Abstract
Introduction
COPD is a leading cause of morbidity and mortality. Self-management interventions are considered important in order to limit the progression of the disease. Computer-tailored interventions could be an effective tool to facilitate self-management.
Methods
This randomized controlled trial tested the effectiveness of a web-based, computer-tailored COPD self-management intervention on physical activity and smoking behavior. Participants were recruited from an online panel and through primary care practices. Those at risk for or diagnosed with COPD, between 40 and 70 years of age, proficient in Dutch, with access to the Internet, and with basic computer skills (n=1,325), were randomly assigned to either the intervention group (n=662) or control group (n=663). The intervention group received the web-based self-management application, while the control group received no intervention. Participants were not blinded to group assignment. After 6 months, the effect of the intervention was assessed for the primary outcomes, smoking cessation and physical activity, by self-reported 7-day point prevalence abstinence and the International Physical Activity Questionnaire – Short Form.
Results
Of the 1,325 participants, 1,071 (80.8%) completed the 6-month follow-up questionnaire. No significant treatment effect was found on either outcome. The application however, was used by only 36% of the participants in the experimental group.
Conclusion
A possible explanation for the nonsignificant effect on the primary outcomes, smoking cessation and physical activity, could be the low exposure to the application as engagement with the program has been shown to be crucial for the effectiveness of computer-tailored interventions. (Netherlands Trial Registry number: NTR3421.)
Keywords: smoking cessation, physical activity, Internet intervention, tailoring, COPD
Background
COPD is one of the leading causes of morbidity and mortality worldwide.1 COPD patients suffer from airflow limitation that is typically progressive and not reversible.2 Adequate patient self-management and behavior modification, such as smoking cessation and increasing the level of physical activity, are recommended to decelerate disease progression.3,4
A relatively small number of studies on the effectiveness of COPD self-management interventions have been conducted, and the evidence on effectiveness remains inconclusive.5 Self-management interventions have mainly focused on educating COPD patients using standardized information, but are now increasingly offering personalized information to patients through counseling with a health care provider.5
Another trend in providing health-promoting information is e-Health, which uses information and communication technology.6 Information provided by e-Health interventions has been individualized using computer-tailored technology, often with disease prevention as a main goal.7–9 This intervention method offers computer-generated, personally relevant information by adapting the content of health-promotion messages to users’ characteristics.9 Personalizing and adapting health messages has been found to help attract and keep users’ attention, increase appreciation, and help users process messages more thoroughly.10–12 Computer-tailored interventions have been shown to effectively improve health behaviors, such as smoking cessation and physical activity.13,14 This intervention strategy has also been successful when targeting multiple behaviors11 and has been found to be more cost-effective than usual care.15 To our knowledge, this promising technique has not yet been tested with the purpose of supporting behavior change in COPD patients.
In the MasterYourBreath (“AdemDeBaas” in Dutch) project, we developed a web-based, computer-tailored self-management application for COPD patients. We evaluated and improved the usability of the prototype16 and conducted a pilot study.17 In the present paper, we report the effectiveness of this intervention on behavioral (physical activity, smoking cessation, and the intention to be more physically active and to quit smoking) and clinical outcomes (clinical disease control and dyspnea).
Methods
Study design
This randomized controlled trial (RCT) compared an intervention group which received a COPD self-management application to a control group that did not receive the intervention. All participants, whether they were assigned to the control or intervention group, were free to receive usual care or use other resources in order to help them manage their disease or improve their lifestyle.
In the Netherlands, a COPD disease-management approach is widely implemented.18 This approach includes a practice nurse who coaches patients to improve their self-management behavior. We originally planned to integrate the intervention in this disease-management approach, but our pilot study had shown that it was not feasible to recruit enough patients to cover the sample size required for our RCT if the practice nurse recruited the patients.17 Instead, to solve the recruitment issues, we invited patients from five general practices by mail and recruited patients from a Dutch online panel. We also broadened our inclusion criteria to include people at risk for COPD as well as people with known COPD.
The Dutch online panel was assembled by the company Flycatcher Internet Research BV (www.flycatcher.eu) which is an institute for online research certified by the International Organization for Standardization. In total, the online panel consisted of 16,000 Dutch-speaking members, who had an email address and were at least 12 years old. All age groups, education levels, and provinces of the Netherlands were represented in the panel. Flycatcher’s members are recruited by Flycatcher through newsletters, send-to-a-friend promotions, third parties’ contact lists used for research (with the permission of the owner of the contact list and the person on the list), and word-of-mouth advertising. Members receive seven research questionnaires a year on average.
Members from the Dutch online panel and the five general practices were eligible for participation in this study if they were diagnosed with COPD or were at moderate or high risk for COPD, were between 40–70 years of age, were proficient in Dutch, and had access to the Internet and basic computer skills. Dutch proficiency and basic computer literacy were gauged by administration of the first online questionnaire. The Respiratory Health Screening Questionnaire (RHSQ)19 was used to assess the subject’s risk for COPD. This questionnaire contains ten items related to important determinants of COPD for individuals of 40 years and older.19 A scoring system for case-finding20,21 was used to determine if an individual was at low (<16.5 points), moderate (16.5–19.5 points), or high risk (>19.5 points) for COPD (sensitivity =58.7%, specificity =77.0%, for the 16.5 cutoff point).20
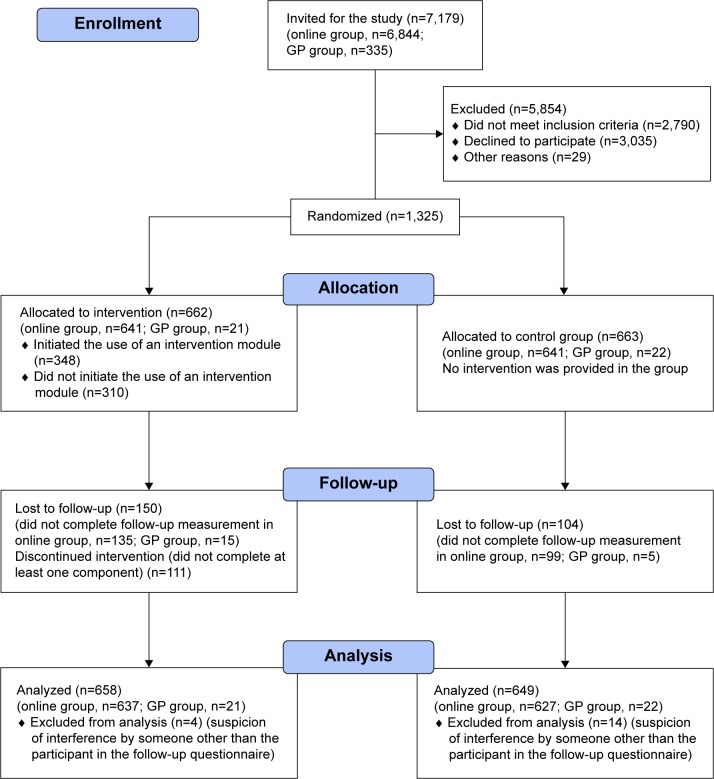
The five general practices were involved in a parallel project21 in which 40- to 70-year-old patients had already been screened for COPD by their general practitioner using the RHSQ. Potentially eligible members of the online panel were invited for the study by an email from Flycatcher, including a study information letter. Members who decided to participate were screened for eligibility by completing the RHSQ. We implemented a scoring algorithm within the online questionnaire, so eligibility could be determined directly after participants completed the questionnaire. Members received a small incentive equal to €2.55 per completed questionnaire (baseline and follow-up). Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) diagram including the two populations.
Figure 1.
Consolidated Standards of Reporting Trials diagram.
Abbreviation: GP, general practice.
The study was approved by the Medical Ethical Committee of Maastricht University Medical Center (METC 12-4-033) and registered with the Netherlands Trial Registry (NTR3421). All participants received an online study information letter and completed an online informed consent form before entering the study. A more detailed description of the methods can be found in a study protocol published elsewhere.22
Randomization
A permuted block design23 with a random block size varying from four to 20 was employed to randomize participants stratified by channel of recruitment (online or through general practice). This approach was chosen in order to achieve balanced and evenly distributed samples for both recruitment strategies. A researcher not involved in data collection or analysis of the results performed the randomization using PROC PLAN in SAS software (v 9.1; SAS Institute, Cary, NC, USA). Due to the study design, it was not feasible to blind participants to group assignments.
Intervention
MasterYourBreath application
The intervention, “MasterYourBreath”,22 was designed to change participants’ health behavior by means of a web-based application providing computer-generated tailored feedback. The intervention was based on earlier studies on computer-tailored feedback for lifestyle changes which have been shown to be effective and cost-effective11,24–26 and adapted to our target groups. The MasterYourBreath application was built using the online application Tailorbuilder (OverNite Software Europe, Sittard, Netherlands).
Participants assigned to the experimental group were asked by email to access the application with a personalized account and use the application ad libitum for 6 months. Participants in the online group received the email from Flycatcher and those in the general practice group from the research team. Application use was monitored by the research team and email prompts were sent to encourage application use,27 mostly within a 2-week time interval addressing new content on the website, as this could increase the number of follow-up visits.28 The application had a modular design, including two behavior-change modules, smoking cessation and physical activity. Each module was equally divided into six intervention components: (1) health-risk appraisal: feedback on the behavior (smoking or physical activity) based on Dutch guidelines; (2) motivational beliefs: feedback on perceived positive and negative consequences of the behavior; (3) social influence: feedback on the social influences of participants’ partner, family, friends, and coworkers on the behavior; (4) goal setting and action plans: feedback on achievement of goals and on action plans in order to achieve their goal; (5) self-efficacy: feedback on perceived barriers to change the behavior; and (6) maintenance: feedback in order to maintain the healthy behavior. Participants could switch behavior-change modules and choose to enter one or more intervention components according to their preference.10
Feedback was personalized using participants’ names and tailored to participants’ characteristics and key behavior determinants of psychosocial constructs, for which the I-Change model served as theoretical framework.29,30 Examples of the key behavior determinants are: pros and cons of physical activity, perceived social support to quit smoking, action plans to increase physical activity, and self-efficacy to cope with barriers to quit smoking. Participants were asked questions to uncover their personal determinants, using questionnaires that have been tested experimentally among Dutch adults in previous studies in the general public.13,31,32 These questionnaires were adjusted for COPD patients during the usability study.16 The questions were used to generate tailored feedback to the participants about their responses. Participants’ previous responses were also incorporated in the feedback so they could track their own behavior change and goal attainment over the course of the study. The six intervention components per module were available to the participants to be completed over time as they chose. This allowed participants the ability to track their behavior changes by comparing the most current answers with the previous answers.
A more detailed description of the intervention and prompt protocol is described elsewhere.22
Website
The computer-tailored application was embedded in a website. The website contained general information about the MasterYourBreath project, COPD/being at risk for COPD, smoking, and physical activity. Online self-management resources, such as videos with home exercises (seven exercises focusing on strength and balance) and hyperlinks to other informative websites, were also included. The tailored feedback and prompts referred participants to the home exercises and other resources.
Data collection
A web-based questionnaire was administered at baseline between May and November of 2012 with a follow-up questionnaire sent out 6 months later. The frequency of reminders for completing these questionnaires was adapted to the response rate. The online group received one reminder to participate in the study and complete the baseline questionnaire. General practice group participants received two additional reminders if they responded to the invitation but did not complete the baseline questionnaire, since the participation rate in this group was low. The online group received one reminder to complete the follow-up questionnaire, whereas the general practice group received two reminders. Data collection ended in July 2013. All data were captured through these questionnaires, except demographic characteristics in the online group, as these were already documented through an annual update process undertaken by Flycatcher.
Outcome measures
Two primary outcomes were measured, one for each health behavior: smoking cessation and physical activity. Smoking cessation was assessed by one item measuring the 7-day point prevalence abstinence,33,34 and the level of physical activity was assessed by the International Physical Activity Questionnaire – Short Form.35
We created a “behavior-change score” by combining the two behaviors (smoking cessation and physical activity). The behavior-change score was only calculated for participants who smoked at baseline or were below the physical activity norm (defined as being physically active for at least 30 minutes a day on 5 days a week at a moderate or vigorous intensity). The efforts of participants were rated as “successful behavior change” if they achieved smoke-free status for 7 consecutive days prior to the follow-up measurement, or if they achieved the norm level of physical activity at follow-up, reflecting a change from their baseline behavior. The actions of participants who smoked or were below the physical activity norm at baseline and achieved neither smoke-free status nor the norm level of physical activity at follow-up were rated as “unsuccessful behavior change”.
Secondary outcomes included secondary smoking cessation measures, health status, and intention to change behavior. Secondary smoking cessation measures were: number of quit attempts during the past 6 months, 24-hour point prevalence abstinence, tobacco consumption, and continued and prolonged abstinence.33,34 To assess participants’ health status, participants were asked if they experienced any form of breathlessness, and if so, the Medical Research Council (MRC) dyspnea scale was administered in order to measure the level of disability.36 Clinical disease control was measured using the Clinical COPD Questionnaire. This questionnaire assesses both patient guideline goals (health-related quality of life) and clinical guideline goals such as prevention of disease progression.37 Intention to change behavior was measured by separate questions for physical activity and smoking. Table 1 presents an overview of all outcomes including how and when they were measured.
Table 1.
Primary and secondary outcomes
| Outcome(s) | Measurement | Scale | Time |
|---|---|---|---|
| Primary | |||
| Smoking cessation: 7-day point prevalence abstinence | 1 item assessing whether participant smoked during the last 7 daysa | 0= did not refrain from smoking during the last 7 days; 1= refrained from smoking during the last 7 days | Follow-up |
| Level of physical activity | IPAQ-SFb | MET minutes a week (last 7 days): vigorous physical activity =8.0 METs; moderate physical activity =4.0 METs; walking =3.3 METs | Baseline and follow-up |
| Secondary | |||
| Quit attempts | 1 item assessing the number of quit attempts during the past 6 monthsa | Number of quit attempts during the past 6 months | Follow-up |
| 24-hour point prevalence abstinence | 1 item assessing whether participant smoked during the last 24 hoursa | 0= did not refrain from smoking during the last 24 hours; 1= refrained from smoking during the last 24 hours | Follow-up |
| Continued abstinence | 1 item assessing when the last serious quit date was, and 1 item assessing smoking behavior since that datea | 0= smoked since the last quit date; 1= did not smoke at all since the last quit date | Follow-up |
| Prolonged abstinence | 1 item assessing when the last serious quit date was, and 1 item assessing smoking behavior since that date, allowing a grace period of 2 weeks in which smoking behavior was not counted as sucha | 0= smoked since 2 weeks after the last quit date; 1= did not smoke at all since 2 weeks after the last quit date | Follow-up |
| Tobacco consumption | 4 items assessing what products (cigarettes, rolling tobacco, cigars, or pipe tobacco) are currently smoked, and 4 items assessing how much of each product is currently smokeda | Number of cigarettesf | Baseline and follow-up |
| Dyspnea status | 1 item, MRC scalec | 1–5; higher score means worse dyspnea | Baseline and follow-up |
| Clinical disease control | 10-item CCQd | 0= very good control; 6= extremely poor control | Baseline and follow-up |
| Intention to quit smoking | 1 item, 7-point Likert scalee | 1= I certainly plan to quit smoking; 7= I certainly do not plan to quit smoking | Baseline and follow-up |
| Intention to increase the level of physical activity | 1 item, 7-point Likert scalee | 1= I certainly plan to be more physically active; 7= I certainly do not plan to be more physically active | Baseline and follow-up |
Notes:
Smoking cessation questions were selected based on the Russel Standard33 and a Dutch guide published by Stivoro that aimed to standardize smoking cessation measures in the Netherlands.34 Self-report has been shown to be reliable in COPD patients: kappa coefficient =0.20 for biochemical validation at 6-month measurement, P=0.003.61
The reliability and validity of the IPAQ-SF have been tested in the Dutch population: test–retest reliability, ρ=0.85; concurrent validity between long and short IPAQ, from ρ=0.85 to 0.88; criterion validity against accelerometer, ρ=0.32.35
The MRC scale is a useful measure for disability. Significant associations were found between disability MRC grade and shuttle distance, St George Respiratory Questionnaire,62 Chronic Respiratory Questionnaire63 scores, mood state, and Nottingham Extended Activities of Daily Living64 scores. Forced expiratory volume in one second was not associated with MRC grade.36
The CCQ is validated in the Dutch population and can be used for COPD patients and individuals at risk for COPD: Cronbach’s alpha =0.91(internal consistency), significantly higher score of people with or at risk for COPD compared to healthy (ex-)smokers (P<0.05) (discriminate validity), significant correlations with 36-Item Short Form Health Survey (ρ=0.48–0.69)65 and St George Respiratory Questionnaire (ρ=0.67–0.72) (internal consistency); correlation with forced expiratory volume in one second % predicted ρ=–0.49 (divergent validity); intra class coefficient =0.94 (test–retest reliability); significant improvement in CCQ found after 2 months’ smoking cessation (responsiveness).37
The intention questions were based on the I-Change model.29,30 The “intention to quit smoking” question has previously been used successfully in a similar intervention study.66
The overall score for tobacco consumption was expressed as the number of cigarettes, whereby one hand-rolled cigarette equaled one commercial cigarette, and one cigar equaled four cigarettes.34 We considered one pipe to equal one cigarette, since no concrete guidelines were available on converting the number of pipes to cigarettes.
Abbreviations: CCQ, Clinical COPD Questionnaire; IPAQ-SF, International Physical Activity Questionnaire – Short Form; MET, metabolic equivalent task; MRC, Medical Research Council.
Baseline measurements
There were several additional baseline measures that were not part of the primary and secondary outcome measures, including demographic characteristics: age, sex, marital status, education level, and current employment status. Several additional questions were asked at baseline to capture smoking behavior. Participants were asked if they had ever smoked and about their number of previous quit attempts. The six-item version of the Fagerström Test for Nicotine Dependence (0= not addicted; 10= highly addicted)38 was included in order to assess the addiction level. Health status was further estimated, measuring COPD status and comorbidities, by asking participants whether they were diagnosed with COPD or any other chronic disease, and which other chronic disease(s).
Sample-size calculation
Sample-size calculations assumed 80% power and a significance level of 0.05 for both behaviors and were completed by PS software version 3.0.43,39 according to Fisher’s exact test. Calculations for smoking indicated that 446 participants per group were necessary at the end of the trial to detect a 10% difference in 7-day point prevalence (20% abstinence in the intervention group, compared to 10% in the control group31). We based this calculation on the assumption that 49.2% of the population with an increased risk for COPD smoked at baseline.40 The number needed for measuring physical activity was smaller and could be obtained following the above sample-size calculation for smoking.22 In another study the standard deviation was 26.63 minutes a day in a Dutch population.41 When including 446 participants per group, a difference of 5 minutes a day, which corresponds to a small standardized effect size (Cohen’s d =0.2), could be detected. In order to allow for a 30% drop-out rate, a baseline total of 1,275 participants was necessary to reach 80% power.
Analyses
Differences at baseline between groups (intervention vs control; and participants who dropped out vs who did not drop out) were compared using chi-square tests for categorical variables and independent-samples t-tests for numerical variables. Data were analyzed according to the intention-to-treat principle. For both primary outcomes, an additional per protocol analysis was conducted. Participants assigned to the experimental group had to have completed at least one of the six intervention components of the specific behavior module to be included in the latter analysis. For the “per protocol” analyses, we conducted two sensitivity analyses with stricter criteria for each primary outcome (smoking cessation and physical activity). For the first analyses, we included only participants who completed at least two intervention components of the specific behavior module. For the second analyses, we included only participants who completed at least three intervention components, since a higher “usage dose” may be necessary to yield a treatment effect.
The uncorrected and corrected effects of the intervention on the primary and secondary outcomes were assessed using logistic regression for categorical outcomes and linear regression for numerical outcomes measured at 6 months. Linear mixed models were used for outcomes measured at baseline and at 6 months to account for the correlation between repeated measurements of the same participant and to include all participants, including those with missing data. As for correction, the models included: the stratification variable – that is, recruitment channel (online or general practices); baseline variables if they showed a statistically significant difference between intervention and control group; and baseline variables that were related to drop out, missing data, and/or related to the outcome at 6 months (P value ≤0.20 in univariable regression analysis) to increase the precision of the intervention effect. To assess potential effect modifiers, the interaction of the treatment variable with age, sex, intention to increase level of physical activity, educational level, dyspnea status, and COPD status were added in the corrected mixed-model analyses for level of physical activity. Primary outcomes were analyzed for subgroups based on age (40–50, 50–60, 60–70), sex, intention to change behavior (those who had no intention or were not sure; those who intended to change), education level (low, middle, high), dyspnea (yes, no), COPD status (diagnosed, at risk).
The robustness of our results of the primary outcome for smoking cessation was tested by conducting a best- and a worst-case scenario, where respondents lost to follow-up were considered to have quit smoking in the best-case scenario and considered to still be smoking in the worst-case scenario. In addition, as a sensitivity analysis, the intervention effect on the behavior-change score was tested using logistic regression analysis.
All statistical analyses were performed using IBM SPSS (v 19). Two-sided P values ≤0.05 were considered statistically significant.
Results
Recruitment
A total of 7,179 individuals were invited for the study of which 3,035 declined to participate, 2,790 did not meet the inclusion criteria, and 29 were excluded because they did not complete the baseline questionnaire (n=24) or provided unreliable responses (n=5). Responses were unreliable if answers were straight lined (ie, the same answer options selected for each set of items) or the questionnaire was completed within 3 minutes (which was considered to be unrealistically fast).
A total of 1,325 participants (1,282 in the online group and 43 in the general practice group) completed the baseline questionnaire and were randomly assigned to the experimental (online group: n=641, general practice group: n=21) or control group (online group: n=641, general practice group: n=22). Of the 1,325 participants, 1,071 (80.8%) completed the 6-month follow-up questionnaire, including 1,048 (81.7%) of the online group and 23 (53.5%) of the general practice group. Eighteen participants of the online group were excluded from further analyses, due to a high level of suspicion of interference by someone other than the participant, (eg, a partner with whom they shared an email address). Participants were excluded when at least two of the following variables did not match their Flycatcher profile on the follow-up questionnaire: sex, day of birth, month of birth, year of birth. If only one variable was inconsistent or day and month were reversed, we suspected a typing error and did not exclude those participants.
In the group of smokers, 447 participants were included of whom 341 completed the follow-up questionnaire. Figure 1 shows the CONSORT diagram of our RCT.
Sample characteristics
Table 2 shows the baseline characteristics of the overall sample and the experimental and control groups separately. The only significant difference between the groups was the employment status of participants (P=0.039). As for the participants who smoked at baseline, we did not find any significant differences in baseline characteristics between the groups.
Table 2.
Baseline characteristics of study participants – overall, experimental and control group
| Characteristic | Overall sample (n=1,307) |
Experimental group (n=658) |
Control group (n=649) |
|---|---|---|---|
| Age, years (mean [SD]) | 57.6 (7.2) | 57.7 (7.3) | 57.6 (7.2) |
| Male (n [%]) | 627 (48.0) | 326 (49.5) | 301 (46.4) |
| Education level (n [%]) | |||
| Primary school/basic vocational school | 386 (29.5) | 191 (29.0) | 195 (30.0) |
| Secondary vocational school/high school degree | 427 (32.7) | 209 (31.8) | 218 (33.6) |
| Higher professional degree/university degree | 494 (37.8) | 258 (39.2) | 236 (36.4) |
| Current employment status (n [%]) | |||
| Employed | 670 (51.3) | 356 (54.1) | 314 (48.4) |
| Not employed | 637 (48.7) | 302 (45.9) | 335 (51.6)* |
| Marital status (n [%]) | |||
| Single/divorced/widowed | 348 (26.6) | 171 (26.0) | 177 (27.3) |
| In a relationship/living together/married | 959 (73.4) | 487 (74.0) | 472 (72.7) |
| COPD status (n [%]) | |||
| Diagnosed with COPD | 284 (21.7) | 146 (22.2) | 138 (21.3) |
| Increased risk for COPD per RHSQ19 | 1,023 (78.3) | 512 (77.8) | 511 (78.7) |
| Comorbidity (n [%]) | |||
| ≥1 chronic condition | 604 (46.2) | 292 (44.4) | 312 (48.1) |
| Respiratory disease | 224 (17.1) | 106 (16.1) | 118 (18.2) |
| Cancer | 53 (4.1) | 30 (4.6) | 23 (3.5) |
| Diabetes | 120 (9.2) | 57 (8.7) | 63 (9.7) |
| Cardiovascular disease | 200 (15.3) | 98 (14.9) | 102 (15.7) |
| Musculoskeletal disorder | 90 (6.9) | 41 (6.2) | 49 (7.6) |
| Other chronic condition | 124 (9.5) | 58 (8.8) | 66 (10.2) |
| MRC dyspnea36 (n=1,305) | |||
| No breathlessness | 359 (27.5) | 177 (26.9) | 182 (28.1) |
| 1 | 523 (40.1) | 264 (40.2) | 259 (40.0) |
| 2 | 318 (24.4) | 167 (25.4) | 151 (23.3) |
| 3 | 75 (5.7) | 34 (5.2) | 41 (6.3) |
| 4 | 19 (1.5) | 9 (1.4) | 10 (1.5) |
| 5 | 11 (0.8) | 6 (0.9) | 5 (0.8) |
| Smoking status | |||
| Currently smoking | 447 (34.2) | 241 (36.6) | 206 (31.7) |
| Currently not smoking | 860 (65.8) | 417 (63.4) | 443 (68.3) |
| Number of cigarettes smoked/day among smokers, n=447 (mean [SD]) | 19.3 (12.1) | 19.0 (12.3) | 19.8 (11.9) |
| FTND score (range 0–10)38 among smokers, n=447 (mean [SD]) | 4.2 (2.3) | 4.1 (2.3) | 4.4 (2.3) |
| Number of previous quit attempts among smokers, n=447 (mean [SD]) | 3.8 (8.8) | 3.1 (4.0) | 4.8 (12.2) |
| Intention to quit smoking (range 1–7) among smokers, n=447 (mean [SD]) | 3.7 (1.9) | 3.7 (2.0) | 3.7 (1.9) |
| Level of physical activity (MET per week), n=1,096 (mean [SD]) | 4,012.6 (3,933.3) | 4,108.7 (4,034.0) | 3,914.1 (3,828.4) |
| Intention to be more physically active (range 1–7) (mean [SD]) | 3.2 (1.7) | 3.2 (1.7) | 3.1 (1.7) |
| CCQ score (range 0–6)37 (mean [SD]) | 1.0 (0.9) | 1.0 (0.9) | 1.0 (0.8) |
Note:
P<0.05.
Abbreviations: CCQ, Clinical COPD Questionnaire; FTND, Fagerström Test for Nicotine Dependence; MET, metabolic equivalent task; MRC, Medical Research Council; RHSQ, Respiratory Health Screening Questionnaire; SD, standard deviation.
More participants were lost to follow-up in the general practice group (46.5%) than in the online group (18.5%) (P<.001), more in the experimental group (22.8%) than in the control group (16%) (P=.002), more smokers (23.7%) than non-smokers (17.2%) (P=.005), and more female (22.6%) than male participants (15.9%) (P=.002). Participants lost to follow-up were also significantly younger (mean =55.9 years) than completing participants (mean =58.1 years) (P<0.001).
Application use
The application was used by 237 (36%) participants of the experimental group (ie, at least one of the six components of a behavior-change module was completed). The average number of components completed by those participants was 2.1 (standard deviation =2.4, range 1–21). For physical activity, 193 (29.3%) of the participants completed at least one intervention component. For smoking cessation, 51 (21.2%) of the smokers at baseline, and seven (1.7%) of the nonsmokers at baseline completed at least one intervention component (although nonsmokers were not included in the effect analyses for smoking cessation). Table 3 shows how many participants completed zero, one, two, or three or more intervention components of both modules.
Table 3.
Number of participants (%) who completed intervention components of the physical activity and smoking cessation modules
| Module | Number of components completed
|
|||
|---|---|---|---|---|
| 0 | 1 | 2 | ≥3 | |
| Physical activity | 465 (70.7) | 107 (16.3) | 48 (7.3) | 38 (5.8) |
| Smoking cessation, among smokers | 190 (78.8) | 29 (12.0) | 12 (5.0) | 10 (4.1) |
Intervention effect
Before correction for baseline characteristics, no significant treatment effect was found for any primary or secondary outcome, except clinical disease control. After correction, all effects were nonsignificant (Table 4).
Table 4.
Effects of the web-based COPD self-management intervention on all primary and secondary outcomes
| Primary and secondary outcomes | Uncorrected effects | Corrected effects |
|---|---|---|
| 7-day point prevalence abstinencea | OR=1.12, (0.45; 2.77*), P=0.810 | OR=1.06, (0.43; 2.66), P=0.895 |
| MET minutes a weekb | b=−64.70, (−455.39; 326.00), P=0.745 | b=−84.33, (−476.39; 307.74), P=0.673 |
| 24-hour point prevalence abstinencea | OR=0.77, (0.36; 1.67), P=0.510 | OR=0.72, (0.33; 1.59), P=0.420 |
| Prolonged abstinencea | OR=0.90, (0.35; 2.34), P=0.834 | OR=0.86, (0.33; 2.25), P=0.766 |
| Continued abstinencea | OR=1.02, (0.39; 2.72), P=0.963 | OR=0.98, (0.37; 2.63), P=0.969 |
| Number of cigarettesc | b=−0.08, (−1.82; 1.65), P=0.925 | b=0.11, (−1.61; 1.84), P=0.899 |
| Intention to quit smokingd | b=−0.01, (−0.31; 0.28), P=0.937 | b=−0.03, (−0.32; 0.26), P=0.826 |
| Number of quit attemptse | b=−0.36, (−1.10; 0.37), P=0.334 | b=−0.38, (−1.11; 0.36), P=0.312 |
| Intention to increase physical activityf | b=0.00, (−0.17; 0.17), P=0.991 | b=0.00, (−0.17; 0.17), P=0.987 |
| Clinical disease controlg | b=−0.06, (−0.11; −0.01), P=0.010 | b=−0.03, (−0.07; 0.01), P=0.134 |
| Dyspnea statush | OR=1.16, (0.89; 1.51), P=0.283 | OR=1.28, (0.92; 1.79), P=0.149 |
Notes:
95% confidence intervals are shown within brackets.
Logistic regression analyses were performed. The corrected analysis only included intention to quit smoking, as including more variables would have overloaded the model. The number of smokers in the general practice group followed up was too small (n=4) to yield reliable results when including recruitment channel in the model.
Linear mixed-model analyses were performed, corrected for age, sex, recruitment channel, smoking status, employment status, comorbidity (yes/no), MRC score, and intention to increase physical activity.
Linear mixed-model analyses were performed, corrected for age, sex, marital status, CCQ score, level of education, MRC score, and FTND score.
Linear mixed-model analyses were performed, corrected for age, sex, level of education, CCQ score, MRC score, number of quit attempts, and employment status.
Linear regression analyses were performed, corrected for age, sex, level of education, CCQ score, MRC score, and FTND score.
Linear mixed-model analyses were performed, corrected for age, sex, recruitment channel, smoking status, employment status, and MRC score.
Linear mixed-model analyses were performed, corrected for age, sex, recruitment channel, smoking status, employment status, COPD status, comorbidity (yes/no), marital status, level of physical activity, MRC score, and level of education.
Logistic regression analyses were performed, corrected for age, sex, recruitment channel, smoking status, employment status, COPD status, comorbidity (yes/no), marital status, level of physical activity, CCQ score, and level of education. Dyspnea status was recoded (0= participants who experienced a form of breathlessness and scored 1–5 on the MRC dyspnea score; 1= participants who indicated to have no breathlessness).
Abbreviations: b, estimated mean difference; CCQ, Clinical COPD Questionnaire; FTND, Fagerström Test for Nicotine Dependence; MET, metabolic equivalent task; MRC, Medical Research Council; OR, odds ratio.
As for sensitivity analyses, similar results were found for the primary outcomes. More specifically, per protocol analyses yielded nonsignificant results for both primary outcomes (Table 5). Regarding physical activity, all interaction terms were nonsignificant. Also, when evaluating for smoking cessation, neither the uncorrected nor corrected effects on 7-day point prevalence abstinence were significant for best- or worst-case scenarios. All subgroup analyses for both outcomes were nonsignificant. Besides, uncorrected and corrected analyses on the behavior-change score, combining the two behaviors, yielded nonsignificant results.
Table 5.
Corrected effects of the per protocol analyses for primary outcomes
| Primary outcomes | At least 1 component completed | At least 2 components completed | At least 3 components completed |
|---|---|---|---|
| 7-day point prevalence abstinencea | OR=1.75, (0.51; 6.00), P=0.371 | OR=3.57, (0.87; 14.73), P=0.078 | No reliable resultsc |
| MET minutes a weekb | b=−101.58, (−653.10; 449.94), P=0.718 | b=120.92, (−683.86; 925.71), P=0.768 | b=813.44, (−383.29; 2,010.17), P=0.182 |
Notes: 95% confidence interval between brackets.
Logistic regression analyses were performed. This analysis did not include covariates due to the small number of events (successful behavior changes).
Linear mixed-model analyses were performed, corrected for age, sex, recruitment channel, smoking status, employment status, comorbidity (yes/no), MRC score, intention to increase physical activity;
no events (successful behavior change) in the experimental group.
Abbreviations: b, estimated mean difference; MET, metabolic equivalent task; OR, odds ratio.
Discussion
This study examined the effects of a computer-tailored COPD self-management intervention. The intervention had no significant impact on the primary outcome measures (physical activity and smoking), or on the secondary outcome measures (intention to change behavior and dyspnea). The only significant effect found was on clinical disease control, but the improvement was too small to have clinical relevance42 and was not significant after correction for relevant baseline characteristics. Moreover, a borderline significant effect for smoking was found when analyzing the effects among those who completed at least two intervention components. Also, the effect size, for both smoking and physical activity, increased as more intervention components were used. Yet, possibly due to the sample size and thus decreased power of the study, these analyses did not yield a significant effect.
Possible explanations for the lack of effect may be: (a) low exposure to the intervention, (b) that the intervention method was not sufficient for our target population, and (c) inadequate content of the intervention itself. Although it was not significant, the trend was for an increased effect size as the participants completed more of the six intervention components. This helps verify the importance of exposure to the application and correlates with other studies which have shown that this is essential for the effectiveness of such interventions.43,44 To enhance exposure to the intervention, we used different strategies to attract participants to the application: sending email prompts every 2 weeks, of which some referred to new content on the website, as this has been shown to effectively increase application use;28 including multiple feedback moments to evaluate participants’ behavior and track their goal achievement;45,46 prompting revisits to the application and evaluate these previously set goals; and embedding a website that provided regular news updates,45–47 such as behavioral journalism stories,48 which were personal stories addressing how other patients overcame potential barriers to use the application and improve their health behavior. Additionally, since the length of the program was of concern in the pilot study,17 we separated the two modules (smoking cessation and physical activity) into six small components, giving participants the opportunity to decide which components they wanted to complete, and consequently, how much time they wanted to spend working with the application. Unfortunately, only one out of three participants completed one or more of the six intervention components. In hindsight, giving participants an option to choose intervention components based on the results of our pilot study was probably not desirable, since it has recently been shown that less freedom of navigation on a website enhances application use.49,50 The intervention did not include ongoing peer or counselor support (eg, by a practice nurse) which could have improved the exposure to the application.47
Another potential cause for our study results could be that the intervention method was not sufficient for our target population. Although similar computer-tailoring approaches have found significant effects among the general population,11,14,25,26 several other studies reported a relatively low success rate of disease-management programs for COPD patients51–53 and found that COPD patients are more likely to have characteristics that are associated with a higher resistance to smoking cessation interventions54 than other target populations. Negative results are not uncommon in COPD self-management studies according to a systematic review by Jonsdottir.5 The author describes the need for a paradigm shift in which a prominent health professional-centered approach should make way for a patient-family-centered approach with emphasis on the relationship with the health care professional. As we were aware of this, the MasterYourBreath intervention was patient-centered, and social influence of family members was addressed in the intervention. However, the application did not enable the active participation of family members. An improvement to future versions could be to integrate the MasterYourBreath intervention with a social media platform to facilitate engagement of the family members in the patient’s self-management process. The relationship with the health care professional was indeed emphasized in the original version of the MasterYourBreath intervention, by integration of the application in primary care, but recruiting the number of participants necessary for an RCT from primary care practices was found to be unfeasible in the pilot study,17 so the original study design was changed.
Another possible cause for the lack of effect could be related to the web-based intervention content itself. We used key behavioral determinants that were experimentally tested in the Dutch population but not validated for COPD patients. The usability study in which we adjusted these determinants for COPD patients16 is not a replacement for a validation study. Behavioral determinants for this specific group might be different from the general Dutch population. For example, COPD patients are likely to experience different barriers to physical activity due to disease complications. Moreover, the main difference we found comparing our application to programs that were very similar but found positive intervention effects11,14,25,26,43,55 was that participants in our study were free to choose which intervention components they wanted to complete. These other programs contained similar tailored messages, but directed participants through a specified intervention pathway. As described previously, this strategy might increase exposure, as it limits freedom of navigation. Instead of shortening the intervention content by tailoring the use of components to user’s preference,10 it may have been more effective to offer participants only components adapted to their level of motivation to change their behavior; Stanczyk et al55 found this strategy effective. Peels et al56 tested a web-based basic version of their program and a version in which they added additional environmental information with links to other resources to increase physical activity in adults aged 50 and over. They found that only the latter was not effective. The authors suspected that participants might have been distracted from the intervention pathway by visiting other resources. Likewise, the provision of additional information and self-management resources in the MasterYourBreath application, including home exercises and links to other websites might have decreased a potential intervention effect, as these could have distracted participants from the intervention components, which was the core content of the intervention.
Limitations
Our study had several limitations. First, despite our relatively large sample of participants, compared to many other COPD self-management studies,5 our study still lacked power concerning the primary outcome for smoking cessation. The number of smokers at the start of the study was lower than expected, and loss to follow-up among smokers was higher than among nonsmokers.
Second, we were not able to evaluate selection bias, because we could not collect additional data to differentiate between participants who enrolled versus those who declined participation. The clinical information that would help us address selection bias was not available from the online recruiting company.
Third, the inclusion of people at risk for COPD may make it more difficult to compare our results with self-management studies that include only COPD patients. However, we argue that including individuals at risk for COPD is clinically relevant, since early smoking cessation is pivotally important for a greater health benefit in COPD.57 Including both diagnosed patients and individuals at risk for COPD also poses a methodological challenge, since these groups may benefit from different interventions. However, the approach to care in the MasterYourBreath program has been tailored to varying levels of COPD (risk), and thus it was able to address differing patient needs.
Fourth, while our intentions were to do so, we were not able to integrate the MasterYourBreath intervention into the Dutch COPD disease-management approach,18 due to recruitment issues.17 We know that it is important that COPD self-management interventions can be incorporated in an existing health care structure.58–60 The recruitment strategy used in this RCT (including an online group and individuals at risk for COPD) was certainly beneficial for the sample size of our RCT, but hampered the integration of our intervention in primary care.
Conclusion
MasterYourBreath, a web-based COPD self-management intervention with tailored feedback, did not show statistically significant effects on health-related behavioral or clinical outcomes. Given the structurally low exposure to the application in this study, we believe more research is needed to find effective strategies to increase the use of the web-based applications by COPD patients. To further explain this phenomenon and to generate hypotheses for better strategies, we will reevaluate our RCT and explore in depth the characteristics of the intervention and the participants that may have contributed to the use and appreciation of the application.
Acknowledgments
The authors would like to thank Onno van Schayck, PhD, for his assistance with the study design; Jos Dirven, MD, for his contribution to participant recruitment; and Jean Muris, PhD, for screening feedback messages on content and providing advice as a COPD specialist. The authors also thank the University of Oklahoma, Health Sciences Center, for providing an office; James W Mold, MD, MPH, for providing general support; and E Wickersham, MD, for editing the manuscript. This study was funded by ZonMw, the Netherlands Organization for Health Research and Development.
Footnotes
Disclosure
Hein de Vries is scientific director of Vision2Health, a company that licenses evidence-based innovative computer- tailored health-communication tools. The other authors declare that they have no competing interests in this work.
References
- 1.Viegi G, Pistelli F, Sherrill DL, Maio S, Baldacci S, Carrozzi L. Definition, epidemiology and natural history of COPD. Eur Respir J. 2007;30(5):993–1013. doi: 10.1183/09031936.00082507. [DOI] [PubMed] [Google Scholar]
- 2.Siafakas NM, Vermeire P, Pride NB, et al. Optimal assessment and management of chronic obstructive pulmonary disease (COPD). The European Respiratory Society Task Force. Eur Respir J. 1995;8(8):1398–1420. doi: 10.1183/09031936.95.08081398. [DOI] [PubMed] [Google Scholar]
- 3.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 4.Bourbeau J, Nault D, Dang-Tan T. Self-management and behaviour modification in COPD. Patient Educ Couns. 2004;52(3):271–277. doi: 10.1016/S0738-3991(03)00102-2. [DOI] [PubMed] [Google Scholar]
- 5.Jonsdottir H. Self-management programmes for people living with chronic obstructive pulmonary disease: a call for a reconceptualisation. J Clin Nurs. 2013;22(5–6):621–637. doi: 10.1111/jocn.12100. [DOI] [PubMed] [Google Scholar]
- 6.Evers KE. eHealth promotion: the use of the Internet for health promotion. Am J Health Promot. 2006;20(4):Suppl 1–7. doi: 10.4278/0890-1171-20.4.1. [DOI] [PubMed] [Google Scholar]
- 7.Lustria ML, Cortese J, Noar SM, Glueckauf RL. Computer-tailored health interventions delivered over the Web: review and analysis of key components. Patient Educ Couns. 2009;74(2):156–173. doi: 10.1016/j.pec.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3–4):214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Vries H, Brug J. Computer-tailored interventions motivating people to adopt health promoting behaviours: introduction to a new approach. Patient Educ Couns. 1999;36(2):99–195. doi: 10.1016/s0738-3991(98)00127-x. [DOI] [PubMed] [Google Scholar]
- 10.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008;23(3):454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Vries H, Kremers SP, Smeets T, Brug J, Eijmael K. The effectiveness of tailored feedback and action plans in an intervention addressing multiple health behaviors. Am J Health Promot. 2008;22(6):417–425. doi: 10.4278/ajhp.22.6.417. [DOI] [PubMed] [Google Scholar]
- 12.Dijkstra A. Working mechanisms of computer-tailored health education: evidence from smoking cessation. Health Educ Res. 2005;20(5):527–539. doi: 10.1093/her/cyh014. [DOI] [PubMed] [Google Scholar]
- 13.Smeets T, Brug J, de Vries H. Effects of tailoring health messages on physical activity. Health Educ Res. 2008;23(3):402–413. doi: 10.1093/her/cyl101. [DOI] [PubMed] [Google Scholar]
- 14.Smit ES, de Vries H, Hoving C. Effectiveness of a Web-based multiple tailored smoking cessation program: a randomized controlled trial among Dutch adult smokers. J Med Internet Res. 2012;14(3):e82. doi: 10.2196/jmir.1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smit ES, Evers SM, de Vries H, Hoving C. Cost-effectiveness and cost-utility of Internet-based computer tailoring for smoking cessation. J Med Internet Res. 2013;15(3):e57. doi: 10.2196/jmir.2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Voncken-Brewster V, Moser A, van der Weijden T, Nagykaldi Z, de Vries H, Tange H. Usability evaluation of an online, tailored self-management intervention for chronic obstructive pulmonary disease patients incorporating behavior change techniques. JMIR Res Protoc. 2013;2(1):e3. doi: 10.2196/resprot.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voncken-Brewster V, Tange H, Moser A, Nagykaldi Z, de Vries H, van der Weijden T. Integrating a tailored e-health self-management application for chronic obstructive pulmonary disease patients into primary care: a pilot study. BMC Fam Pract. 2014;15:4. doi: 10.1186/1471-2296-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steuten L, Vrijhoef B, Van Merode F, Wesseling GJ, Spreeuwenberg C. Evaluation of a regional disease management programme for patients with asthma or chronic obstructive pulmonary disease. Int J Qual Health Care. 2006;18(6):429–436. doi: 10.1093/intqhc/mzl052. [DOI] [PubMed] [Google Scholar]
- 19.Price DB, Tinkelman DG, Halbert RJ, et al. Symptom-based questionnaire for identifying COPD in smokers. Respiration. 2006;73(3):285–295. doi: 10.1159/000090142. [DOI] [PubMed] [Google Scholar]
- 20.Price DB, Tinkelman DG, Nordyke RJ, Isonaka S, Halbert RJ, COPD Questionnaire Study Group Scoring system and clinical application of COPD diagnostic questionnaires. Chest. 2006;129(6):1531–1539. doi: 10.1378/chest.129.6.1531. [DOI] [PubMed] [Google Scholar]
- 21.Dirven JA, Tange HJ, Muris JW, van Haaren KM, Vink G, van Schayck OC. Early detection of COPD in general practice: patient or practice managed? A randomised controlled trial of two strategies in different socioeconomic environments. Prim Care Respir J. 2013;22(3):331–337. doi: 10.4104/pcrj.2013.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Voncken-Brewster V, Tange H, de Vries H, Nagykaldi Z, Winkens B, van der Weijden T. A randomised controlled trial testing a web-based, computer-tailored self-management intervention for people with or at risk for chronic obstructive pulmonary disease: a study protocol. BMC Public Health. 2013;13:557. doi: 10.1186/1471-2458-13-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zelen M. The randomization and stratification of patients to clinical trials. J Chron Dis. 1974;27(7–8):365–375. doi: 10.1016/0021-9681(74)90015-0. [DOI] [PubMed] [Google Scholar]
- 24.Schulz DN, Smit ES, Stanczyk NE, Kremers SP, de Vries H, Evers SM. Economic evaluation of a web-based tailored lifestyle intervention for adults: findings regarding cost-effectiveness and cost-utility from a randomized controlled trial. J Med Internet Res. 2014;16(3):e91. doi: 10.2196/jmir.3159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smeets T, Kremers SPJ, Brug J, De Vries H. Effects of tailored feedback on multiple health behaviors. Ann Behav Med. 2007;33(2):117–123. doi: 10.1007/BF02879892. [DOI] [PubMed] [Google Scholar]
- 26.Schulz DN, Kremers SP, Vandelanotte C, et al. Effects of a web-based tailored multiple-lifestyle intervention for adults: a two-year randomized controlled trial comparing sequential and simultaneous delivery modes. J Med Internet Res. 2014;16(1):e26. doi: 10.2196/jmir.3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res. 2009;11(2):e16. doi: 10.2196/jmir.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schneider F, de Vries H, Candel M, van de Kar A, van Osch L. Periodic email prompts to re-use an internet-delivered computer-tailored lifestyle program: influence of prompt content and timing. J Med Internet Res. 2013;15(1):e23. doi: 10.2196/jmir.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Vries H, Mesters I, van de Steeg H, Honing C. The general public’s information needs and perceptions regarding hereditary cancer: an application of the Integrated Change Model. Patient Educ Couns. 2005;56(2):154–165. doi: 10.1016/j.pec.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 30.de Vries H, Eggers SM, Bolman C. The role of action planning and plan enactment for smoking cessation. BMC Public Health. 2013;13:393. doi: 10.1186/1471-2458-13-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dijkstra A, De Vries H, Roijackers J. Long-term effectiveness of computer-generated tailored feedback in smoking cessation. Health Educ Res. 1998;13(2):207–214. doi: 10.1093/her/13.2.207. [DOI] [PubMed] [Google Scholar]
- 32.Dijkstra A, de Vries H, Bakker M. Pros and cons of quitting, self-efficacy, and the stages of change in smoking cessation. J Consult Clin Psychol. 1996;64(4):758–763. doi: 10.1037//0022-006x.64.4.758. [DOI] [PubMed] [Google Scholar]
- 33.West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100(3):299–303. doi: 10.1111/j.1360-0443.2004.00995.x. [DOI] [PubMed] [Google Scholar]
- 34.Mudde AN, Willemsen MC, Kremers S, de Vries H. Meetinstrumenten voor onderzoek naar roken en stoppen met roken [Measurements for research on smoking and smoking cessation] 2nd ed. The Hague: Stivoro; 2006. Dutch. [Google Scholar]
- 35.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 36.Bestall J, Paul E, Garrod R, Garnham R, Jones P, Wedzicha J. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Molen T, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes. 2003;1:13. doi: 10.1186/1477-7525-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 39.Dupont WD, Plummer WD., Jr Power and sample size calculations. A review and computer program. Control Clin Trials. 1990;11(2):116–128. doi: 10.1016/0197-2456(90)90005-m. [DOI] [PubMed] [Google Scholar]
- 40.Dirven JA, Muris JW, van Schayck CP. COPD screening in general practice using a telephone questionnaire. COPD. 2010;7(5):352–359. doi: 10.3109/15412555.2010.510547. [DOI] [PubMed] [Google Scholar]
- 41.Rütten A, Ziemainz H, Schena F, et al. Using different physical activity measurements in eight European countries. Results of the European Physical Activity Surveillance System (EUPASS) time series survey. Public Health Nutr. 2003;6(4):371–376. doi: 10.1079/PHN2002450. [DOI] [PubMed] [Google Scholar]
- 42.Kocks JW, Tuinenga MG, Uil SM, van den Berg JW, Ståhl E, van der Molen T. Health status measurement in COPD: the minimal clinically important difference of the clinical COPD questionnaire. Respir Res. 2006;7:62. doi: 10.1186/1465-9921-7-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elfeddali I, Bolman C, Candel MJ, Wiers RW, de Vries H. Preventing smoking relapse via Web-based computer-tailored feedback: a randomized controlled trial. J Med Internet Res. 2012;14(4):e109. doi: 10.2196/jmir.2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strecher VJ, McClure J, Alexander G, et al. The role of engagement in a tailored web-based smoking cessation program: randomized controlled trial. J Med Internet Res. 2008;10(5):e36. doi: 10.2196/jmir.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brouwer W, Oenema A, Crutzen R, de Nooijer J, de Vries N, Brug J. What makes people decide to visit and use an internet-delivered behavior-change intervention? A qualitative study among adults. Health Educ. 2009;109(6):460–473. [Google Scholar]
- 46.Brouwer W, Oenema A, Crutzen R, de Nooijer J, de Vries NK, Brug J. An exploration of factors related to dissemination of and exposure to internet-delivered behavior change interventions aimed at adults: a Delphi study approach. J Med Internet Res. 2008;10(2):e10. doi: 10.2196/jmir.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brouwer W, Kroeze W, Crutzen R, et al. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J Med Internet Res. 2011;13(1):e2. doi: 10.2196/jmir.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McAlister A. Behavioral journalism: beyond the marketing model for health communication. Am J Health Promot. 1995;9(6):417–420. doi: 10.4278/0890-1171-9.6.417. [DOI] [PubMed] [Google Scholar]
- 49.Crutzen R, Cyr D, de Vries NK. The role of user control in adherence to and knowledge gained from a website: randomized comparison between a tunneled version and a freedom-of-choice version. J Med Internet Res. 2012;14(2):e45. doi: 10.2196/jmir.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McClure JB, Shortreed SM, Bogart A, et al. The effect of program design on engagement with an internet-based smoking intervention: randomized factorial trial. J Med Internet Res. 2013;15(3):e69. doi: 10.2196/jmir.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness-which ones work? Meta-analysis of published reports. BMJ. 2002;325(7370):925. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ofman JJ, Badamgarav E, Henning JM, et al. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. Am J Med. 2004;117(3):182–192. doi: 10.1016/j.amjmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 53.Mattke S, Seid M, Ma S. Evidence for the effect of disease management: is $1 billion a year a good investment? Am J Manag Care. 2007;13(12):670–676. [PubMed] [Google Scholar]
- 54.Jiménez-Ruiz CA, Masa F, Miravitlles M, et al. Smoking characteristics: differences in attitudes and dependence between healthy smokers and smokers with COPD. Chest. 2001;119(5):1365–1370. doi: 10.1378/chest.119.5.1365. [DOI] [PubMed] [Google Scholar]
- 55.Stanczyk N, Bolman C, van Adrichem M, Candel M, Muris J, de Vries H. Comparison of text and video computer-tailored interventions for smoking cessation: randomized controlled trial. J Med Internet Res. 2014;16(3):e69. doi: 10.2196/jmir.3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peels DA, van Stralen MM, Bolman C, et al. The differentiated effectiveness of a printed versus a Web-based tailored physical activity intervention among adults aged over 50. Health Educ Res. 2014;29(5):870–882. doi: 10.1093/her/cyu039. [DOI] [PubMed] [Google Scholar]
- 57.Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977;1(6077):1645–1648. doi: 10.1136/bmj.1.6077.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Effing T, van der Palen J, Frith P. Education in COPD self-management: only part of the game. Respirology. 2014;19(2):151–152. doi: 10.1111/resp.12231. [DOI] [PubMed] [Google Scholar]
- 59.Effing TW, Bourbeau J, Vercoulen J, et al. Self-management programmes for COPD: moving forward. Chron Respir Dis. 2012;9(1):27–35. doi: 10.1177/1479972311433574. [DOI] [PubMed] [Google Scholar]
- 60.Adams SG, Smith PK, Allan PF, Anzueto A, Pugh JA, Cornell JE. Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167(6):551–561. doi: 10.1001/archinte.167.6.551. [DOI] [PubMed] [Google Scholar]
- 61.Wilson JS, Elborn JS, Fitzsimons D, McCrum-Gardner E. Do smokers with chronic obstructive pulmonary disease report their smoking status reliably? A comparison of self-report and bio-chemical validation. Int J Nurs Stud. 2011;48(7):856–862. doi: 10.1016/j.ijnurstu.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 62.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 63.Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42(10):773–778. doi: 10.1136/thx.42.10.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lincoln NB, Gladman JR. The Extended Activities of Daily Living scale: a further validation. Disabil Rehabil. 1992;14(1):41–43. doi: 10.3109/09638289209166426. [DOI] [PubMed] [Google Scholar]
- 65.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 66.Smit ES, Hoving C, Schelleman-Offermans K, West R, de Vries H. Predictors of successful and unsuccessful quit attempts among smokers motivated to quit. Addict Behav. 2014;39(9):1318–1324. doi: 10.1016/j.addbeh.2014.04.017. [DOI] [PubMed] [Google Scholar]