Dear Editor:
Various treatment methods have been used for solar lentigines, including the application of topical bleaching agents, cryotherapy, and laser therapy1. Among the treatment modalities, laser therapy is known to be superior to the other classic methods and Q-switched Nd:YAG laser (QSNL) has shown good treatment results2. However, almost all previous studies reported the efficacy of laser therapy on the basis of the physicians' global assessment and the patients' own evaluation1,2,3,4. Although evaluations by physicians and patients are standard and classic methods, the subjectivity of these evaluations confers limitations5. In this study, we used a colorimeter to accurately and objectively evaluate the efficacy and adverse effects of the QSNL (535 nm) laser for the treatment of solar lentigo. Twenty Korean volunteers with solar lentigines on the face were enrolled. Informed consent was obtained from the participants, and this clinical study was approved by the local institutional review board. We selected two prominent solar lentigines in each patient, and each patient received two sessions of 535 nm QSNL (Pastelle; WONTECH Co., Ltd., Daejeon, Korea) therapy at 4-week intervals. An additional 4-week follow-up period was conducted after the last treatment.
All lentigines were treated with pulses of QSNL irradiation (20 ns pulse width, 0.7~0.8 J/cm2 energy, and 3~4 mm spot size). Improvement was assessed by comparing the pre- and posttreatment (final visit) photographs. The patients' photographs were reviewed by three independent dermatologists who were blinded to the study. Physicians independently rated the clinical improvement (% disappearance of pigments) as follows: grade 0 (0%~20%), grade 1 (20%~40%), grade 2 (40%~60%), grade 3 (60%~80%), and grade 4 (>80%). For a more objective measurement of improvement, we checked the same solar lentigo lesions three times by using a colorimeter (CR-400; Minolta, Osaka, Japan) both at baseline and at the final visit, and the values were averaged. Three parameters were checked with the colorimeter: the L*, a*, and b* values. For the subjective assessment, the patients checked the degree of improvement at each visit, by grading on a five-point scale. Adverse effects such as pain, hyperpigmentation, erythema, and edema were graded as absent, mild, moderate, severe, and extremely severe. Concerning the therapeutic effect in the 20 patients, 11 patients (55.0%) showed an excellent response after two treatment sessions and 4 patients (20%) had a marked response on the physician's global assessment (Fig. 1, Table 1). The average improvement was 72.25%. In the subjective self-assessment, 18 of 20 patients (90%) reported marked or excellent improvement in the degree of pigmentation after the treatment (Table 1). The L* value on the colorimeter increased from 57.26 to 58.59, which means that the luminescence of the solar lentigo improved after the treatment. The a* value, reflecting skin erythema, ranged from 12.16 to 13.25; therefore, the treatment aggravated the erythema. The b* value decreased from 18.69 to 16.89, which indicates a decreased degree of brown pigmentation in the solar lentigo (Table 1). Fifteen of 20 patients (75%) reported mild to moderate pain during treatment despite the application of topical anesthesia before the treatment. The pain was relieved within 1 to 2 hours after treatment. Postinflammatory hyperpigmentation (PIH) was noted in 4 of 20 patients (20%) within 4 weeks after the last laser therapy, which resolved within 3 months of the treatment. Mild to moderate erythema was noted immediately after treatment in about 80% of patients. Many kinds of lasers have been studied for the treatment of solar lentigines, and some of them have produced excellent results. Continuous or quasi-continuous lasers, such as ablative CO2 lasers, have increased risks of causing textural changes or scar formation1. To overcome these problems, the Q-switched laser, which produces a higher temperature with a short pulse duration, was developed on the basis of the selective photothermolysis of melanosomes and melanin1. The Q-switched laser can remove pigmented lesions without injuring the surrounding tissue2. A previous study that compared the Q-switched and the long-pulse Nd:YAG lasers showed a mean score (maximum, 10) of 4.751 for the degree of pigmentation clearance, in both the patients' and the clinicians' assessments3. In our study, the mean score of improvement based on the physician's assessment was 72.25%. In a previous study in which patients received only a single treatment, improvement of the lentigines was reported; therefore, it can be speculated that multiple treatments will result in a better pigmentation clearance4. In the evaluation with a colorimeter, which could show color changes more accurately and objectively5, the degree of brown coloration of the lentigo improved by a factor of 1.8 (from 18.69 to 16.89) after the treatment, and the luminescence of the lentigo (the L* value in the colorimeter) improved. Although evaluations with the human eye and with photographic measurements, as components of the physician's global assessment, remain important, these methods are subjective in nature and might result in the problem of interobserver variability. With photography, standardization of images (color, background, position, and lighting source) can be difficult, and the results are highly reliant on the photographer. In contrast, the colorimeter has been shown to provide reliable and reproducible data. This instrument has been effective in quantifying even small changes in skin color. It represents a convenient, easy, and objective method for assessing color changes with treatment5. In a study on darker skin types2, the Q-switched laser showed a PIH risk of 10% to 25%; in our study, 20% of patients reported mild or moderate PIH after treatment. In a comparison between QSNL and long-pulse Nd:YAG in the treatment of lentigines, long-pulse Nd:YAG showed less change of hypopigmentation because the long-pulse laser destroyed tissue only through a photothermal effect but the QSNL destroyed tissue through both photothermal and photomechanical reactions2. It may be considered that QSNL has a higher risk of PIH, and that long-pulse lasers are more suitable for darker skin types. However, more purpura developed with the long-pulse Nd:YAG technique, and the increased risk of scar formation is a main concern in long-pulse laser treatment. In this study, we have confirmed the effectiveness and adverse effects of QSNL in the treatment of lentigines, both on the basis of physicians'and patients' subjective assessment, and by using the more objective colorimeter evaluation method.
Fig. 1. (A) Multiple brown spots (solar lentigo) on the face before Q-switched Nd:YAG laser treatment (arrow). (B) The treated solar lentigo (arrow) disappeared while the untreated solar lentigo remained.
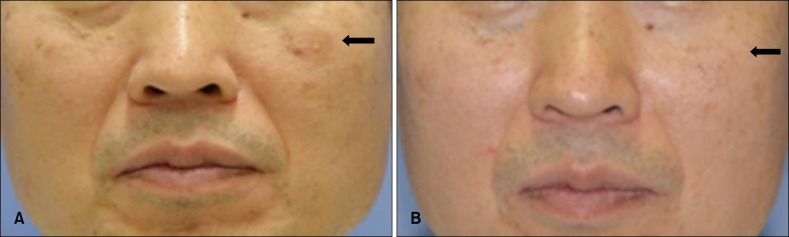
Table 1. The results of Q-switched Nd:YAG laser treatment on the lentigo.
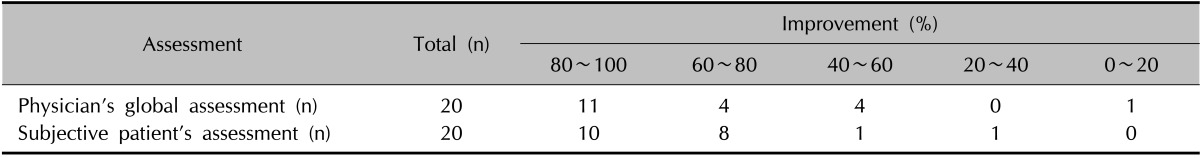
Colorimeter evaluation is as follows. L* value: pretreatment=57.3, posttreatment=58.6; a* value: pretreatment=12.2, posttreatment=13.3; b* value: pretreatment=18.7, posttreatment=16.9. a* value and b* value: p<0.05.
ACKNOWLEDGMENT
This research was supported by Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (MEST) (2012K1A4A3053142).
References
- 1.Ortonne JP, Pandya AG, Lui H, Hexsel D. Treatment of solar lentigines. J Am Acad Dermatol. 2006;54(5 Suppl 2):S262–S271. doi: 10.1016/j.jaad.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 2.Ho SG, Yeung CK, Chan NP, Shek SY, Chan HH. A comparison of Q-switched and long-pulsed alexandrite laser for the treatment of freckles and lentigines in oriental patients. Lasers Surg Med. 2011;43:108–113. doi: 10.1002/lsm.21045. [DOI] [PubMed] [Google Scholar]
- 3.Chan HH, Fung WK, Ying SY, Kono T. An in vivo trial comparing the use of different types of 532 nm Nd:YAG lasers in the treatment of facial lentigines in Oriental patients. Dermatol Surg. 2000;26:743–749. doi: 10.1046/j.1524-4725.2000.00039.x. [DOI] [PubMed] [Google Scholar]
- 4.Murphy MJ, Huang MY. Q-switched ruby laser treatment of benign pigmented lesions in Chinese skin. Ann Acad Med Singapore. 1994;23:60–66. [PubMed] [Google Scholar]
- 5.Taylor S, Westerhof W, Im S, Lim J. Noninvasive techniques for the evaluation of skin color. J Am Acad Dermatol. 2006;54(5 Suppl 2):S282–S290. doi: 10.1016/j.jaad.2005.12.041. [DOI] [PubMed] [Google Scholar]


