Abstract
Objectives
We analysed near-miss and injury events reported to the National Fire Fighter Near-Miss Reporting System (NFFNMRS) to investigate the workplace hazards and safety concerns of Emergency Medical Services (EMS) responders in the USA.
Methods
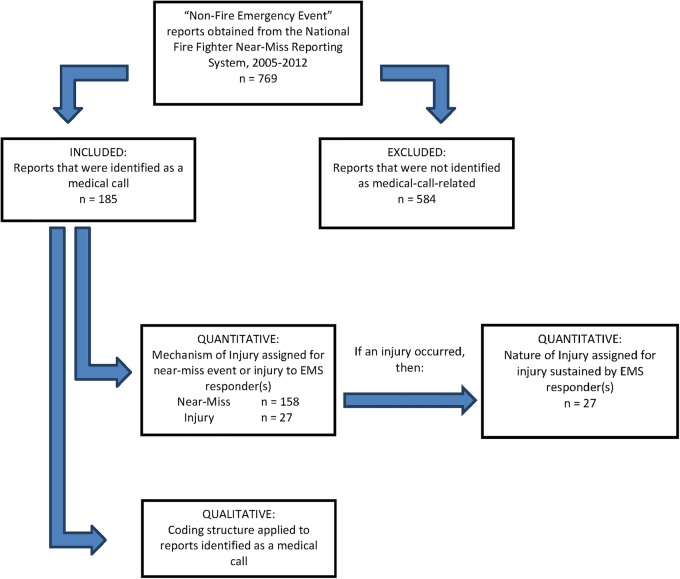
We reviewed 769 ‘non-fire emergency event’ reports from the NFFNMRS using a mixed methods approach. We identified 185 emergency medical calls and analysed their narrative text fields. We assigned Mechanism of Near-Miss/Injury and Nature of Injury codes and then tabulated frequencies (quantitative). We coded major themes regarding work hazards and safety concerns reported by the EMS responders (qualitative).
Results
Of the 185 emergency medical calls, the most commonly identified Mechanisms of Near-Miss/Injury to EMS responders was Assaults, followed by Struck-by Motor Vehicle, and Motor Vehicle Collision. The most commonly identified weapon used in an assault was a firearm. We identified 5 major domains of workplace hazards and safety concerns: Assaults by Patients, Risks from Motor Vehicles, Personal Protective Equipment, Relationships between Emergency Responders, and Policies, Procedures and Practices.
Conclusions
Narrative text from the NFFNMRS is a rich source of data that can be analysed quantitatively and qualitatively to provide insight into near-misses and injuries sustained by EMS responders. Near-miss reporting systems are critical components for occupational hazard surveillance.
Keywords: ACCIDENT & EMERGENCY MEDICINE, OCCUPATIONAL & INDUSTRIAL MEDICINE, PUBLIC HEALTH
Strengths and limitations of this study.
Owing to the voluntary nature of reports submitted to the National Fire Fighter Near-Miss Reporting System (NFFNMRS), the data are considered a convenience sample.
As the system is voluntary, we assume that near-miss events are significantly under-reported.
Assaults and motor vehicle crashes were most commonly reported. We do not know how biased the reporting of certain types of events may be. For example, overexertion is a very common cause of EMS injury, however, near-miss overexertion may not be common enough for an EMS responder to consider reporting.
This is the only system of its kind for the fire service. Even with its limitations, the near-miss reports provided a unique and deeper perspective of the multiple hazards faced by EMS responders.
A strength of our study was its use of mixed methods to extract critical information on EMS work hazards. Quantitatively coding and tabulating narratives for injury cause and nature, coupled with thematic analysis of narratives for hazards important to EMS work, provides greater depth of what EMS workers report to near-miss systems about their work hazards.
Introduction
Emergency Medical Services (EMS) responders in the USA are a critical part of our healthcare system, providing prehospital care to approximately 22 million patients every year.1 According to the 2011 National EMS Assessment, there are an estimated 826 000 licensed and credentialed EMS responders in the USA. They include emergency medical technicians (EMT), EMS responders, paramedics and other workers who perform in an EMS capacity. Common workplace risks encountered by EMS responders include: hazardous environments and extreme temperatures; motor vehicle accidents (MVA) en route to or from a scene; contact with hazardous and infectious materials; assaults; lengthy and erratic work hours; and extreme physical and psychological stressors.2 3 Exposure to such hazards can lead to fatal and non-fatal injuries or illnesses for EMS responders.
According to the National Fire Protection Association's Fire Loss in the US During 2012 report, fire departments responded to 27 705 500 emergency medical calls, a 28% increase from the previous year.4 This increase in medical service calls reflects the changing work of the US Fire and Rescue service and, therefore, warrants a deeper inspection regarding the hazards associated with this growing responsibility.
Currently, there is no standard system that captures all EMS responders’ illnesses and injuries. However, in 2012, the occupational supplement to the National Electronic Injury Surveillance System (NEISS-Work) found that an estimated 24 200 EMS responders were treated in US hospital emergency departments due to occupational injuries and illnesses.5 Of these total injuries and illnesses, 34% were due to overexertion or repeated bodily motion, 22% harmful exposures (ie, potentially infectious materials), 12% contact with objects and equipment, 12% falls, 10% assaults or violent acts, and 9% transportation incidents.5
Qualitative research for occupational groups including nurses, physicians and law enforcement is substantial;6–9 however, we found very little qualitative research investigating hazards and safety concerns unique to EMS responders. Our study aimed to investigate commonly reported injury mechanisms and prevention opportunities among EMS responders who reported events to the National Fire Fighter Near-Miss Reporting System (NFFNMRS).
Methods
Data source
The study sample was obtained from the NFFNMRS, a secure and non-punitive reporting system developed by the International Association of Fire Chiefs (IAFC) and the US Department of Homeland Security. Reports were submitted by members of the fire and rescue community to relay details of a near-miss event. Owing to the voluntary nature of the system, the analyses contained here must be considered as conducted on a convenience sample. There is nothing in the design of the reporting system that would make reports submitted to it representative of, or generalisable to, the entire US fire or EMS services. As the system is voluntary, we assume that near-miss events are grossly under-reported. However, it is the only system of its kind specific to the fire service. There is a new EMS-specific reporting system, the EMS Voluntary Event Notification Tool (E.V.E.N.T.), but its analytical utility is limited at this point in time due to the small number of annual reports (n=11 in 2014).
Even with these limitations, the NFFNMRS reports provided a unique and deeper perspective of the multiple hazards faced by EMS workers.
A near-miss event is defined by NFFNMRS as ‘an unintentional, unsafe occurrence that could have resulted in an injury, fatality, or property damage.’10 The reports to the NFFNMRS system include both near-misses and injuries (an event resulting in harm to the responder). Each report collects 16 quantitative variables about the reporter and the event, and 2 narrative fields describing the event and the lessons learned. The narrative fields were used in this study to gain a rich understanding of the circumstances surrounding near-miss events and injuries among EMS responders during emergency medical calls.
Case inclusion
One of the quantitative variables in the NFFNMRS allows reporters to select an ‘Event Type’, such as ‘fire emergency event’ or ‘non-fire emergency event’. Between 2005 and 2012, we found that 769 ‘non-fire emergency events’ were reported. ‘Non-fire emergency events’ include events such as auto extrications, technical rescues, service calls, and emergency medical calls. We were interested in EMS responders’ hazards during emergency medical activities, so our subsequent analysis focused on this category only. For the purposes of this study, EMS responders on an emergency medical call were defined as Basic Life Support (BLS) or Advanced Life Support (ALS) EMTs, or Paramedics. This included firefighters who are cross-trained to provide patient care during emergency medical calls.
Figure 1 describes the decision process for case inclusion of emergency medical calls. Inclusion criteria for an emergency medical call event were (1) sufficient information to conclude the patient was provided care by a first responder (eg, self-identification as an EMS responder) and (2) sufficient information to conclude that the near-miss event or injury is occurring during an EMS activity (eg, puncture from a needle used on a patient, or an encounter with an armed patient in an ambulance). If a report was determined not to be an emergency medical call, it was assigned an alternative event type and not included in our subsequent analysis.
Figure 1.
Case inclusion diagram (EMS, Emergency Medical Services).
Coding structure and method
The reports categorised as emergency medical calls were first assigned a Mechanism of Near-Miss or Injury (cause) and Nature of Injury (diagnosis) designation based on the International Classification of Disease 9 Clinical Modification Manual (ICD-9-CM). For example, if a responder reported that their arm was struck and fractured by a civilian vehicle, then that narrative was assigned a Mechanism of Injury code of ‘Struck-by Motor Vehicle’, with a Nature of Injury code of ‘Fracture’.
The coding structures (table 1) were informed by previous research that used the NFFNMRS data to analyse reports in the ‘fire emergency events’ category.11 This study identified that non-burn injuries sustained by firefighters during a fire would be coded to Conflagration (fire) using the ICD-9-CM code (ie, E890-E899) due to the hierarchical nature of the coding structure. However, this masked specific hazards (and injuries) that occur during fires, such as electrocutions, falls, smoke inhalation etc. By creating subcategories within the overarching Conflagration category, specific hazards were better identified and recorded, and injury/near-miss causal pathways were outlined. The resultant coding structure extracted more detail from each narrative while honouring the ICD-9-CM hierarchy by retaining the overall cause category as Conflagration (Fire). Similarly in our study, the injury designation structure and qualitative coding structures utilised this approach of creating subcategories within overarching categories to reflect emerging themes in the narrative text.
Table 1.
Quantitative and qualitative coding structures
| Quantitative coding categories | Qualitative coding categories |
|---|---|
| Non-fire emergency event type | Policies, procedures, practices |
| Emergency medical call | Staging policies |
| Technical rescue | Roadway shutdown policies |
| Service call | Vehicle safety policies |
| Motor vehicle accident, auto extrication | Relationships between emergency responders |
| Other | Staffing |
| Mechanism of injury | Feelings |
| Assault | Recovery from work |
| Struck by motor vehicle | Resources |
| Motor vehicle collision | Equipment |
| Firearm | Training |
| Cutting/piercing instruments or objects | PPE (personal protective equipment) |
| Struck by object | Hazards |
| Electric current | Vehicles |
| Poisoning | Assaults |
| Bodily fluid exposure | Biological, chemical |
| Fall | Weather |
| Overexertion | Electrical |
| Natural/environmental | |
| Caught in-between | |
| Air transport | |
| Bite | |
| Burn | |
| Foreign body | |
| Motor vehicle rollover | |
| Machinery/equipment | |
| Nature of injury | |
| Infectious disease | |
| Strain/sprain | |
| Crushing | |
| Fracture | |
| Puncture/laceration | |
| Contusion | |
| Burn | |
| Dislocation | |
| Open wound | |
| Other |
After injury designations were assigned, narratives were then qualitatively coded in batches of 50–100 narratives using NVivo qualitative data analysis software (QSR International Pty Ltd V.10, 2012). Each batch was independently coded by two researchers (BB and RP), then reconciled and merged; the entire research team then resolved existing discrepancies in injury designations, and updated the qualitative coding structure when necessary. This ensured that all emergency medical calls were appropriately included in the analysis project and were coded with consensus. No new themes (referred to as nodes during the coding process) emerged after approximately 200 of the 769 narratives. As a result, the qualitative coding structure was finalised by the researchers and used for the remainder of the coding process.
Results
Quantitative findings
Of the 769 ‘non-fire emergency’ event reports obtained from the NFFNMRS between 2005 and 2012, 24.1% (n=185) were identified as emergency medical calls. Among these reports, the most commonly identified Mechanisms of Near-Miss or Injury were (1) Assault, (2) Struck by Motor Vehicle, and (3) Motor Vehicle Collision (table 2). In the event that an assault was identified, a secondary mechanism was also coded for the type of assault. The most commonly identified instrument was firearm.
Table 2.
Frequency of mechanism of near-miss or injury among EMS responders voluntarily reporting to the NFFNMRS
| Mechanism of near-miss or injury | n (%) |
|---|---|
| Assault* | 48 (25.7) |
| Firearm | 22 |
| Cutting, piercing instruments, objects | 14 |
| Struck by person | 12 |
| Bite | 1 |
| MV EMT, paramedic struck by | 1 |
| Struck by Motor Vehicle | 40 (21.4) |
| MV collision | 31 (16.6) |
| Electric current | 13 (6.9) |
| Poisoning | 12 (6.4) |
| Bodily fluid exposure | 7 (3.7) |
| Fall | 6 (3.2) |
| Firearm | 4 (2.1) |
| Cutting, piercing instruments, objects | 6 (3.2) |
| Struck by | 5 (2.7) |
| Overexertion | 5 (2.7) |
| Natural, environmental | 4 (2.1) |
| Caught in-between | 2 (1.1) |
| Air transport | 1 (0.5) |
| Burn | 1 (0.5) |
| Foreign body | 1 (0.5) |
| MV rollover | 1 (0.5) |
| Total† | 187 |
*A secondary mechanism for type of assault was identified for all narratives with an identified near-miss or injury from assault. One narrative was not assigned a secondary mechanism because the type of near-miss assault was unclear. Three narratives were assigned more than one secondary mechanism for assault.
†Total frequency of mechanism will be greater than n=185 because some narratives were coded with more than one mechanism of near-miss or injury.
EMS, Emergency Medical Services; EMT, emergency medical technicians; MV, motor vehicle; NFFNMRS, National Fire Fighter Near-Miss Reporting System
Twenty-seven of the reports described injury to EMS responders and were coded with a Nature of Injury. The most commonly identified Nature of Injury was infectious disease, or the potential for infectious disease.
Qualitative findings
After text from each narrative was coded into the nine individual nodes (table 1), we used the inductive approach common in grounded theory to explore new or unexpected issues within the data. After text from each narrative was coded into individual nodes, overarching themes were identified. For example, a narrative describing a policy on staging a fire apparatus to protect EMS responders from civilian drivers during an emergency medical call at an MVA would be coded to both the ‘Policies, Procedures and Practices’ node and the ‘Vehicles’ node. Two nodes representing significant EMS responder hazards (Assaults by Patients, Risks from Motor Vehicles), and three nodes reflective of the lessons learned from events are further explored because of their importance in prevention planning in the injury risks of EMS responders (Personal Protective Equipment (PPE); Relationships between Emergency Responders; and Policies, Procedures and Practices).
Assaults by patients
Assault, or risk of assault by a weapon, was a pervasive issue identified in our study sample. Assault weapons ranged from firearms to kitchen knives. One responder reported that when dispatched to a diabetic call, EMS responders were at risk of assault by a patient who grabbed a loaded pistol from a desk nearby (10-0000837).i During a call from a man with difficulty breathing, police and EMS found a combative patient who pulled out a knife and almost stabbed an EMS responder (10-0000667).
EMS responders may not anticipate any danger or threat to themselves while responding to an emergency medical call, as exemplified by one reporter: “We had probably spent an hour and a half with this patient and had no idea he was armed” (07-0001019). Regardless of whether or not an EMS responder anticipates danger, it can appear instantaneously. One responder reported: “Standing in front of the door, I knocked and found almost instantaneously the door being opened with a gentlemen pointing a shotgun at us” (05-0000202). Another responder described a situation in an ambulance in which the ‘patient was calmed’, but later “grabbed the [Officer in Charge]'s neck and started choking her, and immediately placed the [3-inch] blade to her neck” (05-0000267).
In some situations, the assault, or risk of assault, was from a violent patient (08-0000358, 10-0000312, 10-0000667, 10-0000837). Examples included being punched in the face by patients (06-0000291, 10-0000810), and being bitten by a patient while providing care (08-0000358). Responders also reported working with patients who are under the influence of alcohol and drugs (07-0001019) and were found to be carrying weapons (10-0001263).
EMS responders reported the need for police presence when providing patient care to volatile patients: “Patients who are violent or unsettled should be restrained with police assistance and transported under police escort” (05-0000267). In another instance, police had to use mace to control a patient and escort him to the hospital (10-0000667).
EMS responders who recognised their susceptibility of being assaulted by patients, family members or bystanders suggested improved training as one way to address the problem. This was demonstrated by a responder who commented:
If family members observe help arrive but not take any action while awaiting law enforcement, it multiplies the stress level of all involved and can lead to potentially violent confrontations. Obviously, this issue needs more emphasis in training. (07-0000815)
Another EMS responder, concerned about the risk of firearms, expressed the need for training on “how to apply the safety on firearm…[since they] don’t always have the luxury of the police being the only responders to handle weapons” (10-0001236).
Risks from motor vehicles
Motor vehicles emerged as a salient injury hazard for EMS responders. The hazards most commonly associated with motor vehicles included failure to secure vehicles, crashes between vehicles, and medics being swiped by passing cars on highway incidents.
Respondents described hazards from failing to secure passenger or department vehicles from unintentionally moving. When responding to a motor vehicle crash, and prior to extricating victims from the vehicle, it is standard operating procedure for responders to lock the parking brake on the vehicle in order to be sure that the vehicle does not roll while they are extricating or treating the patient. However, there were numerous reports highlighting the irregularity of adherence to such a procedure:
I approached the female and as I began to assess her, I saw that the car was still in gear and the ignition was still in the on position. I told the FF of the problem, shut off the car, and removed the key. No injuries. I used this as a teachable moment, told the FF the concerns, and to always check to see that the car is in park and off, as the car may start to roll and cause injury to the FF or other personnel at the scene. (ID0071)
One of my firefighters was in the car trying to get information from the patient. When the medic arrived, my firefighter got out to let the medic into the car. The patient was high, very high on something…About the time the medic got in the car to talk with the patient, the patient jammed the accelerator and the car lurched forward about 10 feet. I forgot to check and make sure the car was off and in park. I couldn't hear it, feel it, or anything. This reasoning in hindsight is complete bull. Complacency had snuck up on me. Always secure the vehicle and stabilize it. (ID0280)
The risk of a motor vehicle crash going to or from an event was reported frequently throughout the entries. The hazard was experienced at two levels: from the public and from fellow workers.
Public
A large sized SUV pulled out of the post office and hit the patient area of our Type III ambulance. At this time the ALS unit directly behind us hit our rear causing a secondary accident. The other EMT, the Paramedic on board, and I were thrown around the back. All three of us were unbuckled due to the fact we were in the process of CPR, suctioning, and preparing the AED. All of our equipment was then thrown into scrambles. The Medic's diagnostic machine was thrown into the front driving compartment where it broke through the front windshield and then smashed onto the pavement, a $15 000 loss. The patient did not sustain any further injury from this event but all 3 EMTs, both Medics, and the driver of the SUV were hurt. (ID0148)
Worker-to-worker
[I was in a fire truck] traveling south on State Hwy, [another] medic unit was traveling west. At an intersection, [medic unit] almost pulled in front of the big red truck. Big red truck had green light and right of way. Medic unit had to suddenly stop to avoid collision. Both responding to medical emergency…Never trust other emergency vehicles responding. (ID0035)
Respondents reported both the public and fellow first responders putting them at risk of being struck by a moving vehicle when working outside of their apparatus or rig:
Public
The weather was clear and dry and drivers coming toward the scene were looking into the rising sun. The apparatus still had emergency lights on and all occupants were out of it, providing patient care. A police car had been parked behind the fire truck, but had cleared for another call….There was a loud crash behind the apparatus. A passenger car struck a glancing blow to the truck on the driver's side before coming to a stop next to the truck. The occupant appeared to be on his cell phone as the car stopped. Had the truck not been parked where it was the car would've struck all three crew members who were working in front of the apparatus. (ID0275)
Worker-to-worker
I was the driver/operator of an engine on a medical call with a four person crew. I stopped to drop off three crew members with medical equipment. The medic dropped a piece of equipment that went about midway under the engine. There was no lighting to see the crew. I paused and assumed the crew was on the way in. I drove off to turn the engine around to face it outbound. The medic picked up the equipment prior to the engine pulling away. Without me pausing prior to pulling away, this could have been life threatening. (ID0451)
Personal protective equipment
EMS responders frequently discussed the importance of PPE to protect them from hazards they faced while providing patient care. Failure to wear PPE exposed EMS responders to preventable blood-borne pathogens, as reported in one narrative in which an “EMT looked over the [patient’s] wrist and the blood squirted up into the EMT's eye” (05-0000247). Failure to wear latex gloves placed another EMS responder at risk after the patient's blood got into the EMS responder's cut (10-0000365). Owing to frequent contact with bodily fluids, EMS responders repeatedly expressed the significant role of PPE to reduce their risk of contracting infectious diseases (06-0000371, 10-0001203, 11-0000199 and 11-0000314). This perception on the importance of PPE was emphasised when one EMS responder encouraged that masks and gowns be worn during emergency medical calls with high exposure risk (10-0000404).
Lack of other types of PPE, such as nighttime reflective clothing, traffic vests, and bulletproof vests were also mentioned as barriers to safety. EMS responders who provided care on the side of highways or roads reported the need for traffic vests to be more visible to passing vehicles (06-0000621, 07-0000822, 09-0000031, 09-0000419, and 11-0000087). An EMS responder who was struck by a vehicle stated that his “accident could have been avoided if [he] had been provided with the proper nighttime reflective clothing” (06-0000369). Additionally, ballistic or bulletproof vests were reported as useful PPE to avoid injury from violent encounters by EMS responders concerned about being assaulted by weapons (07-0000989and 10-0000435).
Relationships with emergency responders
EMS responders reported a variety of positive and negative relationships when working with other emergency responders. The positive relationships described by many EMS responders suggest the importance of teamwork among those in the profession. In particular, when dealing with patients who became violent, often due to the influence of alcohol and drugs, police assistance mitigated assaults to EMS responders. One report of a BLS responder call described that “there was never any violence acted out on my crew that night. I can't be sure if the outcome would have been the same had the police not arrived when they did” (08-0000651). Another report offered insight into the humility of a police officer who apologised to the EMS responders for missing a razor blade on a patient while checking her for weapons (07-0000808), a mistake similar to those reported in other emergency medical call events (09-0000602, 09-0000739, 09-0000784, 10-0001233).
However, EMS responders also reported that other emergency responders disregarded their safety on scene. One EMS responder shared a negative experience about his interaction with a firefighter: “He made a flippant remark that he was a firefighter and was more than capable of driving ‘just an ambulance’” (06-0000219). Another report offered a similar sentiment that better communication among the Charge EMT, Engine Officer and reporting responder could have prevented the reporting responder's injury altogether (05-0000493).
In one instance, police and firefighter personnel prematurely left the scene of an MVA, “leaving the EMS crew in the dark on the highway without any scene protection” (05-0000595). This is particularly concerning because of the potential for injury risk to EMS responders during MVA incidents. One reporter commented on the change in culture within the service: “…years ago, State Troopers would criticize the fire service for such physical scene protection, calling it ‘overkill.’ Clearly, that is no longer the case hereabouts” (06-0000470).
Policies, procedures and practices
Numerous policies, procedures and practices were reported by EMS responders as both helpful and harmful to their safety while providing patient care.
Staging policies
Staging, the placement of EMS responders as they await next steps on how to proceed from the Incident Commander, was cited as a beneficial practice in a number of situations. For example, staging was cited as useful for violent situations such as active shooter situations (07-0000808), and valuable for MVAs involving power lines. One responder recalled an event where “all responders were moved from the immediate scene to a safe staging area until the utility company could turn off all the power” (07-0000746). EMS responders expressed that the practice of waiting for scenes to become safe before starting medical care was advantageous to avoid injuries (08-0000358 and 11-0000416).
Roadway shutdown policies
Unsafe road conditions caused by civilians were often reported: “The civilian drivers were not the least bit concerned with us” (05-0000155) and, “The trucks did not slow down or change lanes even though all of our emergency lights were activated” (10-0000286). These responses are emblematic of the hazards faced by EMS responders when working along roadways. Many EMS responders recommended implementing policies that would enforce state emergency scene vehicles to shut down lanes and use large apparatuses on highways and roads to protect personnel, especially from civilian drivers (05-0000356, 06-0000470, 07-0000634, 07-0000809, 07-0001002, 08-0000063, 08-0000376, 09-0000419, 09-0000944, 10-0000087, 10-0000195 and 10-0000853).
Vehicle safety policies
EMS responders explained the importance of safe vehicle practices and policies while en route to medical calls and while on the scene. Defensive driving practices and training were attributed to avoiding MVAs and remaining safe on the roads. “Due to our training on intersections and policies and procedures on seatbelt use, we had avoided a potentially deadly outcome for that driver and maybe us” (07-0001047). Another EMS responder reflected on his near-miss event, and emphasised: “If you ever have the opportunity to wear your seatbelt in the patient compartment, it will save your life” (11-0000295).
Discussion
Using data from the NFFNMRS provided a unique opportunity to investigate new and persistent hazards that EMS responders encounter in their work environments. Gallagher and Kupas12 emphasised the importance of an anonymous EMS-self reporting system to allow early recognition of safety issues that impact the safety of firefighters and EMTs. Our study further supports the use of narrative data in occupational injury prevention—the importance of which has previously been encouraged because of the level of detail that it can provide beyond quantitative data.13
In our study, assaults against EMS responders by patients was the most frequently identified mechanism of near-miss or injury. EMS responders reported being threatened or assaulted by patients, family members, and bystanders. We identified multiple social and environmental factors contributing to assaults against EMS responders. A greater awareness of, and improved training on, violent EMS encounters can be incorporated into existing EMS protocols to prevent injuries to EMS responders.
Our results are consistent with the findings that violence against EMS responders is a prevalent and serious issue.2 14–16 EMS responders reporting to the NFFNMRS suggested training to diffuse tense situations with patients/family members as a way to reduce the risk of an assault. Curbside Manner: Stress First Aid for the Street, a programme initiated by the National Fallen Firefighters Foundation teaches EMS responders and firefighters how to provide patients with compassionate, effective care during distressing situations.17 This approach offers ways to help patients and families cope with the stress of a medical event, while also teaching techniques for de-escalating tense situations; this programme helps to ensure EMS responders and patients are safe during EMS interactions. An additional resource is a free online training and education course available on the Center for Disease Control and Prevention website that is used to train healthcare workers on how to handle a violent patient.18 The EMS community has also developed an industry-specific training that emphasises de-escalation over self-defense or weapons (http://www.dt4ems.org).19
Struck-by Motor Vehicle and Motor Vehicle Collision were the second and third most frequently identified mechanisms of near-miss or injury during medical calls. This finding aligns with recent research on non-fatal occupational injuries among EMTs that found that vehicles accounted for 34.2 injuries per 10 000 full-time EMTs for cases resulting in lost work days, and that highway vehicles accounted for 20% of fatal occupational injuries among EMTs in the USA from 2003 to 2007.15 EMS responders in our study expressed the need for more training on road and highway safety. Currently, there are existing initiatives to reduce the number of injuries and fatalities EMS responders sustain while working on roads and highways. The Division of Occupational Health, Safety and Medicine of the International Association of Fire Fighters (IAFF) in collaboration with the US Department of Homeland Security has developed Improving Apparatus Response and Roadway Operations Safety in the Career Fire Service, a programme which aims to improve the safety of emergency responders during vehicle and roadway incident operations.20 The programme teaches emergency responders how to apply basic strategies to safeguard their safety en route to a medical scene, while operating on roadways, as well as departing a scene.
Limitations to our study should be noted. Owing to the voluntary nature of the reporting system, responders who completed a report may not be representative of all EMS responders. While the system accepts reports from everyone, reports are most likely from fire-based EMS agencies. Training and outreach regarding the system was carried out by members of the fire service and given to fire departments specifically. Independent EMS providers may not be aware of the system and, therefore, may not report to it. Additionally, because many firefighters are cross-trained to serve in the capacity of an emergency medical provider, this level of distinction is not easily captured on the quantitative portion of the NFFNMRS form. It was only through the analysis of narrative text that we were able to determine the capacity in which respondents were working (EMS vs a fire). This important distinction allowed us to further evaluate the particular hazards faced by EMS responders specifically. However, the narrative fields on the NFFNMRS reporting form ‘Describe the event’ and ‘Lessons learned’ are so broad that they limit the depth of information regarding occupational near-miss events and injuries specific to EMS responders on an emergency medical call. These limitations reflect the fact that the reporting system was not developed for research purposes. Had it been anticipated that data coming in would be analysed to look at work-related hazards, a more rigorous data system might have been created.21
A strength of our study was its use of mixed methods to extract critical information on EMS work hazards. Quantitatively coding and tabulating narratives for injury cause and nature, coupled with thematic analysis of narratives for hazards important to EMS work, provides greater depth to our understanding of EMS work. Narrative text review enabled the ability to capture emergency medical calls reported by any type of EMS responder, such as a cross-trained firefighter (eg, firefighter using an AED for patient cardiac resuscitation).
Conclusion
Our study finds that the NFFNMRS captures real-life events that the fire and emergency services can use to make practice and policy recommendations to increase EMS responders’ safety during emergency medical calls. Near-miss systems allow EMS responders to anonymously share their lessons learned, and by doing so, educate fellow EMS responders. We identified numerous emergency medical calls that included recommendations for policies, procedures, and practices. For example, as reported in our sample of medical calls, stricter policies regarding highway lane closures during MVAs could minimise the risk of vehicle-related injuries to EMS responders providing patient care on-scene.
Fire departments also benefit from this study, as many firefighters are cross-trained in EMS and could incorporate safer practices and procedures to reduce the number of occupational injuries and illnesses among EMS responders. We encourage fire and rescue service investigators to incorporate narrative data into their research. The narrative data add extensive insight into the concerning issue of patient assault to EMS providers, as well as contributing factors surrounding struck by motor vehicle and motor vehicle collisions. The NFFNMRS serves as a primary source for accounts of near-miss events and injuries within the fire and rescue service, and is recommended for further use by researchers interested in first responder injury prevention.
Acknowledgments
The authors wish to recognise the important work that the International Association of Fire Chiefs (IAFC) is doing to support and maintain the National Fire Fighter Near-Miss Reporting System. They also thank the anonymous EMS responders who voluntarily reported their events and lessons learned to the system so that others would benefit. Lastly, the authors thank Leslie Frey, JD, MPH for her editorial assistance.
Footnotes
Contributors: JAT, AVL and ALD were responsible for the study design. BB and RP coded the narratives using NVivo V.10 qualitative analysis software. BB and RP coded the narratives into Nature and Cause of Injury categories using the rubric developed by AVL and JAT. All the authors contributed to the data analysis and preparation of the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: From 2007-2012, JAT was a contractual consultant epidemiologist to the IAFC.
Ethics approval: This study was approved by the Drexel University Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data from the National Fire Fighter Near-Miss Reporting System are the property of the International Association of Fire Chiefs. To acquire these data, please contact the IAFC.
The reader is directed to the National Fire Fighter Near-Miss Reporting System (http://www.nationalnearmiss.org/) to access the full reports using the Report Numbers referenced in this study. Readers can enter the Report Number into the Google search box field to access the applicable narrative.
References
- 1.Maguire BJ, Walz BJ. Current emergency medical services workforce issues in the United States. J Emerg Manag 2004;2:17–26. [Google Scholar]
- 2.Reichard AA, Jackson LJ. Occupational injuries among emergency responders. Am J Ind Med 2010;53:1–11. 10.1002/ajim.20772 [DOI] [PubMed] [Google Scholar]
- 3.LeBlanc VR, Regehr C, Birze A et al. The association between posttraumatic stress, coping, and acute stress responses in paramedics. Traumatology 2011;17:10 10.1177/1534765611429078 [DOI] [Google Scholar]
- 4.Karter M. Fire loss in the United States during 2012. NFPA, 2013. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Emergency Medical Services Workers: Injury and Illness Data, 2012. http://www.cdc.gov/niosh/topics/ems/data2012.html
- 6.Geiger-Brown J, Trinkoff AM, Nielsen K et al. Nurses’ perception of their work environment, health, and well-being: a qualitative perspective. AAOHN J 2004;52:16–22. [PubMed] [Google Scholar]
- 7.Kingston MJ, Evans SM, Smith BJ, and, et al. Attitudes of doctors and nurses towards incident reporting: a qualitative analysis. Med J Aust 2004;181:36–9. [DOI] [PubMed] [Google Scholar]
- 8.Toch H. Stress in policing. American Psychological Association, 2002. [Google Scholar]
- 9.Kindy D, Petersen S, Parkhurst D. Perilous work: nurses’ experiences in psychiatric units with high risks of assault. Arch Psychiatr Nurs 2005;19:169–75. 10.1016/j.apnu.2005.05.002 [DOI] [PubMed] [Google Scholar]
- 10.International Association of Fire Chiefs. The National Fire Fighter Near-Miss Reporting System. http://www.firefighternearmiss.com
- 11.Taylor JA, Lacovara AV, Smith GS et al. Near-miss narratives from the fire service: a Bayesian analysis. Accid Anal Prev 2014;62:119–29. 10.1016/j.aap.2013.09.012 [DOI] [PubMed] [Google Scholar]
- 12.Gallagher JM, Kupas DF. Experience with an anonymous web-based state ems safety incident reporting system. Prehosp Emerg Care 2012;16:36–42. 10.3109/10903127.2011.626105 [DOI] [PubMed] [Google Scholar]
- 13.Stout N. Analysis of narrative text fields in occupational injury data. In: Feyer A-M, Williamson A, eds. Occupational injury. Risk, prevention and intervention. CRC Press, 1998:15.–. [Google Scholar]
- 14.Mechem CC, Dickinson ET, Shofer FS et al. Injuries from assaults on paramedics and firefighters in an urban emergency medical services system. Prehosp Emerg Care 2002;6:396–401. 10.1080/10903120290938012 [DOI] [PubMed] [Google Scholar]
- 15.Maguire BJ, Smith S. Injuries and fatalities among emergency medical technicians and paramedics in the United States. Prehosp Disaster Med 2013;28:376–82. 10.1017/S1049023X13003555 [DOI] [PubMed] [Google Scholar]
- 16.Heick R, Young T, Peek-Asa C. Occupational injuries among emergency medical service providers in the United States. J Occup Environ Med 2009;51:963–8. 10.1097/JOM.0b013e3181af6b76 [DOI] [PubMed] [Google Scholar]
- 17.National Fall Firefighters Foundation. Curbside Manner: Stress First Aid for the Street. http://flsi13.everyonegoeshome.com/curbside-manner.html
- 18.Centers for Disease Control and Prevention [CDC]. Workplace Safety & Health Topics: Occupational violence. (2013). http://www.cdc.gov/niosh/topics/violence/training_nurses.html
- 19. Defensive Tactics for Escaping, Mitigating, and Surviving. Escaping Violent Encounters for EMS and Fire. http://www.dt4ems.org.
- 20.International Association of Fire Fighters (IAFF). Improving Apparatus Response and Roadway Operations Safety in the Career Fire Service. http://www.iaff.org/hs/evsp/home.html
- 21.Taylor JA, Lacovara AV. From infancy to adolescence: the development and future of the National Fire Fighter Near-Miss Reporting System. New Solut 2015;24: 555–76. 10.2190/NS.24.4.h [DOI] [PubMed] [Google Scholar]