Abstract
Sudden unexplained death in epilepsy (SUDEP) is the cause of premature death of up to 17% of all patients with epilepsy and as many as 50% with chronic refractory epilepsy. However, SUDEP is not widely recognized to exist. The etiology of SUDEP remains unclear, but growing evidence points to peri-ictal respiratory, cardiac, or autonomic nervous system dysfunction. How seizures affect these systems remains uncertain. Here we focus on respiratory mechanisms believed to underlie SUDEP. We highlight clinical evidence that indicates peri-ictal hypoxemia occurs in a large percentage of patients due to central apnea, and identify the proposed anatomical regions of the brain governing these responses. In addition, we discuss animal models used to study peri-ictal respiratory depression. We highlight the role 5-HT neurons play in respiratory control, chemoreception, and arousal. Finally, we discuss the evidence that 5-HT deficits contribute to SUDEP and sudden infant death syndrome and the striking similarities between the two.
1. Introduction
Estimates suggest that up to 6 people die each day in the U.S. of SUDEP, a devastating condition afflicting patients with epilepsy (Shorvon and Tomson, 2011; Thurman, 2011). In most cases, individuals are healthy (excluding the diagnosis of epilepsy), but are unexpectedly found dead, often in the prone position in bed with evidence of a recent seizure. For such a major public health concern, it is surprising that SUDEP remains largely unknown to the general public and, more alarmingly, to many clinicians. According to a recent report, only 56% of Canadian pediatricians who care for epilepsy patients knew that children with epilepsy were at an increased risk of sudden death, and only 33% knew of the term SUDEP (Donner et al., 2012), indicating a critical need for increased education.
SUDEP is defined as “the sudden, unexpected, witnessed or unwitnessed, non-traumatic, and non-drowning death of patients with epilepsy with or without evidence of a seizure, excluding documented status epilepticus, and in which postmortem examination does not reveal a structural or toxicological cause of death” (Nashef, 1997). There are three classifications of SUDEP: first is definite SUDEP, which adheres to the aforementioned definition; second is probable SUDEP where there is no post-mortem examination but the other criteria for SUDEP are met; and finally possible SUDEP in which there are competing causes of death but SUDEP cannot be ruled out.
It is becoming apparent that SUDEP is much more common than previously recognized, but it has been difficult to obtain precise estimates of its incidence. There are many epidemiological studies on SUDEP, but these were done among different populations of patients with different types and severity of seizures making them difficult to compare. The reported rates cover a wide range from 0.09 per 1000 person years among unselected incident cases of epilepsy to 9.3 per 1000 person years among epilepsy surgery candidates (Shorvon and Tomson, 2011). The life time risk of SUDEP ranges from 10-17% in all epilepsy patients to 10-50% in chronic refractory epilepsy patients (Ficker, 2000; Shorvon and Tomson, 2011).
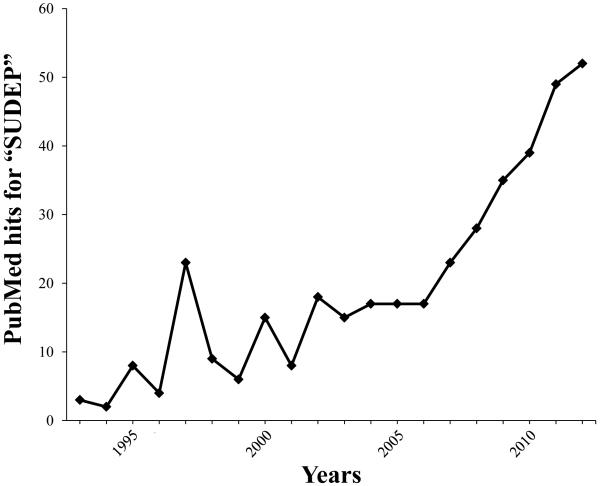
One recent estimate suggests that the annual incidence of SUDEP in refractory epilepsy patients (which make up one-third of all epilepsy patients) is 1/1000 which translates into about 2000-3000 deaths per year in the U.S. (Thurman, 2011). When this incidence is compared to other major neurological disorders (Alzheimer’s disease and stroke each occur at a rate of about 70,000-80,000 deaths per year in the U.S.), SUDEP is relatively uncommon. However, the peak incidence of death for SUDEP is 30 years, so when quantified as years of potential life lost, SUDEP accounts for 73,000 years lost, second only to stroke among neurological disease (Thurman, 2011). From a public health perspective SUDEP is a major problem, yet this has only recently resulted in increased research into the mechanisms of SUDEP. For example, there were only 4 publications in 1993 (Fig. 1) that appeared in a Pubmed search using the term SUDEP. In 2012 there were >50 publications that used SUDEP, showing a significant increase in interest in studying this syndrome (Fig. 1).
Figure 1. SUDEP research is growing at a rapid pace.
In 1993 there were few publications that appeared in a PUBMED search using the term SUDEP. However, in 2012 there was greater than 50 publications with SUDEP in the title. This graph highlights the increased attention SUDEP research has recently received.
Although research on SUDEP has recently begun to expand, many fundamental questions remain unanswered. What are the risk factors for SUDEP? What are the pathophysiological mechanisms underlying SUDEP? How do we effectively study SUDEP in epilepsy patients, and how representative of the human condition are animal models of SUDEP that are utilized for research? How can respiratory physiologists contribute to this field? Are there ways to prevent SUDEP or definitively diagnose it when it does occur? Moreover, there is a crucial need to better standardize research methods from bench to bedside so that definitive conclusions can be made about SUDEP. With increased research and awareness of SUDEP, it is likely that many cases can be prevented.
There have been many risk factors proposed for SUDEP, including: poor compliance with antiepileptic medications, young age at onset of seizures, chronic refractory epilepsy, male sex, and sleeping in the prone position (Shorvon and Tomson, 2011; Thurman, 2011). The most consistent risk factor for SUDEP is the frequency of generalized tonic clonic seizures (GTCS) (Hesdorffer et al., 2011). However, patients who do not experience any GTCS remain at considerably higher risk than the general population. Many of these risk factors are inconsistently reported throughout the literature, highlighting a need to better understand the underlying mechanisms of SUDEP. It is beyond the scope of this review to fully describe all potential mechanisms of SUDEP. Therefore, we will briefly describe cardiac and postictal generalized electroencephalogram (EEG) suppression (PGES), then concentrate on the potential respiratory mechanisms underlying SUDEP for this special issue of Respiratory Physiology and Neurobiology. Furthermore, we highlight the need for a codified methodology for studying SUDEP, in order to appropriately understand this condition.
2. Potential pathophysiological mechanisms in SUDEP
It is important to remember that there are only two ways to die, either you stop breathing or your heart stops. If one occurs then the other is soon to follow. There are many different ictal events that could potentially lead to one of these two outcomes in SUDEP. For example, there is good evidence that seizures can sometimes induce arrhythmias or peri-ictal respiratory depression. Research to date indicates all SUDEP is not caused by a single mechanism, but that different mechanisms can occur in different people. These mechanisms can then cause death by inducing cardiac or respiratory dysfunction or both.
3.1 Cardiac dysfunction in SUDEP
Peri-ictal cardiac dysfunction is thought to play a role in a subset of SUDEP cases (Brotherstone et al., 2010; Neufeld et al., 2009; Surges et al., 2010a; Surges et al., 2010b; Surges et al., 2010c; Surges and Walker, 2010). Tachycardia is the most common ictal autonomic event. In one study of 76 patients tachycardia occurred in 57% of seizures and in 76% of patients at least once, and was significantly correlated with seizure generalization (Rowe, 1987). Seizures can also induce peri-ictal bradycardia or asystole (Lee, 1998; So et al., 2000). Although case studies report a frequent occurrence of post-ictal bradycardia with asystole, in one study patients monitored in an EMU displayed bradycardia in only 2% of seizures (Moseley et al., 2010; Rowe, 1987). Asystole was even more rare, with a rate less than 0.5% (Moseley et al., 2010; Rowe, 1987). In a study of 56 patients with 250 recorded seizures, there was only one episode of ictal bradycardia with asystole. That event was associated with oxygen desaturation below 50% (Bateman et al., 2008), which can be assumed to be due to hypoventilation. Since respiratory monitoring was not done it is not known if the respiratory dysfunction, such as central apnea, was the primary event and asystole was then secondary to the resulting hypoxemia, but that is the most likely scenario. Although some reports give the perception that primary cardiac dysfunction causes a large percentage of SUDEP deaths, the studies described above and others suggest that severe cardiac dysfunction as a primary event actually occurs at a much lower rate (Moseley et al., 2010; Rowe, 1987).
An area of considerable emphasis in SUDEP research is long QT syndrome (LQTS) and the genes underlying that disorder. Mutations in more than 10 different genes cause LQTS (Goldenberg and Moss, 2008). These mutations affect ion channels expressed throughout the body and typically cause a long QT interval in the electrocardiogram (EKG) (Goldenberg and Moss, 2008). This prolonged QT interval can lead to cardiac arrhythmias and sudden death in patients without epilepsy (Goldenberg and Moss, 2008). However, some patients with epilepsy carry these LQTS gene mutations (e.g. KCNH2) and some of those patients have a higher rate of SUDEP (Le Gal et al., 2010). Thus, LQTS gene mutations increase the risk of SUDEP (Goldman et al., 2009). However, every patient with a mutation in one of these genes who dies did not necessarily have a fatal cardiac arrhythmia. Many of the LQTS genes are expressed in both the heart and brain (Cheah et al., 2012; Goldman et al., 2009; Holth et al., 2013), and a mutation in one of them could potentially affect breathing or other vital brain functions. For example, KCNQ1 is expressed in brain stem nuclei that are important for autonomic control of heart rate (Goldman et al., 2009). It is not known how many of these genes are expressed in respiratory nuclei; however, mouse models of LQTS have high rates of spontaneous sudden death (Cheah et al., 2012; Holth et al., 2013). Dravet syndrome is another area of interest in SUDEP research. Patients with SCN1A mutations have cardiac abnormalities and seizures in addition to an increased incidence of sudden death (Genton et al., 2011).
Overall, there is strong evidence highlighting the role of cardiac dysfunction in SUDEP. However, it is important to note that patients who display cardiac abnormalities are significantly more likely to have hypoxemia during seizures (Rowe, 1987; Seyal et al., 2011). It is also important to note that breathing was not recorded during many of the case reports and other studies. Therefore, it is possible that in some cases, respiratory dysfunction could be the primary event that causes secondary effects on the heart that then lead to sudden death. Moreover, patients with LQTS mutations may have subtle respiratory dysfunction made worse during seizures. Alternatively, other patients may have mutations that make them more susceptible to cardiac abnormalities when hypoxia occurs. Peri-ictal cardiac abnormalities need more thorough investigation in order to determine their role in SUDEP.
3.2 Postictal generalized EEG suppression and SUDEP risk
PGES is marked post-ictal flattening of the EEG. It was originally proposed as an “identifiable EEG marker of profound postictal cerebral dysfunction”, and it is hypothesized that PGES could contribute to SUDEP through inhibition of brainstem dysfunction including the cardiorespiratory centers (Lhatoo et al., 2010). A recent study examined 10 cases of SUDEP and found that PGES length is directly correlated with the incidence of SUDEP (Lhatoo et al., 2010). However, a second study found no correlation between PGES duration and SUDEP risk (Surges et al., 2011). Although PGES was recently linked to seizure-associated respiratory function, there was no correlation with post-ictal apnea (Seyal et al., 2012). Furthermore, PGES is not associated with peri-ictal cardiac autonomic instability measured by heart rate in people with convulsive seizures (Lamberts et al., 2012). Thus, there is conflicting evidence on the importance of PGES, and although it is a common occurrence after generalized tonic clonic seizures, it is not believed to cause SUDEP. Instead it may be an EEG marker of some other brain process that underlies depression of cardiorespiratory output. For example, it may signify that there is severe depression of monoamine release by the ascending arousal system, and this could then lead to both postictal coma and peri-ictal cardiorespiratory depression.
3.3 Respiratory control in SUDEP
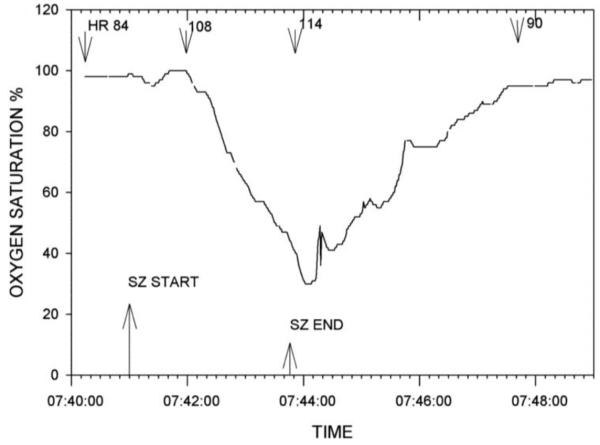
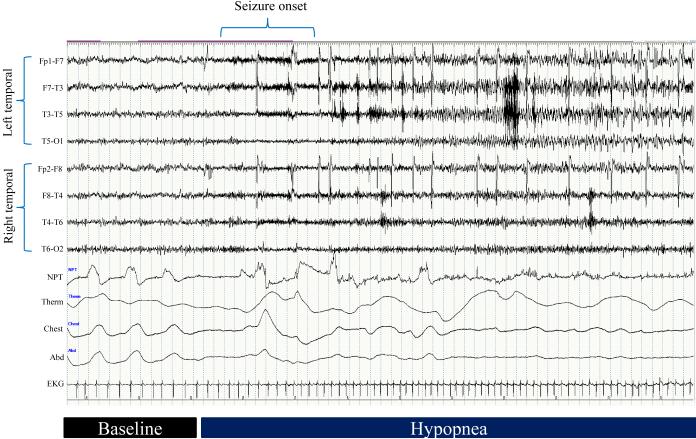
Respiratory abnormalities in epilepsy patients were first reported in 1899, when Hughlings Jackson noted his human patients and monkeys “turning blue” during seizures (Jackson, 1899). Many reports have confirmed what Jackson observed in 1899 (James et al., 1991; Watanabe et al., 1982). For example, Nashef (Nashef et al., 1996) used long term EEG monitoring and respiratory recordings to show that 10 of 17 patients (59%) had apnea concurrent with their seizures. A separate study showed that 10% of generalized seizures caused oxygen desaturation, whereas an even greater 60% of partial seizures caused oxygen desaturation (Blum et al., 2000). Oxygen desaturation during partial seizures can be very severe (Fig. 2) (Bateman et al., 2008). A large study investigated 304 seizures in 56 patients with intractable localization-related epilepsy and reported that oxygen saturation drops below 90% in 33.2% of seizures, below 80% in 10.2% of seizures, and below 70% in 3.6% of seizures (Bateman et al., 2008). This study found apnea is as common during partial seizures as during seizures that secondarily generalized; with 34% of partial seizures showing oxygen desaturation below 90%. Furthermore, they showed that seizure duration is highly correlated with oxygen saturation (Bateman et al., 2008). Studies performed in the University of Iowa EMU confirmed that peri-ictal hypopnea can be severe during partial seizures (Fig. 3). These clinical studies indicate that peri-ictal respiratory dysfunction is common in individuals with epilepsy; much more common than previously realized among neurologists, including those specializing in epilepsy.
Figure 2. PO2 levels can drop dramatically during partial seizures.
Oxygen saturation drops below 40% in a 19-year-old male patient. The patient was awake and sitting in bed during the hypoxic event. Seizure duration is marked by bottom arrows. Heart rate is marked by the upper arrows and beats per minute are given. Modified with permission from Bateman et al. (2008). Bateman L M et al. Brain 2008;131:3239-324
Figure 3. Hypopnea during a complex partial seizure.
This 60 second trace showing respiratory depression related to complex partial seizures in a 67 year old woman with epilepsy. Three of her habitual episodes—consisting of behavioral arrest with mouth movements—were recorded on video-EEG monitoring. All three events were associated with significant respiratory depression characterized by hypopneas and oxygen desaturation as low as 40%. NPT = nasal pressure transducer; Therm = oral/nasal thermisty; Chest = chest movement by respiratory inductance plethysmography; Abd = abdominal movement by respiratory inductance plethymography; EKG = electrocardiogram.
There are a few reported cases of SUDEP or near SUDEP in hospital EMUs (Bateman et al., 2010b; Bird, 1997; Dasheiff Rm, 1986; Lee HW, 1999; McLean and Wimalaratna, 2007), which have provided us the most relevant information available about the mechanisms of death. However, even in these rare cases, although it has been common to make firm conclusions about the causes of death (Tomson et al., 2008), the actual cause of death is not completely clear in many cases, because breathing was assessed solely by visual inspection, a method that is notoriously inaccurate for measurement of ventilation. For example, there can be extreme hypoventilation in the presence of chest wall movements due to paradoxical breathing, airway obstruction, shallow breathing, etc., and these can lead to blood gas abnormalities as severe as those seen with frank apnea. Given the small number of cases of SUDEP in which there were direct measurements of the terminal events including breathing, the mechanisms remain poorly understood. There is a crucial need to understand if peri-ictal cardiac and respiratory dysfunction are usually separate entities, or if they often act together to cause sudden death.
3. From temporal lobe to the respiratory network: pathway to SUDEP
Intracranial stimulation in humans and other species has defined the role certain brain regions play in ventilatory control. In the late 19th century Spencer showed that stimulation of regions near the uncus in different species induces apnea (Spencer, 1894). By the middle of the 20th century, Chapman (Chapman, 1949) showed that stimulation of the orbital surface of the frontal cortex can result in respiratory depression. Stimulating different regions in the temporal lobe of primates also leads to respiratory depression (Kaada and Jasper, 1952). In addition, mechanical and electrical stimulation of the anterior portion of the hippocampal gyrus produces respiratory depression (Kaada and Jasper, 1952); remarkably, mechanical stimulation of the hippocampus leads to cessation of breathing in humans that lasts up to 56 seconds (Kaada and Jasper, 1952). Stimulation of specific nuclei in the amygdala can also lead to diverse alterations in respiration (Bonvalle and Bobo, 1972). Stimulation of the central nucleus of the amygdala induces apnea with a slow return to eupnea in cats (Bonvalle and Bobo, 1972). Conversely, stimulation of the basal and lateral nucleus of the amygdala in cats increases respiratory output (Bonvalle and Bobo, 1972). These data demonstrate that there are regions in the forebrain that modulate central control of breathing. Apnea and hypoventilation, with accompanying oxygen desaturation, is most commonly induced by partial seizures that originate in the temporal lobe (Blum, 2009). Oxygen desaturation is also common when the seizure focus is in the temporal lobe, but not when seizures originate outside of the temporal lobe (Seyal and Bateman, 2009).
These data indicate that anatomical pathways connecting the temporal lobe to brainstem respiratory centers are capable of causing respiratory arrest. Activation of these pathways by a seizure could be a mechanism to induce apnea severe enough to cause SUDEP. Projections from temporal lobe structures connect to the respiratory centers, as well as to the periaqueductal grey which modulates breathing (Hopkins and Holstege, 1978; Subramanian et al., 2008). Direct projections from the central nucleus of the amygdala extend to the nucleus of the solitary tract (NTS) and dorsal motor nucleus of the vagus, and are thought to cause cardiorespiratory changes (Schwaber et al., 1980; Schwaber et al., 1982; Veening et al., 1984). Moreover, neurons in the central nucleus fire in phase with the respiratory rhythm in cats (Harper et al., 1984). These data suggest that abnormal firing of neurons in the amygdala could play a role during peri-ictal respiratory depression.
4. Animal models of peri-ictal respiratory depression
Animal models that recapitulate human SUDEP phenotypes are vital in order to understand the underlying mechanisms. Utilizing current animal models of SUDEP and discovering new animal models will begin to shed light onto the molecular and anatomical pathways involved. In this section, we will discuss current and potential animal models of SUDEP, specifically highlighting mouse models.
DBA/2 mice are a well-established mouse model of audiogenic seizures. When exposed to a 120db tone, DBA/2 mice have a seizure with tonic extension followed by respiratory arrest (Venit et al., 2004). These animals can be resuscitated after seizures using a ventilator, and once resuscitated, eupnea resumes (Purpura, 1972) indicating death is likely due to respiratory failure. DBA/2 mice are genetically predisposed to respiratory failure following seizure activity, and are currently one the most widely accepted mouse models of SUDEP. Moreover, their genetic predisposition to post-ictal respiratory depression indicates that there are possible genetic predictors of SUDEP.
In a commonly cited study, induction of status epilepticus in sheep leads to a death rate of about 38% (Johnston et al., 1997). These sheep do not die from cardiac dysfunction, but display severe ictal and post-ictal central apnea leading to a significant drop in PO2 and an increase in PCO2 followed by death (Johnston et al., 1997). This model shows severe post-ictal apnea and death, and is commonly invoked as a model of SUDEP. However, this is misleading because it does not meet the definition of SUDEP since the sheep were in status epilepiticus.
LQTS genes were briefly discussed above as being important in heart function. However, it is known that these genes are also expressed in the brain, and it is possible they play a role in control of breathing. Recently, KCNQ channels were reported to play a central role in the detection of CO2 in the NTS (Hawryluk et al., 2012). Many other LQTS genes that cause cardiac dysfunction are also expressed at high levels in the brain and are present in respiratory nuclei. For example, KCNQ 1, 2, and 3 are expressed in the NTS (Goldman et al., 2009; Tolstykh GP, 2010; Tolstykh GP, 2008). Alhough cardiac mechanisms have been proposed to underlie SUDEP in a genetic mouse model with KCNQ1 mutations (Goldman et al., 2009), simultaneous plethysmography recordings were not recorded with these cardiac events. Therefore, it is not possible to rule out respiratory dysfunction as being the primary mechanism of sudden death in these mice. Dravet syndrome mice, with mutations in the gene for the Na+-channel SCN1A, also have a high risk of sudden death (Cheah et al., 2012). The mechanism of death in these mice is not an arrhythmia. Marked bradycardia was observed and was attributed to massive parasympathetic output (Kalume et al., 2013). However, recordings of respiratory output were not made so it is not known whether hypoventilation could have contributed to the cause of death. These data suggest that LQTS genes could play a role in respiration, and mutations in these genes as well as SCN1A could lead to breathing dysfunction. It is vital to understand their function in respiratory nuclei.
Maximal electroshock (MES) has been used to study seizures for more than 70 years (Toman et al., 1946). Like DBA/2 mice after induction of AGS, MES induces seizures in other mouse strains (e.g. C57BL/6) with tonic extension and occasionally death. However, the mechanisms of death in MES have yet to be characterized. It is possible that this model does not recapitulate SUDEP since these mice are not epileptic. However, if the mechanisms of death can be defined, MES could be a tool used to study SUDEP.
Some mouse models of Alzheimer’s disease have epilepsy and also show a high rate of sudden death (Roberson et al., 2011). Recent reports indicate an increased comorbidity of epilepsy and Alzheimer’s. Given the high rate of death, it is imperative to understand sudden death in Alzheimer’s mouse models (Noebels, 2011). Another intriguing mouse model of respiratory arrest after seizures is the 5-HT2C receptor null mouse. Like DBA/2 mice, 5-HT2C receptor null mice have AGS with post-ictal respiratory arrest and death (Brennan et al., 1997). DBA/2 and 5-HT2C mice provide two separate pieces of evidence that 5-HT neurons can alter the risk of SUDEP.
5. The link between 5-HT and SUDEP
All 5-HT in the brain comes from a select group of neurons primarily found in the midbrain and medullary raphé nuclei. Although the number of neurons is small, they project to virtually every part of the CNS. 5-HT alters a myriad of brain functions, including: arousal, thermoregulation, circadian rhythms, anxiety, pain, aggression, central chemoreception, and respiratory control. One of the most vital functions of the 5-HT system is the control of breathing. Over the past decade, it was thought that 5-HT played a modulatory role in breathing (Hodges and Richerson, 2008; Lalley, 1986). However, 5-HT neurons have now been shown to indisputably stimulate respiratory output (Depuy et al., 2011; Ptak et al., 2009). They are also part of the ascending arousal system (previously referred to as the reticular activating system). Given that the 5-HT system stimulates respiration and arousal, a defect in this system could contribute to the mechanisms of sudden death after seizures, in which there is depression of consciousness and breathing.
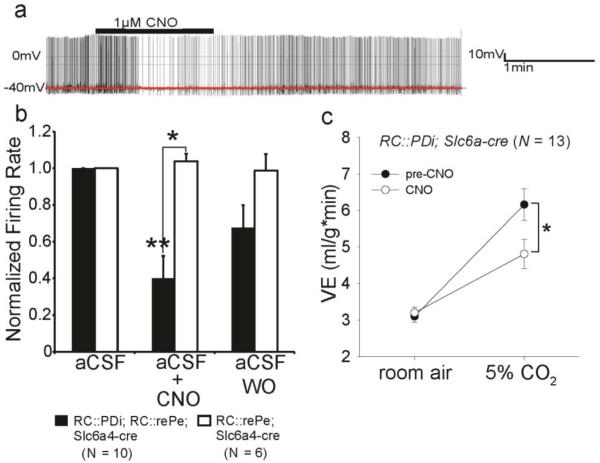
There are excitatory inputs from 5-HT neurons to the respiratory nuclei of the brainstem, and 5-HT2A receptor activation is needed in brain slices containing the pre-B□tzinger complex (PBC) to produce respiratory output (Pena and Ramirez, 2002; Ptak et al., 2009). Furthermore, 5-HT is required to induce bursting pacemaker activity in a subset of neurons in the PBC (Ptak et al., 2009). A subset of 5-HT neurons produce thyrotropin-releasing hormone (TRH), which is critical for bursting pacemaker activity in the NTS and is a strong stimulus for breathing (Dekin et al., 1985; Hedner et al., 1983). Nonselective agents, such as muscimol and ibotenic acid, injected into the raphé nuclei disrupt 5-HT neurons and depress respiratory output (Hodges et al., 2004b; Messier et al., 2002). Lmx1bf/f/p mice, in which virtually all 5-HT neurons are deleted due to genetic manipulation of a transcription factor, Lmx1b, critical for development of 5-HT neurons, have apneic breathing and high mortality as neonates (Hodges et al., 2009a) and a severely blunted hypercapnic ventilatory response (HCVR) as adults (Hodges et al., 2008). Furthermore, acute 5-HT neuron inhibition using DREADD receptors results in a ~50% reduction in 5-HT neuron firing rate, and a similar reduction in the HCVR (Fig. 4) (Ray et al., 2011). Conversely, administration of the 5-HT2A/1C agonist 1-[2,3-dimethoxy-4-iodophenyl]-2-aminopropane (DOI) increases respiratory output in Lmx1bf/f/p mice and reduces neonatal mortality (Hodges et al., 2009b).
Figure 4. Acute silencing of 5-HT neurons leads to decreased 5-HT neuron chemosensitivity in vitro and an impaired HCVR in vivo.
a) Recordings of cultured medullary serotonergic neurons from RC::PDi; RC::rePe; Slc6a4-cre mice show that CNO leads to ~50% suppression of action potential firing or abolishment (not shown) in 5-HT neurons. b) Peak firing rates (normalized to baseline) in aCSF were suppressed with CNO application in RC::PDi; RC::rePe; Slc6a4-cre neurons. c) Mice had a normal increase in ventilation in response to 5% CO2 prior to CNO administration; however, after an IP injection of CNO, these same mice had a blunted HCVR. Modified with permission for Ray et al. 2011. From Ray RS, Corcoran AE, Brust RD, Kim JC, Richerson GB, Nattie E, et al. Impaired respiratory and body temperature control upon acute serotonergic neuron inhibition. Science. 2011;333(6042):637-42. Reprinted with permission from AAAS. Modified with permission from the author.
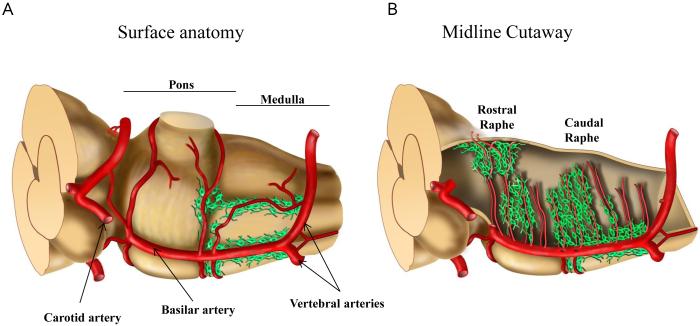
Medullary 5-HT neurons have many properties consistent with central respiratory chemoreceptors. These neurons are located close to the basilar artery and its associated branches (Fig. 5) (Bradley et al., 2002), which allows for accurate monitoring of blood PCO2. In fact, 5-HT neurons throughout the brainstem are found near large arteries, including in the midbrain. Interestingly, the dorsal raphe is located in the only part of the brain that receives arterial supply from branches of the carotid arteries and also the vertebrobasilar system. 5-HT neurons are chemosensitive to small changes in pH in the physiological range (7.4 to 7.2) (Corcoran et al., 2009; Richerson, 1995; Wang et al., 1998; Wang et al., 2001) and focal acidosis in the raphé nuclei increases ventilation in vivo (Bernard et al., 1996; Feldman et al., 2003; Hodges et al., 2004a). Moreover, extracellular recordings from the medullary and midbrain raphé nuclei in awake and behaving cats show a subset of 5-HT neurons increase their firing in response to increased inhaled CO2 (Veasey et al., 1995, 1997). Increased firing of 5-HT neurons stimulates respiratory output (Depuy et al., 2011; Ptak et al., 2009). These and other data provide evidence for an important role for 5-HT neurons in respiratory chemoreception (Richerson, 2004).
Figure 5. Serotonergic neurons throughout the brainstem are located next to large arteries.
Illustration of 5-HT neuron distribution in the medulla. (a) Surface anatomy: 5-HT neurons are adjacent to the basilar artery in the medulla. (b) Midline cutaway: 5-HT neurons surround and are closely associated with penetrating branches off of the basilar artery putting them in perfect position to detect changes in blood PH.
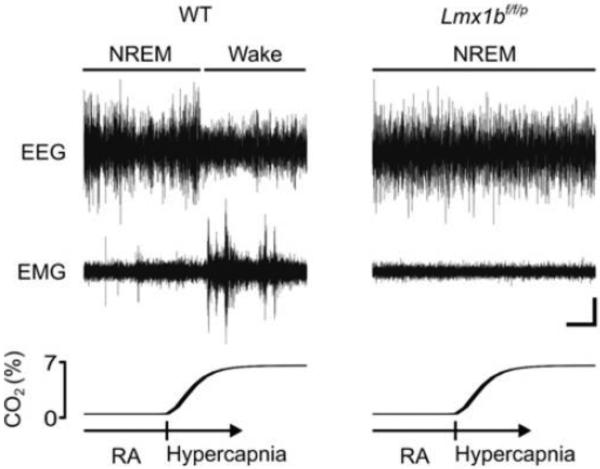
The rostral domain of 5-HT neurons is located in the midbrain. These neurons are also chemosensitive to CO2 (Severson et al., 2003). They are believed to also be central chemoreceptors, but rather than stimulating breathing, they are thought to induce arousal in response to increased arterial PCO2 during sleep. Lmx1bf/f/p mice (with 5-HT neurons deleted) have suppression of a hypercapnic arousal response, and in fact some mice sleep through the entire hypercapnic challenge, whereas this never occurs with WT mice (Fig. 6) (Buchanan and Richerson, 2010). This defect in arousal could be a critical factor in SUDEP. One possible SUDEP scenario is that a patient has a defect in arousal coupled with a blunted HCVR. After he has a seizure and is post-ictal, he would be unresponsive when a blanket or pillow obstructs the airway. He would fail to wake up to relieve the obstruction and ventilation would also not increase. The result would be hypercapnia, hypoxemia and death. Most SUDEP patients are found prone in bed (Kloster and Engelskjon, 1999), which is consistent with this critical pathophysiological mechanism in SUDEP cases.
Figure 6. Mice lacking 5-HT neurons do not display CO2-induced arousal.
EEG (Top), EMG (Middle), and PCO2 (Bottom) traces from WT and Lmx1bf/f/p(no 5-HT neurons) mice showing response to 7% CO2 over a 4 minute period. Whereas wild-type mice display normal arousal to CO2 (as indicated by decreased EEG frequency and increased EMG frequency) Lmx1bf/f/p show no response. (Horizontal scale bar, 30 s; vertical scale bar, 5 μV.) Figure reproduced with permission from the National Academy of Sciences.
Although there is no direct post-mortem evidence of an abnormality in the 5-HT system in cases of SUDEP, there is a growing body of data suggesting a deficit in 5-HT signaling during and after a seizure is involved in post-ictal respiratory depression. It was first found that mice lacking the 5-HT2C receptor have AGS followed by respiratory depression and death (Brennan et al., 1997). Administration of a 5-HT selective reuptake inhibitor (SSRI) in DBA/2 mice significantly reverses respiratory depression and reduces mortality following AGS (Tupal and Faingold, 2006). Moreover, administration of a 5-HT2 receptor antagonist, cyproheptadine, to a subset of DBA/2 mice, which do not have post-ictal respiratory depression, significantly increases the rate of respiratory depression and death (Tupal and Faingold, 2006). Furthermore, DBA/2 mice also have abnormal expression of 5-HT receptors in the brainstem (Uteshev et al., 2010). Finally, epileptic patients taking SSRIs have a lower incidence of seizure-induced apnea during partial seizures compared to patients not on an SSRI (Bateman et al., 2010a). These data suggest that 5-HT signaling could be abnormal in a subset of SUDEP patients, and this abnormality could contribute to respiratory depression and death.
6. Are some cases of SIDS really SUDEP?
Sudden infant death syndrome (SIDS) is defined as the death of an infant less than one year of age which is usually associated with sleep and remains unexplained after autopsy, death scene investigation, and a complete review of the clinical history (Krous et al., 2004). Like SUDEP, SIDS is a diagnosis of exclusion, and about six individuals die in the U.S. daily from each disorder. There are many similarities between the SIDS and SUDEP disorders (Table 1) and deficits in the 5-HT system have been implicated in both. Another possibly related syndrome to SIDS and SUDEP is sudden unexpected death in childhood (SUDC). This syndrome is substantially less common than SIDS and SUDEP, however there may be similar mechanisms leading to death. SUDC could be SIDS in toddlers or be SUDEP in younger children. Although it is intriguing to speculate about SUDC, the relative lack of comprehensive studies investigating SUDC make it difficult to discuss potential mechanisms.
Table 1.
Similarities between SUDEP and SIDS
| SUDEP | SIDS | |
|---|---|---|
| Overall health | Normal other than seizures |
Apparently normal |
| Routine autopsy | Normal | Normal |
| Cause of death | Cardiorespiratory and arousal defects |
Cardiorespiratory and arousal defects |
| Position at death | Frequently prone in bed |
Frequently prone in bed |
| Involvement of 5-HT system |
Probable | Yes |
| Cause of 5-HT dysfunction |
Acute peri-ictal inhibition |
Developmental delay |
| Incidence | ~6 deaths/day in U.S. |
~6 deaths/day in U.S. |
Studies in humans have highlighted a role for the 5-HT system in SIDS pathology. For example, there are 5-HT system abnormalities in post-mortem brains of infants who died from SIDS (Duncan et al., 2010; Kinney et al., 2003; Paterson et al., 2006). 5-HT levels were found to be 26% lower in SIDS cases relative to age-adjusted controls in the medulla (Duncan et al., 2010). In animals, mice lacking the critical 5-HT transcription factor Pet-1 have deficits recovering from short anoxia episodes during post-natal development (Cummings et al., 2011). Moreover, Lmx1bf/f/p mice completely lacking 5-HT neurons have severe episodes of apnea during early post-natal development (Hodges et al., 2009a). Although there is a growing body of evidence suggesting there is an abnormality in the 5-HT system in both SIDS and SUDEP, the mechanisms of 5-HT pathology in each disorder remains unclear. In SIDS, developmental delay of the 5-HT system appears to lead to death, whereas in SUDEP, it is acute dysfunction of this system induced by a seizure that may lead to death. However, one similarity between the pathologies is that they both appear to occur during a depressed state of 5-HT neuronal activity: sleep in SIDS, and the post-ictal period in SUDEP. Often, SUDEP and SIDS patients are found prone in bed suggesting that failure to be aroused by hypercapnia, along with impaired breathing, could be a critical mechanism in each disease. Interestingly, infantile seizures often lead to apnea. For example, a study of infants with acute life threatening events showed that six infants displayed decreased oxygen saturation following an EEG abnormality. Some of these desaturations lasted up to 40 seconds and were severe (Hewertson et al., 1994). Singh (Singh et al., 1993) described two infants with partial seizures and concurrent apnea. The commonalities between the two disorders suggest that in some cases, SIDS might be SUDEP in an infant.
6. Perspectives on SUDEP
Although cardiorespiratory abnormalities have been observed in epileptic patients as early as the turn of the 20th century, there has been little research into these abnormalities until recently. Only lately has the field realized that SUDEP is common. SUDEP research is now growing at a rapid pace; however, there remains a gap in our knowledge regarding many of its features. This lack of knowledge and the difficulty in definitively making its diagnosis make SUDEP very difficult to study.
Currently, EMUs do not regularly record respiratory activity. Given the abundance of evidence suggesting respiratory depression is a critical mechanism of SUDEP, EMU respiratory monitoring will be increasingly important in the future. It is advisable for all EMUs to begin to install this equipment to prevent deaths in the EMU as well as to identify patients that might be at the highest risk for SUDEP. In addition to respiratory recordings, it is important to have simultaneous recordings of heart rate and other physiological responses. A codified methodology for studying SUDEP in the EMU will assist in fully characterizing the mechanisms of sudden death. It will also be critical to establish a uniform definition of apnea. Since respiratory recording equipment is highly sensitive, movement artifact and other abnormalities during a seizure make it difficult to accurately define periods of apnea. Once standardized methods are established, the study of SUDEP and near-SUDEP cases will provide a greater understanding of the events contributing to sudden death. Importantly, hospital lawyers must not prevent doctors from reporting cases of SUDEP that occur in EMUs, which apparently does occur and prevents recognition of a problem that may not be as rare as one would like to believe.
Another important area in SUDEP research is development of animal models that recapitulate human phenotypes. Once again, the methodology and recorded parameters in these models need to be systemized. Currently, there is a lack of concurrent cardiorespiratory and EEG recordings in mouse models, making the development of a small animal EMU critically important. These setups will provide greater insight into the mechanisms of sudden death in animals and will allow greater and more direct translational impact.
Finally, a remaining obstacle is the identification of genetic risk factors associated with SUDEP. Large scale genetic studies of patients who have peri-ictal respiratory depression and those that have near-SUDEP while in the EMU will provide insight into molecular pathways that could be targeted by future treatments. Moreover, these studies may lead to identification of genetic markers for epileptic patients who are at high risk for SUDEP, which could lead to interventions that reduce the risk outside of the hospital.
Highlights.
SUDEP is the leading cause of death in epileptic patients
Multiple mechanisms are thought to be involved, including respiratory dysfunction
Serotonin is critical for control of breathing, chemoreception and arousal
Defects in the serotonin system could be a contributing factor to SUDEP
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bateman LM, Li CS, Lin TC, Seyal M. Serotonin reuptake inhibitors are associated with reduced severity of ictal hypoxemia in medically refractory partial epilepsy. Epilepsia. 2010a;51:2211–2214. doi: 10.1111/j.1528-1167.2010.02594.x. [DOI] [PubMed] [Google Scholar]
- Bateman LM, Li CS, Seyal M. Ictal hypoxemia in localization-related epilepsy: analysis of incidence, severity and risk factors. Brain : a journal of neurology. 2008;131:3239–3245. doi: 10.1093/brain/awn277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman LM, Spitz M, Seyal M. Ictal hypoventilation contributes to cardiac arrhythmia and SUDEP: report on two deaths in video-EEG-monitored patients. Epilepsia. 2010b;51:916–920. doi: 10.1111/j.1528-1167.2009.02513.x. [DOI] [PubMed] [Google Scholar]
- Bernard DG, Li A, Nattie EE. Evidence for central chemoreception in the midline raphe. J Appl Physiol. 1996;80:108–115. doi: 10.1152/jappl.1996.80.1.108. [DOI] [PubMed] [Google Scholar]
- Bird J, Dembny AT, Sandeman D, Butler S. Sudden unexplained death in epilepsy: an intracranially monitored case. Epilepsia. 1997;38(supp 11):s52–56. [Google Scholar]
- Blum AS. Respiratory physiology of seizures. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society. 2009;26:309–315. doi: 10.1097/WNP.0b013e3181b7f14d. [DOI] [PubMed] [Google Scholar]
- Blum AS, Ives JR, Goldberger AL, Al-Aweel IC, Krishnamurthy KB, Drislane FW, Schomer DL. Oxygen desaturations triggered by partial seizures: implications for cardiopulmonary instability in epilepsy. Epilepsia. 2000;41:536–541. doi: 10.1111/j.1528-1157.2000.tb00206.x. [DOI] [PubMed] [Google Scholar]
- Bonvalle M, Bobo EG. Changes in Phrenic Activity and Heart-Rate Elicited by Localized Stimulation of Amygdala and Adjacent Structures. Electroen Clin Neuro. 1972;32:1. doi: 10.1016/0013-4694(72)90223-4. [DOI] [PubMed] [Google Scholar]
- Bradley SR, Pieribone VA, Wang W, Severson CA, Jacobs RA, Richerson GB. Chemosensitive serotonergic neurons are closely associated with large medullary arteries. Nat Neurosci. 2002;5:401–402. doi: 10.1038/nn848. [DOI] [PubMed] [Google Scholar]
- Brennan TJ, Seeley WW, Kilgard M, Schreiner CE, Tecott LH. Sound-induced seizures in serotonin 5-HT2c receptor mutant mice. Nature genetics. 1997;16:387–390. doi: 10.1038/ng0897-387. [DOI] [PubMed] [Google Scholar]
- Brotherstone R, Blackhall B, McLellan A. Lengthening of corrected QT during epileptic seizures. Epilepsia. 2010;51:221–232. doi: 10.1111/j.1528-1167.2009.02281.x. [DOI] [PubMed] [Google Scholar]
- Buchanan GF, Richerson GB. Central serotonin neurons are required for arousal to CO2. Proceedings of the National Academy of Sciences. 2010;107:16354–16359. doi: 10.1073/pnas.1004587107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman W.p., Livingston Rb, Livingston Ke. Frontal lobotomy and electrical stimulation of orbital surface of frontal lobes: Effect on respiration and on blood pressure in man. Archives of Neurology & Psychiatry. 1949;62:701–716. doi: 10.1001/archneurpsyc.1949.02310180002001. [DOI] [PubMed] [Google Scholar]
- Cheah CS, Yu FH, Westenbroek RE, Kalume FK, Oakley JC, Potter GB, Rubenstein JL, Catterall WA. Specific deletion of NaV1.1 sodium channels in inhibitory interneurons causes seizures and premature death in a mouse model of Dravet syndrome. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:14646–14651. doi: 10.1073/pnas.1211591109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran AE, Hodges MR, Wu Y, Wang W, Wylie CJ, Deneris ES, Richerson GB. Medullary serotonin neurons and central CO2 chemoreception. Respiratory physiology & neurobiology. 2009;168:49–58. doi: 10.1016/j.resp.2009.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings KJ, Commons KG, Hewitt JC, Daubenspeck JA, Li A, Kinney HC, Nattie EE. Failed heart rate recovery at a critical age in 5-HT-deficient mice exposed to episodic anoxia: implications for SIDS. J Appl Physiol. 2011;111:825–833. doi: 10.1152/japplphysiol.00336.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasheiff Rm. SUdden unexpected death of epileptic patient due to cardiac arrhythmia after seizure. Archives of neurology. 1986;43:194–196. doi: 10.1001/archneur.1986.00520020080028. D.L.J. [DOI] [PubMed] [Google Scholar]
- Dekin MS, Richerson GB, Getting PA. Thyrotropin-releasing hormone induces rhythmic bursting in neurons of the nucleus tractus solitarius. Science. 1985;229:67–69. doi: 10.1126/science.3925552. [DOI] [PubMed] [Google Scholar]
- Depuy SD, Kanbar R, Coates MB, Stornetta RL, Guyenet PG. Control of breathing by raphe obscurus serotonergic neurons in mice. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:1981–1990. doi: 10.1523/JNEUROSCI.4639-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donner EJ, Jeffs T, Jette N. Knowledge of SUDEP among Canadian Pediatricians. Partners Against Mortality in Epilepsy (PAME); Evanston IL; 2012. [Google Scholar]
- Duncan JR, Paterson DS, Hoffman JM, Mokler DJ, Borenstein NS, Belliveau RA, Krous HF, Haas EA, Stanley C, Nattie EE, Trachtenberg FL, Kinney HC. Brainstem serotonergic deficiency in sudden infant death syndrome. JAMA : the journal of the American Medical Association. 2010;303:430–437. doi: 10.1001/jama.2010.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman JL, Mitchell GS, Nattie EE. Breathing: rhythmicity, plasticity, chemosensitivity. Annual review of neuroscience. 2003;26:239–266. doi: 10.1146/annurev.neuro.26.041002.131103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ficker DM. Sudden unexplained death and injury in epilepsy. Epilepsia. 2000;41(Suppl 2):S7–12. doi: 10.1111/j.1528-1157.2000.tb01519.x. [DOI] [PubMed] [Google Scholar]
- Genton P, Velizarova R, Dravet C. Dravet syndrome: the long-term outcome. Epilepsia. 2011;52(Suppl 2):44–49. doi: 10.1111/j.1528-1167.2011.03001.x. [DOI] [PubMed] [Google Scholar]
- Goldenberg I, Moss AJ. Long QT syndrome. Journal of the American College of Cardiology. 2008;51:2291–2300. doi: 10.1016/j.jacc.2008.02.068. [DOI] [PubMed] [Google Scholar]
- Goldman AM, Glasscock E, Yoo J, Chen TT, Klassen TL, Noebels JL. Arrhythmia in heart and brain: KCNQ1 mutations link epilepsy and sudden unexplained death. Science translational medicine. 2009;1:2ra6. doi: 10.1126/scitranslmed.3000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper RM, Frysinger RC, Trelease RB, Marks JD. State-dependent alteration of respiratory cycle timing by stimulation of the central nucleus of the amygdala. Brain research. 1984;306:1–8. doi: 10.1016/0006-8993(84)90350-0. [DOI] [PubMed] [Google Scholar]
- Hawryluk JM, Moreira TS, Takakura AC, Wenker IC, Tzingounis AV, Mulkey DK. KCNQ Channels Determine Serotonergic Modulation of Ventral Surface Chemoreceptors and Respiratory Drive. The Journal of Neuroscience. 2012;32:16943–16952. doi: 10.1523/JNEUROSCI.3043-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedner J, Hedner T, Wessberg P, Lundberg D, Jonason J. Effects of TRH and TRH analogues on the central regulation of breathing in the rat. Acta physiologica Scandinavica. 1983;117:427–437. doi: 10.1111/j.1748-1716.1983.tb00017.x. [DOI] [PubMed] [Google Scholar]
- Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, Walczak TS, Beghi E, Brodie MJ, Hauser A, Epidemiology I.C.o., Subcommission M. Combined analysis of risk factors for SUDEP. Epilepsia. 2011;52:1150–1159. doi: 10.1111/j.1528-1167.2010.02952.x. [DOI] [PubMed] [Google Scholar]
- Hewertson J, Samuels MP, Southall DP, Poets CF, Boyd SG, Neville BGR. Epileptic Seizure-Induced Hypoxemia in Infants with Apparent Life-Threatening Events. Pediatrics. 1994;94:148–156. [PubMed] [Google Scholar]
- Hodges MR, Martino P, Davis S, Opansky C, Pan LG, Forster HV. Effects on breathing of focal acidosis at multiple medullary raphe sites in awake goats. J Appl Physiol. 2004a;97:2303–2309. doi: 10.1152/japplphysiol.00645.2004. [DOI] [PubMed] [Google Scholar]
- Hodges MR, Opansky C, Qian B, Davis S, Bonis J, Bastasic J, Leekley T, Pan LG, Forster HV. Transient attenuation of CO2 sensitivity after neurotoxic lesions in the medullary raphe area of awake goats. J Appl Physiol. 2004b;97:2236–2247. doi: 10.1152/japplphysiol.00584.2004. [DOI] [PubMed] [Google Scholar]
- Hodges MR, Richerson GB. Contributions of 5-HT neurons to respiratory control: neuromodulatory and trophic effects. Respir Physiol Neurobiol. 2008;164:222–232. doi: 10.1016/j.resp.2008.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges MR, Tattersall GJ, Harris MB, McEvoy SD, Richerson DN, Deneris ES, Johnson RL, Chen ZF, Richerson GB. Defects in breathing and thermoregulation in mice with near-complete absence of central serotonin neurons. Journal of Neuroscience. 2008;28:2495–2505. doi: 10.1523/JNEUROSCI.4729-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges MR, Wehner M, Aungst J, Smith JC, Richerson GB. Transgenic Mice Lacking Serotonin Neurons Have Severe Apnea and High Mortality during Development. The Journal of Neuroscience. 2009a;29:10341–10349. doi: 10.1523/JNEUROSCI.1963-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges MR, Wehner M, Aungst J, Smith JC, Richerson GB. Transgenic mice lacking serotonin neurons have severe apnea and high mortality during development. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009b;29:10341–10349. doi: 10.1523/JNEUROSCI.1963-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holth JK, Bomben VC, Reed JG, Inoue T, Younkin L, Younkin SG, Pautler RG, Botas J, Noebels JL. Tau loss attenuates neuronal network hyperexcitability in mouse and Drosophila genetic models of epilepsy. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2013;33:1651–1659. doi: 10.1523/JNEUROSCI.3191-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins DA, Holstege G. Amygdaloid projections to the mesencephalon, pons and medulla oblongata in the cat. Experimental brain research. Experimentelle Hirnforschung. Experimentation cerebrale. 1978;32:529–547. doi: 10.1007/BF00239551. [DOI] [PubMed] [Google Scholar]
- Jackson JH. On asphyxia in slight epileptic paroxysms. Lancet. 1899;153:79–80. [Google Scholar]
- James MR, Marshall H, Carew-McColl M. Pulse oximetry during apparent tonic-clonic seizures. Lancet. 1991;337:394–395. doi: 10.1016/0140-6736(91)91168-t. [DOI] [PubMed] [Google Scholar]
- Johnston SC, Siedenberg R, Min JK, Jerome EH, Laxer KD. Central apnea and acute cardiac ischemia in a sheep model of epileptic sudden death. Annals of neurology. 1997;42:588–594. doi: 10.1002/ana.410420409. [DOI] [PubMed] [Google Scholar]
- Kaada B.r., Jasper H. REspiratory responses to stimulation of temporal pole, insula, and hippocampal and limbic gyri in man. A.M.A. Archives of Neurology & Psychiatry. 1952;68:609–619. doi: 10.1001/archneurpsyc.1952.02320230035004. [DOI] [PubMed] [Google Scholar]
- Kalume F, Westenbroek RE, Cheah CS, Yu FH, Oakley JC, Scheuer T, Catterall WA. Sudden unexpected death in a mouse model of Dravet syndrome. The Journal of clinical investigation. 2013 doi: 10.1172/JCI66220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney HC, Randall LL, Sleeper LA, Willinger M, Belliveau RA, Zec N, Rava LA, Dominici L, Iyasu S, Randall B, Habbe D, Wilson H, Mandell F, McClain M, Welty TK. Serotonergic brainstem abnormalities in Northern Plains Indians with the sudden infant death syndrome. Journal of neuropathology and experimental neurology. 2003;62:1178–1191. doi: 10.1093/jnen/62.11.1178. [DOI] [PubMed] [Google Scholar]
- Kloster R, Engelskjon T. Sudden unexpected death in epilepsy (SUDEP): a clinical perspective and a search for risk factors. Journal of neurology, neurosurgery, and psychiatry. 1999;67:439–444. doi: 10.1136/jnnp.67.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krous HF, Beckwith JB, Byard RW, Rognum TO, Bajanowski T, Corey T, Cutz E, Hanzlick R, Keens TG, Mitchell EA. Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics. 2004;114:234–238. doi: 10.1542/peds.114.1.234. [DOI] [PubMed] [Google Scholar]
- Lalley PM. Serotoninergic and non-serotoninergic responses of phrenic motoneurones to raphe stimulation in the cat. J Physiol. 1986;380:373–385. doi: 10.1113/jphysiol.1986.sp016291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamberts RJ, Laranjo S, Kalitzin SN, Velis DN, Rocha I, Sander JW, Thijs RD. Postictal generalized EEG suppression is not associated with periictal cardiac autonomic instability in people with convulsive seizures. Epilepsia. 2012 doi: 10.1111/epi.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Gal F, Korff CM, Monso-Hinard C, Mund MT, Morris M, Malafosse A, Schmitt-Mechelke T. A case of SUDEP in a patient with Dravet syndrome with SCN1A mutation. Epilepsia. 2010;51:1915–1918. doi: 10.1111/j.1528-1167.2010.02691.x. [DOI] [PubMed] [Google Scholar]
- Lee HW, Tae WS, Seo DW, Kim SE. Partial seizures manifesting as apnea only in an adult. Epilepsia. 1999;40:1828–1831. doi: 10.1111/j.1528-1157.1999.tb01606.x. H.S. [DOI] [PubMed] [Google Scholar]
- Lee M. EEG video recording of sudden unexpected death in epilepsy (SUDEP) Epilepsia. 1998;39(suppl. 6):123–124. [Google Scholar]
- Lhatoo SD, Faulkner HJ, Dembny K, Trippick K, Johnson C, Bird JM. An electroclinical case-control study of sudden unexpected death in epilepsy. Annals of neurology. 2010;68:787–796. doi: 10.1002/ana.22101. [DOI] [PubMed] [Google Scholar]
- McLean BN, Wimalaratna S. Sudden death in epilepsy recorded in ambulatory EEG. Journal of neurology, neurosurgery, and psychiatry. 2007;78:1395–1397. doi: 10.1136/jnnp.2006.088492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messier ML, Li A, Nattie EE. Muscimol inhibition of medullary raphe neurons decreases the CO2 response and alters sleep in newborn piglets. Respir Physiol Neurobiol. 2002;133:197–214. doi: 10.1016/s1569-9048(02)00168-4. [DOI] [PubMed] [Google Scholar]
- Moseley BD, Nickels K, Britton J, Wirrell E. How common is ictal hypoxemia and bradycardia in children with partial complex and generalized convulsive seizures? Epilepsia. 2010;51:1219–1224. doi: 10.1111/j.1528-1167.2009.02490.x. [DOI] [PubMed] [Google Scholar]
- Nashef L. Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia. 1997;38:S6–8. doi: 10.1111/j.1528-1157.1997.tb06130.x. [DOI] [PubMed] [Google Scholar]
- Nashef L, Walker F, Allen P, Sander JW, Shorvon SD, Fish DR. Apnoea and bradycardia during epileptic seizures: relation to sudden death in epilepsy. Journal of neurology, neurosurgery, and psychiatry. 1996;60:297–300. doi: 10.1136/jnnp.60.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neufeld G, Lazar JM, Chari G, Kamran H, Akajagbor E, Salciccioli L, Kassotis J, Stewart M. Cardiac repolarization indices in epilepsy patients. Cardiology. 2009;114:255–260. doi: 10.1159/000233236. [DOI] [PubMed] [Google Scholar]
- Noebels J. A perfect storm: Converging paths of epilepsy and Alzheimer's dementia intersect in the hippocampal formation. Epilepsia. 2011;52(Suppl 1):39–46. doi: 10.1111/j.1528-1167.2010.02909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson DS, Trachtenberg FL, Thompson EG, Belliveau RA, Beggs AH, Darnall R, Chadwick AE, Krous HF, Kinney HC. Multiple serotonergic brainstem abnormalities in sudden infant death syndrome. JAMA : the journal of the American Medical Association. 2006;296:2124–2132. doi: 10.1001/jama.296.17.2124. [DOI] [PubMed] [Google Scholar]
- Pena F, Ramirez JM. Endogenous activation of serotonin-2A receptors is required for respiratory rhythm generation in vitro. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2002;22:11055–11064. doi: 10.1523/JNEUROSCI.22-24-11055.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptak K, Yamanishi T, Aungst J, Milescu LS, Zhang R, Richerson GB, Smith JC. Raphe neurons stimulate respiratory circuit activity by multiple mechanisms via endogenously released serotonin and substance P. Journal of Neuroscience. 2009;29:3720–3737. doi: 10.1523/JNEUROSCI.5271-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purpura DP. Experimental models of epilepsy--a manual for the laboratory worker. Raven Press; New York: 1972. [Google Scholar]
- Ray RS, Corcoran AE, Brust RD, Kim JC, Richerson GB, Nattie E, Dymecki SM. Impaired respiratory and body temperature control upon acute serotonergic neuron inhibition. Science. 2011;333:637–642. doi: 10.1126/science.1205295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richerson GB. Response to CO2 of neurons in the rostral ventral medulla in vitro. Journal of neurophysiology. 1995;73:933–944. doi: 10.1152/jn.1995.73.3.933. [DOI] [PubMed] [Google Scholar]
- Richerson GB. Serotonergic neurons as carbon dioxide sensors that maintain pH homeostasis. Nature reviews. Neuroscience. 2004;5:449–461. doi: 10.1038/nrn1409. [DOI] [PubMed] [Google Scholar]
- Roberson ED, Halabisky B, Yoo JW, Yao J, Chin J, Yan F, Wu T, Hamto P, Devidze N, Yu GQ, Palop JJ, Noebels JL, Mucke L. Amyloid-beta/Fyn-induced synaptic, network, and cognitive impairments depend on tau levels in multiple mouse models of Alzheimer's disease. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:700–711. doi: 10.1523/JNEUROSCI.4152-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe PC. The Harriet Lane Handbook. 11th Medical Handbook Publishers; Chicago: 1987. [Google Scholar]
- Schwaber JS, Kapp BS, Higgins G. The origin and extent of direct amygdala projections to the region of the dorsal motor nucleus of the vagus and the nucleus of the solitary tract. Neuroscience letters. 1980;20:15–20. doi: 10.1016/0304-3940(80)90226-8. [DOI] [PubMed] [Google Scholar]
- Schwaber JS, Kapp BS, Higgins GA, Rapp PR. Amygdaloid and basal forebrain direct connections with the nucleus of the solitary tract and the dorsal motor nucleus. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1982;2:1424–1438. doi: 10.1523/JNEUROSCI.02-10-01424.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Severson CA, Wang W, Pieribone VA, Dohle CI, Richerson GB. Midbrain serotonergic neurons are central pH chemoreceptors. Nat Neurosci. 2003;6:1139–1140. doi: 10.1038/nn1130. [DOI] [PubMed] [Google Scholar]
- Seyal M, Bateman LM. Ictal apnea linked to contralateral spread of temporal lobe seizures: Intracranial EEG recordings in refractory temporal lobe epilepsy. Epilepsia. 2009;50:2557–2562. doi: 10.1111/j.1528-1167.2009.02245.x. [DOI] [PubMed] [Google Scholar]
- Seyal M, Hardin KA, Bateman LM. Postictal generalized EEG suppression is linked to seizure-associated respiratory dysfunction but not postictal apnea. Epilepsia. 2012;53:825–831. doi: 10.1111/j.1528-1167.2012.03443.x. [DOI] [PubMed] [Google Scholar]
- Seyal M, Pascual F, Lee CY, Li CS, Bateman LM. Seizure-related cardiac repolarization abnormalities are associated with ictal hypoxemia. Epilepsia. 2011;52:2105–2111. doi: 10.1111/j.1528-1167.2011.03262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorvon S, Tomson T. Sudden unexpected death in epilepsy. Lancet. 2011;378:2028–2038. doi: 10.1016/S0140-6736(11)60176-1. [DOI] [PubMed] [Google Scholar]
- Singh B, al Shahwan A, al Deeb SM. Partial seizures presenting as life-threatening apnea. Epilepsia. 1993;34:901–903. doi: 10.1111/j.1528-1157.1993.tb02109.x. [DOI] [PubMed] [Google Scholar]
- So EL, Sam MC, Lagerlund TL. Postictal Central Apnea as a Cause of SUDEP: Evidence From Near-SUDEP Incident. Epilepsia. 2000;41:1494–1497. doi: 10.1111/j.1528-1157.2000.tb00128.x. [DOI] [PubMed] [Google Scholar]
- Spencer WG. The Effect Produced upon Respiration by Faradic Excitation of the Cerebrum in the Monkey, Dog, Cat, and Rabbit. Philosophical Transactions of the Royal Society of London. 1894;B 185:609–657. [Google Scholar]
- Subramanian HH, Balnave RJ, Holstege G. The midbrain periaqueductal gray control of respiration. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2008;28:12274–12283. doi: 10.1523/JNEUROSCI.4168-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surges R, Adjei P, Kallis C, Erhuero J, Scott CA, Bell GS, Sander JW, Walker MC. Pathologic cardiac repolarization in pharmacoresistant epilepsy and its potential role in sudden unexpected death in epilepsy: a case-control study. Epilepsia. 2010a;51:233–242. doi: 10.1111/j.1528-1167.2009.02330.x. [DOI] [PubMed] [Google Scholar]
- Surges R, Scott CA, Walker MC. Enhanced QT shortening and persistent tachycardia after generalized seizures. Neurology. 2010b;74:421–426. doi: 10.1212/WNL.0b013e3181ccc706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surges R, Strzelczyk A, Scott CA, Walker MC, Sander JW. Postictal generalized electroencephalographic suppression is associated with generalized seizures. Epilepsy & behavior : E&B. 2011;21:271–274. doi: 10.1016/j.yebeh.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Surges R, Taggart P, Sander JW, Walker MC. Too long or too short? New insights into abnormal cardiac repolarization in people with chronic epilepsy and its potential role in sudden unexpected death. Epilepsia. 2010c;51:738–744. doi: 10.1111/j.1528-1167.2010.02571.x. [DOI] [PubMed] [Google Scholar]
- Surges R, Walker MC. Peri-ictal heart rates depend on seizure-type. Seizure : the journal of the British Epilepsy Association. 2010;19:453. doi: 10.1016/j.seizure.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Thurman D. The Epidemiology of SUDEP: A Public Health Perspective, Partners Against Mortality in Epilepsy (PAME) American Epilepsy Society; Evanston IL: 2011. [Google Scholar]
- Tolstykh GP. KCNQ channels in the nucleus tractus solitarius of the brainstem might be involved in SUDEP. Epilepsia. 2010;51:S5. C.J. [Google Scholar]
- Tolstykh GP, Shapiro MS. Expression and regulatin of M-type K+ channels in visceral sensory neurons. Biophysical Society 52nd Annual Meeting; 2008. Z.O. [Google Scholar]
- Toman JE, Swinyard EA, Goodman LS. Properties of maximal seizures, and their alteration by anticonvulant drugs and other agents. Journal of neurophysiology. 1946;9:231–239. doi: 10.1152/jn.1946.9.3.231. [DOI] [PubMed] [Google Scholar]
- Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet neurology. 2008;7:1021–1031. doi: 10.1016/S1474-4422(08)70202-3. [DOI] [PubMed] [Google Scholar]
- Tupal S, Faingold CL. Evidence supporting a role of serotonin in modulation of sudden death induced by seizures in DBA/2 mice. Epilepsia. 2006;47:21–26. doi: 10.1111/j.1528-1167.2006.00365.x. [DOI] [PubMed] [Google Scholar]
- Uteshev VV, Tupal S, Mhaskar Y, Faingold CL. Abnormal serotonin receptor expression in DBA/2 mice associated with susceptibility to sudden death due to respiratory arrest. Epilepsy research. 2010;88:183–188. doi: 10.1016/j.eplepsyres.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Veasey SC, Fornal CA, Metzler CW, Jacobs BL. Response of serotonergic caudal raphe neurons in relation to specific motor activities in freely moving cats. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1995;15:5346–5359. doi: 10.1523/JNEUROSCI.15-07-05346.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veasey SC, Fornal CA, Metzler CW, Jacobs BL. Single-unit responses of serotonergic dorsal raphe neurons to specific motor challenges in freely moving cats. Neuroscience. 1997;79:161–169. doi: 10.1016/s0306-4522(96)00673-2. [DOI] [PubMed] [Google Scholar]
- Veening JG, Swanson LW, Sawchenko PE. The organization of projections from the central nucleus of the amygdala to brainstem sites involved in central autonomic regulation: A combined retrograde transport-immunohistochemical study. Brain research. 1984;303:337–357. doi: 10.1016/0006-8993(84)91220-4. [DOI] [PubMed] [Google Scholar]
- Venit EL, Shepard BD, Seyfried TN. Oxygenation prevents sudden death in seizureprone mice. Epilepsia. 2004;45:993–996. doi: 10.1111/j.0013-9580.2004.02304.x. [DOI] [PubMed] [Google Scholar]
- Wang W, Pizzonia JH, Richerson GB. Chemosensitivity of rat medullary raphe neurones in primary tissue culture. J Physiol. 1998;511:433–450. doi: 10.1111/j.1469-7793.1998.433bh.x. Pt 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Tiwari JK, Bradley SR, Zaykin RV, Richerson GB. Acidosis-stimulated neurons of the medullary raphe are serotonergic. Journal of neurophysiology. 2001;85:2224–2235. doi: 10.1152/jn.2001.85.5.2224. [DOI] [PubMed] [Google Scholar]
- Watanabe K, Hara K, Hakamada S, Negoro T, Sugiura M, Matsumoto A, Maehara M. Seizures with apnea in children. Pediatrics. 1982;70:87–90. [PubMed] [Google Scholar]