Abstract
Background
Sleep disruption is common in inflammatory bowel diseases (IBD). However, studies demonstrating a similar prevalence in irritable bowel syndrome (IBS) suggest that nighttime disruption due to diarrhea and abdominal pain may be key drivers of poor sleep quality. Whether inflammation is associated with poor sleep independently has not been examined previously.
Methods
This single center study included subjects with IBD recruited to an ongoing prospective registry who completed a questionnaire assessing sleep quality and mood. Inflammatory marker levels (C-reactive protein (CRP), erythrocyte sedimentation rate (ESR)) and clinical disease activity including nighttime disruption on the day of enrollment was obtained from the medical record. Logistic regression models were used to identify predictors of sleep quality.
Results
The study included 131 subjects (72 women) with a median age of IBD diagnosis of 25 years. Twenty-three subjects (19%) had a high C-reactive protein level (≥ 8mg/dL). Poor sleep was more common in those with high CRP levels than with normal values (70% vs. 39%, p=0.009). This association remained significant on multivariate analysis (Odds ratio (OR) 4.12, 95% confidence interval (CI) 1.38 – 12.29). Adjusting for the presence of nighttime disruption did not significant alter this association (OR 3.16, 95% CI 1.01 – 9.90). High CRP correlated with poor sleep even in patients not experiencing nocturnal symptoms (n=101, OR 4.89, 95% CI 1.24 – 19.36).
Conclusion
High CRP is associated with poor sleep quality in IBD independent of the presence of nighttime disruptions, suggesting a relationship exists between circulating inflammatory markers and sleep.
Keywords: sleep, inflammatory bowel disease, c-reactive protein, inflammation
INTRODUCTION
The inflammatory bowel diseases (IBD), namely Crohn’s disease (CD) and ulcerative colitis (UC), are chronic intestinal disorders that affect an estimated 1.5 million people in the United States1. IBD incurs a significant physical and financial burden on patients with many requiring hospitalization or surgery at some point during the course of their disease2. In addition, IBD also has more subtle effects on wellbeing that impairs quality of life and work productivity3, 4. Though several genetic and immunologic factors that contribute to an individual’s likelihood of contracting IBD have been uncovered, its cause remains elusive1, 5. The role of the external environment in influencing risk of disease and natural history is being increasingly recognized and several factors that increase risk of disease or influence behavior have been described from observational studies6–8. Two such risk factors that appear to have a bidirectional association with IBD, both by modifying risk and natural history of disease, but at the same time being influenced in their occurrence by inflammation and active disease, are sleep impairment and depression9–14.
Sleep problems are remarkably common in society and have been linked to a number of diseases and stressors including acute and chronic illness, physical and psychiatric disorders10, 15–20. In the context of IBD, recent work has suggested both depression and sleep impairment to be common, increase risk of relapses, and even precede a diagnosis of IBD9–14. One possible explanation for the link between depression, impaired sleep quality, and IBD would be that the former two are symptoms of exacerbations of the latter. Several studies have reported a similar prevalence of sleep disturbance in those with IBD as irritable bowel syndrome with such impairment in sleep being strongly influenced by the presence of nocturnal symptoms of diarrhea and abdominal pain in both diseases21, 22. However, impaired sleep quality may be common even in periods of clinical remission10, 21, 23. The mechanism behind such an effect is unclear but may be related to the direct effect of circulating pro-inflammatory cytokines on the central nervous system23–29. Prior studies examining impairment of sleep quality in IBD have not examined the effect of inflammation independent of disruption by nocturnal symptoms. Furthermore, they have relied mainly on use of clinical symptoms to define active disease which is open to confounding posed by the overlay of functional symptoms in such patients.
Consequently, we performed the following study in a well phenotyped IBD cohort with structured assessment of sleep and depression to examine if circulating inflammatory markers correlate with impaired sleep and mood independent of symptoms. We hypothesized that a higher inflammatory burden would result in impaired sleep independent of the presence of nocturnal symptoms.
METHODS
Study Population
This was a single center study that included subjects recruited to the ongoing Prospective Registry for IBD Study at Massachusetts General Hospital (PRISM). Subjects include adults 18 years or older, with CD or UC diagnosed by their treating gastroenterologist according to accepted criteria. After providing informed consent, patients completed their enrollment by providing details regarding demographics, disease and treatment history. Disease diagnosis, location, and phenotype were confirmed by the treating gastroenterologist. Patient information on intake questionnaires was supplemented by review of the electronic medical records.
Assessment of sleep, depression, and inflammatory markers
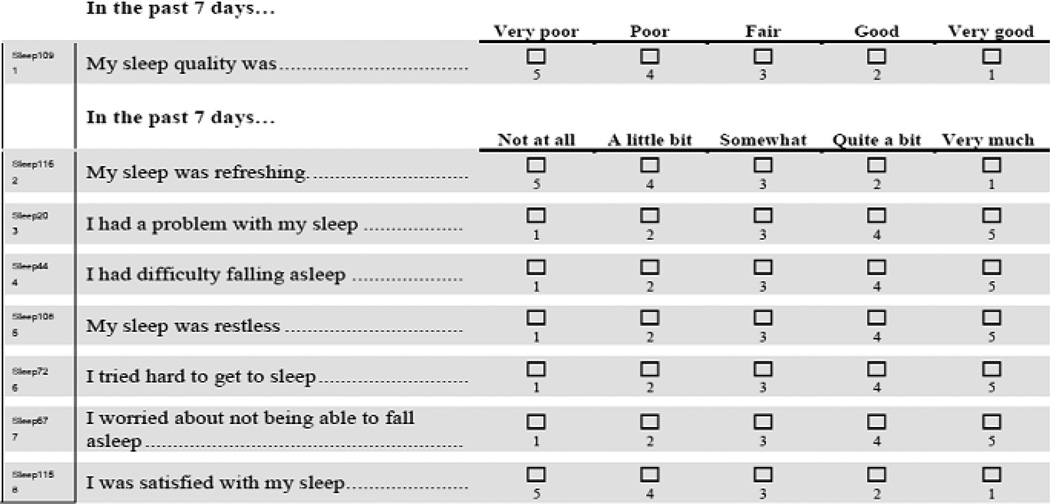
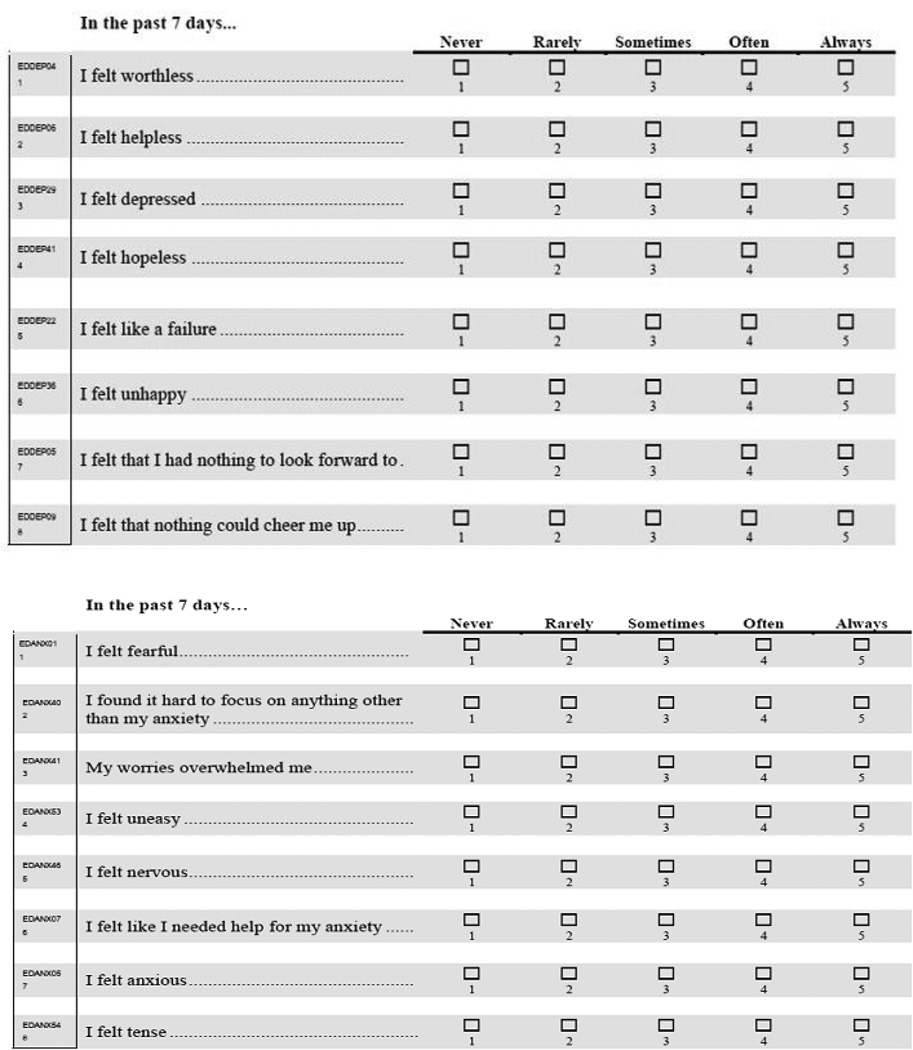
A consecutive subset of patients who were enrolled in PRISM was invited to complete an 8-item questionnaire regarding their sleep quality and a 16-item questionnaire regarding their mood. These questions were derived from the National Institutes of Health (NIH) Patient-Reported Outcome Measurement Information System (PROMIS) bank of questions (www.nihpromis.org, Accessed 10 May 2014)30, 31. Details about their derivation have been published previously. In brief, these questions are developed from an initial pool of items identified from candidate citations that were pilot tested in a national sample of participants. Items from the PROMIS question bank have demonstrated validity in the areas of content, construct, criterion, and responsiveness. For the purpose of this study, patients were asked questions regarding their sleep quality and mood, both encompassing the past seven days (Appendix 1). The questionnaires were scored per standard procedures recommended for scoring the PROMIS questions with higher values representing greater impairment of sleep quality or more depressed mood30, 31. Values above the median for the cohort indicated poor sleep or depressed mood.
Objective assessment of inflammatory activity included the erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP). Only subjects who had these values measured on the day they filled out the sleep and mood questionnaires were included in the study. ESR and CRP levels were defined as being elevated when they were above 20mm/hr and 8mg/dL respectively in accordance with normal values for our laboratory.
Covariates
Information on each subject’s sex, age at diagnosis, duration of disease, and smoking status was assessed by medical records review, self-report, and enrollment interview by a trained research coordinator. Disease location and behavior in CD and disease extent in UC was classified according to the Montreal classification32. Use of medications including immunomodulators (azathioprine, 6-mercaptopurine, methotrexate) and anti-tumor necrosis factor-α biologics (anti-TNF; infliximab, adalimumab, certolizumab pegol) was obtained. Disease activity was recorded based on their physician assessment of their symptoms on the day they completed the sleep and mood questionnaires. Patients were classified as having clinically active disease or in remission by the treating gastroenterologist, and the presence of nighttime symptoms in the week prior to the visit was noted.
Statistical Analysis
Continuous variables were summarized using means and standard deviations with use of medians and interquartile ranges (IQR) when skewed. Categorical variables were expressed as proportions. In our primary analysis, we performed univariate logistic regression models with poor sleep defined as values above the median as a dichotomous outcome. Variables that were found to have a statistically significant effect at p < 0.2 were included in our multivariate logistic regression model examining the association between elevated inflammatory markers and poor sleep adjusting for relevant confounders. To test the robustness of our findings, we repeated the analysis using a linear regression model with the sleep score as a continuous variable. Subgroup analyses were performed excluding those with nocturnal symptoms, and on including the presence of nocturnal symptoms in the multivariate model to see if the association between inflammation and sleep was mediated through nighttime sleep disruption. Data was analyzed using Stata 13.0 (StataCorp, College Station, TX). The Institutional Review Board of Partners Healthcare approved this study.
RESULTS
A total of 131 patients (78 CD; 53 UC) who had completed questionnaires on sleep and mood and had concurrent serum inflammatory markers available were included in this study (Table 1). The median age of diagnosis was 25 years (interquartile range (IQR) 18 – 37 years) and a slight majority (55%) of the cohort was female. Among those with CD, a third had inflammatory disease (37%) while 22% and 41% had stricturing or penetrating disease phenotype respectively. Two-thirds of those with UC had pancolitis (68%). Twenty-nine patients had at least one IBD-related surgery (22%) and seventy-three had current or past use of anti-TNF therapy (56%). None of the patients had obstructive sleep apnea or other diagnosed disorders of sleep. None were on prescription antidepressants or sleep aids.
Table 1.
Characteristics of the study population
| Characteristic | N (%) |
|---|---|
| Age at Diagnosis (years) [Median(IQR)] | 25 (18 – 37) |
| Type of IBD | |
| Crohn’s Disease | 78 (60) |
| Ulcerative Colitis | 53 (40) |
| Sex | |
| Male | 59 (45) |
| Female | 72 (55) |
| Smoking History | |
| None | 87 (67) |
| Former | 36 (28) |
| Current | 6 (5) |
| Prior Surgery | |
| None | 102 (78) |
| Prior Surgery | 29 (22) |
| Family History of IBD | |
| No | 103 (79) |
| Yes | 28 (21) |
| Anti-TNF Use | |
| None | 58 (44) |
| Prior or Current | 73 (56) |
| Sleep Score [Median(IQR)] | 10 (5 – 16) |
| Depression Score [Median(IQR)] | 5 (1 – 14) |
| ESR (mm/hr) [Median(IQR)] | 8 (5 – 16) |
| C-reactive protein (mg/dL) [Median(IQR)] | 2.1 (0.8 – 6.2) |
IQR – interquartile range; Anti-TNF – monoclonal antibodies to tumor necrosis factor α (infliximab, adalimumab, certolizumab pegol); ESR – erythrocyte sedimentation rate; IBD – inflammatory bowel diseases
Sleep was assessed using an 8-item questionnaire and depression through a 16-item questionnaire from the NIH PROMIS question bank
The median CRP and ESR levels of patients were 2 mg/dL (IQR 0.8 – 6.2) and 8mm/hr (IQR 5 – 16) with good correlation between the two inflammatory markers (correlation co-efficient ρ=0.57, p < 0.001). Twenty-three patients (19%) had an elevated CRP and 35 patients (26%) had an elevated ESR. The median sleep score in our cohort was 10 (IQR 5 – 16). Fifty-nine subjects (44%) who had sleep scores above the median were consider to have poor sleep. The median mood score was 5 (IQR 1 – 14). Fifty-five patients (42%) were clinically active and the remaining 58% were in clinical remission. The mean CRP level in those with clinical active disease was significantly greater than those in remission (12.3mg/dL vs. 2.9mg/dL, p=0.0013).
Predictors of impaired sleep
Poor sleep was more common in those with high CRP levels than with normal values (70% vs. 39%, Odds ratio (OR) 3.52, 95% CI 1.33 – 9.33, p=0.009). Similarly, presence of clinically active disease (OR 3.96, 95% CI 1.89 – 8.27) was associated with poor sleep. However, we did not find an association between an elevated ESR and poor sleep (OR 1.72, 95% CI 0.79 – 3.75) (Table 2). Type of IBD, age at diagnosis, gender, disease phenotype, prior surgery, and need for anti-TNF therapy were also not associated with poor sleep. Each 1-point increase in the depression score was associated with increased likelihood of poor sleep (OR 1.10, 95% CI 1.05 – 1.15). There was no difference in BMI between those with poor sleep (25.6kg/m2) compared to those with normal sleep (26.3kg/m2, p=0.57). Since neither IBD type nor phenotype was found to have a significant effect on sleep, further analyses pooled together all subjects.
Table 2.
Univariate analysis of factors associated with poor sleep in patients with inflammatory bowel diseases
| Characteristic | Odds ratio (95% confidence interval) |
|---|---|
| Age at Diagnosis | 0.99 (0.96 – 1.01) |
| Type of IBD | |
| Crohn’s Disease | 1.0 |
| Ulcerative Colitis | 1.07 (0.53 – 2.16) |
| Sex | |
| Male | 1.0 |
| Female | 1.15 (0.57 – 2.30) |
| Smoking History | |
| None | 1.0 |
| Ever | 1.63 (0.78 – 3.43) |
| Prior Surgery | |
| None | 1.0 |
| Prior Surgery | 1.23 (0.54 – 2.81) |
| Anti-TNF Usage | |
| None | 1.0 |
| Prior or Current | 0.96 (0.48 – 1.92) |
| Depression Score | 1.10 (1.05 – 1.15) |
| High C-reactive protein | 3.52 (1.33 – 9.33) |
| High ESR | 1.72 (0.79 – 3.75) |
| Clinically active disease | 3.96 (1.89 – 8.27) |
In a multivariate logistic regression model, only high CRP (4.12, 95% CI 1.38 – 12.29) and increasing depression score (OR 1.10, 95% CI 1.05 – 1.15) were independently associated with poor sleep quality. As there was a high degree of co-linearity between clinically active disease and elevated CRP (81% of those with clinically active disease also had a high CRP, ρ=0.36, p < 0.001), we were not able to include them in the same multivariate model. Examining the sleep score as a continuous variable, elevated CRP was associated with a 3 point higher sleep score when adjusting for potential confounders (+3.2 points, 95% CI +0.31 to + 6.13).
To examine if the association with elevated CRP was mediated through the presence of nighttime symptoms and sleep disruption, we repeated the multivariate analysis in those who reported no nocturnal symptoms (n=101). High CRP remained independently associated with poor sleep quality in this cohort (OR 4.89, 95% I 1.24 – 19.36) when adjusting for depression and smoking status. The association between elevated CRP and poor sleep also remained independent of nocturnal symptoms when adjusting for it in the multivariate model (OR 3.16, 95% CI 1.01 – 9.90).
DISCUSSION
Sleep impacts chronic inflammation15, 17, 23, 26, 28, 29, 33, 34. In relevance to IBD, impaired sleep quality is common and is associated with disease activity10, 13, 21, 22, 25, 35, 36. However, to what extent impairment in sleep quality is due to frequent nocturnal disruptions from symptoms compared to an effect of a systemic pro-inflammatory state is unclear. In this study, we demonstrate that elevated C-reactive protein, a circulating marker of systemic inflammation, is independently associated with impaired sleep quality even in the absence of nocturnal symptoms, supporting a role for inflammation in disrupting sleep in IBD.
The role of sleep in patients with IBD is an area receiving increasing attention10, 25, 36–39. In comparison to healthy controls, patients with IBD report significantly greater sleep impairment21, 22. However in several studies, the impairment of sleep quality in IBD is similar to those with IBS, a chronic gastrointestinal disorder without overt systemic inflammation21, 22 questioning the relative contribution of symptoms and inflammation. Ranjbaran et al. administered the Pittsburgh Sleep Quality Index (PSQI), a validated measure of sleep quality, to 205 subjects including 80 with inactive IBD and 24 with IBS. Both subjects with IBD and IBS reported increased sleep latency and greater frequency of sleep interruption (IBD 70%, IBS 88%)22. In addition, the most common reason for poor sleep quality due to frequent awakening at night was the need to use the bathroom (81% in IBD and 87% of IBS) and abdominal pain (44% of IBD and 71% of IBS). This is consistent with other studies where symptomatic disease activity in IBD was the strongest predictor of impairment of sleep10.
Intriguing epidemiology and laboratory data support a bidirectional association between sleep and disease activity and an impact of circulating inflammatory markers on sleep quality. In a large prospective cohort study including 151,871 women followed over 24 years, we demonstrated that both short and long duration of sleep was independently associated with increased risk of incident UC35. In a different cohort, while disease related symptoms was a key determinant of impaired sleep quality, poor sleep even during remission was associated with an increased risk of symptomatic disease flares at 6 months10. Experimentally, interleukin-6 (IL-6), interleukin-1 (IL-1), and tumor necrosis factor (TNF) directly induces fatigue and sleep22–24, 38–40. Intravenous or intra-cerebroventricular injections of recombinant TNF suppresses rapid-eye-movement (REM sleep)34. In contrast, antibodies against TNF-α improve sleep quality when administered to patients with juvenile idiopathic arthritis41. In our present study, we were not able to examine the association between CRP and sleep quality independent of clinical disease activity as most patients with an elevated CRP also had clinically active disease. Sleep fragmentation has been associated with increased inflammatory cytokines in mouse models and human studies42–44. In this study, we were able to demonstrate that the sleep disruption in IBD is not solely due to nighttime disruptions symptoms as noted in previous studies22 since the association between elevated CRP and poor sleep persisted in the group with no reported nocturnal symptoms.
Another significant association in our study is the relationship between sleep and depression. Large studies have found that symptoms of depression are most likely to be experienced by individuals who sleep either too little or too much, and decreased sleep quality is directly associated with depressive symptoms27, 45–47. In a cohort study including 3,173 patients in the Crohn’s and Colitis Foundation of America’s (CCFA) Partners cohort, co-existing depression was a strong predictor of impaired sleep quality10. Depression has been associated with increased risk of incident disease as well as disease relapses9, 12–14, 46, acting independently through various mechanisms including elevation of circulating inflammatory markers, alteration of the function and number of CD4 and CD8 lymphocytes, and through its effect of the autonomic nervous system and hypothalamus-pituitary-adrenal axis23, 29, 36–38. Despite the co-existence of the two, the association between sleep and CRP persists after adjustment for mood suggesting that these two related factors potentially exert independent effects.
Our study has several strengths and implications. Use of validated sleep measures such as the NIH PROMIS question bank increases the face validity of our assessment of sleep quality and mood. The NIH PROMIS bank of questions have been carefully validated and are reliable for use either in the aggregate with the entire bank of questions, or with inclusion of specific question sets like the 8-item question bank used for the purpose of this study. While other sleep questionnaires like the Pittsburgh Sleep Quality Index (PSQI) may be more widely studied and validated, in a previous study, we demonstrated a strong correlation (co-efficient 0.80, p < 0.0001) between the two questionnaires10, despite differing time periods of study. Additionally, in a previous study, 82% of patients with a T-score above the median also had an abnormal score on the Pittsburgh Sleep Quality Index, validating this cut-off threshold10. For the purpose of this study, night time disruption was assessed without formal structured questionnaires during the clinical encounter. Future studies may need to develop more nuanced methods to identify nighttime disruption due to active symptoms. Additionally, our focus on objective inflammatory markers provides greater certainty as to the presence of active disease in our subjects as opposed to symptom based disease activity scores. Reliance on symptoms may be open to confounding by co-existing functional symptoms. Additionally, objective inflammatory markers also allow us to potentially identify an effect of subclinical active disease as well. Few of the patients were on systemic steroids at the time of completion of this questionnaire. We did not have routine information on extraintestinal symptoms at the time of completion of this questionnaire. However, we do not believe either of these two variables to have differentially affected the association observed in our study. In conjunction with prior literature, our findings support an association between disease activity and sleep in IBD that is not solely due to nighttime awakenings and may be mediated by systemic inflammation. Further studies examining such an effect independent of clinical symptoms and in those with subclinical active disease are warranted. As well, our findings support the importance of routinely assessing sleep duration, quality, and disruption in patients with IBD. Whether this needs to be addressed through behavioral modification or requires pharmacologic therapy, and the impact of such interventions on longitudinal disease activity require further study. There is also an important unmet need to address the impact of nighttime disruption on next day cognitive and psychomotor functioning in patients with IBD.
We acknowledge several limitations to our study that strengthen the necessity for further research in this field. Our study was done at a single referral IBD center and consequently may be skewed towards more severe disease. Our sample size was small but remains one of the largest studies to examine correlation between sleep and C-reactive protein in IBD. As the vast majority of patients who had an elevated C-reactive protein also had clinical symptoms, we were not able to independently examine the effect of symptoms and CRP on sleep quality. Small prospective cohorts have suggested an association between histologic inflammation and sleep quality suggesting that clinically latent disease may have an impact of sleep quality25. Larger studies are required to robustly demonstrate this finding. Nocturnal disruptions were noted through review of the medical records, and consequently may have resulted in misclassification. However, one would expect such misclassification to bias towards the null, supporting the robustness of our findings. We did not have information on use of sleep aids or other medications that may influence sleep quality.
In conclusion, we demonstrate that elevated C-reactive protein levels were associated with impaired sleep quality in patients with inflammatory bowel disease, and this association was independent of the presence of nocturnal symptoms. This suggests that nighttime disruption of sleep is not the sole mechanism for poor sleep quality in patients with IBD and further studies examining the bidirectional association between sleep and inflammation in IBD are warranted.
Acknowledgements
Source of funding: This work is supported by the National Institutes of Health (NIH) (P30 DK043351) to the Center for Study of Inflammatory Bowel Diseases. Ananthakrishnan is supported in part by a grant from the National Institutes of Health (K23 DK097142).
We acknowledge the valuable contributions of the participants and the research staff of our registry.
Appendix 1: Assessment of sleep and mood using the NIH PROMIS questions
Sleep Habits
Mood
Footnotes
Financial Conflicts of Interest: None
This work was presented as a poster at the American College of Gastroenterology Annual Meeting 2014, Philadelphia, PA.
REFERENCES
- 1.Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–2078. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernstein CN, Loftus EV, Jr, Ng SC, et al. Hospitalisations and surgery in Crohn's disease. Gut. 2012;61:622–629. doi: 10.1136/gutjnl-2011-301397. [DOI] [PubMed] [Google Scholar]
- 3.Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: Results of the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007;1:10–20. doi: 10.1016/j.crohns.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Ananthakrishnan AN, Weber LR, Knox JF, et al. Permanent work disability in Crohn's disease. Am J Gastroenterol. 2008;103:154–161. doi: 10.1111/j.1572-0241.2007.01561.x. [DOI] [PubMed] [Google Scholar]
- 5.Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cosnes J, Gower-Rousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785–1794. doi: 10.1053/j.gastro.2011.01.055. [DOI] [PubMed] [Google Scholar]
- 7.Danese S, Fiocchi C. Etiopathogenesis of inflammatory bowel diseases. World J Gastroenterol. 2006;12:4807–4812. doi: 10.3748/wjg.v12.i30.4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ananthakrishnan AN. Environmental Risk Factors for Inflammatory Bowel Diseases: A Review. Dig Dis Sci. 2014 doi: 10.1007/s10620-014-3350-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ananthakrishnan AN, Khalili H, Pan A, et al. Association between depressive symptoms and incidence of Crohn's disease and ulcerative colitis: results from the Nurses' Health Study. Clin Gastroenterol Hepatol. 2013;11:57–62. doi: 10.1016/j.cgh.2012.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ananthakrishnan AN, Long MD, Martin CF, et al. Sleep disturbance and risk of active disease in patients with Crohn's disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2013;11:965–971. doi: 10.1016/j.cgh.2013.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernstein CN, Singh S, Graff LA, et al. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010;105:1994–2002. doi: 10.1038/ajg.2010.140. [DOI] [PubMed] [Google Scholar]
- 12.Bitton A, Dobkin PL, Edwardes MD, et al. Predicting relapse in Crohn's disease: a biopsychosocial model. Gut. 2008;57:1386–1392. doi: 10.1136/gut.2007.134817. [DOI] [PubMed] [Google Scholar]
- 13.Graff LA, Vincent N, Walker JR, et al. A population-based study of fatigue and sleep difficulties in inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:1882–1889. doi: 10.1002/ibd.21580. [DOI] [PubMed] [Google Scholar]
- 14.Singh S, Graff LA, Bernstein CN. Do NSAIDs, antibiotics, infections, or stress trigger flares in IBD? Am J Gastroenterol. 2009;104:1298–1313. doi: 10.1038/ajg.2009.15. quiz 1314. [DOI] [PubMed] [Google Scholar]
- 15.Abad VC, Sarinas PS, Guilleminault C. Sleep and rheumatologic disorders. Sleep Med Rev. 2008;12:211–228. doi: 10.1016/j.smrv.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 17.Brass SD, Duquette P, Proulx-Therrien J, et al. Sleep disorders in patients with multiple sclerosis. Sleep Med Rev. 2010;14:121–129. doi: 10.1016/j.smrv.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Cappuccio FP, Cooper D, D'Elia L, et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 19.Cappuccio FP, D'Elia L, Strazzullo P, et al. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandrasekhara PK, Jayachandran NV, Rajasekhar L, et al. The prevalence and associations of sleep disturbances in patients with systemic lupus erythematosus. Mod Rheumatol. 2009;19:407–415. doi: 10.1007/s10165-009-0185-x. [DOI] [PubMed] [Google Scholar]
- 21.Keefer L, Stepanski EJ, Ranjbaran Z, et al. An initial report of sleep disturbance in inactive inflammatory bowel disease. J Clin Sleep Med. 2006;2:409–416. [PubMed] [Google Scholar]
- 22.Ranjbaran Z, Keefer L, Farhadi A, et al. Impact of sleep disturbances in inflammatory bowel disease. J Gastroenterol Hepatol. 2007;22:1748–1753. doi: 10.1111/j.1440-1746.2006.04820.x. [DOI] [PubMed] [Google Scholar]
- 23.Ranjbaran Z, Keefer L, Stepanski E, et al. The relevance of sleep abnormalities to chronic inflammatory conditions. Inflamm Res. 2007;56:51–57. doi: 10.1007/s00011-006-6067-1. [DOI] [PubMed] [Google Scholar]
- 24.Abedelmalek S, Souissi N, Chtourou H, et al. Effects of partial sleep deprivation on proinflammatory cytokines, growth hormone, and steroid hormone concentrations during repeated brief sprint interval exercise. Chronobiol Int. 2013;30:502–509. doi: 10.3109/07420528.2012.742102. [DOI] [PubMed] [Google Scholar]
- 25.Ali T, Madhoun MF, Orr WC, et al. Assessment of the relationship between quality of sleep and disease activity in inflammatory bowel disease patients. Inflamm Bowel Dis. 2013;19:2440–2443. doi: 10.1097/MIB.0b013e3182a0ea54. [DOI] [PubMed] [Google Scholar]
- 26.Axelsson J, Rehman JU, Akerstedt T, et al. Effects of sustained sleep restriction on mitogen-stimulated cytokines, chemokines and T helper 1/ T helper 2 balance in humans. PLoS One. 2013;8:e82291. doi: 10.1371/journal.pone.0082291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–528. [PMC free article] [PubMed] [Google Scholar]
- 28.Fragiadaki K, Tektonidou MG, Konsta M, et al. Sleep disturbances and interleukin 6 receptor inhibition in rheumatoid arthritis. J Rheumatol. 2012;39:60–62. doi: 10.3899/jrheum.110617. [DOI] [PubMed] [Google Scholar]
- 29.Rohleder N, Aringer M, Boentert M. Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci. 2012;1261:88–96. doi: 10.1111/j.1749-6632.2012.06634.x. [DOI] [PubMed] [Google Scholar]
- 30.Buysse DJ, Yu L, Moul DE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33:781–792. doi: 10.1093/sleep/33.6.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu L, Buysse DJ, Germain A, et al. Development of short forms from the PROMIS sleep disturbance and Sleep-Related Impairment item banks. Behav Sleep Med. 2012;10:6–24. doi: 10.1080/15402002.2012.636266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19(Suppl A):5–36. doi: 10.1155/2005/269076. [DOI] [PubMed] [Google Scholar]
- 33.Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32:200–204. doi: 10.1093/sleep/32.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shoham S, Davenne D, Cady AB, et al. Recombinant tumor necrosis factor and interleukin 1 enhance slow-wave sleep. Am J Physiol. 1987;253:R142–R149. doi: 10.1152/ajpregu.1987.253.1.R142. [DOI] [PubMed] [Google Scholar]
- 35.Ananthakrishnan AN, Khalili H, Konijeti GG, et al. Sleep Duration Affects Risk for Ulcerative Colitis: A Prospective Cohort Study. Clin Gastroenterol Hepatol. 2014 doi: 10.1016/j.cgh.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parekh PJ, Oldfield Iv EC, Challapallisri V, et al. Sleep Disorders and Inflammatory Disease Activity: Chicken or the Egg? Am J Gastroenterol. 2014 doi: 10.1038/ajg.2014.247. [DOI] [PubMed] [Google Scholar]
- 37.Simpson N, Dinges DF. Sleep and inflammation. Nutr Rev. 2007;65:S244–S252. doi: 10.1111/j.1753-4887.2007.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 38.Swanson GR, Burgess HJ, Keshavarzian A. Sleep disturbances and inflammatory bowel disease: a potential trigger for disease flare? Expert Rev Clin Immunol. 2011;7:29–36. doi: 10.1586/eci.10.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tang Y, Preuss F, Turek FW, et al. Sleep deprivation worsens inflammation and delays recovery in a mouse model of colitis. Sleep Med. 2009;10:597–603. doi: 10.1016/j.sleep.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swanson G, Forsyth CB, Tang Y, et al. Role of intestinal circadian genes in alcohol-induced gut leakiness. Alcohol Clin Exp Res. 2012;35:1305–1314. doi: 10.1111/j.1530-0277.2011.01466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ruperto N, Lovell DJ, Li T, et al. Abatacept improves health-related quality of life, pain, sleep quality, and daily participation in subjects with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken) 2010;62:1542–1551. doi: 10.1002/acr.20283. [DOI] [PubMed] [Google Scholar]
- 42.Ali T, Choe J, Awab A, et al. Sleep, immunity and inflammation in gastrointestinal disorders. World J Gastroenterol. 2013;19:9231–9239. doi: 10.3748/wjg.v19.i48.9231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tobaldini E, Cogliati C, Fiorelli EM, et al. One night on-call: sleep deprivation affects cardiac autonomic control and inflammation in physicians. Eur J Intern Med. 2013;24:664–670. doi: 10.1016/j.ejim.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 44.Trammell RA, Verhulst S, Toth LA. Effects of sleep fragmentation on sleep and markers of inflammation in mice. Comp Med. 2014;64:13–24. [PMC free article] [PubMed] [Google Scholar]
- 45.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 46.Graff LA, Walker JR, Bernstein CN. Depression and anxiety in inflammatory bowel disease: a review of comorbidity and management. Inflamm Bowel Dis. 2009;15:1105–1118. doi: 10.1002/ibd.20873. [DOI] [PubMed] [Google Scholar]
- 47.Sutton EL. Psychiatric disorders and sleep issues. Med Clin North Am. 2014;98:1123–1143. doi: 10.1016/j.mcna.2014.06.009. [DOI] [PubMed] [Google Scholar]