Abstract
BACKGROUND
Surgeon volume may be an important predictor of quality and cost outcomes. We evaluated the association between surgeon volume and quality and cost of surgical care in patients with colon cancer.
STUDY DESIGN
We performed a retrospective study of patients who underwent resection for colon cancer, using data from the University HealthSystem Consortium from 2008 to 2011. Outcomes evaluated included use of laparoscopy, ICU admission, postoperative complications, length of stay, and total direct hospital costs by surgeon volume. Surgeon volume was categorized according to high (HVS), medium (MVS), and low (LVS) average annual volumes.
RESULTS
A total of 17,749 patients were included in this study. The average age of the cohort was 65 years and 51% of patients were female. After adjustment for potential confounders, compared with LVS, HVS and MVS were more likely to use laparoscopy (HVS, odds ratio [OR] 1.27, 95% CI 1.15, 1.39; MVS, OR 1.16 95% CI 1.65, 1.26). Postoperative complications were significantly lower in patients operated on by HVS than LVS (OR 0.77 95% CI 0.76, 0.91). The HVS patients were less likely to require reoperation than those in the LVS group (OR 0.70, 95% CI 0.53, 0.92) Total direct costs were $927 (95% CI −$1,567 to −$287) lower in the HVS group compared with the LVS group.
CONCLUSIONS
Higher quality, lower cost care was achieved by HVS in patients undergoing surgery for colon cancer. An assessment of differences in processes of care by surgeon volume may help further define the mechanism for this observed association.
Despite declines in the incidence rates of colorectal cancer over the last decade, it remains the third most common malignancy in the US.1 Laparoscopic-assisted colectomy (LAC) was considered an acceptable approach for colon cancer resection after the Clinical Outcomes of Surgical Therapy (COST) trial demonstrated similar disease-free survival in patients undergoing LAC and open colectomy.2 Multiple randomized controlled trials have either confirmed the findings of the COST trial, or demonstrated increased overall and disease-free survival with LAC.3,4 Laparoscopic-assisted colectomy has also been associated with improved quality of life as well as fewer complications, decreased mortality, and lower costs.5 Even though the use of laparoscopy has steadily increased over time,3 it is still offered to only a minority of patients with CRC.6,7
Previous studies have analyzed morbidity and mortality outcomes in relation to surgeon and hospital volume in colorectal surgery, but the relationship between volume and use of LAC has not been well established.8 Using data from the University HealthSystem Consortium (UHC), we examined LAC use and 30-day outcomes in patients undergoing surgery for colon cancer according to surgeon volume. We hypothesized that higher surgeon volume would be associated with higher use of LAC, lower complication rates, and lower costs, compared with lower volume surgeons, independent of hospital volume.
METHODS
Source of data
The UHC database collects inpatient data from 116 participating academic medical centers and 276 of their affiliates, comprising nearly 95% of US nonprofit medical centers. The database includes all patients hospitalized at participating institutions. Variables collected include ICD-9 (International Classification of Diseases, 9th edition) codes for diagnoses and procedures, physician specialty, length of stay, risk-adjusted severity of illness scores, and hospital associated costs. The UHC converts hospital charges into cost estimates based on federal-wage data for each hospital location, allowing for meaningful cost comparisons between centers, regardless of hospital location.
After exemption status by the IRB was received, the UHC database was queried for adult patients, 18 years or older, with ICD-9 diagnostic codes for colon or rectosigmoid cancers (153.0–153.4, 153.6–153.8, 154.0) present on admission between 2008 and 2011. These years were studied because they allowed for analysis of surgeon volume, as the unique surgeon identification numbers changed in 2012. To identify patients who underwent cancer resection, this cohort was limited to those with ICD-9 procedure codes for open and laparoscopic colectomy (45.71, 45.73–45.76, 45.79, 45.8, 45.81–45.82, 17.33–17.36, 17.39). Patients were excluded if they underwent both colon and mid- to lower-rectal resection in the same hospitalization, or if their hospitalization was urgent or emergent based on categorization in the database.
Outcomes measures
The primary outcome of interest was the use of laparoscopy, which was determined by ICD-9 procedure codes for laparoscopic colectomy. Secondary outcomes were frequency of complications (eg, stroke, pneumonia, hemorrhage/hematoma, reopening of surgical wound, cellulitis, urinary tract infection, myocardial infarction, venous thromboembolism, sepsis), ICU admission rate after initial procedure, inpatient length of stay, and total direct hospital costs. Postoperative complications were coded in the database based on risk pools according to procedure type by UHC. Reoperation was defined by ICD-9 procedure codes for exploratory laparotomy or laparoscopy (54.10, 54.11, 54.12, 54.19), small or large bowel resection (17.33–17.36, 17.39, 45.71, 45.73–45.76, 45.79, 45.8, 45.81–45.82, 48.42, 48.51, 48.52, 48.62, 48.63, 45.00, 45.00–45.02, 45.50–45.52, 45.61–45.63, 46.73), or stoma creation/revision (46.01, 46.03, 46.10, 46.11, 46.13, 46.20, 46.22, 46.23, 46.39) occurring at least 1 day after the primary procedure, including during any readmission stays. Additional covariates used for analysis included age, sex, race, comorbid diagnoses (based on ICD-9 diagnosis codes), 3M APR-DRG Admission Severity of Illness Score (3M Health Information Systems), and insurance status. Severity of illness was reclassified into low (minor and moderate) and high (major and extreme) for ease of analysis.
Surgeon and hospital volume categories
Once the cohort was identified, unique physician identifiers were used to examine the distribution of yearly surgeon volume. Surgeons who performed less than 1 colectomy per year averaged over the 4-year study period were excluded. Surgeon volume was classified as high, medium, or low based on the observed distribution of average annual surgeon volume. High volume was defined as greater than or equal to the 90th percentile (>11 colectomies per year), medium volume between the 50th and 90th percentiles (5 to 11 colectomies per year), and low-volume as the 50th percentile or less (<5 colectomies per year). The 50th percentile cutoff for LVS was chosen instead of the 25th percentile to allow for similar numbers of patients in each group for analysis, in addition to the authors’ decision that there was little clinical relevance for distinguishing between performing 2 colectomies per year (the 25th percentile cutoff) vs 4 per year. Surgical specialty was not assessed in this study because some institutions classify their specialists as generalists. We elected not to make these comparisons because this misclassification may have skewed the results.
In order to account for the potentially confounding effects of hospital volume, a variable for hospital volume was created using unique, decrypted hospital identifiers. Hospital volume was categorized according to quartiles of average yearly volume into low (<9 colectomies per year), medium (9 to 18 colectomies per year), high (19 to 37 colectomies per year), and very high (>37 colectomies per year) volume (Table 1).
Table 1.
Summary of Surgeon and Hospital Volume Groups Over the Study Period
| Variable | Low | Medium | High | Very high |
|---|---|---|---|---|
| Surgeons | ||||
|
| ||||
| Definition of group* | <5 | 5–11 | >11 | – |
|
| ||||
| Surgeons, n | 1,274 | 379 | 64 | – |
|
| ||||
| Cases, † n | 3,916 | 7,038 | 6,975 | – |
|
| ||||
| Hospitals | ||||
|
| ||||
| Definition of group* | <9 | 9–18 | 19–37 | >37 |
|
| ||||
| Hospitals, n | 49 | 48 | 46 | 50 |
|
| ||||
| Cases, † n | 575 | 2,033 | 4,046 | 11,095 |
Average number of colectomies for cancer per year.
Total number of cases over the study period.
Statistical analysis
Bivariate and multivariable regression analyses were used to evaluate differences in the primary and secondary outcomes according to surgeon volume while controlling for the effects of various potentially confounding variables. Differences in selected continuous variables were analyzed by analysis of variance; differences in categorical variables were examined through the use of chi-square tests. Selection of covariates for use in the multivariable regression models was based on a priori knowledge and significant associations observed in our bivariate analyses. An interaction term for hospital volume and surgeon volume was found to be nonsignificant and was not included in the multivariable model. All analyses were conducted with the use of Stata IC version 12.1.
RESULTS
Patient and surgeon characteristics
A total of 17,749 adult men and women who underwent colectomy for cancer between 2008 and 2011 comprised the study sample. The average age of this population was 65 years, and 51% were women (Table 2). Among these patients, 6,795 (38%) underwent colectomy by a high-volume surgeon (HVS), 7,038 (40%) by a medium-volume surgeon (MVS), and 3,916 (22%) by a low-volume surgeon (LVS). The distribution of average annual surgeon volume was right skewed, with an overall median volume of 3.5 colectomies per year (Fig. 1). The median numbers of cases performed per year were: HVS group, 17; MVS group, 7; and LVS group, 2.
Table 2.
Patient Demographics and Baseline Characteristics
| Surgeon volume category* |
||||
|---|---|---|---|---|
| Demographic and characteristics | Low (n = 3,916) | Medium (n = 7,038) | High (n = 6,795) | p Value |
| Age, y, mean (SD) | 66 (13.5) | 65 (13.7) | 65 (13.8) | NS |
|
| ||||
| Male, n (%) | 1,902 (49) | 3,445 (49) | 3,414 (50) | NS |
|
| ||||
| Race, n (%) | ||||
|
| ||||
| White | 2,808 (72) | 5,178 (74) | 4,989 (73) | NS |
|
| ||||
| Black | 539 (14) | 1,007 (14) | 817 (12) | <0.001 |
|
| ||||
| Hispanic | 36 (1) | 48 (1) | 23 (<1) | <0.001 |
|
| ||||
| Asian | 120 (3) | 205 (3) | 236 (3) | NS |
|
| ||||
| Other | 412 (8) | 600 (9) | 730 (11) | <0.001 |
|
| ||||
| Insurance status, n (%) | ||||
|
| ||||
| Private | 1,314 (33) | 2,706 (39) | 2,847 (42) | <0.001 |
|
| ||||
| Public | 2,380 (61) | 4,069 (58) | 3,780 (55) | <0.001 |
|
| ||||
| Self-pay | 24 (<1) | 51 (<1) | 45 (<1) | <0.001 |
|
| ||||
| Other | 198 (5) | 212 (3) | 123 (2) | <0.001 |
|
| ||||
| Comorbidities, n (%) | ||||
|
| ||||
| Hypertension | 2,197 (56) | 3,844 (54) | 3,634 (54) | 0.03 |
|
| ||||
| Diabetes | 847 (22) | 1,389 (20) | 1,300 (19) | 0.01 |
|
| ||||
| Anemia | 856 (22) | 1,448 (21) | 1,220 (18) | <0.001 |
|
| ||||
| COPD | 496 (13) | 844 (13) | 849 (13) | NS |
|
| ||||
| Obesity | 410 (10) | 788 (11) | 844 (12) | 0.01 |
|
| ||||
| Congestive heart failure | 214 (5) | 357 (5) | 331 (5) | NS |
|
| ||||
| Depression | 250 (6) | 472 (7) | 487 (7) | NS |
|
| ||||
| Renal disease | 222 (6) | 373 (5) | 408 (6) | NS |
|
| ||||
| Peripheral vascular disease | 177 (5) | 268 (4) | 271 (4) | NS |
|
| ||||
| Liver disease | 106 (3) | 174 (3) | 153 (2) | NS |
|
| ||||
| Severity of illness category, n (%) | ||||
|
| ||||
| Low (minor/moderate) | 3,533 (90) | 6,480 (92) | 6,216 (91) | 0.004 |
|
| ||||
| High (major/extreme) | 383 (10) | 558 (8) | 579 (9) | 0.004 |
Low, <5 colectomies per year; medium; 5—11 colectomies per year; high, >11 colectomies per year.
Figure 1.

Distribution of average surgeon volume per year.
In examining differences in various baseline patient characteristics in our respective comparison groups, there was a greater proportion of black patients in the LVS and MVS vs HVS groups (Table 2). A considerably greater proportion of patients in the LVS group were publically insured than in the MVS and HVS groups. Baseline clinical characteristics were generally similar, although there were slightly higher proportions of hypertensive, diabetic, and anemic patients in the LVS group, and a trend toward more obese patients was observed with increasing surgeon volume. The vast majority of study patients presented with low severity of illness.
Study outcomes
Between 2008 and 2011, there was an overall increase in the use of laparoscopy, with persistently higher rates in the HVS and MVS groups (Fig. 2). In 2011, rates of laparoscopy were 51% in the HVS group, 49% in the MVS group, and only 41% in the LVS group. Between 2010 and 2011, the biggest increase in laparoscopy use was in the LVS group. Complication rates were generally low and were slightly lower in HVS compared with MVS and LVS (7% vs. 8%) (Table 3). When limited to major and extreme severity of illness category, the difference in complication rates was more apparent, with a 14% complication rate among HVS and 16% and 22% in the MVS and LVS groups, respectively. Reoperation occurred in 4% of LVS patients, and 3% and 4% of the MVS and HVS patients.
Figure 2.
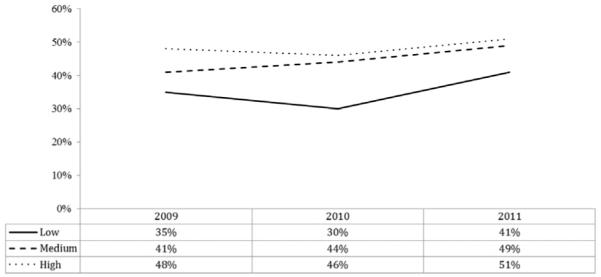
Trend in proportion of colectomies performed using laparoscopy by surgeon volume category.
Table 3.
Unadjusted Outcomes by Surgeon Volume Category
| Surgeon volume category* |
||||
|---|---|---|---|---|
| Outcome | Low | Medium | High | p Value |
| Colectomy type, n (%) | ||||
|
| ||||
| Right | 2,127 (54) | 3,753 (53) | 3,540 (52) | NS |
|
| ||||
| Transverse | 189 (5) | 288 (4) | 240 (4) | 0.004 |
|
| ||||
| Left | 439 (11) | 809 (12) | 829 (12) | NS |
|
| ||||
| Sigmoid | 796 (20) | 1,463 (21) | 1,416 (21) | NS |
|
| ||||
| Total | 116 (3) | 297 (4) | 351 (5) | <0.001 |
|
| ||||
| Other | 249 (7) | 428 (6) | 419 (6) | NS |
|
| ||||
| Any postoperative complication, n (%) | 330 (8) | 531 (8) | 454 (7) | 0.003 |
|
| ||||
| Complications if high severity of illness, n (%) | 86 (22) | 90 (16) | 80 (14) | 0.002 |
|
| ||||
| ICU admission, n (%) | 904 (23) | 1,254 (18) | 1,107 (16) | <0.001 |
|
| ||||
| ICU admission if low severity of illness, n (%) | 725 (21) | 1,023 (16) | 870 (14) | <0.001 |
|
| ||||
| Reoperation, n (%) | 145 (4) | 192 (3) | 160 (2) | <0.001 |
|
| ||||
| Inpatient length of stay, d, mean (SD) | 6 (7) | 6 (7) | 5 (9) | <0.001 |
|
| ||||
| Direct hospital cost, $, mean (SD) | 14,758 (16,323) | 13,602 (14,541) | 13,100 (14,196) | <0.001 |
|
| ||||
| Laparoscopic | 11,898 (9,175) | 11,389 (11,458) | 10,895 (9,905) | <0.001 |
|
| ||||
| Open | 16,589 (19,354) | 15,386 (16,401) | 15,192 (17,050) | <0.001 |
High severity of illness indicates major/extreme severity of illness; low severity of illness indicates minor/moderate severity of illness.
Low, <5 colectomies per year; medium, 5—11 colectomies per year; high, >11 colectomies per year.
Nearly one-quarter of patients in the LVS group were admitted to the ICU postoperatively; however, only 18% of the MVS and 16% of HVS had a postoperative ICU stay. Median length of stay was 1 day longer in the LVS and MVS groups. The HVS patients had the lowest overall mean total direct cost, at $13,100, a mean laparoscopic cost of $10,895, and average open costs of $15,192. As surgeon volume decreased, the costs for both LAC and open colectomy increased (Fig. 3).
Figure 3.

Unadjusted mean overall (all), laparoscopic, and open total direct cost according to surgeon volume category.
After adjusting for relevant covariates, including hospital volume, the odds of LAC (vs open colectomy) were 16% higher for MVS compared with LVS and 27% higher when comparing HVS with LVS (Table 4). Patients operated on by HVS had about one-quarter fewer complications than LVS patients. The odds of reoperation were 30% less among HVS patients (vs LVS group). On adjusted analysis, higher surgeon volume was not found to be associated with ICU admission and length of stay. Finally, total direct costs were significantly lower for both MVS and HVS compared with LVS, regardless of how the procedure was performed (open or laparoscopic).
Table 4.
Multivariable Analyses Assessing the Influence of Surgeon Volume on Outcomes
| Laparoscopy |
Complication |
Reoperation |
ICU admission |
LOS, d |
Cost, $ |
|
|---|---|---|---|---|---|---|
| Variable | Odds ratio (95% CI) | Beta coefficient (95% CI) | ||||
| Surgeon volume category | ||||||
|
| ||||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
|
| ||||||
| Medium | 1.16 (1.06, 1.26) | 0.89 (0.77, 1.03) | 0.77 (0.60, 0.98) | 0.89 (0.80, 1.00) | −0.05 (−0.34, 0.23) | −810 (−1,407, −213) |
|
| ||||||
| High | 1.27 (1.15, 1.39) | 0.77 (0.76, 0.91) | 0.70 (0.53, 0.92) | 0.98 (0.87, 1.10) | −0.01 (−0.31, 0.30) | −927 (−1,567, -287) |
|
| ||||||
| Hospital volume category | ||||||
|
| ||||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
|
| ||||||
| Medium | 1.62 (1.32, 2.00) | 1.53 (1.04, 2.27) | 1.09 (0.62, 1.94) | 0.85 (0.68, 1.05) | 0.48 (−0.17, 1.13) | 1,097 (−334, 2,528) |
|
| ||||||
| High | 1.89 (1.54, 2.31) | 1.61 (1.10, 2.35) | 1.02 (0.59, 1.79) | 0.67 (0.54, 0.83) | 0.39 (−0.21, 1.05) | 2657 (1,279, 4,036) |
|
| ||||||
| Very high | 2.02 (1.66, 2.47) | 1.67 (1.16, 2.43) | 0.96 (0.55, 1.66) | 0.44 (0.35, 0.54) | 0.18 (−.044, 0.79) | 1011 (−343, 2,367) |
|
| ||||||
| Age, per year increase | 1.01 (1.00, 1.01) | 0.99 (0.99, 1.00) | 0.99 (0.98, 1.00) | 1.01 (1.00, 1.01) | 0.00 (−0.01, 0.01) | −25 (−46, -3) |
|
| ||||||
| Female (vs male) | 1.08 (1.01, 1.14) | 0.68 (0.60, 0.76) | 0.72 (0.59, 0.87) | 0.84 (0.77, 0.91) | −0.53 (−0.74, −0.33) | −1,212 (−1,647, −778) |
|
| ||||||
| Race | ||||||
|
| ||||||
| White | Ref. | Ref. | – | Ref. | Ref. | Ref. |
|
| ||||||
| Black | 0.95 (0.87, 1.04) | 1.00 (0.85, 1.20) | – | 0.83 (0.73, 0.94) | 0.59 (0.29, 0.91) | 535 (−127, 1,197) |
|
| ||||||
| Other | 1.35 (1.23, 1.48) | 1.00 (0.85, 1.20) | – | 0.76 (0.68, 0.88) | 0.30 (−0.01, 0.60) | 38 (−613, 688) |
|
| ||||||
| Insurance status | ||||||
|
| ||||||
| Private | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
|
| ||||||
| Public | 0.82 (0.75, 0.89) | 1.52 (1.30, 1.78) | 1.16 (0.90, 1.49) | 1.32 (118, 1.48) | 0.58 (0.30, 0.86) | 705 (119, 1,292) |
|
| ||||||
| Other | 0.71 (0.60, 0.85) | 1.08 (0.77, 1.51) | 0.83 (0.48, 1.44) | 1.21 (0.97, 1.51) | −0.02 (−0.60, 0.55) | −637 (−1,858, 584) |
|
| ||||||
| High severity of illness (vs low) | 0.41 (0.37, 0.47) | 2.42 (2.08, 2.83) | 1.56 (1.20, 2.02) | 2.83 (2.51, 3.19) | 3.78 (3.40, 4.16) | 7,154 (6,357, 7,951) |
|
| ||||||
| Laparoscopic (vs open) | – | 0.57 (0.51, 0.66) | 0.91 (0.74, 1.12) | 0.44 (0.40, 0.48) | −2.12 (−2.33, −1.90) | −2,716 (−3,160, −2,273) |
|
| ||||||
| Procedure | ||||||
|
| ||||||
| Total colectomy | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
|
| ||||||
| Left colectomy | 1.32 (1.10, 1.58) | 0.92 (0.66, 1.25) | 0.57 (0.37, 0.88) | 0.85 (0.68, 1.05) | −1.44 (−2.02, −0.86) | −2,134 (−3,357, −912) |
|
| ||||||
| Right colectomy | 1.72 (1.47, 2.02) | 0.88 (0.67, 1.16) | 0.44 (0.30, 0.65) | 0.69 (0.58, 0.85) | −1.88 (−2.40, −1.35) | −3,739 (−4,832, −2,639) |
|
| ||||||
| Transverse colectomy | 0.94 (0.75, 1.17) | 0.79 (0.53, 1.16) | 0.52 (0.29, 0.94) | 0.73 (0.56, 0.95) | −1.56 (2.28, −0.83) | −3608 (−5,124, −2,092) |
|
| ||||||
| Sigmoid colectomy | 1.72 (1.46, 2.03) | 0.77 (0.57, 1.03) | 0.57 (0.37, 0.84) | 0.66 (0.54, 0.81) | −2.23 (−2.76, −1.68) | −3,427 (−4,573, −2,281) |
|
| ||||||
| Other | 0.52 (0.39, 0.70) | 1.47 (0.98, 2.16) | 1.32 (0.77, 2.25) | 1.09 (0.81, 1.46) | 0.42 (−0.44, 1.27) | 1,925 (127, 3,733) |
|
| ||||||
| Postoperative complications (vs none) | – | – | 15.38 (12.67, 18.67) | 4.35 (3.84, 4.92) | 9.18 (8.79, 9.58) | 18,806 (17,968, 19,643) |
LOS, length of stay; Ref., referent category.
DISCUSSION
This large observational study of adult men and women who underwent colectomy for colon cancer examined several health outcomes in relation to surgeon volume. Our results suggest higher rates of laparoscopy, fewer complications, and lower cost surgery was achieved by higher-volume surgeons. After adjustment for relevant confounders, both HVS and MVS were more likely to use laparoscopy than LVS. Lower complication rates were achieved by HVS, after adjusting for admission severity of illness. The LVS admitted more of their patients to the ICU after the procedure. Cost was lower for MVS and HVS, compared with LVS.
Colorectal cancer (CRC)-related care has a tremendous impact on health care costs. In 2010, the cost of treating CRC was estimated to be more than $14 billion, nearly half of which was spent on patients in the first year after diagnosis.9 Aging of the US population will likely lead to an increase in the number of patients with CRC and add to its financial burden. The Affordable Care Act (ACA),10 passed in March 2010, demands low-cost care that maintains a high standard of quality. High-prevalence and high-cost diseases, like CRC, provide ideal targets for these reform efforts. In order to ensure policy changes are in the best interests of patients, quality indicators and their effects on cost need to be evaluated. This analysis of the relationship between surgeon-volume laparoscopy use, 30-day outcomes, and costs after elective colectomy for cancer was performed with that goal in mind.
Laparoscopy use
Established improvements in morbidity, mortality, and quality of life led us to identify LAC as a quality indicator in surgery for colon cancer.5,11-16 We demonstrated an overall rate of LAC use of 45% during the study period, with an increase from 42% to 48% between 2009 and 2011; these are higher than rates published from NSQIP in 2008 (34%), but similar to those from the Nationwide Inpatient Sample in 2009 (42.6%).7,17 An important consideration for this difference is the use of Common Procedural Terminology (CPT) codes in NSQIP and ICD-9 procedure codes in the Nationwide Inpatient Sample and UHC. We showed higher rates of laparoscopy use for HVS and MVS compared with LVS. An explanation for our findings of lower LAC rates among LVS may be related to the well-established steep learning curves for laparoscopic colectomies.18,19 Colectomies are likely a small portion of these surgeons’ practices, and the surgeons are unable to dedicate the time and resources necessary for learning and adopting a new technique.
Thirty-day outcomes
The association between improved outcomes and higher hospital or surgeon volume has been identified for many procedures, including colon cancer surgery.8 The primary outcome of interest in previous studies analyzing the volume-outcome relationship in colon cancer patients has been all-cause mortality.18,20 Mortality rates for elective colon resection are, however, low (1% to 2%), and the most important predictors of mortality are patient related, including older age and comorbidities, rather than systems-related factors.21,22 Therefore, we focused our analyses on outcomes related to resource use and hospital-associated costs, rather than mortality. Consistent with previous studies, our data demonstrated lower post-operative complication rates, shorter length of stay, and lower costs in association with higher surgeon volume.23,24
Intensive care unit admission after elective procedures is a surrogate marker for excess resource use that has not been previously analyzed with respect to surgeon volume. The rate of ICU admission for patients with low severity of illness was 7% higher in the LVS group than in the HVS group. However, after adjustment for hospital volume, this difference was no longer seen. This may be explained by differences in patterns of care by hospital volume, in which low-volume surgeons may be operating at hospitals with lower thresholds for ICU admission after surgery.
Study strengths and limitations
Compared with other studies that have previously used administrative data, we were able to provide data from a national cohort of patients, which may provide more generalizable results. Unique surgeon and hospital identifiers allowed for categorization of both surgeon and hospital volume directly, rather than using hospital volume as a surrogate marker for surgeon volume. Therefore, we were able to analyze differences in outcomes by surgeon volume while adjusting for the confounding influence of hospital volume. A unique aspect of our study is our categorization of surgeon volume. We believe our method of categorizing surgeon volume by distribution of the data, rather than quartiles of patients per category, allows for a more clinically relevant comparison of surgeon volume.
However, our study is not without limitations. First, it is susceptible to the pitfalls of using administrative claims data, including errors in coding and evidence of statistical significance regardless of clinical significance. To reduce the potential for bias toward high volume surgeons, surgeons who were documented as having performed the procedure less than once per year on average were excluded from the analysis. Second, given the nature of the data, analysis of the impact of surgeon volume on oncologic outcomes of interest, including nodal status, cancer-survival rates, and long-term outcomes, was not possible. Third, we were also unable to analyze anastomotic leak rates because this variable does not exist in UHC. Finally, while we were unable to account for selection bias, surgeon experience, and decision-making, we did adjust for admission severity of illness, which accounts for comorbidities that usually influence decisions in the pre-, intra-, and postoperative periods.
CONCLUSIONS
At a time when health care reform aims to reduce health care costs in the US while maintaining quality care, analysis of quality and cost outcomes has high importance. Our results suggest higher quality, lower cost care can be achieved by surgeons performing a higher volume of colectomies for colon cancer, independent of hospital volume. Surgeon volume may be an important factor to consider when policies aimed at improving quality and reducing costs are developed. Processes of care after surgery for colon cancer need to be further studied to allow for implementation of interventions that will lead to improved outcomes in a cost-effective manner after surgery for colon cancer.
Acknowledgments
Support: Dr Santry received the University of Massachusetts Clinical Scholar Award (HPS) UL1RR031982, 1KL2RR031981-01, and UL1TR000161 from the NIH.
Abbreviations and Acronyms
- CRC
colorectal cancer
- HVS
high volume surgeon
- LAC
laparoscopic-assisted colectomy
- LVS
low volume surgeon
- MVS
medium volume surgeon
- OR
odds ratio
- UHC
University HealthSystem Consortium
Footnotes
Disclosure Information: Nothing to disclose.
Presented at the New England Surgical Society 94th Annual Meeting, Hartford, CT, September 2013.
REFERENCES
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Clinical Outcomes of Surgical Therapy Study Group A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 3.Sticca RP, Alberts SR, Mahoney MR, et al. Current use and surgical efficacy of laparoscopic colectomy in colon cancer. J Am Coll Surg. 2013;217:56–62. doi: 10.1016/j.jamcollsurg.2013.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonjer HJ, Hop WC, Nelson H, et al. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007;142:298–303. doi: 10.1001/archsurg.142.3.298. [DOI] [PubMed] [Google Scholar]
- 5.Vaid S, Tucker J, Bell T, et al. Cost analysis of laparoscopic versus open colectomy in patients with colon cancer: results from a large nationwide population database. Am Surg. 2012;78:635–641. [PubMed] [Google Scholar]
- 6.Rea JD, Cone MM, Diggs BS, et al. Utilization of laparoscopic colectomy in the United States before and after the clinical outcomes of surgical therapy study group trial. Ann Surg. 2011;254:281–288. doi: 10.1097/SLA.0b013e3182251aa3. [DOI] [PubMed] [Google Scholar]
- 7.Ozhathil DK, Li Y, Smith JK, et al. Colectomy performance improvement within NSQIP 2005-2008. J Surg Res. 2011;171:e9–13. doi: 10.1016/j.jss.2011.06.052. [DOI] [PubMed] [Google Scholar]
- 8.Pieper D, Mathes T, Neugebauer E, et al. State of evidence on the relationship between high-volume hospitals and outcomes in surgery: a systematic review of systematic reviews. J Am Coll Surg. 2013;216:1015–1025.e18. doi: 10.1016/j.jamcollsurg.2012.12.049. [DOI] [PubMed] [Google Scholar]
- 9.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103:117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kocher R, Emanuel EJ, DeParle NA. The Affordable Care Act and the future of clinical medicine: the opportunities and challenges. Ann Intern Med. 2010;153:536–539. doi: 10.7326/0003-4819-153-8-201010190-00274. [DOI] [PubMed] [Google Scholar]
- 11.Stucky CC, Pockaj BA, Novotny PJ, et al. Long-term follow-up and individual item analysis of quality of life assessments related to laparoscopic-assisted colectomy in the COST trial 93-46-53 (INT 0146) Ann Surg Oncol. 2011;18:2422–2431. doi: 10.1245/s10434-011-1650-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delaney CP, Chang E, Senagore AJ, et al. Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg. 2008;247:819–824. doi: 10.1097/SLA.0b013e31816d950e. [DOI] [PubMed] [Google Scholar]
- 13.Senagore AJ, Stulberg JJ, Byrnes J, et al. A national comparison of laparoscopic vs. open colectomy using the National Surgical Quality Improvement Project data. Dis Colon Rectum. 2009;52:183–186. doi: 10.1007/DCR.0b013e31819ad4a4. [DOI] [PubMed] [Google Scholar]
- 14.Hardiman K, Chang ET, Diggs BS, et al. Laparoscopic colectomy reduces morbidity and mortality in obese patients. Surg Endosc. 2013;27:2907–2910. doi: 10.1007/s00464-013-2853-3. [DOI] [PubMed] [Google Scholar]
- 15.Veldkamp R, Kuhry E, Hop WC, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 16.Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 17.Kang CY, Halabi WJ, Luo R, et al. Laparoscopic colorectal surgery: a better look into the latest trends. Arch Surg. 2012;147:724–731. doi: 10.1001/archsurg.2012.358. [DOI] [PubMed] [Google Scholar]
- 18.Tekkis PP, Senagore AJ, Delaney CP, et al. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005;242:83–91. doi: 10.1097/01.sla.0000167857.14690.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reichenbach DJ, Tackett AD, Harris J, et al. Laparoscopic colon resection early in the learning curve: what is the appropriate setting? Ann Surg. 2006;243:730–735. doi: 10.1097/01.sla.0000220039.26524.fa. discussion 735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogers SOJ, Wolf RE, Zaslavsky AM, et al. Relation of surgeon and hospital volume to processes and outcomes of colorectal cancer surgery. Ann Surg. 2006;244:1003–1011. doi: 10.1097/01.sla.0000231759.10432.a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Masoomi H, Kang CY, Chen A, et al. Predictive factors of in-hospital mortality in colon and rectal surgery. J Am Coll Surg. 2012;215:255–261. doi: 10.1016/j.jamcollsurg.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 22.Billeter AT, Polk HCJ, Hohmann SF, et al. Mortality after elective colon resection: the search for outcomes that define quality in surgical practice. J Am Coll Surg. 2012;214:436–443. doi: 10.1016/j.jamcollsurg.2011.12.018. discussion 443. [DOI] [PubMed] [Google Scholar]
- 23.Billingsley KG, Morris AM, Dominitz JA, et al. Surgeon and hospital characteristics as predictors of major adverse outcomes following colon cancer surgery: understanding the volume-outcome relationship. Arch Surg. 2007;142:23–31. doi: 10.1001/archsurg.142.1.23. discussion 32. [DOI] [PubMed] [Google Scholar]
- 24.Harmon JW, Tang DG, Gordon TA, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg. 1999;230:404–411. doi: 10.1097/00000658-199909000-00013. discussion 411. [DOI] [PMC free article] [PubMed] [Google Scholar]


