, Independent Living, Intellect, and Zest in the Elderly Study in Boston, Massachusetts (MOBILIZE Boston Study). The study design and methods have been described previously16. At enrollment, participants met the following inclusion criteria: age ≥70 years, ability to speak and understand English, ability to walk across a room, visual ability to read written material, Mini-Mental State Examination (MMSE) score ≥18, and expected residence in the area for at least 2 years. All participants in the current study also met criteria for hypertension, which included an average baseline blood pressure over 140 systolic and/or 90 diastolic on 2 seated measures, and/or the use of antihypertensive medications. All participants underwent a complete baseline home interview and clinical laboratory assessment as previously described16, which included data on comorbidities, medications, functional and cognitive status, physical performance, blood pressure, height, and weight. All data were collected by trained research assistants.
A subset of 313 participants with accessible temporal acoustic windows underwent transcranial Doppler ultrasound measures of cerebral blood flow velocity (see below). All participants submitted completed falls study calendars monthly during the follow-up period, however 14 participants (2.3%) did not know, refused to answer, or could not be reached for additional follow-up questions on the time, location (indoor vs. outdoor), and injury status of falls events. The study was approved by the Institutional Review Board of Hebrew SeniorLife, and all participants provided written informed consent.
Medication Use
Use of antihypertensive medications was assessed at baseline during an in-person interview by asking the participant to report all medications that were taken for at least a 2-week period. Dose information was recorded from medication bottles. All drug data were coded according to the Iowa Drug Information System (IDIS) and antihypertensives were classified into the following 6 categories: alpha blockers, ACEIs, ARBs, beta blockers, diuretics, and calcium channel blockers. In addition, we grouped participants into those taking any antihypertensive medications and those on angiotensin system-blocking medications (ACE or ARBs). We also assessed the use of statins and psychotropic medications.
Daily medication dose was calculated by multiplying the prescribed strength by the number of times taken per day and the number of days taken per week, divided by seven. We then computed the median dose among all users and dichotomized the dose into standard or low (≤ median) and high (> median) levels. For example, high dose amlodipine was ≥ 7.5 mg daily, while standard or low dose was ≤ 5.0 mg. Details are provided in Supplemental Table S1. A geriatrician (LAL) and pharmacist (II) reviewed these dose categories for each antihypertensive medication to ensure face validity.
Cerebral Blood Flow
During the baseline clinic visit, heart rate (HR) was measured by a continuous electrocardiogram (ECG) and beat-to-beat arterial pressure (ABP) was measured by photoplethysmography (Finapres, Ohmeda Monitoring Systems, Englewood, CO)17. End-tidal CO2 was measured using a Vacumed CO2 Analyzer (Ventura, CA) attached to a nasal cannula. Transcranial Doppler ultrasonography (TCD) (MultiDop X4, DWLTranscranial Doppler Systems Inc., Sterling, VA) was used to measure middle cerebral artery (MCA) mean blood flow velocity (BFV) while sitting and during changes in end-tidal carbon dioxide (CO2 vasoreactivity, see below).18 The MCA signal was identified according to standard criteria19 and recorded at a depth of 50 to 60 mm. The envelope of the velocity waveform, derived from a fast-Fourier analysis of the Doppler frequency signal, was digitized at 500 Hz, displayed simultaneously with the ABP, ECG, and end-tidal CO2 signals, and stored for later off-line analysis. Previous studies, using a variety of techniques (133Xe, SPECT, MRI) and stimuli, have validated transcranial Doppler measures of relative changes in cerebral flow velocity as representative of changes in cerebral blood flow.20, 21
To assess CO2 vasoreactivity, BFV was measured continuously in the MCA while participants inspired a gas mixture of 8% CO2, 21% O2, and balance nitrogen for 2 minutes and then mildly hyperventilated to an end-tidal CO2 of approximately 25 mm Hg for 2 minutes. MCA BFV was plotted against end tidal CO2 while breathing room air, 8% CO2, or hyperventilating. Cerebral vasoreactivity was measured as the slope of this relationship and expressed as change in BFV per mm Hg change in end-tidal CO2.
Falls Assessment
A fall was defined as unintentionally coming to rest on the floor, ground, or other lower surface. Falls were ascertained by self-report using monthly falls calendar postcards and telephone interviews for participants who did not return the calendar. Any participant reporting a fall received a follow-up telephone call to collect more information about the location and circumstances of the fall. An indoor fall was defined as one that occurred inside the participant's home, inside someone else's home, inside another building, or inside another location. Outdoor falls were those reported to have occurred anywhere outside of these locations. Injurious falls were those reported to have resulted in any physical injury or required treatment in an emergency department or hospital. The primary outcome variable was one or more falls within a one year follow-up period.
Statistical Analysis
Participant characteristics and fall risk factors were summarized by means and standard deviations or percentages, and compared between fallers and nonfallers, and treated and untreated participants, using t-tests for continuous variables and chi-square tests for categorical variables. We determined the proportion of individuals reporting any fall, and one or more indoor, outdoor, and injurious falls over a one-year followup period. We also determined the prevalence of the use of six classes of antihypertensive medications, including alpha blockers, ACEIs, ARBs, beta blockers, diuretics, and calcium channel blockers. Since only 4 participants were taking vasodilating beta-blockers we were not able to examine this subclass.
Multivariate logistic regression was used to assess the association between antihypertensive medication use and each category of falls, adjusting for relevant covariates and factors found in bivariate analyses to be significantly associated with falls. Covariates included baseline blood pressure, a sum of comorbidities22, education, race, body mass index (BMI), psychotropic medication use (sedatives, hypnotics, antidepressants, and antipsychotics), and time spent engaging in outdoor activities according to the Physical Activity Scale for the Elderly (PASE)23. In post-hoc analyses we also stratified our sample by participants with and without falls in the year prior to the baseline assessment and examined the relationship between antihypertensive medications and subsequent falls in each group.
In subgroup analyses, we studied the effects of each of the six classes of antihypertensive medication on four different outcome variables: total falls, outdoor falls, indoor falls, and injurious falls. For outdoor and indoor falls, we also adjusted the analyses for estimates of time spent engaging in outdoor and indoor activities using self-reported data from the PASE instrument.
Finally, we examined the relationship between the dose of each antihypertensive medication (high dose, low or standard dose, and none), grouped by medication class, and each of the falls outcomes using similar multivariate logistic regression models, adjusted for the same covariates as in the two-group models. We used ANOVA-based F statistics for omnibus tests of differences in risk between dose groups, followed by Tukey post-hoc tests for comparisons among groups.
Finally, in order to explore the degree to which cerebral blood flow could account for associations between antihypertensive medications and falls, we compared odds ratios generated in the presence and absence of measures of cerebral blood flow. These analyses were restricted to the subsample of participants with transcranial Doppler ultrasound measures and complete data (N=301). The percent change in the odds ratio relating a given medication to falls when cerebral blood flow was added to the model was used to quantify a possible mediating effect.
Data were analyzed using SAS software version 9.3 (SAS Institute, Cary, NC, USA). Means are presented with their standard deviation in parentheses. Differences were considered statistically significant at P < .05 (2 tailed).
RESULTS
Participant Characteristics
The mean age of the 598 hypertensive participants was 78.4 (5.4) years; 372 (62.2%) were female, 449 (75.1%) were white, and 259 (43.4%) had a bachelor's degree or higher. Two hundred sixty-two participants (89.5%) were regularly taking antihypertensive medications at the start of the study. The proportion of participants reporting use of antihypertensive medication subclasses were ARBs (12.8%), ACEIs (34.7%), alpha-blockers (7.1%), beta-blockers (51.9%), calcium channel blockers (29.3%), and diuretics (47.0%).
Among the 598 participants, 541 falls were recorded during the one-year followup; 331 (55.3%) participants reported no falls, and 267 (44.7%) reported one or more falls. Eighty-two (13.7%) participants reported falling outdoors, 127 (21.2%) reported falling indoors, 44 (7.4%) reported falling both indoors and outdoors, and 164 (27.4%) reported falls resulting in injury. Fourteen (2.3%) participants reported falling but were unavailable for follow-up questioning on details of the fall event. The total number of falls per person during the follow-up period ranged from 0 to 17.
Table 1 presents the demographic and clinical characteristics of hypertensive participants who did and did not fall during the one-year follow-up period. Fallers reported higher levels of education, greater use of psychotropic medications, more depressive symptoms, and a higher rate of previous falls. They were more likely to be white, less likely to be cognitively impaired, and had slightly lower systolic blood pressures compared to non-fallers. Although fallers had a slightly lower prevalence of diabetes, their total number of comorbidities, including congestive heart failure, was higher.
Table 1.
Baseline Characteristics of MOBILIZE Boston Participants with Hypertension According to Falls Status (N = 598)
| Risk Factor | Fallers (n = 267) | Non-fallers (n = 331) | P-value |
|---|---|---|---|
| Sociodemographic & Health Status | |||
| Age, mean ± SD | 78.5 ± 5.6 | 78.3 ± 5.3 | 0.70 |
| Female, n (%) | 166 (62.2) | 206 (62.2) | 0.73 |
| White, n (%) | 216 (80.9) | 233 (70.4) | <0.001 |
| Body mass index, kg/m2, mean ± SD | 27.6 ± 5.1 | 27.8 ± 5.2 | 0.65 |
| Education, n (%) | <0.001 | ||
| < high school, | 26 (9.7) | 59 (17.9) | |
| High school/ vocational | 104 (39.0) | 149 (45.2) | |
| ≥ 4 y College | 137 (51.3) | 122 (37.0) | |
| Medical conditions | |||
| N (%) | |||
| Stroke, | 31 (11.6) | 38 (11.6) | 0.99 |
| Diabetes mellitus | 49 (18.6) | 79 (24.2) | 0.10 |
| Hyperlipidemia, | 155 (62.0) | 207 (63.7) | 0.68 |
| Congestive heart failure | 20 (7.6) | 17 (5.2) | 0.24 |
| Comorbidity count, mean ± SD | 3.4 ± 1.6 | 3.2 ± 1.5 | <0.002 |
| Participants with falls in past year, N (%) | 137 (51) | 79 (24%) | <0.01 |
| Medication use, n (%) | |||
| Antihypertensive medication | 238 (89.5) | 297 (90.6) | 0.66 |
| Alpha-blocker | 18 (6.8) | 24 (7.3) | 0.79 |
| Angiotensin system-blocking medication | 118 (44.4) | 157 (47.9) | 0.39 |
| Angiotensin-receptor blocker | 37 (13.9) | 39 (11.9) | 0.46 |
| Angiotensin-converting enzyme inhibitor | 83 (31.2) | 123 (37.5) | 0.11 |
| Beta-blocker | 142 (53.4) | 166 (50.6) | 0.50 |
| Calcium Channel Blockers | 62 (23.3) | 112 (34.2) | 0.004 |
| Any diuretic | 114 (42.9) | 165 (50.3) | 0.07 |
| Statin | 129 (48.5) | 184 (56.1) | 0.07 |
| Psychotropic medication | 26 (9.8) | 17 (5.2) | 0.03 |
| Cognitive function | |||
| Mini-Mental State Examination score, mean ± SD | 27.0 ± 2.8 | 26.7 ± 2.7 | <0.004 |
| CES-D score, mean ± SD | 13.1 ± 11.2 | 9.6 ± 10.6 | <0.001 |
| Trail Making Test Part B, mean ± SD | 86.2 ± 62.8 | 100.4 ± 67.7 | <0.001 |
| Hemodynamics | |||
| Supine systolic blood pressure, mean ± SD | 130.8 ± 18.2 | 134.1 ± 19.8 | 0.02 |
| Orthostatic Hypotension*, n (%) | |||
| Orthostatic Systolic BP change, Supine to standing at 1 min. | 32 (12.0) | 43 (13.0) | 0.71 |
| −1.8 ± 13.5 | −3.0 ± 13.0 | 0.21 | |
| Orthostatic Diastolic BP change, Supine to standing at 1 min. | 2.3 ± 7.4 | −1.8 ± 6.4 | 0.52 |
Orthostatic Hypotension was defined as ≥20 mmHg decline in Systolic BP and/or ≥ 10 mm Hg decline in diastolic BP going from supine to standing at 1 minute.
Table 2 shows the cerebral hemodynamic characteristics of participants who underwent the transcranial Doppler assessment. Fallers had significantly lower cerebral blood flow velocity and CO2 vasoreactivity than non-fallers.
Table 2.
Hemodynamic Characteristics of Participants who Underwent Transcranial Doppler Assessment (N = 313)
| Risk Factor | Fallers (n = 146) | Non-fallers (n = 167) | P-value |
|---|---|---|---|
| Hemodynamics | |||
| Cerebral blood flow, cm/s, mean ± SD | 39.0 ± 9.2 | 42.3 ± 11.5 | 0.02 |
| CO2 vasoreactivity, cm/sec/mmHg, mean ± SD | 1.17 ± 0.39 | 1.27 ± 0.46 | 0.04 |
We also compared characteristics of participants taking antihypertensive medications to those not taking these medications (See Supplemental Tables S2 and S3). The group taking antihypertensive medications had significantly lower blood pressures, more comorbidities, a higher prevalence of diabetes, and a lower prevalence of orthostatic hypotension, but no difference in previous fall rates.
Relationship between Antihypertensive Use and Falls
As shown in Table 1, nonfallers were more likely to be taking calcium channel blockers than fallers. There were no differences in the use of other antihypertensive medications between fallers and nonfallers. Multivariate logistic regression analyses revealed that the association between overall antihypertensive medication use and all falls was not statistically significant after adjusting for significant covariates (OR=0.76, 95% CI = 0.42–1.35). Table 3 shows the results of adjusted multivariate logistic regression analyses for the relationships between antihypertensive medication classes and different types of falls over a 1 year followup period. No single class of antihypertensive medication was associated with an increased risk of falls. In fact, calcium channel blocker use was associated with a reduced risk of all falls (OR=0.62, 95% CI = 0.42 - 0.91) and indoor falls (OR=0.57, 95% CI = 0.36 - 0.91), and ACEI use was associated with a reduced risk of injurious falls (OR=0.62, 95% CI=0.39 - 0.96). When the participants were stratified according to a past history of falls, those with previous falls also had a lower risk of all, outdoor, and injurious falls during the one year follow-up period if they were taking calcium channel blockers or ACEIs (see Supplemental Table S4).
Table 3.
Adjusted Multivariate Logistic Regression Analyses for the Relationship Between Antihypertensive Medication Classes and Falls Over 1 Year
| CVD med category | All Falls OR (95% CI) | Outdoor Falls OR (95% CI) | Indoor Falls OR (95% CI) | Injurious Falls OR (95% CI) |
|---|---|---|---|---|
| Alpha-blockers | 0.99 (0.51, 1.92) | 1.10 (0.47, 2.55) | 1.21 (0.58, 2.50) | 0.61 (0.24, 1.54) |
| Angiotensin-receptor blockers | 1.12 (0.66, 1.91) | 1.35 (0.71, 2.58) | 0.64 (0.32, 1.29) | 1.01 (0.54, 1.87) |
| Angiotensin-converting enzyme inhibitors | 0.76 (0.53, 1.11) | 0.64 (0.39, 1.04) | 0.80 (0.52, 1.22) | 0.62 (0.39, 0.96)† |
| Beta-blockers | 1.09 (0.77, 1.54) | 0.84 (0.54, 1.31) | 1.07 (0.72, 1.61) | 0.93 (0.62, 1.39) |
| Diuretics | 0.80 (0.56, 1.13) | 0.74 (0.47, 1.16) | 0.90 (0.60, 1.35) | 0.84 (0.56, 1.27) |
| Calcium channel blockers | 0.62 (0.42, 0.91)† | 0.68 (0.41, 1.14) | 0.57 (0.36, 0.91)† | 0.74 (0.47, 1.17) |
Data shown are Odds Ratios (OR) and 95% confidence intervals (CI).
* Adjusted for blood pressure measured at baseline, comorbidity count, education, race, body mass index, psychotropic medication use, and time spent engaging in outdoor activities.
P < 0.05
Effect of Medication Dose
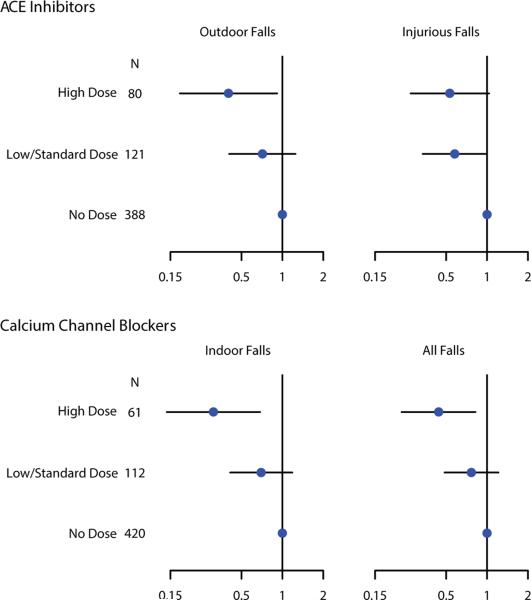
As shown in Figure 1, higher doses of calcium channel blockers were associated with a lower risk of all falls (OR = 0.44, 95% CI = 0.24 - 0.82, P=0.03) and indoor falls (OR = 0.31 , 95% CI = 0.14 – 0.69, P=0.01) compared to those not taking calcium channel blocking medications. Higher doses of ACEIs were associated with a significantly lower risk of outdoor falls (OR = 0.40, 95% CI = 0.18 – 0.92, P=0.04) and all doses were associated with marginally significant reductions in injurious falls (OR = 0.58, 95% CI = 0.34 – 0.99, P= 0.05 for low or standard doses, and OR= 0.53, 95% CI = 0.27 – 1.04, P = 0.07 for high doses) compared to those not taking ACEIs.
Figure 1.
Estimated odds ratios (dots) and corresponding 95% confidence intervals (lines) for different types of falls during one-year of followup, according to dose of drug class. N is the size of the sample taking each dose of drug. The odds of falls in participants taking low or standard doses (at or below the median) and participants taking high doses (above the median) are shown in reference to participants taking no medications (no dose) in a given drug class. Odds Ratios are displayed on each horizontal axis.
The Effect of Medications on Cerebral Blood Flow
Among the 6 classes of antihypertensive medications examined, only calcium channel blocker use was associated with a statistically significant increase in cerebral blood flow velocity. Participants taking calcium channel blockers had a baseline cerebral blood flow velocity of 43.3 ± 12.5 cm/s compared to 40.0 ± 9.8 cm/s in those not taking these medications (P=0.02). There was also a modest dose effect of calcium channel blockers on cerebral blood flow velocity. Blood flow velocity in participants taking no calcium blocking medications was 40.0 ± 9.8 cm/s, those taking standard/low doses was 43.7 ± 13.5 cm/s, and those taking high doses was 42.3 ± 10.0 cm/s (P = 0.03). Post-hoc pairwise comparisons showed that the standard/low dose group had significantly higher cerebral blood flow values than the no calcium blocker group (P = 0.01) and the remaining pairwise comparisons failed to meet statistical significance.
There was a non-significant trend toward increased cerebral blood flow velocity in those taking ACEIs (42.0 ± 9.9 cm/sec) compared to those not taking these drugs (40.1 ± 11.0 cm/sec, P=0.14). There was a monotonic trend toward higher doses of ACEIs being associated with higher average cerebral blood flow values, but this relationship also failed to meet statistical significance (none 40.1 ± 11.0 cm/s, standard/low 41.8 ± 9.0 cm/s, high 42.5 ± 11.2 cm/s, P = 0.15).
None of the antihypertensive medications was associated with CO2 vasoreactivity.
Relationship Between Cerebral Blood Flow and Falls
Increased cerebral blood flow velocity was also associated with a reduced risk of all falls (Odds Ratio (OR) per 10 cm/sec increase in blood flow velocity = 0.75, 95% CI = 0.59 - 0.94, P = 0.01), indoor falls (OR per 10 cm/sec increase in blood flow velocity = 0.76, 95% CI = 0.57 – 1.00, P = 0.05), and injurious falls (OR per 10 cm/sec increase in blood flow velocity = 0.74, 95% CI = 0.56 – 0.98, P=0.04). When cerebral blood flow velocity was added to the regression model relating calcium channel blockers to falls, the relationship between calcium channel blockers and total and indoor falls was attenuated by 19% and 29%, respectively (See Table 4).
Table 4.
Adjusted Mediation Models - The Mediating Effect of Cerebral Blood Flow on the Relation between Calcium Channel Blocker Use and Risk of Falls
| Model Key Outcome Exposure | Drug Effect on Falls* OR (95%CI) | Drug Effect on Falls After Adjustment for Cerebral Blood Flow* OR (95%CI) | Percent Drug Effect on Falls Influenced by Cerebral Blood Flow | Direction of the Influence of Cerebral Blood Flow on Drug Effect on Falls |
|---|---|---|---|---|
| All Falls | ||||
| Calcium channel blocker | 0.59 (0.41, 0.84) | 0.70 (0.41, 1.20) | 19% | Attenuation of effect (-) |
| Indoor Falls | ||||
| Calcium channel blocker | 0.56 (0.36, 0.85) | 0.72 (0.38, 1.35) | 29% | Attenuation of effect (-) |
Data shown are Odds ratios (OR) and 95% confidence intervals (CI).
Adjusted for blood pressure measured at baseline, comorbidity count, education, race, body mass index, psychotropic medication use, and time spent engaging in outdoor activities.
DISCUSSION
The results of this study suggest that the chronic use of antihypertensive medications by community-dwelling elderly people with hypertension may not be as strong a risk factor for falls as previously thought. Neither standard nor high doses of antihypertensive agents were associated with falls. Moreover, ACEIs were associated with a reduced risk of injurious falls and Calcium Channel Blockers were associated with a reduced risk of all falls and indoor falls.
Our findings are supported by the previous studies of Wong et al, which also showed a lower risk of falls among community-dwelling older adults taking renin angiotensin system blocking medications14, and Callisaya et. al., who showed a minimal effect of antihypertensive drugs on falls in therapeutic doses24. In the latter study only a very high dose of these medications, over 3 times the daily defined dose, was significantly associated with falls. Although our participants were not on doses this high, we found that elderly people taking relatively large doses of calcium channel blockers and ACEIs had a lower risk of falls compared to those not taking these medications.
Our results differ from those of Tinetti et al3, who found a statistically significant increased risk of serious fall injuries only with moderately intense doses of antihypertensive medications in the Medicare Current Beneficiary Survey population, and an increased risk with high intensity doses in participants with a previous history of falls. It is hard to know how the doses used in the Tinetti study compare to ours. Furthermore, our population was slightly younger (78 vs 80 years), healthier (less stroke, diabetes, and heart failure), and better educated (82-90% completed more than a high school education compared to 30-34%). When we stratified our participants according to those with and without previous falls, even the higher risk participants with previous falls had a lower risk of subsequent falls if they were taking calcium channel blockers or ACEIs. In the Tinetti study no particular class of antihypertensive medication was associated with injurious falls.
One potential mechanism by which the calcium channel blockers could participate in the prevention of falls is through an increase in cerebral blood flow and prevention of ischemic brain injury. Our analysis showing attenuation of the association between calcium channel blockers and falls when controlled for cerebral blood flow is consistent with this mechanism, but does not imply causality and requires validation in future clinical trials. This line of reasoning may seem counterintuitive, since antihypertensives are thought to decrease cerebral perfusion by reducing blood pressure. It is supported, however, by a small body of evidence showing that the long-term control of high blood pressure may improve systemic and cerebral hemodynamics7, 8, 10. We have previously shown that the use of the calcium channel blocker Nicardipine in elderly hypertensive people with a history of coronary artery disease can reduce postprandial hypotension25. The chronic use of several antihypertensive medications has also been shown to reduce orthostatic hypotension26. Nimodipine has been demonstrated to improve regional cerebral blood flow in rats6 and cerebral oxygenation and blood volume in healthy humans27. Other studies have shown that the ARB, Telmisartan, can increase regional cerebral blood flow in hypertensive patients with chronic-stage stroke28 or Alzheimer's Disease29, and Candesartan can increase cerebral blood flow in healthy hypertensive participants with low baseline cerebral blood flow7. We previously showed increases in cerebral blood flow in hypertensive participants whose blood pressure was controlled with a lisinopril-based regimen for 6 months8. Our current results with ACEIs are limited by relatively small sample sizes, but they suggest that this class of medication may be associated with a lower incidence of injurious falls due to other mechanisms.
One unique aspect of this study is that it examined different types of falls that may have different pathophysiologic mechanisms. For example, indoor falls are more likely to occur in frail individuals with multiple chronic conditions, while outdoor falls tend to occur in healthier, more ambulatory individuals with greater exposures to environmental hazards30. Calcium channel blockers were associated with fewer indoors and all types of falls, while ACEIs were associated with fewer injurious falls. The reasons for these differences are not known, but it is possible that the ACEIs improved skeletal muscle function31, thereby enabling people taking them to better protect themselves during a fall through compensatory motor responses.
There are several limitations to our study. Unfortunately, we could not conduct a randomized trial comparing different classes of antihypertensive agents on rates of falls. We did not have information on adherence or changes in medications during the follow-up period, which precluded us from determining whether the risk of falling was affected by changes in the frequency or dose of medications. In addition, the number of participants taking some classes of medications (e.g., alpha-blockers and ARBs) was relatively small, limiting our power to detect statistically significant effects on falls. We considered the possibility that participants taking antihypertensive medications were healthier, and therefore less likely to fall. However, those taking these medications had more comorbidities and diabetes, which would have biased the results toward more falls in this group.
Not all of our participants had an adequate temporal acoustic window for transcranial Doppler measurements of cerebral blood flow velocity. Previous studies using the MOBILIZE Boston Study cohort have shown that elderly participants with suitable bone windows tend to be healthier than those without32. It is possible that antihypertensive medications have different effects on cerebral hemodynamics in people with and without transcranial Doppler windows. Unfortunately, our cerebral blood flow measurements were limited to only the middle cerebral artery territory of the brain. However, this territory includes the prefrontal motor cortex that largely controls mobility. Unfortunately, we were unable to assess cerebral blood flow at the time of a fall. Despite these limitations, this study has the unique advantages of using a population-based sample, rigorous longitudinal falls followup, novel subcategories of falls, and well-established non-invasive measures of cerebral hemodynamics.
PERSPECTIVES
Given the known benefits of treating hypertension in elderly people33, the withholding of antihypertensive medications to prevent falls may not be a justifiable medical practice. Although the acute administration of any hypotensive medication can precipitate a fall or syncope, the careful up-titration and long-term administration of the lowest effective doses of these medications does not appear to increase falls risk.
Supplementary Material
Novelty and Significance:
What is new? This paper provides new information on the possible roles of medication class, dose, and cerebral blood flow on the relationship between antihypertensive medications and different types of falls in elderly people.
What is relevant? Both the treatment of hypertension and prevention of falls are important health promotion goals, yet they may be in conflict if antihypertensive medications increase the risk of falls, as some previous studies suggest.
Summary:
In community-dwelling elderly people standard and high doses of antihypertensive medications are not associated with an increased risk of falls.
Treatment with calcium channel blockers or ACEIs are associated with a lower risk of falls.
Acknowledgments
SOURCES OF FUNDING
This study was supported by grants P01 AG04390, P30 AG031679, R37 AG25037, and R01 AG041785 from the National Institute on Aging, and R01 NS085002 from the National Institute of Neurological Disorders and Stroke, Bethesda, MD. Drs. Tchalla, Dantoine, and Lipsitz were supported in part by the Limoges University Foundation, University Hospital Center of Limoges (CHU de Limoges), and Regional Council of Limousin, France. Dr. Lipsitz holds the Irving and Edyth S. Usen and Family Chair in Geriatric Medicine at Hebrew SeniorLife.
Footnotes
Financial Conflicts of Authors: None.
REFERENCES
- 1.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47:30–39. doi: 10.1111/j.1532-5415.1999.tb01898.x. [DOI] [PubMed] [Google Scholar]
- 2.Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, Marra CA. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, Zhou B, Lin H. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–595. doi: 10.1001/jamainternmed.2013.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shannon RP, Wei JY, Rosa RM, Epstein FH, Rowe JW. The effect of age and sodium depletion on cardiovascular response to orthostasis. Hypertension. 1986;8:438–443. doi: 10.1161/01.hyp.8.5.438. [DOI] [PubMed] [Google Scholar]
- 5.Gribbin J, Hubbard R, Gladman JR, Smith C, Lewis S. Risk of falls associated with antihypertensive medication: population-based case-control study. Age Ageing. 2010;39:592–597. doi: 10.1093/ageing/afq092. [DOI] [PubMed] [Google Scholar]
- 6.Zhang R, Witkowski S, Fu Q, Claassen JA, Levine BD. Cerebral hemodynamics after short- and long-term reduction in blood pressure in mild and moderate hypertension. Hypertension. 2007;49:1149–1155. doi: 10.1161/HYPERTENSIONAHA.106.084939. [DOI] [PubMed] [Google Scholar]
- 7.Hajjar I, Hart M, Chen YL, Mack W, Novak V, C Chui H, Lipsitz L. Antihypertensive therapy and cerebral hemodynamics in executive mild cognitive impairment: results of a pilot randomized clinical trial. J Am Geriatr Soc. 2013;61:194–201. doi: 10.1111/jgs.12100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipsitz LA, Gagnon M, Vyas M, Iloputaife I, Kiely DK, Sorond F, Serrador J, Cheng DM, Babikian V, Cupples LA. Antihypertensive therapy increases cerebral blood flow and carotid distensibility in hypertensive elderly subjects. Hypertension. 2005;45:216–221. doi: 10.1161/01.HYP.0000153094.09615.11. [DOI] [PubMed] [Google Scholar]
- 9.Muller M, van der Graaf Y, Visseren FL, Mali WP, Geerlings MI. Hypertension and longitudinal changes in cerebral blood flow: the SMART-MR study. Ann Neurol. 2012;71:825–833. doi: 10.1002/ana.23554. [DOI] [PubMed] [Google Scholar]
- 10.Tryambake D, He J, Firbank MJ, O'Brien JT, Blamire AM, Ford GA. Intensive blood pressure lowering increases cerebral blood flow in older subjects with hypertension. Hypertension. 2013;61:1309–1315. doi: 10.1161/HYPERTENSIONAHA.112.200972. [DOI] [PubMed] [Google Scholar]
- 11.Verhaaren BF, Vernooij MW, de Boer R, Hofman A, Niessen WJ, van der Lugt A, Ikram MA. High blood pressure and cerebral white matter lesion progression in the general population. Hypertension. 2013;61:1354–1359. doi: 10.1161/HYPERTENSIONAHA.111.00430. [DOI] [PubMed] [Google Scholar]
- 12.Srikanth V, Beare R, Blizzard L, Phan T, Stapleton J, Chen J, Callisaya M, Martin K, Reutens D. Cerebral white matter lesions, gait, and the risk of incident falls: a prospective population-based study. Stroke. 2009;40:175–180. doi: 10.1161/STROKEAHA.108.524355. [DOI] [PubMed] [Google Scholar]
- 13.Zheng JJ, Delbaere K, Close JC, Sachdev PS, Lord SR. Impact of white matter lesions on physical functioning and fall risk in older people: a systematic review. Stroke. 2011;42:2086–2090. doi: 10.1161/STROKEAHA.110.610360. [DOI] [PubMed] [Google Scholar]
- 14.Wong AK, Lord SR, Sturnieks DL, Delbaere K, Trollor JN, Close JC. Angiotensin system-blocking medications are associated with fewer falls over 12 months in community-dwelling older people. J Am Geriatr Soc. 2013;61:776–781. doi: 10.1111/jgs.12205. [DOI] [PubMed] [Google Scholar]
- 15.Callisaya ML, Sharman JE, Close J, Lord SR, Srikanth VK. Greater daily defined dose of antihypertensive medication increases the risk of falls in older people--a population-based study. J Am Geriatr Soc. 2014;62:1527–3153. doi: 10.1111/jgs.12925. [DOI] [PubMed] [Google Scholar]
- 16.Leveille SG, Kiel DP, Jones RN, Roman A, Hannan MT, Sorond FA, Kang HG, Samelson EJ, Gagnon M, Freeman M, Lipsitz LA. The MOBILIZE Boston Study: design and methods of a prospective cohort study of novel risk factors for falls in an older population. BMC Geriatr. 2008;8:16. doi: 10.1186/1471-2318-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorond FA, Khavari R, Serrador JM, Lipsitz LA. Regional cerebral autoregulation during orthostatic stress: age-related differences. J Gerontol A Biol Sci Med Sci. 2005;60:1484–1487. doi: 10.1093/gerona/60.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sorond FA, Serrador JM, Jones RN, Shaffer ML, Lipsitz LA. The sit-to-stand technique for the measurement of dynamic cerebral autoregulation. Ultrasound Med Biol. 2009;35:21–29. doi: 10.1016/j.ultrasmedbio.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982;57:769–774. doi: 10.3171/jns.1982.57.6.0769. [DOI] [PubMed] [Google Scholar]
- 20.Serrador JM, Picot PA, Rutt BK, Shoemaker JK, Bondar RL. MRI measures of middle cerebral artery diameter in conscious humans during simulated orthostasis. Stroke. 2000;31:1672–1678. doi: 10.1161/01.str.31.7.1672. [DOI] [PubMed] [Google Scholar]
- 21.Vorstrup S, Zbornikova V, Sjoholm H, Skoglund L, Ryding E. CBF and transcranial Doppler sonography during vasodilatory stress tests in patients with common carotid artery occlusion. Neurol Res. 1992;14:31–38. doi: 10.1080/01616412.1992.11740007. [DOI] [PubMed] [Google Scholar]
- 22.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 23.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 24.Callisaya ML, Sharman JE, Close J, Lord SR, Srikanth VK. Greater daily defined dose of antihypertensive medication increases the risk of falls in older people-a population-based study. J Am Geriatr Soc. 2014;62:1527–1533. doi: 10.1111/jgs.12925. [DOI] [PubMed] [Google Scholar]
- 25.Connelly CM, Waksmonski C, Gagnon MM, Lipsitz LA. Effects of isosorbide dinitrate and nicardipine hydrochloride on postprandial blood pressure in elderly patients with stable angina pectoris or healed myocardial infarction. Am J Cardiol. 1995;75:291–293. doi: 10.1016/0002-9149(95)80041-p. [DOI] [PubMed] [Google Scholar]
- 26.Masuo K, Mikami H, Ogihara T, Tuck ML. Changes in frequency of orthostatic hypotension in elderly hypertensive patients under medications. Am J Hypertens. 1996;9:263–268. doi: 10.1016/0895-7061(95)00348-7. [DOI] [PubMed] [Google Scholar]
- 27.Canova D, Roatta S, Micieli G, Bosone D. Cerebral oxygenation and haemodynamic effects induced by nimodipine in healthy subjects. Funct Neurol. 2012;27:169–176. [PMC free article] [PubMed] [Google Scholar]
- 28.Deguchi I, Furuya D, Fukuoka T, Tanahashi N. Effects of telmisartan on the cerebral circulation of hypertensive patients with chronic-stage stroke. Hypertens Res. 2012;35:1171–1175. doi: 10.1038/hr.2012.105. [DOI] [PubMed] [Google Scholar]
- 29.Kume K, Hanyu H, Sakurai H, Takada Y, Onuma T, Iwamoto T. Effects of telmisartan on cognition and regional cerebral blood flow in hypertensive patients with Alzheimer's disease. Geriatr Gerontol Int. 2012;12:207–214. doi: 10.1111/j.1447-0594.2011.00746.x. [DOI] [PubMed] [Google Scholar]
- 30.Kelsey JL, Procter-Gray E, Berry SD, Hannan MT, Kiel DP, Lipsitz LA, Li W. Reevaluating the implications of recurrent falls in older adults: location changes the inference. J Am Geriatr Soc. 2012;60:517–524. doi: 10.1111/j.1532-5415.2011.03834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Onder G, Vedova CD, Pahor M. Effects of ACE inhibitors on skeletal muscle. Curr Pharm Des. 2006;12:2057–2064. doi: 10.2174/138161206777442137. [DOI] [PubMed] [Google Scholar]
- 32.Sorond FA, Galica A, Serrador JM, Kiely DK, Iloputaife I, Cupples LA, Lipsitz LA. Cerebrovascular hemodynamics, gait, and falls in an elderly population: MOBILIZE Boston Study. Neurology. 2010;74:1627–1633. doi: 10.1212/WNL.0b013e3181df0982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.