Abstract
Background
The treatment of post-inflammatory hyperpigmentation (PIH) remains challenging. Tranexamic acid, a well-known anti-fibrinolytic drug, has recently demonstrated a curative effect towards melasma and ultraviolet-induced PIH in Asian countries. However, the precise mechanism of its inhibitory effect on melanogenesis is not fully understood.
Objective
In order to clarify the inhibitory effect of tranexamic acid on PIH, we investigated its effects on mouse melanocytes (i.e., melan-a cells) and human melanocytes.
Methods
Melan-a cells and human melanocytes were cultured with fractional CO2 laser-treated keratinocyte-conditioned media. Melanin content and tyrosinase activity were evaluated in cells treated with or without tranexamic acid. Protein levels of tyrosinase, tyrosinase-related protein (TRP)-1, and TRP-2 were evaluated in melan-a cells. Signaling pathway molecules involved in melanogenesis in melanoma cells were also investigated.
Results
Tranexamic acid-treated melanocytes exhibited reduced melanin content and tyrosinase activity. Tranexamic acid also decreased tyrosinase, TRP-1, and TRP-2 protein levels. This inhibitory effect on melanogenesis was considered to be involved in extracellular signal-regulated kinase signaling pathways and subsequently microphthalmia-associated transcription factor degradation.
Conclusion
Tranexamic acid may be an attractive candidate for the treatment of PIH.
Keywords: Hyperpigmentation, Melanocytes, Tranexamic acid
INTRODUCTION
Pigmentation disorders are common skin diseases whose dermatologic treatment remains challenging. Although pigmentation disorders can occur in both sexes regardless of skin type, they are more problematic in people with darker complexions, such as Asians1. In this context, postinflammatory hyperpigmentation (PIH) after cosmetic procedures including laser treatment and peeling is an important issue that decreases treatment satisfaction in Asian women.
Tyrosinase is the key enzyme involved in this process and regulates the rate-limiting steps of melanogenesis2. Therefore, many studies have focused on finding tyrosinase inhibitors3. Accordingly, tyrosinase inhibitors including hydroquinone, ascorbic acid, kojic acid, and arbutin have been applied for the treatment of hyperpigmentation1. However, studies aiming to find more effective and safe treatments for hyperpigmentation are ongoing.
Tranexamic acid (trans-4-amino-methylcyclohexanecarboxylic acid, TA) has recently been used to reduce pigmentation in melasma and ultraviolet-induced hyperpigmentation4,5,6,7. TA is a well-known anti-fibrinolytic agent that inhibits the plasmin/plasminogen system; thus, it has been used to prevent blood loss during surgery8. In addition to its hemostatic effects, TA exhibits anti-allergic and anti-inflammatory effects on various skin diseases such as angioedema7. Its anti-inflammatory mechanism appears to be related to its inhibitory effect on melanogenesis6,7. However, the exact action mechanisms of TA on melanogenesis and its related pathways have not been elucidated. Moreover, most previous reports of its inhibitory effects on melanogenesis in vitro involved the condition of ultraviolet-induced hyperpigmentation using animal skin or melanocytes5,6. Therefore, it is necessary to determine the effects and mechanism of TA on laser-induced hyperpigmentation as well as on human melanocytes.
Therefore, this study investigated the effects of TA on murine and human melanocytes under laser-induced melanin production. In addition, we studied the effects of TA on the expressions of enzymes responsible for melanogenesis as well as melanogenesis-related signal transduction pathways.
MATERIALS AND METHODS
Cell culture
HaCaT keratinocytes, a spontaneously immortalized human keratinocyte cell line, were cultured in Dulbecco's modified Eagle medium supplemented with 10% heat-inactivated fetal bovine serum (FBS), 100 units/ml penicillin and 100 mg/ml streptomycin at 37℃ in a 10% CO2 atmosphere in a humidified incubator.
Murine melanocytes (melan-a cells) originally derived from C57BL/6 J (black, a/a) mice were a generous gift from Prof. Dorothy C. Bennett (St. George's Hospital, London, UK). Melan-a cells were cultured in RPMI 1640 medium (Sigma-Aldrich Co., St. Louis, MO, USA) containing 10% heat-inactivated FBS, 100 units/ml penicillin, 100 mg/ml streptomycin, and 200 nM phorbol 12-myristate 13-acetate at 37℃ in 10% CO2. The culture medium was changed twice weekly, and the cells were subcultured once weekly.
B16F10 mouse melanoma cells were obtained from the American Type Culture Collection (Manassas, VA, USA). B16F10 cells were cultured in Dulbecco's modified Eagle medium supplemented with 100 units/ml penicillin, 100 mg/ml streptomycin, and 10% FBS. The cells were then incubated in 5% CO2 at 37℃ and subcultured every 3 days.
Laser-treated keratinocyte-conditioned medium
HaCaT keratinocytes (6×104 cells/ml) were seeded in 24-well plates and treated in serum-free conditions with a fractional CO2 laser (eCO2; Lutronic, Seoul, Korea). Each treatment session used pulse energy of 100 mJ per fixed 8-mm-diameter microbeam at a density of 100 spots/cm2. After 24 hours, the supernatant medium was harvested, mixed 1:1 with RPMI 1640 medium, and supplemented with 10% heat-inactivated FBS, 100 units/ml penicillin, 100 mg/ml streptomycin, and 200 nM phorbol 12-myristate 13-acetate to make laser-treated keratinocyte-conditioned medium (LT-KCM).
Similarly, for human melanocytes (Invitrogen Co., Eugene, OR, USA), supernatant medium was harvested and mixed 1:1 with Medium 254 (Invitrogen Co.) supplemented with Human Melanocyte Growth Supplement (Invitrogen Co.) to make LT-KCM.
Measurement of inflammatory mediators in conditioned media
The concentrations of inflammatory mediators in KCM and LT-KCM, including interleukin (IL)-1α, IL-8, and prostaglandin E2 (PGE2), were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems Inc., Minneapolis, MN, USA for IL-1α and IL-8; Cayman Chemical, Ann Arbor, MI, USA for PGE2). For these assays, KCM and LT-KCM media samples were diluted in ELISA buffer (supplied by the manufacturers) to a final volume of 200 µl. ELISAs were performed according to the manufacturers' instructions.
Measurement of melanin content
The melanin contents of melan-a cells and human melanocytes grown in KCM and LT-KCM were determined. Melan-a cells (2×104 cells/ml) were seeded on 48-well plates with 10, 50, and or 100 mg/L TA (Hangzhou Huajin Pharma Co. Ltd., Hangzhou, China) in LT-KCM in triplicate. Similarly, human melanocytes (5×104 cells/ml) were seeded on 24-well plates with 10, 50, and or 100 mg/l TA in LT-KCM in triplicate.
The medium was changed daily. After 5 days of culture, the cells were lysed with 1 ml 1 N NaOH. Then, 200 ml of each crude cell extract was transferred to 96-well plates. Melanin content was measured by a microplate reader (Molecular Devices Inc., Sunnyvale, CA, USA) at 405 nm and adjusted by total protein content in consideration of cell viability. Protein content was determined by the Bradford method using Bio-Rad protein assay kit (Bio-Rad Laboratories Inc., Hercules, CA, USA). Arbutin (Sigma-Aldrich Co.), a well-known melanogenesis inhibitor, was used as a positive control.
Measurement of tyrosinase activity
The tyrosinase activities of melan-a cells and human melanocytes grown in KCM as well as that of melan-a cells grown in LT-KCM were determined. Melan-a cells were pretreated with arbutin and 10, 50, and or 100 mg/L TA for 3 days, washed twice with ice-cold phosphate-buffered saline, and lysed in lysis buffer (PO4 buffer 80 mM+1% Triton X-100+PMSF 100 mg/ml) for 2 hours in a deep freezer. Lysates were centrifuged at 12,000g for 15 minutes to remove insoluble material. Protein content was determined by the Bradford method using Bio-Rad protein assay kit. A 50-µl aliquot of the samples was mixed with 100 ml sodium phosphate 100 mM (pH 7.0) at 37℃ for 5 minutes, followed by the addition of 50 ml l-DOPA 100 mM. After incubation at 37℃, absorbance was measured at 475 nm using a microplate reader.
Western blot analysis
Melan-a cells (5×105 cells/ml) were seeded on 60-mm culture dishes and treated with TA (10, 50, and or 100 mg/L). After 3 days of incubation, the cells were lysed with radioimmune precipitation assay buffer (Sigma-Aldrich Co.), and protein concentrations were determined using a Bio-Rad protein assay kit. Equal amounts of proteins were boiled for 3 minutes, chilled on ice, subjected to 8% to 10% sodiumdodecylsulfate-polyacrylamide gel electrophoresis (SDS-PAGE), and transferred to a nitrocellulose membrane (Amersham International, Little Chalfont, UK). After the membranes were blocked using 5% skim milk in Tris-buffered saline containing 0.1% Tween 20 for 1 hour, they were incubated with primary polyclonal anti-tyrosinase antibody, anti-tyrosinase-related protein (TRP)-1 antibody, and anti-TRP-2 antibody (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA). The membranes were subsequently incubated with the secondary antibody horseradish peroxidase-conjugated rabbit anti-goat immunoglobulin G antibody (Santa Cruz Biotechnology Inc.). Blotted antibodies were visualized by chemiluminescence (Amersham International). Anti-β-actin (Sigma-Aldrich Co.) was used as a loading control.
B16F10 cells (5×105 cells/ml) were seeded on 60-mm culture dishes, serum starved for 24 hours, washed with phosphate-buffered saline, and treated with 10 mg/ml TA for 5 minutes, 30 minutes, 3 hours, 6 hours, 24 hours, 48 hours, or 72 hours. Cells were lysed with pro-prep protein lysis buffer (Intron, Seongnam, Korea) and centrifuged at 13,000g for 10 minutes. Protein concentrations were determined using a bicinchoninic acid protein assay kit (Sigma-Aldrich Co.). Protein (15 µg) was separated by SDS-PAGE and transferred to nitrocellulose membranes, which were subsequently blocked using 5% skim milk in Tris-buffered saline containing 0.1% Tween 20. The membranes were incubated with appropriate primary antibodies including phospho-extracellular kinase and extracellular kinase (ERK) (1:1,000; Cell Signaling Technology, Danvers, MA, USA) and microphthalmia-associated transcription factor (MITF) (Abcam, Cambridge, UK) for 4 hours and then with anti-rabbit or anti-mouse horseradish peroxidase-conjugated antibody (1:2,000, Santa Cruz Biotechnology Inc.). Blotted antibodies were visualized by chemiluminescence (Pierce, Rockford, IL, USA). The membranes were re-probed with anti-β-actin antibody (1:10,000).
Image analysis was performed using ImageJ (http://rsb.info.nih.gov/ij/) to quantify the relative band density.
Statistical analysis
Statistical analyses were performed by SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Each experiment was performed at least 3 times, and the results are expressed as mean±standard deviation. The statistical significance of the differences between groups was assessed by Student's t-test. The level of significance was set at p<0.05.
RESULTS
Inflammatory mediators in conditioned media
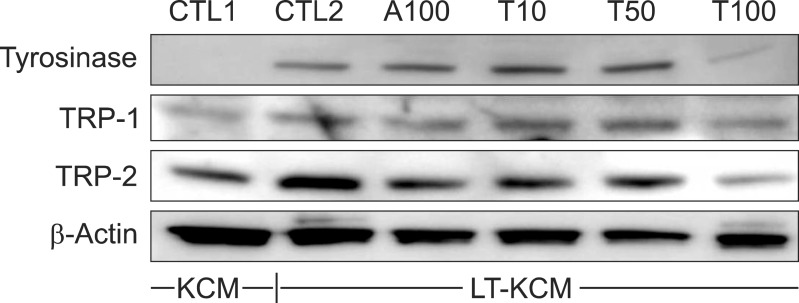
As KCM itself can induce melanogenesis7, we measured the concentrations of inflammatory mediators in both KCM and LT-KCM. IL-1α, IL-8, and PGE2, which contribute to the activation of melanocytes during inflammation9, were detected. The release of these mediators was significantly higher in LT-KCM (p<0.01), indicating laser treatment induced more inflammatory mediators (Fig. 1).
Fig. 1. Laser-treated keratinocyte-conditioned medium induced significant increases of inflammatory mediators. Inflammatory mediators including interleukin (IL)-1, IL-8, and prostaglandin E2 (PGE2) were significantly higher in laser-treated keratinocyteconditioned medium (blue) than non-treated keratinocyteconditioned medium (red). Data are mean±standard deviation. **p<0.01; Student's t-test.
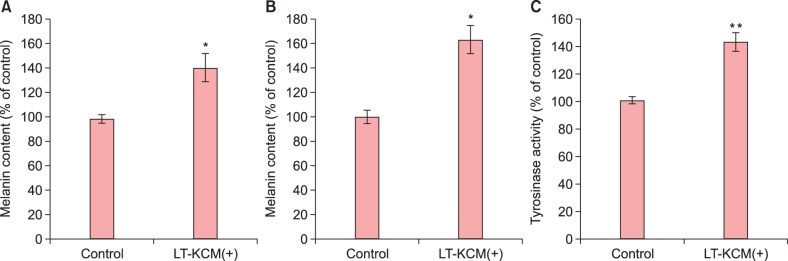
Effects of laser-treated keratinocyte-conditioned medium on melanin synthesis and tyrosinase activity
Both melan-a cells and human melanocytes grown in the presence of LT-KCM showed increased melanin content (adjusted for protein content) (Fig. 2A, B). Tyrosinase activity was significantly higher (p<0.01) in melan-a cells cultured with LT-KCM than without (Fig. 2C).
Fig. 2. Laser-treated keratinocyte-conditioned medium (LT-KCM) induced increased melanin content and tyrosinase activity. Melan-a cells and human melanocytes were cultured in the presence of LT-KCM. The melanin contents (% of control) in both melan-a cells (A) and human melanocytes (B) are shown. Tyrosinase activity (% of control) in cultured melan-a cells (C) is shown. Data are mean±standard deviation. *p<0.05, **p<0.01; Student's t-test.
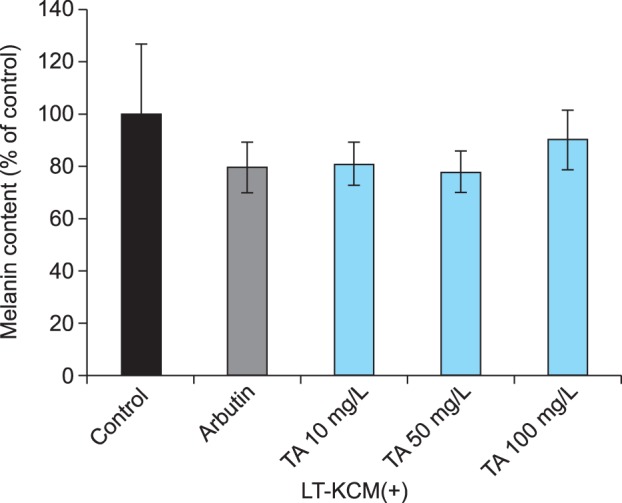
Effects of tranexamic acid on melanin synthesis and tyrosinase activity
TA inhibited melanin synthesis in LT-KCM. TA-treated melan-a cells exhibited a dose-dependent reduction in melanin content adjusted by protein content (Fig. 3). In human melanocytes grown in LT-KCM, 10, 50, and 100 mg/L. TA seemed to inhibit melanin content; however, the inhibition was not significant (p=0.296, 0.238, and 0.584, respectively; Fig. 4). Although arbutin and 100 mg/L TA markedly reduced melanin content without adjustment (data not shown), the decreased protein content affected the adjusted melanin content.
Fig. 3. Tranexamic acid (TA) decreased melanin content in melan-a cells. Melan-a cells were cultured in the presence of laser-treated keratinocyte-conditioned medium (LT-KCM). Arbutin and tranexamic acid inhibited melanin content in cultured melan-a cells. Data are mean±standard deviation. *p<0.05, **p<0.01; Student's t-test.
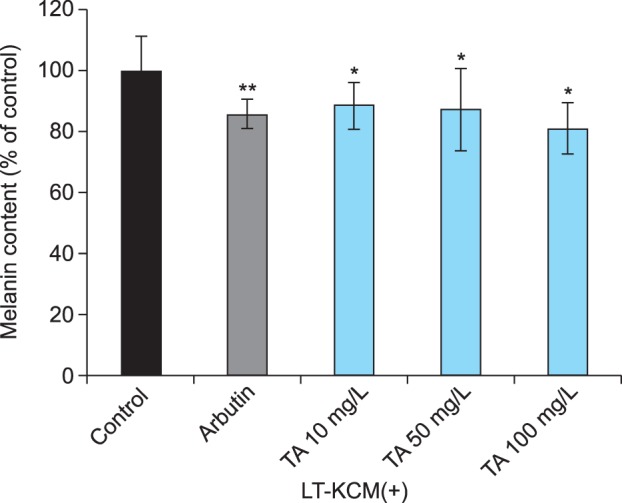
Fig. 4. Tranexamic acid (TA) decreased melanin content in human melanocytes. Human melanocytes were cultured in the presence of laser-treated keratinocyte-conditioned medium (LT-KCM). Data are mean±standard deviation.
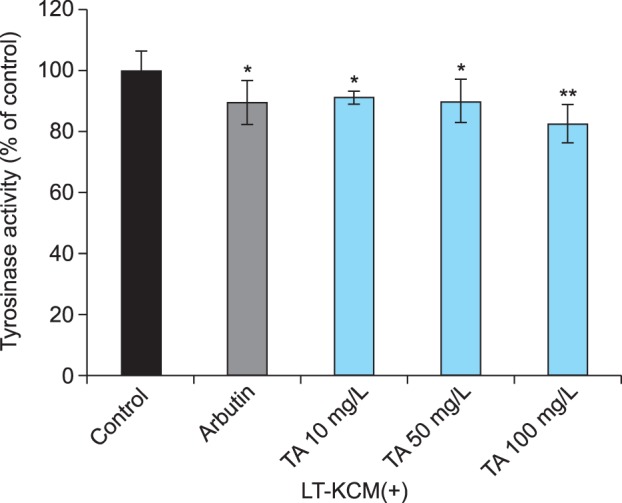
Furthermore, TA significantly reduced tyrosinase activity in melan-a cells in a dose-dependent manner (Fig. 5). This finding corresponded with the reduction in melanin content in melan-a cells (Fig. 3).
Fig. 5. Tranexamic acid (TA) reduced tyrosinase activity in melan-a cells. Melan-a cells were cultured in the presence of laser-treated keratinocyte-conditioned medium (LT-KCM). Arbutin and tranexamic acid reduced tyrosinase activity (% of control) in cultured melan-a cells. Data are mean±standard deviation. *p<0.05, **p<0.01; Student's t-test.
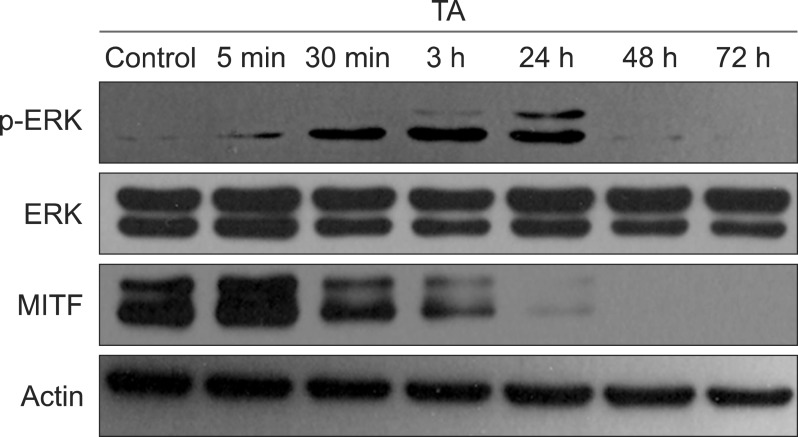
Effects of tranexamic acid on expressions of melanogenesis-related enzymes
In order to clarify the inhibitory effect of TA on melanogenesis, the protein levels of tyrosinase, TRP-1, and TRP-2 in melan-a cells were investigated by western blot analysis.
Tyrosinase, TRP-1, and TRP-2 protein levels were elevated in melan-a cells cultured with laser-treated KCM (Fig. 6). However, after TA treatment, their protein levels decreased in a dose-dependent manner, which was confirmed by image analysis quantifying the densities of each band (data not shown).
Fig. 6. Tranexamic acid (TA) decreased protein levels of melanogenesis-related enzymes. Protein levels of tyrosinase, tyrosinase-related protein (TRP)-1, and TRP-2 were higher in melan-a cells cultured with laser-treated keratinocyte-conditioned medium (LT-KCM) than keratinocyte conditioned medium (KCM) (CTL1 vs. CTL2) in western blot analysis. However, after TA treatment, their protein levels decreased in a dose-dependent manner. Arbutin (A100) was used as a positive control, and equal protein loading was confirmed by using β-actin. CTL1: control 1 (KCM without laser treatment), CTL2: control 2 (LT-KCM), A100: arbutin 100 mg/L, T10: 10 mg/L TA, T50: 50 mg/L TA, T100: 100 mg/L TA.
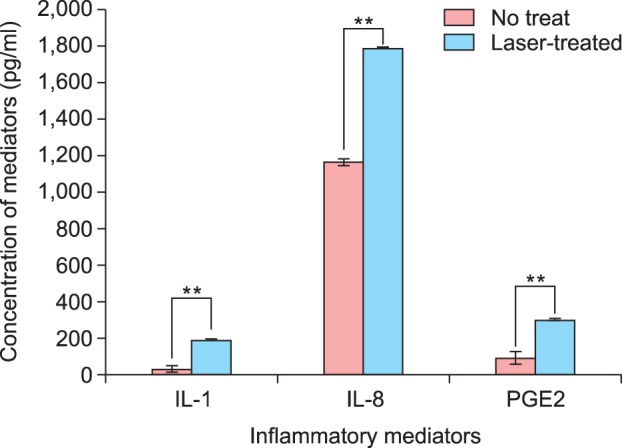
Effects of tranexamic acid on expressions of signaling pathway molecules involved in melanogenesis
On the basis of the above results, we hypothesized TA affects the expressions of MITF, which plays a key role in melanogenesis. Therefore, we evaluated MITF protein expression after TA treatment in B16F10 cells. We also studied the ERK signaling pathway, which is known to be involved in MITF phosphorylation and degradation10. TA induced sustained activation of ERK; in particular, phosphorylated ERK was elevated until 24 hours after TA treatment (Fig. 7). Meanwhile, MITF decreased in a time-dependent manner.
Fig. 7. Tranexamic acid (TA) stimulated the extracellular signal-regulated kinase (ERK) signaling pathway and decreased protein levels of microphthalmia-associated transcription factor (MITF). Protein levels of ERK, phosphorylated ERK (p-ERK), and MITF after TA treatment were evaluated by western blot analysis using B16F10 cells. Sustained activation of ERK was observed; in particular, p-ERK was elevated until 24 hours after TA treatment. MITF protein level decreased in a time-dependent manner.
DISCUSSION
TA has been used in Japan for decades to treat melasma. However, there was no report of its melanogenesis-inhibiting effect or action mechanism in English until 1998. TA is a well-known plasmin inhibitor. It blocks the conversion of plasminogen to plasmin by inhibiting plasminogen activator through the formation of a reversible complex with plasminogen7,11. In 1998, Maeda and Naganuma6 reported ultraviolet-induced hyperpigmentation and pigmentation induced by topical application of arachidonic acid in guinea pigs were reduced by topical application of TA in a dose-dependent manner. They suggest TA inhibits ultraviolet-induced plasmin activity in keratinocytes by preventing the binding of plasminogen to the keratinocyte, which ultimately results in less free arachidonic acid and diminished ability to produce prostaglandins6. This was the first report demonstrating that TA prevents ultraviolet-induced pigmentation in vivo. Maeda and Tomita7 published another interesting study in 20077. They showed that single-chain urokinase-type plasminogen activator (sc-uPA) generated by keratinocytes increased the activity of melanocytes in vitro and that TA might reduce hyperpigmentation of melasma patients by blocking the effect of sc-uPA. These findings collectively suggest TA acts by blocking sc-uPA and plasmin, which ultimately prevents arachidonic acid and prostaglandin synthesis.
In the present study, TA reduced melanin synthesis in both cultured murine and human melanocytes in LT-KCM, a highly inflammatory condition. As shown in Fig. 1, this medium contained high levels of inflammatory mediators including IL-1α, IL-8, and PGE2. In the previous study mentioned above7, KCM itself stimulated melanocyte activity. Melanocytes stimulated by IL-1 and tumor necrosis factor-α contribute to cutaneous inflammation via IL-89. Moreover, prostaglandins, which are well-known inflammatory mediators, act as melanogenic stimulators9,12. In particular, PGE2 is reported to stimulate tyrosinase activation via prostaglandin E receptor 4 signaling, resulting in cyclic adenosine monophosphate production13. These inflammatory mediators were significantly higher in the fractional CO2 LT-KCM in the present study than KCM without laser treatment. This suggests laser treatment induces more intense inflammatory conditions that might lead to melanogenesis. As expected, melanin content and tyrosinase activity were higher in LT-KCM than the control media (Fig. 2). Several recent reports demonstrate the usefulness of LT-KCM for evaluating changes of melanogenic cytokine profiles14,15. Although LT-KCM has an intrinsic limitation in representing PIH, it adequately reproduces the intense inflammatory conditions leading to melanogenesis. Although TA reduced melanin content and tyrosinase activity in melan-a cells in LT-KCM, the effect of TA on cultured human melanocytes was not definitive in the present study. The amount of melanin was markedly reduced, especially with arbutin and 100 mg/L TA treatment. However, the decrease of melanin content as a percentage of the control was not statistically significant; a similar result was found even in the arbutin group (positive control). This is likely because the human melanocytes were much more vulnerable to laser treatment and/or test compounds (e.g., arbutin and TA) than melan-a cells. Damaged human melanocytes might consequently affect the results of protein assays and adjusted melanin contents. Tyrosinase is the rate-limiting enzyme in melanin biosynthesis. Therefore, melanin content in cells is correlated with tyrosinase protein level and catalytic activity16. The present results suggest TA may inhibit melanin synthesis, decreasing melanin content and tyrosinase activity (Fig. 3,4,5). Concordantly, tyrosinase protein levels in melan-a cells decreased with TA in a dose-dependent manner (Fig. 6). These results suggest TA downregulates cellular tyrosinase activity in melanocytes or possibly the transcription of tyrosinase mRNA; this suggestion is based on the capability of TA to decrease TRP-1 and TRP-2 levels in addition to tyrosinase levels, because these melanogenic enzymes are regulated by the same key transcription factor, MITF. The effect of TA on MITF protein expression was elucidated by evaluating MITF protein level after TA treatment (Fig. 7). As previous studies show ERK activation leads to MITF phosphorylation and subsequent degradation10,17,18, we also evaluated protein levels of unphosphorylated and phosphorylated ERK. TA stimulated the ERK signaling pathway and downregulated MITF protein level (Fig. 7). Interestingly, ERK phosphorylation was strongly induced 24 hours after TA treatment, whereas MITF protein was detected only 24 hours after TA treatment. These findings are concordant with previous observations that the activation of the ERK signaling pathway induces MITF degradation, resulting in reduced melanogenesis10,17,18. Furthermore, our results support our hypothesis that TA itself attenuates melanogenesis by regulating tyrosinase transcription in addition to its well-known anti-inflammatory effect.
In summary, TA reduces inflammation-induced melanogenesis by decreasing tyrosinase protein expression, which involves ERK pathway activation and the subsequent decrease of MITF protein expression. Our findings suggest TA has potential for the treatment of PIH after laser treatment, a common concern in people with darker skin complexions.
ACKNOWLEDGMENT
This study was supported by research grants from the Asan Institute of Life Science (2012-415, 2013-415) and Amore Pacific Skin Science 2011.
References
- 1.Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: a review of clinical trials. J Am Acad Dermatol. 2006;55:1048–1065. doi: 10.1016/j.jaad.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Costin GE, Hearing VJ. Human skin pigmentation: melanocytes modulate skin color in response to stress. FASEB J. 2007;21:976–994. doi: 10.1096/fj.06-6649rev. [DOI] [PubMed] [Google Scholar]
- 3.Ando H, Kondoh H, Ichihashi M, Hearing VJ. Approaches to identify inhibitors of melanin biosynthesis via the quality control of tyrosinase. J Invest Dermatol. 2007;127:751–761. doi: 10.1038/sj.jid.5700683. [DOI] [PubMed] [Google Scholar]
- 4.Lee JH, Park JG, Lim SH, Kim JY, Ahn KY, Kim MY, et al. Localized intradermal microinjection of tranexamic acid for treatment of melasma in Asian patients: a preliminary clinical trial. Dermatol Surg. 2006;32:626–631. doi: 10.1111/j.1524-4725.2006.32133.x. [DOI] [PubMed] [Google Scholar]
- 5.Li D, Shi Y, Li M, Liu J, Feng X. Tranexamic acid can treat ultraviolet radiation-induced pigmentation in guinea pigs. Eur J Dermatol. 2010;20:289–292. doi: 10.1684/ejd.2010.0912. [DOI] [PubMed] [Google Scholar]
- 6.Maeda K, Naganuma M. Topical trans-4-aminomethylcyclohexanecarboxylic acid prevents ultraviolet radiation-induced pigmentation. J Photochem Photobiol B. 1998;47:136–141. doi: 10.1016/s1011-1344(98)00212-7. [DOI] [PubMed] [Google Scholar]
- 7.Maeda K, Tomita Y. Mechanism of the inhibitory effect of tranexamic acid on melanogenesis in cultured human melanocytes in the presence of keratinocyte-conditioned medium. J Health Sci. 2007;53:389–396. [Google Scholar]
- 8.Horrow JC, Van Riper DF, Strong MD, Brodsky I, Parmet JL. Hemostatic effects of tranexamic acid and desmopressin during cardiac surgery. Circulation. 1991;84:2063–2070. doi: 10.1161/01.cir.84.5.2063. [DOI] [PubMed] [Google Scholar]
- 9.Park HY, Pongpudpunth M, Lee J, Yaar M. Biology of melanocyte. In: Wolff K, Goldsmith LA, I.Katz S, Gilchrest BA, Paller AS, Lefell DJ, editors. Fitzpatrick's dermatology in general medicine. 7th ed. Columbus: McGraw-Hill; 2008. pp. 591–607. [Google Scholar]
- 10.Kim DS, Park SH, Kwon SB, Park ES, Huh CH, Youn SW, et al. Sphingosylphosphorylcholine-induced ERK activation inhibits melanin synthesis in human melanocytes. Pigment Cell Res. 2006;19:146–153. doi: 10.1111/j.1600-0749.2005.00287.x. [DOI] [PubMed] [Google Scholar]
- 11.Dunn CJ, Goa KL. Tranexamic acid: a review of its use in surgery and other indications. Drugs. 1999;57:1005–1032. doi: 10.2165/00003495-199957060-00017. [DOI] [PubMed] [Google Scholar]
- 12.Morelli JG, Norris DA. Influence of inflammatory mediators and cytokines on human melanocyte function. J Invest Dermatol. 1993;100(2 Suppl):191S–195S. [PubMed] [Google Scholar]
- 13.Starner RJ, McClelland L, Abdel-Malek Z, Fricke A, Scott G. PGE(2) is a UVR-inducible autocrine factor for human melanocytes that stimulates tyrosinase activation. Exp Dermatol. 2010;19:682–684. doi: 10.1111/j.1600-0625.2010.01074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yun WJ, Bang SH, Min KH, Kim SW, Lee MW, Chang SE. Epidermal growth factor and epidermal growth factor signaling attenuate laser-induced melanogenesis. Dermatol Surg. 2013;39:1903–1911. doi: 10.1111/dsu.12348. [DOI] [PubMed] [Google Scholar]
- 15.Burd A, Zhu N, Poon VK. A study of Q-switched Nd:YAG laser irradiation and paracrine function in human skin cells. Photodermatol Photoimmunol Photomed. 2005;21:131–137. doi: 10.1111/j.1600-0781.2005.00155.x. [DOI] [PubMed] [Google Scholar]
- 16.Chang TS. An updated review of tyrosinase inhibitors. Int J Mol Sci. 2009;10:2440–2475. doi: 10.3390/ijms10062440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hemesath TJ, Price ER, Takemoto C, Badalian T, Fisher DE. MAP kinase links the transcription factor Microphthalmia to c-Kit signalling in melanocytes. Nature. 1998;391:298–301. doi: 10.1038/34681. [DOI] [PubMed] [Google Scholar]
- 18.Wu M, Hemesath TJ, Takemoto CM, Horstmann MA, Wells AG, Price ER, et al. c-Kit triggers dual phosphorylations, which couple activation and degradation of the essential melanocyte factor Mi. Genes Dev. 2000;14:301–312. [PMC free article] [PubMed] [Google Scholar]