Abstract
Porokeratosis is characterized clinically by annular plaques with a distinct peripheral keratotic ridge and histologically by the cornoid lamella. Porokeratosis with follicular involvement is rarely reported. To provide the basis of that follicular porokeratosis is a clinical variant or not. Biopsy was taken from three patients who were diagnosed porokeratosis. Routine stain was made and reviewed the literatures about well-documented cases of porokeratosis with follicular involvement. Porokeratosis with follicular involvement may have some clinical features: asymptomatic, erythematous, brownish or skin-color, less than 1 cm in the areas excluding palm and plantar, which commonly involved on middle-age. But there have still not enough proof as an independent clinical variant.
Keywords: Porokeratosis, follicular involvement, dermatopathology
Introduction
Porokeratosis, a genodermatosis with disorder of keratinization, is characterized clinically by annular plaques with a distinct peripheral keratotic ridge and histologically by the cornoid lamella [1]. The lesions have a predilection for the limbs and trunk, but face, natal cleft, genitocrural and perianal regions, and scrotum are rarely involved [2]. Porokeratosis of Mibelli was the first described type, and since then at least five clinical types have been described [1]. A new clinical variant follicular porokeratosis has been noticed [2]. We present three cases of porokeratosis on the rare areas with follicular involvement.
Case report
Case 1
A 35-year-old man presented with brownish papules on the perianal area for 1 year accompanied with itchiness for 1 month. The patient noted that the lesions had been present since last year but they were asymptomatic. He was otherwise healthy with no known history of other diseases and drug allergy. There were no similar lesions noted in the other family members.
Physical examination showed there were multiple sporadically distributed 1-5mm in diameter sized brownish papules along the gluteal folds sparing the anus (Figure 1A). No other skin lesions were found in the genitogluteal region or elsewhere. A provisional clinical diagnosis of Bowenoid papulosis was made. One of the papules was biopsied.
Figure 1.
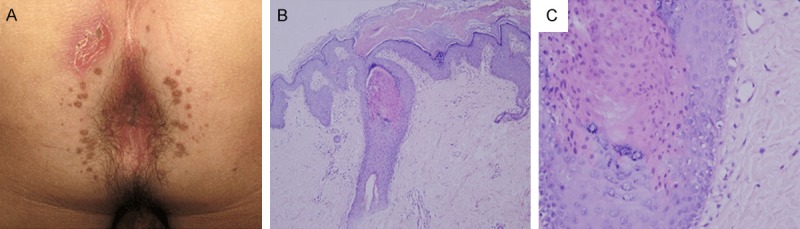
A. Multiple, sporadic, brownish papules, 1-5 mm in diameter in size, along the gluteal folds sparing the anus. B. On the histopathological examination one of the papules , one cornoid lamella, a thin column of parakeratotic cells with an absent underlying granular zone and dyskeratotic cells in the spinous layer, involved in the hair follicle (HE, original magnification ×100). C. The parakeratotic column with absence of underlying granular layer was observed (HE, original magnification ×400).
Histopathological examination showed cornoid lamella, a thin column of parakeratotic cells with an absent underlying granular zone and dyskeratotic cells in the spinous layer, and no epidermal atypia and loss of architecture. Multiple serial sections revealed one cornoid lamella involving the follicular infundibulum (Figure 1B, 1C). These findings suggested a diagnosis of follicular porokeratosis.
Case 2
A 50-year-old man presented with multiple asymptomatic erythematous plaques on the upper back and occipitonuchal area for 30 years. At the very early years the lesions became more and larger slowly with mild itchy occasionally. However, the lesions did not increase in size and number obviously for many years. He was otherwise healthy with no known history of other diseases and drug allergy. There were no similar lesions noted in the other family members.
Physical examination showed multiple asymptomatic erythematous plaques with a peripheral elevated keratotic ridge on the upper back and occipitonuchal area (Figure 2A). No other skin lesions were found on the other areas.
Figure 2.
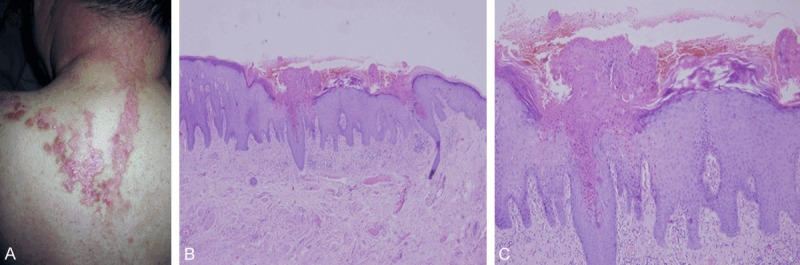
A. Multiple asymptomatic erythematous plaques with a peripheral grooved keratotic ridge on the upper back and occipitonuchal area. B. On the histopathological examination of case 2, two cornoid lamella, one of them involved in the hair follicle (HE, original magnification ×40). C. A close view of the cornoid lamella involvement in follicular infundibulum (HE, original magnification ×100).
Histopathological examination showed the similarity with the case 1. Cornoid lamella involved in the hair follicle was found (Figure 2B, 2C). The typical histopathology suggested the diagnosis of porokeratosis involvement in hair follicle.
Case 3
A 76-year-old man presented with multiple disseminated small elevated black-brown colored keratotic eruptions on the face and both upper limbs for more than 3 years. He was otherwise healthy with no known history of other diseases and drug allergy. There were no similar lesions noted in the other family members.
Physical examination revealed multiple disseminated small black-brown colored keratotic eruptions with elevated borders on the face and both upper limbs (Figure 3A). No other skin lesions were found on the trunk or elsewhere.
Figure 3.
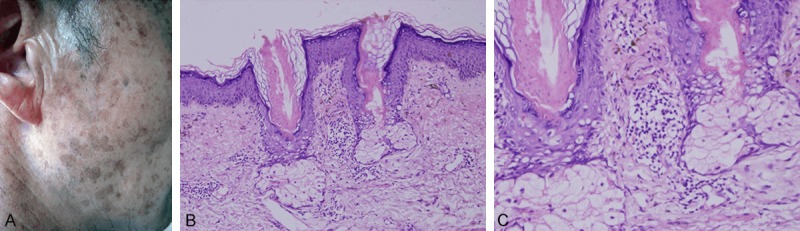
A. multiple disseminated small elevated black-brown keratotic eruptions on the face. B. On the histopathological examination of case 3, three cornoid lamella, all of them involved in the hair follicles (HE, original magnification ×200). C. A close view of the cornoid lamella involvement in the hair follicles (HE, original magnification ×400).
Histopathological examination showed that cornoid lamella exclusively involved in the hair follicle (Figure 3B, 3C). The typical histopathology suggested the diagnosis of porokeratosis involvement in hair follicle.
Discussion
To date, there have been 15 well-documented cases of porokeratosis with follicular involvement in the literature including our three cases [3-12]. The clinical and histopathological features of these 15 cases were summarized and analyzed.
The age and gender of all the patients were summarized as shown in Table 1. The ratio of female to male was almost 2:3. The peak age of the cases was 20 to 60 years old. The youngest patient was 19 years old, while the oldest was 85 years old.
Table 1.
Age and gender of the patients
| Age (years) | Female | Male | Total |
|---|---|---|---|
| < 20 | 0 | 1 | 1 |
| 20~40 | 4 | 2 | 6 |
| 40~60 | 2 | 3 | 5 |
| > 60 | 0 | 3 | 3 |
| Total | 6 | 9 | 15 |
Only one case had definite family history [3], which the similar lesions occurred on her mother, brother and daughter. However, 14 patients were labeled with “no” or “no-noted”.
Most patients presented with asymptomatic lesions (11 of 15). Three patients and our first patient complained of itchiness [4,5,11].
Based on the literatures, 10 cases had definitely noted the size. The size of the lesions varied from 0.2 cm to a half-palm size, but the majority was less than 1cm in diameter (6/10). The color of the lesions was erythematous (8/15), brownish (4/15), and skin-colored (3/15). Sun-exposed areas were the major location of the lesions. 10 and 4 cases out of 15 were found on the sun-exposed and non-exposed locations respectively. Besides, the lesions were located on both the sun-exposed and non-exposed areas in only one case [6].
There were 15 cases were classified by the classical subtypes of porokeratosis (Table 2). To date, porokeratosis punctata palmaris et plantaris had not been reported with involvement in the follicle. The lesions were found predominantly in porokeratosis of Mibelli and disseminated superficial actinic porokeratosis (10 of 15) and 8 of them involved exclusively in the follicle. The ratio of exclusive and included follicular involvement was almost 2:1.
Table 2.
Summary of clinical diagnosis and histopathology with follicular involvement by porokeratosis
| Histopathology | PM | DSAP | Linear Porokeratosis | Localized Porokeratosis | SDP | Total |
|---|---|---|---|---|---|---|
| Exclusive hair follicle | 5 | 3 | 1 | 1 | 0 | 10 |
| Included hair follicle | 1 | 1 | 0 | 1 | 2 | 5 |
| Total | 6 | 4 | 1 | 2 | 2 | 15 |
PM: Porokeratosis of Mibelli; DSAP: Disseminated superficial actinic porokeratosis; SDP: Superficial disseminated porokeratosis.
Porokeratosis can be classified into six classical subtypes: porokeratosis of Mibelli (PM), disseminated superficial actinic porokeratosis (DSAP), superficial disseminated porokeratosis (SDP), porokeratosis punctata palmaris et plantaris, linear porokeratosis (LP), and localized porokeratosis. [1] Follicular involvement of porokeratosis is rare. To date, there have been 12 well-documented cases in the literatures. Five cases of them involve in the trunk and extremities [3-6]. Five cases are in the face [4,7-10], and the other two cases are in the gluteal area [11,12]. According to the descriptions of lesions, 12 cases can be classified as the following: 5 cases are diagnosed PM [3,4,8,9,11], 3 are DSAP [3,5,7], 2 are SDP [4,12], 1 is LP [6] and 1 is localized porokeratosis [10].
Follicular porokeratosis as a new type of porokeratosis had been proposed. It is known from the literatures that there had two ideas about the follicular porokeratosis. Most of the authors believe that the follicular porokeratosis is a rare pathological variant of porokeratosis, which is characterized by the presence of cornoid lamellae located exclusively in the follicle [7-9]. Moreover, two retrospective studies showed that cornoid lamella with follicular involvement were not coincident. A histological review of 61 cases with DSAP, [13] found involvement of typical cornoid lamella within the hair follicle and eccrine ostia in 41% (25/61 cases). And the other of 86 porokeratosis lesions from 73 patients with multiple lesions found occurrence of cornoid lamellae at the follicular infundibulum in 44% (32/73 cases) [4]. The correlation of the special histopathological presentation and clinical types is uncertain. Porokeratosis with follicular involvement may be more common than we thought. The other idea is that follicular porokeratosis have distinctive clinical and histopathological presentation. Follicular porokeratosis as a new clinical subtype of porokeratosis had been listed. 2 However, the clinical feature is not described [2]. Pongpudpunth et al. [5] reported a 41-year-old man with follicular-centered papules on the trunk and upper extremities. They favored the histopathological presentation of follicular porokeratosis. In addition, he proposed the different clinical features of multiple, small, follicle-centered lesions in either a sun-exposed or non-sun-exposed area.
In conclusion, there has a common sense that follicular porokeratosis is a pathologic variant. Porokeratosis with follicular involvement present some clinical features: asymptomatic, erythematous, brownish or skin-color, less than 1 cm in the areas excluding palm and plantar, which commonly involved on middle-age patients. But there have still not enough proof as an independent clinical variant. Moreover, it is still unclear that how to explain the reason of follicular involvement. Therefore, we believe our cases of porokeratosis involved in the follicle can enrich the knowledge of porokeratosis.
Acknowledgements
The source of finding: The National Natural Science Fund of China (No. 81172588).
Disclosure of conflict of interest
None.
References
- 1.McKee HP, Calonje E, Granter RS. Pathology of the skin, with clinical correlation. 3rd edition. China: Peking University Medical Press; 2006. Disorders of Keratinization; pp. 74–7. [Google Scholar]
- 2.Weedon D. Skin pathology. 3rd ed. Edinburgh: Churchill Livingstone; 2010. Disorders of epidermal maturation and keratinization; pp. 262–4. [Google Scholar]
- 3.de Almeida HL Jr, Guarenti IM, de Castro LA, Rocha NM. Follicular involvement in porokeratosis. J Eur Acad Dermatol Venereol. 2007;21:104. doi: 10.1111/j.1468-3083.2006.01798.x. [DOI] [PubMed] [Google Scholar]
- 4.Minami-Hori M, Ishida-Yamamoto A, Iizuka H. Cornoid lamellae associated with follicular infundibulum and acrosyringium in porokeratosis. J Dermatol. 2009;36:125–30. doi: 10.1111/j.1346-8138.2009.00610.x. [DOI] [PubMed] [Google Scholar]
- 5.Pongpudpunth M, Farber J, Mahalingham M. Follicular porokeratosis: distinct clinical entity or histologic variant? J Cutan Pathol. 2009;36:1195–9. doi: 10.1111/j.1600-0560.2009.01266.x. [DOI] [PubMed] [Google Scholar]
- 6.Vaishnani JB, Bosamiya SS, Sapariya BJ, Udhreja PR. Linear porokeratosis with follicular involvement. Indian J Dermatol. 2011;56:460–1. doi: 10.4103/0019-5154.84715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang NS, Gruson LM, Kamino H. Facial follicular porokeratosis: a case report. Am J Dermatopathol. 2010;32:720–2. doi: 10.1097/DAD.0b013e3181d18910. [DOI] [PubMed] [Google Scholar]
- 8.Rocha-Sousa VL, Costa JB, de Aquino Paulo-Filho T, Rocha KB, da Trindade-Neto PB. Follicular porokeratosis on the face. Am J Dermatopathol. 2011;33:636–8. doi: 10.1097/DAD.0b013e318203fc47. [DOI] [PubMed] [Google Scholar]
- 9.Lee Y, Choi EH. Exclusive facial porokeratosis: Histopathologically showing follicular cornoid lamellae. J Dermatol. 2011;38:1072–5. doi: 10.1111/j.1346-8138.2011.01260.x. [DOI] [PubMed] [Google Scholar]
- 10.Rifaioğlu EN, Ozyalvaçlı G. Follicular porokeratosis at alae nasi; a case report and short review of literature. Indian J Dermatol. 2014;59:398–400. doi: 10.4103/0019-5154.135496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yong AS, Singh M, Goulding JM, Swale VJ. Follicular porokeratosis of Mibelli on the buttocks. Clin Exp Dermatol. 2009;34:43–5. doi: 10.1111/j.1365-2230.2008.02879.x. [DOI] [PubMed] [Google Scholar]
- 12.Takiguchi RH, White KP, White CR Jr, Simpson EL. Verrucous porokeratosis of the gluteal cleft (porokeratosis ptychotropica): a rare disorder easily misdiagnosed. J Cutan Pathol. 2010;37:802–7. doi: 10.1111/j.1600-0560.2009.01387.x. [DOI] [PubMed] [Google Scholar]
- 13.Shumack S, Commens C, Kossard S. Disseminated superficial actinic porokeratosis, A histological review of 61 cases with particular reference to lymphocytic inflammation. Am J Dermatopathol. 1991;13:26. [PubMed] [Google Scholar]


