Abstract
Background
A source of frustration during laparoscopic cholecystectomy involves extraction of the gallbladder through port sites smaller than the gallbladder itself. We describe the development and testing of a novel device for the safe, minimal enlargement of laparoscopic port sites to extract large, stone-filled gallbladders from the abdomen.
Methods
The study device consists of a handle with a retraction tongue to shield the specimen and a guide for a scalpel to incise the fascia within the incision. Patients enrolled underwent laparoscopic cholecystectomy. Gallbladder extraction was attempted. If standard measures failed, the device was implemented. Extraction time and device utility scores were recorded for each patient. Patients returned 3 - 4 weeks post-operatively for assessment of pain level, cosmetic effect, and presence of infectious complications.
Results
Twenty (51%) of 39 patients required the device. Average extraction time for the first 8 patients was 120 seconds. After interim analysis, an improved device was used in twelve patients, and average extraction time was 24 seconds. There were no adverse events. Post-operative pain ratings and incision cosmesis were comparable between patients with and without use of the device.
Conclusion
The study device enables safe and rapid extraction of impacted gallbladders through the abdominal wall.
Keywords: Laparoscopic cholecystectomy, laparoscopic surgery, safety
Introduction
Laparoscopic cholecystectomy has become one of the most common general surgical procedures, with estimates of up to 500,000 annually.1 Operative times are short and generally have good outcomes; however, a source of frustration commonly encountered involves extraction of the gallbladder through a port site smaller than the gallbladder itself. Not every laparoscopic cholecystectomy is associated with a prolonged extraction. However, in difficult cases, with large and stone filled gallbladders, the organ cannot be removed until the surgical incision is elongated. This can lead to lengthened operative times, with increased cost to the patient and to the institution.
There is little in the literature regarding what proportion of patients undergoing laparoscopic cholecystectomy will experience prolonged or difficult extraction; however anecdotal estimates suggest 20-30% of patients have this problem. Furthermore, difficult extraction may lead to rupture of the gallbladder with spillage of bile and gallstones in rare cases. 2 Anecdotal cases support concern about the associated risk; thus, it is common surgical practice to avoid bile spillage. 3,4 Furthermore, when gallbladder carcinoma is present, whether known or incidental, biliary spillage has been associated with worsened prognosis, likely due to peritoneal dissemination. 5,6 The diagnosis of cancer often is not made until post-operative pathologic examination; thus spillage risk must be minimized for all patients. 7
Few studies have attempted to discern the optimal method for gallbladder extraction from the abdominal cavity; however, one study found incision extension to result in no increase in morbidity. 8 Such extension is often technically awkward and entails significant potential risk to the patient, because available tools are not designed for this purpose. Other methods currently employed by surgeons include stretching of the incision using brute force, also without specialized instruments. Collectively, these approaches can result in sequelae of stretching such as bruising and excessive pain, or may result in puncture of the specimen bag. Given the proliferation of minimally invasive approaches to many abdominal operations, an approach for safe and rapid incision extension with specimen extraction may be of use in a variety of settings.
Materials and Methods
Study Device
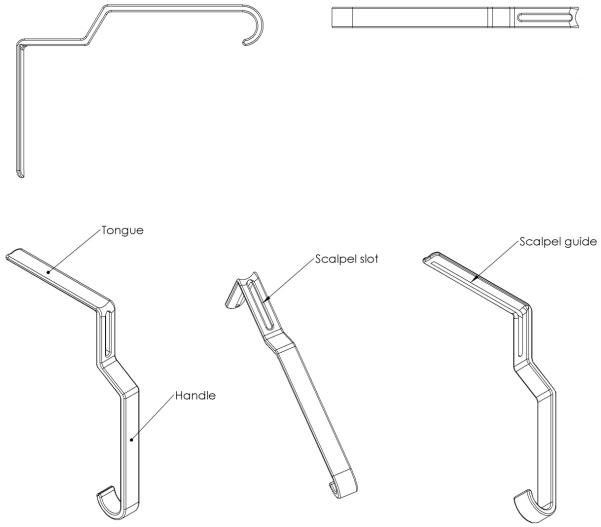
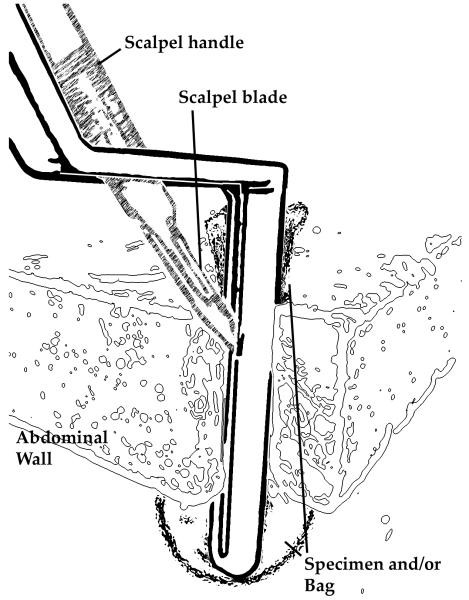
The study device (Laparoscopic Incision Safe Removal Device, LISRD) was developed by 3 of the co-authors (JJ, WG, CS). It is a sterilizable and reusable surgical tool constructed of polished 304 stainless steel, with a handle at one end and a blunt tongue at the other end (Figure 1). The intended use is to insert the tongue of the instrument through the port site beside the endocatch bag containing the gallbladder. The tongue slides along the bag and gallbladder, separating them from the abdominal wall. Retraction force is then applied to the handle of the instrument, as gentle traction is applied simultaneously to the string of the endocatch bag. A #11 blade scalpel is then slid between the tongue of the instrument and the abdominal wall in a vertical motion. (Figure 2) Because the layer of the abdominal wall that is obstructing specimen removal is under the greatest tension, the obstructing layer is incised more than the rest of the abdominal wall during this process. Skin is incised during this process, however is typically not the obstructing layer and thus is minimally incised. A groove on the tongue of the instrument provides guidance for the scalpel blade. Once the incision is adequately extended, gentle traction on the gallbladder bag will safely remove it from the patient’s abdomen with minimal extension. With adequate pneumoperitoneum, small bowel and other viscera are well out of the way of the specimen removal site. Furthermore, the retraction tongue provides some additional protection of these structures in much the same manner as the specimen bag is protected during incision extension.
Figure 1.
Schematic representation of study device.
Figure 2.
Example of the study device use in a laparoscopic incision.
The initial study device was constructed of two pieces of steel with a single weld. After use on 8 study patients, a second-generation device was produced by selective laser scintering with minor design revisions. These revisions included removal of the weld and extending the slit to the proximal surface of the retraction tongue. This device was used in the remaining patients.
Clinical Trial Design
Following IRB approval (UVA HSR IRB# 15296), this single institution, single surgeon study was offered to patients presenting for laparoscopic cholecystectomy with diagnoses perceived as high risk for difficult gallbladder extraction: cholelithiasis with or without complicating features. The study surgeon (PTH) has expertise in laparoscopic techniques and had no role in initial development of the device. Primary goals of the study were to assess the safety and utility of this device in extraction of difficult gallbladders during laparoscopic cholecystectomy, as measured by surgeon’s assessment and by measuring the time necessary to extract difficult gallbladders from the abdomen using the device. Fascial and skin closure was undertaken in the usual methods utilized by the study surgeon, which involved primary fascial closure or use of a Carter Thomason ™ device (Cooper Surgical) and subcuticular suture closure of the skin. The study was designed to allow an interim analysis of utility, followed by redesign and retesting of the device. Secondary goals were to gain familiarity with use of the study device, and to determine the proportion of enrolled patients in which the study device is deemed necessary by the study surgeon. As a pilot study, it was felt that use of the device in 20 patients would be appropriate to obtain preliminary data on safety and utility of the device and to enable redesign and testing if needed.
Intraoperative and Postoperative Study Procedures
After the gallbladder was mobilized from the liver and placed in an Ethicon Endocatch ™ specimen bag, removal through the 12 mm umbilical port site was attempted. If the gallbladder was easily withdrawn through the port site, the device was not used. However, if removal through the port site was not successful, and the surgeon considered using measures other than gentle traction on the specimen bag, the device was implemented. Length of time for extraction was recorded from insertion of the device until the specimen removal. The study surgeon scored the following series of device utilization characteristics for each patient: overall utility, insertion positioning, extension and groove guide, retraction sturdiness, specimen removal, and blade removal. Device utilization characteristics were scored on a 5 point Likert scale, with values from 1 (outstanding benefit) to 5 (hindrance to procedure). All patients consenting to use of the device were followed for the occurrence of adverse events during the post-operative period. Intended follow-up was in 3 to 4 weeks based on institution practice for patients undergoing laparoscopic cholecystectomy. At this return visit, enrolled patients were assessed for overall pain level during the post-operative period as reported by the patient using a pain scale ranging from 1 (no pain) to 5 (severe pain). Cosmetic result was reported by the patient and study surgeon and measured on a Likert scale from 1 (excellent result) to 5 (poor result). Patients were also evaluated for infectious complications during the post-operative period. Means and standard deviations were calculated for each for each of the scored intra-operative device utilization characteristics. Single factor analysis of variance was used to assess the statistical significance (p-values) of the difference in mean cosmesis and post-operative pain scores between patients in the device and no device groups. Mean time for extraction using the device was calculated separately for the first 8 patients with the initial device and the remaining 12 with the improved device.
Results
Thirty-nine patients were consented and enrolled in the study. Three patients were excluded from the analysis following consent, due either to conversion to an open procedure (1), withdrawal of consent prior to surgery (1), or an inability to obtain the device immediately prior to the operation (1). Among the 36 included patients, there were 20 (56%) with difficult gallbladder extraction, requiring use of the device.
Table 1 presents a summary of indications for the operation, device use duration, and device utilization characteristics, for patients allocated to the initial device. Table 2 presents similar summary information for patients allocated to the revised device. Biliary colic and chronic cholecystitis were the most common indications. Average extraction time among the first 8 patients with use of the device was 120 seconds (range 27-416 sec; Table 1). After a planned interim analysis, an improved device was produced and used in the next 12 patients, for whom the average extraction time was 24 seconds (range 10-42 sec; Table 2). No adverse events were reported for any patient in the study. Follow-up data for cosmesis and pain were available for 27 (75%) of the 36 evaluable patients on the study, including 17 of 20 (85%) patients in the device group and 9 of 16 (56%) patients in the non-device group. Mean follow-up for the entire cohort of patients was 30 days (σ = 14 days). For the device group average follow-up was 31 days (σ = 15), and for the no device group average follow-up was 28 days (σ = 12). Post-operative pain rating and incision cosmesis were comparable between patient groups (Table 3). No wound infections or other wound complications were encountered in either group.
Table 1. Results for patients allocated to initial device (n = 8).
| Indication for Operation | Frequency (%) |
|---|---|
| Biliary Colic | 4 (50%) |
| Choledocholithiasis | 1 (12%) |
| Chronic Cholecystitis | 2 (25%) |
| Chronic Cholecystitis w/ hydrops | 1 (12%) |
| Mean (Std) | |
| Time for removal (in seconds) | 120 (124.5) |
| Utilization characteristics – surgeon assessment | Mean (Std) |
| Overall utility | 1.5 (0.5) |
| Insertion positioning | 1.4 (0.5) |
| Extension and grove guide | 1.6 (0.5) |
| Retraction sturdiness | 1.0 (0.0) |
| Specimen removal | 1.9 (0.8) |
| Blade removal | 1.0 (0.0) |
Note: Utilization characteristic categories are scored on five point ordinal scale, with 1 indicating outstanding benefit and 5 indicating hindrance to procedure.
Table 2. Results for patients allocated to revised device (n = 12).
| Indication for Operation | Frequency (%) |
|---|---|
| Biliary Colic | 4 (33%) |
| Acute Cholecystitis | 2 (17%) |
| Chronic Cholecystitis | 3 (25%) |
| Gallstone Pancreatitis | 1 (8%) |
| Symptomatic Cholelithiasis | 2 (17%) |
| Mean (Std) | |
| Time for removal (in seconds) | 24.3 (9.4) |
| Utilization characteristics | Mean (Std) |
| Overall utility | 1.1 (0.3) |
| Insertion positioning | 1.0 (0.0) |
| Extension and grove guide | 1.0 (0.0) |
| Retraction sturdiness | 1.0 (0.0) |
| Specimen removal | 1.3 (0.5) |
| Blade removal | 1.0 (0.0) |
Note: Utilization characteristic categories are scored on five point ordinal scale, with 1 indicating outstanding benefit and 5 indicating hindrance to procedure.
Table 3.
Comparison of cosmesis and post-operative pain scores between patients in device and no device groups
| Device group (n = 17) |
No device group (n = 9) |
||
|---|---|---|---|
| Outcome | Mean (Std) |
Mean (Std) |
P-Value |
| Cosmesis Rating by Surgeon |
1.1 (0.5) | 1.1 (0.3) | 0.9716 |
| Cosmesis Rating by Patient |
1.1 (0.2) | 1.1 (0.3) | 0.6501 |
| Post-operative Pain | 1.9 (0.7) | 2.1 (1.2) | 0.6694 |
Note: Findings are scored on five point ordinal scale, with 1 indicating outstanding cosmetic result and 5 indicating poor cosmetic result.
Discussion
Shortly after laparoscopic cholecystectomy became popular, a number of methods for extracting stone-filled gallbladders were proposed, including multiple devices that never achieved widespread use. 9-11 Ultimately, popular techniques suggested in surgical texts are to stretch the incision and fascia using a Kelly clamp or to use a Kelly clamp as a retractor while incising the fascia and extending the incision.12 Those technique utilize tools that were not designed for such a purpose and risk damage to the specimen, potentially leading to spillage of bile or stones. Furthermore, those technique can be cumbersome and can lead to an inordinate amount of time required for this seemingly simple step of an otherwise uncomplicated operation. The device utilized in the present trial enabled rapid and simple gallbladder extraction without apparent complications.
A further finding of this study is the high proportion of patients who experience difficult gallbladder extraction. To our knowledge, data of this kind have not been previously reported. Inclusion criteria for the current trial excluded patients with biliary dyskinesia, thus difficult extraction rates for unselected patients undergoing laparoscopic cholecystectomy may be lower in practice. Furthermore, this may be dependent on patient population and may differ in a community setting, as opposed to the academic medical center where the study was performed.
The current study has several limitations. This study was meant as a pilot study, and not meant to draw comparison between techniques. Such a comparison would require a larger number of patients and randomization. Data from this trial however are useful for the design and powering of a future randomized trial. Furthermore, follow-up rates were lower than anticipated, and lower in those that did not undergo use of the device. This was likely due to random chance with a small patient cohort. Reasons for this were varied, including some patients who moved out of the area before follow-up and others who simply missed appointments during the time of the study.
The data show that time to removal of the gallbladder was very rapid (mean 24 sec) with the optimized device, and that the device is safe and easy to use. Thus, the device and techniques utilized in this study represent a novel solution to a source of frustration with a very common operation and warrant further consideration in order to decrease operative time and to increase surgeon satisfaction in dealing with this very common problem. Based on these data, approval to utilize this device outside of study protocol is being sought, and further study in the form of a larger randomized trial of device use compared to standard methods may be helpful to quantify benefits to use of this novel device.
Acknowledgments
Funding: This work was supported by a grant from the Biomedical Innovation Fund of the Ivy Foundation of the University of Virginia.
Footnotes
This work was presented in poster presentation format at the 2013 Digestive Disease Week.
References
- 1.Olsen DO. Laparoscopic cholecystectomy. The American Journal of Surgery. 1991;161(3):339–344. doi: 10.1016/0002-9610(91)90592-2. doi: 10.1016/0002-9610(91)90592-2. [DOI] [PubMed] [Google Scholar]
- 2.Dreznik Z, Soper NJ. Trocar site abscess due to spilled gallstones: An unusual late complication of laparoscopic cholecystectomy. Surg Laparosc Endosc. 1993;3(3):223–224. [PubMed] [Google Scholar]
- 3.Battaglia DM, Fornasier VL, Mamazza J. Gallstone in abdominal wall--a complication of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11(1):50–52. [PubMed] [Google Scholar]
- 4.Zulfikaroglu B, Ozalp N, Mahir Ozmen M, Koc M. What happens to the lost gallstone during laparoscopic cholecystectomy? Surg Endosc. 2003;17(1):158. doi: 10.1007/s00464-002-4242-1. doi: 10.1007/s00464-002-4242-1. [DOI] [PubMed] [Google Scholar]
- 5.Sarli L, Contini S, Sansebastiano G, Gobbi S, Costi R, Roncoroni L. Does laparoscopic cholecystectomy worsen the prognosis of unsuspected gallbladder cancer? Arch Surg. 2000;135(11):1340–1344. doi: 10.1001/archsurg.135.11.1340. [DOI] [PubMed] [Google Scholar]
- 6.Wullstein C, Woeste G, Barkhausen S, Gross E, Hopt UT. Do complications related to laparoscopic cholecystectomy influence the prognosis of gallbladder cancer? Surg Endosc. 2002;16(5):828–832. doi: 10.1007/s00464-001-9085-7. doi: 10.1007/s00464-001-9085-7. [DOI] [PubMed] [Google Scholar]
- 7.Kim JH, Kim WH, Kim JH, Yoo BM, Kim MW. Unsuspected gallbladder cancer diagnosed after laparoscopic cholecystectomy: Focus on acute cholecystitis. World J Surg. 2010;34(1):114–120. doi: 10.1007/s00268-009-0279-9. doi: 10.1007/s00268-009-0279-9; 10.1007/s00268-009-0279-9. [DOI] [PubMed] [Google Scholar]
- 8.Bordelon BM, Hobday KA, Hunter JG. Incision extension is the optimal method of difficult gallbladder extraction at laparoscopic cholecystectomy. Surg Endosc. 1992;6(5):225–227. doi: 10.1007/BF02498808. [DOI] [PubMed] [Google Scholar]
- 9.Sackier JM, Hunter JG, Paz-Partlow M, Cuschieri A. The rotary gallstone lithotrite to aid gallbladder extraction in laparoscopic cholecystectomy. Surg Endosc. 1992;6(5):235–238. doi: 10.1007/BF02498810. [DOI] [PubMed] [Google Scholar]
- 10.Bickel A, Szabo A, Shtamler B. A safe simple method for removal of the gallbladder through the umbilical trocar site during laparoscopic cholecystectomy. J Laparoendosc Surg. 1993;3(5):485–487. doi: 10.1089/lps.1993.3.485. [DOI] [PubMed] [Google Scholar]
- 11.Kanehira E, Omura K, Kawai K, Ishikawa N, Watanabe Y. A new extraction bag to facilitate stone extraction in laparoscopic cholecystectomy: In vitro experiments. Endosc Surg Allied Technol. 1994;2(6):297–299. [PubMed] [Google Scholar]
- 12.John Hunter ST. Laparoscopic cholecystectomy, intraoperative cholangiography, and common bile duct exploration. In: Josef Fisher KB, editor. Mastery of surgery. 5th ed. Lippincott, Williams, and Wilkins; Philadelphia, PA: 2006. pp. 1116–1128. [Google Scholar]