Abstract
In the present study we analyzed the anti-proliferative effect of tocilizumab, a humanized recombinant monoclonal interleukin 6 receptor (IL-6R) antibody, against non-small cell lung cancer (NSCLC) cells, including A549, H460, H358 and H1299 cells. The cell cycle distribution of NSCLCs was analyzed using fluorescence-activated cell sorting and gene expression using quantitative polymerase chain reaction. Cell lysates treated with tocilizumab were immunoblotted with antibodies against signal transducer and activator of transcription 3 (STAT3), phospho-STAT3, extracellular-signal-regulated kinases (ERK), phospho-ERK, nuclear factor κB (NFκB) and phospho-NFκB. Significant growth inhibition of NSCLC cells was observed following treatment with tocilizumab. Proliferation was significantly decreased by approximately 10–40% in A549, H460, H1299 and H358 cells, with an inhibition rate that was comparable with that of the typical anticancer drugs methotrexate and 5-fluorouracil. NSCLC cell populations were accumulated in the sub-G1 phase by treatment with tocilizumab. Western blot analyses revealed a possible activation of the NFκB pathway by tocilizumab. Overall, these data indicate that tocilizumab has anticancer potency via apoptosis induction as an agonistic IL-6R regulator. Therefore, we suggest that this anti-IL-6R antibody may be utilized as a new targeting molecule for NSCLC therapies.
Keywords: tocilizumab, interleukin 6 signaling, non-small cell lung cancer, NFκB, anti-proliferation
Introduction
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, accounting for more than 80% of cases. As a class, NSCLC is relatively insensitive to chemotherapy compared with small cell carcinoma. A number of drugs are useful for NSCLC as systemic therapy, including platinum agents (cisplatin and carboplatin), taxanes (paclitaxel and docetaxel), vinorelbine, vinblastine, etoposide, pemetrexed and gemcitabine. However, despite advances in chemotherapeutic drugs, the prognosis of lung cancer remains poor, with an overall 5-year survival rate of less than 14% in the USA and even lower (5–10%) in Europe and other countries (1).
A number of investigators have attempted to develop specific targeting molecules, including antibodies and antagonists, for the treatment of NSCLC. Bevacizumab is a recombinant monoclonal antibody that blocks vascular endothelial growth factor. Erlotinib is a small molecule inhibitor of epidermal growth factor receptor (EGFR), and crizotinib is a small molecule inhibitor that targets anaplastic lymphoma kinase and hepatocyte growth factor receptor c-MET. Cetuximab is a monoclonal antibody that targets EGFR.
The pathway of interleukin 6/interleukin 6 receptor (IL-6/IL-6R) signaling regulates diverse biological activities, including cell growth and differentiation, in immune and hematopoietic systems (2). However, IL-6/IL-6R signaling is also known to promote tumor growth and survival in several organ systems (3). The plasma IL-6 levels of cancer patients were observed to correlate with the clinical and pathological variety and survival in prostate cancer (4), ovarian cancer (5), breast cancer (6) and colorectal cancer (7). Tocilizumab is a humanized recombinant IgG1k monoclonal antibody against IL-6R (8). It is approved by the FDA and used in clinics to treat rheumatoid arthritis and juvenile idiopathic arthritis patients (9). It has also been demonstrated that tocilizumab has an anti-proliferative effect on glioma cells via inhibition of the JAK-STAT3 pathway (10). Furthermore, there is evidence that IL-6/IL-6 signaling affects NSCLC tumorigenesis (11).
In a previous study (12), we demonstrated the possibility of using IL-6R as a selective anticancer drug target using an H460 lung cancer stem cell model. Here, we investigate the effect of IL-6R blockage on the proliferation of NSCLC cells using the IL-6R-targeted antibody tocilizumab.
Materials and methods
Cell culture
NSCLC cell lines H460, A549, H1299 and H358 were obtained from the Korean Cell Line Bank (KCLB, Seoul, Korea). The cells were grown in RPMI-1640 medium (Gibco Life Technologies, Carlsbad, CA, USA) with 10% heat-inactivated fetal bovine serum (Gibco) and 1% penicillin/streptomycin (Gibco) at 37°C in a humidified incubator (5% CO2), as recommended by KLCB.
Cell proliferation assay
The anticancer drugs methotrexate (MTX) and 5-fluorouracil (5-FU) were purchased from Sigma-Aldrich (St. Louis, MO, USA), and tocilizumab was kindly donated by Dr Misahiko Mihara at Chugai Pharmaceutical Co. Ltd. (Shizuoka, Japan). The anti-proliferation activity of tocilizumab, MTX and 5-FU in NSCLC cells in vitro was measured using the EZ-Cytox kit (Daeillab, Seoul, Korea). Ten microliters of tocilizumab, MTX or 5-FU were added to 96-well plates containing 104 cells per well in 100 µl medium. The final concentrations of tocilizumab were 10, 100 and 1000 ng/ml. The final concentrations of MTX and 5-FU were 50 and 25 µg/ml, respectively. Following a 24-h incubation, WST-1 solution (Daeillab) was added, and the optical density was analyzed using the ELISA plate reader Magellan™ (Tecan, Männedorf, Switzerland) at reference wavelengths of 450 and 620 nm.
Cell cycle analysis
The NSCLC cells were seeded at 2.0×105 cells/well in 6-well plates. The cells were allowed to recover for 24 h and then treated with tocilizumab. To analyze the cell cycle distribution, the cells were collected after a 24-h incubation and washed with phosphate-buffered saline (PBS). The cells were fixed in 70% ethanol and stored overnight at 4°C. For the analysis, the cells were transferred to PBS and incubated with ribonuclease A (50 µg/ml) at room temperature for 5 min. The cells were then stained with 10 µg/ml propidium iodide (PI) and incubated at 37°C for 10 min. Finally, the cells were analyzed using fluorescence-activated cell sorting.
RNA extraction and quantitative polymerase chain reaction (qPCR)
qPCR was performed to identify the gene expression level of IL-6R in the NSCLC cells based on the expression of a housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (GAPDH), as an internal control. RNA was quantified by its absorption at 260 nm and stored at −80°C before use. Briefly, first-strand cDNA was synthesized from 2 µg total RNA with Superscript III transcriptase (Invitrogen Life Technologies, Carlsbad, CA, USA). PCR amplification was performed with specific primer pairs designed from published human gene sequences (13). qPCR was performed using SYBR-Green (Takara Bio Inc., Shiga, Japan) and a Bio-Rad machine (Bio-Rad Laboratories Inc., Hercules, CA, USA). DNA was amplified using 60 cycles of denaturation for 5 sec at 95°C and annealing for 40 sec at 60°C.
Protein extraction and western blot analysis
Whole-cell lysates were extracted using the Pro-Prep protein extraction solution plus protease inhibitor cocktail (Intron Biotechnology, Seongnam, Korea) according to the method described in the manufacturer's guidelines. Cell lysates were separated using 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), transferred to a nitrocellulose membrane (Bio-Rad), and immunoblotted with antibodies against the following: signal transducer and activator of transcription 3 (STAT3), phospho-STAT3, extracellular-signal-regulated kinases (ERK), phospho-ERK, nuclear factor κB (NFκB) and phospho-NFκB (Cell Signaling Technology, Inc., Beverly, MA, USA). After incubating with the secondary antibody, the membranes were developed using enhanced chemiluminescence. ImageJ software (NIH, USA) was used to analyze the results.
Statistical analysis
The results are expressed as the means ± standard deviation. Analysis of variance was used to compare differences among the groups. P<0.05 was considered to indicate a statistically significant difference. Statistical analyses were performed with Statistical Analysis Systems software (SPSS version 20; IBM SPSS, Armonk, NY, USA).
Results
Cell proliferation
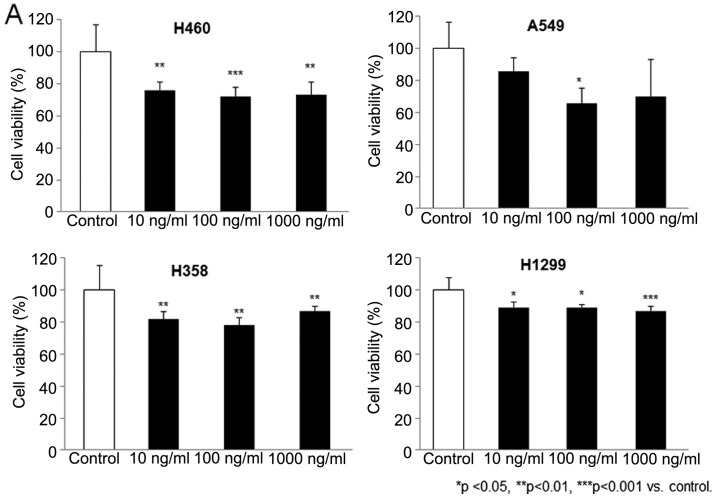
H460, A549, H1299 and H358 cells were treated in triplicate with tocilizumab at concentrations of 10, 100 and 1000 ng/ml. The inhibition of cell growth was examined by a commercial kit and an ELISA reading system after 24 h of treatment and was calculated as the percentage of viable cells relative to untreated cell cultures. As shown in Fig. 1A, tocilizumab demonstrated substantial growth inhibition in the NSCLC cells. Following exposure to tocilizumab at a 100 ng/ml concentration, cell growth was significantly decreased by 27.75±5.81, 34.23±9.49, 22.14±4.87 and 10.81±1.94% in the H460, A549, H1299 and H358 cells, respectively. In addition, the anti-proliferative effect of tocilizumab (100 ng/ml) was compared with that of the conventionally used anticancer drugs MTX and 5-FU in the NSCLC cells. The concentrations of MTX (50 mg/ml) and 5-FU (25 mg/ml) were based on those used in our previous study (12). MTX is a novel drug that acts as an inhibitor of folate metabolism, and 5-FU is an irreversible inhibitor of thymidylate synthase. These drugs have been used in the treatment of NSCLC patients for some time. As shown in Fig. 1B, the cell growth inhibition rate of tocilizumab in the NSCLC cells was similar or only slightly lower than that of MTX and 5-FU.
Figure 1.
Growth inhibitory activity of tocilizumab against non-small cell lung cancer cell lines: H460, A549, H1299 and H358 cells. The cells were treated with the indicated concentrations of tocilizumab for 24 h (A). The percent cell viability was determined by WST-1 assay. The anti-proliferative effect of tocilizumab was also compared with that of typical anticancer drugs methotrexate (MTX) and 5-fluorouracil (5-FU). (B) Data are expressed as the means ± SEM (n=4). *P<0.05, **P<0.01, ***P<0.001 vs. control.
Cell cycle distribution
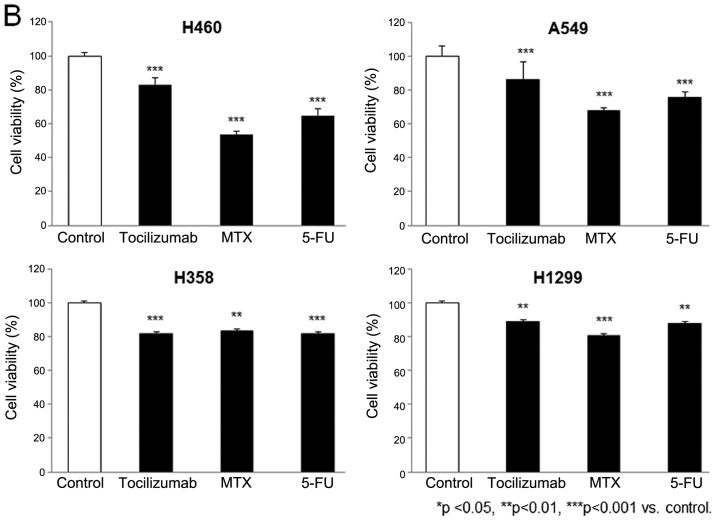
A flow cytometric cell cycle analysis was performed to determine whether the results of the cell assay reflected cytostatic or cytotoxic effects due to cell cycle arrest or apoptosis. NSCLC cells were treated with 100 ng/ml tocilizumab. After 24 h of drug treatment, the cells were fixed and suspended in PI and measured in comparison with untreated cells. Morphological changes in the apoptotic cells, including shrinkage, rounding and membrane blebbing, were also observed following the tocilizumab treatment. As shown in Fig. 2, a significant accumulation of the cell population in the sub-G1 phase was observed in the H460 and A549 cells following drug treatment. Similar effects on the cell cycle were observed with tocilizumab concentrations of 10 and 1000 ng/ml. Following tocilizumab treatment, 8.73% of the H460 cell population was arrested in the sub-G1 phase in contrast to 0.21% of the untreated control cells (Fig. 2A). In addition, 25.01% of the A549 cell population was in the sub-G1 phase following drug treatment, compared with only 1.74% of the untreated control cells (Fig. 2B). Although there was no significant difference in the H358 and H1299 cells between the treated and untreated groups, minor increases were observed following tocilizumab treatment: 1.73% of H358 cells were in the sub-G1 phase compared with 1.28% of the untreated control cells (Fig. 2C), and 3.64% of H1299 cells were in the sub-G1 phase compared with 2.34% of the untreated control cells (Fig. 2D).
Figure 2.
Effect of tocilizumab on cell cycle distribution in non-small cell lung cancer (NSCLC) cells. NSCLC cells H460, A549, H1299 and H358 were treated with 100 ng/ml tocilizumab for 24 h. The cell cycle distribution was analyzed by flow cytometry. The percentage of cells in the G0/G1, S and G2/M phases of the cell cycle are expressed as the means ± SEM (n=3). M1, sub-G1; M2, G0/G1; M3, S; M4, G2/M.
Gene expression and immunoblotting
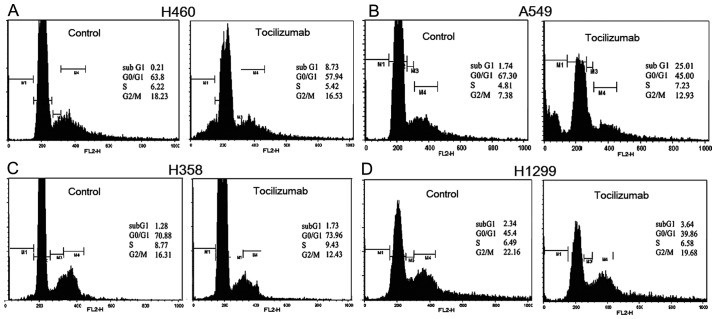
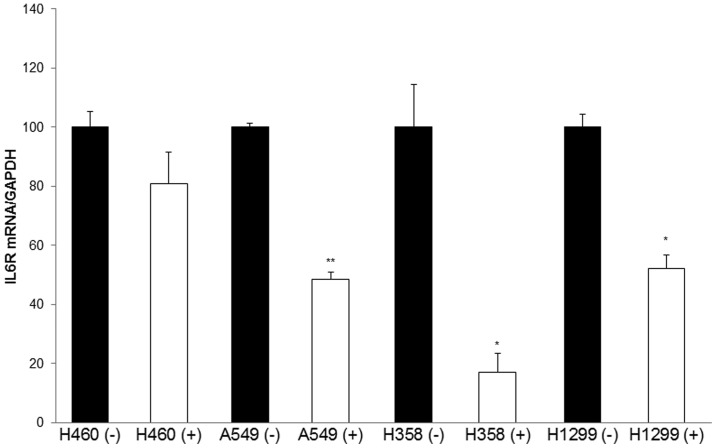
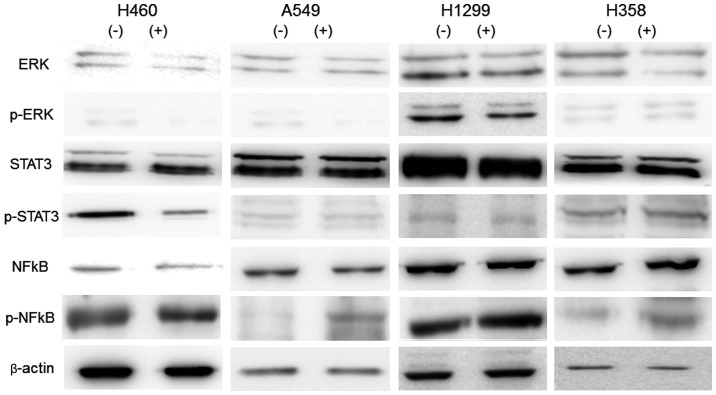
The mRNA expression of IL-6R was analyzed in H460, A549, H1299 and H358 cells using qPCR. The transcript levels were normalized to the expression of GAPDH. The data in Fig. 3 reveal marked decreases in IL-6R expression with tocilizumab at a concentration of 100 ng/ml. Tocilizumab significantly reduced the mRNA levels of IL-6R by 50% in A549, 77% in H358, 48% in H1299, and 20% in H460 cells. The principal transcriptional factors in the IL-6R/IL-6 signaling pathway regulating cell differentiation and growth are ERK1/2, STAT3 and NFκB. Thus, we estimated the influence of tocilizumab on the levels of activation of these factors in NSCLC cells. The cells were treated with 100 ng/ml tocilizumab, and protein lysates were obtained after 24 h of drug exposure. The levels of the transcription factors and their phosphorylated forms in whole-cell lysates were analyzed by western blotting using commercially available antibodies. As shown in Fig. 4, tocilizumab did not alter the levels of the proteins ERK1/2, STAT3 and NFκB and phosphorylated ERK1/2 and STAT3. However, phosphorylated NFκB was considerably increased by tocilizumab treatment in the NSCLC cells.
Figure 3.
Regulation of interleukin-6 receptor (IL-6R) mRNA levels in non-small cell lung cancer cells H460, A549, H358 and H1299 following tocilizumab treatment at 100 ng/ml. The mRNA levels were analyzed by quantitative polymerase chain reaction. GAPDH, glyceraldehyde-3-phosphate dehydrogenase; (+) tocilizumab treatment; (−) no tocilizumab treatment. *P<0.05 vs. the non-treated group, **P<0.01 vs. the non-treated group.
Figure 4.
Tocilizumab activates the nuclear factor κB (NFκB) pathway. Cell lysates were immunoblotted with antibodies against signal transducer and activator of transcription 3 (STAT3), phospho-STAT3 (p-STAT3), extracellular-signal-regulated kinases (ERK), phospho-ERK (p-ERK), nuclear factor κB (NFκB) and phospho-NFκB (p-NFκB). (+) Tocilizumab treatment; (−) no tocilizumab treatment.
Discussion
IL-6 plays a significant role in the neoplastic process through its action on cancer cell adhesion, motility, proliferation, tumor-specific antigen expression and thrombopoiesis (14). IL-6, with its known functions in immune response, acute phase reaction and hematopoiesis, was considered a therapeutic target approximately two decades ago. The aim of this study was to assess whether an anti-IL-6R antibody could be utilized as a new targeting molecule for NSCLC therapy. Another anti-IL-6 antibody, siltuximab, has been demonstrated to have potential benefits in the treatment of various human cancers, including multiple myeloma, breast cancer and prostate cancer, either as a single agent or in combination with other chemotherapy drugs (14–17). It has also been indicated that anti-IL-6R antibodies may be a potential agent for the suppression of colon cancer progression (18,19). These earlier investigations have revealed IL-6R as a potent target for antibody treatment in anticancer therapy. To our knowledge, there has been no study describing the utilization of an anti-IL-6/IL-6R antibody in NSCLC cancer therapy.
Tocilizumab is a fully humanized monoclonal antibody against IL-6R that was approved for the treatment of patients with rheumatoid arthritis (20). In Japan, tocilizumab has also been approved for the treatment of polyarticular-course juvenile idiopathic arthritis, systemic-onset juvenile idiopathic arthritis and Castleman's disease (21). However, this drug was initially investigated in the field of oncology. Mouse monoclonal antibodies against human IL-6 were noted to be effective in a patient with plasma cell leukemia (22). The mouse monoclonal antibody bound to the human IL-6R, inhibiting IL-6 function, and demonstrated strong antitumor cell activity against multiple myeloma cells (23). In our study, tocilizumab exhibited a significant growth inhibition in NSCLC cells (H460, A549, H1299 and H358), with proliferation significantly decreased by approximately 40% in A549 cells. The growth inhibition rates of tocilizumab in NSCLC cells were comparable with those of MTX and 5-FU, classically used anticancer drugs. This finding indicates that tocilizumab has a potent antitumor activity against NSCLC. Kudo et al (10) described the antitumor effect of tocilizumab in U87MG glioma cells and the critical role of the IL-6 signaling pathway in glioma cell proliferation. We further examined whether the result of our cell assay was a reflection of cytostatic or cytotoxic effects due to cell cycle arrest. Compared with the untreated control, tocilizumab treatment resulted in an approximate 40-fold increase in sub-G1 phase arrest in H460 cells and an approximately 14-fold increase in A549 cells. H358 and H1299 cells also exhibited approximately 1.3- and 1.5-fold increases, respectively, in the cell population in the sub-G1 phase. The statistical accumulation of the cell population in the sub-G1 phase demonstrates that significant apoptosis occurred in NSCLC cells following tocilizumab treatment.
The mRNA expression of IL-6R was analyzed in NSCLC cells. Tocilizumab significantly reduced the mRNA levels of IL-6R by 20–80%. Although we have no direct data for the downregulation of IL-6R at the protein level, the above results may indicate that tocilizumab has a regulatory function. It is known that ERK1/2, STAT3 and NFκB are involved in the signaling pathway of IL-6R/IL-6 as vital transcriptional factors in tumor proliferation (24). In our study, tocilizumab did not alter the levels of the ERK1/2, STAT3, NFκB and phosphorylated ERK1/2 and STAT3 proteins, but this antibody did considerably increase the expression of phosphorylated NFκB in NSCLC cells. This result indicates that the phosphorylation of NFκB may be an significant factor in the anti-proliferative activity of tocilizumab. NFκB is a key transcriptional regulator of genes involved in inflammatory responses as well as genes regulating cell proliferation and metastasis in carcinogenesis (25). NFκB is considered to function either as an inhibitor or an activator of apoptotic cell death. The nuclear accumulation and transcriptional activity of NFκB are increased in T-cell lymphoma cells and are responsible for their increased proliferation (26). However, evidence has also revealed a pro-apoptotic role for NFκB. Martin (27) emphasized the balance of NFκB activation with regard to pro-apoptotic and anti-apoptotic effects at the level of target gene activation. Although a number of phosphorylation sites on NFκB proteins have been characterized, it remains unclear how phosphorylation regulates the activities of related proteins and controls target gene expression (28).
Our study revealed the anti-proliferation potency of tocilizumab on NSCLC cells via apoptosis induction and IL-6R signaling alteration. Therefore, we suggest that the IL-6R antibody may be utilized as a new targeting molecule in NSCLC cancer therapies.
Acknowledgements
This paper was supported by Konkuk University in 2013.
References
- 1.Lam WK, Watkins DN. Lung cancer: future directions. Respirology. 2007;12:471–477. doi: 10.1111/j.1440-1843.2007.01105.x. [DOI] [PubMed] [Google Scholar]
- 2.Kishimoto T, Akira S, Narazaki M, Taga T. Interleukin-6 family of cytokines and gp130. Blood. 1995;86:1243–1254. [PubMed] [Google Scholar]
- 3.Hodge DR, Hurt EM, Farrar WL. The role of IL-6 and STAT3 in inflammation and cancer. Eur J Cancer. 2005;41:2502–2512. doi: 10.1016/j.ejca.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 4.Michalaki V, Syrigos K, Charles P, Waxman J. Serum levels of IL-6 and TNF-alpha correlate with clinicopathological features and patient survival in patients with prostate cancer. Br J Cancer. 2004;90:2312–2316. doi: 10.1038/sj.bjc.6601814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Plante M, Rubin SC, Wong GY, Federici MG, Finstad CL, Gastl GA. Interleukin-6 level in serum and ascites as a prognostic factor in patients with epithelial ovarian cancer. Cancer. 1994;73:1882–1888. doi: 10.1002/1097-0142(19940401)73:7<1882::AID-CNCR2820730718>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 6.Zhang GJ, Adachi I. Serum interleukin-6 levels correlate to tumor progression and prognosis in metastatic breast carcinoma. Anticancer Res. 1999;19:1427–1432. [PubMed] [Google Scholar]
- 7.Chung YC, Chang YF. Serum interleukin-6 levels reflect the disease status of colorectal cancer. J Surg Oncol. 2003;83:222–226. doi: 10.1002/jso.10269. [DOI] [PubMed] [Google Scholar]
- 8.Ohsugi Y, Kishimoto T. The recombinant humanized anti-IL-6 receptor antibody tocilizumab, an innovative drug for the treatment of rheumatoid arthritis. Expert Opin Biol Ther. 2008;8:669–681. doi: 10.1517/14712598.8.5.669. [DOI] [PubMed] [Google Scholar]
- 9.Bongartz T. Tocilizumab for rheumatoid and juvenile idiopathic arthritis. Lancet. 2008;371:961–963. doi: 10.1016/S0140-6736(08)60428-6. [DOI] [PubMed] [Google Scholar]
- 10.Kudo M, Jono H, Shinriki S, Yano S, Nakamura H, Makino K, Hide T, Muta D, Ueda M, Ota K, et al. Antitumor effect of humanized anti-interleukin-6 receptor antibody (tocilizumab) on glioma cell proliferation. Laboratory investigation. J Neurosurg. 2009;111:219–225. doi: 10.3171/2008.12.JNS081284. [DOI] [PubMed] [Google Scholar]
- 11.Haura EB, Livingston S, Coppola D. Autocrine interleukin-6/interleukin-6 receptor stimulation in non-small-cell lung cancer. Clin Lung Cancer. 2006;7:273–275. doi: 10.3816/CLC.2006.n.006. [DOI] [PubMed] [Google Scholar]
- 12.Yi H, Cho HJ, Cho SM, Jo K, Park JA, Kim NH, Amidon GL, Kim JS, Shin HC. Blockade of interleukin-6 receptor suppresses the proliferation of H460 lung cancer stem cells. Int J Oncol. 2012;41:310–316. doi: 10.3892/ijo.2012.1447. [DOI] [PubMed] [Google Scholar]
- 13.Koyama Y, Mitsui N, Suzuki N, Yanagisawa M, Sanuki R, Isokawa K, Shimizu N, Maeno M. Effect of compressive force on the expression of inflammatory cytokines and their receptors in osteoblastic Saos-2 cells. Arch Oral Biol. 2008;53:488–496. doi: 10.1016/j.archoralbio.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Jiang XP, Yang DC, Elliott RL, Head JF. Down-regulation of expression of interleukin-6 and its receptor results in growth inhibition of MCF-7 breast cancer cells. Anticancer Res. 2011;31:2899–2906. [PubMed] [Google Scholar]
- 15.Yao X, Huang J, Zhong H, Shen N, Faggioni R, Fung M, Yao Y. Targeting interleukin-6 in inflammatory autoimmune diseases and cancers. Pharmacol Ther. 2014;141:125–139. doi: 10.1016/j.pharmthera.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Fizazi K, De Bono JS, Flechon A, Heidenreich A, Voog E, Davis NB, Qi M, Bandekar R, Vermeulen JT, Cornfeld M, Hudes GR. Randomised phase II study of siltuximab (CNTO 328), an anti-IL-6 monoclonal antibody, in combination with mitoxantrone/prednisone versus mitoxantrone/prednisone alone in metastatic castration-resistant prostate cancer. Eur J Cancer. 2012;48:85–93. doi: 10.1016/j.ejca.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Hunsucker SA, Magarotto V, Kuhn DJ, Kornblau SM, Wang M, Weber DM, Thomas SK, Shah JJ, Voorhees PM, Xie H, et al. Blockade of interleukin-6 signalling with siltuximab enhances melphalan cytotoxicity in preclinical models of multiple myeloma. Br J Haematol. 2011;152:579–592. doi: 10.1111/j.1365-2141.2010.08533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu CP, Chen YL, Huang CC, Chou CC, Liu CL, Hung CH, Kao TY, Chung YC. Anti-interleukin-6 receptor antibody inhibits the progression in human colon carcinoma cells. Eur J Clin Invest. 2011;41:277–284. doi: 10.1111/j.1365-2362.2010.02405.x. [DOI] [PubMed] [Google Scholar]
- 19.Schneider MR, Hoeflich A, Fischer JR, Wolf E, Sordat B, Lahm H. Interleukin-6 stimulates clonogenic growth of primary and metastatic human colon carcinoma cells. Cancer Lett. 2000;151:31–38. doi: 10.1016/S0304-3835(99)00401-2. [DOI] [PubMed] [Google Scholar]
- 20.Yilmaz S, Simsek I. Early intervention in the treatment of rheumatoid arthritis: focus on tocilizumab. Ther Clin Risk Manag. 2013;9:403–408. doi: 10.2147/TCRM.S35784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oldfield V, Dhillon S, Plosker GL. Tocilizumab: a review of its use in the management of rheumatoid arthritis. Drugs. 2009;69:609–632. doi: 10.2165/00003495-200969050-00007. [DOI] [PubMed] [Google Scholar]
- 22.Klein B, Wijdenes J, Zhang XG, Jourdan M, Boiron JM, Brochier J, Liautard J, Merlin M, Clement C, Morel-Fournier B, et al. Murine anti-interleukin-6 monoclonal antibody therapy for a patient with plasma cell leukemia. Blood. 1991;78:1198–1204. [PubMed] [Google Scholar]
- 23.Sato K, Tsuchiya M, Saldanha J, Koishihara Y, Ohsugi Y, Kishimoto T, Bendig MM. Reshaping a human antibody to inhibit the interleukin 6-dependent tumor cell growth. Cancer Res. 1993;53:851–856. [PubMed] [Google Scholar]
- 24.Stärkel P, Charette N, Borbath I, Schneider-Merck T, De Saeger C, Abarca J, Leclercq I, Horsmans Y. Ras inhibition in hepatocarcinoma by S-trans-trans-farnesylthiosalicyclic acid: association of its tumor preventive effect with cell proliferation, cell cycle events and angiogenesis. Mol Carcinog. 2012;51:816–825. doi: 10.1002/mc.20849. [DOI] [PubMed] [Google Scholar]
- 25.Sorriento D, Illario M, Finelli R, Iaccarino G. To NFκB or not to NFκB: The Dilemma on How to Inhibit a Cancer Cell Fate Regulator. Transl Med UniSa. 2012;4:73–85. [PMC free article] [PubMed] [Google Scholar]
- 26.Chang TP, Vancurova I. NFκB function and regulation in cutaneous T-cell lymphoma. Am J Cancer Res. 2013;3:433–445. [PMC free article] [PubMed] [Google Scholar]
- 27.Martin AG. NFκB anti-apoptotic or pro-apoptotic, maybe both. Cell Cycle. 2010;9:3131–3132. doi: 10.4161/cc.9.16.12780. [DOI] [PubMed] [Google Scholar]
- 28.Viatour P, Merville MP, Bours V, Chariot A. Phosphorylation of NF-kappaB and IkappaB proteins: implications in cancer and inflammation. Trends Biochem Sci. 2005;30:43–52. doi: 10.1016/j.tibs.2004.11.009. [DOI] [PubMed] [Google Scholar]