Abstract
Background
More frequent cooking at home may help improve diet quality and be associated with food values, particularly for individuals participating in the Supplemental Nutrition Assistance Program (SNAP).
Objective
To examine patterns of fruit and vegetable consumption and food values among adults (aged 20 and older) in the United States, by SNAP participation and household cooking frequency.
Methods
Analysis of cross-sectional 24-hour dietary recall data obtained from the National Health and Nutrition Examination Survey 2007-2010 (N=9,560).
Results
A lower percentage of SNAP participants consumed fruit (total: 35% vs. 46%, p=0.001; fresh: 30% vs. 41%, p<0.001) and vegetables (total: 49% vs. 58%, p=0.004; fresh: 35% vs. 47%, p<0.001) than those ineligible for SNAP. Among SNAP participants, cooking > 6 times/week was associated with greater vegetable consumption compared to cooking < 2 times/week (175 grams vs. 98 grams, p=0.003). SNAP-eligible individuals who cooked ≥ 2 times/week were more to report price (medium cookers: 47% vs. 33%, p=0.001; high cookers: 52% vs. 40%, p<0.001), ease of preparation (medium cookers: 36% vs. 28%, p=0.002; high cookers: 36% vs. 24%, p<0.001) and how long food keeps (medium cookers: 57% vs. 45%, p<0.001; high cookers: 61% vs. 50%, p<0.001) as important compared to SNAP-ineligible individuals.
Conclusions
Fruit and vegetable consumption in the United States is low regardless of cooking frequency. Efforts to improve diet quality should consider values on which food purchases are based.
INTRODUCTION
In response to persistently high rates of obesity and associated weight-related diseases,1-3 particularly among low-income populations,4 the potential for home cooking to improve diet quality is attracting increasing interest in the United States.5-11 Foods consumed at home and greater cooking frequency are, on average, associated with better diet quality.12-14 Although Americans spend less time cooking than in the past,10, 15-17 across all income groups people report cooking frequently (5 times/week).13
The Supplemental Nutrition Assistance Program (SNAP) provided more than $75 billion in benefits to approximately 47 million Americans in 2013.18 As SNAP transitioned from a primary focus on reducing hunger and food insecurity, funding for SNAP education (SNAP-Ed), SNAP's obesity prevention and nutrition education initiative, increased from $661 thousand when it began in 1992 to $379 million in 2010.19 SNAP-Ed aims to help participants make healthy food choices within their limited budget, including increasing fresh fruits and vegetable consumption, a key goal of the Dietary Guidelines for Americans.20, 21 Encouraging home cooking is a key strategy for achieving this goal, and in addition to other program activities, SNAP-Ed catalogues budget friendly recipes targeted to participants on their website.22 Findings regarding the relationship between SNAP participation and diet quality are mixed; some evidence indicates that SNAP participation improves diet quality,23, 24 and increases fruit and vegetable consumption23 whereas other studies show the opposite.25-27
Numerous interventions focus on increasing access to fruits and vegetables, and promoting healthy eating though educational programs including cooking classes.6, 28-39 These programs often target low-income Americans who typically consume fewer fruits and vegetables. However, all Americans, regardless of income, do not consume the recommended daily servings of fruits and vegetables.27, 40-43 Prior research indicates that cooking frequency, complexity, and confidence are associated with increased fruit and vegetable consumption.44-46 In contrast, other evidence suggests that more time spent cooking is not associated with increased vegetable consumption.9
Food values (beliefs which motivate food selections) may, in turn, influence the decision to cook. The values which shape food choices (taste, price, convenience, quality, nutrition)47, 48 are similar to commonly cited barriers to healthy home cooking – time, price, convenience and cooking knowledge/skills and confidence.49-51 Evidence about whether individual values related to food purchasing differ by cooking frequency is missing from the literature.
The primary purpose of this descriptive study is to examine patterns of fruit and vegetable consumption among U.S. adults by SNAP status and cooking frequency. We additionally describe differences in food purchase values by SNAP status and cooking frequency. The key contributions of this study are updating prior estimates of fruit and vegetable consumption by SNAP status and examination of whether this relationship is modified by cooking frequency. A better understanding in this area may identify modifiable behavioral targets to increase the frequency of cooking at home, particularly among low-income Americans who are eligible for SNAP.
METHODS
Data and design
Data was obtained by combining two waves of data collection (2007-2008 and 2009-2010) from the National Health and Nutrition Examination Survey (NHANES). The NHANES is a cross-sectional, nationally representative, population-based survey designed to collect information on the health status, nutritional intake and health-related behaviors of the U.S. population. Participants are selected based on a multi-stage, clustered, probability sampling strategy.52 A complete description of data-collection procedures and analytic guidelines are available elsewhere (www.cdc.gov/nchs/nhanes.htm). Analysis was restricted to data from 2007-2010 based on the availability of key variables of interest.
Study Sample
The study sample included adults aged 20 and older with complete and reliable single 24-hour dietary recalls (as determined by the NHANES staff). Survey respondents were excluded if they were pregnant or had diabetes at the time of data collection (N=1,491) due to differences in dietary requirements for these groups compared to the general population. We also excluded individuals from analysis who lacked complete information on the key independent variables of interest (defined in detail below): nine individuals who responded with a cooking frequency greater than 7 days, 112 individuals with missing values for cooking frequency, and nine individuals with missing information on SNAP status were excluded from analysis. Missingness for both cooking frequency and SNAP status represented 0.01% of the total sample. The final analytic sample included 9,560 adults all of whom had complete cooking frequency, SNAP status and dietary recall data.
Measures
Cooking Frequency Status
Cooking frequency was assessed by the survey question, “During the past seven days, how many times did you or someone else in your family cook food for dinner or supper at home?” Household cooking frequency was categorized into three groups based on the definition in the existing literature:11, 13 low (0 to 1 times, N=802), medium (2 to 5 times, N=3,704) and high (6 to 7 times, N=5,063).
SNAP Status
SNAP eligibility is determined by having a household income ≤130% of the federal poverty level (FPL) and $2000 in countable assets.53 Consistent with prior literature, SNAP status was defined three ways based on self-reported SNAP participation and self-reported household income: 1) receiving SNAP; 2) income-eligible but not receiving SNAP; and 3) income-ineligible for SNAP.54
Fruit and Vegetable Consumption
Fruits and vegetables were defined two ways; 1) total fruits/vegetables including raw, fresh, frozen, canned, dried and pickled, 2) fresh fruits/vegetables including only raw or cooked from raw. White potatoes and sauces (e.g. tomato sauce) were excluded from the vegetable category. White potatoes and tomato sauce comprise almost half of average daily vegetable consumption in the U.S.42 Potatoes and tomato sauce are associated with higher intake of sodium and total calories.42 By excluding potatoes and tomato sauce from our analysis we restrict our vegetable category to other vegetables associated with higher fiber and low caloric intake, the increased consumption of which is recommended by the Dietary Guidelines for Americans.21 For complete fruit and vegetable definitions see Appendix A.
Food Purchase Values
Food purchase values were based on responses to questions assessing the importance of several domains (price, nutrition, taste, ease of food preparation, how well food keeps) related to food purchasing. Thus, food purchase values refer to how important the above are to individuals when making decisions about what food to purchase. Response categories to these survey questions were very important, somewhat important, not too important, or not at all important. Food purchase values were dichotomized as very important vs. otherwise based on the cut points in the data. Twenty percent of individuals in the dataset were excluded from the analysis due to missing information for all food values. The outcomes of fruit and vegetable consumption (percent of people consuming and volume of consumption) did not differ systematically between individuals with complete food values data and those without with the exception of the percent of people consuming total fruit (which was higher in the group with complete information on food values, p=0.01).
Socioeconomic and Demographic Study Covariates
Covariates for this analysis included gender, race/ethnicity (non-Hispanic white, non-Hispanic Black, Hispanic, other), age (20-44, 45-64, ≥65), education (<high school, high school or GED, >high school), marital status (married, not currently married), employment status (not employed, part time (1-34 hours), and full time (≥35 hours)), country of birth (US born, born in another country), household size, (1-3 person household, ≥4 person household) and household food security. Household food security is measured in NHANES via an 18-question questionnaire and then categorized (by the NHANES staff) based on those measures into four categories: full, marginal, low and very low food security.55 For this analysis, the low and very low categories were collapsed based on cut points in the data.
Analysis
All analyses used appropriate survey weights to account for the unequal probability of being selected due to the complex sampling strategy employed by NHANES, non-response or incomplete dietary recall data and whether the dietary recall was recorded on a weekend or weekday. The “svyset” and “svy” STATA commands were used to adjust for weights, primary sampling units and strata in order to account for the complex survey design. Analyses were performed using STATA, version 12 (StataCorp, L.P. College Station, TX). Multivariate logistic models, adjusted for the covariates described above, were used to estimate the relationship between SNAP status and the probability of consuming any fruits and vegetables (total or fresh). Next, an interaction term between cooking frequency and SNAP status was added to see if cooking frequency modifies the probability of consuming fruits or vegetables. Generalized linear models including the interaction between SNAP status and cooking frequency and covariates described above were then used to examine the relationship between household cooking frequency, SNAP status and volume of fruit and vegetable consumption (among consumers).
Finally, SNAP participants and income eligible non-participants were combined into one category to compare SNAP eligible (≤130% FPL) and SNAP ineligible (>130% FPL) individuals. Multivariate logistic models including an interaction term between cooking frequency and SNAP eligibility were estimated with the food values as outcomes measures. All covariates were included based on prior literature, regardless of significance.11, 44 We additionally replicated the above analyses with pregnant women and individuals with diabetes included in the sample. Significance of all differences between groups was considered at p<0.05, and all tests were two-sided. Tables and figures report predicted probabilities or predicted means based on the adjusted models.
RESULTS
Table 1 presents the characteristics of the study sample overall and by SNAP participation status. Among American adults 20 years or older in 2007-2010, 9 percent received SNAP benefits, 11 percent were eligible to participate in SNAP but did not, and 80 percent were ineligible to participate in SNAP. Nine percent of SNAP participants, 11 percent of eligible non-participants and 7 percent of ineligible non-participants cooked dinner 0-1 times/week. Two-thirds (62%) of SNAP participants cooked dinner 6-7 times/week compared with 46 percent of ineligible non-participants. SNAP participants were more likely to be female, younger, and were more likely to be from households with four or more members.
TABLE 1.
Characteristics of US adults (aged ≥20 y) in the National Health and Nutrition Examination Survey (NHANES) 2007-20101
| TOTAL | Received SNAP | Eligible, but no SNAP | Ineligible for SNAP | P for diff | |
|---|---|---|---|---|---|
| Total [n (%)] | 9560 (100) | 1,191 (9) | 1,576 (11) | 6,793 (80) | |
| Cooking Dinner Frequency [n (%)] | |||||
| Low (0-1 times/week) | 802 (8) | 86 (9) | 147 (11) | 569 (7) | <0.001 |
| Medium (2-5 times/week) | 3,698 (44) | 352 (30) | 466 (33) | 2,881 (47) | |
| High (6-7 times/week) | 5,060 (48) | 753 (62) | 964 (56) | 3,343 (46) | |
| Cooking dinner frequency [mean (SE)] | 5.02 (0.05) | 5.43 (0.10) | 5.15 (0.11) | 4.96 (0.06) | <0.001 |
| Meals not prepared at home [mean (SE)] | 3.82 (0.07) | 2.65 (0.15) | 3.06 (0.14) | 4.07 (0.07) | <0.001 |
| Sex [n (%)] | |||||
| Female | 4,855 (52) | 683 (60) | 814 (54) | 3,358 (51) | <0.001 |
| Male | 4,705 (48) | 508 (40) | 762 (46) | 3,435 (49) | |
| Race-ethnicity [n (%)] | |||||
| Non-Hispanic white | 4,737 (71) | 477 (49) | 657 (54) | 3,603 (75) | <0.001 |
| Non-Hispanic black | 1,739 (11) | 264 (22) | 232 (12) | 1,243 (9) | |
| Hispanic | 2,648 (13) | 391 (24) | 595 (27) | 1,662 (10) | |
| Other | 436 (6) | 59 (5) | 92 (7) | 285 (6) | |
| Age [n (%)] | |||||
| 20-44 y | 4,306 (49) | 716 (66) | 758 (59) | 2,832 (46) | <0.001 |
| 45-64 y | 3,144 (36) | 337 (27) | 441 (24) | 2,366 (38) | |
| ≥65 y | 2,110 (15) | 138 (6) | 377 (17) | 1,595 (16) | |
| Marital status [n (%)] | |||||
| Currently married | 4,971 (55) | 393 (30) | 632 (35) | 3,946 (60) | <0.001 |
| Not currently married | 4,586 (45) | 798 (70) | 944 (65) | 2,844 (40) | |
| Employment status [n (%)] | |||||
| Not employed | 4,059 (37) | 722 (61) | 819 (50) | 2,518 (32) | <0.001 |
| Part time (1-34 hours) | 1,264 (15) | 155 (13) | 253 (18) | 856 (15) | |
| Full time (>35 hours) | 4,016 (48) | 304 (25) | 473 (32) | 3,239 (53) | |
| Country of Birth [n (%)] | |||||
| Born in the United States | 7,104 (84) | 871 (81) | 965 (69) | 5,268 (86) | <0.001 |
| Born in another country | 2,455 (16) | 320 (19) | 611 (31) | 1,524 (14) | |
| Household Size [n (%)] | |||||
| 1, 2 or 3 person household | 5,856 (65) | 544 (45) | 882 (58) | 4,430 (68) | <0.001 |
| 4 or greater person household | 3,704 (35) | 647 (55) | 694 (42) | 2,363 (32) | |
| Food Security [n (%)] | |||||
| Full food security | 6,800 (79) | 425 (36) | 839 (57) | 5,546 (87) | <0.001 |
| Marginal food security | 1,000 (8) | 201 (16) | 245 (13) | 554 (6) | |
| Low/ very low food security | 1,758 (13) | 565 (48) | 492 (30) | 701 (7) |
Percentage of US population estimated with survey weights to adjust for unequal probability of sampling
2Healthy weight [BMI (kg/m2) 18.5-24.99], Overweight (BMI 25-29.99), Obese (BMI ≥ 30)
Table 2 presents the predicted percent of adults who consume any fruits and vegetables by SNAP status. Compared to those ineligible for SNAP, fewer SNAP participants consumed fruit (total: 35% vs. 46%, p=0.001; fresh: 30% vs. 41%, p<0.001) and vegetables (total: 49% vs. 58%, p=0.001; fresh: 35% vs. 47%, p<0.001). SNAP participants were also less likely to consume fruits (total: 35% vs. 41%, p=0.03; fresh: 30% vs. 36%, p=0.04) and vegetables (total: 49% vs. 55%, p=0.04; fresh: 35% vs. 44%, p=0.004) than income eligible non-participants. Eligible non-participants were less likely to consume fruit (total: 41% vs. 46%, p=0.03; fresh: 36% vs. 41%, p=0.04) than ineligible non-participants.
TABLE 2.
Predicted percent of adults who consume any fruits and vegetables by SNAP participation status, NHANES 2007-2010.
| TOTAL | Received SNAP | Eligible, but no SNAP | Ineligible for SNAP | |
|---|---|---|---|---|
| Mean ± SEM1 | Mean ± SEM | Mean ± SEM | Mean ± SEM | |
| Percent Consuming Any Fruit | ||||
| Totala | 44.5 ± 1.2 | 34.9 ± 2.5* | 40.7 ± 2.5* † | 46.1 ± 1.2 |
| Freshb | 39.6 ± 1.1 | 29.7 ± 2.3* | 36.4 ± 2.3* † | 41.2 ± 1.2 |
| Percent Consuming Any Vegetablesc | ||||
| Totala | 57.0 ± 1.1 | 49.4 ± 2.2* | 54.5 ± 1.8† | 58.2 ± 1.2 |
| Freshb | 45.3 ± 1.1 | 35.3 ± 2.3* | 43.9 ± 2.2† | 46.6 ± 1.2 |
Note: Multivariate regression was used to adjust for age, sex, race/ethnicity, marital status, employment status, if born in the US, household size, and household food security; S.E.M. = standard error of the mean.
Total" category includes raw, fresh, frozen, canned, dried and pickled fruits or vegetables.
"Fresh" category includes only raw or cooked from raw fruits or vegetables.
Vegetables exclude white potatoes.
Difference from those ineligible for SNAP significant at p<0.05
Difference between SNAP participants and income eligible non-participants significant at p<0.05
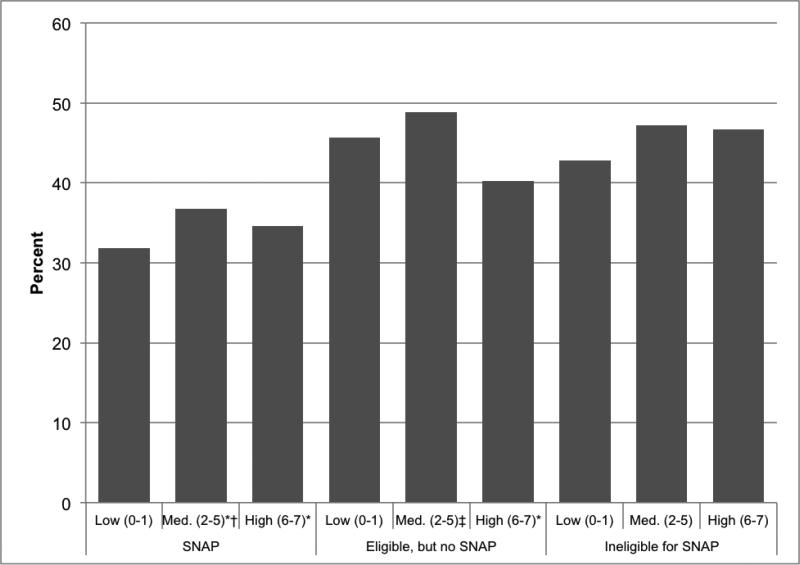
The predicted percent of adults who consume fresh vegetables by household cooking frequency and SNAP status is presented in Figure 1. Among medium (37% vs. 47%, p=0.02) and high (35% vs. 47%, p=0.001) cooking frequency households, SNAP participants were less likely to consume fresh vegetables than those ineligible for SNAP. Among eligible non-participants, medium household cooking frequency was associated with greater probability of fresh vegetable consumption than high cooking frequency (49% vs. 40%, p=0.04).
FIGURE 1.
Predicted percent of adults who consume fresh vegetablesa by household cooking frequencyb and SNAP participation status, NHANES 2007-2010.
Note: Multivariate regression was used to adjust for age, sex, race/ethnicity, marital status, employment status, if born in the US, household size, and household food security.
a “Fresh vegetables includes only raw or cooked from raw vegetables (excluding white potatoes).
b Household cooking frequency defined at days/week someone in the household cooked dinner. * Difference from those ineligible for SNAP within cooking frequency categories significant at p<0.05 † Difference between SNAP participants and income eligible non-participants within cooking frequency categories significant at p<0.05 ‡ Difference from high cookers within SNAP status significant at p<0.05
§ Difference between low and medium cookers within SNAP status significant at p<0.05
Table 3 reports the volume of fruit and vegetable consumption (among those who consumed any fruits or vegetables) by SNAP and cooking status. There were few notable differences in total or fresh fruit consumption by SNAP status or household cooking frequency. Compared to low cooking frequency, high cooking frequency was associated with greater consumption of vegetables among SNAP participants (175 grams vs. 98 grams, p=0.003). Among income-ineligible non-participants, high household cooking frequency was associated with greater consumption of total vegetables compared to low cooking frequency (163 grams vs. 124 grams, p=0.001) and medium cooking frequency households (163 grams vs. 142 grams, p=0.02).
TABLE 3.
Predicted overall energy consumption (kcal), and fruit and vegetable consumption (grams) among adults by household cooking frequencya and SNAP participation status (aged ≥20 y), NHANES 2007-2010
| ALL | Received SNAP | Eligible, but no SNAP | Ineligible for SNAP | |
|---|---|---|---|---|
| Mean ± SEM | Mean ± SEM | Mean ± SEM | Mean ± SEM | |
| Grams of total fruitb (g/day) | ||||
| Overall | 203 ± 4 | 201 ± 15 | 186 ± 12 | 206 ± 4 |
| Low cooking frequency (0-1) | 198 ± 11 | 237 ± 22‡ | 156 ± 22† | 200 ± 13 |
| Medium cooking frequency (2-5) | 194 ± 6‡ | 207 ± 30 | 164±8* ‡ | 197 ± 7 |
| High cooking frequency (6-7) | 211 ± 6 | 194 ± 11* | 207 ± 16 | 213 ± 5 |
| Grams of fresh fruitc (g/day) | ||||
| Overall | 178 ± 4 | 171 ± 14 | 167 ± 10 | 179 ± 5 |
| Low cooking frequency (0-1) | 175 ± 10 | 194 ± 33 | 131 ± 20* | 180 ± 11 |
| Medium cooking frequency (2-5) | 173 ± 6 | 184 ± 29 | 146±9* ‡ | 176 ± 7 |
| High cooking frequency (6-7) | 181 ± 6 | 158 ± 12* | 184 ± 16 | 182 ± 6 |
| Grams of total vegetablesb,d (g/day) | ||||
| Overall | 150 ± 4 | 152 ± 11 | 141 ± 7 | 151 ± 5 |
| Low cooking frequency (0-1) | 126 ± 7‡ | 98 ± 17‡ | 159 ± 19† | 124 ± 8† |
| Medium cooking frequency (2-5) | 141 ± 3‡ | 133 ± 12 | 137 ±10 | 142 ± 4‡ |
| High cooking frequency (6-7) | 162 ± 7 | 175 ± 18 | 143 ± 10† | 163 ± 8 |
| Grams of fresh vegetablesc,d (g/day) | ||||
| Overall | 102 ± 3 | 86 ± 7* | 100 ± 6 | 105 ± 4 |
| Low cooking frequency (0-1) | 87 ± 9‡ | 63 ± 21 | 121 ± 20 | 84 ± 10‡ |
| Medium cooking frequency (2-5) | 100 ± 3 | 97 ± 14 | 108 ± 10 | 99 ± 3‡ |
| High cooking frequency (6-7) | 108 ± 4 | 80 ± 6* | 91 ± 7* | 112 ± 5 |
Note: Multivariate regression was used to adjust for age, sex, race/ethnicity, marital status, employment status, if born in the US, household size, and household food security; S.E.M. = standard error of the mean.
Household cooking frequency defined at days/week someone in the household cooked dinner.
“Total” category include raw, fresh, frozen, canned, dried and pickled fruits or vegetables. Fruit and vegetable intake (all and fresh) calculated only among consumers.
“Fresh” category includes only raw or cooked from raw fruits or vegetables.
Vegetables exclude white potatoes.
Difference from those ineligible for SNAP within cooking frequency categories significant at p<0.05
Difference between SNAP participants and income eligible non-participants within cooking frequency categories significant at p<0.05
Difference from high cookers within SNAP status significant at p<0.05
§Difference between low and medium cookers within SNAP status significant at p<0.05
High household cooking frequency was also associated greater consumption of fresh vegetables than individuals living in low (112 grams vs. 84 grams, p=0.01) and medium (112 grams vs. 99 grams, p=0.02) cooking frequency households among income-ineligible non-participants. Among households with high cooking frequency, income eligible non-participants consumed less total vegetables than SNAP participants (143 grams vs. 175 grams, p=0.05) and ineligible non-participants consumed more fresh vegetables than SNAP participants (112 grams vs. 80 grams, p=0.001) and income eligible non-participants (112 grams vs. 91 grams, p=0.02) among households that cooked with high frequency.
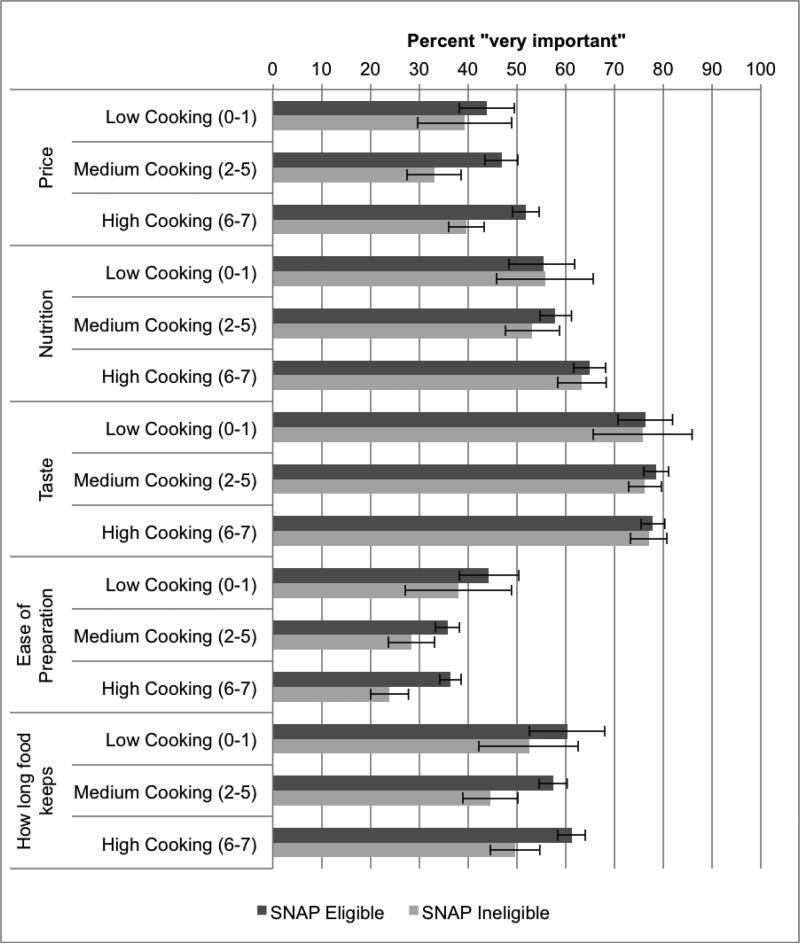
Figure 2 reports the predicted percentage of adults who consider price, nutrition, taste, ease of preparation and how long food keeps as being very important when making food decisions by cooking frequency and SNAP eligibility. Here, SNAP participants and income eligible non-participants have been combined to form one “SNAP eligible” category. Among all groups, 75-78% reported taste as being very important. Compared to SNAP ineligible individuals, price was more important to SNAP eligible individuals in medium (47% vs. 33%, p=0.001) and high (52% vs. 40%, p<0.001) cooking frequency households. Increased cooking frequency was associated with greater importance placed on nutrition among SNAP eligible (low vs. high cooking frequency: 55% vs. 65%, p=0.05) and SNAP ineligible (medium vs. high cooking frequency: 53% vs. 63%, p<0.001) individuals. SNAP eligible individuals also placed greater importance on ease of preparation (medium cookers: 36% vs. 28%, p=0.002; high cookers: 36% vs. 24%, p<0.001) and how long food keeps (medium cookers: 57% vs. 45%, p<0.001; high cookers: 61% vs. 50%, p<0.001) compared to SNAP ineligible individuals.
FIGURE 2.
Predicted percent of adults who identify the following values as “very important” when making food purchase decisions by SNAP eligibilitya and household cooking frequencyb, NHANES 2007-2010.
Note: Multivariate regression was used to adjust for age, sex, race/ethnicity, marital status, employment status, if born in the US, household size, and household food security. Bars indicate 95% confidence intervals.
a SNAP participants and income-eligible non-participants were combined to form one “SNAP eligible” category
bHousehold cooking frequency defined at days/week someone in the household cooked dinner
In separate analyses we re-estimated the above analyses with pregnant women and diabetics included in the sample (N=11,028). The results described above were robust, and yielded results that were substantively similar to the results presented above. These analyses are available upon request.
DISCUSSION
This study examined fruit and vegetable consumption and food values among American adults, by SNAP status and cooking frequency. SNAP participants were least likely to consume any fruits or vegetables compared to those not participating in the program, regardless of cooking frequency. Frequent cooking (>6 times/week) was associated with increased volume of consumption of fresh vegetables only among those ineligible for SNAP.
Consistent with prior literature, this study shows that regardless of SNAP participation status, Americans are not consuming the recommended amount of fruits and vegetables,21, 27, 43 and that lower-income and SNAP participation are associated with lower fruit and vegetable consumption.25, 26, 40, 41 The study findings are also consistent with prior studies showing that the positive correlation between home cooking and diet quality is not as strong or consistent among lower-income, SNAP eligible individuals as in higher-income populations.45, 56
While fruit and vegetable consumption is low overall, these results show few differences by SNAP status suggesting that income may not be a primary barrier to produce consumption. Rather, our examination of values influencing food purchase decisions, like prior research, suggests that price, perishability, and ease of preparation are particularly important to those eligible for SNAP.48 Therefore, the identification of strategies to increase fruit and vegetable consumption, particularly among Americans eligible for the SNAP program, should consider a reduced emphasis on ‘fresh’ –commonly promoted in programs such as the Let's Move campaign among others47, 60, 61 – and an increased emphasis on non-fresh alternatives (e.g., canned, frozen, dried) as they may be less expensive, easier to use, and be less perishable.
SNAP should consider exploring policy changes to incentivize healthy home cooking among participants. For example, SNAP benefits can currently be used at farmer's markets and, in some states may be doubled when used for fresh, locally grown fruits and vegetables.57 Applying these incentives to non-fresh alternatives at supermarkets (e.g., frozen) may help to increase produce use in household cooking. The SNAP benefit structure could be modified so that the Thrifty Food Plan includes alternative fruits and vegetables requiring less time and preparation. SNAP-Ed could expand to teach comprehensive cooking skills education including how to navigate the grocery store, budgeting, meal planning, safe storage, and quick and easy cooking techniques.
The present study has several limitations. First, the data are cross-sectional, so associations but not causal inferences can be made. The reliance on self-reported data for the single 24-hour dietary recall may introduce bias due to underreporting and unreliability resulting from recall and social desirability bias. Furthermore, single 24-hour dietary recalls are reliable on a group level, not on an individual level. The analysis of the association between food values, cooking frequency and SNAP eligibility could have been subject to self selection bias as there were some statistically significant differences along many of the study covariates between the approximately 80% of the study sample with complete food values data and the approximately 20% of the sample excluded from that analysis due to missing food values data. Fruit and vegetable consumption may be underestimated due to our relatively conservative categorization fruits and vegetables. In addition, SNAP participation is underestimated in the NHANES compared to USDA national estimates, which also could have biased our results towards the null. The cooking measure only reports frequency of cooking dinner; the frequency of cooking other meals and whether the fruits and vegetables consumed were cooked at home is unknowable due to limitations of the data. And, importantly, the interpretation of cooking could vary widely across the study population.58 Finally, the associations observed between SNAP participation and fruit and vegetable consumption (as well as the importance of food values) may be biased towards the null due to self-selection into the SNAP program. Specifically, SNAP participants and non-participants may differ by unobserved characteristics that are also related to their fruit and vegetable consumption and cooking habits.59 SNAP participants are often worse off than non-participants with regard to financial and nutritional need,60 and SNAP participation has previously been found to be associated with greater food insecurity and worse diet quality.61, 62
CONCLUSION
In conclusion, Americans consume far fewer fruits and vegetables than recommended. Consumption of fresh produce is especially low among SNAP participants, regardless of cooking frequency. Among higher-income populations, greater cooking frequency is associated with increased consumption of total and fresh vegetables. Low-income populations eligible for SNAP consider price, ease of preparation and perishability of food items as very important to their food purchase decisions. Efforts to shift the balance from consumption of foods away from home to more home cooked meals and increased produce consumption should consider the contexts and constraints in which food choices take place.
Highlights.
We analyzed NHANES data on fruit and vegetable consumption and food values in the US.
Fewer SNAP participants consumed fruit and vegetables than non-participants.
Higher cooking frequency is associated with greater vegetable consumption.
How long food keeps and ease of preparation are important for low-income individuals.
SNAP participants consume little fresh produce regardless of cooking frequency.
ACKNOWLEDGEMENTS
JAW conceived of the study and developed the hypotheses. JAW performed the statistical analysis. JAW and SNB contributed to the interpretation of the study findings. JAW drafted the manuscript and both authors contributed to the final draft. JAW had full access to all the data and takes responsibility for the integrity of the data and the accuracy of the analysis. The authors gratefully acknowledge the work of Seanna Vine, MPH in compiling the data set.
SNB was supported by a grant from the National Heart, Lung, and Blood Institute (1K01HL096409).
APPENDIX A
Total Fruit
Includes raw, fresh, frozen, canned, in syrup, dried (w or w/out sugar), chips, apple sauce, sweetened, pickled, spiced, juice packed. Juice, pie-filling, fried, battered, maraschino cherries, fruit in other dishes (e.g. ambrosia, relish, fruit salads. fruit cocktails) are not included.
Fresh Fruit
Fruits included above with fresh or raw in the description.
Total Vegetables
Includes raw, cooked (w or w/out added fat), fresh/frozen/raw/canned, salads with no dressing or cheese, dried/dehydrated, peas, olives, corn, pickled. The NHANES category of starchy vegetables (white potatoes, cassava), chips, anything with sauce, cheese or dressing, candied, casserole, battered, fried, soup, juice, stuffed, scalloped, creamed, soufflé, yeast, fritters, anything with meat, pasta or egg, catsup, salsa, aspic are not included.
Fresh Vegetables
Anything included above with the words raw, cooked from fresh (w or w/out fat added), or stewed from fresh.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: JAW has no financial disclosures.
Conflicts of interest: None.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132(6):2087–102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 3.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–45. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 4.Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009;67(Suppl 1):S36–9. doi: 10.1111/j.1753-4887.2009.00157.x. [DOI] [PubMed] [Google Scholar]
- 5.Bowen S, Elliott S, Brenton J. The Joy of Cooking? Contexts. 2014;13(3):20–25. [Google Scholar]
- 6.Condrasky MD, Griffin SG, Catalano PM, Clark C. A formative evaluation of the Cooking with a Chef program. Journal of extension. 2010;48(2):2FEA1. [Google Scholar]
- 7.Hartmann C, Dohle S, Siegrist M. Importance of cooking skills for balanced food choices. Appetite. 2013;65:125–131. doi: 10.1016/j.appet.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Lichtenstein AH, Ludwig DS. Bring back home economics education. JAMA. 2010;303(18):1857–8. doi: 10.1001/jama.2010.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mancino LG, C.A. 2012 Agricultural and Applied Economics Association, 2012 Annual Meeting. Seattle, Washington: 2012. Does More Cooking Mean Better Eating? Estimating the relationship between time spent in food preparation and diet quality. p. 21. [Google Scholar]
- 10.Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965-1966 to 2007-2008. Nutr J. 2013;12:45. doi: 10.1186/1475-2891-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Virudachalam S, Long JA, Harhay MO, Polsky DE, Feudtner C. Prevalence and patterns of cooking dinner at home in the USA: National Health and Nutrition Examination Survey (NHANES) 2007–2008. Public Health Nutrition. 2013:1–9. doi: 10.1017/S1368980013002589. FirstView. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Todd JE, Mancino L, Lin B-H. The impact of food away from home on adult diet quality. US Department of Agriculture, Economic Research Service; 2010. [Google Scholar]
- 13.Wolfson JA, Bleich SN. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutrition. 2014:1–10. doi: 10.1017/S1368980014001943. FirstView. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin B-H, Guthrie JF. Nutritional quality of food prepared at home and away from home, 1977-2008: United States Department of Agriculture. Economic Research Service; 2012. [Google Scholar]
- 15.Kolodinsky JM, Goldstein AB. Time use and food pattern influences on obesity. Obesity. 2011;19(12):2327–2335. doi: 10.1038/oby.2011.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamrick KS, Andrews M, Guthrie J, Hopkins D, McClelland K. How Much Time Do Americans Spend on Food? US Department of Agriculture, Economic Research Service; 2011. [Google Scholar]
- 17.Zick CD, Stevens RB. Trends in Americans' food-related time use: 1975-2006. Public Health Nutr. 2010;13(7):1064–72. doi: 10.1017/S1368980009992138. [DOI] [PubMed] [Google Scholar]
- 18.United States Department of Agriculture [2014 October 9];Supplemental Nutrition Assistance Program Participation and Costs. 2014 Available from: http://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap.
- 19.United States Department of Agriculture [2014 June 2];Approved federal funds for SNAP education by fiscal year. 2014 Available from: http://www.nal.usda.gov/fsn/ApprovedFederalFundsSNAP-Ed01202010.pdf.
- 20.United States Department of Agriculture [2014 June 2];Supplemetal Nutrition Assistance Program Education Guidance. 2014 Available from: http://snap.nal.usda.gov/snap/Guidance/FinalFY2015SNAP-EdGuidance.pdf.
- 21.United States Department of Agriculture and United States Department of Health and Human Services . Dietary Guidelines for Americans, 2010. 7th Edition ed. U.S. Government Printing Office; Washington D.C.: 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United States Department of Agriculture [2014 October 8];What's Cooking? USDA Mixing Bowl. Available from: http://www.whatscooking.fns.usda.gov/
- 23.Gregory C, Ver Ploeg M, Andrews M, Coleman-Jensen A. Supplemental Nutrition Assistance Program (SNAP) Participation Leads to Modest Changes in Diet Quality. Economic Research Report. 2013:147. [Google Scholar]
- 24.Gleason P, Rangarajan A, Olson CM. Dietary intake and dietary attitudes among food stamp participants and other low-income individuals. Mathematica Policy Research, Incorporated. 2000 [Google Scholar]
- 25.Leung CW, Ding EL, Catalano PJ, Villamor E, Rimm EB, Willett WC. Dietary intake and dietary quality of low-income adults in the Supplemental Nutrition Assistance Program. Am J Clin Nutr. 2012;96(5):977–88. doi: 10.3945/ajcn.112.040014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cole N, Fox MK. US Department of Agriculture. Food and Nutrition Service, Office of Research, Nutrition and Analysis; 2008. Diet quality of Americans by food stamp participation status: Data from the National Health and Nutrition Examination Survey, 1999-2004. [Google Scholar]
- 27.Middaugh AL, Fisk PS, Brunt A, Rhee YS. Few Associations between Income and Fruit and Vegetable Consumption. Journal of Nutrition Education and Behavior. 2012;44(3):196–203. doi: 10.1016/j.jneb.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Bish B, Regis K, Gottesman MM. Educating parents about portion sizes for preschoolers. J Pediatr Health Care. 2005;19(1):54–9. doi: 10.1016/j.pedhc.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Cohen JF, Smit LA, Parker E, Austin SB, Frazier AL, Economos CD, et al. Long-term impact of a chef on school lunch consumption: findings from a 2-year pilot study in Boston middle schools. J Acad Nutr Diet. 2012;112(6):927–33. doi: 10.1016/j.jand.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 30.Condrasky M, Hegler M, Sharp JL. Application of cooking with a chef for school food service professionals. Topics in Clinical Nutrition. 2011;26(2):171–178. [Google Scholar]
- 31.Cooking Matters. Cooking Matters Program- what we do. 2014 May 8; Available from: http://cookingmatters.org/what-we-do.
- 32.Davis JN, Ventura EE, Cook LT, Gyllenhammer LE, Gatto NM. LA Sprouts: a gardening, nutrition, and cooking intervention for Latino youth improves diet and reduces obesity. J Am Diet Assoc. 2011;111(8):1224–30. doi: 10.1016/j.jada.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 33.Flynn MM, Reinert S, Schiff AR. A Six-Week Cooking Program of Plant-Based Recipes Improves Food Security, Body Weight, and Food Purchases for Food Pantry Clients. Journal of Hunger and Environmental Nutrition. 2013;8(1):73–84. [Google Scholar]
- 34.Garber AB. The S.O.U.L Food Project: Facts and findings from a program that sought to increase fruit and vegetable consumption and improve cooking habits in West Harlem [Ed.D.] Teachers College, Columbia University; United States -- New York: 2007. [Google Scholar]
- 35.Gittelsohn J, Song HJ, Suratkar S, Kumar MB, Henry EG, Sharma S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav. 2010;37(3):390–402. doi: 10.1177/1090198109343886. [DOI] [PubMed] [Google Scholar]
- 36.Levy J, Auld G. Cooking classes outperform cooking demonstrations for college sophomores. Journal of Nutrition Education and Behavior. 2004;36(4):197–203. doi: 10.1016/s1499-4046(06)60234-0. [DOI] [PubMed] [Google Scholar]
- 37.Olsen NJ, Buch-Andersen T, Handel MN, Ostergaard LM, Pedersen J, Seeger C, et al. The Healthy Start project: a randomized, controlled intervention to prevent overweight among normal weight, preschool children at high risk of future overweight. BMC Public Health. 2012;12:590. doi: 10.1186/1471-2458-12-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tessaro I, Rye S, Parker L, Trangsrud K, Mangone C, McCrone S, et al. Cookin' Up Health: developing a nutrition intervention for a rural Appalachian population. Health Promot Pract. 2006;7(2):252–7. doi: 10.1177/1524839905278887. [DOI] [PubMed] [Google Scholar]
- 39.Young CR, Aquilante JL, Solomon S, Colby L, Kawinzi MA, Uy N, et al. Improving fruit and vegetable consumption among low-income customers at farmers markets: Philly Food Bucks, Philadelphia, Pennsylvania, 2011. Preventing chronic disease. 2013:10. doi: 10.5888/pcd10.120356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grimm KA, Foltz JL, Blanck HM, Scanlon KS. Household Income Disparities in Fruit and Vegetable Consumption by State and Territory: Results of the 2009 Behavioral Risk Factor Surveillance System. Journal of the Academy of Nutrition and Dietetics. 2012;112(12):2014–2021. doi: 10.1016/j.jand.2012.08.030. [DOI] [PubMed] [Google Scholar]
- 41.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. Journal of the Academy of Nutrition and Dietetics. 2012;112(5):624–635. e6. doi: 10.1016/j.jand.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin B-H, Wendt M, Guthrie JF. Impact on energy, sodium and dietary fibre intakes of vegetables prepared at home and away from home in the USA. Public health nutrition. 2013;16(11):1937–1943. doi: 10.1017/S1368980013001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Casagrande SS, Wang Y, Anderson C, Gary TL. Have Americans Increased Their Fruit and Vegetable Intake?: The Trends Between 1988 and 2002. American Journal of Preventive Medicine. 2007;32(4):257–263. doi: 10.1016/j.amepre.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 44.Lang T, Caraher M, Dixon P, Carr-Hill R. Cooking skills and health. Health Education Authority. 1999 [Google Scholar]
- 45.McLaughlin C, Tarasuk V, Kreiger N. An examination of at-home food preparation activity among low-income, food-insecure women. Journal of the American Dietetic Association. 2003;103(11):1506–1512. doi: 10.1016/j.jada.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 46.Larson NI, Perry CL, Story M, Neumark-Sztainer D. Food preparation by young adults is associated with better diet quality. J Am Diet Assoc. 2006;106(12):2001–7. doi: 10.1016/j.jada.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 47.Furst T, Connors M, Bisogni CA, Sobal J, Falk LW. Food Choice: A Conceptual Model of the Process. Appetite. 1996;26(3):247–266. doi: 10.1006/appe.1996.0019. [DOI] [PubMed] [Google Scholar]
- 48.Glanz K, Basil M, Maibach E, Goldberg J, Snyder DAN. Why Americans Eat What They Do: Taste, Nutrition, Cost, Convenience, and Weight Control Concerns as Influences on Food Consumption. Journal of the American Dietetic Association. 1998;98(10):1118–1126. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 49.Soliah LAL, Walter JM, Jones SA. Benefits and Barriers to Healthful Eating What Are the Consequences of Decreased Food Preparation Ability? American Journal of Lifestyle Medicine. 2012;6(2):152–158. [Google Scholar]
- 50.Caraher M, Dixon P, Lang T, Carr-Hill R. The state of cooking in England: the relationship of cooking skills to food choices. British Food Journal. 1999;1(8):590–607. [Google Scholar]
- 51.Celnik D, Gillespie L, Lean MEJ. Time-scarcity, ready-meals, ill-health and the obesity epidemic. Trends in Food Science & Technology. 2012;27(1):4–11. [Google Scholar]
- 52.Centers for Disease Control . National Health and Nutrition Examination Survey. In: Hyattsville MD, editor. Statistics NCfH. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 53.United States Department of Agriculture Supplemental Nutrition Assistance Program participation and costs. 2013 Available from: http://www.fns.usda.gov/pd/SNAPsummary.htm.
- 54.Bleich SN, Vine S, Wolfson JA. American adults eligible for the Supplemental Nutritional Assistance Program consume more sugary beverages than ineligible adults. Preventive medicine. 2013 doi: 10.1016/j.ypmed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bickel G NM, Price C, Hamilton W, J. C. Guide to Measuring Household Food Security. U.S. Department of Agriculture; 2000. [Google Scholar]
- 56.Engler-Stringer R, Stringer B, Haines T. Complexity of Food Preparation and Food Security Status: In Low-income Young Women. Canadian Journal of Dietetic Practice and Research. 2011;72(3):133–6. doi: 10.3148/72.3.2011.133. [DOI] [PubMed] [Google Scholar]
- 57.Fair Food Network [2014 October 16];Double Up Food Bucks. 2014 Available from: http://doubleupfoodbucks.org/
- 58.Short F. Kitchen secrets: The meaning of cooking in everyday life. Berg. 2006 [Google Scholar]
- 59.Gundersen C, Kreider B. Food Stamps and Food Insecurity: What Can Be Learned in the Presence of Nonclassical Measurement Error? The Journal of Human Resources. 2008;43(2):352–382. [Google Scholar]
- 60.Nord M. Does SNAP Decrease Food Insecurity?: Untangling the Self-Selection Effect. DIANE Publishing; 2010. [Google Scholar]
- 61.Wilde PE. Measuring the Effect of Food Stamps on Food Insecurity and Hunger: Research and Policy Considerations. The Journal of Nutrition. 2007;137(2):307–310. doi: 10.1093/jn/137.2.307. [DOI] [PubMed] [Google Scholar]
- 62.Jensen HH. Food Insecurity and the Food Stamp Program. American Journal of Agricultural Economics. 2002;84(5):1215–1228. [Google Scholar]