Abstract
The association between metabolic syndrome (MS) and bone health remains unclear. We aimed to study the association between MS and hip bone geometry (HBG), femoral neck bone mineral density (FN-BMD), and the risk of osteoporosis and incident fractures. Data of 2040 women and 1510 men participants in the third visit (1997–1999) of the Rotterdam Study (RSI-3), a prospective population based cohort, were available (mean follow-up 6.7 years). MS was defined according to the recent harmonized definition. HBG parameters were measured at the third round visit whereas FN-BMD was assessed at the third round and 5 years later. Incident fractures were identified from medical registry data. After correcting for age, body mass index (BMI), lifestyle factors and medication use, individuals with MS had lower bone width (β = -0.054, P = 0.003), lower cortical buckling ratio (β = -0.81, P = 0.003) and lower odds of having osteoporosis (odds ratio =0.56, P = 0.007) in women but not in men. Similarly, MS was associated with higher FN-BMD only in women (β = 0.028, P=0.001). In the analyses of MS components, the glucose component (unrelated to diabetes status) was positively associated with FN-BMD in both genders (β = 0.016, P = 0.01 for women and β = 0.022, P = 0.004 for men). In men, waist circumference was inversely associated with FN-BMD (β = -0.03, P = 0.004). No association was observed with fracture risk in either sex. In conclusion, women with MS had higher FN-BMD independent of BMI. The glucose component of MS was associated with high FN-BMD in both genders, highlighting the need to preserve glycemic control to prevent skeletal complications.
Introduction
Osteoporosis, a systemic skeletal disease, is an important public health problem due to its increased risk for fractures, high morbidity and mortality and significant health care costs [1,2]. Different factors have been associated with osteoporosis including abdominal obesity, hypertension, dyslipidemia and abnormal glucose metabolism, which are considered components of metabolic syndrome. These components might affect bone differently. Obesity may lead to increased bone mineral density (BMD) because it is associated with higher 17β-estradiol levels and higher mechanical load, which may protect bone [3,4]. Visceral fat accumulation is associated with higher levels of pro-inflammatory cytokines, which may up-regulate receptor activators of nuclear kappa B ligand, leading to increased bone resorption and therefore decreased BMD[5–7]. Also, although hyperglycemia is a predictor of osteoporotic fractures [8], the association between high glucose levels or insulin resistance with BMD is not well defined. For example, diabetic individuals have higher BMD but increased risk of fractures [9–11]. Similarly, the evidence for associations between dyslipidemia and hypertension with bone metabolism is still inconclusive and the overall association between MS and bone health remains unclear [12–15]. Two recent meta-analyses on the association between MS and BMD and fractures, were not conclusive and whether metabolic syndrome might be associated with bone health beyond the contribution of the individual components remains unclear [16,17]. Moreover, sex-differences have been suggested in this relationship, mainly due to differences in body fat distribution between men and women, but yet not clearly defined [18–20]. Recently, a new cluster of criteria for diagnosis of MS had been presented with an emphasis on gender and ethnic differences in the measure of central obesity [21], which has not been adequately studied in relation to bone.
We aimed to study the association between MS, femoral neck BMD (FN-BMD), hip bone geometry (HBG), osteoporosis, and fractures among elderly Dutch men and women, participants of the Rotterdam Study and if these associations were independent of body mass index (BMI). We examined whether MS was associated with FN-BMD and HBG parameters in females and males using a cross-sectional design and to determine whether MS predicts FN-BMD, and incident fractures using a longitudinal design.
Materials and Methods
Study Population
The study was performed within the framework of the Rotterdam Study, a population-based cohort among persons ≥55 years and older living in the Ommoord district of Rotterdam, the Netherlands. The rationale and design of the Rotterdam Study is described elsewhere [22]. The study was approved by the Medical Ethical Committee of Erasmus University, and all participants gave informed consent. The present study used data from the baseline examination of the third wave of the first cohort (RS-I-3) (1997–1999), in which 2,463 females and 1750 males participated and FN-BMD was measured at the fourth round (RSI-4) (2002–2004).
Population for Analysis
Metabolic syndrome, FN-BMD, hip bone geometry and osteoporosis
Among 2463 females and 1750 males, 402 women and 231 men did not have fasting samples or measures of at least on component of MS, and were therefore excluded from the analysis. Furthermore, FN-BMD at RSI-3 (1997–1999), was not assessed in 534 females and 353 males, leaving 1527 females and 1166 males for the cross-sectional analysis regarding MS, FN-BMD and osteoporosis. For the analysis concerning MS and HBG, 124 female and 48 males were further excluded because of no-available information on HBG data (S1 and S2 Figs).
Metabolic syndrome and fractures risk
Among 2061 females and 1519 males with information available on MS components at RSI-3, 29 subjects (21 females and 9 males) were excluded because there was no data on fracture follow-up, hence leaving 2040 females and 1510 males for the analysis on MS and fracture risk. Furthermore, for each type of fracture, prevalent cases were excluded from the analysis (S1 and S2 Figs).
Metabolic Syndrome Definition
MS was defined according to the new criteria announced by a joint scientific statement from the International Diabetes Federation (IDF), the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI), World Heart Federation, International Atherosclerosis Society and International Association for the Study of Obesity [21]. Participants with three or more of the following components were classified as having MS: (1) abdominal obesity (waist circumference (WC) ≥102 cm for men or ≥88 cm for women); (2) high triglycerides (TG) (≥150 mg/dL) (3) low HDL (≤40 mg/dL for men or ≤50 mg/dL for women) (4) elevated blood pressure (BP) (systolic BP ≥130 and/or diastolic BP ≤85 mmHg) or (5) high glucose (fasting glucose level ≥100 mg/dL). The criteria for abdominal obesity were adopted from the cutoffs for European people region [21].
Skeletal Assessments
All events, including incident fractures and death, were reported by general practitioners (GPs) in the research area by means of a computerized system. All reported events were verified by two trained research physicians, who independently reviewed and coded the information. Subsequently, all coded events were reviewed by a medical expert for final classification. Subjects were followed from their baseline visit until January 1, 2007 or until a first fracture or death occurred. FN-BMD (g/cm2) at the RS1-3 (1997–1999) was measured by Dual-energy X-ray absorptiometry (DXA) using a Lunar DPX-L densitometer [23](Lunar Radiation Corp., Madison, WI, USA) and analyzed with DPX-IQ v.4.7d software whereas at the RS1-4 (2002–2004), FN-BMD was measured using a GE Lunar Prodigy bone densitometer. No cross-calibration between the two measures was performed. From the FN-BMD, sex-specific T-scores were calculated using the NHANES reference population [24]. Peak bone mass, as converted to the corresponding Lunar value, was 1.04 ± 0.14 g/cm2 for women and 1.13 ± 0.16 g/cm2 for men. Osteoporosis was defined as a T-score below -2.5 SD whereas osteopenia as a T-score between -1.0 and -2.5. Hip structural analysis [25] was used to measure HBG from the DXA scans of the femur narrow neck region as described previously [26].
Assessment of Covariates
At the third visit, smoking habits were coded as current, and former/never. BMI was calculated as weight (in kg)/height (in m2). Information on medication use at the third round visit included the use of diuretics, hormonal replacement therapy, systemic corticosteroids, drugs for bone and other musculoskeletal diseases. A faller was defined as an individual with a history of one, two, or more falls without precipitating trauma (e.g., car accident or sport injury) in the 12 months preceding the interview at the third round visit. Falling frequency was then recorded as never or at least one. At the third visit to the research center, the total weekly duration of physical activity was assessed by an adapted version of the Zutphen Physical Activity Questionnaire and the LASA Physical Activity Questionnaire. The Dutch Healthy Diet (DHD)-index assessed at the first wave of the Rotterdam Study (1989–1993), was used to take into account overall dietary quality. The DHD represents compliance to the Dutch Guidelines for a Healthy Diet as assessed from the FFQ at baseline [27].
Statistical Analysis
Continuous variables were reported as mean ± SD unless stated otherwise and categorical variables were presented as percentages. Linear regression models and logistic regression were used to determine the cross-sectional association between MS and the number of MS components with FN-BMD, HBG parameters and osteoporosis. For the longitudinal association of MS and its components with FN-BMD, linear regression models were fitted in generalized estimated equations (GEE) with exchangeable correlation structure adjusting for the within-subject correlations due to the repeated measurements of FN-BMD in the same individual (partial Pearson correlation = 0.93 and intra-class correlation = 0.96) [28]. Risk of incident fractures was evaluated for the association with MS and the number of different MS components using Cox proportional hazard regression models. The proportional hazard assumption of the Cox model was checked by the visual inspection of log minus log plots and by performing an interaction test with time. Models for fracture, FN-BMD, and hip geometry were corrected for potential confounders, including age, height, smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index; cross-sectional FN-BMD and HBG were additionally adjusted for BMI and weight respectively, longitudinal analysis on FN-BMD were additionally adjusted for BMI and the two time points FN-BMD measurements were performed (index time) (to adjust also for the lack of cross-calibration between the two measures of BMD) and the interaction between MS (or MS component) and the index time whereas fracture analysis were further adjusted for weight. To analyze the relationship between individual features of MS and FN-BMD, GEE was performed after adjusting for the possible covariates described above with respect to the presence of each component. All analyses were conducted separately for men and women because of gender differences in MS and bone parameters (also the formal tests of interaction (sex×MS) in BMI adjusted models were statistically significant). To correct for multiple testing, a two-tailed P value of 0.025 or less was considered as statistically significant.
To examine if diabetic individuals could influence the associations, we re-ran all analyses excluding subjects with MS who had diabetes mellitus at the third round visit. To adjust for potential bias associated with missing data we used multiple imputation procedure (N = 5 imputations). Rubin’s method was used for the pooled regression coefficients (β) and 95% Confidence Intervals. All analyses were performed using SPSS statistical software (SPSS, version 21.0; SPSS Inc, Chicago, Illinois).
Results
The baseline characteristics of the study population included in the analysis of MS with FN-BMD are shown in Table 1. Six hundred ninety eight (45.7%) female and 435 (37.3%) male participants had MS. On average, female participants were older than men (72.38 vs. 72.04) and were more likely to have osteoporosis (18.2% vs. 14.8%). Anthropometric, lifestyle and other characteristics of the excluded participants did not substantially differ from the participants included in the study (data not shown).
Table 1. Baseline characteristics for participants.
| Women (N = 1,527) | Men (N = 1,166) | |
|---|---|---|
| Age | 72.38 ±6.81 | 72.04 ±6,51 |
| Metabolic Syndrome (n, %) | 698 (45.7) | 435 (37,3) |
| Bone mineral density, 1st round (g/cm2) | 0.82 ± 0.14 | 0.93 ± 0.14 |
| Bone mineral density, 2nd round (g/cm2)* | 0.82 ± 0.13 | 0.92 ± 0.13 |
| Cortical thickness (cm)** | 0.13 ± 0.04 | 0.15 ± 0.03 |
| Bone width (cm)** | 2.93 ± 0.32 | 3.37 ± 0.30 |
| Section modulus (cm3)** | 0.97 ± 0.31 | 1.41 ± 0.34 |
| Cortical buckling ratio** | 13.50 ± 5.00 | 13.15 ± 3.96 |
| Osteoporosis (n, %) | 278 (18.2) | 172 (14.8) |
| Osteopenia (n, %) | 855 (56.0) | 640 (54.6) |
| Diabetes Mellitus (n,%) | 194 (12.7) | 172 (14.8) |
| BMI (kg/m2) | 27.15 ±4.25 | 26.35 ±3.19 |
| Smoking (Yes) (n,%) | 216 (14.0) | 201 (17.2) |
| Physical activity (min/week) | 2820.62 ±1103.74 | 2519.15 ±1178 |
| Alcohol intake (g/day) | 1,57 (396821.4) | 4.29 (79364.3) |
| Dutch Healthy Diet-Index | 50.84 ±9.92 | 45.55 ±9.78 |
| Fallings in the last 12 months (n, %) | 415 (27.2) | 225 (19.3) |
| Diuretic drugs (n,%) | 264 (17.3) | 163 (14.0) |
| HRT (n,%) | 66 (4.3) | 3 (0.26) |
| Corticosteroid drugs (n,%) | 51 (3.3) | 25 (2.1) |
| Bone drugs (n,%) | 56 (3.86) | 6 (0.53) |
| Other musculoskeletal drugs (n,%) | 32 (2.1) | 6 (0.53) |
HRT: Hormone replacement therapy
*999 female and 768 male individuals with available measure of BMD at the second round
**1,403 female and 1,118 male individuals with available measure of hip bone geometry
Cross-sectional association between Metabolic Syndrome, FN-BMD, Hip Bone Geometry and Osteoporosis
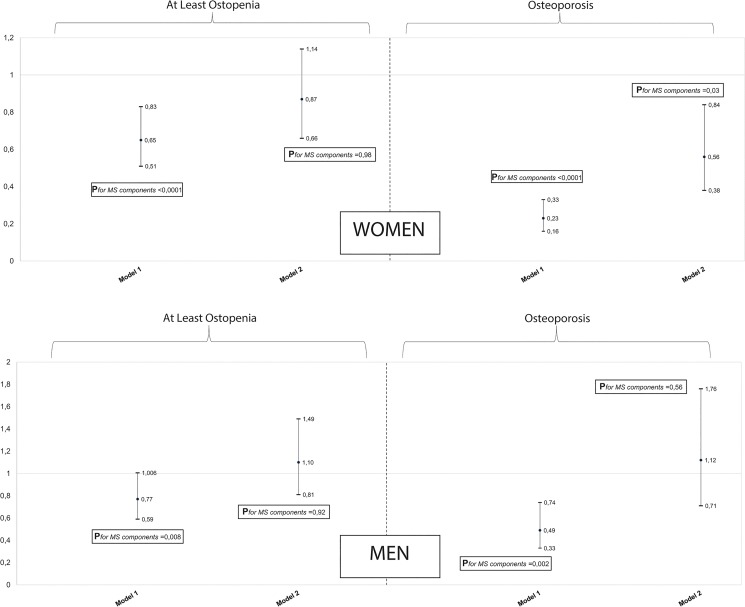
In females, in age-adjusted models, MS was associated with higher FN-BMD (β = 0.056, P = 4.5 10−17), higher cortical thickness (β = 0.01, P = 6.2 10−07), higher section modulus (β = 0.053, P = 0.001), lower cortical buckling ratio (β = -1.93, P = 2.2 10−11) whereas no association was found with bone width (β = -0.033, P = 0.055) (Table 2). After additional adjustments for confounding by BMI, height, lifestyle factors and medication use, the associations were attenuated or reversed (Table 2); however MS was still positively associated with FN-BMD (β = 0.017, P = 0.010), bone width (β = -0.054, P = 0.003) and cortical buckling ratio (β = -0.81, P = 0.003) (Table 2). Similarly, in the multivariable models, the number of MS components was positively associated with FN-BMD (β = 0.006,P = 0.012), femoral neck width (β = -0.026, P<0.001) and cortical buckling ratio (β = -0.26, P = 0.011) whereas no association was observed between MS and cortical thickness or section modulus in females (P>0.025) (Table 2). Also, MS and the number of its components, were inversely associated with osteopenia and osteoporosis in age-adjusted models (osteopenia: OR = 0.65, P = 3.2 10−04, Pfor no. of MS components<0.0001; osteoporosis: OR = 0.23, P = 3.3 10−16, Pfor no. of MS components<0.0001) (Fig 1). After adjustment for BMI although attenuated, the inverse association between MS and osteoporosis remained significant (OR = 0.56, P = 0.006) (Fig 1). Also, a positive association was observed between the number of MS features and osteoporosis in the multivariable model Pfor no. of MS components = 0.03) (Fig 1). Additional adjustment for other confounders did not affect the results (data not shown). In males, MS was associated with higher FN-BMD (β = 0.031, P = 7.4 10−05), higher cortical thickness (β = 0.009, P = 9.3 10−07), higher section modulus (β = 0.096, P = 3.0 10−07) and lower cortical buckling ratio (β = -0.88, P = 2.2 10−04) in age-adjusted models (Table 2). However, after adjustment for BMI and height, MS was neither statistically significantly associated with FN-BMD nor with hip bone geometry parameters (Table 2). Similarly, there was no association between number of MS components, FN-BMD and hip bone geometry in the fully adjusted models (Table 2). Also, in age-adjusted models, MS was inversely associated with osteoporosis but not with osteopenia (osteopenia: OR = 0.77, P = 0.056, Pfor no. of MS components = 0.008; osteoporosis: OR = 0.49, P = 0.001, Pfor no. of MS components = 0.002) (Fig 1). However, no association was observed between MS and its components with osteopenia or osteoporosis after adjustment for BMI (Fig 1) and other confounders (data not shown).
Table 2. The cross-sectional association of metabolic syndrome with bone mineral density and bone geometry.
| Women | Men | ||||
|---|---|---|---|---|---|
| FN-BMD, n = 1,527 | FN-BMD, n = 1,166 | ||||
| Metabolic Syndrome | β (95%CI) | P-value | Metabolic Syndrome | β (95%CI) | P-value |
| Model 1 | 0.056 (0.043; 0.069) | 4.5 10−17 | Model 1 | 0.031 (0.015; 0.047) | 7.4 10−5 |
| Model 2 | 0.018 (0.003; 0.030) | 0.007 | Model 2 | -0.005 (-0.014; 0.003) | 0.55 |
| Model 3 | 0.017 (0.004; 0.030) | 0.10 | Model 3 | -0.002 (-0.020; 0.015) | 0.82 |
| No. of MS components | No. of MS components | ||||
| Model 1 | 0.022 (0.017; 0.026) | 8.08 10−20 | Model 1 | 0.012 (0.006; 0.018) | 9.6 10−5 |
| Model 2 | 0.007 (0.002;0.011) | 0.009 | Model 2 | -0.004 (-0.007; 0.001) | 0.30 |
| Model 3 | 0.006 (0.001; 0.011) | 0.012 | Model 3 | -0.002 (-0.009; 0.005) | 0.53 |
| Cortical thickness, n = 1,403 | Cortical thickness, n = 1,118 | ||||
| Metabolic Syndrome | β (95%CI) | P-value | Metabolic Syndrome | β (95%CI) | P-value |
| Model 1 | 0.010 (0.005; 0.014) | 6.2 10−7 | Model 1 | 0.009 (0.005; 0.012) | 9.3 10−7 |
| Model 2 | 0.001 (-0.003; 0.005) | 0.69 | Model 2 | -0.001 (-0.003; 0.001) | 0.56 |
| Model 3 | 0.001 (-0.004; 0.006) | 0.73 | Model 3 | -0.0005 (-0.004; 0.003) | 0.80 |
| No. of MS components | No. of MS components | ||||
| Model 1 | 0.004 (0.003; 0.006) | 1.33 10−8 | Model 1 | 0.003 (0.002; 0.005) | 7.3 10−7 |
| Model 2 | 0.001 (-0.001; 0.002) | 0.42 | Model 2 | -0.001 (-0.002; 0.000) | 0.26 |
| Model 3 | 0.001 (-0.001; 0.002) | 0.49 | Model 3 | -0.001 (-0.002; 0.001) | 0.45 |
| Bone width, n = 1,403 | Bone width, n = 1,118 | ||||
| Metabolic Syndrome | β (95%CI) | P-value | Metabolic Syndrome | β (95%CI) | P-value |
| Model 1 | -0.033 (-0.068; 0.001) | 0.055 | Model 1 | 0.006 (-0.003; 0.042) | 0.76 |
| Model 2 | -0.051 (-0.09; -0.015) | 0.005 | Model 2 | -0.030 (-0.068; 0.008) | 0.12 |
| Model 3 | -0.054 (-0.091; -0.018) | 0.003 | Model 3 | -0.029 (-0.068; 0.010) | 0.14 |
| No. of MS components | No. of MS components | ||||
| Model 1 | -0.015 (-0.027; -0.002) | 0.021 | Model 1 | 0.001 (-0.014; 0.015) | 0.93 |
| Model 2 | -0.025 (-0.038; -0.011) | 0.0003 | Model 2 | -0.014 (-0.029; 0.001) | 0.076 |
| Model 3 | -0.026 (-0.039; -0.012) | 0.0002 | Model 3 | -0.013 (-0.029; 0.002) | 0.097 |
| Section Modulus, n = 1,403 | Section Modulus, n = 1,118 | ||||
| Metabolic Syndrome | β (95%CI) | P-value | Metabolic Syndrome | β (95%CI) | P-value |
| Model 1 | 0.053 (0.021; 0.086) | 0.001 | Model 1 | 0.096 (0.056; 0.136) | 3.0 10−7 |
| Model 2 | -0.029 (-0.062; 0.003) | 0.08 | Model 2 | -0.028 (-0.068; 0.011) | 0.159 |
| Model 3 | -0.03 (-0.063; 0.003) | 0.078 | Model 3 | -0.021 (-0.061; 0.019) | 0.30 |
| No. of MS components | No. of MS components | ||||
| Model 1 | 0.024 (0.012; 0.036) | 5.6 10−5 | Model 1 | 0.036 (0.021; 0.052) | 5.0 10−7 |
| Model 2 | -0.011 (-0.023; 0.002) | 0.09 | Model 2 | -0.017 (-0.032; -0.001) | 0.036 |
| Model 3 | -0.011 (-0.023; 0.001) | 0.08 | Model 3 | -0.014 (-0.030; 0.002) | 0.094 |
| Cortical Buckling Ratio, n = 1,403 | Cortical Buckling Ratio, n = 1,118 | ||||
| Metabolic Syndrome | β (95%CI) | P-value | Metabolic Syndrome | β (95%CI) | P-value |
| Model 1 | -1.93 (-2.42; -1.43) | 2.2 10−11 | Model 1 | -0.88 (-1.35; -0.41) | 2.2 10−4 |
| Model 2 | -0.79 (-1.32; -0.26) | 0.004 | Model 2 | 0.036 (-0.23; 03037) | 0.89 |
| Model 3 | -0.81 (-1.34; -0.27) | 0.003 | Model 3 | -0.049 (-0.56; 0.46) | 0.85 |
| No. of MS components | No. of MS components | ||||
| Model 1 | -0.71 (-0.89; -0.53) | 3.1 10−12 | Model 1 | -0.314 (-0.50; -0.13) | 0.001 |
| Model 2 | -0.25 (-0.45; -0.06) | 0.012 | Model 2 | 0.101 (-0.003; 0.21) | 0.33 |
| Model 3 | -0.26 (-0.46; -0.06) | 0.011 | Model 3 | 0.07 (-0.14; 0.27) | 0.51 |
MS, metabolic syndrome; FN-BMD, femoral neck bone mineral density
Model 1: Adjusted for age
Model 2: Model 1 +body mass index and height for FN-BMD and weight + height for hip bone geometry parameters.
Model 3: Model 2 + smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index.
Fig 1. The association between metabolic syndrome, osteopenia and osteoporosis in women and men.
Reference group are subjects with no osteopenia, neither osteoporosis: Confounders include age, body mass index, height, smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index.
Longitudinal Association between Metabolic Syndrome and FN-BMD
Similar to the cross-sectional analysis, MS and the number of its features was positively associated with FN-BMD (β = 0.028, P = 0.001; Pfor no. of MS components = 0.001) in the multivariable model in females, which tended to go away across time (interaction MS x index time: β = -0.008, p = 0.031; interaction MS component x index time: β = -0.003, p = 0.021). No association was observed between MS or its features and adjusted FN-BMD in males (Table 3).
Table 3. The longitudinal association of metabolic syndrome with bone mineral density.
| Women (N = 1,527) | Men (N = 1,166)# | ||||
|---|---|---|---|---|---|
| Metabolic syndrome (Yes vs. No) | FN-BMD | P-value | Metabolic syndrome (Yes vs. No) | FN-BMD | P-value |
| Model 1: β, 95% CI | 0.063 (0.048; 0.079) | 2.44 10−15 | Model 1: β, 95% CI | 0.031 (0.015; 0.047) | 0.0001 |
| Model 2: β, 95% CI | 0.028 (0.015; 0.042) | 0.001 | Model 2: β, 95% CI | -0.006 (-0.016; 0.004) | 0.58 |
| Model 3: β, 95% CI | 0.028 (0.012; 0.043)* | 0.001 | Model 3: β, 95% CI | -0.002 (-0.022; 0.017) | 0.83 |
| No. of MS components (continuous) | No. of MS components (continuous) | ||||
| Model 1: β, 95% CI | 0.025 (0.019; 0.030) | 5.4 10−20 | Model 1: β, 95% CI | 0.013 (0.006; 0.020) | 0.0003 |
| Model 2: β, 95% CI | 0.011 (0.005;0.016) | 0.0004 | Model 2: β, 95% CI | -0.003 (-0.007; 0.001) | 0.46 |
| Model 3: β, 95% CI | 0.010 (0.004; 0.016)** | 0.001 | Model 3: β, 95% CI | -0.001 (-0.009; 0.006) | 0.75 |
MS, metabolic syndrome; FN-BMD, femoral neck bone mineral density
Model 1: Adjusted for age and type of DXA scan
Model 2: Model 1 +body mass index and height
Model 3: Model 2 + smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index.
*index time (time points when the DXA measurements were performed), β = -0.012, p<0.001; interaction MS x index time: β = -0.008, p = 0.031
** index time, β = -0.012, p<0.001; interaction MS component x index time: β = -0.003, p = 0.021
#no significant interaction between MS (or MS component) and index time (p>0.50) was observed in any of the analysis in men and therefore data are not shown
Association between Metabolic Syndrome and Fracture Risk
In females, no association was observed between MS and any type of fractures, neither in age and gender adjusted model, nor in the multivariable model (HR = 0.91: 95%CI: 0.73–1.15) (Table 4). Also no association was observed for non-vertebral fractures (HR = 0.94: 95%CI: 0.73–1.21) or vertebral fractures (HR = 0.83: 95%CI: 0.56–1.24) (Table 3). Similarly, there was no significant association between MS with any type of fractures or with subtypes of fractures in males (Table 4). Nevertheless, in males, significant inverse associations were observed between numbers of MS components with any type of fractures (P = 0.015) and with non-vertebral fractures (P = 0.017) (Table 3).
Table 4. Metabolic syndrome and fracture risk.
| Women | Men | ||||
|---|---|---|---|---|---|
| All Fractures (371) | All Fractures (147) | ||||
| Metabolic Syndrome | Hazard ratio (95%CI) | P-value | Metabolic Syndrome | Hazard ratio (95%CI) | P-value |
| Model 1 | 0.85 (0.69–1.04) | 0.12 | Model 1 | 0.85 (0.60–1.20) | 0.36 |
| Model 2 | 0.91 (0.72–1.14) | 0.40 | Model 2 | 0.74 (0.69–1.08) | 0.12 |
| Model 3 | 0.91 (0.73–1.15) | 0.43 | Model 3 | 0.68 (0.46–1.006) | 0.054 |
| No. of MS components | No. of MS components | ||||
| Model 1 | 0.94 (0.87–1.02) | 0.11 | Model 1 | 0.92 (0.81–1.06) | 0.24 |
| Model 2 | 0.97 (0.89–1.05) | 0.44 | Model 2 | 0.86 (0.74–1.001) | 0.055 |
| Model 3 | 0.97 (0.89–1.06) | 0.47 | Model 3 | 0.82 (0.70–0.9964) | 0.015 |
| Non-Vertebral Fractures (307) | Non-Vertebral Fractures (102) | ||||
| Metabolic Syndrome | Hazard ratio (95%CI) | P-value | Metabolic Syndrome | Hazard ratio (95%CI) | P-value |
| Model 1 | 0.90 (0.72–1.13) | 0.36 | Model 1 | 0.89 (0.59–1.35) | 0.59 |
| Model 2 | 0.94 (0.73–1.21) | 0.63 | Model 2 | 0.69 (0.55–1.88) | 0.12 |
| Model 3 | 0.94 (0.73–1.21) | 0.61 | Model 3 | 0.64 (0.40–1.03) | 0.068 |
| No. of MS components | No. of MS components | ||||
| Model 1 | 0.96 (0.89–1.05) | 0.38 | Model 1 | 0.94 (0.79–1.10) | 0.42 |
| Model 2 | 0.98 (0.89–1.08) | 0.70 | Model 2 | 0.83 (0.68–1.01) | 0.047 |
| Model 3 | 0.98 (0.89–1.08) | 0.66 | Model 3 | 0.75 (0.66–0.96) | 0.017 |
| Vertebral Fractures (123) | Vertebral Fractures (62) | ||||
| Metabolic Syndrome | Hazard ratio (95%CI) | P-value | Metabolic Syndrome | Hazard ratio (95%CI) | P-value |
| Model 1 | 0.68 (0.47–0.98) | 0.039 | Model 1 | 0.65 (0.37–1.13) | 0.13 |
| Model 2 | 0.80 (0.53–1.19) | 0.27 | Model 2 | 0.67 (0.49–1.25) | 0.20 |
| Model 3 | 0.83 (0.56–1.24) | 0.36 | Model 3 | 0.60 (0.32–1.14) | 0.12 |
| No. of MS components | No. of MS components | ||||
| Model 1 | 0.84 (0.73–0.96) | 0.01 | Model 1 | 0.84 (0.6–1.03) | 0.10 |
| Model 2 | 0.86 (0.76–1.03) | 0.11 | Model 2 | 0.85 (0.75–1.07) | 0.17 |
| Model 3 | 0.90 (0.77–1.05) | 0.18 | Model 3 | 0.81 (0.64–1.03) | 0.09 |
“( )”, number of fractures
Model 1: Adjusted for age
Model 2: Model 1 +Height and Weight
Model 3: Model 2 + smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index.
Additional Analysis
S1 Table shows the effect of individual components of MS on the adjusted FN-BMD. In both genders, elevated glucose levels were associated with higher BMD (in females: β = 0.016, P = 0.01; in males: β = 0.022, P = 0.004). In women, but not in men, HDL-cholesterol was positively associated with FN-BMD (β = 0.013, P = 0.01). In men but not in women, waist circumference component was inversely associated with FN-BMD (in males: β = -0.030, P = 0.004). No association was observed between other components of MS and adjusted FN-BMD in either gender.
Exclusion of subjects with MS having diabetes mellitus (194 females and 172 males) did not substantially change any of the results (data not shown). Moreover, substitution in the multivariable models of BMI with weight and vice versa, did not change any of the results (data not shown).
Discussion
To our knowledge, this is the first study to simultaneously examine the association between metabolic syndrome, FN-BMD, HBG parameters, osteoporosis and fracture risk by using the most recent definition of MS. Females with MS, have significantly higher BMD, narrower bone at the hip, and increased bone instability (lower buckling ratio), lower odds of having osteoporosis than non-MS individuals, independent of BMI. In males, the positive association of MS with BMD and HBG geometry was explained by BMI. Our results on fracture risk, suggest no consistent influence of MS in either gender.
According to the observational data in the past decade, the relationship between MS and its components, BMD and fracture risk is controversial. In line with our findings, a recent meta-analysis showed that MS may have beneficial influence on BMD in Caucasian individuals [16]. Also, another meta-analysis on MS and fracture risk, concluded that individuals with MS are not at higher risk of having fractures [17]. MS is a cluster of conditions, interacting with each other, and therefore the mechanism behind the effect of MS on BMD and fractures risk is complicated and has not yet been investigated in detail. Although, the association between individual components of MS and bone metabolism have been extensively studied, the results are yet inconclusive. (1) For example, central obesity has been associated with higher BMD in some studies, but some others and our study as well have shown detrimental effects[29,30]. Also, obesity, is a risk factor for fractures of the humerus and ankle, but protects against fractures of hip and vertebral bodies [31–33]. (2) Elevated glucose levels have been linked to better, worse or similar bone outcomes [18,34,35]. (3) Hypertension is postulated to be associated with low bone mass due to urinary calcium excretion and therefore increase fracture risk [36], but, contrary to common belief, intensive antihypertensive treatment was not associated with an increased risk of falls or non-spine fractures in patients with type 2 diabetes in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) randomized trial [37]. Hypertriglyceridemia contributes to a lower risk of fractures, which may partly be explained by the interaction with protein matrix and bone minerals [12,38]. However, Kim et al [39] and Adami et al [13] found that high triglyceride levels and low HDL-cholesterol were negatively associated with BMD. Therefore, as observed in the current study, the combined effects of these components on bone metabolism may be beneficial or insignificant.
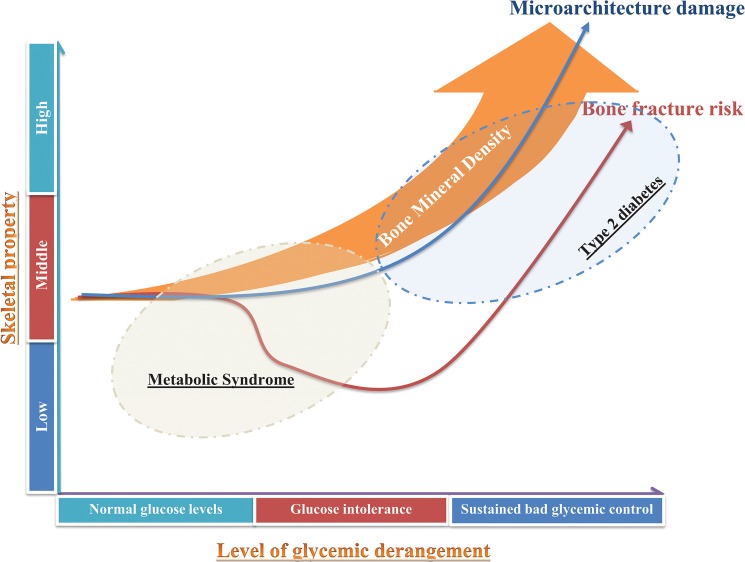
The positive association between MS and BMD observed in the present study was mainly driven by glucose levels. MS is a risk factor for type 2 diabetes mellitus which has been associated with an increase in fracture risk. In contrast to MS individuals, evaluation of BMD may not be adequate for predicting fracture risk in patients with type 2 diabetes, who are unlikely to be diagnosed with osteoporosis and increased risk of fracture [10]. In the large Rotterdam Study, we previously showed that, similar to MS individuals, diabetic patients have higher BMD and stronger bone geometry, which would protect them against fractures [10]. However, in contrast to MS individuals, diabetic individuals have an increased fracture risk, which was shown to be driven by poor glycemic control [10]. We postulate that increased bone fragility may be caused by chronically elevated glucose levels, which may lead to accumulation of microcracks and/or cortical porosity. MS is a health condition which predisposes to type 2 diabetes mellitus, but may not yet be characterized by chronically elevated glucose levels. In the present study, the positive association between MS and BMD persisted also after exclusion of subjects with MS who had diabetes mellitus. Thus, it is likely that, microcracks and/or cortical porosity may not be present in MS individuals which may explain why MS subjects do not yet experience a high risk of fractures (Fig 2). Follow-up studies focusing on the health life trend of MS individuals in relation to bone are thus needed.
Fig 2. Level of glycemic derangement, bone architecture and fracture risk.
Cartoon depicting the differences in bone mineral density, fracture risk and changes in bone microarchitecture across the stages of glucose derangement. Metabolic syndrome and diabetes mellitus individuals have higher BMD but do not experience yet an increase in fracture risk. With sustained bad glycemic control, the damage of bone microarchitecture represented by accumulation of microcracks and cortical porosity becomes a possibility which may explain the bone fragility and fracture susceptibility despite the observed increase in BMD. Drawing is not to scale.
The current study shows that no gender differences are observed between MS and unadjusted BMD and fracture risk, but that gender differences become prominent after adjustment for BMI and that in men, the observed positive association between MS and BMD and hip bone geometry parameters is explained by obesity. Similar to our observations, the meta-analysis investigating the association between MS and unadjusted BMD concluded that there were no gender differences [16]. Also, the recent meta-analysis examining the association between MS and fracture risk did not observed any difference between men and women with similar estimates to our study [17]. In contrast, gender differences in the association between MS and BMI-adjusted BMD have been previously described, showing less beneficial effects of MS on bone health in men than in women [39,40]. In contrast to our results, both studies observed a decrease in FN-BMD with increasing number of MS components in men, but not in women. However, both studies were characterized by other ethnicities or were performed in a younger population. It has been shown that the association between MS and BMD differs by ethnicity [16]. Also, BMD declines by age and this decline differs by gender [41]. In a twin study, fat mass and body fat distribution seem to have different relationships with BMD according to gender and age [42]. Since fat deposition differs according to gender, it has been hypothesized that mechanical effect and estrogen synthesis predominate in women, while bone-deleterious effects of fat, related to oxidative stress and chronic inflammation, predominate in men [43]. Therefore, bone mass in males with MS may be more influenced by visceral fat than in women which may explain the dilution of the association after adjustment for BMI and the relationship between waist circumference and BMD in men and not in women.
There are several strength of our present study. First, this is a large prospective population based study of 3,458 individuals, with comprehensive follow up of more than 6.7 years on average. We were also able to examine both cross-sectional and longitudinal the associations between MS, BMD and osteoporosis. Additionally, the present study had various indices of bone outcomes available, including hip bone geometry parameters and fracture incidence. Moreover, in contrast to other studies, we used the most recent definition of MS. Yet our study has some limitations. We did not have measures of glucose control, such as HBA1C which could have strengthened our results. Secondly, the subjects in this study were only caucasians. Ethnic differences in the association between MS and/or its components and bone have been previously reported. Thus, our findings may not be extended to non-caucasian groups.
In conclusion, MS is associated with higher BMD, increase instability and narrower bone, which is mainly driven by elevated glucose levels. In men but not in women, higher FN-BMD was mainly explained by body mass index and body fat distribution. We postulate that the bone of MS individuals is not yet characterized by an accumulation of microcracks (cortical porosity) that would reflect sustained impairment of bone structure, and therefore yet an increased risk of fragility, as observed in diabetic individuals. These highlight the importance of maintaining glycemic control in individuals with MS to pervert skeletal complications and preserve bone health.
Supporting Information
(PDF)
(PDF)
FN-BMD: femoral neck bone mineral density. *Waist circumference: ≥102 cm for men or ≥88 cm for women; Triglyceride: ≥150 mg/Dl; HDL-cholesterol:≤40 mg/dL for men or ≤50 mg/dL for women; fasting glucose ≥100 mg/Dl; blood pressure: systolic BP ≥130 and/or diastolic BP ≤85 mmHg. 1: triglyceride component, HDL-cholesterol component, hypertension component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 2: waist circumference component, HDL-cholesterol component, hypertension component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 3: waist circumference component, triglyceride component, hypertension component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 4: waist circumference component, triglyceride component, HDL-cholesterol component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 5: waist circumference component, triglyceride component, HDL-cholesterol component, hypertension component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index.
(DOCX)
Data Availability
All the data relevant to this study are freely available in the paper and supplemental files. Individual level data from the Rotterdam Study participants can be made available per request and approval of the Rotterdam Study Management Team (secretariat.epi@erasmusmc.nl<mailto:secretariat.epi@erasmusmc.nl>).
Funding Statement
TM, JCK and OHF work in ErasmusAGE, a center for aging research across the life course funded by Nestlé Nutrition (Nestec Ltd.); Metagenics Inc.; and AXA. Additional support from the Netherlands Organization for Health Research (NWO) was provided to FR (ZonMw VIDI 016.136.367) and AD (ZonMW VENI 916.12.154) who also received an EUR Fellowship. These funding sources had no role in design and conduct of this manuscript; collection, management, analysis, and interpretation of the data; and preparation, review or approval of this manuscript.
References
- 1. Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality Risk Associated With Low-Trauma Osteoporotic Fracture and Subsequent Fracture in Men and Women. Jama-Journal of the American Medical Association 301: 513–521. 10.1001/jama.2009.50 [DOI] [PubMed] [Google Scholar]
- 2. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. LANCET 353: 878–882. [DOI] [PubMed] [Google Scholar]
- 3. Nelson LR, Bulun SE (2001) Estrogen production and action. Journal of the American Academy of Dermatology 45: S116–S124. [DOI] [PubMed] [Google Scholar]
- 4. Ohta H, Ikeda T, Masuzawa T, Makita K, Suda Y, Nozawa S (1993) Differences in Axial Bone-Mineral Density, Serum Levels of Sex Steroids, and Bone Metabolism between Postmenopausal and Age-Matched and Body Size-Matched Premenopausal Subjects. Bone 14: 111–116. [DOI] [PubMed] [Google Scholar]
- 5. Hofbauer LC, Schoppet M (2004) Clinical implications of the osteoprotegerin/RANKL/RANK system for bone and vascular diseases. Jama-Journal of the American Medical Association 292: 490–495. [DOI] [PubMed] [Google Scholar]
- 6. Smith BJ, Lerner MR, Bu SY, Lucas EA, Hanas JS, Lightfoot SA, et al. (2006) Systemic bone loss and induction of coronary vessel disease in a rat model of chronic inflammation. Bone 38: 378–386. [DOI] [PubMed] [Google Scholar]
- 7. Campos RMS, de Piano A, da Silva PL, Carnier J, Sanches PL, Corgosinho FC, et al. (2012) The role of pro/anti-inflammatory adipokines on bone metabolism in NAFLD obese adolescents: effects of long-term interdisciplinary therapy. Endocrine 42: 146–156. [DOI] [PubMed] [Google Scholar]
- 8. Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166: 495–505. [DOI] [PubMed] [Google Scholar]
- 9. Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, et al. (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305: 2184–2192. 10.1001/jama.2011.715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oei L, Zillikens MC, Dehghan A, Buitendijk GHS, Castano-Betancourt MC, Estrada K, et al. (2013) High Bone Mineral Density and Fracture Risk in Type 2 Diabetes as Skeletal Complications of Inadequate Glucose Control The Rotterdam Study. Diabetes Care 36: 1619–1628. 10.2337/dc12-1188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ma LL, Oei L, Jiang LD, Estrada K, Chen HY, Wang Z, et al. (2012) Association between bone mineral density and type 2 diabetes mellitus: a meta-analysis of observational studies. European Journal of Epidemiology 27: 319–332. 10.1007/s10654-012-9674-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yamaguchi T, Sugimoto T, Yano S, Yamauchi M, Sowa H, Chen QX, et al. (2002) Plasma lipids and osteoporosis in postmenopausal women. Endocrine Journal 49: 211–217. [DOI] [PubMed] [Google Scholar]
- 13. Adami S, Braga V, Zamboni M, Gatti D, Rossini M, Bakri J, et al. (2004) Relationship between lipids and bone mass in 2 cohorts of healthy women and men. Calcified Tissue International 74: 136–142. [DOI] [PubMed] [Google Scholar]
- 14. Tsuda K, Nishio I, Masuyama Y (2001) Bone mineral density in women with essential hypertension. American Journal of Hypertension 14: 704–707. [DOI] [PubMed] [Google Scholar]
- 15. Cappuccio FP, Meilahn E, Zmuda JM, Cauley JA, Grp SOFR (1999) High blood pressure and bone-mineral loss In elderly white women: a prospective study. LANCET 354: 971–975. [DOI] [PubMed] [Google Scholar]
- 16. Xue P, Gao P, Li YK (2012) The association between metabolic syndrome and bone mineral density: a meta-analysis. Endocrine 42: 546–554. 10.1007/s12020-012-9684-1 [DOI] [PubMed] [Google Scholar]
- 17. Sun K, Liu JM, Lu N, Sun HX, Ning G (2014) Association between metabolic syndrome and bone fractures: a meta-analysis of observational studies. Bmc Endocrine Disorders 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yamaguchi T, Kanazawa I, Yamamoto M, Kurioka S, Yamauchi M, Yano S, et al. (2009) Associations between components of the metabolic syndrome versus bone mineral density and vertebral fractures in patients with type 2 diabetes. Bone 45: 174–179. 10.1016/j.bone.2009.05.003 [DOI] [PubMed] [Google Scholar]
- 19. BarrettConnor E, KritzSilverstein D (1996) Does hyperinsulinemia preserve bone? DIABETES CARE 19: 1388–1392. [DOI] [PubMed] [Google Scholar]
- 20. Kim H, Oh HJ, Choi H, Choi WH, Lim SK, Kim JG (2013) The association between bone mineral density and metabolic syndrome: a Korean population-based study. J Bone Miner Metab 31: 571–578. 10.1007/s00774-013-0446-9 [DOI] [PubMed] [Google Scholar]
- 21. Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. (2009) Harmonizing the Metabolic Syndrome A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120: 1640–1645. 10.1161/CIRCULATIONAHA.109.192644 [DOI] [PubMed] [Google Scholar]
- 22. Hofman A, Murad SD, van Duijn CM, Franco OH, Goedegebure A, Ikram MA, et al. (2013) The Rotterdam Study: 2014 objectives and design update. European Journal of Epidemiology 28: 889–926. 10.1007/s10654-013-9866-z [DOI] [PubMed] [Google Scholar]
- 23. Burger H, de Laet CEDH, van Daele PLA, Weel AEAM, Witteman JCM, Hofman A, et al. (1998) Risk factors for increased bone loss in an elderly population—The Rotterdam Study. American Journal of Epidemiology 147: 871–879. [DOI] [PubMed] [Google Scholar]
- 24. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, et al. (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporosis International 8: 468–489. [DOI] [PubMed] [Google Scholar]
- 25. Beck TJ, Looker AC, Ruff CB, Sievanen H, Wahner HW (2000) Structural trends in the aging femoral neck and proximal shaft: Analysis of the Third National Health and Nutrition Examination Survey dual-energy X-ray absorptiometry data. Journal of Bone and Mineral Research 15: 2297–2304. [DOI] [PubMed] [Google Scholar]
- 26. Rivadeneira F, Zillikens MC, De Laet CE, Hofman A, Uitterlinden AG, Beck TJ, et al. (2007) Femoral neck BMD is a strong predictor of hip fracture susceptibility in elderly men and women because it detects cortical bone instability: The Rotterdam study. Journal of Bone and Mineral Research 22: 1781–1790. [DOI] [PubMed] [Google Scholar]
- 27. Klipstein-Grobusch K, den Breeijen JH, Goldbohm RA, Geleijnse JM, Hofman A, Grobbee DE, et al. (1998) Dietary assessment in the elderly: validation of a semiquantitative food frequency questionnaire. Eur J Clin Nutr 52: 588–596. [DOI] [PubMed] [Google Scholar]
- 28. Zeger SL, Liang KY, Albert PS (1988) Models for Longitudinal Data—a Generalized Estimating Equation Approach. Biometrics 44: 1049–1060. [PubMed] [Google Scholar]
- 29. Edelstein SL, Barrettconnor E (1993) Relation between Body-Size and Bone-Mineral Density in Elderly Men and Women. American Journal of Epidemiology 138: 160–169. [DOI] [PubMed] [Google Scholar]
- 30. Jankowska EA, Rogucka E, Medras M (2001) Are general obesity and visceral adiposity in men linked to reduced bone mineral content resulting from normal ageing? A population-based study. Andrologia 33: 384–389. [DOI] [PubMed] [Google Scholar]
- 31. Schott AM, Cormier C, Hans D, Favier F, Hausherr E, Dargent-Molina P, et al. (1998) How hip and whole-body bone mineral density predict hip fracture in elderly women: The EPIDOS prospective study. Osteoporosis International 8: 247–254. [DOI] [PubMed] [Google Scholar]
- 32. Gnudi S, Sitta E, Lisi L (2009) Relationship of body mass index with main limb fragility fractures in postmenopausal women. Journal of Bone and Mineral Metabolism 27: 479–484. 10.1007/s00774-009-0056-8 [DOI] [PubMed] [Google Scholar]
- 33. Spaine LA, Bollen SR (1996) 'The bigger they come…': The relationship between body mass index and severity of ankle fractures. Injury-International Journal of the Care of the Injured 27: 687–689. [DOI] [PubMed] [Google Scholar]
- 34. Kinjo M, Setoguchi S, Solomon DH (2007) Bone mineral density in adults with the metabolic syndrome: Analysis in a population-based US sample. Journal of Clinical Endocrinology & Metabolism 92: 4161–4164. [DOI] [PubMed] [Google Scholar]
- 35. Holmberg AH, Nilsson PM, Nilsson JA, Akesson K (2008) The association between hyperglycemia and fracture risk in middle age. A prospective, population-based study of 22,444 men and 10,902 women. Journal of Clinical Endocrinology & Metabolism 93: 815–822. [DOI] [PubMed] [Google Scholar]
- 36. Vestergaard P, Rejnmark L, Mosekilde L (2009) Hypertension Is a Risk Factor for Fractures. Calcified Tissue International 84: 103–111. 10.1007/s00223-008-9198-2 [DOI] [PubMed] [Google Scholar]
- 37.Margolis KL, Palermo L, Vittinghoff E, Evans GW, Atkinson HH, Hamilton BP, et al. (2014) Intensive Blood Pressure Control, Falls, and Fractures in Patients with Type 2 Diabetes: The ACCORD Trial. J Gen Intern Med. [DOI] [PMC free article] [PubMed]
- 38. Xu SH, Yu JQJ (2006) Beneath the minerals, a layer of round lipid particles was identified to mediate collagen calcification in compact bone formation. Biophysical Journal 91: 4221–4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kim HY, Choe JW, Kim HK, Bae SJ, Kim BJ, Lee SH, et al. (2010) Negative Association between Metabolic Syndrome and Bone Mineral Density in Koreans, Especially in Men. Calcified Tissue International 86: 350–358. 10.1007/s00223-010-9347-2 [DOI] [PubMed] [Google Scholar]
- 40. Kim H, Oh HJ, Choi H, Choi WH, Lim SK, Kim JG (2013) The association between bone mineral density and metabolic syndrome: a Korean population-based study. Journal of Bone and Mineral Metabolism 31: 571–578. 10.1007/s00774-013-0446-9 [DOI] [PubMed] [Google Scholar]
- 41. Krall EA, DawsonHughes B, Hirst K, Gallagher JC, Sherman SS, Dalsky G (1997) Bone mineral density and biochemical markers of bone turnover in healthy elderly men and women. Journals of Gerontology Series a-Biological Sciences and Medical Sciences 52: M61–M67. [DOI] [PubMed] [Google Scholar]
- 42. Makovey J, Naganathan V, Sambrook P (2005) Gender differences in relationships between body composition components, their distribution and bone mineral density: a cross-sectional opposite sex twin study. Osteoporosis International 16: 1495–1505. [DOI] [PubMed] [Google Scholar]
- 43. Hernandez JL, Olmos JM, Gonzalez-Macias J (2011) Metabolic syndrome, fractures and gender. Maturitas 68: 217–223. 10.1016/j.maturitas.2010.12.010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
FN-BMD: femoral neck bone mineral density. *Waist circumference: ≥102 cm for men or ≥88 cm for women; Triglyceride: ≥150 mg/Dl; HDL-cholesterol:≤40 mg/dL for men or ≤50 mg/dL for women; fasting glucose ≥100 mg/Dl; blood pressure: systolic BP ≥130 and/or diastolic BP ≤85 mmHg. 1: triglyceride component, HDL-cholesterol component, hypertension component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 2: waist circumference component, HDL-cholesterol component, hypertension component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 3: waist circumference component, triglyceride component, hypertension component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 4: waist circumference component, triglyceride component, HDL-cholesterol component, glucose component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index. 5: waist circumference component, triglyceride component, HDL-cholesterol component, hypertension component, age, index time, BMI and height. smoking status, physical activity, alcohol intake, fallings in the last 12 months, use of diuretics drugs, use of hormone replacement therapy, use of corticosteroids drugs, use of drugs for bone and other musculoskeletal diseases and Dutch Healthy Diet Index.
(DOCX)
Data Availability Statement
All the data relevant to this study are freely available in the paper and supplemental files. Individual level data from the Rotterdam Study participants can be made available per request and approval of the Rotterdam Study Management Team (secretariat.epi@erasmusmc.nl<mailto:secretariat.epi@erasmusmc.nl>).