Abstract
The genomic landscape of children with acute myeloid leukemia (AML) who do not carry any cytogenetic abnormality (CN-AML) is particularly heterogeneous and challenging, being characterized by different clinical outcomes. To provide new genetic insights into this AML subset, we analyzed through RNA-seq 13 pediatric CN-AML cases, corroborating our findings in an independent cohort of 168 AML patients enrolled in the AIEOP AML 2002/01 study. We identified a chimeric transcript involving NUP98 and PHF23, resulting from a cryptic t(11;17)(p15;p13) translocation, demonstrating, for the first time, that NUP98-PHF23 is a novel recurrent (2.6 %) abnormality in pediatric CN-AML.
Keywords: NUP98 gene fusions, Pediatric acute myeloid leukemia, PHD domain
Findings
Childhood acute myeloid leukemia (AML) is a heterogeneous disease with current survival rates of approximately 60–70 %. Cytogenetics, recurrent molecular abnormalities, and early response to treatment are the main factors influencing outcome [1]. However, around 20 % of pediatric AML do not carry any known cytogenetic abnormality (cytogenetically normal-AML or CN-AML). In order to shed light on this subgroup we performed whole-transcriptome sequencing (WTS) in 13 pediatric CN-AML cases, corroborating relevant findings in an independent cohort of 168 cases.
Sequencing was performed on a HiScanSQ sequencer (Illumina), and bioinformatic analysis was performed as previously described [2]. In 2 (CN-AML_54, CN-AML_66) out of 13 cases analyzed, we identified a chimeric transcript involving nucleoporin 98 kDa (NUP98) and PHD finger protein 23 (PHF23) genes, resulting from a cryptic translocation t(11;17)(p15;p13) (Fig. 1a and Table 1). In both cases, we identified an in-frame fusion between NUP98 exon 13 and PHF23 exon 4 (Fig. 1b). To date, the cryptic translocation t(11;17)(p15;p13) has been described only once in an adult AML patient [3], but never in a pediatric AML cohort. Different from what was previously reported by Reader and colleagues [3], in this study the recurrent breakpoint in PHF23 was always identified at the beginning of exon 4 and not within it (Fig. 1a and b).
Fig. 1.
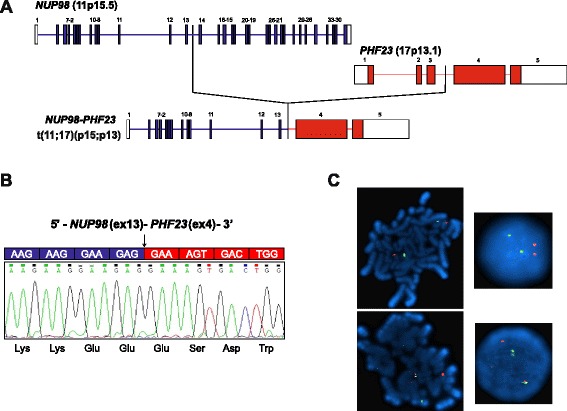
Identification of NUP98-PHF23 in pediatric CN-AML. a Schematic representation of NUP98-PHF23 fusion identified by RNA-seq in pediatric CN-AML. Fusion occurs between exon 13 of NUP98 and exon 4 of PHF23. b Electropherogram from Sanger sequencing of the region surrounding the breakpoint confirmed the in-frame fusion. A black arrow indicates the fusion breakpoint, predicted sequence of the fusion protein is shown. c FISH analysis was performed on metaphases and interphase cells using three BlueFISH probes (BlueGnome Ltd., Cambridge), according to the manufacturer’s instructions. BAC clones RP11-120E20 and RP11-348A20 (red) were used to probe the NUP98 gene on chromosome 11, while the BAC clone RP11-542C16 (green) was used to target the PHF23 gene on chromosome 17. Normal metaphases (upper left) and interphase nuclei (upper right) showed two red signals representing normal copies of NUP98 and two green signals representing normal copies of PHF23. Abnormal metaphases (lower left) and interphase cells (lower right) containing the NUP98-PHF23 fusion gene showed one red (NUP98), one green (PHF23) and one yellow fusion signal, which represents the juxtaposition of the translocated portions of the two genes
Table 1.
Clinical features of pediatric CN-AML patients harboring the NUP98-PHF23 fusion gene
| Id | Age, years | Gender | WBC, x 109/L | FAB | BM blast, % at diagnosis | Extramedullary involvement | HSCT (type) | CR after induction therapy | Relapse (site) | Disease-free duration (months) | Survival duration (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CN-AML_54a | 2.9 | M | 187 | M1 | 90 | No | Yes (AUTO) | Yes | Yes (BM) | 5 | 30b |
| CN-AML_66a | 9.0 | M | 1.2 | M0 | 70 | No | Yes (MUD) | Yes | – | 65 | 66 |
| CN-AML_3 | 9.7 | M | 6.9 | M4 | 40 | No | Yes (MUD) | Yes | – | 40 | 41 |
| CN-AML_4 | 7.0 | M | 1.8 | M5A | 54 | No | Yes (AUTO) | Yes | – | 103 | 104 |
AUTO autologous, CR complete remission, HSCT hematopoietic stem cell transplantation, MUD matched unrelated donor, BM bone marrow, WBC white blood cells
apatients identified by RNA-seq
bdead patient
To assess the incidence of NUP98-PHF23 fusion in pediatric CN-AML, we examined through RT-PCR analysis and Sanger sequencing a validation cohort of 168 AML children enrolled in the AIEOP AML 2002/01 study [4]; one-hundred thirty-nine patients (76 males and 63 females, median age at diagnosis 7.7 years, range 17 days to 17.9 years) were negative for known recurrent genetic abnormalities involving MLL, CBFB, and FLT3, while the remaining 29 patients (15 males and 14 females, median age at diagnosis 11.8 years, range 3 to 17.4 years) harbored internal tandem duplication of FLT3 (FLT3-ITD), this latter abnormality being chosen because we previously reported a strong association between NUP98-NSD1 rearrangement and FLT3-ITD [5]. With the exception of FAB M3 (acute promyelocytic leukemia), all the FAB types were represented in the validation cohort. RNA was extracted from fresh bone marrow at diagnosis, and multiplex RT-PCR was used. Sequencing by Sanger method was applied to all cases positive by PCR to NUP98-PHF23 fusion gene. Overall, 2 out of 139 CN-AML cases were found to harbor NUP98-PHF23 (Table 1). NUP98-PHF23 was not found in any patient harboring FLT3-ITD. Fluorescence in-situ hybridization confirmed the cryptic chromosomal translocation t(7;11)(p15;p13) leading to the fusion between NUP98 and PHF23 in all cases (Fig. 1c).
So far, many NUP98-rearrangements have been found to be associated with both de novo and therapy-related AML but also with T-cell acute lymphoblastic leukemia with over 28 different partner genes [6]. Recently, the fusion NUP98-JARID1A has been described to be a recurrent event in pediatric acute megakaryoblastic leukemia (11 %), with a distinct HOX gene-expression pattern [7].
Conversely, chromosomal rearrangements and/or mutations of PHF23 have never been previously described in children with AML. Located on the reverse strand of 17p13.1, PHF23 encodes for a protein containing a plant homeodomain (PHD) finger [8] involved in chromatin remodeling [3]. Expression of NUP98-PHF23 has been demonstrated to impair the differentiation of myeloid progenitor cells and promote leukemia development in vitro and in vivo [8–10]. Cells expressing NUP98-PHF23 are sensitive to disulfiram, an FDA-approved drug, demonstrating the feasibility of targeting this oncoprotein [9].
In summary, we identified, for the first time in childhood AML, a NUP98-PHF23 fusion, demonstrating that this genomic aberrancy is not exceptional (tentative frequency of 2.6 %) in pediatric CN-AML. These findings enforce the role of epigenetic regulators in pediatric AML and suggest novel therapeutic targets for this disease.
Acknowledgements
This work was supported by grants from Fondazione Ginevra Caltagirone and Fondazione Umberto Veronesi (Milan), by Cariparo IRP-Istituto di Ricerca Pediatrica-Città della Speranza (Padova) and from AIRC (Associazione Italiana Ricerca sul Cancro), special grant 5x1.000 to FL. We acknowledge the contribution of Dr. Anna Leslz for cytogenetic analysis and Maria Grazia Giacometti and Katia Polato for sample preparations.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MT performed the research, coordinated the work, analyzed data, and wrote the paper. RM coordinated the work, analyzed data, and wrote the paper. MT and AA performed the whole-transcriptome massively parallel sequencing. VI performed bioinformatics analyses. MP, EM, and VB performed the screening in the validation cohort. DZ collected and analyzed clinical data. SS performed the cytogenetic analyses. GB, AP, and FL designed and supervised the research. CR and FL equally contributed to the critical revision and writing of the manuscript. All authors read and approved the final version of the manuscript.
References
- 1.Tarlock K, Meshinchi S. Pediatric acute myeloid leukemia: biology and therapeutic implications of genomic variants. Pediatr Clin North Am. 2015;62(1):75–93. doi: 10.1016/j.pcl.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 2.Masetti R, Pigazzi M, Togni M, Astolfi A, Indio V, Manara E, et al. CBFA2T3-GLIS2 fusion transcript is a novel common feature in pediatric, cytogenetically normal AML, not restricted to FAB M7 subtype. Blood. 2013;121(17):3469–72. doi: 10.1182/blood-2012-11-469825. [DOI] [PubMed] [Google Scholar]
- 3.Reader JC, Meekins JS, Gojo I, Ning Y. A novel NUP98-PHF23 fusion resulting from a cryptic translocation t(11;17)(p15;p13) in acute myeloid leukemia. Leukemia. 2007;21(4):842–4. doi: 10.1038/sj.leu.2404579. [DOI] [PubMed] [Google Scholar]
- 4.Pession A, Masetti R, Rizzari C, Putti MC, Casale F, Fagioli F, et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood. 2013;122(2):170–8. doi: 10.1182/blood-2013-03-491621. [DOI] [PubMed] [Google Scholar]
- 5.Pigazzi M, Manara E, Bisio V, Aveic S, Masetti R, Menna G, et al. Screening of novel genetic aberrations in pediatric acute myeloid leukemia: a report from the AIEOP AML-2002 study group. Blood. 2012;120(18):3860–2. doi: 10.1182/blood-2012-09-454454. [DOI] [PubMed] [Google Scholar]
- 6.Gough SM, Slape CI, Aplan PD. NUP98 gene fusions and hematopoietic malignancies: common themes and new biologic insights. Blood. 2011;118(24):6247–57. doi: 10.1182/blood-2011-07-328880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Rooij JD, Hollink IH, Arentsen-Peters ST, van Galen JF, Berna Beverloo H, Baruchel A, et al. NUP98/JARID1A is a novel recurrent abnormality in pediatric acute megakaryoblastic leukemia with a distinct HOX gene expression pattern. Leukemia. 2013;27(12):2280–8. doi: 10.1038/leu.2013.87. [DOI] [PubMed] [Google Scholar]
- 8.Reader JC, Leng Q, Rassool FV, Ning Y. Regulation of differentiation by a PHD domain in the NUP98-PHF23 fusion protein. Leuk Res. 2010;34(8):1094–7. doi: 10.1016/j.leukres.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 9.Gough SM, Lee F, Yang F, Walker RL, Zhu YJ, Pineda M, et al. NUP98-PHF23 is a chromatin-modifying oncoprotein that causes a wide array of leukemias sensitive to inhibition of PHD histone reader function. Cancer Discov. 2014;4(5):564–77. doi: 10.1158/2159-8290.CD-13-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang GG, Song J, Wang Z, Dormann HL, Casadio F, Li H, et al. Haematopoietic malignancies caused by dysregulation of a chromatin-binding PHD finger. Nature. 2009;459(7248):847–51. doi: 10.1038/nature08036. [DOI] [PMC free article] [PubMed] [Google Scholar]


