Abstract
There are limited population-based data available describing trends in the long-term prognosis of patients discharged from the hospital after an initial acute myocardial infarction (AMI). Our objectives were to describe multi-decade trends in post-discharge mortality, and their association with hospital management practices, among patients discharged from all central Massachusetts (MA) medical centers after a first AMI. Residents of the Worcester, MA, metropolitan area discharged from all central MA hospitals after a first AMI between 1975 and 2009 comprised the study population (n=8,728). Multivariable-adjusted logistic regression analyses were used to examine the association between year of hospitalization and 1-year post-discharge mortality. The average age of this population was 66 years and 40% were women. Patients hospitalized in 1999-2009, as compared with those discharged in 1975-1984, were older, more likely to be women, and have multiple previously-diagnosed comorbidities. Hospital use of invasive cardiac interventions and medications increased markedly over time. Unadjusted 1-year mortality rates were 12.9%, 12.5%, and 15.8% for patients discharged during 1975-1984, 1986-1997, and 1999-2009, respectively. After adjusting for several demographic characteristics, clinical factors, and in-hospital complications, there were no significant differences in the odds of dying at 1 year post-discharge during the years under study. After further adjustment for hospital treatment practices, the odds of dying at 1 year post-discharge was 2.43 (95% confidence intervals=1.83-3.23) times higher in patients hospitalized in1999-2009 than in 1975-1984. In conclusion, the increased use of invasive cardiac interventions and pharmacotherapies was associated with enhanced long-term survival among patients hospitalized for a first AMI.
Keywords: epidemiology, mortality, acute myocardial infarction
Introduction
The primary objective of our large community-based study was to examine changing trends in long-term prognosis among residents of central Massachusetts (MA) discharged from all central MA medical centers after a first AMI over an approximate 35-year period (1975-2009). A secondary study goal was to understand whether, and to what extent, increases in the use of effective cardiac treatment approaches during the patient's index hospitalization were associated with changes in long-term mortality. Data from the population-based Worcester Heart Attack Study were used for purposes of this investigation.1–4
Methods
Described elsewhere in detail,1–4 the Worcester Heart Attack Study is an ongoing population-based investigation describing long-term trends in the epidemiology of AMI in residents of the Worcester, MA, metropolitan area (2000 census= 478,000) hospitalized at all 16 medical centers in Central MA on an approximate biennial basis during 1975, 1978, 1981, 1984, 1986, 1988, 1990, 1991, 1993, 1995, 1997, 1999, 2001, 2003, 2005, 2007, and 2009.1–4 In 2000, the median age of residents of the Worcester metropolitan area was 37 years, 49% were men, 89% were white, and approximately 25% had a bachelor's degree or higher.4 Due to hospital closures, mergers, or conversion to long-term care or rehabilitation facilities, fewer hospitals (n=11) have been providing care to greater Worcester residents during the most recent years of this community-wide investigation.
Computerized printouts of patients discharged from all greater Worcester hospitals with possible AMI [International Classification of Disease (ICD) 9 codes: 410-414, 786.5] were identified. Cases of possible AMI were independently validated using predefined criteria for AMI;1–4 these criteria included a suggestive clinical history, increases in several serum biomarkers (e.g., creatine kinase (CK), CK-MB, and troponin values), and serial electrocardiographic findings during hospitalization consistent with the presence of AMI. Patients who satisfied at least 2 of these 3 criteria, and were residents of the Worcester metropolitan area, were included.
For purposes of the present study, we restricted our sample to adult residents of the Worcester metropolitan area who survived their index hospitalization for a first AMI between 1975 and 2009. Patients with an initial AMI were identified by either mention in the review of hospital charts that this was the patient's first admission for an AMI or through the review of previous hospital records and electrocardiograms that failed to indicate the occurrence of a previous AMI. This study was approved by the Institutional Review Board at the University of Massachusetts Medical School.
Trained nurses and physicians abstracted information on patients’ demographic characteristics, medical history, clinical data, and treatment practices through the review of hospital medical records. These factors included patient's socio-demographic characteristics (age, sex, race, marital status), year of hospitalization, hospital length of stay, history of previously diagnosed comorbidities (e.g., stroke, diabetes, heart failure), AMI type [Q-wave vs. non-Q-wave; ST-segment elevation myocardial infarction (STEMI) vs. non-ST-segment elevation myocardial infarction (NSTEMI)],5,6 and the development of important in-hospital complications including atrial fibrillation,7 cardiogenic shock,8 heart failure,9 and stroke.10
Data on the receipt of thrombolytic therapy and 3 coronary diagnostic and interventional procedures [cardiac catheterization, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG) surgery] during hospitalization, and pharmacotherapies at the time of hospital discharge, including the prescribing of 6 effective cardiac medications [angiotensin converting inhibitors (ACE-I)/angiotensin receptor blockers (ARBs), anticoagulants, aspirin, beta blockers, calcium channel blockers, and lipid lowering agents], were obtained. While we collected follow-up information on all study patients through 2012, we examined trends in 1-year post-hospital discharge all-cause mortality rates. This time point was chosen since a number of prior investigations11,12 have shown this follow-up point to be a particularly high-risk period for dying among patients discharged from the hospital after an AMI. The approaches used to ascertain survival status after hospital discharge included a review of medical records for additional hospitalizations and a statewide and national search of death certificates for residents of the Worcester metropolitan area.
For ease of analysis and interpretation, we aggregated the 17 individual study years into approximate 3 decade-long time periods (1975-1984, earliest; 1986-1997, middle; and 1999-2009, most recent) for purposes of examining changing trends in 1 year post-discharge mortality rates. These time period categorizations reflect major changes in the management of patients hospitalized with AMI that have occurred over time from the use of mainstay therapies, such as aspirin and beta blockers during the earliest years under study, to the use of thrombolytic therapy in the mid-1980s, to the use of more aggressive and invasive interventions including PCI and lipid lowering therapy during the most recent decade under study. Differences in the distribution of various patient demographic and clinical characteristics, development of in-hospital clinical complications, and hospital treatment practices between the 3 time periods were examined using the ANOVA test for continuous variables and the chi-square test for categorical variables. The Cochran-Armitage tests and linear regression models were used to test for linear trends over time among categorical variables and continuous variables, respectively.
Long-term mortality after hospital discharge was examined by calculating 1-year all-cause mortality rates as we did not collect information on cause-specific mortality. Multivariable-adjusted logistic regression analyses were performed to examine the association between the main explanatory variable of time period of hospitalization (1975-1984, earliest; 1986-1997, middle; and 1999-2009, most recent) and the outcome of 1-year post-discharge all-cause mortality (dead vs. alive) while adjusting for several potentially confounding variables of prognostic importance. Since the 3 time periods reflect changes in the management of patients hospitalized with AMI, and a linear relationship with the outcome of total mortality was not assumed, we dummy coded this variable with the earliest period (1975-1984) serving as the reference group. Several covariates associated with long-term mortality in patients discharged from the hospital after AMI in prior studies13–17 were examined sequentially in 4 blocks. The first block included age, sex, race, marital status, and previously diagnosed comorbid conditions (i.e., angina, diabetes, heart failure, hypertension, and stroke). The second block included AMI type (Q-wave vs. non-Q-wave), in-hospital clinical complications (i.e., atrial fibrillation, heart failure, cardiogenic shock), and hospital length of stay. The third block included in-hospital management practices as represented by the receipt of thrombolytic therapy and 3 coronary diagnostic and interventional procedures (i.e., cardiac catheterization, PCI, and CABG). The fourth block included the prescribing of 4 guideline-recommended cardiac medications (i.e., ACE-I/ARBs, aspirin, beta blockers, and lipid lowering agents) at the time of hospital discharge. Based on their clinical relevance and preliminary univariate associations, all potential covariates were retained and fitted into multivariable logistic regression models by adding the blocks of variables sequentially.
We also repeated our multivariable-adjusted logistic regression analyses restricted to patients hospitalized during the most recent decade under study (1999-2009) for purposes of providing a relatively contemporary perspective into the association between year of hospitalization and 1-year all-cause mortality. For this analysis, we also adjusted for type of AMI (STEMI and NSTEMI) since information about whether the patient's ECG showed changes in ST segment elevation or otherwise was only obtained from 1999 on. Our results were presented as multivariable adjusted odds ratios (OR) and accompanying 95% confidence intervals (CI), which were calculated based on standard errors clustered at the hospital level to account for potential within-hospital correlation with variance adjustment .18
Results
The study population consisted of 8,728 adult residents of the Worcester metropolitan area who survived their hospitalization for an independently confirmed first AMI at all central MA medical centers between 1975 and 2009. Overall, the average age of this patient population was 66.4 years, 60.0% were men, 95.4% were white, and 61.0% were married. Patients discharged from all greater Worcester hospitals after a first AMI during recent, as compared with earlier, study years were significantly older, were more likely to be women, and were less likely to be married. The proportion of patients with a Q-wave MI, and the average hospital stay, declined markedly over time (Table 1).
Table 1.
Characteristics of patients who survived a first acute myocardial infarction (AMI) according to time period of hospitalization: Worcester Heart Attack Study, 1975-2009
| Variable | 1975-1984 (n=1,820) | 1986-1997 (n=3,407) | 1999-2009 (n=3,501) |
|---|---|---|---|
| Mean Age (years)* | 63.8 | 66.3 | 67.9 |
| Age (years)* | |||
| <55 | 24.7% | 21.0% | 21.5% |
| 55-64 | 27.8% | 20.7% | 19.9% |
| 65-74 | 15.5% | 21.9% | 25.1% |
| 75-84 | 15.5% | 21.9% | 25.1% |
| ≥85 | 6.2% | 8.4% | 13.4% |
| Men* | 64.3% | 59.5% | 58.2% |
| White* | 97.2% | 96.1% | 93.7% |
| Married* | 67.1% | 62.2% | 56.6% |
| ST-segment myocardial infarction | - | - | 40.0% |
| Q-wave* | 64.7% | 51.3% | 27.6% |
| Mean hospital length of stay (days) * | 16.8 | 9.5 | 5.5 |
| Angina pectoris* | 18.4% | 19.0% | 12.8% |
| Heart failure* | 6.5% | 7.8% | 13.8% |
| Hypertension* | 44.1% | 51.7% | 65.5% |
| Stroke* | 4.6% | 6.7% | 8.3% |
| Diabetes mellitus* | 18.5% | 23.2% | 27.1% |
P-values derived from Analysis of variance (ANOVA) tests for continuous variables and chi-square tests for categorical variables were all <0.001; p-values for trend tests derived from Cochran-Armitage tests for categorical variables and linear regression models for continuous variables were all <0.001.
During the most recent years under study, patients who survived their initial AMI were more likely to have a history of heart failure, hypertension, diabetes, or stroke than patients hospitalized during earlier study periods (Table 1). The proportion of patients with multiple (≥2) comorbidities increased from 24.2% in 1975-1984 to 36.6% in 1999-2009 (p for trend <0.001).
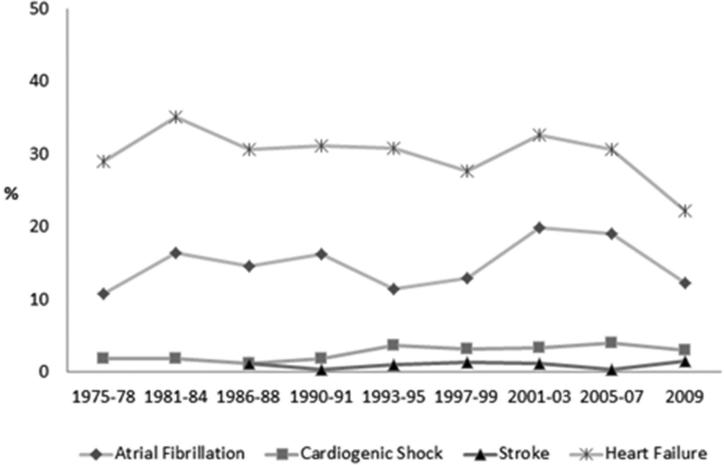
Overall, the likelihood of developing cardiogenic shock or a stroke during the patient's index hospitalization remained relatively low (2.7% and 1.0%, respectively) whereas the incidence rates of in-hospital heart failure and atrial fibrillation were considerably higher (30.5% and 15.2%, respectively). In general, we observed an upward trend in the proportion of patients who developed cardiogenic shock (p for trend <0.001) and atrial fibrillation (p for trend<0.001) but a downward trend in the development of acute heart failure (p for trend=0.043) from the earliest to the most recent years under study; the development of acute stoke remained low and stable throughout the years under study (p=0.67) (Figure 1).
Figure 1.
In-hospital clinical complications among patients who survived a first acute myocardial infarction (AMI): Worcester Heart Attack Study, 1975-2009
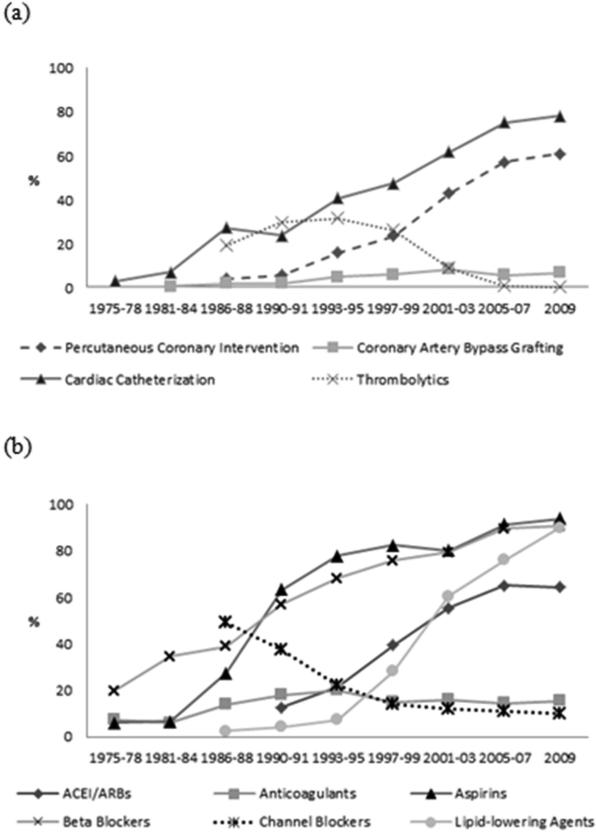
The use of cardiac catheterization and PCI has increased markedly over time whereas the proportion of patients undergoing CABG surgery during their index hospitalization has increased but remained relatively low during the years under study (all p values for trend <0.001). The use of thrombolytic therapy increased during the 1990's but markedly decreased thereafter. Cardiac catheterization, PCI, CABG surgery, and thrombolytic therapy were used in 78.2%, 60.8%, 6.7%, and 0.2%, of patients who survived a first AMI in 2009 (Figure 2a).
Figure 2.
In-hospital coronary procedures and thrombolytic therapy, and cardiac medications at the time of hospital discharge among patients who survived a first acute myocardial infarction (AMI): Worcester heart Attack Study, 1975-2009. (a) In-hospital coronary procedures and thrombolytic therapy (b) Cardiac medications at hospital discharge
Marked increases in the prescribing of ACEI/ARBs, aspirin, beta blockers, and lipid-lowering medications at the time of hospital discharge were observed during the years under study (p for trend <0.001) (Figure 2b). On the other hand, use of calcium channel blockers has declined markedly during recent years (p for trend <0.001). The use of anticoagulants among patients who survived a first AMI increased through the mid-1990's, declined in the late 1990's, and remained stable during the 2000's (Figure 2b). ACEI/ARBs, aspirin, beta blockers, and lipid-lowering medications were prescribed at the time of hospital discharge in 94.0%, 64.4%, 90.7%, and 90.1% , respectively, of patients who survived a first AMI in 2009.
The overall (1975-2009) 1-year all-cause death rates after hospital discharge for patients who survived a first AMI were 13.9%. The average 1-year all-cause mortality rates remained relatively stable from 1975-1984 (12.9%) to 1986-1997 (12.5%), but increased during 1999-2009 (15.8%). In examining changing trends in 1-year all-cause mortality after hospital discharge, our unadjusted analyses showed that, compared with patients surviving an initial AMI in 1975-1984, there were no significant differences in the odds of dying at 1 year post discharge among patients surviving a first AMI in 1986-1997 and in 1999-2009 (Table 2).
Table 2.
Crude and multivariable adjusted odds of dying at 1-year after hospital discharge for patients who survived a first acute myocardial infarction (AMI): Worcester Heart Attack Study, 1975-2009
| Unadjusted | Adjusted for sociodemographics and comorbidities* | Further adjusted for in-hospital factors† | Further adjusted for in-hospital management‡ | Further adjusted for discharge medications§ | |
|---|---|---|---|---|---|
| Crude OR (95% CI) | Adjusted OR (95% CI) | ||||
| 1975-1984 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1986-1997 | 0.96 (0.64-1.45) | 0.72 (0.53-0.97) | 0.80 (0.60-1.08) | 1.13 (0.85-1.51) | 1.30 (0.97-1.74) |
| 1999-2009 | 1.27 (0.80-2.02) | 0.73 (0.51-1.04) | 0.82 (0.59-1.15) | 1.65 (1.25-2.17) | 2.43 (1.83-3.23) |
| 1999/2001 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2003/2005 | 0.84 (0.56-1.25) | 0.69 (0.50-0.96) | 0.68 (0.48-0.97) | 0.84 (0.60-1.17) | 0.96 (0.67-1.35) |
| 2007/2009 | 0.71 (0.46-1.08 ) | 0.62 (0.44-0.86) | 0.62 (0.47-0.83) | 0.89 (0.70-1.15) | 1.13 (0.86-1.48) |
OR: odds ratios; CI: confidence intervals
Adjusted for age, sex, race, marital status, and comorbid conditions (angina, diabetes, heart failure, hypertension, and stroke).
Adjusted for sociodemographics, comorbid conditions, AMI type, in-hospital clinical complications (atrial fibrillation, heart failure, cardiogenic shock), and hospital length of stay.
Adjusted for sociodemographics, comorbid conditions, in-hospital factors, and in-hospital management as represented by thrombolytic therapy and receipt of 3 coronary interventional procedures (cardiac catheterization, PCI, and CABG).
Adjusted for sociodemographics, comorbid conditions, in-hospital factors, in-hospital management, and prescribing of 4 guideline-recommended cardiac medications (ACE-I/ARBs, aspirin, beta blockers, and lipid lowering agents) at the time of hospital discharge.
After sequentially adjusting for several demographic characteristics, clinical factors, and in-hospital clinical complications, there were no significant differences in the odds of dying at 1 year post discharge among patients surviving an initial AMI in 1986-1997 and 1999-2009, compared with those hospitalized in 1975-1984. However, after further adjustment for hospital treatment practices, there was a borderline significant trend (p=0.08) toward an increased risk of dying at 1 year post discharge among patients hospitalized in 1986-1997; the odds of dying from all causes at 1 year post discharge was approximately 2.4 times higher in patients discharged from the hospital in 1999-2009 compared with those discharged during 1975-1984 (Table 2).
We repeated these crude and multivariable adjusted analyses in patients who were hospitalized during the most recent decade under study (1999-2009) to reflect more recent trends in long-term prognosis. The unadjusted analyses showed that, compared with patients discharged after an initial AMI in 1999/2001 (referent group), there was no significant difference in the odds of dying at 1 year post discharge among patients hospitalized in 2003/2005 and in 2007/2009 (Table 2). After controlling for several demographic characteristics, clinical factors, and inhospital complications, the odds of dying at 1 year post discharge was significantly decreased among patients hospitalized in 2003/2005 and 2007/2009, compared with those hospitalized in 1999/2001. However, after further adjustment for hospital treatment practices, there was no significant difference in the odds of dying at 1 year post discharge among patients hospitalized in 2003/2005 and in 2007/2009, in comparison with those hospitalized in 1999/2001 (Table 2).
Discussion
The results of this community-wide study suggest that there have been considerable changes in the demographic, clinical, and treatment profile of greater Worcester residents who survived their hospitalization for a first AMI at all central MA medical centers between 1975 and 2009. The hospital use of invasive coronary interventions and effective cardiac medications increased markedly over time. The average post-discharge 1-year all-cause mortality rates remained relatively stable from 1975-1984 to 1986-1997, but increased slightly during 1999-2009. Using multivariable-adjusted regression analyses, after adjustment for demographic characteristics, clinical factors, and in-hospital complications, no significant differences in the odds of dying at 1 year after hospital discharge were observed during the years under study. Once we adjusted for the receipt of various hospital treatment practices during hospitalization, however, the odds of dying at 1 year post discharge among patients hospitalized during the most recent years under study actually increased, suggesting the beneficial impact of these treatment modalities on the long-term prognosis of discharged patients.
Although several population-based studies13,19 have reported encouraging declines in the in-hospital and 30 day mortality rates in patients hospitalized with a first AMI, there are data to suggest that favorable short-term trends in mortality may not extend to patient's long-term prognosis after hospital discharge.13,19 The current investigation and several prior studies13,19 have shown that the 1-year all-cause death rates among patients discharged after a first AMI remains relatively high, emphasizing the need for continued surveillance and optimization of the medical care of these patients.
Our study showed that the unadjusted 1-year all-cause mortality rates among patients discharged from all central MA medical centers after a first AMI have actually increased in the most recent patient cohort (1999-2009), which likely reflects the increasingly older patient population with a greater prevalence of multiple comorbidities. A prior study of 285,397 patients hospitalized with a first AMI at nonfederal acute care hospitals in New Jersey between 1986 and 2007 also found that the 1-year post-discharge mortality rates increased from 12.1% in 1986 to 13.9% in 2007;13 the increased risk of dying over time was most evident in the oldest patients and were primarily due to non-cardiovascular causes of death.13 In a study of 2,816 residents of Olmsted County, MN, hospitalized with an incident AMI between 1987 and 2006, there were no changes in 1 year post-discharge mortality during the years under study.19
These findings suggest that improving the long-term outcomes of patients discharged from the hospital after a first AMI will likely require expanding the use of existing, and novel, preventive and/or therapeutic strategies in these patients after hospital discharge, and these treatment plans need to take into account the age and presence of other comorbid conditions in these patients. To effectively implement these strategies, collaboration of care management between patients and their providers, and strong partnership between cardiologists and primary care physicians, remain crucial to the success of effective post-discharge care transitions.
Consistent with the results of several population-based investigations, we showed that the use of coronary interventional procedures and effective cardiac medications has increased markedly over the past several decades.20–22 Despite the potential for confounding by indication given the nonrandomized nature of the present community-based investigation, our multivariable regression analyses showed that the increased use of invasive interventions and evidence-based pharmacotherapies was associated with increased post discharge survival among patients hospitalized for a first AMI during the most recent decade under study.
Several prior studies have examined the effects of hospital treatment practices on patient's long-term prognosis.15,16 In a study of 4,451 patients aged 35-64 years with a first AMI from the Perth MONICA cohort (1984-2005), improving trends in 1 year and longer survival were observed and were associated with an increased use of evidence-based treatments during hospitalization and in the 12 months after the index event.16 A recent study examined the use of treatment approaches and outcomes in a random sample of 1,226 patients 75 years and older who were hospitalized for AMI in Minneapolis/St. Paul, and Göteborg, Sweden in 2001-2002. The use of PCI was markedly higher in Minneapolis/St. Paul than in Göteborg, and the long-term survival at 1, 3, and 5 years was greater among patients in Minneapolis/St. Paul compared with those from Göteborg, likely related to the greater utilization of PCI.15
Although clinical trials remain the gold standard for examining treatment efficacy, data from observational studies can provide important complementary insights into the effectiveness of treatments in the broader community setting. These studies, however, often have several limitations including the lack of data on patients’ post-discharge cognitive and psychosocial status, changes in healthy lifestyle practices, and long-term adherence to evidence-based treatment after hospital discharge for AMI. Current data suggests less than optimal patient adherence to evidence-based therapies after AMI,23 and non-adherence to these effective medications has been associated with an increased risk of cardiovascular mortality.24 Inasmuch, ongoing dialogues between patients and their providers about the importance of adhering to effective pharmacotherapies on a long-term basis remain important. Future studies examining the increasing use of conventional and more novel treatment strategies, and post-discharge transitions of care, in higher-risk patients remain needed to achieve greater declines in long-term mortality in this patient population.
The strengths of the present study include its community-based design and examination of multiple decade long trends in long-term mortality rates and hospital treatment practices among hospital survivors of an initial AMI. Several limitations need to be acknowledged. Since our study only included patients who had been discharged from the hospital after an initial AMI at all central MA medical centers, one needs to be careful in extrapolating our findings to persons who died before hospitalization, or to those who reside in other geographic areas. Since our study patients were predominantly white, the generalizability of our findings to other race/ethnic groups may be limited. Our study examined pharmacotherapies prescribed at the time of hospital discharge. However, patients might have been prescribed these medications as outpatients. There is the potential for unmeasured confounding in our observed associations since we did not have information available on several patient-associated characteristics, such as income, education, psychological factors, and treatment preference, and we were unable to collect information on other factors that have been shown to affect long-term prognosis after AMI, including the severity of the AMI, and patients’ adherence to various post-discharge treatment regimens after being discharged from the hospital after a first AMI.
Acknowledgements
We are indebted to the physicians and nurses who have worked on the Worcester Heart Attack Study for the past several decades.
Grant Support: This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434). Partial salary support for Drs. Gore and Goldberg was provided for by National Institutes of Health grant 1U01HL105268-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981): the Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 2.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): the Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 4.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975-2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jneid H, Anderson JL, Wright RS, Adams CD, Bridges CR, Casey DE, Jr, Ettinger SM, Fesmire FM, Ganiats TG, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Fo. J Am Coll Cardiol. 2012;60:645–681. doi: 10.1016/j.jacc.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 6.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg RJ, Yarzebski J, Lessard D, Wu J, Gore JM. Recent trends in the incidence rates of and death rates from atrial fibrillation complicating initial acute myocardial infarction: a community-wide perspective. Am Heart J. 2002;143:519–527. doi: 10.1067/mhj.2002.120410. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Spencer F a, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009;119:1211–1219. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McManus DD, Chinali M, Saczynski JS, Gore JM, Yarzebski J, Spencer FA, Lessard D, Goldberg RJ. 30-Year Trends in Heart Failure in Patients Hospitalized With Acute Myocardial Infarction. Am J Cardiol. 2011;107:353–359. doi: 10.1016/j.amjcard.2010.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saczynski JS, Spencer FA, Gore JM, Gurwitz JH, Yarzebski J, Lessard D, Goldberg RJ. Twenty-year trends in the incidence of stroke complicating acute myocardial infarction: Worcester Heart Attack Study. Arch Intern Med. 2008;168:2104–2110. doi: 10.1001/archinte.168.19.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldberg RJ, McCormick D, Gurwitz JH, Yarzebski J, Lessard D, Gore JM. Age-related trends in short-and long-term survival after acute myocardial infarction: a 20-year population-based perspective (1975–1995). Am J Cardiol. 1998;82:1311–1317. doi: 10.1016/s0002-9149(98)00633-x. [DOI] [PubMed] [Google Scholar]
- 12.Furman M, Dauerman H, Goldberg R, Yarzebski J, Lessard D, Gore J. Twenty-two year (1975 to 1997) trends in the incidence, in-hospital and long-term case fatality rates from initial Q-wave and non-Q-wave myocardial infarction. J Am Coll Cardiol. 2001;37:1571–1580. doi: 10.1016/s0735-1097(01)01203-7. [DOI] [PubMed] [Google Scholar]
- 13.Kostis WJ, Deng Y, Pantazopoulos JS, Moreyra AE, Kostis JB. Trends in mortality of acute myocardial infarction after discharge from the hospital. Circ Cardiovasc Qual Outcomes. 2010;3:581–589. doi: 10.1161/CIRCOUTCOMES.110.957803. [DOI] [PubMed] [Google Scholar]
- 14.Tjia J, Allison J, Saczynski JS, Tisminetzky M, Givens JL, Lapane K, Lessard D, Goldberg RJ. Encouraging trends in acute myocardial infarction survival in the oldest old. Am J Med. 2013;126:798–804. doi: 10.1016/j.amjmed.2013.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith LG, Herlitz J, Karlsson T, Berger AK, Luepker R V. International comparison of treatment and long-term outcomes for acute myocardial infarction in the elderly: Minneapolis/St. Paul, MN, USA and Göteborg, Sweden. Eur Heart J. 2013;34:3191–3197. doi: 10.1093/eurheartj/eht196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Briffa T, Hickling S, Knuiman M, Hobbs M, Hung J, Sanfilippo FM, Jamrozik K, Thompson PL. Long term survival after evidence based treatment of acute myocardial infarction and revascularisation: follow-up of population based Perth MONICA cohort, 1984-2005. BMJ. 2009;338:b36. doi: 10.1136/bmj.b36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Botkin NF, Spencer FA, Goldberg RJ, Lessard D, Yarzebski J, Gore JM. Changing trends in the long-term prognosis of patients with acute myocardial infarction: a population-based perspective. Am Heart J. 2006;151:199–205. doi: 10.1016/j.ahj.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Morel JG. Logistic Regression under Complex Survey Designs. Surv Methodol. 1989;15:203–223. [Google Scholar]
- 19.Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123:259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 21.Yeh R, Sidney S, Chandra M, Sorel M, Selby J, Go A. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 22.Jernberg T, Johanson P, Held C, Svennblad B, Lindbäck J, Wallentin L. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA. 2011;305:1677–1684. doi: 10.1001/jama.2011.522. [DOI] [PubMed] [Google Scholar]
- 23.Tuppin P, Neumann A, Danchin N, de Peretti C, Weill A, Ricordeau P, Allemand H. Evidence-based pharmacotherapy after myocardial infarction in France: adherence-associated factors and relationship with 30-month mortality and rehospitalization. Arch Cardiovasc Dis. 2010;103:363–375. doi: 10.1016/j.acvd.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Ho PM, Magid DJ, Shetterly SM, Olson KL, Maddox TM, Peterson PN, Masoudi FA, Rumsfeld JS. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155:772–779. doi: 10.1016/j.ahj.2007.12.011. [DOI] [PubMed] [Google Scholar]