Abstract
The infectious agents of the transmissible spongiform encephalopathies are composed of amyloidogenic prion protein, PrPSc. Real-time quaking-induced conversion can amplify very small amounts of PrPSc seeds in tissues/body fluids of patients or animals. Using this in vitro PrP-amyloid amplification assay, we quantitated the seeding activity of affected human brains. End-point assay using serially diluted brain homogenates of sporadic Creutzfeldt–Jakob disease patients demonstrated that 50% seeding dose (SD50) is reached approximately 1010/g brain (values varies 108.79–10.63/g). A genetic case (GSS-P102L) yielded a similar level of seeding activity in an autopsy brain sample. The range of PrPSc concentrations in the samples, determined by dot-blot assay, was 0.6–5.4 μg/g brain; therefore, we estimated that 1 SD50 unit was equivalent to 0.06–0.27 fg of PrPSc. The SD50 values of the affected brains dropped more than three orders of magnitude after autoclaving at 121°C. This new method for quantitation of human prion activity provides a new way to reduce the risk of iatrogenic prion transmission.
Introduction
Human prion diseases (HPD) are neurodegenerative diseases caused by accumulation of amyloidogenic prion protein (PrPSc), which is generated from the cellular prion protein (PrPC) via a conformational change. PrPSc is detected not only in neuronal tissues, but also in lymphoid tissues (e.g., spleen, tonsil, lymph node) [1, 2] and muscles of some sporadic Creutzfeldt—Jakob disease (CJD) (sCJD) patients [1]. In cases of variant CJD, PrPSc has been detected in blood, rectum, adrenal gland, and thymus [3]. Accidental iatrogenic transmission of prion has occurred due to use of human growth hormone [4], dura mater grafts [5], corneal grafts [6], and blood [7–9] from HPD patients or carriers. Infectivity mainly resides in the neural tissues of sCJD patients, whereas prion infectivity in extraneural tissue is low, and it is difficult to estimate the exact infectivity. Transmission studies of human prion, conducted in chimpanzees and other primates [10–14], demonstrated that it takes more than 12 months to develop the syndrome. Normal rodents infected with human prion require prolonged incubation times to develop illness because of the so-called species barrier. Since then, several lines of transgenic mice expressing human prion protein (or human—mouse chimeric protein) have been produced, and some of them exhibited abbreviated incubation times of 110 days following infection with human prion [15]. Quantitation of infectivity of tissue from a patient with HPD can be achieved by animal bioassay using humanized mice [16, 17]; however, these mice have different susceptibilities to human prion strains [18–20], and the assays are still highly time-consuming and costly.
Previously, we developed the real-time quaking-induced conversion (RT-QUIC) assay for detection of very small amounts of abnormal PrP in tissue and body fluids. This technique provides a highly sensitive means for detecting prion-seeding activity using human recombinant PrP as a substrate [21]. Recent studies showed that seeding activity in vitro, determined by end-point RT-QUIC, parallels the infectivity of prion-containing animal specimens [22, 23]. Moreover, these studies demonstrate that RT-QUIC is more sensitive than bioassay. Although bioassay is the only tool currently available for determining the known infectivity of human prion, in the future it will be possible to replace LD50 (50% lethal dose) with SD50 (50% seeding dose). To define the distribution of infectivity in human bodies, we applied end-point RT-QUIC to evaluation of human prion seeding activity in brains from patients with human prion disease.
Materials and Methods
Patients
Sporadic CJD was diagnosed according to Parchi’s classification [24], i.e., based on the genotype at codon 129 of PRNP gene (methionine homozygous [MM], valine homozygous [VV], or heterozygous [MV]), and the physicochemical properties of PrPSc. Autopsy brains from 10 patients with prion diseases were subjected to study after histopathological confirmation of the clinical diagnosis. There were six cases of sCJD MM1 and a single case each of the MM2-cortical form, the MM2-thalamic form, MV2, and Gerstmann—Sträussler—Scheinker syndrome (GSS) associated with a mutation of Pro to Leu at codon 102 of PRNP (P102L) (Table 1).
Table 1. Summary of patients with prion disease.
| Patient number | Sex | Age at death (years) | codon 129 | WB type | mutation | log SD50/ g brain (Mean ± S.D.) | PrP-res/brain (μg/g) |
|---|---|---|---|---|---|---|---|
| 1 | male | 73 | MM | 1 | - | 10.07 ± 0.19 | 1.1 |
| 2 | male | 64 | MM | 1 | - | 10.63 ± 0.43 | 5.4 |
| 3 | male | 70 | MM | 1 | - | 10.08 ± 0.58 | 3.3 |
| 4 | male | 74 | MM | 1 | - | 9.92 ± 0.59 | 1 |
| 5 | female | 75 | MM | 1 | - | 9.96 ± 0.44 | 1.1 |
| 6 | female | 64 | MM | 1 | - | 9.71 ± 0.40 | 0.6 |
| 7 | female | 43 | MM | - | P102L | 10.13 ± 0.25 | 1.1 |
| 8 | male | 69 | MV | 2 | - | 10.21 ± 0.26 | 0.9 |
| 9* | male | 35 | MM | 2 | - | 10.08 ± 0.36 | 2.3 |
| 10** | male | 67 | MM | 2 | - | 8.79 ± 0.26 | N.D |
Clinical data and the SD50 concentrations in the brain homogenates from patients with prion disease.
*: MM2 cortical form
**: MM2 thalamic form. N.D.: not detected. MM: methionine homozygosity at codon 129 of PRNP. MV: methionine/valine heterozygosity at codon 129 of PRNP. S.D.: standard deviation. P102L: Pro-to-Leu point mutation at codon 102 of PRNP. WB: Western-blotting assay
Two brain specimens were used as control. One of the donors suffered dementia with Lewy bodies (DLB), and in the other case the cause of death was dissecting aortic aneurysm without any brain damage. Written informed consent to participate in the study was given by all patients’ families. The protocol for investigation was approved by the Ethics Committee of Nagasaki University Hospital (ID: 10042823), and the study was registered with the University Hospital Medical Information Network (ID: UMIN000003301). The protocol was also granted ethical approval for the use of brain tissues by the Japan Surveillance Unit for human prion diseases. Analysis of the PRNP gene was conducted by Dr. Kitamoto of the Japan Surveillance Unit.
Brain homogenate preparation and heat treatment
All samples were taken from frontal cortex and stored at -80°C. Brain tissues were homogenized at 10% (w/v) in ice-cold phosphate-buffered saline (PBS) supplemented with a protease inhibitor mixture (Roche, Mannheim, Germany) using a multi-bead shocker (Yasui Kikai, Osaka, Japan), and stored at -80°C. Aliquots of 10% brain homogenates were inactivated by autoclaving (SX700HY, TOMY, Tokyo, Japan) at 121°C for 20–60 min.
RT-QUIC
Purification of recombinant human PrP (rHuPrP: residues 23–231, codon 129M) was performed as previously described [25]. After purification, rHuPrP was stored at -80°C. Brain homogenates (BHs) (10% [w/v]) were serially diluted (10-fold) with artificial cerebrospinal fluid (A-CSF) containing 125 mM NaCl, 2.5 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 0.2 ng/ml BSA, and 0.05% glucose. rHuPrP, suspended in 95 μl of RT-QUIC buffer (500 mM NaCl, 50 mM PIPES pH7.0, 10 μM Thioflavin T (ThT), and1 mM EDTA), was loaded into each well of a 96-well plate and mixed with 5 μl of brain sample, and then the assay was monitored for 53 h. Four to eight replicates of each diluted sample were measured. The SD50 was calculated by the Spearman—Kärber method [23]. We arbitrarily designated positive reactions as those with fluorescence intensities more than double of the average of negative controls.
Dot blotting
Dot blotting was performed to determine the amount of PrP-res in brain homogenates. BHs (10% [w/v]) were incubated with 20 μg/ml proteinase K for 30 min at 37°C. Protease was inactivated by the addition of 2 mM Pefabloc sc (Shigma-Aldrich, Buchs, Switzerland). rHuPrP was used to generate a standard curve; the concentrations of unknown samples were determined by interpolation on the graph. Samples (Human recPrP and 10% BHs) were blotted onto nitrocellulose membrane (GE Healthcare, Freilburg, Germany). PrP-res on the membrane was denatured with 3 M GdnSCN. After blocking with 5% skim milk in TBST (10 mM Tris-HCl [pH 7.8], 100 mM NaCl, 0.1% Tween 20) for 1 h at room temperature, the membrane was incubated overnight at 4°C with the primary antibody (AB) (6H4, Prionics, Zürich, Switzerland 1:5000) in 1% skim milk in TBST; after washing, the membrane was incubated for 1 h at room temperature with the secondary AB (anti-mouse IgG HRP, GE Healthcare, Buckinghamshire, UK, 1:5000) in 1% skim milk in TBST. Quantitative detection of PrP-res was performed using a LAS-3000 luminescent image analyzer (Fujifilm, Tokyo, Japan).
Results
End-point RT-QUIC revealed high seeding activities in human brains affected with sporadic and genetic prion diseases.
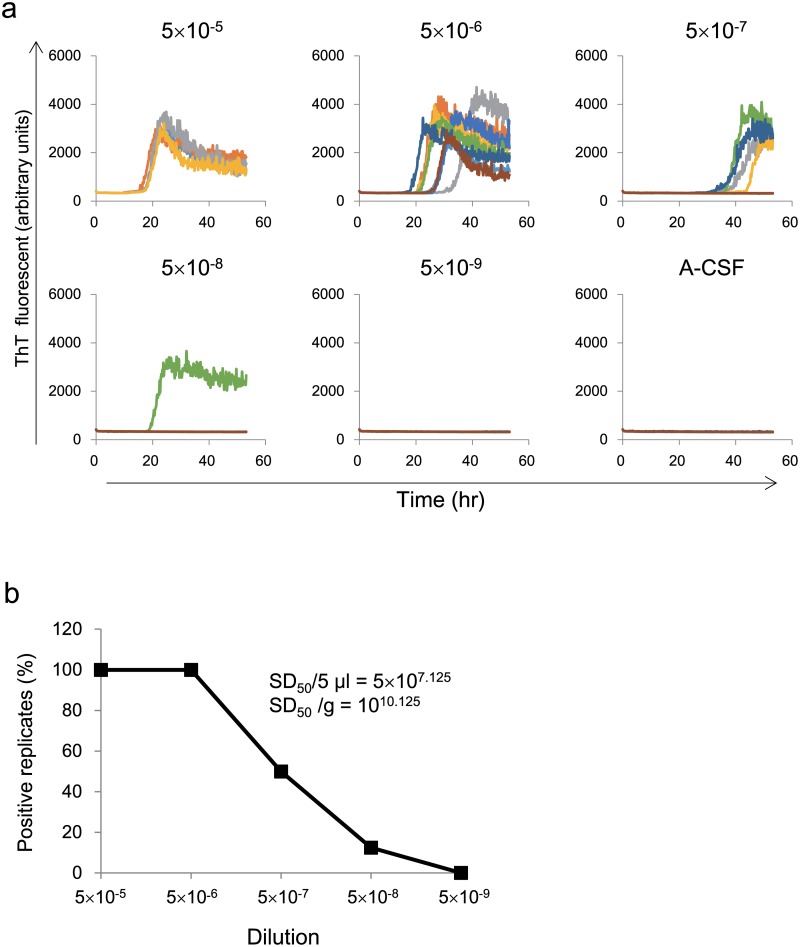
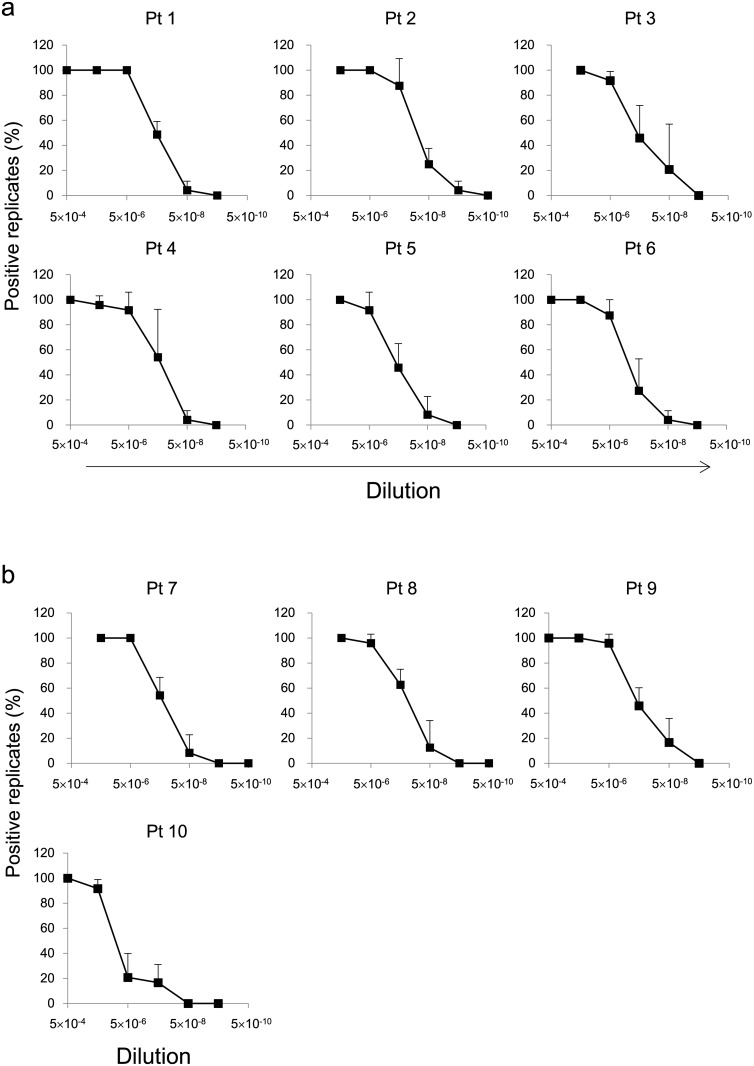
We first analyzed patient no.1 (patient 1, sCJD MM-1). Brain homogenate was diluted from 5×10–5 to 5×10–9 and subjected to end-point RT-QUIC assay to quantitate seeding activity. The fluorescence of ThT was elevated at dilutions from 5×10–5 to 5×10–8, then at 5×10–9 dilution there was yielded no reaction, as did a negative controls (non-CJD BH, DLB-BH, and A-CSF) (S1 Fig). The percentage of positive reaction decreased in a sigmoidal curve within the dilution range and the SD50 was calculated (Fig 1a). We were successfully able to analyze eight other sporadic CJDs and a genetic case, GSS-P102L; in all of these cases, the SD50 values were similar (it reached around 10 log10 SD50/g of brain) (Figs 1b, 2 and Table 1).
Fig 1. Quantitation of seeding activity in brain tissue from a sporadic CJD patient using end-point RT-QUIC.
(a) BH (Pt 1) was diluted (5 × 10–5 to 5 × 10–9) and subjected to RT-QUIC reaction containing human recPrP substrate. The fluorescence of ThT was elevated at dilutions from 5 × 10–5 to 5 × 10–8. The 5×10–9 dilution yielded no reaction, as did a negative control consisting of A-CSF. (b) The percentage of positive reaction decreased in a sigmoidal curve within the dilution range when BH was used as the seed. The SD50 was calculated using the Spearman—Kärber method.
Fig 2. End-point RT-QUIC analysis of 10 brain specimens from patients with prion diseases.
End-point RT-QUIC assay was performed three times. (a) Brain tissues from six patients with sCJD-MM1 were used to seed the RT-QUIC reaction. (b) Samples of GSS-P102L, sCJD-MV2, and sCJD-MM2 (cortical and thalamic forms) were used to seed RT-QUIC reaction.
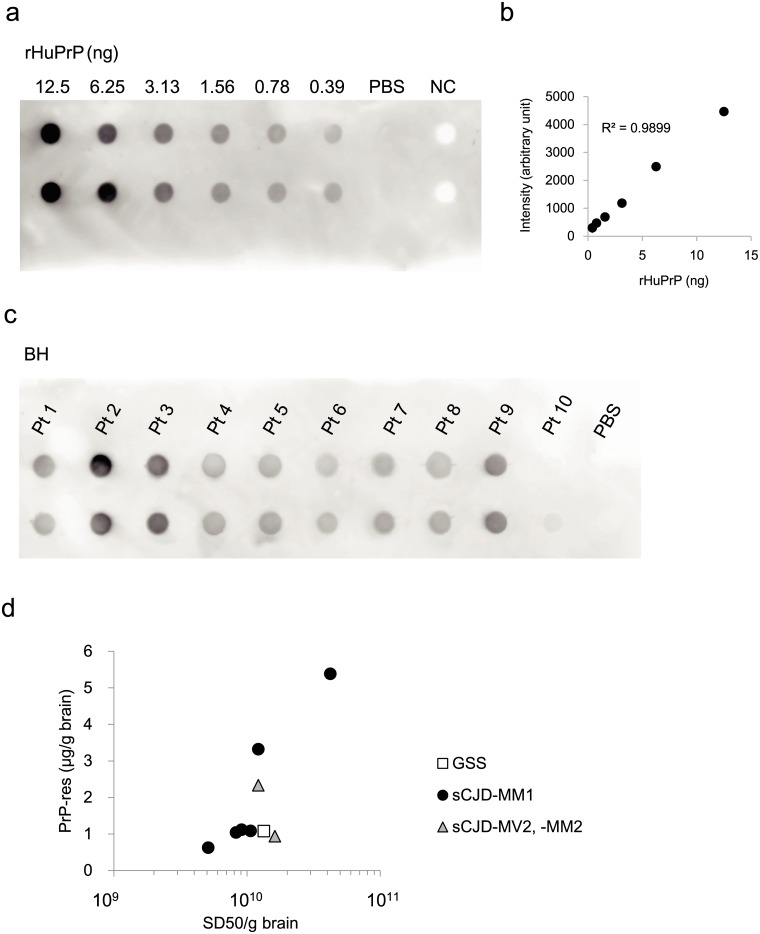
1 SD50 unit is equivalent to 0.12 fg of PrP-res
We quantified PrP-res in the brain samples by dot blotting. Based on the signals of recombinant human PrP (rHuPrP) (Fig 3a and 3b), the linearity of the standard curve was observed in the range of 0.39–12.5 ng protein (R2 = 0.9899), we determined the amount or the concentration of PrP-res (Fig 3c and Table 1). The concentrations of PrP-res in BH samples were in the range 0.6–5.4 μg/g (PrP-res/brain). In those samples, MM1 (patient 2) had the highest level of PrP-res (5.4 μg/g), whereas the MM2 thalamic form (patient 10) had the lowest level, below the detection limits. Similarly, in terms of the value of SD50, patient 2 was the highest and patient 10 was the lowest (Table 1). In cases of CJD-MM1, SD50 was linearly correlated with the level of PrP-res (R2 = 0.8173) (Fig 3d) and 1 SD50 unit corresponded to 0.12 femto gram of PrP-res.
Fig 3. Correlation between SD50 and PrP-res in the brain.
(a) Human recPrP was serial diluted and tested by dot blotting. (b) A standard curve was constructed using diluted human recPrP. (c) Dot-blotting of BHs from patients with prion diseases. Pt 10 (MM2-thalamic form) had a very weak signal and fell below the limit of detection. (d) There was a linear correlation between SD50 and the level of PrPSc in nine patient’s brains (y = 1.281 × 10-10x, R2 = 0.7192). NC = Normal brain homogenate. y = value of PrP-res (μg/g brain). x = value of SD50/g brain
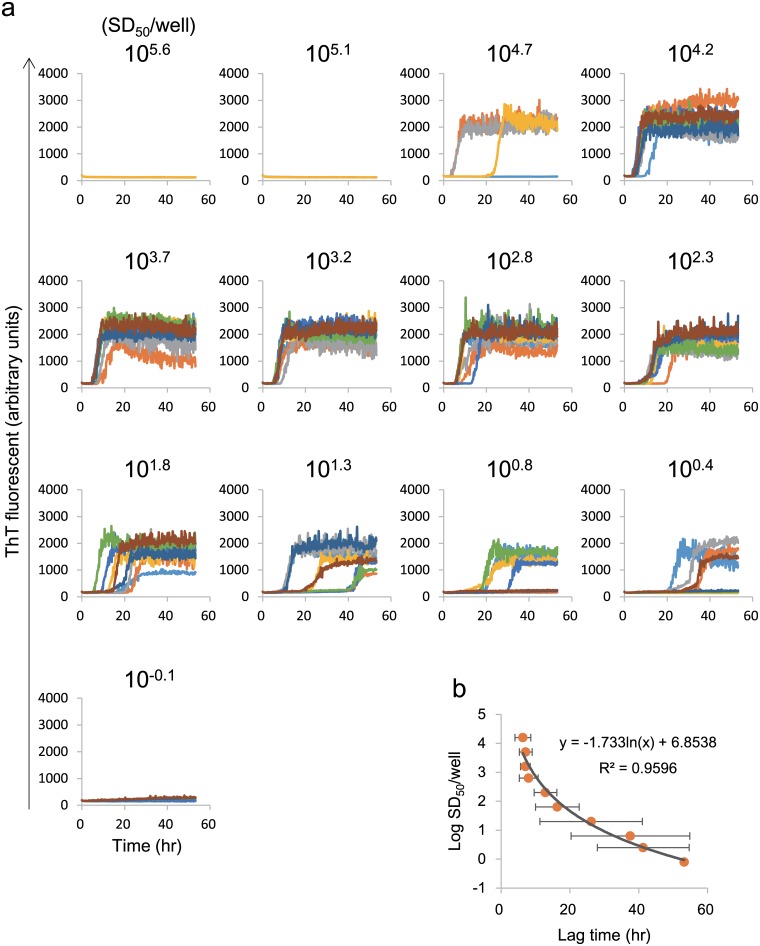
The lag time of RT-QUIC reaction are well correlated to amount of seeds but not applicable for quantitative assay instead of SD50
RT-QUIC reactions exhibited elevation of ThT fluorescence after a lag phase of 15–18 h after seeding with a 5 × 10–5 diluted brain sample, and the duration of the lag phase increased along with higher dilutions. As a recent study by others has suggested a correlation between concentration of prion and lag time of RT-QUIC [26], we performed RT-QUIC in combination with three-fold serial dilution to confirm that the lag time can be used as a quantitative parameter instead of SD50 (Fig 4a). The correlation coefficient obtained from linear regression between PrP-res and lag time was lower than that obtained by polynomial regression between these two parameters y=-1.733ln(x)+6.8538 (R2 = 0.9596). Of note, there was little difference among the higher concentration specimens (SD50 value of 104.2 to 102.8). On the other hand, lower concentration of brain specimens (SD50 value of 101.3 to 100.4) had larger standard deviations (Fig 4b), resulting huge overlap of data between different dilutions. We also observed inhibition of the RT-QUIC reaction seeded with 5 μl of seed containing 1 to 0.1% (SD50 value of 105.6 to 104.7) brain tissue. Taken together, although the good correlation was observed between seeding activity and lag time, these data suggest the limitations on the use of “lag time” as a parameter for prion activity under our experimental condition.
Fig 4. Preparation of standard curves based on lag phase and aggregate area in RT-QUIC.
(a) Brain specimen from a patient with sCJD (patient 4) was subjected to serial three-fold dilution and RT-QUIC reaction, with four replicates for each dilution. (b) Standard curves (gray line) based on lag phase.
End-point QUIC can quantitatively evaluate the effect of treatment on human prion directly.
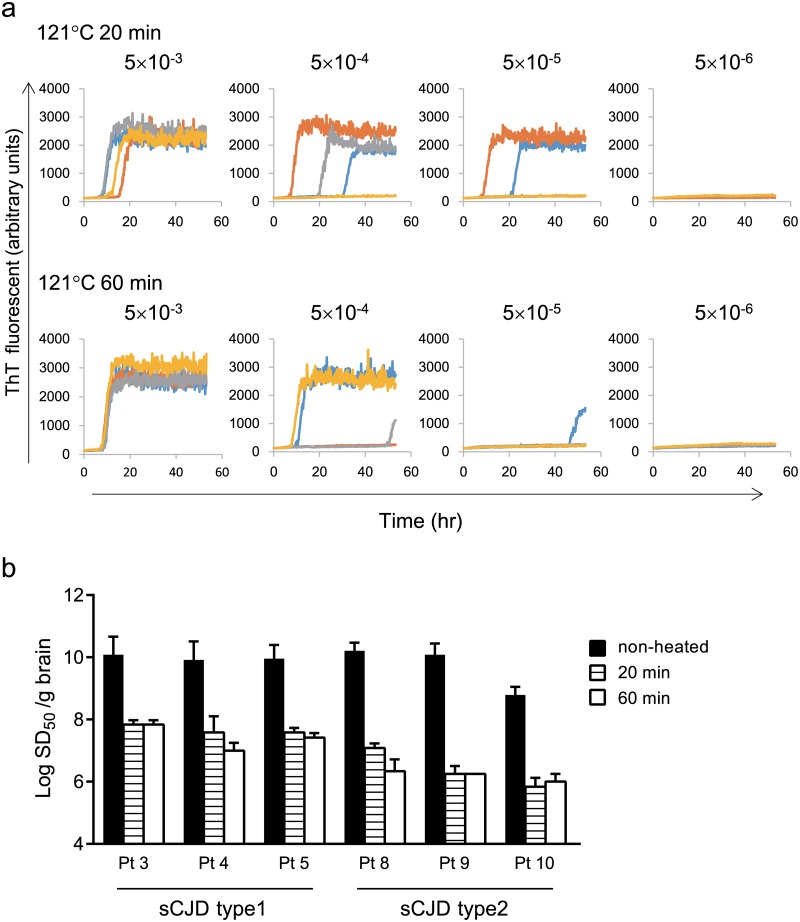
Next, we tested the RT-QUIC assay to evaluate decontamination methods. After autoclave treatment, brain homogenates from patients 3–5 and 8–10 were subjected to end-point RT-QUIC. Heat treatment at 121°C for 20 and 60 min decreased the SD50 by 2.25 and 3.88 orders of magnitude, respectively (Fig 5b). Fig 5a shows that brain from CJD (MM1) subjected to 121°C for 20 min and 60 min yielded an SD50 value of 107.75 and 107.5/g brain. CJD type 2 (patients 8–10) tended to be affected by heat treatment more than CJD type 1 (patients 3–5).
Fig 5. Reduction of seeding activity by heat treatment.
(a) Brain from patient with sCJD-MM1 (patient 3) was treated at 121°C for 20 min or 60 min, and seeding activity was tested by end-point RT-QUIC. (b) Remaining SD50 after heat treatment. Black represents non-treated CJD-BH (patients 3–5 and 8–10). Horizontal stripes and white represents SD50 after heat treatment for 20 min and 60 min, respectively. Heat treatment caused reduction of SD50 (2.25 to 3.88 orders of magnitude). Data are presented as means ± standard deviation.
Discussion
The end-point RT-QUIC assay enables us to quantitate human prion seeding activity in brains from patients with prion disease. In brains from sCJD-MM1, the average SD50 was 1010.06. According to a previous report, LD50 of brain tissues from patients with sCJD-MM1 falls within the range 107–9 LD50 /g [18]. Although our bioassays of these brain tissues is ongoing, it is likely that SD50 could be 10–100 times more sensitive than LD50, because similar differences between SD50 and LD50 were seen in experiments using hamster prion 263K [23]. Notably, it was also possible to determine SD50 using the MM2-cortical form, the MM2-thalamic form, MV2, and a case of GSS-P102L.
There was a linear correlation between SD50 and the level of PrP-res in the brains of six patients with CJD-MM1 (R2 = 0.8173). Based on estimation by dot-blot analysis, 1 SD50 was equivalent to 0.1 fg of PrP-res, suggesting that our RT-QUIC can detect PrP over a wider range than conventional Western blotting or ELISA. SD50 from all samples (10 patients, including MM2-cortical, MM2-thalamic, MV2, and GSS-P102L) exhibited a low correlation with the level of PrP-res (R2 = 0.7532), possibly because resistance to protease digestion of PrP is not always the same as seeding activity.
Inhibition of the RT-QUIC reaction were seen in samples seeded with 1 to 0.1% brain tissue and 0.2% (5 × 10–2 dilution) spleen tissue (S2 Fig). A spleen specimens from a patient with sCJD yielded an SD50 value of 107.5/g tissue. There was no positive reaction when normal spleen tissue was used as the seed (data not shown). Tissue samples include an inhibitor of RT-QUIC reaction; therefore, in order to quantitate seeding activity in tissue samples, it is important to reduce the concentration of this inhibitor by dilution.
Effective decontamination methods are essential in order to avoid iatrogenic transmission of prion diseases by contaminated medical equipment [27, 28]. PrPSc is resistant to chemical disinfectants such as ethanol and formaldehyde. By contrast, bioassays revealed that autoclaving at 121°C for 30 min and 60 min reduced infectivity of CJD inoculated mouse brain by 3.1 and 3.8 log10 units/g tissue, respectively [29]. Here, we conducted our preliminary assessments using human brain treated with simple heating. Heat treatments at 121°C for 20 min and 60 min reduced SD50 by 2.25 and 3.88 orders of magnitude, respectively. In the future, we will have to reassess LD50 using humanized mice and evaluate SD50 by RT-QUIC in all organs. Because RT-QUIC is an easy and rapid assay for determining prion activity, this approach provides a new way to evaluate biological patient specimens and reassess the safety of donated organs.
Supporting Information
Brain specimens from patients with prion disease (Patients 2–10) and non-prion disease were diluted (5 × 10–5) and subjected to RT-QUIC reaction. Positive reactions were observed in RT-QUIC reactions using brain tissues from patients with prion disease. There was no response in the presence of non-prion samples (Non-PrD 1 and 2).
(PDF)
Spleen specimen from the patient with sCJD was diluted (5 × 10–2 to 5 × 10–5) and subjected to RT-QUIC reaction.
(PDF)
Acknowledgments
We are grateful to all the members of the Prion Disease Surveillance Committee, Japan, for collecting data and offering advice. In addition, we thank Dr. Kitamoto of the Department of Neurological Science, Tohoku University School of Medicine, for the prion protein and gene analysis, and A. Matsuo for her technical assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by Grants-in-Aid from the Research Committee of Surveillance and Infection Control of Prion Disease and from the Research Committee of Prion Disease and Slow Virus Infection of the Ministry of Health, Labour and Welfare of Japan. Dr. Satoh received research support from a Grant-in Aid for Scientific Research (C) (24591268) and Scientific Research (B) (Overseas Academic Research) (14507303) from the Ministry of Education, Culture, Sports, Science and Technology of Japan and the Japan Society for the Promotion of Science. This work was supported by Grants-in-Aid from the Research Committee on Surveillance and Infection Control of Prion Disease of the Ministry of Health, Labour and Welfare of Japan. Dr. Atarashi received research support from a Grant-in-Aid for Scientific Research (B) (23300127) from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and a grant from the Ministry of Health, Labour and Welfare of Japan, as well as a grant from the Takeda Science Foundation. Dr. Sano received research support from a Grant-in-Aid for Young Scientific Researchers (B) (23790998) from the Ministry of Education, Culture, Sports, Science and Technology of Japan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Glatzel M, Abela E, Maissen M, Aguzzi A. Extraneural pathologic prion protein in sporadic Creutzfeldt-Jakob disease. The New England journal of medicine. 2003;349(19):1812–20. Epub 2003/11/07. 10.1056/NEJMoa030351 . [DOI] [PubMed] [Google Scholar]
- 2. Rubenstein R, Chang B. Re-assessment of PrP(Sc) distribution in sporadic and variant CJD. PloS one. 2013;8(7):e66352 Epub 2013/07/12. 10.1371/journal.pone.0066352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wadsworth JD, Joiner S, Hill AF, Campbell TA, Desbruslais M, Luthert PJ, et al. Tissue distribution of protease resistant prion protein in variant Creutzfeldt-Jakob disease using a highly sensitive immunoblotting assay. Lancet. 2001;358(9277):171–80. Epub 2001/07/31. . [DOI] [PubMed] [Google Scholar]
- 4. Koch TK, Berg BO, De Armond SJ, Gravina RF. Creutzfeldt-Jakob disease in a young adult with idiopathic hypopituitarism. Possible relation to the administration of cadaveric human growth hormone. The New England journal of medicine. 1985;313(12):731–3. Epub 1985/09/19. 10.1056/nejm198509193131206 . [DOI] [PubMed] [Google Scholar]
- 5. Thadani V, Penar PL, Partington J, Kalb R, Janssen R, Schonberger LB, et al. Creutzfeldt-Jakob disease probably acquired from a cadaveric dura mater graft. Case report. Journal of neurosurgery. 1988;69(5):766–9. Epub 1988/11/01. 10.3171/jns.1988.69.5.0766 . [DOI] [PubMed] [Google Scholar]
- 6. Duffy P, Wolf J, Collins G, DeVoe AG, Streeten B, Cowen D. Letter: Possible person-to-person transmission of Creutzfeldt-Jakob disease. The New England journal of medicine. 1974;290(12):692–3. Epub 1974/03/21. . [PubMed] [Google Scholar]
- 7. Llewelyn CA, Hewitt PE, Knight RS, Amar K, Cousens S, Mackenzie J, et al. Possible transmission of variant Creutzfeldt-Jakob disease by blood transfusion. Lancet. 2004;363(9407):417–21. Epub 2004/02/14. 10.1016/s0140-6736(04)15486-x . [DOI] [PubMed] [Google Scholar]
- 8. Peden AH, Head MW, Ritchie DL, Bell JE, Ironside JW. Preclinical vCJD after blood transfusion in a PRNP codon 129 heterozygous patient. Lancet. 2004;364(9433):527–9. Epub 2004/08/11. 10.1016/s0140-6736(04)16811-6 . [DOI] [PubMed] [Google Scholar]
- 9. Wroe SJ, Pal S, Siddique D, Hyare H, Macfarlane R, Joiner S, et al. Clinical presentation and pre-mortem diagnosis of variant Creutzfeldt-Jakob disease associated with blood transfusion: a case report. Lancet. 2006;368(9552):2061–7. Epub 2006/12/13. 10.1016/s0140-6736(06)69835-8 . [DOI] [PubMed] [Google Scholar]
- 10. Gajdusek DC, Gibbs CJ, Alpers M. Experimental transmission of a Kuru-like syndrome to chimpanzees. Nature. 1966;209(5025):794–6. Epub 1966/02/19. . [DOI] [PubMed] [Google Scholar]
- 11. Gajdusek DC, Gibbs CJ Jr., Alpers M. Transmission and passage of experimenal "kuru" to chimpanzees. Science (New York, NY). 1967;155(3759):212–4. Epub 1967/01/13. . [PubMed] [Google Scholar]
- 12. Gibbs CJ Jr., Gajdusek DC. Transmission of scrapie to the cynomolgus monkey (Macaca fascicularis). Nature. 1972;236(5341):73–4. Epub 1972/03/10. . [DOI] [PubMed] [Google Scholar]
- 13. Gibbs CJ Jr., Gajdusek DC, Asher DM, Alpers MP, Beck E, Daniel PM, et al. Creutzfeldt-Jakob disease (spongiform encephalopathy): transmission to the chimpanzee. Science (New York, NY). 1968;161(3839):388–9. Epub 1968/07/26. . [DOI] [PubMed] [Google Scholar]
- 14. Gibbs CJ Jr., Gajdusek DC. Infection as the etiology of spongiform encephalopathy (Creutzfeldt-Jakob disease). Science (New York, NY). 1969;165(3897):1023–5. Epub 1969/09/05. . [DOI] [PubMed] [Google Scholar]
- 15. Korth C, Kaneko K, Groth D, Heye N, Telling G, Mastrianni J, et al. Abbreviated incubation times for human prions in mice expressing a chimeric mouse-human prion protein transgene. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(8):4784–9. Epub 2003/04/10. 10.1073/pnas.2627989100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Collinge J, Palmer MS, Sidle KC, Hill AF, Gowland I, Meads J, et al. Unaltered susceptibility to BSE in transgenic mice expressing human prion protein. Nature. 1995;378(6559):779–83. Epub 1995/12/21. 10.1038/378779a0 . [DOI] [PubMed] [Google Scholar]
- 17. Hill AF, Desbruslais M, Joiner S, Sidle KC, Gowland I, Collinge J, et al. The same prion strain causes vCJD and BSE. Nature. 1997;389(6650):448–50, 526 Epub 1997/10/23 22:27. 10.1038/38925 . [DOI] [PubMed] [Google Scholar]
- 18. Taguchi Y, Mohri S, Ironside JW, Muramoto T, Kitamoto T. Humanized knock-in mice expressing chimeric prion protein showed varied susceptibility to different human prions. The American journal of pathology. 2003;163(6):2585–93. Epub 2003/11/25. 10.1016/s0002-9440(10)63613-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Telling GC, Scott M, Hsiao KK, Foster D, Yang SL, Torchia M, et al. Transmission of Creutzfeldt-Jakob disease from humans to transgenic mice expressing chimeric human-mouse prion protein. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(21):9936–40. Epub 1994/10/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Telling GC, Scott M, Mastrianni J, Gabizon R, Torchia M, Cohen FE, et al. Prion propagation in mice expressing human and chimeric PrP transgenes implicates the interaction of cellular PrP with another protein. Cell. 1995;83(1):79–90. Epub 1995/10/06. . [DOI] [PubMed] [Google Scholar]
- 21. Atarashi R, Satoh K, Sano K, Fuse T, Yamaguchi N, Ishibashi D, et al. Ultrasensitive human prion detection in cerebrospinal fluid by real-time quaking-induced conversion. Nature medicine. 2011;17(2):175–8. Epub 2011/02/01. 10.1038/nm.2294 . [DOI] [PubMed] [Google Scholar]
- 22. Vascellari S, Orru CD, Hughson AG, King D, Barron R, Wilham JM, et al. Prion seeding activities of mouse scrapie strains with divergent PrPSc protease sensitivities and amyloid plaque content using RT-QuIC and eQuIC. PloS one. 2012;7(11):e48969 Epub 2012/11/10. 10.1371/journal.pone.0048969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wilham JM, Orru CD, Bessen RA, Atarashi R, Sano K, Race B, et al. Rapid end-point quantitation of prion seeding activity with sensitivity comparable to bioassays. PLoS pathogens. 2010;6(12):e1001217 10.1371/journal.ppat.1001217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Parchi P, Giese A, Capellari S, Brown P, Schulz-Schaeffer W, Windl O, et al. Classification of sporadic Creutzfeldt-Jakob disease based on molecular and phenotypic analysis of 300 subjects. Annals of neurology. 1999;46(2):224–33. Epub 1999/08/12. . [PubMed] [Google Scholar]
- 25. Atarashi R, Moore RA, Sim VL, Hughson AG, Dorward DW, Onwubiko HA, et al. Ultrasensitive detection of scrapie prion protein using seeded conversion of recombinant prion protein. Nature methods. 2007;4(8):645–50. Epub 2007/07/24. 10.1038/nmeth1066 . [DOI] [PubMed] [Google Scholar]
- 26. Shi S, Mitteregger-Kretzschmar G, Giese A, Kretzschmar HA. Establishing quantitative real-time quaking-induced conversion (qRT-QuIC) for highly sensitive detection and quantification of PrPSc in prion-infected tissues. Acta neuropathologica communications. 2013;1(1):44 Epub 2013/11/21. 10.1186/2051-5960-1-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bernoulli C, Siegfried J, Baumgartner G, Regli F, Rabinowicz T, Gajdusek DC, et al. Danger of accidental person-to-person transmission of Creutzfeldt-Jakob disease by surgery. Lancet. 1977;1(8009):478–9. Epub 1977/02/26. . [DOI] [PubMed] [Google Scholar]
- 28. Will RG, Matthews WB. Evidence for case-to-case transmission of Creutzfeldt-Jakob disease. Journal of neurology, neurosurgery, and psychiatry. 1982;45(3):235–8. Epub 1982/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Taguchi F, Tamai Y, Uchida K, Kitajima R, Kojima H, Kawaguchi T, et al. Proposal for a procedure for complete inactivation of the Creutzfeldt-Jakob disease agent. Archives of virology. 1991;119(3–4):297–301. Epub 1991/01/01. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Brain specimens from patients with prion disease (Patients 2–10) and non-prion disease were diluted (5 × 10–5) and subjected to RT-QUIC reaction. Positive reactions were observed in RT-QUIC reactions using brain tissues from patients with prion disease. There was no response in the presence of non-prion samples (Non-PrD 1 and 2).
(PDF)
Spleen specimen from the patient with sCJD was diluted (5 × 10–2 to 5 × 10–5) and subjected to RT-QUIC reaction.
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.