Abstract
Background: Authors of the Diagnostic and Statistical Manual, Fifth Edition (DSM-V) have recommended to “integrate dimensions into clinical practice.” The epidemiology and associated phenomenology of formal thought disorder (FTD) have been described but not reviewed. We aimed to carry out a systematic review of FTD to this end. Methods: A systematic review of FTD literature, from 1978 to 2013, using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Results: A total of 881 abstracts were reviewed and 120 articles met inclusion criteria; articles describing FTD factor structure (n = 15), prevalence and longitudinal course (n = 41), role in diagnosis (n = 22), associated clinical variables (n = 56), and influence on outcome (n = 35) were included. Prevalence estimates for FTD in psychosis range from 5% to 91%. Dividing FTD into domains, by factor analysis, can accurately identify 91% of psychotic diagnoses. FTD is associated with increased clinical severity. Poorer outcomes are predicted by negative thought disorder, more so than the typical construct of “disorganized speech.” Conclusion: FTD is a common symptom of psychosis and may be considered a marker of illness severity. Detailed dimensional assessment of FTD can clarify diagnosis and may help predict prognosis.
Key words: formal thought disorder, thought disorder, phenomenology, epidemiology, prognosis, psychosis, schizophrenia, language, communication
Introduction
Formal thought disorder (FTD) has long been of interest to phenomenologists. Since Bleuler’s description of “loosening of associations,” it has been considered a core symptom of psychosis.1 The clinical conceptualization of FTD has evolved over time and it is now known that a variety of cognitive and linguistic abnormalities are associated with it.2,3 FTD was once thought to be specific to schizophrenia but is now known to manifest in affective psychoses, nonpsychotic illnesses, and normal controls.4 Despite some promising findings in FTD research to date, a great deal about this symptom remains either uncertain or undiscovered.5–7 The clinical heterogeneity of FTD is relevant in this regard; its core clinical phenotype is yet to be conclusively defined.
FTD is an objective sign observed on mental state examination, which differentiates it from symptoms such as delusions and hallucinations. Up to 18 different abnormalities in the rate and organization of speech are described in FTD rating scales and it is unlikely that FTD is a discrete entity. Instead, it reflects a cluster of related cognitive, linguistic, and affective disturbances. Accordingly, FTD research has been approached from a diverse range of clinical perspectives, eg, neurolinguistics, cognitive neuroscience, and psychiatry.
Previous reviews have highlighted the role of semantic priming abnormalities, impaired executive functioning, and, potentially, genetics in the etiology of FTD.2,3,5 Neurobiological studies have implicated certain brain regions, such as the superior temporal gyrus, and receptors, such as N-methyl-d-aspartate, in its genesis.6–9 These diverse etiologies for FTD may help to explain the lack of consensus as to how to best conceptualize this symptom to date. It remains to be clarified how the depth of phenomenological detail that has been described in association with FTD is of clinical relevance.
The Diagnostic and Statistical Manual, Fifth Edition (DSM-V) recommends the integration of “dimensions into clinical practice.”10 This emphasis on dimensions is relevant to FTD, however the DSM-V is less prescriptive in its description of this symptom than for other domains of psychosis. This is a matter of concern, given that all psychiatric research is ultimately grounded in precise phenomenology. It is timely, therefore, to return to the clinical conceptualization on which FTD research is based. To this end, we sought to carry out a review of the epidemiological and phenomenological research in FTD. We aimed to establish the clinical significance of FTD, including its place in the dimensional assessment of psychosis and highlight potential areas for future research.
Aims and Objectives
To examine the epidemiology and phenomenology of FTD in mental illness, in order to describe the core clinical phenotype of this symptom.
The objectives of this paper are to review:
1. The factor structure of FTD.
2. The epidemiology of FTD.
3. The clinical and demographic variables associated with FTD.
4. The prognostic value of FTD in mental illness.
Methodology
Identification of Studies
This review conforms to the criteria outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) current statement.11 A formal search strategy was devised using both Medical Subject Headings (MeSH) and free-text search strings with the aim of collating all published studies on the factor analysis (FA), epidemiology, associated phenomenology, and outcomes of FTD. We used this strategy to search the medical databases (PubMed, Medline, and PsycInfo) covering the years 1978–2014 with limits set on humans. Titles and abstracts were reviewed and irrelevant studies excluded. We then searched the full text and reference lists of the remaining studies for other potentially salient work.
PubMed Search Strategy
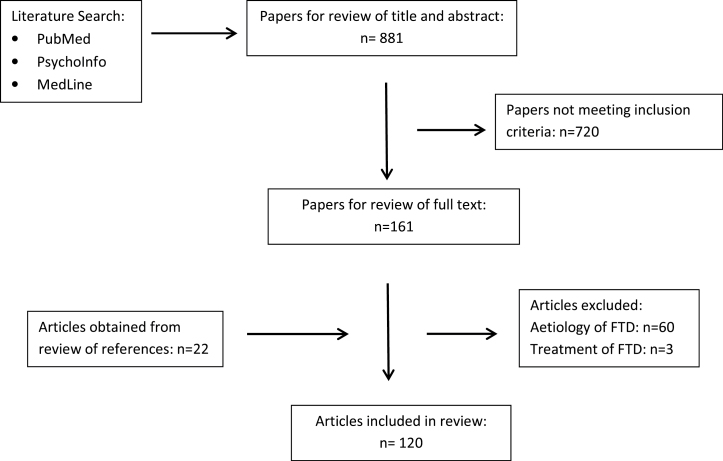
We performed free-text search (using quoted phrases such as “formal thought disorder,” “epidemiology,” and “prognosis”) which produced a set of 496 papers. The MeSH heading “Schizophrenia and disorders with Psychotic features” was combined with the MeSH headings “factor analysis,” “statistical,” and “prognosis” to retrieve 44 further relevant studies. Further free-text searches for well-known authors in the area of FTD research produced 341 references. In total, we considered abstracts of 881 published articles and, from these, the full texts of 161 articles were reviewed by E.R. and L.C. Where controversy occurred, a decision to include or exclude was made by the senior author M.C. A total of 120 articles were included in the review, 22 of which were obtained by hand-searching references. A flowchart of our search strategy is outlined in figure 1.
Fig. 1.
Flowchart of search strategy for systematic review.
Inclusion of Studies
We included studies that described the factor structure, epidemiology, associated phenomenology, or outcome of FTD in mental illness.
Exclusion of Studies
We excluded studies that reported on treatment or intervention for FTD. We also excluded studies where the sole aim was to investigate the etiology of FTD, eg, underlying cognitive or biological causes, as this has been the subject of several reviews to date.2,3,5
Results
The Factor Structure of FTD (n = 15)
Bleuler described “loosening of associations” as a fundamental symptom of schizophrenia.1 He also emphasized the role of pressured speech, perseveration, blocking, and clanging and highlighted how topics of “emotional concern” are often the subject of abnormally associated thoughts. The assessment of FTD has since been operationalized and there have been 15 FA studies of FTD published in the English language. Ten of these have examined the factor structure of the Thought, Language, and Communication Disorders (TLC) scale, which describes 18 types of FTD.4,12–25 The TLC scale was hypothesized to reflect “thought,” “language,” and “communication” disorders; however, this division may not reflect FTD factor structure.23,26–28 Many other FTD scales have been developed, including the Scale for the Assessment of Positive Symptoms (SAPS), Scale for the Assessment of Negative Symptoms (SANS), the Positive and Negative Syndrome Scale (PANSS) for Schizophrenia, the Brief Psychiatric Rating Scale (BPRS), the Present State Examination (PSE), the Thought Disorder Index (TDI), the Thought and Language Index (TLI), and the Communication Disturbances Index (CDI), all of which are clinician-rated scales.15,29–35 A self-report FTD scale has also been developed.22
FA studies generally comprise inpatients with a diagnosis of schizophrenia; however, other diagnoses have been examined, most commonly: mania, depression, the at-risk mental state (ARMS), and normal controls. The number of FTD factors identified may be influenced by the age profile of study participants, diagnostic heterogeneity, clinical status (acute or remitted psychosis), medication status, and the number of thought disorder items included in the analyses.16,17,36 Andreasen originally proposed a dichotomous, “negative” (poverty of speech and poverty of content) and “positive” (pressure of speech, tangentiality, derailment, incoherence, and illogicality) structure of FTD.13 These FTD subtypes were hypothesized to occupy opposite ends of a single spectrum of abnormal speech, however they have been shown to be weakly correlated (r = .27).18 They are differentiated by the fact that negative thought disorder is associated with poorer treatment response, lower educational attainment, and poorer functioning, whereas positive thought disorder has no such associations.19 Up to 7 different domains of FTD, within the TLC scale, have been identified, with the majority of variance (range: 42%–78%) accounted for by 2 or 3 domains. The well-circumscribed “disorganization domain” is characterized by FTD items typical of Bleuler’s “loosening of associations” (tangentiality, derailment, incoherence, illogicality, circumstantiality, and loss of goal). Some investigators (n = 5) identify a “negative” domain, comprising poverty of speech, poverty of content of speech, with or without perseveration. Others (n = 5) identify a “verbosity” or “productivity” domain in which pressure of speech and poverty of speech both load, albeit inversely. Frequently (n = 4), pressure of speech will load on the disorganization domain, reflecting the blurring of categorical boundaries between mania and schizophreniform disorders.
Andreasen gave examples of poverty of speech (negative FTD) and incoherence (positive FTD) in her seminal article on FTD28:
Poverty of speech:
Interviewer: “Were you working before you came to the hospital?”
Patient: “No”
Interviewer: What kind of jobs have you had in the past?”
Patient: “Oh, some janitor jobs, painting”
Interviewer: “What kind of work do you do?”
Patient: “I don’t. I don’t like any kind work. That’s silly”
Incoherence:
Interviewer: “Why do you think people believe in God?”
Patient: “Um, because making a do in life. Isn’t none of that stuff about evolution guiding isn’t true anymore now. It all happened a long time ago. It happened in eons and eons and stuff they wouldn’t believe in him. The time that Jesus Christ people believe in their thing people believed in, Jehovah God that they didn’t believe in Jesus Christ that much.”
The Prevalence and Longitudinal Course of FTD (n = 41)
Prevalence.
Observational studies, based mainly on inpatient populations, quote high prevalence rates for FTD based on structured assessments, most frequently the TLC scale. However, the literature in this area is very difficult to compare, due to the lack of cutoff scores to indicate the presence of FTD, the absence of validation studies in the general population, and the paucity of studies that employ more than one FTD assessment scale for comparative purposes. The single largest study (n = 1665) recorded that 50.39% of patients with schizophrenia demonstrated FTD (PANSS).37 In a mixed diagnostic sample (n = 660), the prevalence was 72.7% (TLC scale).24 Comparing mania and schizophrenia, findings are conflicting: some find FTD to be more frequent,4,38,39 others find that it is less frequent,17,40 and still others find that it is equally prevalent in mania as in schizophrenia.41,42 Relative prevalence may depend on whether a narrow or broad definition of FTD is employed.17,40 Up to 60% of patients with schizoaffective disorder, and 53% of depressed patients, have been reported to display FTD.13,26 Prevalence estimates based on bizarre idiosyncratic thinking (BIT) range from 36% in nonpsychotic disorders (including personality disorders, neurosis, and depression) to 81% in schizophrenia (n = 191).43 Using the OPCRIT criteria, however, FTD prevalence among inpatients with schizophrenia-spectrum disorders was estimated to be only 27.4% (n = 336); this is likely to be more reflective of DSM guidelines that FTD should be “severe enough to substantially impair effective communication.”44,45 Not only present in acute mania or schizophrenia, FTD has also been described in those with nonpsychotic disorders, as well as those in remitted psychosis.4,43 It likely that FTD exists on a continuum with normal speech, as 6% of normal controls have evidence of it.26,46,47 Disordered speech appears to progress along an exponential, rather than linear, gradient of increasing prevalence and severity, from normal to acutely psychotic or manic.
Longitudinal Course.
The most comprehensive longitudinal study of FTD is the Chicago Follow-up Study (inpatient sample, n = 77–191), which assessed BIT over 8 years.43,48–51 BIT is a relatively broad construct, related to intelligence levels, and rated on the idiosyncrasy of responses given to stimuli, usually proverbs.52–54 Persistent BIT was found to be rare in nonpsychotic disorders (4%) and most common in those with schizophrenia (24%); intermediate rates of persistence are observed in nonschizophrenia psychotic disorders and schizoaffective disorder. The presence of BIT at follow-up assessment was best predicted by diagnosis and premorbid social and academic functioning. If severe BIT was present at follow-up, it usually reflected a chronic, unremitting illness, rather than an acute relapse of schizophrenia.
Bowie reported on a 2.3-year follow-up of FTD in a geriatric population and found that disorganized speech remained stable, while underproductive speech deteriorated.55 Over 6 months, Andreasen and Grove found that FTD remitted to a greater extent in those with mania and schizoaffective disorder than schizophrenia.4 This finding was replicated by Jampala et al.40 Wilcox et al found no difference in FTD severity between diagnostic groups at baseline, however, at 10- and 20-year follow-up, it was significantly more severe in those with schizophrenia compared with other diagnoses.46 Winokur et al reported that FTD prevalence remained stable over the first 10 episodes of illness in those with psychotic disorders.56
About 4.5 years after index admission, those with deficit syndrome demonstrate significant deterioration in FTD compared with nondeficit schizophrenia.57 Parnas et al reported that FTD increases in the 6 years following first episode, ie, nondeficit schizophrenia (n = 67), however methodological limitations were acknowledged in this study.58 Other investigators, examining smaller study samples, have reported that FTD either improves59–61 or remains stable61–65 at follow-up, with negative thought disorder more commonly persisting at follow-up when compared to positive FTD.61,64
Diagnostic Category and FTD (n = 22)
Severity, subtype, and temporal course of FTD differentiate between diagnostic categories of psychosis, particularly mania and schizophrenia. Whether FTD in mania is more severe38–40,66 or equally severe32,67 as that in schizophrenia depends on how broad a definition of FTD is employed.17,40 FTD, taken as a global measure, is more likely to persist in those with schizophrenia. FTD is associated with “core” or “Kraepelinian” schizophrenia, which is equivalent to the deficit syndrome, and it may also help distinguish paranoid from nonparanoid schizophrenia.68–70 The potential for circular reasoning when using FTD to differentiate between psychotic disorders must be acknowledged, as FTD is one of the diagnostic criteria of psychosis.
Andreasen and Grove viewed FTD as a positive and negative dichotomy, with “empty disorganized” speech in schizophrenia and “fluent disorganized” speech in mania.4 Others have found that verbal productivity alone distinguishes mania from schizophrenia.41,42 Those with schizophrenia have more “disorganization and idiosyncratic speech” than mania, in which there is more playful and “combinatory thinking”; this study reported that speech in schizoaffective disorder was more similar to schizophrenia than mania.67,71–73 Wykes and Leff found that the speech of those with mania was more cohesive that that in schizophrenia.74 Docherty et al concluded that those with mania produce more speech, and, proportionately, more ambiguous word meanings, than those with schizophrenia in which there was more missing-information references.32 Taylor et al demonstrated that 91% of mania and schizophrenia diagnoses could be distinguished, based on relative severities of “verbiage disturbance” and “disconnected speech.”17 Most recently, Cuesta and Peralta found that schizophrenia was differentiated from other psychotic disorders only by the severity of idiosyncratic and impoverished speech; there was no difference in severity of disorganized speech when verbosity was controlled for.24 Hoffman et al’s conclusion sums up some of the concepts described; those with mania displayed greater quantities of speech, and more deviance within that speech, than those with schizophrenia, however the overall coherence of manic speech was greater than that observed in those with schizophrenia, where there is “diminished discourse planning abilities.”39
FTD and Associated Variables (n = 56)
Age, Demography, and FTD.
It is likely that FTD prevalence and severity varies across the lifespan. In child and adolescent populations, FTD prevalence ranges widely, between 40% and 100%.75,76 However, it may not be possible to reliably interpret comparisons between FTD prevalence in adolescents and adults, due to methodological issues relating to the Kiddie FTD scale.77,78 Children and adolescents with mania may display less severe FTD than adults.79,80 Furthermore, studies of FTD in the children of people with schizophrenia suggest that FTD is a stable trait for children affected.25
Neither Schultz nor Cuesta found any correlation between FTD and age, in those with early-onset psychosis, suggesting that FTD prevalence remains stable over time.24,81 Early-onset schizophrenia is associated with significantly more prevalent positive and negative FTD than those with late-onset illness (27.4% vs 10.4%, P = .005 and 11% vs 2.2%, P = .01 respectively, total n = 470).44 Pearlson’s chart review had originally noted this trend (prevalence 5.6% in late-onset illness and 54.5% in early-onset illness), a finding confirmed in 5 other studies.82–87 There have been 2 exceptions to these findings, however methodological limitations, relating to those studies, were acknowledged by the investigators.88,89 Variation in the defined age cut-off for “late-onset psychosis” is noteworthy; it ranges from 45 to 65 years of age.
Apart from age, no other basic demographic variables appear to influence the presence or severity of FTD. Some have reported that those in rural areas, with lower educational achievement and those of Afrikaner, rather than American descent, demonstrate more severe FTD.21,90–92 These findings have not been replicated.
Comorbid Substance Abuse and FTD.
Comorbid substance abuse impacts on the presence, severity, and longitudinal course of FTD in psychosis, although study design may impact on these findings. Cannabis abuse in the 6-month and 12-month time period, prior to first-episode psychosis, is associated with more severe FTD at presentation (n = 502).93,94 However, a smaller study (n = 125) found the reverse and Soyka et al found no association between the presence of FTD and a history of substance-use disorder (either lifetime or over the past 3 months) in schizophrenia (total n = 447).95,96 Cannabis abuse predicts the presence of significantly worse FTD at 5.5-year follow-up in those with schizophrenia.97 Similarly, the presence of comorbid substance abuse disorder predicts a worse clinical course in schizophrenia, including a trend toward more severe FTD at 5-year follow-up.98 Within a substance-abusing population, FTD was one of 6 variables demonstrated to predict a diagnosis of schizophrenia (present in 30% of those with schizophrenia vs 12% without), a result similar to the findings of Cornelius et al.99,100
Comorbid Physical Conditions and FTD.
FTD has been studied in children with epilepsy, where it is associated with communication deficits, seizure control, type of epilepsy, and intelligence level.101–103 FTD has been consistently found to be related to intelligence levels in children in epilepsy populations, and results may therefore reflect general intellectual functioning rather than FTD specifically.78
FTD, Anxiety, and Affect.
The presence of FTD is negatively correlated with the diagnosis of anxiety disorder in schizophrenia; it is postulated that those affected are less prone to interpretational biases thought to underlie anxiety disorders.104 Similarly, schizophrenia patients with comorbid obsessive compulsive disorder have significantly less severe FTD and affective flattening than those without; a possible protective effect of obsessive symptoms on “psychic disintegration” is suggested.105 Docherty et al found that negative conversation topics provoked an increase in positive, but not negative, FTD to a greater extent than topics that resulted in positive affect.106 These findings were observed particularly in those with a positive family history of schizophrenia.107
Social Functioning and FTD.
Concurrent social functioning appears to be significantly affected by the presence of FTD. Among community-dwelling individuals with schizophrenia, verbal underproductivity predicts observer-rated social skills, while disconnectivity predicts social behavior in role play situations.108 Additionally, positive FTD is predicted by poor appreciation of irony and poor mind-reading, while negative FTD is predicted by poor understanding of metaphors.109 Two further studies found FTD to be the only symptom domain to impact on measures of social behavior.110,111 FTD may affect specific areas of social functioning, while sparing others; Cutting and Murphy showed that FTD was associated with poor conversational skills but had no impact on a test of knowledge of the real world.112 Notably, Cramer et al reported 2 negative studies investigating the impact of FTD on social functioning and social cognition, as did Perry et al.113–115 It is likely that negative, but not positive FTD, adversely affects objective quality of life, a construct related to social functioning.116,117
Illness Severity and FTD.
For those who demonstrate FTD, hospital admission is both more likely and significantly longer, and involuntary admission is more likely.21,37,118,119 FTD might serve as a “severity index” for those with mania because it is associated with higher psychotic symptom burden and earlier age of illness onset, although those with FTD and mania improve to the same degree as those without FTD.40 Vocisano et al also found that those with “deteriorated” affective disorder were significantly more likely to demonstrate FTD.120 Similarly, verbal disconnectedness, but not verbal productivity, is significantly more severe in those with “Kraepelinian” schizophrenia.69 Two studies have found FTD to be the sole measure of psychopathology associated with poor insight,121,122 although it is possible those exhibiting FTD are aware of their communication deficit.123 An exception to these findings is Barrera’s study, which found no significant association between insight and FTD.124
The Impact of FTD on Outcome (n = 35)
At-Risk Mental State.
The description of “cognitive slippage” in the speech of children of those with schizophrenia lead to a series of studies investigating FTD as a risk factor for the development of psychosis.125 Verbal associative processes, rather than FTD, were found not to predict transition to psychosis in high-risk individuals, however formalized assessments of FTD subsequently found otherwise.126 At 18-month follow-up, the stand-alone predictive value of FTD as a predictor of transition to psychosis in the ARMS was relatively low (hazard ratio: 2.38). When included with 5 other clinical variables, however, the prediction model had an 83.3% positive predictive value for transition.127 At 2-year follow-up, illogical thinking was uniquely predictive of conversion to psychosis (OR: 4.64).128 It has been suggested that FTD is specific to the risk of transition to schizophrenia, more so than affective disorder and, furthermore, that FTD subtypes have different associations with outcome.77,129–132 Negative FTD predicts the development of schizophrenia, regardless of genetic risk, while positive FTD is more likely to be present in those who had an affective component to their presentation.18 Overall, it appears that negative FTD better predicts conversion to schizophrenia-like psychosis than positive FTD.133,134 Investigation of thought processes in ARMS samples may help our understanding of the progression from mental health to mental illness. The understanding of normal thinking development in children continues to evolve,135 and the need for standardization of neurocognitive measures in this population has been highlighted.136
Established Psychotic Illness.
The Chicago Follow-Up Study provides the most comprehensive data on the impact of FTD on outcome in mental illness. Cohorts of up to 186 patients were followed in this study and BIT at baseline was found to have no predictive value for social outcome at 1.5, 2, and 4 years.49 Conversely, the clinical course of BIT was found to influence overall outcome, work functioning, rehospitalization, and clinical symptoms up to 18 months post-hospitalization.137,138 A more persistent course of BIT was associated with worse outcome and a dose-response relationship was also apparent. BIT has a degree of predictive value in affective disorders, but more so in schizophrenia and particularly when present in the chronic rather than the acute stages. Earlier outcome reports, from the Chicago Study, were limited by the absence of any form of controlling for confounders in statistical analysis. More recent reports from this study, in which confounders were controlled for, indicate that BIT explains only 10%–15% of the variance in social and occupational functioning.50,139 The authors acknowledge that negative symptoms have a greater impact on functioning that FTD, thereby highlighting the limited stand-alone usefulness of FTD in prognosticating functional outcomes in mental illness.
There have been few other longitudinal examinations of FTD and functional outcomes. Andreasen and Grove reported that, 6 months following admission, negative FTD was the strongest predictor of global functioning, while positive FTD had no significant correlation.4 Docherty et al demonstrated that psychotic symptoms at follow-up were predicted by the baseline presence of low verbal productivity in those with schizophrenia or reference failure in those with mania.140 Tirupati et al found that for community-dwelling, newly diagnosed patients with schizophrenia, FTD predicted worse global outcome at 1 year.141 Similarly, Knight et al reported that incoherence was correlated with global clinical outcome in schizophrenia.142 Within a chronically institutionalized cohort, verbal underproductivity predicted impaired social skills at 2.5-year follow-up to a greater extent than disconnected speech.143 In an ARMS cohort, role functioning was predicted by referential cohesion, while social role functioning was predicted by poverty of content of speech at follow-up.128 It is apparent from these studies that the predictive value of FTD, with respect to functional outcomes, is related to the presence of negative FTD rather than disorganized speech.
Wilcox et al found that FTD was the only variable to predict relapse in depression (7-year follow-up), manic psychosis (3 years), schizophrenia (2 years), and new-onset psychosis (10 and 20 years).46,144–146 Negative FTD predicted relapse to a greater extent than did positive FTD. In new-onset psychosis, negative FTD predicted both clinical outcomes (rehospitalization and BPRS score) and employment status. Positive FTD, however, was found to have “little prognostic value” in this study.46 Jorgensen and Aagaard found that FTD predicted relapse in psychosis, and Harvey et al reported that negative FTD predicted the presence of psychosis at follow-up in those with schizophrenia, although not in those with mania.64,147 Lastly, the presence of baseline FTD was shown to predict failed outpatient treatment of mania after 1 month.148 There are several examples of negative findings in the literature, with respect to the predictive value of FTD in schizophrenia, for follow-up periods up to 15 years in duration.58,149–151
Discussion
Choice of Rating Scale
Most clinical and epidemiological FTD research has employed the TLC scale, however it reflects acute clinical states and is relatively insensitive to more subtle forms of speech disturbance, as discussed by Docherty.152 The use of multiple scales is preferable when exploring the association between FTD and neuropsychological deficits or functioning. While many have argued that FTD reflects a language deficit, some have found that ratings of FTD are weakly, or not at all, related to linguistic variables such as fluency, complexity, and cohesion.153,154 Further comparative studies of the TLC scale with other FTD scales, and more sophisticated neurolinguistic assessments, are required. Assessment of speech is influenced by the choice of clinical scale employed, as well as the rating clinician, and investigators need to demonstrate adequate interrater reliability in FTD assessment.155
Conceptualization of FTD
Although there is still no consensus factor structure for FTD, it is likely to comprise abnormalities related to the organization, rate, impoverishment, and degree of idi- osyncrasy of speech. The construct of FTD described in daily clinical practice, however, is represented mostly by positive FTD or the disorganized domain of FTD. When considered in isolation, the acute thought-disordered state resolves in most individuals, but FTD may also be considered a trait marker, or endophenotype, of psychosis.156 As it exists along a continuum with normal speech, FTD exhibits characteristics both of a categorical and dimensional form of psychopathology. Factor analyses have found that FTD generally loads on the disorganization symptom dimension, together with bizarre behavior, inappropriate affect and, perhaps, inattention.157–159 This dimension explains a greater amount of the variance of psychotic symptoms than FTD alone. While some studies of psychopathology in early psychosis have identified a disorganization dimension,160,161 not all do,162 suggesting that this dimension may evolve over the course of psychosis.
The descriptor, “formal,” in the term FTD helps distinguish disorganization in the flow of speech (ie, FTD) from abnormalities in speech content (eg, delusions, which some still describe as a type of thought disorder). There is an argument, however, for revising the term FTD to that of “speech disorder.”163 Another issue with respect to FTD terminology relates to negative FTD, which has clinical correlates distinct from that of disorganized speech, and is also likely to have distinct neurocognitive and neuroimaging underpinnings.164,165 Negative FTD, therefore, is not simply the opposite of positive thought disorder. It is comprised mainly of poverty of speech and may be more appropriately classified as a type of negative symptom, ie, alogia, as it is in the DSM-V. Ultimately, diagnostic systems should emphasize relative severities of symptoms rather than absolute presence or absence; the ratio of negative to disorganized FTD is a case in point.
Epidemiology of FTD
Accurate prevalence data for FTD are lacking, for the reasons outlined. Nonetheless, an estimate of clinically significant FTD prevalence is 27.4%, as reported by Howard et al. FTD is very rare in late-onset psychotic illnesses and remains stable in early-onset illness; this phenotypic difference in clinical presentation warrants further investigation from the perspective of putative neurocognitive and neurobiological explanations. We could identify only one case report in the literature of speech and language intervention in an adult with schizophrenia and FTD.166 If this intervention is to be considered in the treatment of those with speech disorders, a more detailed understanding of the extent of speech disorders, as well as their associated functional impairments, needs to be established.
Phenomenology of FTD and Implications for Clinicians
Categorical differences between diagnoses, with respect to FTD, do not exist, and clinicians should focus on a more dimensional assessment of speech in mental illness. The relative severity of disorganized, idiosyncratic, pressured, and impoverished speech is likely to be a key factor in differentiating between schizophreniform and mood disorders. It may also be useful to consider disorganized speech a trait marker in the presentation of mental illness and an indicator of increased risk of transition to psychosis in those with ARMS. Much of the prognostic value of FTD quoted in the literature reflects the effect of negative FTD; the evidence for positive FTD having strong prognostic value is relatively weaker, unless it persists over time. The main prognostic value of positive FTD seems to be its ability to predict a more severe symptomatic course of illness.
Directions for Future FTD Research
There is a need to evaluate the factor structure of FTD in mixed diagnostic samples, for those in the early stages of psychosis and, if possible, in unmedicated individuals. Validation of the TLC scale in normal population samples, including among relatives of patients with psychosis, should be carried out. This would help to clarify the role of FTD as an endophenotype and to establish TLC scale cutoff scores. Improved understanding of the development of normal thinking processes in children would complement the existing literature on speech disturbance in the ARMS. Significant advances have been made in the area of neurolinguistics, and there is a need for comparative studies of the TLC scale with more sophisticated neurolinguistic assessments.167,168 Distillation of the FTD clinical phenotype will help to guide future research examining its neurolinguistic and neurobiological underpinnings, as well as its impact on functioning. Lastly, research into interventions, other than antipsychotic medication, are warranted, given the impact of FTD on outcome and its persistence in subgroups of patients, despite standard treatment.
Funding
Health Research Board of Ireland (grant reference code HPF-2013-468).
Acknowledgments
We would like to acknowledge Carla Senf and Angela Kearney, from the St John of God Hospital Library Service, for their assistance in sourcing articles included in this review. We also thank Mr Andrew King, from the School of English in Trinity College Dublin, for proof-reading the final manuscript. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Bleuler E. Dementia Praecox or the Group of Schizophrenias. Translated by Zinkin J. New York: International Universities Press; 1958. [Google Scholar]
- 2. DeLisi LE. Speech disorder in schizophrenia: review of the literature and exploration of its relation to the uniquely human capacity for language. Schizophr Bull. 2001;27:481–496. [DOI] [PubMed] [Google Scholar]
- 3. Kerns JG, Berenbaum H. Cognitive impairments associated with formal thought disorder in people with schizophrenia. J Abnorm Psychol. 2002;111:211–224. [PubMed] [Google Scholar]
- 4. Andreasen NC, Grove WM. Thought, language, and communication in schizophrenia: diagnosis and prognosis. Schizophr Bull. 1986;12:348–359. [DOI] [PubMed] [Google Scholar]
- 5. Pomarol-Clotet E, Oh TM, Laws KR, McKenna PJ. Semantic priming in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2008;192:92–97. [DOI] [PubMed] [Google Scholar]
- 6. Leube D, Whitney C, Kircher T. The neural correlates of ego-disturbances (passivity phenomena) and formal thought disorder in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2008;258(suppl 5):22–27. [DOI] [PubMed] [Google Scholar]
- 7. Levy DL, Coleman MJ, Sung H, et al. The Genetic Basis of Thought Disorder and Language and Communication Disturbances in Schizophrenia. J Neurolinguistics. 2010;23:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Adler CM, Goldberg TE, Malhotra AK, Pickar D, Breier A. Effects of ketamine on thought disorder, working memory, and semantic memory in healthy volunteers. Biol Psychiatry. 1998;43:811–816. [DOI] [PubMed] [Google Scholar]
- 9. Adler CM, Malhotra AK, Elman I, et al. Comparison of ketamine-induced thought disorder in healthy volunteers and thought disorder in schizophrenia. Am J Psychiatry. 1999;156:1646–1649. [DOI] [PubMed] [Google Scholar]
- 10. Heckers S, Barch DM, Bustillo J, et al. Structure of the psychotic disorders classification in DSM-5. Schizophr Res. 2013;150:11–14. [DOI] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Open Med 2009;3:e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 12. Simpson DM, Davis GC. Measuring thought disorder with clinical rating scales in schizophrenic and nonschizophrenic patients. Psychiatry Res. 1985;15:313–318. [DOI] [PubMed] [Google Scholar]
- 13. Andreasen NC. Thought, language, and communication disorders. II. Diagnostic significance. Arch Gen Psychiatry. 1979;36:1325–1330. [DOI] [PubMed] [Google Scholar]
- 14. Berenbaum H, Oltmanns TF, Gottesman II. Formal thought disorder in schizophrenics and their twins. J Abnorm Psychol. 1985;94:3–16. [DOI] [PubMed] [Google Scholar]
- 15. Liddle PF, Ngan ET, Caissie SL, et al. Thought and Language Index: an instrument for assessing thought and language in schizophrenia. Br J Psychiatry. 2002;181:326–330. [DOI] [PubMed] [Google Scholar]
- 16. Gordinier SW, Docherty NM. Factor analysis of the Communication Disturbances Index. Psychiatry Res. 2001;101:55–62. [DOI] [PubMed] [Google Scholar]
- 17. Taylor MA, Reed R, Berenbaum S. Patterns of speech disorders in schizophrenia and mania. J Nerv Ment Dis. 1994;182:319–326. [DOI] [PubMed] [Google Scholar]
- 18. Ott SL, Roberts S, Rock D, Allen J, Erlenmeyer-Kimling L. Positive and negative thought disorder and psychopathology in childhood among subjects with adulthood schizophrenia. Schizophr Res. 2002;58:231–239. [DOI] [PubMed] [Google Scholar]
- 19. Peralta V, Cuesta MJ, de Leon J. Formal thought disorder in schizophrenia: a factor analytic study. Compr Psychiatry. 1992;33:105–110. [DOI] [PubMed] [Google Scholar]
- 20. Harvey PD, Lenzenweger MF, Keefe RS, Pogge DL, Serper MR, Mohs RC. Empirical assessment of the factorial structure of clinical symptoms in schizophrenic patients: formal thought disorder. Psychiatry Res. 1992;44:141–151. [DOI] [PubMed] [Google Scholar]
- 21. Andreou C, Bozikas VP, Papouliakos I, et al. Factor structure of the Greek translation of the Scale for the Assessment of Thought, Language and Communication. Aust N Z J Psychiatry. 2008;42:636–642. [DOI] [PubMed] [Google Scholar]
- 22. Barrera A, McKenna PJ, Berrios GE. Two new scales of formal thought disorder in schizophrenia. Psychiatry Res. 2008;157:225–234. [DOI] [PubMed] [Google Scholar]
- 23. Cuesta MJ, Peralta V. Thought disorder in schizophrenia. Testing models through confirmatory factor analysis. Eur Arch Psychiatry Clin Neurosci. 1999;249:55–61. [DOI] [PubMed] [Google Scholar]
- 24. Cuesta MJ, Peralta V. Testing the hypothesis that formal thought disorders are severe mood disorders. Schizophr Bull. 2011;37:1136–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Parnas J, Schulsinger H. Continuity of formal thought disorder from childhood to adulthood in a high-risk sample. Acta Psychiatr Scand. 1986;74:246–251. [DOI] [PubMed] [Google Scholar]
- 26. Andreasen NC. Scale for the assessment of thought, language, and communication (TLC). Schizophr Bull. 1986;12:473–482. [DOI] [PubMed] [Google Scholar]
- 27. Davis GC, Simpson DM, Foster D, Arison Z, Post M. Reliability of Andreasen’s thought, language and communications disorder scale. Hillside J Clin Psychiatry. 1986;8:25–33. [PubMed] [Google Scholar]
- 28. Andreasen NC. Thought, language, and communication disorders. I. Clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36:1315–1321. [DOI] [PubMed] [Google Scholar]
- 29. Andreasen NC. The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA: The University of Iowa Press; 1983. [Google Scholar]
- 30. Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS). Iowa City, IA: The University of Iowa Press; 1983. [Google Scholar]
- 31. Johnston MH, Holzman PS. Assessing Schizophrenic Thinking. San Francisco, CA: Jossey-Bass; 1979. [Google Scholar]
- 32. Docherty NM, DeRosa M, Andreasen NC. Communication disturbances in schizophrenia and mania. Arch Gen Psychiatry. 1996;53:358–364. [DOI] [PubMed] [Google Scholar]
- 33. Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 34. Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep 1962;10:799–812. [Google Scholar]
- 35. Wing JK, Cooper JE, Sartorius N. The Measurement and Classification of Psychiatric Symptoms. Cambridge: Cambridge University Press; 1974. [Google Scholar]
- 36. Spohn HE, Coyne L, Larson J, Mittleman F, Spray J, Hayes K. Episodic and residual thought pathology in chronic schizophrenics: effect of neuroleptics. Schizophr Bull. 1986;12:394–407. [DOI] [PubMed] [Google Scholar]
- 37. Breier A, Berg PH. The psychosis of schizophrenia: prevalence, response to atypical antipsychotics, and prediction of outcome. Biol Psychiatry. 1999;46:361–364. [DOI] [PubMed] [Google Scholar]
- 38. Marengo J, Harrow M. Thought disorder. A function of schizophrenia, mania, or psychosis? J Nerv Ment Dis. 1985;173:35–41. [PubMed] [Google Scholar]
- 39. Hoffman RE, Stopek S, Andreasen NC. A comparative study of manic vs schizophrenic speech disorganization. Arch Gen Psychiatry. 1986;43:831–838. [DOI] [PubMed] [Google Scholar]
- 40. Jampala VC, Taylor MA, Abrams R. The diagnostic implications of formal thought disorder in mania and schizophrenia: a reassessment. Am J Psychiatry. 1989;146:459–463. [DOI] [PubMed] [Google Scholar]
- 41. Harvey PD, Earle-Boyer EA, Wielgus MS. The consistency of thought disorder in mania and schizophrenia. An assessment of acute psychotics. J Nerv Ment Dis. 1984;172:458–463. [DOI] [PubMed] [Google Scholar]
- 42. Oltmanns TF, Murphy R, Berenbaum H, Dunlop SR. Rating verbal communication impairment in schizophrenia and affective disorders. Schizophr Bull. 1985;11:292–299. [DOI] [PubMed] [Google Scholar]
- 43. Marengo JT, Harrow M. Schizophrenic thought disorder at follow-up. A persistent or episodic course? Arch Gen Psychiatry. 1987;44:651–659. [DOI] [PubMed] [Google Scholar]
- 44. Howard R, Castle D, Wessely S, Murray R. A comparative study of 470 cases of early-onset and late-onset schizophrenia. Br J Psychiatry. 1993;163:352–357. [DOI] [PubMed] [Google Scholar]
- 45. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 46. Wilcox J, Winokur G, Tsuang M. Predictive value of thought disorder in new-onset psychosis. Compr Psychiatry. 2012;53:674–678. [DOI] [PubMed] [Google Scholar]
- 47. Remberk B, Namysłowska I, Rybakowski F. Cognitive impairment and formal thought disorders in parents of early-onset schizophrenia patients. Neuropsychobiology. 2012;65:206–215. [DOI] [PubMed] [Google Scholar]
- 48. Harrow M, Silverstein M, Marengo J. Disordered thinking. Arch Gen Psychiatry. 1983;40:765–771. [DOI] [PubMed] [Google Scholar]
- 49. Harrow M, Marengo JT. Schizophrenic thought disorder at followup: its persistence and prognostic significance. Schizophr Bull. 1986;12:373–393. [DOI] [PubMed] [Google Scholar]
- 50. Marengo JT, Harrow M. Longitudinal courses of thought disorder in schizophrenia and schizoaffective disorder. Schizophr Bull. 1997;23:273–285. [DOI] [PubMed] [Google Scholar]
- 51. Harrow M, Grossman LS, Silverstein ML, Meltzer HY, Kettering RL. A longitudinal study of thought disorder in manic patients. Arch Gen Psychiatry. 1986;43:781–785. [DOI] [PubMed] [Google Scholar]
- 52. Harrow M, Quinlan D. Disordered Thinking and Schizophrenic Psychopathology. Gardner Press; 1985. [Google Scholar]
- 53. Marengo JT, Harrow M, Lanin-Kettering I, Wilson A. Evaluating bizarre-idiosyncratic thinking: a comprehensive index of positive thought disorder. Schizophr Bull. 1986;12:497–511. [DOI] [PubMed] [Google Scholar]
- 54. Mercado CL, Johannesen JK, Bell MD. Thought disorder severity in compromised, deteriorated, and preserved intellectual course of schizophrenia. J Nerv Ment Dis. 2011;199:111–116. [DOI] [PubMed] [Google Scholar]
- 55. Bowie CR, Tsapelas I, Friedman J, Parrella M, White L, Harvey PD. The longitudinal course of thought disorder in geriatric patients with chronic schizophrenia. Am J Psychiatry. 2005;162:793–795. [DOI] [PubMed] [Google Scholar]
- 56. Winokur G, Scharfetter C, Angst J. Stability of psychotic symptomatology (delusions, hallucinations), affective syndromes, and schizophrenic symptoms (thought disorder, incongruent affect) over episodes in remitting psychoses. Eur Arch Psychiatry Neurol Sci. 1985;234:303–307. [DOI] [PubMed] [Google Scholar]
- 57. Fenton WS, McGlashan TH. Antecedents, symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151:351–356. [DOI] [PubMed] [Google Scholar]
- 58. Parnas J, Jørgensen A, Teasdale TW, Schulsinger F, Mednick SA. Temporal course of symptoms and social functioning in relapsing schizophrenics: a 6-year follow-up. Compr Psychiatry. 1988;29:361–371. [DOI] [PubMed] [Google Scholar]
- 59. Fusar-Poli P, Broome MR, Woolley JB, et al. Altered brain function directly related to structural abnormalities in people at ultra high risk of psychosis: longitudinal VBM-fMRI study. J Psychiatr Res. 2011;45:190–198. [DOI] [PubMed] [Google Scholar]
- 60. Gouzoulis-Mayfrank E, Voss T, Mörth D, Thelen B, Spitzer M, Meincke U. Semantic hyperpriming in thought-disordered patients with schizophrenia: state or trait?–a longitudinal investigation. Schizophr Res. 2003;65:65–73. [DOI] [PubMed] [Google Scholar]
- 61. Ragin AB, Oltmanns TF. Communicability and thought disorder in schizophrenics and other diagnostic groups. A follow-up study. Br J Psychiatry. 1987;150:494–500. [DOI] [PubMed] [Google Scholar]
- 62. Earle-Boyer EA, Levinson JC, Grant R, Harvey PD. The consistency of thought disorder in mania and schizophrenia. II. An assessment at consecutive admissions. J Nerv Ment Dis. 1986;174:443–447. [DOI] [PubMed] [Google Scholar]
- 63. Docherty NM, Cohen AS, Nienow TM, Dinzeo TJ, Dangelmaier RE. Stability of formal thought disorder and referential communication disturbances in schizophrenia. J Abnorm Psychol. 2003;112:469–475. [DOI] [PubMed] [Google Scholar]
- 64. Harvey PD, Docherty NM, Serper MR, Rasmussen M. Cognitive deficits and thought disorder: II. An 8-month followup study. Schizophr Bull. 1990;16:147–156. [DOI] [PubMed] [Google Scholar]
- 65. Metsänen M, Wahlberg KE, Hakko H, Saarento O, Tienari P. Thought Disorder Index: a longitudinal study of severity levels and schizophrenia factors. J Psychiatr Res. 2006;40:258–266. [DOI] [PubMed] [Google Scholar]
- 66. Harrow M, Grossman LS, Silverstein ML, Meltzer HY. Thought pathology in manic and schizophrenic patients. Its occurrence at hospital admission and seven weeks later. Arch Gen Psychiatry. 1982;39:665–671. [DOI] [PubMed] [Google Scholar]
- 67. Solovay MR, Shenton ME, Holzman PS. Comparative studies of thought disorders. I. Mania and schizophrenia. Arch Gen Psychiatry. 1987;44:13–20. [DOI] [PubMed] [Google Scholar]
- 68. Taylor MA, Amir N. Are schizophrenia and affective disorder related?: the problem of schizoaffective disorder and the discrimination of the psychoses by signs and symptoms. Compr Psychiatry. 1994;35:420–429. [DOI] [PubMed] [Google Scholar]
- 69. Keefe RS, Frescka E, Apter SH, et al. Clinical characteristics of Kraepelinian schizophrenia: replication and extension of previous findings. Am J Psychiatry. 1996;153:806–811. [DOI] [PubMed] [Google Scholar]
- 70. Mazumdar PK, Chaturvedi SK, Gopinath PS. A study of thought disorder in paranoid and non-paranoid schizophrenia. Psychopathology. 1991;24:166–169. [DOI] [PubMed] [Google Scholar]
- 71. Shenton ME, Solovay MR, Holzman P. Comparative studies of thought disorders. II. Schizoaffective disorder. Arch Gen Psychiatry. 1987;44:21–30. [DOI] [PubMed] [Google Scholar]
- 72. Holzman PS, Shenton ME, Solovay MR. Quality of thought disorder in differential diagnosis. Schizophr Bull. 1986;12:360–371. [DOI] [PubMed] [Google Scholar]
- 73. Daniels EK, Shenton ME, Holzman PS, et al. Patterns of thought disorder associated with right cortical damage, schizophrenia, and mania. Am J Psychiatry. 1988;145:944–949. [DOI] [PubMed] [Google Scholar]
- 74. Wykes T, Leff J. Disordered speech: differences between manics and schizophrenics. Brain Lang. 1982;15:117–124. [DOI] [PubMed] [Google Scholar]
- 75. Russell AT. The clinical presentation of childhood-onset schizophrenia. Schizophr Bull. 1994;20:631–646. [DOI] [PubMed] [Google Scholar]
- 76. Green WH, Padron-Gayol M, Hardesty AS, Bassiri M. Schizophrenia with childhood onset: a phenomenological study of 38 cases. J Am Acad Child Adolesc Psychiatry. 1992;31:968–976. [DOI] [PubMed] [Google Scholar]
- 77. Caplan R, Guthrie D, Fish B, Tanguay PE, David-Lando G. The Kiddie Formal Thought Disorder Rating Scale: clinical assessment, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1989;28:408–416. [DOI] [PubMed] [Google Scholar]
- 78. de Bruin EI, Verheij F, Wiegman T, Ferdinand RF. Assessment of formal thought disorder: the relation between the Kiddie Formal Thought Disorder Rating Scale and clinical judgment. Psychiatry Res. 2007;149:239–246. [DOI] [PubMed] [Google Scholar]
- 79. McElroy SL, Strakowski SM, West SA, Keck PE, Jr, McConville BJ. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry. 1997;154:44–49. [DOI] [PubMed] [Google Scholar]
- 80. Patel NC, Delbello MP, Keck PE, Jr, Strakowski SM. Phenomenology associated with age at onset in patients with bipolar disorder at their first psychiatric hospitalization. Bipolar Disord. 2006;8:91–94. [DOI] [PubMed] [Google Scholar]
- 81. Schultz SK, Miller DD, Oliver SE, Arndt S, Flaum M, Andreasen NC. The life course of schizophrenia: age and symptom dimensions. Schizophr Res. 1997;23:15–23. [DOI] [PubMed] [Google Scholar]
- 82. Pearlson GD, Kreger L, Rabins PV, et al. A chart review study of late-onset and early-onset schizophrenia. Am J Psychiatry. 1989;146:1568–1574. [DOI] [PubMed] [Google Scholar]
- 83. Almeida OP, Howard RJ, Levy R, David AS. Psychotic states arising in late life (late paraphrenia) psychopathology and nosology. Br J Psychiatry. 1995;166:205–214. [DOI] [PubMed] [Google Scholar]
- 84. Howard R, Almeida O, Levy R. Phenomenology, demography and diagnosis in late paraphrenia. Psychol Med. 1994;24:397–410. [DOI] [PubMed] [Google Scholar]
- 85. Brodaty H, Sachdev P, Rose N, Rylands K, Prenter L. Schizophrenia with onset after age 50 years. I: phenomenology and risk factors. Br J Psychiatry. 1999;175:410–415. [DOI] [PubMed] [Google Scholar]
- 86. Ostling S, Skoog I. Psychotic symptoms and paranoid ideation in a nondemented population-based sample of the very old. Arch Gen Psychiatry. 2002;59:53–59. [DOI] [PubMed] [Google Scholar]
- 87. Ostling S, Börjesson-Hanson A, Skoog I. Psychotic symptoms and paranoid ideation in a population-based sample of 95-year-olds. Am J Geriatr Psychiatry. 2007;15:999–1004. [DOI] [PubMed] [Google Scholar]
- 88. Harvey PD, Lombardi J, Leibman M, et al. Age-related differences in formal thought disorder in chronically hospitalized schizophrenic patients: a cross-sectional study across nine decades. Am J Psychiatry. 1997;154:205–210. [DOI] [PubMed] [Google Scholar]
- 89. Maeda K, Kasai K, Uetsuki M, et al. Increased positive thought disorder with illness duration in patients with schizophrenia. Psychiatry Clin Neurosci. 2007;61:687–690. [DOI] [PubMed] [Google Scholar]
- 90. Mazumdar PK, Chaturvedi SK, Gopinath PS. Thought disorder and its correlation with clinicodemographic variables in schizophrenia. Psychopathology. 1994;27:37–42. [DOI] [PubMed] [Google Scholar]
- 91. Sobin C, Roos JL, Pretorius H, Lundy LS, Karayiorgou M. A comparison study of early non-psychotic deviant behavior in Afrikaner and US patients with schizophrenia or schizoaffective disorder. Psychiatry Res. 2003;117:113–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Mazumdar PK, Chaturvedi SK, Gopinath PS. A study of thought, language and communication (T.L.C) disorders in schizophrenia. Indian J Psychiatry. 1988;30:263–274. [PMC free article] [PubMed] [Google Scholar]
- 93. Stone JM, Fisher HL, Major B, et al. Cannabis use and first-episode psychosis: relationship with manic and psychotic symptoms, and with age at presentation. Psychol Med 2013;1–8. [DOI] [PubMed] [Google Scholar]
- 94. Boydell J, Dean K, Dutta R, Giouroukou E, Fearon P, Murray R. A comparison of symptoms and family history in schizophrenia with and without prior cannabis use: implications for the concept of cannabis psychosis. Schizophr Res. 2007;93:203–210. [DOI] [PubMed] [Google Scholar]
- 95. Soyka M, Albus M, Immler B, Kathmann N, Hippius H. Psychopathology in dual diagnosis and non-addicted schizophrenics–are there differences? Eur Arch Psychiatry Clin Neurosci. 2001;251:232–238. [DOI] [PubMed] [Google Scholar]
- 96. Bersani G, Orlandi V, Kotzalidis GD, Pancheri P. Cannabis and schizophrenia: impact on onset, course, psychopathology and outcomes. Eur Arch Psychiatry Clin Neurosci. 2002;252:86–92. [DOI] [PubMed] [Google Scholar]
- 97. Caspari D. Cannabis and schizophrenia: results of a follow-up study. Eur Arch Psychiatry Clin Neurosci. 1999;249:45–49. [DOI] [PubMed] [Google Scholar]
- 98. Bühler B, Hambrecht M, Löffler W, an der Heiden W, Häfner H. Precipitation and determination of the onset and course of schizophrenia by substance abuse–a retrospective and prospective study of 232 population-based first illness episodes. Schizophr Res. 2002;54:243–251. [DOI] [PubMed] [Google Scholar]
- 99. Rosenthal RN, Miner CR. Differential diagnosis of substance-induced psychosis and schizophrenia in patients with substance use disorders. Schizophr Bull. 1997;23:187–193. [DOI] [PubMed] [Google Scholar]
- 100. Cornelius JR, Mezzich J, Fabrega H, Jr, Cornelius MD, Myers J, Ulrich RF. Characterizing organic hallucinosis. Compr Psychiatry. 1991;32:338–344. [DOI] [PubMed] [Google Scholar]
- 101. Caplan R, Guthrie D, Komo S, et al. Social communication in children with epilepsy. J Child Psychol Psychiatry. 2002;43:245–253. [DOI] [PubMed] [Google Scholar]
- 102. Caplan R, Arbelle S, Guthrie D, et al. Formal thought disorder and psychopathology in pediatric primary generalized and complex partial epilepsy. J Am Acad Child Adolesc Psychiatry. 1997;36:1286–1294. [DOI] [PubMed] [Google Scholar]
- 103. Caplan R, Guthrie D, Shields WD, Mori L. Formal thought disorder in pediatric complex partial seizure disorder. J Child Psychol Psychiatry. 1992;33:1399–1412. [DOI] [PubMed] [Google Scholar]
- 104. Huppert JD, Smith TE. Anxiety and schizophrenia: the interaction of subtypes of anxiety and psychotic symptoms. CNS Spectr. 2005;10:721–731. [DOI] [PubMed] [Google Scholar]
- 105. Poyurovsky M, Fuchs C, Weizman A. Obsessive-compulsive disorder in patients with first-episode schizophrenia. Am J Psychiatry. 1999;156:1998–2000. [DOI] [PubMed] [Google Scholar]
- 106. Docherty NM, Evans IM, Sledge WH, Seibyl JP, Krystal JH. Affective reactivity of language in schizophrenia. J Nerv Ment Dis. 1994;182:98–102. [DOI] [PubMed] [Google Scholar]
- 107. Docherty NM, Grosh ES, Wexler BE. Affective reactivity of cognitive functioning and family history in schizophrenia. Biol Psychiatry. 1996;39:59–64. [DOI] [PubMed] [Google Scholar]
- 108. Bowie CR, Gupta M, Holshausen K. Disconnected and underproductive speech in schizophrenia: unique relationships across multiple indicators of social functioning. Schizophr Res. 2011;131:152–156. [DOI] [PubMed] [Google Scholar]
- 109. Langdon R, Coltheart M, Ward PB, Catts SV. Disturbed communication in schizophrenia: the role of poor pragmatics and poor mind-reading. Psychol Med. 2002;32:1273–1284. [DOI] [PubMed] [Google Scholar]
- 110. Smith TE, Hull JW, Goodman M, et al. The relative influences of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. J Nerv Ment Dis. 1999;187:102–108. [DOI] [PubMed] [Google Scholar]
- 111. Köther U, Veckenstedt R, Vitzthum F, et al. “Don’t give me that look” - overconfidence in false mental state perception in schizophrenia. Psychiatry Res. 2012;196:1–8. [DOI] [PubMed] [Google Scholar]
- 112. Cutting J, Murphy D. Schizophrenic thought disorder. A psychological and organic interpretation. Br J Psychiatry. 1988;152:310–319. [DOI] [PubMed] [Google Scholar]
- 113. Cramer P, Weegmann M, O’Neil M. Schizophrenia and the perception of emotions. How accurately do schizophrenics judge the emotional states of others? Br J Psychiatry. 1989;155:225–228. [DOI] [PubMed] [Google Scholar]
- 114. Cramer P, Bowen J, O’Neill M. Schizophrenics and social judgement. Why do schizophrenics get it wrong? Br J Psychiatry. 1992;160:481–487. [DOI] [PubMed] [Google Scholar]
- 115. Perry W, Moore D, Braff D. Gender differences on thought disturbance measures among schizophrenic patients. Am J Psychiatry. 1995;152:1298–1301. [DOI] [PubMed] [Google Scholar]
- 116. Tan EJ, Thomas N, Rossell SL. Speech disturbances and quality of life in schizophrenia: differential impacts on functioning and life satisfaction. Compr Psychiatry. 2014;55:693–698. [DOI] [PubMed] [Google Scholar]
- 117. Ulas H, Akdede BB, Ozbay D, Alptekin K. Effect of thought disorders on quality of life in patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:332–335. [DOI] [PubMed] [Google Scholar]
- 118. Lenz G, Katschnig H, David H. Symptoms, diagnosis and time in hospital. A polydiagnostic study of schizophrenia. Psychopathology. 1986;19:253–258. [DOI] [PubMed] [Google Scholar]
- 119. Renwick L, Jackson D, Foley S, et al. Depression and quality of life in first-episode psychosis. Compr Psychiatry. 2012;53:451–455. [DOI] [PubMed] [Google Scholar]
- 120. Vocisano C, Klein DN, Keefe RS. Lifetime comorbidity, lifetime history of psychosis and suicide attempts, and current symptoms of patients with deteriorated affective disorder. Psychiatry Res. 1997;73:33–45. [DOI] [PubMed] [Google Scholar]
- 121. Baier M, DeShay E, Owens K, et al. The relationship between insight and clinical factors for persons with schizophrenia. Arch Psychiatr Nurs. 2000;14:259–265. [DOI] [PubMed] [Google Scholar]
- 122. Smith TE, Hull JW, Huppert JD, Silverstein SM, Anthony DT, McClough JF. Insight and recovery from psychosis in chronic schizophrenia and schizoaffective disorder patients. J Psychiatr Res. 2004;38:169–176. [DOI] [PubMed] [Google Scholar]
- 123. McGrath J, Allman R. Awareness and unawareness of thought disorder. Aust N Z J Psychiatry. 2000;34:35–42. [DOI] [PubMed] [Google Scholar]
- 124. Barrera A, McKenna PJ, Berrios GE. Formal thought disorder, neuropsychology and insight in schizophrenia. Psychopathology. 2009;42:264–269. [DOI] [PubMed] [Google Scholar]
- 125. Weintraub S. Risk factors in schizophrenia: the Stony Brook High-Risk Project. Schizophr Bull. 1987;13:439–450. [DOI] [PubMed] [Google Scholar]
- 126. Griffith JJ, Mednick SA, Schulsinger F, Diderichsen B. Verbal associative disturbances in children at high risk for schizophrenia. J Abnorm Psychol. 1980;89:125–131. [DOI] [PubMed] [Google Scholar]
- 127. Ruhrmann S, Schultze-Lutter F, Salokangas RK, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010;67:241–251. [DOI] [PubMed] [Google Scholar]
- 128. Bearden CE, Wu KN, Caplan R, Cannon TD. Thought disorder and communication deviance as predictors of outcome in youth at clinical high risk for psychosis. J Am Acad Child Adolesc Psychiatry. 2011;50:669–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Dworkin RH, Green SR, Small NE, Warner ML, Cornblatt BA, Erlenmeyer-Kimling L. Positive and negative symptoms and social competence in adolescents at risk for schizophrenia and affective disorder. Am J Psychiatry. 1990;147:1234–1236. [DOI] [PubMed] [Google Scholar]
- 130. Dworkin RH, Bernstein G, Kaplansky LM, et al. Social competence and positive and negative symptoms: a longitudinal study of children and adolescents at risk for schizophrenia and affective disorder. Am J Psychiatry. 1991;148:1182–1188. [DOI] [PubMed] [Google Scholar]
- 131. Arboleda C, Holzman PS. Thought disorder in children at risk for psychosis. Arch Gen Psychiatry. 1985;42:1004–1013. [DOI] [PubMed] [Google Scholar]
- 132. Gooding DC, Coleman MJ, Roberts SA, Shenton ME, Levy DL, Erlenmeyer-Kimling L. Thought disorder in offspring of schizophrenic parents: findings from the New York High-Risk Project. Schizophr Bull. 2012;38:263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Gooding DC, Ott SL, Roberts SA, Erlenmeyer-Kimling L. Thought disorder in mid-childhood as a predictor of adulthood diagnostic outcome: findings from the New York High-Risk Project. Psychol Med. 2013;43:1003–1012. [DOI] [PubMed] [Google Scholar]
- 134. Wilcox J, Briones D, Quadri S, Tsuang M. Prognostic implications of paranoia and thought disorder in new onset psychosis. Compr Psychiatry. 2014;55:813–817. [DOI] [PubMed] [Google Scholar]
- 135. Koziol LF, Lutz JT. From movement to thought: the development of executive function. Appl Neuropsychol Child. 2013;2:104–115. [DOI] [PubMed] [Google Scholar]
- 136. Konstantopoulos K, Vogazianos P, Thodi C, Nikopoulou-Smyrni P. A normative study of the Children’s Color Trails Test (CCTT) in the Cypriot population. Child Neuropsychol 2014;1–8. [DOI] [PubMed] [Google Scholar]
- 137. Harrow M, Marengo J, McDonald C. The early course of schizophrenic thought disorder. Schizophr Bull. 1986;12:208–224. [DOI] [PubMed] [Google Scholar]
- 138. Pogue-Geile MF, Harrow M. Negative and positive symptoms in schizophrenia and depression: a followup. Schizophr Bull. 1984;10:371–387. [DOI] [PubMed] [Google Scholar]
- 139. Racenstein JM, Penn D, Harrow M, Schleser R. Thought disorder and psychosocial functioning in schizophrenia: the concurrent and predictive relationships. J Nerv Ment Dis. 1999;187:281–289. [DOI] [PubMed] [Google Scholar]
- 140. Docherty N, Schnur M, Harvey PD. Reference performance and positive and negative thought disorder: a follow-up study of manics and schizophrenics. J Abnorm Psychol. 1988;97:437–442. [DOI] [PubMed] [Google Scholar]
- 141. Tirupati NS, Rangaswamy T, Raman P. Duration of untreated psychosis and treatment outcome in schizophrenia patients untreated for many years. Aust N Z J Psychiatry. 2004;38:339–343. [DOI] [PubMed] [Google Scholar]
- 142. Knight RA, Elliott DS, Roff JD, Watson CG. Concurrent and predictive validity of components of disordered thinking in schizophrenia. Schizophr Bull. 1986;12:427–446. [DOI] [PubMed] [Google Scholar]
- 143. Bowie CR, Harvey PD. Communication abnormalities predict functional outcomes in chronic schizophrenia: differential associations with social and adaptive functions. Schizophr Res. 2008;103:240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Wilcox JA, Ramirez AL, Baida-Fragoso N. The prognostic value of thought disorder in psychotic depression. Ann Clin Psychiatry. 2000;12:1–4. [DOI] [PubMed] [Google Scholar]
- 145. Wilcox JA. The predictive value of thought disorder in manic psychosis. Psychopathology. 1992;25:161–165. [DOI] [PubMed] [Google Scholar]
- 146. Wilcox JA. Thought disorder and relapse in schizophrenia. Psychopathology. 1990;23:153–156. [DOI] [PubMed] [Google Scholar]
- 147. Jørgensen P, Aagaard J. Clinical predictors of course and outcome in delusional psychosis. Acta Psychiatr Scand. 1988;77:332–337. [DOI] [PubMed] [Google Scholar]
- 148. Young RC, Nysewander RW, Schreiber MT. Mania ratings at discharge from hospital: a follow-up. J Nerv Ment Dis. 1982;170:638–639. [DOI] [PubMed] [Google Scholar]
- 149. Tsoi WF, Wong KE. A 15-year follow-up study of Chinese schizophrenic patients. Acta Psychiatr Scand. 1991;84:217–220. [DOI] [PubMed] [Google Scholar]
- 150. Tsoi WF, Kua EH. Predicting the outcome of schizophrenia ten years later. Aust N Z J Psychiatry. 1992;26:257–261. [PubMed] [Google Scholar]
- 151. Foo TW, Hoo TK. Selection of chronic schizophrenic patients for rehabilitation. J Clin Epidemiol. 1988;41:883–887. [DOI] [PubMed] [Google Scholar]
- 152. Docherty NM. On identifying the processes underlying schizophrenic speech disorder. Schizophr Bull. 2012;38:1327–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Chaika EO. Understanding Psychotic Speech: BeyondFreud and Chomsky. Springfield, UK: Charls C. Thomas; 1990. [Google Scholar]
- 154. Lott PR, Guggenbühl S, Schneeberger A, Pulver AE, Stassen HH. Linguistic analysis of the speech output of schizophrenic, bipolar, and depressive patients. Psychopathology. 2002;35:220–227. [DOI] [PubMed] [Google Scholar]
- 155. Faber R, Abrams R, Taylor MA, Kasprison A, Morris C, Weisz R. Comparison of schizophrenic patients with formal thought disorder and neurologically impaired patients with aphasia. Am J Psychiatry. 1983;140:1348–1351. [DOI] [PubMed] [Google Scholar]
- 156. Wahlberg KE, Wynne LC, Oja H, et al. Thought Disorder Index of Finnish adoptees and communication deviance of their adoptive parents. Psychol Med. 2000;30:127–136. [DOI] [PubMed] [Google Scholar]
- 157. Andreasen NC, Arndt S, Alliger R, Miller D, Flaum M. Symptoms of schizophrenia. Methods, meanings, and mechanisms. Arch Gen Psychiatry. 1995;52:341–351. [DOI] [PubMed] [Google Scholar]
- 158. Peralta V, Cuesta MJ. How many and which are the psychopathological dimensions in schizophrenia? Issues influencing their ascertainment. Schizophr Res. 2001;49:269–285. [DOI] [PubMed] [Google Scholar]
- 159. Serretti A, Olgiati P. Dimensions of major psychoses: a confirmatory factor analysis of six competing models. Psychiatry Res. 2004;127:101–109. [DOI] [PubMed] [Google Scholar]
- 160. Peralta V, Moreno-Izco L, Calvo-Barrena L, Cuesta MJ. The low- and higher-order factor structure of symptoms in patients with a first episode of psychosis. Schizophr Res. 2013;147:116–124. [DOI] [PubMed] [Google Scholar]
- 161. Vázquez-Barquero JL, Lastra I, Cuesta Nuñez MJ, Herrera Castanedo S, Dunn G. Patterns of positive and negative symptoms in first episode schizophrenia. Br J Psychiatry. 1996;168:693–701. [DOI] [PubMed] [Google Scholar]
- 162. Ventura J, Nuechterlein KH, Subotnik KL, Gutkind D, Gilbert EA. Symptom dimensions in recent-onset schizophrenia and mania: a principal components analysis of the 24-item Brief Psychiatric Rating Scale. Psychiatry Res. 2000;97:129–135. [DOI] [PubMed] [Google Scholar]
- 163. Chaika E. Thought disorder or speech disorder in schizophrenia? Schizophr Bull. 1982;8:587–594. [DOI] [PubMed] [Google Scholar]
- 164. Silverstein ML, Marengo JT, Fogg L. Two types of thought disorder and lateralized neuropsychological dysfunction. Schizophr Bull. 1991;17:679–687. [DOI] [PubMed] [Google Scholar]
- 165. Sans-Sansa B, McKenna PJ, Canales-Rodríguez EJ, et al. Association of formal thought disorder in schizophrenia with structural brain abnormalities in language-related cortical regions. Schizophr Res. 2013;146:308–313. [DOI] [PubMed] [Google Scholar]
- 166. Clegg J, Brumfitt S, Parks RW, Woodruff PW. Speech and language therapy intervention in schizophrenia: a case study. Int J Lang Commun Disord. 2007;42(suppl 1):81–101. [DOI] [PubMed] [Google Scholar]
- 167. Kuperberg GR, McGuire PK, David AS. Reduced sensitivity to linguistic context in schizophrenic thought disorder: evidence from on-line monitoring for words in linguistically anomalous sentences. J Abnorm Psychol. 1998;107:423–434. [DOI] [PubMed] [Google Scholar]
- 168. Kuperberg GR, McGuire PK, David AS. Sensitivity to linguistic anomalies in spoken sentences: a case study approach to understanding thought disorder in schizophrenia. Psychol Med. 2000;30:345–357. [DOI] [PubMed] [Google Scholar]