Abstract
Objective
Lack of longitudinal patient outcome data is an important barrier in emergency medical services (EMS) research. We aimed to demonstrate the feasibility of linking prehospital data from the California EMS Information Systems (CEMSIS) database to outcomes data from the California Office of Statewide Health Planning and Development (OSHPD) database for patients with out-of-hospital cardiac arrest (OHCA).
Methods
We included patients age 18 years or older who sustained non-traumatic OHCA and were included in the 2010–2011 CEMSIS databases. The CEMSIS database is a unified EMS data collection system for California. The OSHPD database is a comprehensive data collection system for patient-level inpatient and emergency department encounters in California. OHCA patients were identified in the CEMSIS database using cardiac rhythm, procedures, medications, and provider impression. Probabilistic linkage blocks were created using in hospital death or one of the following primary or secondary diagnoses (I CD-9-CM) in the OSHPD databases: cardiac arrest (427.5), sudden death (798), ventricular tachycardia (427.1), ventricular fibrillation (427.4), and acute myocardial infarction (410.xx). Blocking variables included incident date, gender, date of birth, age, and/or destination facility. Due to the volume of cases, match thresholds were established based on clerical record review for each block individually. Match variables included incident date, destination facility, date of birth, sex, race, and ethnicity.
Results
Of the 14,603 cases of OHCA we identified in the prehospital databases, 91 (0.6%) duplicate records were excluded. Overall, 46% of the data used in the linkage algorithm were missing in CEMSIS. We linked 4,961/14,512 (34.2%) records. Linkage rates varied significantly by local EMS agency, ranging from 1.4% to 61.1% (OR for linkage 0.009–0.76; p<0.0001). After excluding the local EMS agency with the outlying low linkage rate, we linked 4,934/12,596 (39.2%) records.
Conclusion
Probabilistic linkage of CEMSIS prehospital data with OSHPD outcomes data was severely limited by the completeness of the EMS data. States and EMS agencies should aim to overcome data limitations so that more effective linkages are possible.
Keywords: Medical record linkage, Cardiac arrest, Emergency medical services
Introduction
Out-of-hospital cardiac arrest (OHCA) occurs at a rate of approximately 52 cases per 100,000 population and carries a very high mortality rate.1 Emergency Medical Services (EMS) treatment for OHCA significantly affects survival,2, 3 and OHCA has been recognized as a priority condition for EMS research.4 However, relevant patient outcomes in OHCA, such as neurologically intact survival, can often not be measured at the time of the EMS encounter. The EMS Outcomes Project identified this lack of patient outcomes data as a significant barrier to EMS research and advocated the linkage of prehospital records to hospital, clinic, and autopsy records.5
Probabilistic linkage is a technique used to match records in different datasets when unique identifiers are not available. In the United States, EMS data have been successfully linked to outcomes data using deterministic and probabilistic techniques in other disease conditions6–8 including trauma,9, 10 ST segment elevation myocardial infarction (STEMI),11 and stroke.12 Linking EMS records involving OHCA poses additional challenges due to the nature of this condition, and linkage of OHCA records to long-term outcome data is poorly studied.13
The goal of this study is to determine the feasibility of linking prehospital data from the statewide California EMS Information Systems (CEMSIS) database with outcomes data from the California Office of Statewide Health Planning and Development (OSHPD) Emergency Department Data (EDD) and Patient Discharge Data (PDD) databases for patients with OHCA in California.
Methods
Study design
We conducted a retrospective cohort study involving adult non-traumatic OHCA patients in the CEMSIS database from 1/1/2010 to 12/31/2011. This study was exempt from review by our Institutional Review Board and was approved by the California Committee for the Protection of Human Subjects.
Population and Setting
CEMSIS database
The CEMSIS database is intended to be a comprehensive and unified EMS data collection system for California. CEMSIS is an outgrowth of the National Highway Traffic Safety Administration’s National EMS Information System (NEMSIS). The project was funded and developed specifically to correspond with the national database for collecting patient data to assist efforts in injury prevention, but it offers a larger picture of EMS as all EMS responses are included in the database. The goal of CEMSIS is to use compiled EMS data to create a timely, accurate and uniform overview of EMS use and outcomes to assist in policy development, system evaluation, prevention activities, and quality improvement measures. Thirteen local EMS agencies representing 33% of the California population submitted data for 2010–2011, one local EMS agency representing 26% of the population submitted data in 2010 only, and one local EMS agency representing 2% of the population submitted data in 2011 only.
OSHPD database
The OSHPD database is a comprehensive data collection system for patient-level inpatient and emergency department encounters in California. An encounter record is submitted each time a patient is discharged following inpatient admission in a licensed hospital and each time a patient is treated in a licensed emergency department in California. These facilities are required by law (California Health and Safety Code Section 128736) to report their encounter data to OSHPD via the online Medical Information Reporting for California System. These data do not represent a sample, but rather surveillance with 100% coverage. Veterans Affairs hospitals and other military facilities are exempt.
Study Protocol
Cases of OHCA were identified in CEMSIS if they met at least one of the following criteria:
Presence of cardiac arrest at any time during the EMS event
Cardiac arrest etiology of presumed cardiac, respiratory, or “other” etiology
Cardiac arrest resuscitation attempted included: defibrillation, ventilation, chest compressions, or not attempted due to signs of circulation
Any documented cardiac arrest rhythm
Return of spontaneous circulation documented
-
EMS provider impression of non-traumatic cardiac arrest or respiratory arrest
We included patients with cardiac arrest documented by EMS but no EMS resuscitation attempted. These cases may have received bystander CPR or defibrillation prior to EMS arrival that resulted in return of circulation.
Aid prior to EMS arrival included cardiopulmonary resuscitation, defibrillation, precordial thump, or vagal maneuvers
Procedures performed by EMS included cardiopulmonary resuscitation, defibrillation, or precordial thump
-
Medications administered by EMS included epinephrine AND amiodarone, lidocaine, or atropine
Receipt of epinephrine alone was not used as an inclusion criterion to prevent the inclusion of patients with anaphylaxis without OHCA. Patients who received epinephrine alone were not strictly excluded; they were included if they met one of the other inclusion criteria.
CEMSIS cases with an etiology of trauma, drowning, and electrocution were excluded. Cases with an EMS provider primary or secondary impression of “obviously dead” were excluded. Cases with missing incident date were also excluded. Destination hospital was a free text field in the CEMSIS database, and hospital names were standardized manually prior to linkage.
Potential cases of OHCA were identified in OHSPD if they died in the hospital or had at least one of the following primary and/or secondary ICD-9-CM diagnosis codes:
(410) Acute myocardial infarction
(411) Other acute/subacute ischemic heart disease
(427) Cardiac dysrhythmias (includes 427.5 Cardiac Arrest)
(428) Heart failure
(429) Ill-defined descriptions and complications of heart disease
(458) Hypotension
(785.5) Shock, unspec.
(786.03) Apnea
(798) Sudden death, cause unknown
(799.0) Asphyxia
(799.1) Respiratory arrest
(958.4) Traumatic shock
Inpatient records with a source of admission indicating that the patient was transferred from another facility were excluded. We intentionally included broad diagnoses to capture the inpatient records of all cases of OHCA in CEMSIS.
We used probabilistic linkage techniques to link records between the CEMSIS and OSHPD databases.14–16 Match weights were assigned based on probabilistic linkage techniques. Within each match block, a probabilistic match weight was determined for each match variable (identifier) based on the value-specific probability of agreement in true matches and the probability of random agreement for non-matches. To obtain the overall probabilistic match weight that can be interpreted as evidence in favor of a match, weights from all match variables were combined.
The following linkage blocks were created based on OSHPD discharge diagnoses (ICD-9-CM):
Acute myocardial infarction (410.x)
Cardiac arrest (427.5)
Ventricular tachycardia (427.1) and Ventricular fibrillation (427.4)
Sudden Death Cause Unknown (798.x)
Death (based on disposition in OSHPD database)
Resuscitative procedures - Cardiopulmonary resuscitation (99.60), Atrial cardioversion (99.61), Other electric countershock of heart (99.62), Closed chest cardiac massage (99.63), Carotid sinus stimulation (99.64), Other conversion of cardiac rhythm (99.69), Hypothermia (99.81)
Any encounter at a facility that occurs in the EMS data
Within each linkage block, five iterations were performed using the following blocking variables:
Admission date, gender, age in years, destination facility
Admission date, gender, date of birth
Admission date, age in years, destination facility
Admission date, gender, destination facility
Admission date, gender, age in years
Match variables included incident date, destination facility, date of birth, sex, race, ethnicity and patient ZIP code of residence. When destination facility was not available in CEMSIS, proximity of incident ZIP code to hospital ZIP code was used to limit possible matches in the OSHPD databases. When date of birth was not available in CEMSIS, age in years was utilized. Due to the volume of cases, match thresholds were established based on clerical record review for each block individually. Match weights above the set threshold were considered true matches, and match weights below the threshold were considered non-matches. Additionally, those matches with probabilistic match weights near the threshold were manually reviewed to determine whether the records represented a match or non-match. The blocking strategy for this linkage was to obtain the highest-quality matches first and then to loosen the criteria to allow other records to match. Match weights were chosen to ensure that matches were of good quality.
Outcomes
Our primary outcome was the percent of CEMSIS records of OHCA successfully matched to OSHPD records. Secondary outcomes were match rates by local EMS agency.
Data Analysis
Data are presented using descriptive statistics. Logistic regression with factor variable analysis was performed to evaluate the association between local EMS agency and linkage to OHSPD records. Analyses were performed using SAS (SAS Institute, Cary, NC) and Stata (StataCorp, College Station, TX).
Results
We identified 14,603 records with evidence of OHCA in CEMSIS. Ninety-one duplicate records were excluded (Figure 1). Of the remaining 14,512 records, 7,666 (53%) were missing date of birth; 11,053 (76%) were missing race; 11,103 (77%) were missing ethnicity, 7,972 (55%) were missing patient’s residence zip code; and 6,528 (45%) were missing destination facility information.
Figure 1.
Linkage flow chart.
OHCA = Out-of-hospital cardiac arrest; CEMSIS = California Emergency Medical Services Information Systems; OSHPD = Office of Statewide Health Planning and Development
We matched 4,961 (34.2%) records with OSHPD data (Figure 1). Match results and mean match weights for each of the 31 iterations are shown in the Appendix. Seven hundred twenty-three records were linked to the emergency department database and 4,238 were linked to the inpatient database. Demographic characteristics of patients with matched versus unmatched CEMSIS records are shown in Table 1.
Table 1.
Patient characteristics in linked versus unlinked records.
| Linked (N=4,961) | Unlinked (N=9,551) | Overall (N=14,512) | ||||
|---|---|---|---|---|---|---|
| Age (years)* | 68 (56–80) | 69 (55–82) | 69 (55–82) | |||
| Gender | ||||||
| Male | 2,895 | 58.4% | 5,498 | 57.6% | 8,393 | 57.8% |
| Female | 2,055 | 41.4% | 3,878 | 40.6% | 5,933 | 40.9% |
| Missing | 11 | 0.2% | 175 | 1.8% | 186 | 1.3% |
| Race | ||||||
| White | 1,239 | 25.0% | 1,217 | 12.7% | 2,456 | 16.9% |
| Black | 185 | 3.7% | 138 | 1.4% | 323 | 2.2% |
| Asian | 135 | 2.7% | 114 | 1.2% | 249 | 1.7% |
| Other | 213 | 4.3% | 223 | 2.3% | 431 | 3.0% |
| Missing | 3,194 | 64.4% | 7,859 | 82.3% | 11,053 | 76.2% |
| Ethnicity | ||||||
| Hispanic | 295 | 5.9% | 309 | 3.2% | 604 | 4.2% |
| Non-Hispanic | 1,470 | 29.6% | 1,335 | 14.0% | 2,805 | 19.3% |
| Missing | 3,196 | 64.4% | 7,907 | 82.8% | 11,103 | 76.5% |
Data are presented as median (interquartile range).
Linkage rates varied significantly by local EMS agency, ranging from 1.4% to 61.1% (OR for linkage 0.009–0.76; p<0.0001; Table 2). Overall, the percentage of data fields completed by each local EMS agency correlated with the percentage of records from the local EMS agency matched to OSHPD data (Figure 2). After excluding the local EMS agency with the outlying low linkage rate, we linked 4,934/12,596 (39.2%) records.
Table 2.
Linkage rates by Local EMS Agency.
| LEMSA | Total Cases | Linked Cases | Linkage Rate | Odds Ratio* | 95% CI |
|---|---|---|---|---|---|
| A | 779 | 476 | 61% | 1.00 | -- |
| B | 5743 | 1844 | 32% | 0.30 | (0.26–0.35) |
| C | 446 | 168 | 38% | 0.38 | (0.30–0.49) |
| D | 916 | 408 | 45% | 0.51 | (0.42–0.62) |
| E | 213 | 116 | 54% | 0.76 | (0.56–1.03) |
| F | 1916 | 27 | 1% | 0.009 | (0.006–0.014) |
| G | 367 | 200 | 54% | 0.76 | (0.59–0.98) |
| H | 32 | 9 | 28% | 0.25 | (0.11–0.55) |
| I | 521 | 212 | 41% | 0.44 | (0.35–0.55) |
| J | 1151 | 588 | 51% | 0.66 | (0.55–0.80) |
| K | 474 | 194 | 41% | 0.44 | (0.35–0.56) |
| L | 1194 | 491 | 41% | 0.44 | (0.37–0.53) |
| M | 355 | 120 | 34% | 0.33 | (0.25–0.42) |
| N | 330 | 77 | 23% | 0.19 | (0.14–0.26) |
| O | 75 | 31 | 41% | 0.45 | (0.28–0.73) |
p-value <0.0001
EMS=Emergency medical services; LEMSA=Local EMS agency; CI = Confidence interval
Figure 2.
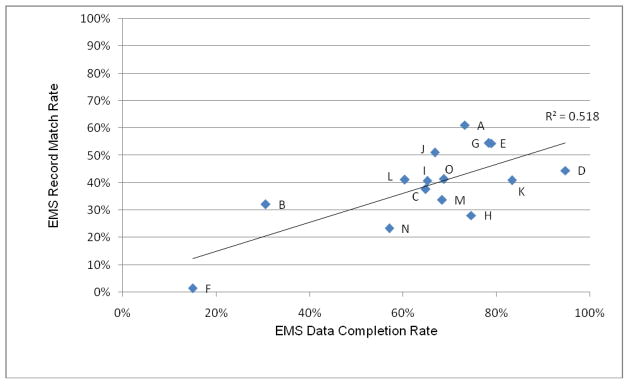
EMS data completion and match rates for local EMS agencies
EMS = Emergency medical services
Local EMS agencies are labeled A through O.
Discussion
We demonstrated the limited feasibility of matching prehospital data from the CEMSIS database with hospital outcomes data from the OSHPD databases to create a complete “episode of care” for patients with OHCA. EMS patient care reports are particularly valuable in OHCA, as they contain elements associated with patient outcomes, such as EMS response times, bystander interventions, initial arrest rhythm, and witnessed versus non-witnessed status,17, 18 that may not be documented elsewhere in patients’ medical records. These data are important for quality improvement and research programs. This model provides the methodological foundation for future EMS outcomes studies.
We selected a probabilistic over deterministic linkage algorithm. Deterministic linkage techniques are typically chosen when few identifiers that are reliably coded are used to connect two databases. Deterministic linkages are inefficient when many match variables are used or when coding errors may exist in the match variables. In the latter situation, probabilistic linkage can allow for small amounts of disagreement, whereas deterministic linkage would not result in a match. While a deterministic approach may have provided greater match specificity, we felt that the sensitivity provided by a probabilistic approach was important given the limitations of our data. The linkage variables in our data had a substantial amount of missing data. Furthermore, the linkage variables we had were not reliable, with m-probabilities showing that we only had three variables for which the value agreed on >90% of matches: gender, incident date, and destination facility.
Based on the published OHCA incidence of 52.1 per 100,000 population, we expected to identify approximately 18,000 cases of OHCA in the CEMSIS database based on the population served by contributing local EMS agencies. While we identified 78% of predicted cases using multiple inclusion criteria, queries that rely on one or a few fields to identify cases would be unlikely to capture all cases, limiting the utility of CEMSIS for future studies.
While probabilistic linkage of these datasets was feasible, our linkage rate was lower than those previously reported for EMS and hospital records linkage.7, 9, 11, 13 OHSPD data has been previously linked to several other databases using a similar algorithm,19–21 making it unlikely to be limiting the success of our linkage. Several other factors likely account for this discrepancy. First, a substantial number of OHCA cases end with prehospital termination of resuscitation without transport to an acute care hospital. Prehospital termination of resuscitation was not reliably recorded in CEMSIS. Data from the Cardiac Arrest Registry to Enhance Survival indicate that over 22% of OHCA cases result in prehospital termination of resuscitation,22 and data from the Resuscitation Outcomes Consortium show that 64% of all OHCA patients and 37% of OHCA patients with EMS resuscitation attempted were not transported.1 While these data were not captured in the CEMSIS database, we suspect that prehospital termination of resuscitation and death upon EMS arrival account for the majority of unlinked records. Second, CEMSIS records were missing a substantial number of the data fields used in the linkage algorithm. Last, a small number of patients (<1%) were transported to an acute care hospital that does not contribute to the OSHPD database. These hospitals include Veterans Affairs and other military facilities as well as those located outside California.
We faced challenges similar to those noted in other EMS linkage papers. First, we encountered non-standardized hospital names and codes in the CEMSIS database that required manual standardization prior to linkage. Fosbol, et al., reported similar challenges in their linkage of EMS and hospital records.11 Second, we noted significant variation in linkage rate between local EMS agencies. While some variation may have been due to differences in practices regarding prehospital termination of resuscitation, our findings suggest that missing data play an important role. A similar inverse relationship between missing data and match rate has been demonstrated in trauma registries.9 As in other systems,6 the local EMS agencies voluntarily reported data to CEMSIS. Some local EMS agencies submitted datasets that contained a very limited number of records and/or variables. Providing local EMS agencies with the knowledge regarding the importance of complete data and potential incentives, such as access to the linked patient outcomes dataset for their agencies, is one strategy to increase participation and data completeness. This is an important issue for groups managing prehospital databases. Such personnel should implement interventions to improve the completeness of prehospital databases.
Limitations
We restricted OSHPD records to those with diagnoses most likely to be assigned to patients with OHCA. While this decision decreased the likelihood of records matching at random, we may have excluded some patients with OHCA who had alternative diagnoses reported to OSHPD. Varying the linkage criteria altered our match results. Thus, we selected criteria that yielded conservative results and increased the likelihood that we were identifying true CEMSIS-OHSPD matches. We spent considerable time and effort trying to lower the match thresholds, but lowering them resulted in many mismatches. We do not believe that our poor match rate was a result of the match threshold. Instead, we believe that poor match results are due to missing or incorrectly captured EMS data. We found that match quality hinged upon the quality of the EMS data (Figure 2).
Conclusions
Probabilistic linkage of CEMSIS prehospital data with OSHPD outcomes data appears feasible but was severely limited by the completeness of the EMS data. We identified several barriers contributing to the incompleteness of the EMS data. States and EMS agencies should aim to overcome these barriers so that more effective linkages are possible.
Acknowledgments
Financial Support: The project described was supported by the ZOLL-National Association of EMS Physicians EMS Resuscitation Research Fellowship, the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through grant #UL1 TR000002 and the National Heart, Lung, and Blood (NHLBI) Research Career Development Programs in Emergency Medicine through grant #5K12HL108964-03.
Funding Sources:
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant #UL1 TR000002. The first author is supported by the National Heart, Lung, and Blood (NHLBI) Research Career Development Programs in Emergency Medicine through grant #5K12HL108964-03 and the ZOLL-National Association of EMS Physicians EMS Resuscitation Research Fellowship.
Appendix. Linkage blocks and match results by block
| Linkage Blocks | Number of Matched Records | Percent of Total Matched Records | Mean Weight for Matched Records |
|---|---|---|---|
| Block 1: In-hospital deaths and sudden cardiac death (ICD-9-CM 798.x) | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 619 | 12.5% | 60.45 |
| Step 2: Admission Date, Gender, Date of Birth | 511 | 10.3% | 65.47 |
| Step 3: Admission Date, Age (Years), Facility | 16 | 0.3% | 54.78 |
| Step 4: Admission Date, Gender, Facility | 318 | 6.4% | 41.83 |
| Step 5: Admission Date, Gender, Age (Years) | 518 | 10.4% | 46.09 |
|
| |||
| Block 2: Cardiac arrest (ICD-9-CM 427.5) | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 215 | 4.3% | 59.98 |
| Step 2: Admission Date, Gender, Date of Birth | 47 | 0.9% | 65.87 |
| Step 3: Admission Date, Age (Years), Facility | 2 | 0.0% | 55.12 |
| Step 4: Admission Date, Gender, Facility | 21 | 0.4% | 45.92 |
| Step 5: Admission Date, Gender, Age (Years) | 48 | 1.0% | 51.50 |
|
| |||
| Block 3: Ventricular tachycardia (427.1) and fibrillation (427.4) | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 119 | 2.4% | 61.77 |
| Step 2: Admission Date, Gender, Date of Birth | 34 | 0.7% | 61.83 |
| Step 3: Admission Date, Age (Years), Facility | 1 | 0.0% | 58.71 |
| Step 4: Admission Date, Gender, Facility | 108 | 2.2% | 40.02 |
| Step 5: Admission Date, Gender, Age (Years) | 70 | 1.4% | 38.97 |
|
| |||
| Block 4: Acute myocardial infarction (410.x) | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 76 | 1.5% | 56.38 |
| Step 2: Admission Date, Gender, Date of Birth | 50 | 1.0% | 54.70 |
| Step 3: Admission Date, Age (Years), Facility | 6 | 0.1% | 57.28 |
| Step 4: Admission Date, Gender, Facility | 180 | 3.6% | 41.34 |
| Step 5: Admission Date, Gender, Age (Years) | 92 | 1.9% | 38.67 |
|
| |||
| Block 5: Resuscitative procedures* | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 6 | 0.1% | 62.41 |
| Step 2: Admission Date, Gender, Date of Birth | 3 | 0.1% | 63.82 |
| Step 3: Admission Date, Age (Years), Facility | -- | -- | -- |
| Step 4: Admission Date, Gender, Facility | 5 | 0.1% | 42.17 |
| Step 5: Admission Date, Gender, Age (Years) | 3 | 0.1% | 37.03 |
|
| |||
| Block 6: Enounters at any facility in CEMSIS data with restrictions** | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 743 | 15.0% | 51.28 |
| Step 2: Admission Date, Gender, Date of Birth | -- | -- | -- |
| Step 3: Admission Date, Age (Years), Facility | 44 | 0.9% | 48.12 |
| Step 4: Admission Date, Gender, Facility | 605 | 12.2% | 48.52 |
| Step 5: Admission Date, Gender, Age (Years) | -- | -- | -- |
|
| |||
| Block 7: Encounters at any facility in CEMSIS data | |||
| Step 1: Admission Date, Gender, Age (Years), Facility | 265 | 5.3% | |
| Step 2: Admission Date, Gender, Date of Birth | -- | -- | -- |
| Step 3: Admission Date, Age (Years), Facility | 0 | 0.0% | n/a |
| Step 4: Admission Date, Gender, Facility | 0 | 0.0% | n/a |
| Step 5: Admission Date, Gender, Age (Years) | -- | -- | -- |
|
| |||
| TOTAL | 4961 | 100.0% | 52.10 |
CEMSIS = California Emergency Medical Services Information System
-- Step was not performed
Resuscitative procedures included: Cardiopulmonary resuscitation (99.60), Atrial cardioversion (99.61), Other electric countershock of heart (99.62), Closed chest cardiac massage (99.63), Carotid sinus stimulation (99.64), Other conversion of cardiac rhythm (99.69), Hypothermia (99.81)
Restrictions: ED records with a disposition of home were excluded. Records with an inpatient length of stay of shorter than three days, no cardiac arrest diagnosis, and survival to discharge were excluded.
Footnotes
Declaration of Interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Previous Presentation: None.
References
- 1.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aufderheide TP, Alexander C, Lick C, Myers B, Romig L, Vartanian L, Stothert J, McKnite S, Matsuura T, Yannopoulos D, Lurie K. From laboratory science to six emergency medical services systems: New understanding of the physiology of cardiopulmonary resuscitation increases survival rates after cardiac arrest. Critical care medicine. 2008;36(11 Suppl):S397–404. doi: 10.1097/ccm.0b013e31818a7e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salvucci A., Jr Improving SCA survival. A comprehensive approach to improving SCA outcomes helped raise Ventura County’s v-tach/v-fib survival rate above 50% EMS magazine. 2009;386(12):44. 8–9. [PubMed] [Google Scholar]
- 4.Maio RF, Garrison HG, Spaite DW, Desmond JS, Gregor MA, Cayten CG, Chew JL, Jr, Hill EM, Joyce SM, MacKenzie EJ, Miller DR, O’Malley PJ, Stiell IG. Emergency medical services outcomes project I (EMSOP I): prioritizing conditions for outcomes research. Ann Emerg Med. 1999;33(4):423–32. doi: 10.1016/s0196-0644(99)70307-0. [DOI] [PubMed] [Google Scholar]
- 5.Spaite DW, Maio R, Garrison HG, Desmond JS, Gregor MA, Stiell IG, Cayten CG, Chew JL, Jr, Mackenzie EJ, Miller DR, O’Malley PJ. Emergency Medical Services Outcomes Project (EMSOP) II: developing the foundation and conceptual models for out-of-hospital outcomes research. Ann Emerg Med. 2001;37(6):657–63. doi: 10.1067/mem.2001.115215. [DOI] [PubMed] [Google Scholar]
- 6.Newgard CD, Zive D, Malveau S, Leopold R, Worrall W, Sahni R. Developing a statewide emergency medical services database linked to hospital outcomes: a feasibility study. Prehosp Emerg Care. 2011;15(3):303–19. doi: 10.3109/10903127.2011.561404. [DOI] [PubMed] [Google Scholar]
- 7.Hettinger AZ, Cushman JT, Shah MN, Noyes K. Emergency medical dispatch codes association with emergency department outcomes. Prehosp Emerg Care. 2013;17(1):29–37. doi: 10.3109/10903127.2012.710716. [DOI] [PubMed] [Google Scholar]
- 8.Cone DC, Irvine KA, Middleton PM. The methodology of the Australian Prehospital Outcomes Study of Longitudinal Epidemiology (APOStLE) Project. Prehosp Emerg Care. 2012;16 (4):505–12. doi: 10.3109/10903127.2012.689929. [DOI] [PubMed] [Google Scholar]
- 9.Newgard C, Malveau S, Staudenmayer K, Wang NE, Hsia RY, Mann NC, Holmes JF, Kuppermann N, Haukoos JS, Bulger EM, Dai M, Cook LJ. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19(4):469–80. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newgard CD, Richardson D, Holmes JF, Rea TD, Hsia RY, Mann NC, Staudenmayer K, Barton ED, Bulger EM, Haukoos JS The Western Emergency Services Translational Research Network Westrn I. Physiologic field triage criteria for identifying seriously injured older adults. Prehosp Emerg Care. 2014;18(4):461–70. doi: 10.3109/10903127.2014.912707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fosbol EL, Granger CB, Peterson ED, Lin L, Lytle BL, Shofer FS, Lohmeier C, Mears GD, Garvey JL, Corbett CC, Jollis JG, Glickman SW. Prehospital system delay in ST-segment elevation myocardial infarction care: a novel linkage of emergency medicine services and in hospital registry data. Am Heart J. 2013;165(3):363–70. doi: 10.1016/j.ahj.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Govindarajan PCL, Ghilarducci D, Johnston SC. Probabilistic Matching of Computerized Emergency Medical Services (EMS) records and Emergency Department and Patient Discharge Data: a Novel Approach to Evaluation of Prehospital Stroke Care. Stroke. 2012;(43):A2721. [Google Scholar]
- 13.Waien SA. Linking large administrative databases: a method for conducting emergency medical services cohort studies using existing data. Acad Emerg Med. 1997;4(11):1087–95. doi: 10.1111/j.1553-2712.1997.tb03684.x. [DOI] [PubMed] [Google Scholar]
- 14.Winkler WE. Proceedings of the Section of Survey Research Methods. American Statistical Association; 1994. Advanced Methods of Record Linkage; pp. 467–72. [Google Scholar]
- 15.Mader TJ, Nathanson BH, Soares WE, 3rd, Coute RA, McNally BF. Comparative Effectiveness of Therapeutic Hypothermia After Out-of-Hospital Cardiac Arrest: Insight from a Large Data Registry. Ther Hypothermia Temp Manag. 2014;4(1):21–31. doi: 10.1089/ther.2013.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newcombe HB. Handbook of Record Linkage: Methods for Health and Statistical Studies, Administration, and Business. Oxford: Oxford University Press; 1988. [Google Scholar]
- 17.Stub D, Smith K, Bray JE, Bernard S, Duffy SJ, Kaye DM. Hospital characteristics are associated with patient outcomes following out-of-hospital cardiac arrest. Heart. 2011;97(18):1489–94. doi: 10.1136/hrt.2011.226431. [DOI] [PubMed] [Google Scholar]
- 18.Stiell IG, Wells GA, DeMaio VJ, Spaite DW, Field BJ, 3rd, Munkley DP, Lyver MB, Luinstra LG, Ward R. Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario Prehospital Advanced Life Support. Ann Emerg Med. 1999;33(1):44–50. doi: 10.1016/s0196-0644(99)70415-4. [DOI] [PubMed] [Google Scholar]
- 19.Herrchen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput Biomed Res. 1997;30(4):290–305. doi: 10.1006/cbmr.1997.1448. [DOI] [PubMed] [Google Scholar]
- 20.Smith LH, Danielsen B, Allen ME, Cress R. Cancer associated with obstetric delivery: results of linkage with the California cancer registry. Am J Obstet Gynecol. 2003;189(4):1128–35. doi: 10.1067/s0002-9378(03)00537-4. [DOI] [PubMed] [Google Scholar]
- 21.Parker JP, Li Z, Damberg CL, Danielsen B, Carlisle DM. Administrative versus clinical data for coronary artery bypass graft surgery report cards: the view from California. Med Care. 2006;44(7):687–95. doi: 10.1097/01.mlr.0000215815.70506.b6. [DOI] [PubMed] [Google Scholar]
- 22.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, Kellermann A. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60(8):1–19. [PubMed] [Google Scholar]



